FINGOLIMOD HYDROCHLORIDE capsule
FINGOLIMOD HYDROCHLORIDE by
Drug Labeling and Warnings
FINGOLIMOD HYDROCHLORIDE by is a Prescription medication manufactured, distributed, or labeled by Accord Healthcare Inc., Intas Pharmaceuticals Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use FINGOLIMOD CAPSULES safely and effectively. See full prescribing information for FINGOLIMOD CAPSULES.
FINGOLIMOD capsules, for oral use
Initial U.S. Approval: 2010INDICATIONS AND USAGE
Fingolimod hydrochloride is a sphingosine 1-phosphate receptor modulator indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in patients 10 years of age and older. ( 1)
DOSAGE AND ADMINISTRATION
- Assessments are required prior to initiating fingolimod. ( 2.1)
- Recommended dosage for adults and pediatric patients (10 years of age and older) weighing more than 40 kg: 0.5 mg orally once-daily, with or without food. ( 2.2, 2.3)
- First-Dose Monitoring (including reinitiation after discontinuation greater than 14 days and dose increases):
- Observe all patients for bradycardia for at least 6 hours; monitor pulse and blood pressure hourly. Electrocardiograms (ECGs) prior to dosing and at end of observation period required. ( 2.4)
- Monitor until resolution if heart rate <45 beats per minute (bpm) in adults, < 55 bpm in patients aged 12 years and above, or < 60 bpm in pediatric patients aged 10 to below 12 years,atrioventricular (AV) block, or if lowest postdose heart rate is at the end of the observation period. ( 2.4)
- Monitor symptomatic bradycardia with ECG until resolved. Continue overnight if intervention is required; repeat first-dose monitoring for second dose. ( 2.4)
- Observe patients overnight if at higher risk of symptomatic bradycardia, heart block, prolonged QTc interval, or if taking drugs with known risk of torsades de pointes. ( 2.4, 7.1)
DOSAGE FORMS AND STRENGTHS
0.5 mg hard capsules ( 3)
CONTRAINDICATIONS
- Recent myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure with hospitalization, or Class III/IV heart failure. ( 4)
- History of Mobitz Type II 2 nddegree or 3 rddegree AV block or sick sinus syndrome, unless patient has a pacemaker. ( 4)
- Baseline QTc interval ≥500 msec. ( 4)
- Cardiac arrhythmias requiring anti-arrhythmic treatment with Class Ia or Class III anti-arrhythmic drugs. ( 4)
- Hypersensitivity to fingolimod or its excipients. ( 4)
WARNINGS AND PRECAUTIONS
- Infections:Fingolimod hydrochloride may increase the risk. Obtain a complete blood count (CBC) before initiating treatment. Monitor for infection during treatment and for 2 months after discontinuation. Do not start in patients with active infections. ( 5.2)
- Progressive Multifocal Leukoencephalopathy (PML):Withhold fingolimod hydrochloride at the first sign or symptom suggestive of PML. ( 5.3)
- Macular Edema:Examine the fundus before and 3 to 4 months after treatment start. Diabetes mellitus and uveitis increase the risk. ( 5.4)
- Liver Injury:Obtain liver enzyme results before initiation and periodically during treatment. Closely monitor patients with severe hepatic impairment. Discontinue if there is evidence of liver injury without other cause. ( 5.5, 8.6, 12.3)
- Posterior Reversible Encephalopathy Syndrome (PRES):If suspected, discontinue fingolimod hydrochloride. ( 5.6)
- Respiratory Effects:Evaluate when clinically indicated. ( 5.7)
- Fetal Risk:May cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and to use an effective method of contraception during treatment and for 2 months after stopping fingolimod hydrochloride. ( 5.8, 8.1, 8.3)
- Severe Increase in Disability After Stopping Fingolimod Hydrochloride:Monitor for development of severe increase in disability following discontinuation and begin appropriate treatment as needed. ( 5.9)
- Tumefactive MS:Consider when severe MS relapse occurs during treatment or after discontinuation. Obtain imaging and begin treatment as needed. ( 5.10)
- Increased Blood Pressure (BP):Monitor BP during treatment. ( 5.11)
- Malignancies:Suspicious skin lesions should be evaluated. ( 5.12)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥10% and greater than placebo): Headache, liver transaminase elevation, diarrhea, cough, influenza, sinusitis, back pain, abdominal pain, and pain in extremity ( 6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Accord Healthcare Inc. at 1-866-941-7875 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 2/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Assessment Prior to Initiating Fingolimod Capsules
2.2 Important Administration Instructions
2.3 Recommended Dosage
2.4 First-Dose Monitoring
2.5 Monitoring After Reinitiation of Therapy Following Discontinuation
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Bradyarrhythmia and Atrioventricular Blocks
5.2 Infections
5.3 Progressive Multifocal Leukoencephalopathy
5.4 Macular Edema
5.5 Liver Injury
5.6 Posterior Reversible Encephalopathy Syndrome
5.7 Respiratory Effects
5.8 Fetal Risk
5.9 Severe Increase in Disability After Stopping Fingolimod Hydrochloride
5.10 Tumefactive Multiple Sclerosis
5.11 Increased Blood Pressure
5.12 Malignancies
5.13 Immune System Effects Following Fingolimod Hydrochloride Discontinuation
5.14 Hypersensitivity Reactions
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 QT Prolonging Drugs
7.2 Ketoconazole
7.3 Vaccines
7.4 Antineoplastic, Immunosuppressive, or Immune-Modulating Therapies
7.5 Drugs That Slow Heart Rate or Atrioventricular Conduction (e.g., beta blockers or diltiazem)
7.6 Laboratory Test Interaction
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Adults
14.2 Pediatric Patients (10 to less than 18 Years of Age)
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Assessment Prior to Initiating Fingolimod Capsules
Cardiac Evaluation
Obtain a cardiac evaluation in patients with certain preexisting conditions [ see Warnings and Precautions (5.1)] Prior to starting treatment, determine whether patients are taking drugs that could slow heart rate or atrioventricular (AV) conduction [ see Dosage and Administration (2.4), Drug Interactions (7.5)]
Complete Blood Count (CBC)
Review results of a recent CBC [ see Warnings and Precautions (5.2), Drug Interactions (7.6)]
Serum Transaminases (ALT and AST) and Total Bilirubin Levels
Prior to starting treatment with fingolimod capsules (i.e., within 6 months), obtain serum transaminases [alanine transaminase (ALT) and aspartate transferase (AST)] and total bilirubin levels [see Warnings and Precautions (5.5)] .Prior Medications
If patients are taking antineoplastic, immunosuppressive, or immune-modulating therapies, or if there is a history of prior use of these drugs, consider possible unintended additive immunosuppressive effects before initiating treatment with fingolimod capsules[ see Warnings and Precautions (5.2), Drug Interactions (7.4)]
Vaccinations
Test patients for antibodies to varicella zoster virus (VZV) before initiating fingolimod capsules; VZV vaccination of antibody-negative patients is recommended prior to commencing treatment with fingolimod capsules[ see Warnings and Precautions (5.2).] It is recommended that pediatric patients if possible, complete all immunizations in accordance with current immunization guidelines prior to initiating fingolimod capsules therapy.
2.2 Important Administration Instructions
Patients who initiate fingolimod capsules, and those who reinitiate treatment after discontinuation for longer than 14 days, require first-dose monitoring. This monitoring is also recommended when the dose is increased in pediatric patients.[ see Dosage and Administration (2.4,2.5)]
Fingolimod capsules can be taken with or without food.
2.3 Recommended Dosage
In adults and pediatric patients 10 years of age and older weighing more than 40 kg, the recommended dosage of fingolimod capsules is 0.5 mg orally once-daily.
Fingolimod doses higher than 0.5 mg are associated with a greater incidence of adverse reactions without additional benefit.
2.4 First-Dose Monitoring
Initiation of fingolimod capsules treatment results in a decrease in heart rate, for which monitoring is recommended [ see Warnings and Precautions (5.1), Clinical Pharmacology (12.2)]. Prior to dosing and at the end of the observation period, obtain an electrocardiogram (ECG) in all patients.
First 6-Hour Monitoring
Administer the first dose of fingolimod capsules in a setting in which resources to appropriately manage symptomatic bradycardia are available. Monitor all patients for 6 hours after the first dose for signs and symptoms of bradycardia with hourly pulse and blood pressure measurement.
Additional Monitoring After 6-Hour Monitoring
Continue monitoring until the abnormality resolves if any of the following is present (even in the absence of symptoms) after 6 hours:
- the heart rate 6 hours postdose is less than 45 beats per minute (bpm) in adults, less than 55 bpm in pediatric patients 12 years of age and older, or less than 60 bpm in pediatric patients 10 or 11 years of age;
- the heart rate 6 hours postdose is at the lowest value postdose suggesting that the maximum pharmacodynamic effect on the heart may not have occurred;
- the ECG 6 hours postdose shows new onset second degree or higher atrioventricular (AV) block;
If postdose symptomatic bradycardia occurs, initiate appropriate management, begin continuous ECG monitoring, and continue monitoring until the symptoms have resolved if no pharmacological treatment is required. If pharmacological treatment is required, continue monitoring overnight and repeat 6-hour monitoring after the second dose.
Overnight Monitoring
Continuous overnight ECG monitoring in a medical facility should be instituted:
- in patients that require pharmacologic intervention for symptomatic bradycardia. In these patients, the first-dose monitoring strategy should be repeated after the second dose of fingolimod capsules;
- in patients with some preexisting heart and cerebrovascular conditions [ see Warnings and Precautions (5.1)];
- in patients with a prolonged QTc interval before dosing or during 6 -hour observation, or at additional risk for QT prolongation, or on concurrent therapy with QT prolonging drugs with a known risk of torsades de pointes [ see Warnings and Precautions (5.1), Drug Interactions (7.1)];
- in patients receiving concurrent therapy with drugs that slow heart rate or AV conduction [ see Drug Interactions (7.5)].
2.5 Monitoring After Reinitiation of Therapy Following Discontinuation
When restarting fingolimod capsules after discontinuation for more than 14 days after the first month of treatment, perform first-dose monitoring, because effects on heart rate and AV conduction may recur on reintroduction of fingolimod capsules treatment [ see Dosage and Administration (2.4)]. The same precautions (first-dose monitoring) as for initial dosing are applicable. Within the first 2 weeks of treatment, first-dose procedures are recommended after interruption of 1 day or more; during Weeks 3 and 4 of treatment, first-dose procedures are recommended after treatment interruption of more than 7 days.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Fingolimod capsules are contraindicated in patients who have:
- in the last 6 months experienced myocardial infarction, unstable angina, stroke, transient ischemic attack (TIA), decompensated heart failure requiring hospitalization or Class III/IV heart failure
- a history or presence of Mobitz Type II second-degree or third-degree AV block or sick sinus syndrome, unless patient has a functioning pacemaker [ see Warnings and Precautions (5.1)]
- a baseline QTc interval ≥500 msec
- cardiac arrhythmias requiring anti-arrhythmic treatment with Class Ia or Class III anti-arrhythmic drugs
- had a hypersensitivity reaction to fingolimod or any of the excipients in fingolimod capsules. Observed reactions include rash, urticaria and angioedema upon treatment initiation. [see Warnings and Precautions (5.14)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Bradyarrhythmia and Atrioventricular Blocks
Because of a risk for bradyarrhythmia and AV blocks, patients should be monitored during fingolimod hydrochloride treatment initiation [ see Dosage and Administration (2.4)].
Reduction in Heart Rate
After the first dose of fingolimod hydrochloride, the heart rate decrease starts within an hour. On Day 1, the maximum decline in heart rate generally occurs within 6 hours and recovers, although not to baseline levels, by 8 to 10 hours postdose. Because of physiological diurnal variation, there is a second period of heart rate decrease within 24 hours after the first dose. In some patients, heart rate decrease during the second period is more pronounced than the decrease observed in the first 6 hours. Heart rates below 40 bpm in adults, and below 50 bpm in pediatric patients occurred rarely. In controlled clinical trials in adult patients, adverse reactions of symptomatic bradycardia following the first dose were reported in 0.6% of patients receiving fingolimod hydrochloride 0.5 mg, and in 0.1% of patients on placebo. Patients who experienced bradycardia were generally asymptomatic, but some patients experienced hypotension, dizziness, fatigue, palpitations, and/or chest pain that usually resolved within the first 24 hours on treatment.
Patients with some preexisting conditions (e.g., ischemic heart disease, history of myocardial infarction, congestive heart failure, history of cardiac arrest, cerebrovascular disease, uncontrolled hypertension, history of symptomatic bradycardia, history of recurrent syncope, severe untreated sleep apnea, AV block, sinoatrial heart block) may poorly tolerate the fingolimod hydrochloride-induced bradycardia, or experience serious rhythm disturbances after the first dose of fingolimod hydrochloride. Prior to treatment with fingolimod hydrochloride, these patients should have a cardiac evaluation by a physician appropriately trained to conduct such evaluation, and if treated with fingolimod hydrochloride, should be monitored overnight with continuous ECG in a medical facility after the first dose.
Since initiation of fingolimod hydrochloride treatment, results in decreased heart rate and may prolong the QT interval, patients with a prolonged QTc interval (>450 msec adult and pediatric males, >470 msec adult females, or >460 msec pediatric females) before dosing or during 6-hour observation, or at additional risk for QT prolongation (e.g., hypokalemia, hypomagnesemia, congenital long-QT syndrome), or on concurrent therapy with QT prolonging drugs with a known risk of torsades de pointes (e.g., citalopram, chlorpromazine, haloperidol, methadone, erythromycin) should be monitored overnight with continuous ECG in a medical facility.
Following the second dose, a further decrease in heart rate may occur when compared to the heart rate prior to the second dose, but this change is of a smaller magnitude than that observed following the first dose. With continued dosing, the heart rate returns to baseline within 1 month of chronic treatment. Clinical data indicate effects of fingolimod hydrochloride on heart rate are maximal after the first dose although milder effects on heart rate may persist for, on average, 2 to 4 weeks after initiation of therapy at which time heart rate generally returns to baseline. Physicians should continue to be alert to patient reports of cardiac symptoms.
Atrioventricular Blocks
Initiation of fingolimod hydrochloride treatment has resulted in transient AV conduction delays. In controlled clinical trials in adult patients, first-degree AV block after the first dose occurred in 4.7% of patients receiving fingolimod hydrochloride and 1.6% of patients on placebo. In a study of 697 patients with available 24-hour Holter monitoring data after their first dose (N=351 receiving fingolimod hydrochloride and N=346 on placebo), second-degree AV blocks (Mobitz Types I [Wenckebach] or 2:1 AV blocks) occurred in 4% (N=14) of patients receiving fingolimod hydrochloride and 2% (N=7) of patients on placebo. Of the 14 patients receiving fingolimod capsules, 7 patients had 2:1 AV block (5 patients within the first 6 hours postdose and 2 patients after 6 hours postdose). All second degree AV blocks on placebo were Mobitz Type I and occurred after the first 12 hours postdose. The conduction abnormalities were usually transient and asymptomatic, and resolved within the first 24 hours on treatment, but they occasionally required treatment with atropine or isoproterenol.
Postmarketing Experience
In the postmarketing setting, third-degree AV block and AV block with junctional escape have been observed during the first-dose 6-hour observation period with fingolimod hydrochloride. Isolated delayed onset events, including transient asystole and unexplained death, have occurred within 24 hours of the first dose. These events were confounded by concomitant medications and/or preexisting disease, and the relationship to fingolimod hydrochloride is uncertain. Cases of syncope were also reported after the first dose of fingolimod hydrochloride.
5.2 Infections
Risk of Infections
Fingolimod hydrochloride causes a dose-dependent reduction in peripheral lymphocyte count to 20% to 30% of baseline values because of reversible sequestration of lymphocytes in lymphoid tissues. Fingolimod hydrochloride may therefore increase the risk of infections, some serious in nature [ see Clinical Pharmacology (12.2)]. Life-threatening and fatal infections have occurred in association with fingolimod hydrochloride.
Before initiating treatment with fingolimod hydrochloride, a recent CBC (i.e., within 6 months or after discontinuation of prior therapy) should be available. Consider suspending treatment with fingolimod hydrochloride if a patient develops a serious infection, and reassess the benefits and risks prior to reinitiation of therapy. Because the elimination of fingolimod after discontinuation may take up to 2 months, continue monitoring for infections throughout this period. Instruct patients receiving fingolimod capsules to report symptoms of infections to a physician. Patients with active acute or chronic infections should not start treatment until the infection(s) is resolved.
In MS placebo-controlled trials in adult patients, the overall rate of infections (72%) with fingolimod hydrochloride was similar to placebo. However, bronchitis, herpes zoster, influenza, sinusitis, and pneumonia were more common in fingolimod hydrochloride-treated patients. Serious infections occurred at a rate of 2.3% in the fingolimod hydrochloride group versus 1.6% in the placebo group.
In the postmarketing setting, serious infections with opportunistic pathogens including viruses (e.g., John Cunningham virus [JCV], herpes simplex viruses 1 and 2, varicella zoster virus), fungi (e.g., cryptococci), and bacteria (e.g., atypical mycobacteria) have been reported with fingolimod hydrochloride. Patients with symptoms and signs consistent with any of these infections should undergo prompt diagnostic evaluation and appropriate treatment.
Herpes Viral Infections
In placebo-controlled trials in adult patients, the rate of herpetic infections was 9% in patients receiving fingolimod hydrochloride 0.5 mg and 7% on placebo.
Two patients died of herpetic infections during controlled trials. One death was due to disseminated primary herpes zoster and the other was to herpes simplex encephalitis. In both cases, the patients were taking a 1.25 mg dose of fingolimod (higher than the recommended 0.5 mg dose) and had received high-dose corticosteroid therapy to treat suspected MS relapses.
Serious, life-threatening events of disseminated varicella zoster and herpes simplex infections, including cases of encephalitis and multiorgan failure, have occurred with fingolimod hydrochloride in the postmarketing setting. Include disseminated herpetic infections in the differential diagnosis of patients who are receiving fingolimod hydrochloride and present with an atypical MS relapse or multiorgan failure.
Cases of Kaposi’s sarcoma have been reported in the postmarketing setting. Kaposi’s sarcoma is an angioproliferative disorder that is associated with infection with human herpes virus 8 (HHV-8). Patients with symptoms or signs consistent with Kaposi’s sarcoma should be referred for prompt diagnostic evaluation and management.
Cryptococcal Infections
Cryptococcal infections, including cases of fatal cryptococcal meningitis and disseminated cryptococcal infections, have been reported with fingolimod hydrochloride in the postmarketing setting. Cryptococcal infections have generally occurred after approximately 2 years of fingolimod hydrochloride treatment, but may occur earlier. The relationship between the risk of cryptococcal infection and the duration of treatment is unknown. Patients with symptoms and signs consistent with a cryptococcal infection should undergo prompt diagnostic evaluation and treatment.
Prior and Concomitant Treatment with Antineoplastic, Immunosuppressive, or Immune-Modulating Therapies
In clinical studies, patients who received fingolimod hydrochloride did not receive concomitant treatment with antineoplastic, non-corticosteroid immunosuppressive, or immune-modulating therapies used for treatment of MS. Concomitant use of fingolimod hydrochloride with any of these therapies, and also with corticosteroids, would be expected to increase the risk of immunosuppression [see Drug Interactions (7.4)] .
When switching to fingolimod hydrochloride from immune-modulating or immunosuppressive medications, consider the duration of their effects and their mode of action to avoid unintended additive immunosuppressive effects.
Varicella Zoster Virus Antibody Testing/Vaccination
Patients without a healthcare professional confirmed history of chickenpox or without documentation of a full course of vaccination against VZV should be tested for antibodies to VZV before initiating fingolimod hydrochloride. VZV vaccination of antibody-negative patients is recommended prior to commencing treatment with fingolimod hydrochloride, following which initiation of treatment with fingolimod hydrochloride should be postponed for 1 month to allow the full effect of vaccination to occur [see Drug Interactions (7.3), Use in Specific Populations (8.4)].
Human Papilloma Virus Infection
Human papilloma virus (HPV) infections, including papilloma, dysplasia, warts, and HPV-related cancer, have been reported in patients treated with fingolimod hydrochloride in the postmarketing setting. Vaccination against HPV should be considered prior to treatment initiation with fingolimod hydrochloride, taking into account vaccination recommendations. Cancer screening, including Papanicolaou (Pap) test, is recommended as per standard of care for patients using an immunosuppressive therapy.
5.3 Progressive Multifocal Leukoencephalopathy
Cases of progressive multifocal leukoencephalopathy (PML) have occurred in patients with MS who received fingolimod hydrochloride in the postmarketing setting. PML is an opportunistic viral infection of the brain caused by the JC virus (JCV) that typically only occurs in patients who are immunocompromised, and that usually leads to death or severe disability. PML has occurred in patients who had not been treated previously with natalizumab, which has a known association with PML, were not taking any other immunosuppressive or immunomodulatory medications concomitantly, and did not have any ongoing systemic medical conditions resulting in compromised immune system function. The majority of cases have occurred in patients treated with fingolimod hydrochloride for at least 2 years. The relationship between the risk of PML and the duration of treatment is unknown.
At the first sign or symptom suggestive of PML, withhold fingolimod hydrochloride and perform an appropriate diagnostic evaluation. Typical symptoms associated with PML are diverse, progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes.
Magnetic reasonace imaging (MRI) findings may be apparent before clinical signs or symptoms. Cases of PML, diagnosed based on MRI findings and the detection of JCV DNA in the cerebrospinal fluid in the absence of clinical signs or symptoms specific to PML, have been reported in patients treated with MS medications associated with PML, including fingolimod hydrochloride. Many of these patients subsequently became symptomatic with PML. Therefore, monitoring with MRI for signs that may be consistent with PML may be useful, and any suspicious findings should lead to further investigation to allow for an early diagnosis of PML, if present. Lower PML-related mortality and morbidity have been reported following discontinuation of another MS medication associated with PML in patients with PML who were initially asymptomatic compared to patients with PML who had characteristic clinical signs and symptoms at diagnosis. It is not known whether these differences are due to early detection and discontinuation of MS treatment or due to differences in disease in these patients.
If PML is confirmed, treatment with fingolimod hydrochloride should be discontinued.
Immune reconstitution inflammatory syndrome (IRIS) has been reported in patients treated with S1P receptor modulators, including fingolimod hydrochloride, who developed PML and subsequently discontinued treatment. IRIS presents as a clinical decline in the patient’s condition that may be rapid, can lead to serious neurological complications or death, and is often associated with characteristic changes on MRI. The time to onset of IRIS in patients with PML was generally within a few months after S1P receptor modulator discontinuation. Monitoring for development of IRIS and appropriate treatment of the associated inflammation should be undertaken.5.4 Macular Edema
Fingolimod increases the risk of macular edema. Perform an examination of the fundus including the macula in all patients before starting treatment, again 3 to 4 months after starting treatment, and again at any time after a patient reports visual disturbances while on fingolimod hydrochloride therapy.
A dose-dependent increase in the risk of macular edema occurred in the fingolimod hydrochloride clinical development program.
In 2-year double-blind, placebo-controlled studies in adult patients with multiple sclerosis, macular edema with or without visual symptoms occurred in 1.5% of patients (11/799) treated with fingolimod 1.25 mg, 0.5% of patients (4/783) treated with fingolimod hydrochloride 0.5 mg, and 0.4% of patients (3/773) treated with placebo. Macular edema occurred predominantly during the first 3 to 4 months of therapy. These clinical trials excluded patients with diabetes mellitus, a known risk factor for macular edema (see below Macular Edema in Patients with History of Uveitis or Diabetes Mellitus). Symptoms of macular edema included blurred vision and decreased visual acuity. Routine ophthalmological examination detected macular edema in some patients with no visual symptoms. Macular edema generally partially or completely resolved with or without treatment after drug discontinuation. Some patients had residual visual acuity loss even after resolution of macular edema. Macular edema has also been reported in patients taking fingolimod hydrochloride in the postmarketing setting, usually within the first 6 months of treatment.
Continuation of fingolimod hydrochloride in patients who develop macular edema has not been evaluated. A decision on whether or not to discontinue fingolimod hydrochloride therapy should include an assessment of the potential benefits and risks for the individual patient. The risk of recurrence after rechallenge has not been evaluated.
Macular Edema in Patients with History of Uveitis or Diabetes Mellitus
Patients with a history of uveitis and patients with diabetes mellitus are at increased risk of macular edema during fingolimod hydrochloride therapy. The incidence of macular edema is also increased in MS patients with a history of uveitis. In the combined clinical trial experience in adult patients with all doses of fingolimod, the rate of macular edema was approximately 20% in MS patients with a history of uveitis versus 0.6% in those without a history of uveitis. Fingolimod hydrochloride has not been tested in MS patients with diabetes mellitus. In addition to the examination of the fundus including the macula prior to treatment and at 3 to 4 months after starting treatment, MS patients with diabetes mellitus or a history of uveitis should have regular follow-up examinations.
5.5 Liver Injury
Clinically significant liver injury has occurred in patients treated with fingolimod hydrochloride in the postmarketing setting. Signs of liver injury, including markedly elevated serum hepatic enzymes and elevated total bilirubin, have occurred as early as ten days after the first dose and have also been reported after prolonged use. Cases of acute liver failure requiring liver transplant have been reported.
In 2-year placebo-controlled clinical trials in adult patients, elevation of liver enzymes (ALT, AST and GGT) to 3-fold the upper limit of normal (ULN) or greater occurred in 14% of patients treated with fingolimod hydrochloride 0.5 mg and 3% of patients on placebo. Elevations 5-fold the ULN or greater occurred in 4.5% of patients on fingolimod hydrochloride and 1% of patients on placebo. The majority of elevations occurred within 6 to 9 months. In clinical trials, fingolimod hydrochloride was discontinued if the elevation exceeded 5 times the ULN. Serum transaminase levels returned to normal within approximately 2 months after discontinuation of fingolimod hydrochloride. Recurrence of liver transaminase elevations occurred with rechallenge in some patients.
Prior to starting treatment with fingolimod hydrochloride (within 6 months), obtain serum transaminases (ALT and AST) and total bilirubin levels. Obtain transaminase levels and total bilirubin levels periodically until two months after fingolimod hydrochloride discontinuation.
Patients should be monitored for signs and symptoms of any hepatic injury. Measure liver transaminase and bilirubin levels promptly in patients who report symptoms that may indicate liver injury, including new or worsening fatigue, anorexia, right upper abdominal discomfort, dark urine, or jaundice. In this clinical context, if the patient is found to have an alanine aminotransferase (ALT) greater than three times the reference range with serum total bilirubin greater than two times the reference range, treatment with fingolimod hydrochloride should be interrupted. Treatment should not be resumed if a plausible alternative etiology for the signs and symptoms cannot be established, because these patients are at risk for severe drug-induced liver injury.
Because fingolimod hydrochloride exposure is doubled in patients with severe hepatic impairment, these patients should be closely monitored, as the risk of adverse reactions is greater [ see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
5.6 Posterior Reversible Encephalopathy Syndrome
There have been rare cases of posterior reversible encephalopathy syndrome (PRES) reported in adult patients receiving fingolimod hydrochloride. Symptoms reported included sudden onset of severe headache, altered mental status, visual disturbances, and seizure. Symptoms of PRES are usually reversible but may evolve into ischemic stroke or cerebral hemorrhage. Delay in diagnosis and treatment may lead to permanent neurological sequelae. If PRES is suspected, fingolimod hydrochloride should be discontinued.
5.7 Respiratory Effects
Dose-dependent reductions in forced expiratory volume over 1 second (FEV1) and diffusion lung capacity for carbon monoxide (DLCO) were observed in patients treated with fingolimod hydrochloride as early as 1 month after treatment initiation. In 2-year placebo-controlled trials in adult patients, the reduction from baseline in the percent of predicted values for FEV1 at the time of last assessment on drug was 2.8% for fingolimod hydrochloride 0.5 mg and 1.0% for placebo. For DLCO, the reduction from baseline in percent of predicted values at the time of last assessment on drug was 3.3% for fingolimod hydrochloride 0.5 mg and 0.5% for placebo. The changes in FEV1 appear to be reversible after treatment discontinuation. There is insufficient information to determine the reversibility of the decrease of DLCO after drug discontinuation. In MS placebo-controlled trials in adult patients, dyspnea was reported in 9% of patients receiving fingolimod hydrochloride 0.5 mg and 7% of patients receiving placebo. Several patients discontinued fingolimod hydrochloride because of unexplained dyspnea during the extension (uncontrolled) studies. Fingolimod hydrochloride has not been tested in MS patients with compromised respiratory function.
Spirometric evaluation of respiratory function and evaluation of DLCO should be performed during therapy with fingolimod hydrochloride if clinically indicated.
5.8 Fetal Risk
Based on findings from animal studies, fingolimod hydrochloride may cause fetal harm when administered to a pregnant woman. In animal reproduction studies conducted in rats and rabbits, developmental toxicity was observed with administration of fingolimod at doses less than the recommended human dose. Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Because it takes approximately 2 months to eliminate fingolimod hydrochloride from the body, advise females of reproductive potential to use effective contraception to avoid pregnancy during and for 2 months after stopping fingolimod hydrochloride treatment [see Use in Specific Populations (8.1, 8.3)] .
5.9 Severe Increase in Disability After Stopping Fingolimod Hydrochloride
Severe increase in disability accompanied by multiple new lesions on MRI has been reported after discontinuation of fingolimod hydrochloride in the postmarketing setting. Patients in most of these reported cases did not return to the functional status they had before stopping fingolimod hydrochloride. The increase in disability generally occurred within 12 weeks after stopping fingolimod hydrochloride, but was reported up to 24 weeks after fingolimod hydrochloride discontinuation.
Monitor patients for development of severe increase in disability following discontinuation of fingolimod hydrochloride and begin appropriate treatment as needed.
After stopping fingolimod hydrochloride in the setting of PML, monitor for development of immune reconstitution inflammatory syndrome (PML-IRIS) [see Warnings and Precautions (5.3)]
5.10 Tumefactive Multiple Sclerosis
MS relapses with tumefactive demyelinating lesions on imaging have been observed during fingolimod hydrochloride therapy and after fingolimod hydrochloride discontinuation in the postmarketing setting. Most reported cases of tumefactive MS in patients receiving fingolimod hydrochloride have occurred within the first 9 months after fingolimod hydrochloride initiation, but tumefactive MS may occur at any point during treatment. Cases of tumefactive MS have also been reported within the first 4 months after fingolimod hydrochloride discontinuation. Tumefactive MS should be considered when a severe MS relapse occurs during fingolimod hydrochloride treatment, especially during initiation, or after discontinuation of fingolimod hydrochloride, prompting imaging evaluation and initiation of appropriate treatment.
5.11 Increased Blood Pressure
In adult MS controlled clinical trials, patients treated with fingolimod hydrochloride 0.5 mg had an average increase over placebo of approximately 3 mmHg in systolic pressure, and approximately 2 mmHg in diastolic pressure, first detected after approximately 1 month of treatment initiation, and persisting with continued treatment. Hypertension was reported as an adverse reaction in 8% of patients on fingolimod hydrochloride 0.5 mg and in 4% of patients on placebo. Blood pressure (BP) should be monitored during treatment with fingolimod hydrochloride.
5.12 Malignancies
Cutaneous Malignancies
The risk of basal cell carcinoma (BCC) and melanoma is increased in patients treated with fingolimod hydrochloride. In two-year placebo-controlled trials in adult patients, the incidence of BCC was 2% in patients on fingolimod hydrochloride 0.5 mg and 1% in patients on placebo [ see Adverse Reactions (6.1)]. Melanoma, squamous cell carcinoma and Merkel cell carcinoma have been reported with fingolimod hydrochloride in the postmarketing setting. Periodic skin examination is recommended for all patients, particularly those with risk factors for skin cancer. Providers and patients are advised to monitor for suspicious skin lesions. If a suspicious skin lesion is observed, it should be promptly evaluated. As usual for patients with increased risk for skin cancer, exposure to sunlight and ultraviolet light should be limited by wearing protective clothing and using a sunscreen with a high protection factor.Lymphoma
Cases of lymphoma, including both T-cell and B-cell types and CNS lymphoma, have occurred in patients receiving fingolimod hydrochloride. The reporting rate of non-Hodgkin lymphoma with fingolimod hydrochloride is greater than that expected in the general population adjusted by age, gender, and region. Cutaneous T-cell lymphoma (including mycosis fungoides) has also been reported with fingolimod hydrochloride in the postmarketing setting.5.13 Immune System Effects Following Fingolimod Hydrochloride Discontinuation
Fingolimod remains in the blood and has pharmacodynamic effects, including decreased lymphocyte counts, for up to 2 months following the last dose of fingolimod hydrochloride. Lymphocyte counts generally return to the normal range within 1 to 2 months of stopping therapy [see Clinical Pharmacology (12.2)] . Because of the continuing pharmacodynamic effects of fingolimod, initiating other drugs during this period warrants the same considerations needed for concomitant administration (e.g., risk of additive immunosuppressant effects) [see Drug Interactions (7.4)] .
5.14 Hypersensitivity Reactions
Hypersensitivity reactions, including rash, urticaria, and angioedema have been reported with fingolimod hydrochloride in the postmarketing setting. Fingolimod hydrochloride capsules are contraindicated in patients with history of hypersensitivity to fingolimod or any of its excipients [see Contraindications (4)] .
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in labeling:
- Bradyarrhythmia and Atrioventricular Blocks [
see
Warnings and Precautions (5.1)]
- Infections [
see
Warnings and Precautions (5.2)]
- Progressive Multifocal Leukoencephalopathy [
see
Warnings and Precautions (5.3)]
- Macular Edema [
see
Warnings and Precautions (5.4)]
- Liver Injury [
see
Warnings and Precautions (5.5)]
- Posterior Reversible Encephalopathy Syndrome [
see
Warnings and Precautions (5.6)]
- Respiratory Effects [ see Warnings and Precautions (5.7)]
- Fetal Risk [see Warnings and Precautions (5.8)]
- Severe Increase in Disability after Stopping Fingolimod Hydrochloride [see Warnings and Precautions (5.9)]
- Tumefactive Multiple Sclerosis [see Warnings and Precautions (5.10)]
- Increased Blood Pressure [see Warnings and Precautions (5.11)]
- Malignancies [see Warnings and Precautions (5.12)]
- Immune System Effects Following Fingolimod Hydrochloride Discontinuation [see Warnings and Precautions (5.13)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.14)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
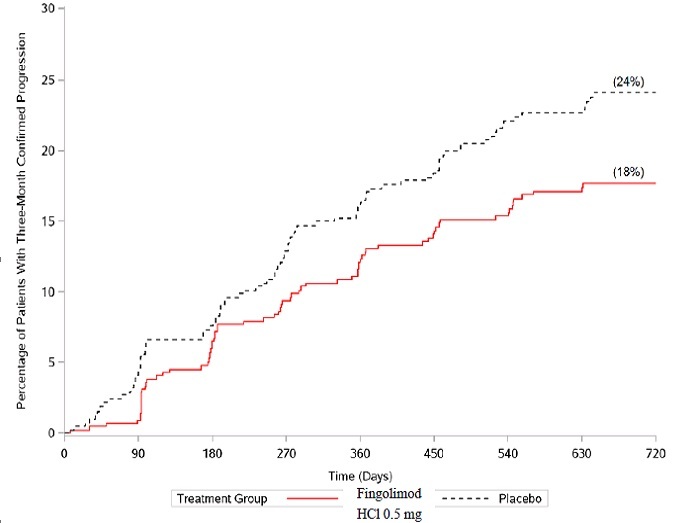
Adults
In clinical trials (Studies 1, 2, and 3), a total of 1212 patients with relapsing forms of multiple sclerosis received fingolimod hydrochloride 0.5 mg. This included 783 patients who received fingolimod hydrochloride 0.5 mg in the 2-year placebo-controlled trials (Studies 1 and 3) and 429 patients who received fingolimod hydrochloride 0.5 mg in the 1-year active-controlled trial (Study 2). The overall exposure in the controlled trials was equivalent to 1716 person-years. Approximately 1000 patients received at least 2 years of treatment with fingolimod hydrochloride 0.5 mg. In all clinical studies, including uncontrolled extension studies, the exposure to fingolimod hydrochloride 0.5 mg was approximately 4119 person-years.
In placebo-controlled trials, the most frequent adverse reactions (incidence ≥10% and greater than placebo) for fingolimod hydrochloride 0.5 mg were headache, liver transaminase elevation, diarrhea, cough, influenza, sinusitis, back pain, abdominal pain, and pain in extremity. Adverse events that led to treatment discontinuation and occurred in more than 1% of patients taking fingolimod hydrochloride 0.5 mg, were serum transaminase elevations (4.7% compared to 1% on placebo) and basal cell carcinoma (1% compared to 0.5% on placebo).
Table 1 lists adverse reactions in clinical studies in adults that occurred in ≥ 1% of fingolimod hydrochloride-treated patients and ≥ 1% higher rate than for placebo.
Table 1: Adverse Reactions Reported in Adult Studies 1 and 3 (Occurring in ≥1% of Patients and Reported for Fingolimod Hydrochloride 0.5 mg at ≥1% Higher Rate Than for Placebo) Abbreviations: ALT, alanine transaminase; AST, aspartate transferase; GGT, gamma-glutamyl transferase. Adverse drug reactions
Fingolimod Hydrochloride 0.5 mg
N=783
%
Placebo
N=773
%Infections Influenza 11 8 Sinusitis 11 8 Bronchitis 8 5 Herpes zoster 2 1 Tinea versicolor 2 <1 Cardiac disorders Bradycardia 3 1 Nervous system disorders Headache 25 24 Migraine 6 4 Gastrointestinal disorders Nausea 13 12 Diarrhea 13 10 Abdominal pain 11 10 General disorders and administration-site conditions Asthenia 2 1 Musculoskeletal and connective tissue disorders Back pain 10 9 Pain in extremity 10 7 Skin and subcutaneous tissue disorders Alopecia 3 2 Actinic keratosis 2 1 Investigations Liver transaminase elevations
(ALT/GGT/AST)15 4 Blood triglycerides increased 3 1 Respiratory, thoracic, and mediastinal disorders Cough 12 11 Dyspnea 9 7 Eye disorders Vision blurred 4 2 Vascular disorders Hypertension 8 4 Blood and lymphatic system disorders Lymphopenia 7 <1 Leukopenia 2 <1 Neoplasms benign, malignant, and unspecified
(including cysts and polyps)Skin papilloma 3 2 Basal cell carcinoma 2 1 Adverse reactions of seizure, dizziness, pneumonia, eczema and pruritus were also reported in Studies 1 and 3, but did not meet the reporting rate criteria for inclusion in Table 1 (difference was less than 1%).
Adverse reactions with fingolimod hydrochloride 0.5 mg in Study 2, the 1-year active-controlled (versus interferon beta-1a) study were generally similar to those in Studies 1 and 3.Vascular Events
Vascular events, including ischemic and hemorrhagic strokes, and peripheral arterial occlusive disease were reported in premarketing clinical trials in patients who received fingolimod hydrochloride doses (1.25 mg to 5 mg) higher than recommended for use in MS. Similar events have been reported with fingolimod hydrochloride in the postmarketing setting although a causal relationship has not been established.Seizure
Cases of seizures, including status epilepticus, have been reported with the use of fingolimod hydrochloride in clinical trials and in the postmarketing setting in adults. [see Adverse Reactions (6.2)] In adult clinical trials, the rate of seizures was 0.9% in fingolimod hydrochloride-treated patients and 0.3% in placebo-treated patients. It is unknown whether these events were related to the effects of multiple sclerosis alone, to fingolimod hydrochloride, or to a combination of both.Pediatric
Patients 10 Years of Age and Older
In the controlled pediatric trial (Study 4), the safety profile in pediatric patients receiving fingolimod hydrochloride 0.5 mg daily was similar to that seen in adult patients.
In the pediatric study, cases of seizures were reported in 5.6% of fingolimod hydrochloride -treated patients and 0.9% of interferon beta-1a-treated patients [see Use in Specific Populations (8.4)].6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of fingolimod hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System Disorders:Hemolytic anemia and thrombocytopenia
Hepatobiliary Disorders:Liver injury [ see Warnings and Precautions (5.5)]
Infections:Infections, including cryptococcal infections [see Warnings and Precautions (5.2)] , human papilloma virus (HPV) infection, including papilloma, dysplasia, warts and HPV-related cancer [see Warnings and Precautions (5.2)] , progressive multifocal leukoencephalopathy [see Warnings and Precautions (5.3)]
Musculoskeletal and connective tissue disorders:Arthralgia, myalgia
Nervous System Disorders:Posterior reversible encephalopathy syndrome [ see Warnings and Precautions (5.6)] , seizures, including status epilepticus [see Adverse Reactions (6.1)]
Neoplasms, Benign, Malignant, and Unspecified (including cysts and polyps):melanoma, Merkel cell carcinoma, and cutaneous T-cell lymphoma (including mycosis fungoides) [ see Warnings and Precautions (5.12)]
Skin and Subcutaneous Tissue Disorders:Hypersensitivity[ see Warnings and Precautions (5.14)]
- Bradyarrhythmia and Atrioventricular Blocks [
see
Warnings and Precautions (5.1)]
-
7 DRUG INTERACTIONS
7.1 QT Prolonging Drugs
Fingolimod hydrochloride has not been studied in patients treated with drugs that prolong the QT interval. Drugs that prolong the QT interval have been associated with cases of torsades de pointes in patients with bradycardia. Since initiation of fingolimod hydrochloride treatment results in decreased heart rate and may prolong the QT interval, patients on QT prolonging drugs with a known risk of torsades de pointes (e.g., citalopram, chlorpromazine, haloperidol, methadone, erythromycin) should be monitored overnight with continuous ECG in a medical facility [ see Dosage and Administration (2.4), Warnings and Precautions (5.1)].
7.2 Ketoconazole
The blood levels of fingolimod and fingolimod-phosphate are increased by 1.7-fold when used concomitantly with ketoconazole. Patients who use fingolimod hydrochloride and systemic ketoconazole concomitantly should be closely monitored, as the risk of adverse reactions is greater.
7.3 Vaccines
Fingolimod hydrochloride reduces the immune response to vaccination. Vaccination may be less effective during and for up to 2 months after discontinuation of treatment with fingolimod hydrochloride [ see Clinical Pharmacology (12.2)]. Avoid the use of live attenuated vaccines during and for 2 months after treatment with fingolimod hydrochloride because of the risk of infection.. It is recommended that pediatric patients, if possible, be brought up to date with all immunizations in agreement with current immunization guidelines prior to initiating fingolimod capsules therapy.
7.4 Antineoplastic, Immunosuppressive, or Immune-Modulating Therapies
Antineoplastic, immune-modulating, or immunosuppressive therapies, (including corticosteroids) are expected to increase the risk of immunosuppression, and the risk of additive immune system effects must be considered if these therapies are coadministered with fingolimod hydrochloride. When switching from drugs with prolonged immune effects, such as natalizumab, teriflunomide or mitoxantrone, the duration and mode of action of these drugs must be considered to avoid unintended additive immunosuppressive effects when initiating fingolimod hydrochloride [ see Warnings and Precautions (5.2)].
7.5 Drugs That Slow Heart Rate or Atrioventricular Conduction (e.g., beta blockers or diltiazem)
Experience with fingolimod hydrochloride in patients receiving concurrent therapy with drugs that slow the heart rate or AV conduction (e.g., beta blockers, digoxin, or heart rate-slowing calcium channel blockers, such as diltiazem or verapamil) is limited. Because initiation of fingolimod hydrochloride treatment may result in an additional decrease in heart rate, concomitant use of these drugs during fingolimod hydrochloride initiation may be associated with severe bradycardia or heart block. Seek advice from the physician prescribing these drugs regarding the possibility to switch to drugs that do not slow the heart rate or atrioventricular conduction before initiating fingolimod hydrochloride. Patients who cannot switch should have overnight continuous ECG monitoring after the first dose [ see Dosage and Administration (2.4), Warnings and Precautions (5.1)].
7.6 Laboratory Test Interaction
Because fingolimod hydrochloride reduces blood lymphocyte counts via redistribution in secondary lymphoid organs, peripheral blood lymphocyte counts cannot be utilized to evaluate the lymphocyte subset status of a patient treated with fingolimod hydrochloride. A recent CBC should be available before initiating treatment with fingolimod hydrochloride.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal studies, fingolimod hydrochloride may cause fetal harm when administered to a pregnant woman. Data from prospective reports to the fingolimod pregnancy registry are currently not sufficient to allow for an adequate assessment of the drug-associated risk for birth defects and miscarriage in humans.
In oral studies conducted in rats and rabbits, fingolimod demonstrated developmental toxicity, including an increase in malformations (rats) and embryolethality, when given to pregnant animals. In rats, the highest no-effect dose was less than the recommended human dose of 0.5 mg/day on a body surface area (mg/m 2) basis. The most common fetal visceral malformations in rats were persistent truncus arteriosus and ventricular septal defect. The receptor affected by fingolimod (sphingosine 1-phosphate receptor) is known to be involved in vascular formation during embryogenesis (see Data). Advise pregnant women of the potential risk to a fetus.
In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Clinical Considerations
In females planning to become pregnant, fingolimod hydrochloride should be stopped 2 months before planned conception.
The possibility of severe increase in disability should be considered in women who discontinue or are considering discontinuation of fingolimod hydrochloride because of pregnancy or planned pregnancy. In many of the cases in which increase in disability was reported after stopping fingolimod hydrochloride, patients had stopped fingolimod hydrochloride because of pregnancy or planned pregnancy [see Warnings and Precautions (5.9)] .
Data
Animal Data
When fingolimod was orally administered to pregnant rats during the period of organogenesis (0, 0.03, 0.1, and 0.3 mg/kg/day or 0, 1, 3, and 10 mg/kg/day), increased incidences of fetal malformations and embryofetal deaths were observed at all but the lowest dose tested (0.03 mg/kg/day), which is less than the recommended human dose (RHD) on a mg/m 2basis. Oral administration to pregnant rabbits during organogenesis (0, 0.5, 1.5, and 5 mg/kg/day) resulted in increased incidences of embryofetal mortality and fetal growth retardation at the mid and high doses. The no-effect dose for these effects in rabbits (0.5 mg/kg/day) is approximately 20 times the RHD on a mg/m 2basis.
When fingolimod was orally administered to female rats during pregnancy and lactation (0, 0.05, 0.15, and 0.5 mg/kg/day), pup survival was decreased at all doses and a neurobehavioral (learning) deficit was seen in offspring at the high dose. The low-effect dose of 0.05 mg/kg/day is similar to the RHD on a mg/m 2basis.
8.2 Lactation
Risk Summary
There are no data on the presence of fingolimod in human milk, the effects on the breastfed infant, or the effects of the drug on milk production. Fingolimod is excreted in the milk of treated rats. When a drug is present in animal milk, it is likely that the drug will be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for fingolimod hydrochloride and any potential adverse effects on the breastfed infant from fingolimod hydrochloride or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
The pregnancy status of females of reproductive potential should be verified prior to starting treatment with fingolimod hydrochloride [see Use in Specific Populations (8.1)]. .
Contraception
Before initiation of fingolimod hydrochloride treatment, females of reproductive potential should be counseled on the potential for a serious risk to the fetus and the need for effective contraception during treatment with fingolimod hydrochloride. [see Warnings and Precautions (5.8)and Use in Specific Populations (8.1)] Since it takes approximately 2 months to eliminate the compound from the body after stopping treatment, the potential risk to the fetus may persist and women should use effective contraception during this period [see Warnings and Precautions (5.8, 5.13)]
8.4 Pediatric Use
Safety and effectiveness of fingolimod hydrochloride for the treatment of relapsing forms of multiple sclerosis in pediatric patients 10 to less than 18 years of age were established in one randomized, double-blind clinical study in 215 patients (fingolimod hydrochloride n = 107; intramuscular interferon (IFN) beta-1a n = 108) [see Clinical Studies (14.2)].
In the controlled pediatric study, the safety profile in pediatric patients (10 to less than 18 years of age) receiving fingolimod hydrochloride 0.5 mg daily was similar to that seen in adult patients. In the pediatric study, cases of seizures were reported in 5.6% of fingolimod-treated patients and 0.9% of interferon beta-1a-treated patients
It is recommended that pediatric patients if possible, complete all immunizations in accordance with current immunization guidelines prior to initiating fingolimod capsules therapy.Safety and effectiveness of fingolimod hydrochloride in pediatric patients below the age of 10 years have not been established.
Juvenile Animal Toxicity Data
In a study in which fingolimod (0.3, 1.5, or 7.5 mg/kg/day) was orally administered to young rats from weaning through sexual maturity, changes in bone mineral density and persistent neurobehavioral impairment (altered auditory startle) were observed at all doses. Delayed sexual maturation was noted in females at the highest dose tested and in males at all doses.
The bone changes observed in fingolimod-treated juvenile rats are consistent with a reported role of S1P in the regulation of bone mineral homeostasis.
When fingolimod (0.5 or 5 mg/kg/day) was orally administered to rats from the neonatal period through sexual maturity, a marked decrease in T-cell dependent antibody response was observed at both doses. This effect had not fully recovered by 6 to 8 weeks after the end of treatment.
Overall, a no-effect dose for adverse developmental effects in juvenile animals was not identified.
8.5 Geriatric Use
Clinical MS studies of fingolimod hydrochloride did not include sufficient numbers of patients aged 65 years and over to determine whether they respond differently than younger patients. Fingolimod hydrochloride should be used with caution in patients aged 65 years and over, reflecting the greater frequency of decreased hepatic, or renal, function and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
Because fingolimod, but not fingolimod-phosphate, exposure is doubled in patients with severe hepatic impairment, patients with severe hepatic impairment should be closely monitored, as the risk of adverse reactions may be greater [ see Warnings and Precautions (5.5), Clinical Pharmacology (12.3)].
No dose adjustment is needed in patients with mild or moderate hepatic impairment.
8.7 Renal Impairment
The blood level of some fingolimod hydrochloride metabolites is increased (up to 13-fold) in patients with severe renal impairment [ see Clinical Pharmacology (12.3)]. The toxicity of these metabolites has not been fully explored. The blood level of these metabolites has not been assessed in patients with mild or moderate renal impairment.
-
10 OVERDOSAGE
Fingolimod hydrochloride can induce bradycardia as well as AV conduction blocks (including complete AV block). The decline in heart rate usually starts within 1 hour of the first dose and is maximal within 6 hours in most patients [ see Warnings and Precautions (5.1)]. In case of fingolimod hydrochloride overdosage, observe patients overnight with continuous ECG monitoring in a medical facility, and obtain regular measurements of blood pressure [ see Dosage and Administration (2.4)].
Neither dialysis nor plasma exchange results in removal of fingolimod from the body.
-
11 DESCRIPTION
Fingolimod is a sphingosine 1-phosphate receptor modulator.
Chemically, fingolimod is 2-amino-2-[2-(4-octylphenyl)ethyl]propan-1,3-diol hydrochloride. Its structure is shown below:
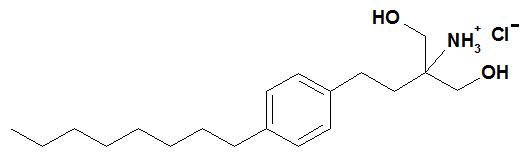
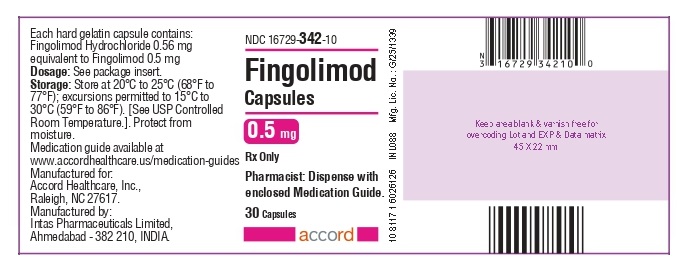
Fingolimod hydrochloride is a white to practically white powder that is freely soluble in water and alcohol and soluble in propylene glycol. It has a molecular weight of 343.93 g/mol.
Fingolimod hydrochloride is provided as 0.5 mg hard gelatin capsules for oral use. Each capsule contains 0.56 mg of fingolimod hydrochloride, equivalent to 0.5 mg of fingolimod.
Each fingolimod 0.5 mg capsule contains the following inactive ingredients: magnesium stearate, pregelatinized starch (maize).
Capsule shell contains gelatin, iron oxide yellow and titanium dioxide;
Black imprinting ink contains shellac, iron oxide black and potassium hydroxide.
Yellow imprinting ink contains shellac and iron oxide yellow.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fingolimod is metabolized by sphingosine kinase to the active metabolite, fingolimod-phosphate. Fingolimod-phosphate is a sphingosine 1-phosphate receptor modulator, and binds with high affinity to sphingosine 1-phosphate receptors 1, 3, 4, and 5. Fingolimod-phosphate blocks the capacity of lymphocytes to egress from lymph nodes, reducing the number of lymphocytes in peripheral blood. The mechanism by which fingolimod exerts therapeutic effects in multiple sclerosis is unknown, but may involve reduction of lymphocyte migration into the central nervous system.
12.2 Pharmacodynamics
Heart Rate and Rhythm
Fingolimod causes a transient reduction in heart rate and AV conduction at treatment initiation [ see Warnings and Precautions (5.1)].
Heart rate progressively increases after the first day, returning to baseline values within 1 month of the start of chronic treatment.
Autonomic responses of the heart, including diurnal variation of heart rate and response to exercise, are not affected by fingolimod treatment.
Fingolimod treatment is not associated with a decrease in cardiac output.
Potential to Prolong the QT Interval
In a thorough QT interval study of doses of 1.25 or 2.5 mg fingolimod at steady-state, when a negative chronotropic effect of fingolimod was still present, fingolimod treatment resulted in a prolongation of QTc, with the upper boundary of the 90% confidence interval (CI) of 14.0 msec. There is no consistent signal of increased incidence of QTc outliers, either absolute or change from baseline, associated with fingolimod treatment. In MS studies, there was no clinically relevant prolongation of the QT interval, but patients at risk for QT prolongation were not included in clinical studies.
Immune System
Effects on Immune Cell Numbers in the Blood
In a study in which 12 adult subjects received fingolimod hydrochloride 0.5 mg daily, the lymphocyte count decreased to approximately 60% of baseline within 4 to 6 hours after the first dose. With continued daily dosing, the lymphocyte count continued to decrease over a 2-week period, reaching a nadir count of approximately 500 cells/mcL or approximately 30% of baseline. In a placebo-controlled study in 1272 MS patients (of whom 425 received fingolimod 0.5 mg daily and 418 received placebo), 18% (N=78) of patients on fingolimod 0.5 mg reached a nadir of <200 cells/mcL on at least 1 occasion. No patient on placebo reached a nadir of <200 cells/mcL. Low lymphocyte counts are maintained with chronic daily dosing of fingolimod hydrochloride 0.5 mg daily.
Chronic fingolimod dosing leads to a mild decrease in the neutrophil count to approximately 80% of baseline. Monocytes are unaffected by fingolimod.
Peripheral lymphocyte count increases are evident within days of stopping fingolimod treatment and typically normal counts are reached within 1 to 2 months.
Effect on Antibody Response
Fingolimod hydrochloride reduces the immune response to vaccination, as evaluated in 2 studies.
In the first study, the immunogenicity of keyhole limpet hemocyanin (KLH) and pneumococcal polysaccharide vaccine (PPV-23) immunization were assessed by IgM and IgG titers in a steady-state, randomized, placebo-controlled study in healthy adult volunteers. Compared to placebo, antigen-specific IgM titers were decreased by 91% and 25% in response to KLH and PPV-23, respectively, in subjects on fingolimod hydrochloride 0.5 mg. Similarly, IgG titers were decreased by 45% and 50%, in response to KLH and PPV-23, respectively, in subjects on fingolimod hydrochloride 0.5 mg daily compared to placebo. The responder rate for fingolimod hydrochloride 0.5 mg as measured by the number of subjects with a >4-fold increase in KLH IgG was comparable to placebo and 25% lower for PPV-23 IgG, while the number of subjects with a >4 fold increase in KLH and PPV-23 IgM was 75% and 40% lower, respectively, compared to placebo. The capacity to mount a skin delayed-type hypersensitivity reaction to Candida and tetanus toxoid was decreased by approximately 30% in subjects on fingolimod hydrochloride 0.5 mg daily, compared to placebo. Immunologic responses were further decreased with fingolimod 1.25 mg (a dose higher than recommended in MS) [ see Warnings and Precautions (5.2)].
In the second study, the immunogenicity of Northern hemisphere seasonal influenza and tetanus toxoid vaccination was assessed in a 12-week steady-state, randomized, placebo-controlled study of fingolimod hydrochloride 0.5 mg in adult multiple sclerosis patients (n=136). The responder rate 3 weeks after vaccination, defined as seroconversion or a ≥4-fold increase in antibody directed against at least 1 of the 3 influenza strains, was 54% for fingolimod hydrochloride 0.5 mg and 85% in the placebo group. The responder rate 3 weeks after vaccination, defined as seroconversion or a ≥4-fold increase in antibody directed against tetanus toxoid was 40% for fingolimod hydrochloride 0.5 mg and 61% in the placebo group.
Pulmonary Function
Single fingolimod doses ≥5 mg (10-fold the recommended dose) are associated with a dose-dependent increase in airway resistance. In a 14-day study of 0.5, 1.25, or 5 mg/day, fingolimod was not associated with impaired oxygenation or oxygen desaturation with exercise or an increase in airway responsiveness to methacholine. Subjects on fingolimod treatment had a normal bronchodilator response to inhaled beta-agonists.
In a 14-day placebo-controlled study of adult patients with moderate asthma, no effect was seen for fingolimod hydrochloride 0.5 mg (recommended dose in MS). A 10% reduction in mean FEV1 at 6 hours after dosing was observed in adult patients receiving fingolimod 1.25 mg (a dose higher than recommended for use in MS) on Day 10 of treatment. Fingolimod 1.25 mg was associated with a 5-fold increase in the use of rescue short acting beta-agonists.
12.3 Pharmacokinetics
Absorption
The T max of fingolimod is 12 to 16 hours. The apparent absolute oral bioavailability is 93%.
Food intake does not alter C maxor (AUC) of fingolimod or fingolimod-phosphate. Therefore, fingolimod capsules may be taken without regard to meals.
Steady-state blood concentrations are reached within 1 to 2 months following once-daily administration and steady-state levels are approximately 10-fold greater than with the initial dose.
Distribution
Fingolimod highly (86%) distributes in red blood cells. Fingolimod-phosphate has a smaller uptake in blood cells of <17%. Fingolimod and fingolimod-phosphate are >99.7% protein bound. Fingolimod and fingolimod-phosphate protein binding is not altered by renal or hepatic impairment.
Fingolimod is extensively distributed to body tissues with a volume of distribution of about 1200±260 L.
Metabolism
The biotransformation of fingolimod in humans occurs by 3 main pathways: by reversible stereoselective phosphorylation to the pharmacologically active (S)-enantiomer of fingolimod-phosphate, by oxidative biotransformation catalyzed mainly by the cytochrome P450 4F2 (CYP4F2) and possibly other CYP4F isoenzymes with subsequent fatty acid-like degradation to inactive metabolites, and by formation of pharmacologically inactive non-polar ceramide analogs of fingolimod.
Inhibitors or inducers of CYP4F2 and possibly other CYP4F isozymes might alter the exposure of fingolimod or fingolimod-phosphate. In vitro studies in hepatocytes indicated that CYP3A4 may contribute to fingolimod metabolism in the case of strong induction of CYP3A4.
Following single oral administration of [ 14C] fingolimod, the major fingolimod-related components in blood, as judged from their contribution to the AUC up to 816 hours post-dose of total radiolabeled components, are fingolimod itself (23.3%), fingolimod-phosphate (10.3%), and inactive metabolites [M3 carboxylic acid metabolite (8.3%), M29 ceramide metabolite (8.9%), and M30 ceramide metabolite (7.3%)].
Elimination
Fingolimod blood clearance is 6.3±2.3 L/h, and the average apparent terminal half-life (t 1/2) is 6 to 9 days. Blood levels of fingolimod-phosphate decline in parallel with those of fingolimod in the terminal phase, yielding similar half-lives for both.
After oral administration, about 81% of the dose is slowly excreted in the urine as inactive metabolites. Fingolimod and fingolimod-phosphate are not excreted intact in urine but are the major components in the feces with amounts of each representing less than 2.5% of the dose.
Specific Populations
Pediatric PatientsThe median fingolimod-phosphate (fingolimod-P) concentration in pediatric MS patients aged 10 to less than 18 years was 1.10 ng/mL, as compared to 1.35 ng/mL in adult MS patients.
Geriatric Patients
The mechanism for elimination and results from population pharmacokinetics suggest that dose adjustment would not be necessary in elderly patients. However, clinical experience in patients aged above 65 years is limited.
Gender
Gender has no clinically significant influence on fingolimod and fingolimod-phosphate pharmacokinetics.
Race
The effects of race on fingolimod and fingolimod-phosphate pharmacokinetics cannot be adequately assessed due to a low number of non-white patients in the clinical program.
Renal Impairment
In adult patients with severe renal impairment, fingolimod C maxand AUC are increased by 32% and 43%, respectively, and fingolimod-phosphate C maxand AUC are increased by 25% and 14%, respectively, with no change in apparent elimination half-life. Based on these findings, the fingolimod hydrochloride 0.5 mg dose is appropriate for use in adult patients with renal impairment. Fingolimod hydrochloride 0.5 mg are appropriate for use in pediatric patients with renal impairment. The systemic exposure of 2 metabolites (M2 and M3) is increased by 3- and 13-fold, respectively. The toxicity of these metabolites has not been fully characterized.
A study in patients with mild or moderate renal impairment has not been conducted.
Hepatic Impairment
In subjects with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, and C), no change in fingolimod C maxwas observed, but fingolimod AUC 0-∞was increased respectively by 12%, 44%, and 103%. In patients with severe hepatic impairment (Child-Pugh class C) fingolimod-phosphate C maxwas decreased by 22% and AUC 0-96hours was decreased by 29%. The pharmacokinetics of fingolimod-phosphate was not evaluated in patients with mild or moderate hepatic impairment. The apparent elimination half-life of fingolimod is unchanged in subjects with mild hepatic impairment, but is prolonged by about 50% in patients with moderate or severe hepatic impairment.
Patients with severe hepatic impairment (Child-Pugh class C) should be closely monitored, as the risk of adverse reactions is greater [see Warnings and Precautions (5.5)] .
No dose adjustment is needed in patients with mild or moderate hepatic impairment (Child-Pugh class A and B).
Drug Interactions
Ketoconazole
The coadministration of ketoconazole (a potent inhibitor of CYP3A and CYP4F) 200 mg twice daily at steady-state and a single dose of fingolimod 5 mg led to a 70% increase in AUC of fingolimod and fingolimod-phosphate. Patients who use fingolimod hydrochloride and systemic ketoconazole concomitantly should be closely monitored, as the risk of adverse reactions is greater [ see Drug Interactions (7.2)].
Carbamazepine
The coadministration of carbamazepine (a potent CYP450 enzyme inducer) 600 mg twice daily at steady-state and a single dose of fingolimod 2 mg decreased blood concentrations (AUC) of fingolimod and fingolimod-phosphate by approximately 40%. The clinical impact of this decrease is unknown.
Other strong CYP450 enzyme inducers, e.g., rifampicin, phenytoin, phenobarbital, and St. John’s wort, may also reduce AUC of fingolimod and fingolimod-phosphate. The clinical impact of this potential decrease is unknown.
Potential of Fingolimod and Fingolimod-phosphate to Inhibit the Metabolism of Comedications
In vitro inhibition studies using pooled human liver microsomes and specific metabolic probe substrates demonstrate that fingolimod has little or no capacity to inhibit the activity of the following CYP enzymes: CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, CYP3A4/5, or CYP4A9/11 (fingolimod only) and similarly fingolimod-phosphate has little or no capacity to inhibit the activity of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, or CYP3A4 at concentrations up to 3 orders of magnitude of therapeutic concentrations. Therefore, fingolimod and fingolimod-phosphate are unlikely to reduce the clearance of drugs that are mainly cleared through metabolism by the major CYP isoenzymes described above.
Potential of Fingolimod and Fingolimod-phosphate to Induce its Own and/or the Metabolism of Comedications
Fingolimod was examined for its potential to induce human CYP3A4, CYP1A2, CYP4F2, and MDR1 (P-glycoprotein) mRNA and CYP3A, CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP4F2 activity in primary human hepatocytes. Fingolimod did not induce mRNA or activity of the different CYP enzymes and MDR1 with respect to the vehicle control; therefore, no clinically relevant induction of the tested CYP enzymes or MDR1 by fingolimod are expected at therapeutic concentrations. Fingolimod-phosphate was also examined for its potential to induce mRNA and/or activity of human CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP3A, CYP4F2, CYP4F3B, and CYP4F12. Fingolimod-phosphate is not expected to have clinically significant induction effects on these enzymes at therapeutic doses of fingolimod. In vitro experiments did not provide an indication of CYP induction by fingolimod-phosphate.
Transporters
Based on in vitro data, fingolimod as well as fingolimod-phosphate are not expected to inhibit the uptake of comedications and/or biologics transported by the organic anion transporting polypeptides OATP1B1, OATP1B3, or the sodium taurocholate co-transporting polypeptide (NTCP). Similarly, they are not expected to inhibit the efflux of comedications and/or biologics transported by the breast cancer resistance protein (BCRP), the bile salt export pump (BSEP), the multidrug resistance-associated protein 2 (MRP2), or P-glycoprotein (P-gp) at therapeutic concentrations.
Oral Contraceptives
The coadministration of fingolimod 0.5 mg daily with oral contraceptives (ethinylestradiol and levonorgestrel) did not elicit any clinically significant change in oral contraceptives exposure. Fingolimod and fingolimod-phosphate exposure were consistent with those from previous studies. No interaction studies have been performed with oral contraceptives containing other progestagens; however, an effect of fingolimod on their exposure is not expected.
Cyclosporine
The pharmacokinetics of single-dose fingolimod was not altered during coadministration with cyclosporine at steady-state, nor was cyclosporine steady-state pharmacokinetics altered by fingolimod. These data indicate that fingolimod hydrochloride is unlikely to reduce or increase the clearance of drugs cleared mainly by CYP3A4. Potent inhibition of transporters MDR1 (P-gp), MRP2, and OATP-1B1 does not influence fingolimod disposition.
Isoproterenol, Atropine, Atenolol, and Diltiazem
Single-dose fingolimod and fingolimod-phosphate exposure was not altered by coadministered isoproterenol or atropine. Likewise, the single-dose pharmacokinetics of fingolimod and fingolimod-phosphate and the steady-state pharmacokinetics of both atenolol and diltiazem were unchanged during the coadministration of the latter 2 drugs individually with fingolimod.
Population Pharmacokinetics Analysis
A population pharmacokinetics evaluation performed in MS patients did not provide evidence for a significant effect of fluoxetine and paroxetine (strong CYP2D6 inhibitors) on fingolimod or fingolimod-phosphate predose concentrations. In addition, the following commonly coprescribed substances had no clinically relevant effect (<20%) on fingolimod or fingolimod-phosphate predose concentrations: baclofen, gabapentin, oxybutynin, amantadine, modafinil, amitriptyline, pregabalin, and corticosteroids.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Oral carcinogenicity studies of fingolimod were conducted in mice and rats. In mice, fingolimod was administered at oral doses of 0, 0.025, 0.25, and 2.5 mg/kg/day for up to 2 years. The incidence of malignant lymphoma was increased in males and females at the mid and high dose. The lowest dose tested (0.025 mg/kg/day) is less than the RHD of 0.5 mg/day on a body surface area (mg/m 2) basis. In rats, fingolimod was administered at oral doses of 0, 0.05, 0.15, 0.5, and 2.5 mg/kg/day. No increase in tumors was observed. The highest dose tested (2.5 mg/kg/day) is approximately 50 times the RHD on a mg/m 2basis.
Fingolimod was negative in a battery of in vitro (Ames, mouse lymphoma thymidine kinase, chromosomal aberration in mammalian cells) and in vivo (micronucleus in mouse and rat) assays.
When fingolimod was administered orally (0, 1, 3, and 10 mg/kg/day) to male and female rats prior to and during mating, and continuing to Day 7 of gestation in females, no effect on fertility was observed up to the highest dose tested (10 mg/kg), which is approximately 200 times the RHD on a mg/m 2basis.
13.2 Animal Toxicology and/or Pharmacology
Lung toxicity was observed in 2 different strains of rats and in dogs and monkeys. The primary findings included increase in lung weight, associated with smooth muscle hypertrophy, hyperdistention of the alveoli, and/or increased collagen. Insufficient or lack of pulmonary collapse at necropsy, generally correlated with microscopic changes, was observed in all species. In rats and monkeys, lung toxicity was observed at all oral doses tested in chronic studies. The lowest doses tested in rats (0.05 mg/kg/day in the 2-year carcinogenicity study) and monkeys (0.5 mg/kg/day in the 39-week toxicity study) are similar to and approximately 20 times the RHD on a mg/m 2basis, respectively.
In the 52-week oral study in monkeys, respiratory distress associated with ketamine administration was observed at doses of 3 and 10 mg/kg/day; the most affected animal became hypoxic and required oxygenation. As ketamine is not generally associated with respiratory depression, this effect was attributed to fingolimod. In a subsequent study in rats, ketamine was shown to potentiate the bronchoconstrictive effects of fingolimod. The relevance of these findings to humans is unknown.
-
14 CLINICAL STUDIES
14.1 Adults
The efficacy of fingolimod hydrochloride was demonstrated in 2 studies that evaluated once-daily doses of fingolimod hydrochloride 0.5 mg and 1.25 mg in patients with relapsing-remitting MS (RRMS). Both studies included patients who had experienced at least 2 clinical relapses during the 2 years prior to randomization or at least 1 clinical relapse during the 1 year prior to randomization, and had an Expanded Disability Status Scale (EDSS) score from 0 to 5.5. Study 1 was a 2-year randomized, double-blind, placebo-controlled study in patients with RRMS who had not received any interferon-beta or glatiramer acetate for at least the previous 3 months and had not received any natalizumab for at least the previous 6 months. Neurological evaluations were performed at screening, every 3 months and at time of suspected relapse.
MRI evaluations were performed at screening, Month 6, Month 12, and Month 24. The primary endpoint was the annualized relapse rate.Median age was 37 years, median disease duration was 6.7 years and median EDSS score at baseline was 2.0. Patients were randomized to receive fingolimod hydrochloride 0.5 mg (N=425), 1.25 mg (N=429), or placebo (N=418) for up to 24 months. Median time on study drug was 717 days on 0.5 mg, 715 days on 1.25 mg, and 719 days on placebo.
The annualized relapse rate was significantly lower in patients treated with fingolimod hydrochloride than in patients who received placebo. The secondary endpoint was the time to 3-month confirmed disability progression as measured by at least a 1-point increase from baseline in EDSS (0.5-point increase for patients with baseline EDSS of 5.5) sustained for 3 months. Time to onset of 3-month confirmed disability progression was significantly delayed with fingolimod hydrochloride treatment compared to placebo. The 1.25 mg dose resulted in no additional benefit over the fingolimod hydrochloride 0.5 mg dose. The results for this study are shown in Table 2and Figure 1
Table 2: Clinical and MRI Results of Study 1 Abbreviation: CI, confidence interval. All analyses of clinical endpoints were intent-to–treat. MRI analysis used evaluable dataset.
‡Hazard ratio is an estimate of the relative risk of having the event of disability progression on fingolimod hydrochloride as compared to placebo.Fingolimod Hydrochloride 0.5 mg N=425 Placebo N=418 p-value Clinical endpoints Annualized relapse rate (primary endpoint) 0.18 0.40 <0.001 Percentage of patients without relapse 70% 46% <0.001 Hazard ratio ‡of disability progression
(95% CI)0.70
(0.52, 0.96)0.02 MRI endpoint Mean (median) number of new or newly enlarging T2 lesions over 24 months 2.5 (0) 9.8 (5.0) <0.001 Mean (median) number of T1 Gd-enhancing lesions at Month 24 0.2 (0) 1.1 (0) <0.001 Figure 1 Time to 3-Month Confirmed Disability Progression – Study 1 (ITT population)
Study 2 was a 1-year randomized, double-blind, double-dummy, active-controlled study in patients with RRMS who had not received any natalizumab in the previous 6 months. Prior therapy with interferon-beta or glatiramer acetate up to the time of randomization was permitted.
Neurological evaluations were performed at screening, every 3 months, and at the time of suspected relapses. MRI evaluations were performed at screening and at Month 12. The primary endpoint was the annualized relapse rate.
Median age was 36 years, median disease duration was 5.9 years, and median EDSS score at baseline was 2.0. Patients were randomized to receive fingolimod hydrochloride 0.5 mg (N=431), 1.25 mg (N=426), or interferon beta-1a, 30 mcg via the intramuscular route (IM) once weekly (N=435) for up to 12 months. Median time on study drug was 365 days on fingolimod hydrochloride 0.5 mg, 354 days on 1.25 mg, and 361 days on interferon beta-1a IM.
The annualized relapse rate was significantly lower in patients treated with fingolimod hydrochloride 0.5 mg than in patients who received interferon beta-1a IM. The key secondary endpoints were number of new and newly enlarging T2 lesions and time to onset of 3-month confirmed disability progression as measured by at least a 1-point increase from baseline in EDSS (0.5 point increase for those with baseline EDSS of 5.5) sustained for 3 months. The number of new and newly enlarging T2 lesions was significantly lower in patients treated with fingolimod hydrochloride than in patients who received interferon beta-1a IM. There was no significant difference in the time to 3-month confirmed disability progression between fingolimod hydrochloride and interferon beta-1a-treated patients at 1 year. The 1.25 mg dose resulted in no additional benefit over the fingolimod hydrochloride 0.5 mg dose. The results for this study are shown in Table 3.
Table 3: Clinical and MRI Results of Study 2 Abbreviation: CI, confidence interval. All analyses of clinical endpoints were intent-to–treat. MRI analysis used evaluable dataset.
‡Hazard ratio is an estimate of the relative risk of having the event of disability progression on fingolimod hydrochloride as compared to control.Fingolimod Hydrochloride 0.5 mg N=429 Interferon beta-1a IM30 mcgN=431 p-value Clinical endpoints Annualized relapse rate (primary endpoint) 0.16 0.33 <0.001 Percentage of patients without relapse 83% 70% <0.001 Hazard ratio‡ of disability progression
(95% CI)0.71
(0.42, 1.21)0.21 MRI endpoint Mean (median) number of new or newly enlarging T2 lesions over 12 months 1.6 (0) 2.6 (1.0) 0.002 Mean (median) number of T1 Gd-enhancing lesions at Month 12 0.2 (0) 0.5 (0) <0.001 Pooled results of study 1 and study 2 showed a consistent and statistically significant reduction of annualized relapse rate compared to comparator in subgroups defined by gender, age, prior MS therapy, and disease activity.
14.2 Pediatric Patients (10 to less than 18 Years of Age)
Study 4 (NCT 01892722) evaluated the efficacy of once-daily oral doses of fingolimod hydrochloride 0.5 mg in pediatric patients 10 to less than 18 years of age with relapsing-remitting multiple sclerosis. Study 4 was a 215-patient, double-blind, randomized, clinical trial that compared fingolimod hydrochloride to intramuscular interferon beta-1a. Prior therapy with interferon-beta, dimethyl fumarate, or glatiramer acetate up to the time of randomization was permitted. The study included patients who had experienced at least 1 clinical relapse during the year prior or 2 relapses during the 2 years prior to screening, or evidence of 1 or more Gd-enhancing lesions on MRI within 6 months prior to randomization, and had an EDSS score from 0 to 5.5. Neurological evaluations were scheduled at screening, every 3 months, and at the time of suspected relapses. MRI evaluations were performed at screening and every 6 months throughout the study. The primary endpoint was the annualized relapse rate.
At baseline, the median age was 16 years, median disease duration since first symptom was 1.5 years, and median EDSS score was 1.5. One patient received no study drug and is excluded from the analysis of efficacy. Median duration of exposure to study drug was 634 days in the fingolimod hydrochloride group (n = 107) and 547 days in the interferon beta-1a group (n=107). In the fingolimod hydrochloride group, 6.5% of patients did not complete the study, compared to 18.5% in the interferon beta-1a group.
The primary endpoint, the annualized relapse rate (ARR), was significantly lower in patients treated with fingolimod hydrochloride (0.122) than in patients who received interferon beta-1a (0.675). Relative reduction in ARR was 81.9%. The annualized rate of the number of new or newly enlarged T2 lesions up to Month 24 (key secondary endpoint) was significantly lower in patients treated with fingolimod hydrochloride, as was the number of Gd-enhancing T1 lesions per scan up to Month 24.
Table 4 summarizes the results of Study 4.
Table 4: Clinical and MRI Results of Study 4 Abbreviations: IM, intramuscular; MRI, magnetic resonance imaging; PO, by mouth All analyses of clinical endpoints were on full analysis set. MRI analyses used the evaluable dataset. *Indicates statistical significance vs. Interferon beta-1a IM at two-sided 0.05 level. Fingolimod Hydrochloride
0.5 mg
PO
N = 107Interferon
beta-1a
30 mcg IM
N = 107p-value Relative reduction Clinical endpoints Annualized relapse rate (primary endpoint) 0.122 0.675 < 0.001* 81.9% Percent of patients remaining relapse-free at 24 months 86.0% 45.8% MRI endpoints Annualized rate of the number of new or newly enlarging T2 lesions 4.393 9.269 < 0.001* 52.6% Mean number of Gd-enhancing T1 lesions per scan up to Month 24 0.436 1.282 < 0.001* 66.0% -
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
0.5 mg fingolimod capsules are bright yellow opaque/white opaque size “3” hard gelatin capsules imprinted with “FO 0.5 mg” on cap and two radial bands on the capsule body with yellow ink containing white to off white powder. Fingolimod capsules are supplied in HDPE bottle and blister packs as follow.
HDPE Bottles:
Bottles of 7 count comes in a child-resistant package: NDC: 16729-342-89
Bottles of 30 count comes in a child-resistant package: NDC: 16729-342-10
Bottles of 90 count comes in a child-resistant package: NDC: 16729-342-15
Bottles of 1000 count: NDC: 16729-342-17
Blister Packs:
Carton of 28 capsules containing 4 blister strips of 7 capsules per blister strip comes in a child-resistant package: NDC: 16729-342-88
Carton of 7 capsules containing 1 blister strip of 7 capsules per blister strip comes in a child-resistant package: NDC: 16729-342-87
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Tell patients not to discontinue fingolimod capsules without first discussing this with the prescribing physician. Advise patients to contact their physician if they accidently take more fingolimod capsules than prescribed.
Cardiac Effects
Advise patients that initiation of fingolimod hydrochloride treatment results in a transient decrease in heart rate. Inform patients that they will need to be observed in the doctor's office or other facility for at least 6 hours after the first dose, after reinitiation if treatment is interrupted or discontinued for certain periods, and after the dosage is increased. [ see Dosage and Administration (2.4), Warnings and Precautions (5.1)]
Risk of Infections
Inform patients that they may have an increased risk of infections, some of which could be life-threatening, when taking fingolimod hydrochloride, and that they should contact their physician if they develop symptoms of infection. Advise patients that the use of some vaccines should be avoided during treatment with fingolimod hydrochloride and for 2 months after discontinuation. Recommend to patients that they delay treatment with fingolimod hydrochloride until after VZV vaccination if they have not had chickenpox or a previous VZV vaccination. Inform patients that prior or concomitant use of drugs that suppress the immune system may increase the risk of infection. [ see Warnings and Precautions (5.2)]
Progressive Multifocal Leukoencephalopathy
Inform patients that cases of progressive multifocal leukoencephalopathy (PML) have occurred in patients who received fingolimod hydrochloride. Inform the patient that PML is characterized by a progression of deficits and usually leads to death or severe disability over weeks or months. Instruct the patient of the importance of contacting their doctor if they develop any symptoms suggestive of PML. Inform the patient that typical symptoms associated with PML are diverse, progress over days to weeks, and include progressive weakness on one side of the body or clumsiness of limbs, disturbance of vision, and changes in thinking, memory, and orientation leading to confusion and personality changes [see Warnings and Precautions (5.3)].
Macular Edema
Advise patients that fingolimod hydrochloride may cause macular edema, and that they should contact their physician if they experience any changes in their vision. Inform patients with diabetes mellitus or a history of uveitis that their risk of macular edema is increased. [ see Warnings and Precautions (5.4)]
Hepatic Effects
Inform patients that fingolimod hydrochloride may cause liver injury. Advise patients that they should contact their physician if they have any unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, or jaundice and/or dark urine [ see Warnings and Precautions (5.5)].
Posterior Reversible Encephalopathy Syndrome
Advise patients to immediately report to their healthcare provider any symptoms involving sudden onset of severe headache, altered mental status, visual disturbances, or seizure. Inform patients that delayed treatment could lead to permanent neurological sequelae [ see Warnings and Precautions (5.6)]
Respiratory Effects
Advise patients that they should contact their physician if they experience new onset or worsening of dyspnea. [ see Warnings and Precautions (5.7)]
Fetal Risk
- Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise females to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.8)and Use in Specific Populations (8.1, 8.3)] .
- Advise female patients of reproductive potential to use effective contraception during treatment with fingolimod capsules and for 2 months after the final dose [see Use in Specific Populations (8.3)] .
Severe Increase in Disability After Stopping Fingolimod Hydrochloride
Inform patients that severe increase in disability has been reported after discontinuation of fingolimod hydrochloride. Advise patients to contact their physician if they develop worsening symptoms of MS following discontinuation of fingolimod hydrochloride [ see Warnings and Precautions (5.9)]Malignancies
Advise patients that basal cell carcinoma and melanoma are associated with use of fingolimod hydrochloride. Advise patients that any suspicious skin lesions should be promptly evaluated. Advise patients to limit exposure to sunlight and ultraviolet light by wearing protective clothing and using a sunscreen with a high protection factor. Inform patients that lymphoma has also occurred in patients receiving fingolimod hydrochloride[ see Warnings and Precautions (5.12)]
Persistence of Fingolimod Hydrochloride Effects After Drug Discontinuation
Advise patients that fingolimod hydrochloride remains in the blood and continues to have effects, including decreased blood lymphocyte counts, for up to 2 months following the last dose. [ see Warnings and Precautions (5.13)]
Hypersensitivity Reactions
Advise patients that fingolimod hydrochloride may cause hypersensitivity reactions including rash, urticaria, and angioedema. Advise patients to contact their physician if they have any symptoms associated with hypersensitivity. [ see Warnings and Precautions (5.14)]
Pregnancy
Instruct patients that if they are pregnant or plan to become pregnant while taking fingolimod capsules they should inform their physician.
Manufactured For:
Accord Healthcare, Inc.,
8041 Arco Corporate Drive,
Suite 200,
Raleigh, NC 27617,
USA
Manufactured By:
Intas Pharmaceuticals Limited,
Plot No. : 457, 458,
Village Matoda,
Bavla Road, Ta.- Sanand,
Dist.- Ahmedabad– 382 210,
INDIA.
10 4016 1 6026128
Issued February 2024
-
MEDICATION GUIDE
This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: February 2024 MEDICATION GUIDE
Fingolimod Capsules
(fin-GOL-i-mod)Read this Medication Guide before you start taking fingolimod capsules and each time you get a refill. There may be new information. If you are the parent of a child who is being treated with fingolimod capsules, the following information applies to your child. This information does not take the place of talking to your doctor about your medical condition or your treatment.
What is the most important information I should know about fingolimod capsules?
Fingolimod capsules may cause serious side effects, including:
-
Slow heart rate (bradycardia or bradyarrhythmia) when you start taking fingolimod capsules.
Fingolimod capsules can cause your heart rate to slow down, especially after you take your first dose. You will have a test, called an electrocardiogram (ECG), to check the electrical activity of your heart before you take your first dose of fingolimod capsules. All adults and children will be observed by a healthcare professional for at least 6 hours after taking their first dose of fingolimod capsules. Children should also be observed by a healthcare professional for at least 6 hours after taking their first dose of 0.5 mg of fingolimod capsules when switching from the 0.25 mg dose.After you take your first dose of fingolimod capsules, and after a child takes their first dose of 0.5 mg of fingolimod capsules when switching from the 0.25 mg dose:- Your pulse and blood pressure should be checked every hour.
- You should be observed by a healthcare professional to see if you have any serious side effects. If your heart rate slows down too much, you may have symptoms, such as:
- dizziness
- tiredness
- feeling like your heart is beating slowly or skipping beats
- chest pain
- If you have any of the symptoms of slow heart rate, they will usually happen during the first 6 hours after your first dose of fingolimod capsules. Symptoms can happen up to 24 hours after you take your first fingolimod capsules dose.
- 6 hours after you take your first dose of fingolimod capsules you will have another ECG. If your ECG shows any heart problems or if your heart rate is still too low or continues to decrease, you will continue to be observed.
- If you have any serious side effects after your first dose of fingolimod capsules, especially those that require treatment with other medicines, you will stay in the medical facility to be observed overnight. You will also be observed for any serious side effects for at least 6 hours after you take your second dose of fingolimod capsules the next day.
- If you have certain types of heart problems, or if you are taking certain types of medicines that can affect your heart, you will be observed overnight after you take your first dose of fingolimod capsules.
Your slow heart rate will usually return to normal within 1 month after you start taking fingolimod capsules. Call your doctor or go to the nearest hospital emergency room right away if you have any symptoms of a slow heart rate.
If you miss 1 or more doses of fingolimod capsules,you may need to be observed by a healthcare professional when you take your next dose. Call your doctor if you miss a dose of fingolimod capsules. See “How should I take fingolimod capsules?”
- Pregnancy.Please consult your doctor before getting pregnant. You should avoid becoming pregnant while taking fingolimod capsules or in the two months after you stop taking it because of the risk of harm to the baby.
-
Infections.Fingolimod capsules can increase your risk of serious infections that can be life-threatening and cause death. You should not receive
livevaccines during treatment with fingolimod capsules and for 2 months after you stop taking fingolimod capsules. Talk to your doctor before you receive a vaccine during treatment and for 2 months after treatment with fingolimod capsules. If you receive a live vaccine, you may get the infection the vaccine was meant to prevent. Vaccines may not work as well when given during treatment with fingolimod capsules.
Human Papilloma Virus (HPV). Due to risk of HPV infection please consult your doctor for routine pap smear.
Fingolimod capsules lowers the number of white blood cells (lymphocytes) in your blood. This will usually go back to normal within 2 months of stopping treatment. Your doctor may do a blood test to check your white blood cells before you start taking fingolimod capsules. Call your doctor right away if you have any of these symptoms of an infection during treatment with fingolimod capsules, and for 2 months after your last dose of fingolimod capsules:
- fever
- tiredness
- body aches
- chills
- nausea
- vomiting
- headache with fever, neck stiffness, sensitivity to light, nausea, or confusion (these may be symptoms of meningitis, an infection of the lining around your brain and spine)
- 4. Progressive multifocal leukoencephalopathy (PML).PML is a rare brain infection that usually leads to death or severe disability. If PML happens, it usually happens in people with weakened immune systems but has happened in people who do not have weakened immune systems. Symptoms of PML get worse over days to weeks. Call your doctor right away if you have any new or worsening symptoms of PML, that have lasted several days, including:
- weakness on 1 side of your body
- loss of coordination in your arms and legs
- decreased strength
- problems with balance
- changes in your vision
- changes in your thinking or memory
- confusion
- changes in your personality
-
5. A problem with your vision called macular edema.Macular edema can cause some of the same vision symptoms as a multiple sclerosis (MS) attack (optic neuritis). You may not notice any symptoms with macular edema. If macular edema happens, it usually starts in the first 3 to 4 months after you start taking fingolimod capsules. Your doctor should test your vision before you start taking fingolimod capsules and 3 to 4 months after you start taking fingolimod capsules, or any time you notice vision changes during treatment with fingolimod capsules. Your risk of macular edema is higher if you have diabetes or have had an inflammation of your eye called uveitis.
Call your doctor right away if you have any of the following:
- blurriness or shadows in the center of your vision
- a blind spot in the center of your vision
- sensitivity to light
- unusually colored (tinted) vision
What are fingolimod capsules?
Fingolimod capsules are a prescription medicine used to treat relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults and children 10 years of age and older.
It is not known if fingolimod capsules are safe and effective in children under 10 years of age.Who should not take fingolimod capsules?
Do not take fingolimod capsules if you:- have had a heart attack, unstable angina, stroke or mini-stroke (transient ischemic attack or TIA) or certain types of heart failure in the last 6 months.
- have certain types of irregular or abnormal heartbeat (arrhythmia), including patients in whom a heart finding called prolonged QT is seen on ECG before starting fingolimod capsules.
- have a heart rhythm problem that needs treatment with certain medicines.
- are allergic to fingolimod or any of the ingredients in fingolimod capsules. See the end of this leaflet for a complete list of ingredients in fingolimod capsules. Symptoms of an allergic reaction may include: rash, itchy hives, or swelling of the lips, tongue or face.
What should I tell my doctor before taking fingolimod capsules?
Before you take fingolimod capsules, tell your doctor about all your medical conditions, including if you had or now have:- an irregular or abnormal heartbeat (arrhythmia).
- a history of stroke or mini-stroke.
- heart problems, including heart attack or angina.
- a history of repeated fainting (syncope).
- a fever or infection, or you are unable to fight infections due to a disease or take or have taken medicines that lower your immune system.
- recently received a vaccine or are scheduled to receive a vaccine.
- chickenpox or have received the vaccine for chickenpox. Your doctor may do a blood test for chickenpox virus. You may need to get the full course of the vaccine for chickenpox and then wait 1 month before you start taking fingolimod capsules.
- your child has completed their vaccination schedule. Your child needs to have completed their vaccination schedule before starting treatment with fingolimod capsules.
- eye problems, especially an inflammation of the eye called uveitis.
- diabetes.
- breathing problems, including during your sleep.
- liver problems.
- high blood pressure.
- types of skin cancer called basal cell carcinoma (BCC) or melanoma.
- are pregnant or plan to become pregnant. Fingolimod capsules may harm your unborn baby. Talk to your doctor if you are pregnant or are planning to become pregnant. Tell your doctor right away if you become pregnant while taking fingolimod capsules or if you become pregnant within 2 months after you stop taking fingolimod capsules.
- You should stop taking fingolimod capsules 2 months before trying to become pregnant.
- If you are a female who can become pregnant, you should use effective birth control during your treatment with fingolimod capsules and for at least 2 months after you stop taking fingolimod capsules.
- are breastfeeding or plan to breastfeed. It is not known if fingolimod hydrochloride passes into your breast milk. Talk to your doctor about the best way to feed your baby if you take fingolimod capsules.
Tell your doctor about all the medicines you take or have recently taken,including prescription and over-the- counter medicines, vitamins, and herbal supplements.
Especially tell your doctor if you take medicines that affect your immune system, including corticosteroids, or have taken them in the past.
Know the medicines you take. Keep a list of your medicines with you to show your doctor and pharmacist when you get a new medicine.
Using fingolimod capsules and other medicines together may affect each other causing serious side effects.How should I take fingolimod capsules?
- Adults and children will be observed by a healthcare professional for at least 6 hours after taking their first dose of fingolimod capsules. Children should also be observed by a healthcare professional for at least 6 hours after taking their first dose of 0.5 mg of fingolimod capsules when switching from the 0.25 mg dose. See “What is the most important information I should know about fingolimod capsules?”
- Take fingolimod capsules exactly as your doctor tells you to take it.
- Take fingolimod capsules 1 time each day.
- If you take too much fingolimod capsules, call your doctor or go to the nearest hospital emergency room right away.
- Take fingolimod capsules with or without food.
- Do not stop taking fingolimod capsules without talking with your doctor first.
- Call your doctor right away if you miss a dose of fingolimod capsules. You may need to be observed by a healthcare professional for at least 6 hours when you take your next dose. If you need to be observed by a healthcare professional when you take your next dose of fingolimod capsules you will have:
- an ECG before you take your dose
- hourly pulse and blood pressure measurements after you take the dose
- an ECG 6 hours after your dose
- If you have certain types of heart problems, or if you are taking certain types of medicines that can affect your heart, you will be observed overnight by a healthcare professional in a medical facility after you take your dose of fingolimod capsules.
- If you have serious side effects after taking a dose of fingolimod capsules, especially those that require treatment with other medicines, you will stay in the medical facility to be observed overnight. If you were observed overnight, you will also be observed for any serious side effects for at least 6 hours after you take your second dose of fingolimod capsules.
See “What is the most important information I should know about fingolimod capsules?”
What are possible side effects of fingolimod capsules?
Fingolimod capsules can cause serious side effects, including:- See “What is the most important information I should know about fingolimod capsules?”
- swelling and narrowing of the blood vessels in your brain.A condition called PRES (Posterior Reversible Encephalopathy Syndrome) has happened rarely in adults taking fingolimod capsules. Symptoms of PRES usually get better when you stop taking fingolimod capsules. However, if left untreated, it may lead to a stroke. Call your doctor right away if you have any of the following symptoms:
- sudden severe headache
- sudden confusion
- sudden loss of vision or other changes in your vision
- seizure
- liver damage.Fingolimod capsules may cause liver damage. Your doctor should do blood tests to check your liver before you start taking fingolimod capsules and periodically during treatment. Call your doctor right away if you have any of the following symptoms of liver damage:
- nausea
- vomiting
- stomach pain
- tiredness
- loss of appetite
- your skin or the whites of your eyes turn yellow
- dark urine
- breathing problems.Some people who take fingolimod capsules have shortness of breath. Call your doctor right away if you have new or worsening breathing problems.
- severe worsening of multiple sclerosis after stopping fingolimod capsules.When fingolimod capsules is stopped, symptoms of MS can return and become worse compared to before or during treatment. Many people who have worsening of MS symptoms after stopping fingolimod capsules do not return to the level of function that they had before stopping fingolimod capsules. This worsening happens most often within 12 weeks after stopping fingolimod capsules, but can happen later. Always talk to your doctor before you stop taking fingolimod capsules for any reason. Tell your doctor if you have worsening symptoms of MS after stopping fingolimod capsules.
- increased blood pressure.Your doctor should check your blood pressure during treatment with fingolimod capsules.
- types of skin cancer called basal cell carcinoma (BCC) and melanoma.Tell your doctor if you have any changes in the appearance of your skin, including changes in a mole, a new darkened area on your skin, a sore that does not heal, or growths on your skin, such as a bump that may be shiny, pearly white, skin-colored, or pink. Your doctor should check your skin for any changes during treatment with fingolimod capsules. Limit the amount of time you spend in sunlight and ultraviolet (UV) light. Wear protective clothing and use a sunscreen with a high sun protection factor.
- allergic reactions.Call your doctor if you have symptoms of an allergic reaction, including a rash, itchy hives, or swelling of the lips, tongue or face.
The most common side effects of fingolimod capsules include:
- headache
- abnormal liver tests
- diarrhea
- cough
- flu
- inflammation of the sinuses (sinusitis)
- back pain
- stomach-area (abdominal) pain
- pain in arms or legs
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of fingolimod capsules. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store fingolimod capsules?
- Store fingolimod capsules in the original bottle or blister pack in a dry place.
- Bottles of 7’s and 90’s count & blister of 7’s and 28’s count comes in a child-resistant package.
- Store fingolimod capsules at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep fingolimod capsules and all medicines out of the reach of children.
General information about the safe and effective use of fingolimod capsules.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use fingolimod capsules for a condition for which it was not prescribed. Do not give fingolimod capsules to other people, even if they have the same symptoms that you have. It may harm them. This Medication Guide summarizes the most important information about fingolimod capsules. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about fingolimod capsules that is written for health professionals.What are the ingredients in fingolimod capsules?
0.5 mg capsules
Active ingredient:fingolimod hydrochloride
Inactive ingredients:magnesium stearate, pregelatinized starch (maize).
Capsule shell contains gelatin, iron oxide yellow and titanium dioxide; Black imprinting ink contains shellac, iron oxide black and potassium hydroxide. Yellow imprinting ink contains shellac and iron oxide yellow.
Medication guide available at www.accordhealthcare.us/medication-guides
Manufactured For:Accord Healthcare, Inc.,
8041 Arco Corporate Drive,
Suite 200,
Raleigh, NC 27617,
USA.
Manufactured By:Intas Pharmaceuticals Limited,
Plot No. : 457, 458,
Village – Matoda,
Bavla Road, Ta.- Sanand,
Dist.- Ahmedabad – 382 210,
INDIA.
10 4016 1 6026128
-
Slow heart rate (bradycardia or bradyarrhythmia) when you start taking fingolimod capsules.
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FINGOLIMOD HYDROCHLORIDE
fingolimod hydrochloride capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 16729-342 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FINGOLIMOD HYDROCHLORIDE (UNII: G926EC510T) (FINGOLIMOD - UNII:3QN8BYN5QF) FINGOLIMOD 0.5 mg Inactive Ingredients Ingredient Name Strength MAGNESIUM STEARATE (UNII: 70097M6I30) STARCH, CORN (UNII: O8232NY3SJ) GELATIN (UNII: 2G86QN327L) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SHELLAC (UNII: 46N107B71O) FERROSOFERRIC OXIDE (UNII: XM0M87F357) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) Product Characteristics Color yellow (bright yellow opaque) , white (white opaque) Score no score Shape CAPSULE Size 16mm Flavor Imprint Code FO;0;5;mg Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 16729-342-89 7 in 1 BOTTLE; Type 0: Not a Combination Product 04/01/2028 2 NDC: 16729-342-10 30 in 1 BOTTLE; Type 0: Not a Combination Product 10/18/2022 3 NDC: 16729-342-15 90 in 1 BOTTLE; Type 0: Not a Combination Product 04/01/2028 4 NDC: 16729-342-17 1000 in 1 BOTTLE; Type 0: Not a Combination Product 04/01/2028 5 NDC: 16729-342-88 28 in 1 CARTON; Type 0: Not a Combination Product 04/01/2028 6 NDC: 16729-342-87 7 in 1 CARTON; Type 0: Not a Combination Product 04/01/2028 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207991 10/18/2022 Labeler - Accord Healthcare Inc. (604222237) Establishment Name Address ID/FEI Business Operations Intas Pharmaceuticals Limited 725927649 manufacture(16729-342) , analysis(16729-342)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.