These highlights do not include all the information needed to use FORFIVO XL® safely and effectively. See full prescribing information for FORFIVO XL. FORFIVO XL (bupropion hydrochloride extended-release tablets), for oral useInitial U.S. Approval: 1985
Forfivo by
Drug Labeling and Warnings
Forfivo by is a Prescription medication manufactured, distributed, or labeled by Edgemont Pharmaceuticals, LLC, Pillar5 Pharma, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
FORFIVO XL- bupropion hydrochloride tablet, film coated, extended release
Edgemont Pharmaceuticals, LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use FORFIVO XL® safely and effectively. See full prescribing information for FORFIVO XL.
FORFIVO XL (bupropion hydrochloride extended-release tablets), for oral use Initial U.S. Approval: 1985 WARNING: SUICIDAL THOUGHTS AND BEHAVIORS; AND NEUROPSYCHIATRIC REACTIONSSee full prescribing information for complete boxed warningRECENT MAJOR CHANGES
Boxed Warning 05/2017 Dosage and Administration, Discontinuation (2.4) 08/2016 Dosage and Administration, Switching To/From MAOIs (2.7) 08/2016 Dosage and Administration, Use with Reversible MAOIs (2.8) 08/2016 Contraindications, MAOIs (4) 08/2016 Warnings and Precautions, Neuropsychiatric Adverse Events (5.2) 05/2017 Warnings and Precautions, Seizure (5.3) 08/2016 Warnings and Precautions, Hypertension (5.4) 08/2016 INDICATIONS AND USAGEFORFIVO XL is an aminoketone antidepressant indicated for the treatment of major depressive disorder (MDD) (1). The efficacy was established in two 4-week trials, one 6-week trial with bupropion immediate-release formulation, and one maintenance trial with bupropion sustained-release formulation, all in adults (14). Periodically re-evaluate long-term usefulness for the individual patient (1). DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions are (incidence ≥ 5%; ≥ 2 times placebo rate): dry mouth, nausea, insomnia, dizziness, pharyngitis, abdominal pain, agitation, anxiety, tremor, palpitation, sweating, tinnitus, myalgia, anorexia, urinary frequency, rash (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Edgemont Pharmaceuticals, LLC at 1-888- 594-4332 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 8/2016 |
FULL PRESCRIBING INFORMATION
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
SUICIDALITY AND ANTIDEPRESSANT DRUGS
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short term trials. These trials did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in subjects over age 24; there was a reduction in risk with antidepressant use in subjects aged 65 and older[see Warnings and Precautions (5.1)].
In patients of all ages who are started on antidepressant therapy, monitor closely for worsening and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber. FORFIVO XL is not approved for use in pediatric patients[see Warnings and Precautions (5.1)].
1 INDICATIONS AND USAGE
FORFIVO XL (bupropion hydrochloride extended-release tablets) is indicated for the treatment of major depressive disorder (MDD), as defined by the Diagnostic and Statistical Manual (DSM).
The efficacy of the immediate-release formulation of bupropion was established in two 4-week controlled inpatient trials and one 6-week controlled outpatient trial of adult patients with MDD. The efficacy of the sustained-release formulation of bupropion in the maintenance treatment of MDD was established in a long-term (up to 44 weeks), placebo-controlled trial in patients who had responded to bupropion in an 8-week study of acute treatment [see Clinical Studies (14)].
The physician who elects to use FORFIVO XL for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
2 DOSAGE AND ADMINISTRATION
2.1 General Instructions for Use
One tablet (450 mg) of FORFIVO XL should be taken once daily without regard to meals. FORFIVO XL should be swallowed whole and not crushed, divided, or chewed.
2.2 Initial Treatment with FORFIVO XL
Do not initiate treatment with FORFIVO XL because the 450-mg tablet is the only available dose formulation. Use another bupropion formulation for initial dose titration (referring to prescribing information of other bupropion products).
FORFIVO XL can be used in patients who are receiving 300 mg/day of another bupropion formulation for at least 2 weeks, and require a dosage of 450 mg/day.
Patients who are currently being treated with other bupropion products at 450 mg/day can be switched to an equivalent dose of FORFIVO XL once daily.
2.3 Maintenance Treatment with FORFIVO XL
It is generally agreed that acute episodes of depression require several months or longer of sustained antidepressant treatment beyond the response in the acute episode. It is unknown whether the 450-mg dose needed for maintenance treatment is identical to the dose that provided an initial response. Periodically reassess the need for maintenance treatment and the appropriate dose for such treatment.
2.4 To Discontinue FORFIVO XL, Taper the Dose
Because the 450-mg tablet is the only available dose formulation, use another bupropion formulation for tapering the dose prior to discontinuation (referring to prescribing information of other bupropion products).
2.5 Patients with Impaired Hepatic Function
Because there is no lower dose strength for FORFIVO XL, FORFIVO XL is not recommended in patients with hepatic impairment [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
2.6 Patients with Impaired Renal Function
Because there is no lower dose strength for FORFIVO XL, FORFIVO XL is not recommended in patients with renal impairment [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.7 Switching a Patient To or From a Monoamine Oxidase Inhibitor (MAOI) Antidepressant
At least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of therapy with FORFIVO XL. Conversely, at least 14 days should be allowed after stopping FORFIVO XL before starting an MAOI antidepressant [see Contraindications (4) and Drug Interactions (7.6)].
2.8 Use of FORFIVO XL with Reversible MAOIs Such as Linezolid or Methylene Blue
Do not start FORFIVO XL in a patient who is being treated with a reversible MAOI such as linezolid or intravenous methylene blue. Drug interactions can increase the risk of hypertensive reactions. In a patient who requires more urgent treatment of a psychiatric condition, nonpharmacological interventions, including hospitalization, should be considered [see Contraindications (4)].
In some cases, a patient already receiving therapy with FORFIVO XL may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of hypertensive reactions in a particular patient, FORFIVO XL should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for 2 weeks or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with FORFIVO XL may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue.
The risk of administering methylene blue by nonintravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with FORFIVO XL is unclear. The clinician should, nevertheless, be aware of the possibility of a drug interaction with such use [see Contraindications (4) and Drug Interactions (7.6)].
3 DOSAGE FORMS AND STRENGTHS
FORFIVO XL Extended-Release Tablets, 450 mg of bupropion hydrochloride, are white to off-white, oblong-shaped tablets with the logo “Forfivo” printed on one side.
4 CONTRAINDICATIONS
- FORFIVO XL is contraindicated in patients with a seizure disorder [see Warnings and Precautions (5.3)].
- FORFIVO XL is contraindicated in patients treated currently with other bupropion products because the incidence of seizure is dose dependent [see Warnings and Precautions (5.3)].
- FORFIVO XL is contraindicated in patients with a current or prior diagnosis of bulimia or anorexia nervosa because a higher incidence of seizures was observed in such patients treated with bupropion [see Warnings and Precautions (5.3)].
- FORFIVO XL is contraindicated in patients undergoing abrupt discontinuation of alcohol, benzodiazepines, barbiturates, and antiepileptic drugs [see Warnings and Precautions (5.3) and Drug Interactions (7.3)].
- The use of MAOIs (intended to treat psychiatric disorders) concomitantly with FORFIVO XL or within 14 days of discontinuing treatment with FORFIVO XL is contraindicated. There is an increased risk of hypertensive reactions when FORFIVO XL is used concomitantly with MAOIs. The use of FORFIVO XL within 14 days of discontinuing treatment with an MAOI is also contraindicated. Starting FORFIVO XL in a patient treated with reversible MAOIs such as linezolid or intravenous methylene blue is contraindicated [see Dosage and Administration (2.8), Warnings and Precautions (5.4), and Drug Interactions (7.6)].
- FORFIVO XL is contraindicated in patients with known hypersensitivity to bupropion or the other ingredients of FORFIVO XL tablets. Anaphylactoid/anaphylactic reactions and Stevens-Johnson syndrome have been reported [see Warnings and Precautions (5.8)].
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults
Patients with MDD, both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment.
Pooled analyses of short-term, placebo-controlled trials of antidepressant drugs (SSRIs and others) show that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with MDD and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
|
Age Range |
Drug-Placebo Difference in Number of Cases of Suicidality per |
|
Increases Compared to Placebo |
|
|
< 18 |
14 additional cases |
|
18-24 |
5 additional cases |
|
Decreases Compared to Placebo |
|
|
25-64 |
1 fewer case |
|
≥ 65 |
6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, ie, beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases [see Boxed Warning and Use in Specific Populations (8.4)].
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania have been reported in adult and pediatric patients being treated with antidepressants for MDD as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient’s presenting symptoms.
Families and caregivers of patients being treated with antidepressants for MDD or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers [see Patient Counseling Information (17)]. Prescriptions for FORFIVO XL should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
5.2 Neuropsychiatric Adverse Events and Suicide Risk in Smoking Cessation Treatment
FORFIVO XL is not approved for smoking cessation treatment, but bupropion hydrochloride sustained-release is approved for this use. Serious neuropsychiatric adverse events have been reported in patients taking bupropion for smoking cessation. These postmarketing reports have included changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, agitation, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide [see Adverse Reactions (6.2)]. Some patients who stopped smoking may have been experiencing symptoms of nicotine withdrawal, including depressed mood. Depression, rarely including suicidal ideation, has been reported in smokers undergoing a smoking cessation attempt without medication. However, some of these adverse events occurred in patients taking bupropion who continued to smoke.
Neuropsychiatric adverse events occurred in patients without and with pre-existing psychiatric disease; some patients experienced worsening of their psychiatric illnesses. Observe patients for the occurrence of neuropsychiatric adverse events. Advise patients and caregivers that the patient should stop taking FORFIVO XL and contact a healthcare provider immediately if agitation, depressed mood, or changes in behavior or thinking that are not typical for the patient are observed, or if the patient develops suicidal ideation or suicidal behavior. In many postmarketing cases, resolution of symptoms after discontinuation of bupropion was reported. However, the symptoms persisted in some cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve.
5.3 Seizure
Bupropion can cause seizure. The risk of seizure is dose related. FORFIVO XL should be discontinued and not restarted in patients who experience a seizure while on treatment.
The risk of seizures is also related to patient factors, clinical situations, and concomitant medications that lower the seizure threshold. Consider these risks before initiating treatment with FORFIVO XL. FORFIVO XL is contraindicated in patients with a seizure disorder or conditions that increase the risk of seizure (eg, severe head injury, arteriovenous malformation, central nervous system [CNS] tumor or CNS infection, severe stroke, anorexia nervosa or bulimia, or abrupt discontinuation of alcohol, benzodiazepines, barbiturates, and antiepileptic drugs) [see Contraindications (4)]. The following conditions can also increase the risk of seizure: concomitant use of other medications that lower the seizure threshold (eg, other bupropion products, antipsychotics, tricyclic antidepressants, theophylline, and systemic corticosteroids), metabolic disorders (eg, hypoglycemia, hyponatremia, severe hepatic impairment, and hypoxia), or use of illicit drugs (eg, cocaine) or abuse or misuse of prescription drugs such as CNS stimulants. Additional predisposing conditions include diabetes mellitus treated with oral hypoglycemic drugs or insulin, use of anorectic drugs, excessive use of alcohol, use of benzodiazepines, sedatives/hypnotics, or opiates.
Incidence of Seizure with Bupropion Use
The incidence of seizure with bupropion extended-release has not been formally evaluated in clinical trials. In studies using bupropion hydrochloride sustained-release up to 300 mg/day, the incidence of seizure was approximately 0.1% (1/1000 patients). In a large prospective, follow-up study, the seizure incidence was approximately 0.4% (13/3200 patients) with bupropion hydrochloride immediate-release in the range of 300 to 450 mg/day.
Additional data accumulated for bupropion immediate-release suggests that the estimated seizure incidence increases almost tenfold between 450 and 600 mg/day. The 600-mg dose is twice the usual adult dose and one and one-third the maximum recommended daily dose (450 mg) of FORFIVO XL. This disproportionate increase in seizure incidence with dose incrementation calls for caution in dosing.
5.4 Hypertension
Treatment with FORFIVO XL can result in elevated blood pressure and hypertension. Assess blood pressure before initiating treatment with FORFIVO XL, and monitor periodically during treatment. The risk of hypertension is increased if FORFIVO XL is used concomitantly with MAOIs or other drugs that increase dopaminergic or noradrenergic activity [see Contraindications (4)].
Data from a comparative trial of the sustained-release formulation of bupropion hydrochloride, nicotine transdermal system (NTS), the combination of sustained-release bupropion hydrochloride plus NTS, and placebo as an aid to smoking cessation suggest a higher incidence of treatment-emergent hypertension in patients treated with the combination of sustained-release bupropion hydrochloride and NTS. In this trial, 6.1% of subjects treated with the combination of sustained-release bupropion and NTS had treatment-emergent hypertension compared to 2.5%, 1.6%, and 3.1% of subjects treated with sustained-release bupropion, NTS, and placebo, respectively. The majority of these subjects had evidence of pre-existing hypertension. Three subjects (1.2%) treated with the combination of sustained-release bupropion and NTS and 1 subject (0.4%) treated with NTS had study medication discontinued due to hypertension compared with none of the subjects treated with sustained-release bupropion or placebo. Monitoring of blood pressure is recommended in patients who receive the combination of bupropion and nicotine replacement.
In a clinical trial of bupropion immediate-release in MDD subjects with stable congestive heart failure (N = 36), bupropion was associated with an exacerbation of pre-existing hypertension in 2 patients, leading to discontinuation of bupropion treatment. There are no controlled studies assessing the safety of bupropion in patients with a recent history of myocardial infarction or unstable cardiac disease.
5.5 Activation of Mania/Hypomania
Antidepressant treatment can precipitate a manic, mixed, or hypomanic manic episode. The risk appears to be increased in patients with bipolar disorder or who have risk factors for bipolar disorder. Prior to initiating FORFIVO XL, screen patients for a history of bipolar disorder and the presence of risk factors for bipolar disorder (eg, family history of bipolar disorder, suicide, or depression). FORFIVO XL is not approved for the treatment of bipolar depression.
5.6 Psychosis and Other Neuropsychiatric Reactions
Depressed patients treated with bupropion have had a variety of neuropsychiatric signs and symptoms, including delusions, hallucinations, psychosis, concentration disturbance, paranoia, and confusion. Some of these patients had a diagnosis of bipolar disorder. In some cases, these symptoms abated upon dose reduction and/or withdrawal of treatment. Discontinue FORFIVO XL if these reactions occur.
5.7 Angle-closure Glaucoma
Angle-closure Glaucoma: The pupillary dilation that occurs following use of many antidepressant drugs including FORFIVO XL may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.8 Hypersensitivity Reactions
Anaphylactoid/anaphylactic reactions have occurred during clinical trials with bupropion. Reactions have been characterized by symptoms such as pruritus, urticaria, angioedema, and dyspnea, requiring medical treatment. In addition, there have been rare, spontaneous postmarketing reports of erythema multiforme, Stevens-Johnson syndrome, and anaphylactic shock associated with bupropion. Instruct patients to discontinue FORFIVO XL and consult a healthcare provider if they develop an allergic or anaphylactoid/anaphylactic reaction (eg, skin rash, pruritus, hives, chest pain, edema, and shortness of breath) during treatment.
There are reports of arthralgia, myalgia, fever with rash, and other symptoms of serum sickness suggestive of delayed hypersensitivity.
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Suicidal thoughts and behaviors in children, adolescents, and young adults [see Warnings and Precautions (5.1)]
- Neuropsychiatric symptoms and suicide risk in smoking cessation treatment [see Warnings and Precautions (5.2)]
- Seizure [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Activation of mania or hypomania [see Warnings and Precautions (5.5)]
- Psychosis and other neuropsychiatric events [see Warnings and Precautions (5.6)]
- Angle-closure Glaucoma [see Warnings and Precautions (5.7)]
- Hypersensitivity reactions [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Commonly Observed Adverse Reactions in Controlled Clinical Trials of Sustained-release Bupropion Hydrochloride
Adverse reactions that occurred in at least 5% of patients treated with bupropion hydrochloride sustained-release (300 and 400 mg/day) and at a rate at least twice the placebo rate are listed below.
300 mg/day of bupropion hydrochloride sustained-release: anorexia, dry mouth, rash, sweating, tinnitus, and tremor.
400 mg/day of bupropion hydrochloride sustained-release: abdominal pain, agitation, anxiety, dizziness, dry mouth, insomnia, myalgia, nausea, palpitation, pharyngitis, sweating, tinnitus, and urinary frequency.
FORFIVO XL is bioequivalent to three 150-mg tablets of WELLBUTRIN XL®, which has been demonstrated to have similar bioavailability both to the immediate-release and the sustained-release formulations of bupropion. The information included under this subsection and under subsection 6.2 is based primarily on data from controlled clinical trials with the sustained-release and extended-release formulations of bupropion hydrochloride.
Major Depressive Disorder
Adverse Reactions Leading to Discontinuation of Treatment with Bupropion Hydrochloride Immediate-release, Bupropion Hydrochloride Sustained-release, and Bupropion Hydrochloride Extended-release Formulations in Major Depressive Disorder Trials
In placebo-controlled clinical trials with bupropion hydrochloride sustained-release, 4%, 9%, and 11% of the placebo, 300 mg/day, and 400 mg/day groups, respectively, discontinued treatment because of adverse reactions. The specific adverse reactions leading to discontinuation in at least 1% of the 300-mg/day or 400-mg/day groups and at a rate at least twice the placebo rate are listed in Table 2.
|
Adverse Reaction Term |
Placebo
|
Bupropion Hydrochloride
|
Bupropion Hydrochloride
|
|
Rash |
0.0% |
2.4% |
0.9% |
|
Nausea |
0.3% |
0.8% |
1.8% |
|
Agitation |
0.3% |
0.3% |
1.8% |
|
Migraine |
0.3% |
0.0% |
1.8% |
In clinical trials with bupropion hydrochloride immediate-release, 10% of patients and volunteers discontinued due to an adverse reaction. Reactions resulting in discontinuation (in addition to those listed above for the sustained-release formulation) included vomiting, seizures, and sleep disturbances.
Adverse Reactions Occurring at an Incidence of > 1% in Patients Treated With Bupropion Hydrochloride Immediate-release or Bupropion Hydrochloride Sustained-release Formulations in Major Depressive Disorder Trials
Table 3 summarizes the adverse reactions that occurred in placebo-controlled trials in patients treated with bupropion hydrochloride sustained-release at 300 mg/day and 400 mg/day. These include reactions that occurred in either the 300-mg/day or 400-mg/day group at an incidence of 1% or more and were more frequent than in the placebo group.
| a = Incidence based on the number of female patients. — = Denotes adverse reactions occurring in greater than 0 but less than 0.5% of patients. |
|||||||
|
Body System/Adverse Reaction |
Placebo (n = 385) |
Bupropion Hydrochloride
|
Bupropion Hydrochloride
|
||||
|
Body (General) | |||||||
|
Headache |
23% |
26% |
25% |
||||
|
Infection |
6% |
8% |
9% |
||||
|
Abdominal pain |
2% |
3% |
9% |
||||
|
Asthenia |
2% |
2% |
4% |
||||
|
Chest pain |
1% |
3% |
4% |
||||
|
Pain |
2% |
2% |
3% |
||||
|
Fever |
— |
1% |
2% |
||||
|
Cardiovascular | |||||||
|
Palpitation |
2% |
2% |
6% |
||||
|
Flushing |
— |
1% |
4% |
||||
|
Migraine |
1% |
1% |
4% |
||||
|
Hot flashes |
1% |
1% |
3% |
||||
|
Digestive | |||||||
|
Dry mouth |
7% |
17% |
24% |
||||
|
Nausea |
8% |
13% |
18% |
||||
|
Constipation |
7% |
10% |
5% |
||||
|
Diarrhea |
6% |
5% |
7% |
||||
|
Anorexia |
2% |
5% |
3% |
||||
|
Vomiting |
2% |
4% |
2% |
||||
|
Dysphagia |
0% |
0% |
2% |
||||
|
Musculoskeletal | |||||||
|
Myalgia |
3% |
2% |
6% |
||||
|
Arthralgia |
1% |
1% |
4% |
||||
|
Arthritis |
0% |
0% |
2% |
||||
|
Twitch |
— |
1% |
2% |
||||
|
Nervous System | |||||||
|
Insomnia |
6% |
11% |
16% |
||||
|
Dizziness |
5% |
7% |
11% |
||||
|
Agitation |
2% |
3% |
9% |
||||
|
Anxiety |
3% |
5% |
6% |
||||
|
Tremor |
1% |
6% |
3% |
||||
|
Nervousness |
3% |
5% |
3% |
||||
|
Somnolence |
2% |
2% |
3% |
||||
|
Irritability |
2% |
3% |
2% |
||||
|
Memory decreased |
1% |
— |
3% |
||||
|
Paresthesia |
1% |
1% |
2% |
||||
|
Central nervous system stimulation |
1% |
2% |
1% |
||||
|
Respiratory | |||||||
|
Pharyngitis |
2% |
3% |
11% |
||||
|
Sinusitis |
2% |
3% |
1% |
||||
|
Increased cough |
1% |
1% |
2% |
||||
|
Skin | |||||||
|
Sweating |
2% |
6% |
5% |
||||
|
Rash |
1% |
5% |
4% |
||||
|
Pruritus |
2% |
2% |
4% |
||||
|
Urticaria |
0% |
2% |
1% |
||||
|
Special Senses | |||||||
|
Tinnitus |
2% |
6% |
6% |
||||
|
Taste perversion |
— |
2% |
4% |
||||
|
Blurred vision or diplopia |
2% |
3% |
2% |
||||
|
Urogenital | |||||||
|
Urinary frequency |
2% |
2% |
5% |
||||
|
Urinary urgency |
0% |
— |
2% |
||||
|
Vaginal hemorrhagea |
— |
0% |
2% |
||||
|
Urinary tract infection |
— |
1% |
0% |
||||
The following additional adverse reactions occurred in controlled trials of bupropion hydrochloride immediate-release (300 to 600 mg/day) at an incidence of at least 1% more frequently than in the placebo group: cardiac arrhythmia (5% vs 4%), hypertension (4% vs 2%), hypotension (3% vs 2%), menstrual complaints (5% vs 1%), akathisia (2% vs 1%), impaired sleep quality (4% vs 2%), sensory disturbance (4% vs 3%), confusion (8% vs 5%), decreased libido (3% vs 2%), hostility (6% vs 4%), auditory disturbance (5% vs 3%), and gustatory disturbance (3% vs 1%).
Changes in Body Weight
Table 4 presents the incidence of body weight changes (≥ 5 lbs) in the short-term MDD trials using bupropion hydrochloride sustained-release. There was a dose-related decrease in body weight.
|
Weight Change |
Placebo
|
Bupropion Hydrochloride
|
Bupropion Hydrochloride
|
|
Gained > 5 lbs |
4% |
3% |
2% |
|
Lost > 5 lbs |
6% |
14% |
19% |
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of bupropion hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body (General)—chills, facial edema, edema, peripheral edema, musculoskeletal chest pain, photosensitivity, and malaise.
Cardiovascular—postural hypotension, hypertension, stroke, vasodilation, syncope, complete atrioventricular block, extrasystoles, myocardial infarction, phlebitis, and pulmonary embolism.
Digestive—abnormal liver function, bruxism, gastric reflux, gingivitis, glossitis, increased salivation, jaundice, mouth ulcers, stomatitis, thirst, edema of tongue, colitis, esophagitis, gastrointestinal hemorrhage, gum hemorrhage, hepatitis, intestinal perforation, liver damage, pancreatitis, and stomach ulcer.
Endocrine—hyperglycemia, hypoglycemia, and syndrome of inappropriate antidiuretic hormone secretion.
Hemic and Lymphatic—ecchymosis, anemia, leukocytosis, leukopenia, lymphadenopathy, pancytopenia, and thrombocytopenia. Altered PT and/or INR, associated with hemorrhagic or thrombotic complications, were observed when bupropion was coadministered with warfarin.
Metabolic and Nutritional—glycosuria.
Musculoskeletal—leg cramps, fever/rhabdomyolysis, and muscle weakness.
Nervous System—abnormal coordination, depersonalization, emotional lability, hyperkinesia, hypertonia, hypesthesia, vertigo, amnesia, ataxia, derealization, abnormal electroencephalogram (EEG), aggression, akinesia, aphasia, coma, dysarthria, dyskinesia, dystonia, euphoria, extrapyramidal syndrome, hypokinesia, increased libido, neuralgia, neuropathy, paranoid ideation, restlessness, suicide attempt, and unmasking tardive dyskinesia.
Respiratory—bronchospasm and pneumonia.
Skin—maculopapular rash, alopecia, angioedema, exfoliative dermatitis, and hirsutism.
Special Senses—accommodation abnormality, dry eye, deafness, increased intraocular pressure, angle-closure glaucoma, and mydriasis.
Urogenital—impotence, polyuria, prostate disorder, abnormal ejaculation, cystitis, dyspareunia, dysuria, gynecomastia, menopause, painful erection, salpingitis, urinary incontinence, urinary retention, and vaginitis.
7 DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect FORFIVO XL
Bupropion is primarily metabolized to hydroxybupropion by CYP2B6. Therefore, the potential exists for drug interactions between FORFIVO XL and drugs that are inhibitors or inducers of CYP2B6.
Inhibitors of CYP2B6
Ticlopidine and Clopidogrel: Concomitant treatment with these drugs can increase bupropion exposures but decrease hydroxybupropion exposure. Coadministration of FORFIVO XL with ticlopidine or clopidogrel is not recommended [see Clinical Pharmacology (12.3)].
Inducers of CYP2B6
Ritonavir, Lopinavir,and Efavirenz: Concomitant treatment with these drugs can decrease bupropion and hydroxybupropion exposure. Patients receiving any of these drugs with bupropion may need increased doses of bupropion, but the maximum recommended dose of bupropion should not be exceeded [see Clinical Pharmacology (12.3)].
Carbamazepine, Phenobarbital, and Phenytoin: Although not systematically studied, these drugs may induce metabolism of bupropion and may decrease bupropion exposure [see Clinical Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary to increase the dose of bupropion but the maximum recommended dose should not be exceeded.
7.2 Potential for FORFIVO XL to Affect Other Drugs
Drugs Metabolized by CYP2D6
Bupropion and its metabolites (erythrohydrobupropion, threohydrobupropion, and hydroxybupropion) are CYP2D6 inhibitors. Therefore, coadministration of bupropion with drugs that are metabolized by CYP2D6 can increase the exposures of drugs that are substrates of CYP2D6. Such drugs include antidepressants (eg, venlafaxine, nortriptyline, imipramine, desipramine, paroxetine, fluoxetine, and sertraline), antipsychotics (eg, haloperidol, risperidone, and thioridazine), beta-blockers (eg, metoprolol), and Type 1C antiarrhythmics (eg, propafenone, and flecainide). When used concomitantly with bupropion, it may be necessary to decrease the dose of these CYP2D6 substrates, particularly for drugs with a narrow therapeutic index.
Drugs that require metabolic activation by CYP2D6 to be effective (eg, tamoxifen) theoretically could have reduced efficacy when administered concomitantly with inhibitors of CYP2D6 such as bupropion. Patients treated concomitantly with FORFIVO XL and such drugs may require increased doses of the drug [see Clinical Pharmacology (12.3)].
7.3 Drugs that Lower Seizure Threshold
Because there is no lower strength for FORFIVO XL, concurrent administration of FORFIVO XL tablets and agents that lower the seizure threshold (eg, other bupropion products, antipsychotics, antidepressants, theophylline, or systemic corticosteroids) should be undertaken only with extreme caution [see Warnings and Precautions (5.3)].
7.4 Dopaminergic Drugs (Levodopa and Amantadine)
Bupropion, levodopa, and amantadine have dopamine agonist effects. CNS toxicity has been reported when bupropion was coadministered with levodopa or amantadine. Adverse reactions have included restlessness, agitation, tremor, ataxia, gait disturbance, vertigo, and dizziness. It is presumed that the toxicity results from cumulative dopamine agonist effects. Because there is no lower strength for FORFIVO XL, administration of FORFIVO XL tablets to patients receiving either levodopa or amantadine concurrently should be undertaken with caution.
7.5 Use with Alcohol
In postmarketing experience, there have been rare reports of adverse neuropsychiatric events or reduced alcohol tolerance in patients who were drinking alcohol during treatment with bupropion. Alcohol increased the release rate of FORFIVO XL in vitro. The consumption of alcohol during treatment with FORFIVO XL should be avoided.
7.6 Monoamine Oxidase Inhibitors (MAOIs)
Bupropion inhibits the reuptake of dopamine and norepinephrine. Concomitant use of MAOIs and bupropion is contraindicated because there is an increased risk of hypertensive reactions if bupropion is used concomitantly with MAOIs. Studies in animals demonstrate that the acute toxicity of bupropion is enhanced by the MAOI phenelzine. At least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of treatment with FORFIVO XL. Conversely, at least 14 days should be allowed after stopping FORFIVO XL before starting an MAOI antidepressant [see Dosage and Administration (2.7, 2.8) and Contraindications (4)].
7.7 Drug-Laboratory Test Interactions
False-positive urine immunoassay screening tests for amphetamines have been reported in patients taking bupropion. This is due to lack of specificity of some screening tests. False-positive test results may result even following discontinuation of bupropion therapy. Confirmatory tests such as gas chromatography/mass spectrometry, will distinguish bupropion from amphetamines.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Risk Summary
Data from epidemiological studies including pregnant women exposed to bupropion in the first trimester indicate no increased risk of congenital malformations. All pregnancies regardless of drug exposure have a background rate of 2% to 4% for major malformations and 15% to 20% for pregnancy loss. No clear evidence of teratogenic activity was found in reproductive developmental studies conducted in rats and rabbits. However, in rabbits, slightly increased incidences of fetal malformations and skeletal variations were observed at doses approximately equal to the maximum recommended human dose (MRHD) and greater and decreased fetal weights were seen at doses twice the MRHD and greater. FORFIVO XL should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Clinical Considerations
Consider the risk of untreated depression when discontinuing or changing treatment with antidepressant medications during pregnancy and postpartum.
Human Data
Data from the international bupropion Pregnancy Registry (675 first-trimester exposures) and a retrospective cohort study using the United Healthcare database (1213 first-trimester exposures) did not show an increased risk for malformations overall.
No increased risk for cardiovascular malformations overall has been observed after bupropion exposure during the first trimester. The prospectively observed rate of cardiovascular malformations in pregnancies with exposure to bupropion in the first trimester from the international Pregnancy Registry was 1.3% (9 cardiovascular malformations/675 first-trimester maternal bupropion exposures), which is similar to the background rate of cardiovascular malformations (approximately 1%). Data from the United Healthcare database and a case-control study (6853 infants with cardiovascular malformations and 5753 with non-cardiovascular malformations) from the National Birth Defects Prevention Study (NBDPS) did not show an increased risk for cardiovascular malformations overall after bupropion exposure during the first trimester.
Study findings on bupropion exposure during the first trimester and risk for left ventricular outflow tract obstruction (LVOTO) are inconsistent and do not allow conclusions regarding possible association. The United Healthcare database lacked sufficient power to evaluate this association; the NBDPS found increased risk for LVOTO (N = 10; adjusted OR = 2.6; 95% CI: 1.2, 5.7) and the Slone Epidemiology case-control study did not find increased risk for LVOTO.
Study findings on bupropion exposure during the first trimester and risk for ventricular septal defect (VSD) are inconsistent and do not allow conclusions regarding a possible association. The Slone Epidemiology study found an increased risk for VSD following first-trimester maternal bupropion exposure (N = 17; adjusted OR = 2.5; 95% CI: 1.3, 5.0) but did not find an increased risk for any other cardiovascular malformations studied (including LVOTO, as above). The NBDPS and United Healthcare database study did not find an association between first-trimester maternal bupropion exposure and VSD.
For the findings of LVOTO and VSD, the studies were limited by the small number of exposed cases, inconsistent findings among studies, and the potential for chance findings from multiple comparisons in case-control studies.
Animal Data
In studies conducted in rats and rabbits, bupropion was administered orally at doses of up to 450 and 150 mg/kg/day, respectively (approximately 11 and 7 times the MRHD, respectively, on a mg/m2 basis), during the period of organogenesis. No clear evidence of teratogenic activity was found in either species; however, in rabbits, slightly increased incidences of fetal malformations and skeletal variations were observed at the lowest dose tested (25 mg/kg/day, approximately equal to the MRHD on a mg/m2 basis) and greater. Decreased fetal weights were observed at 50 mg/kg and greater. When rats were administered bupropion at oral doses of up to 300 mg/kg/day (approximately 7 times the MRHD on a mg/m2 basis) prior to mating and throughout pregnancy and lactation, there were no apparent adverse effects on offspring development.
8.3 Nursing Mothers
Bupropion and its metabolites are present in human milk. In a lactation study of 10 women, levels of orally dosed bupropion and its active metabolites were measured in expressed milk. The average daily infant exposure (assuming 150 mL/kg daily consumption) to bupropion and its active metabolites was 2% of the maternal weight-adjusted dose. Exercise caution when FORFIVO XL is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness in the pediatric population have not been established. When considering the use of FORFIVO XL in a child or adolescent, balance the potential risks with the clinical need [see Boxed Warning, and Warnings and Precautions (5.1)].
8.5 Geriatric Use
Of the approximately 6000 patients who participated in clinical trials with bupropion hydrochloride sustained-release tablets (depression and smoking cessation studies), 275 were ≥ 65 years of age and 47 were ≥ 75 years of age. In addition, several hundred patients ≥ 65 years of age participated in clinical trials using the immediate-release formulation of bupropion hydrochloride (depression studies). No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and excreted by the kidneys. The risk of adverse reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, it may be necessary to consider this factor in dose selection; it may be useful to monitor renal function [see Dosage and Administration (2.6), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
8.6 Renal Impairment
Because there is no lower strength for FORFIVO XL, FORFIVO XL is not recommended in patients with renal impairment [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Because there is no lower strength for FORFIVO XL, FORFIVO XL is not recommended in patients with hepatic impairment [see Clinical Pharmacology (12.3)].
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Humans
Controlled clinical studies of bupropion hydrochloride (immediate-release formulation) conducted in normal volunteers, in subjects with a history of multiple drug abuse, and in depressed patients demonstrated an increase in motor activity and agitation/excitement.
In a population of individuals experienced with drugs of abuse, a single dose of 400 mg of bupropion hydrochloride produced mild amphetamine-like activity as compared to placebo on the Morphine-Benzedrine Subscale of the Addiction Research Center Inventories (ARCI), and a score intermediate between placebo and amphetamine on the Liking Scale of the ARCI. These scales measure general feelings of euphoria and drug desirability.
Findings in clinical trials, however, are not known to reliably predict the abuse potential of drugs. Nonetheless, evidence from single-dose studies does suggest that the recommended daily dosage of bupropion when administered in divided doses is not likely to be significantly reinforcing to amphetamine or CNS-stimulant abusers. However, higher doses (that could not be tested because of the risk of seizure) might be modestly attractive to those who abuse CNS-stimulant drugs.
Bupropion hydrochloride extended-release tablets are intended for oral use only. The inhalation of crushed tablets or injection of dissolved bupropion has been reported. Seizures and/or cases of death have been reported when bupropion has been administered intranasally or by parenteral injection.
Animals
Studies in rodents and primates demonstrated that bupropion exhibits some pharmacologic actions common to psychostimulants. In rodents, it has been shown to increase locomotor activity, elicit a mild stereotyped behavioral response, and increase rates of responding in several schedule-controlled behavior paradigms. In primate models assessing the positive reinforcing effects of psychoactive drugs, bupropion was self-administered intravenously. In rats, bupropion produced amphetamine-like and cocaine-like discriminative stimulus effects in drug discrimination paradigms used to characterize the subjective effects of psychoactive drugs.
10 OVERDOSAGE
10.1 Human Overdose Experience
Overdoses of up to 30 g or more of bupropion have been reported. Seizure was reported in approximately one third of all cases. Other serious reactions reported with overdoses of bupropion alone included hallucinations, loss of consciousness, sinus tachycardia, and ECG changes such as conduction disturbances or arrhythmias. Fever, muscle rigidity, rhabdomyolysis, hypotension, stupor, coma, and respiratory failure have been reported mainly when bupropion was part of multiple drug overdoses.
Although most patients recovered without sequelae, deaths associated with overdoses of bupropion alone have been reported in patients ingesting large doses of the drug. Multiple uncontrolled seizures, bradycardia, cardiac failure, and cardiac arrest prior to death were reported in these patients.
10.2 Overdosage Management
Consult a Certified Poison Control Center for up-to-date guidance and advice. Telephone numbers for certified poison control centers are listed in the Physicians’ Desk Reference (PDR). Call 1-800-222-1222 or refer to www.poison.org.
There are no known antidotes for bupropion. In case of an overdose, provide supportive care, including close medical supervision and monitoring. Consider the possibility of multiple drug overdose.
11 DESCRIPTION
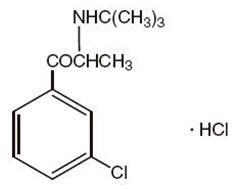
FORFIVO XL (bupropion hydrochloride), an antidepressant of the aminoketone class, is chemically unrelated to tricyclic, tetracyclic, selective serotonin re-uptake inhibitor, or other known antidepressant agents. Its structure closely resembles that of diethylpropion; it is related to phenylethylamines. It is designated as (±)-2-(tert-Butylamino)-3'-chloropropiophenone hydrochloride. The molecular weight is 276.2. The empirical formula is C13H18ClNO·HCl. Bupropion hydrochloride powder is white or almost white, crystalline, and soluble in water. It has a bitter taste and produces the sensation of local anesthesia on the oral mucosa. The structural formula is:
FORFIVO XL tablets are supplied for oral administration of 450 mg of bupropion hydrochloride as white to off-white extended-release tablets. Each film-coated tablet contains the labeled amount of bupropion hydrochloride and the inactive ingredients: hydroxypropyl cellulose, hydrochloric acid, polyvinyl pyrrolidone and polyvinyl acetate blend, polyethylene oxide, stearic acid, colloidal silicon dioxide, magnesium stearate, hydroxypropylmethyl cellulose, triacetin, talc, methacrylic acid copolymer, polyethylene glycol 8000, titanium dioxide and carboxymethyl cellulose sodium. The logo “Forfivo” is printed on one side of the tablet with edible black ink.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of bupropion is unknown, as is the case with other antidepressants. However, it is presumed that this action is mediated by noradrenergic and/or dopaminergic mechanisms. Bupropion is a relatively weak inhibitor of the neuronal uptake of norepinephrine and dopamine, and does not inhibit monoamine oxidase or the reuptake of serotonin.
12.3 Pharmacokinetics
Bupropion is a racemic mixture. The pharmacologic activity and pharmacokinetics of the individual enantiomers have not been studied.
Following single dosing under fasted conditions of FORFIVO XL tablets, the maximum peak plasma concentration (Cmax), and the area under the plasma concentration versus time curve of bupropion from zero to infinity (AUCinf), were 207.46 (± 59.40) ng/mL, and 2147.53 (± 664.12) nghr/mL, respectively. The elimination half-life (± SD) of bupropion after a single dose was 14.44 (± 5.00) hours.
In a single-dose study under fasting conditions, one FORFIVO XL tablet given once daily and three WELLBUTRIN XL 150 mg tablets once daily were evaluated. Equivalence was demonstrated for peak concentration and area under the curve for bupropion and the 3 metabolites (hydroxybupropion, erythrohydrobupropion, and threohydrobupropion).
Absorption
Following single oral administration of FORFIVO XL tablets to healthy volunteers, the median time to peak plasma concentrations for bupropion was approximately 5 hours under fasted conditions, and 12 hours under fed conditions. The presence of food did not affect the maximum peak plasma concentration for bupropion, however, mean systemic exposure to bupropion was increased by 25% when FORFIVO XL tablets were taken with food. The food effect is not considered clinically significant and FORFIVO XL can be taken with or without food.
Distribution
In vitro tests show that bupropion is 84% bound to human plasma proteins at concentrations up to 200 mcg/mL. The extent of protein binding of the hydroxybupropion metabolite is similar to that for bupropion, whereas the extent of protein binding of the threohydrobupropion metabolite is about half that of bupropion.
Metabolism
Bupropion is extensively metabolized in humans. Three metabolites are active: hydroxybupropion, which is formed via hydroxylation of the tert-butyl group of bupropion, and the amino-alcohol isomers threohydrobupropion and erythrohydrobupropion, which are formed via reduction of the carbonyl group. In vitro findings suggest that CYP2B6 is the principal isoenzyme involved in the formation of hydroxybupropion, while cytochrome P450 isoenzymes are not involved in the formation of threohydrobupropion. Oxidation of the bupropion side chain results in the formation of a glycine conjugate of meta-chlorobenzoic acid, which is then excreted as the major urinary metabolite. The potency and toxicity of the metabolites relative to bupropion have not been fully characterized. However, it has been demonstrated in an antidepressant screening test in mice that hydroxybupropion is one half as potent as bupropion, while threohydrobupropion and erythrohydrobupropion are 5-fold less potent than bupropion. This may be of clinical importance because the plasma concentrations of the metabolites are as high or higher than those of bupropion.
In humans, peak plasma concentrations of hydroxybupropion occur approximately 10 hours after administration of a single dose of FORFIVO XL under fasted conditions and 16 hours under fed conditions. Following administration of WELLBUTRIN XL, peak plasma concentrations of hydroxybupropion are approximately 7 times the peak level of the parent drug at steady state. The elimination half-life of hydroxybupropion is approximately 20 (± 5) hours, and its AUC at steady state is about 13 times that of bupropion. The times to peak concentrations for the erythrohydrobupropion and threohydrobupropion metabolites are similar to that of the hydroxybupropion metabolite. However, the elimination half-lives of erythrohydrobupropion and threohydrobupropion are longer, approximately 33 (± 10) and 37 (± 13) hours, respectively, and steady-state AUCs are 1.4 and 7 times that of bupropion, respectively.
Bupropion and its metabolites exhibit linear kinetics following chronic administration of 300 to 450 mg/day of bupropion hydrochloride.
Elimination
Following oral administration of 200 mg of 14C-bupropion in humans, 87% and 10% of the radioactive dose were recovered in the urine and feces, respectively. Only 0.5% of the oral dose was excreted as unchanged bupropion.
Population Subgroups
Factors or conditions altering metabolic capacity (eg, liver disease, congestive heart failure [CHF], age, concomitant medications, etc) or elimination may be expected to influence the degree and extent of accumulation of the active metabolites of bupropion. The elimination of the major metabolites of bupropion may be affected by reduced renal or hepatic function because they are moderately polar compounds and are likely to undergo further metabolism or conjugation in the liver prior to urinary excretion.
Renal Impairment
There is limited information on the pharmacokinetics of bupropion in patients with renal impairment. An intertrial comparison between normal subjects and patients with end-stage renal failure demonstrated that the parent drug Cmax and AUC values were comparable in the 2 groups, whereas the hydroxybupropion and threohydrobupropion metabolites had a 2.3- and 2.8-fold increase, respectively, in AUC for subjects with end-stage renal failure. A second study, comparing normal subjects and subjects with moderate to severe renal impairment (GFR 30.9 ± 10.8 mL/min) showed that after a single 150-mg dose of sustained-release bupropion, exposure to bupropion was approximately 2-fold higher in subjects with impaired renal function while levels of the hydroxybupropion and threo/erythrohydrobupropion (combined) metabolites were similar in the 2 groups. Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and subsequently excreted by the kidneys. The elimination of the major metabolites of bupropion may be reduced by impaired renal function [see Dosage and Administration (2.6) and Use in Specific Populations (8.6)].
Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of bupropion was characterized in 2 single-dose studies, one in subjects with alcoholic liver disease and one in subjects with mild to severe cirrhosis. The first trial demonstrated that the half-life of hydroxybupropion was significantly longer in 8 subjects with alcoholic liver disease than in 8 healthy volunteers (32 ± 14 hours versus 21 ± 5 hours, respectively). Although not statistically significant, the AUCs for bupropion and hydroxybupropion were more variable and tended to be greater (by 53% to 57%) in patients with alcoholic liver disease. The differences in half-life for bupropion and the other metabolites in the 2 groups were minimal.
The second trial demonstrated no statistically significant differences in the pharmacokinetics of bupropion and its active metabolites in 9 subjects with mild to moderate hepatic cirrhosis compared to 8 healthy volunteers. However, more variability was observed in some of the pharmacokinetic parameters for bupropion (AUC, Cmax, and Tmax) and its active metabolites (t½) in subjects with mild to moderate hepatic cirrhosis. In addition, in patients with severe hepatic cirrhosis, the bupropion Cmax and AUC were substantially increased (mean difference: by approximately 70% and 3-fold, respectively) and more variable when compared to values in healthy volunteers; the mean bupropion half-life was also longer (29 hours in subjects with severe hepatic cirrhosis vs 19 hours in healthy subjects). For the metabolite hydroxybupropion, the mean Cmax was approximately 69% lower. For the combined amino-alcohol isomers threohydrobupropion and erythrohydrobupropion, the mean Cmax was approximately 31% lower. The mean AUC increased by about 1.5-fold for hydroxybupropion and about 2.5-fold for threo/erythrohydrobupropion. The median Tmax was observed 19 hours later for hydroxybupropion and 31 hours later for threo/erythrohydrobupropion. The mean half-lives for hydroxybupropion and threo/erythrohydrobupropion were increased 5- and 2-fold, respectively, in patients with severe hepatic cirrhosis compared to healthy volunteers [see Dosage and Administration (2.5) and Use in Specific Populations (8.7)].
Left Ventricular Dysfunction
During a chronic dosing study with bupropion in 14 depressed patients with left ventricular dysfunction (history of CHF or an enlarged heart on x-ray), there was no apparent effect on the pharmacokinetics of bupropion or its metabolites, compared to healthy volunteers.
Age
The effects of age on the pharmacokinetics of bupropion and its metabolites have not been fully characterized, but an exploration of steady-state bupropion concentrations from several depression efficacy studies involving patients dosed in a range of 300 to 750 mg/day, on a 3 times daily schedule, revealed no relationship between age (18 to 83 years) and plasma concentration of bupropion. A single-dose pharmacokinetic study demonstrated that the disposition of bupropion and its metabolites in elderly subjects was similar to that in younger subjects. These data suggest that there is no prominent effect of age on bupropion concentration; however, another single- and multiple-dose pharmacokinetic study suggested that the elderly are at increased risk for accumulation of bupropion and its metabolites [see Use in Specific Populations (8.5)].
Gender
A single-dose study involving 12 healthy male and 12 healthy female volunteers revealed no sex-related differences in the pharmacokinetic parameters of bupropion. In addition, pooled analysis of bupropion pharmacokinetic data from 90 healthy male and 90 healthy female volunteers revealed no sex-related differences in the peak plasma concentrations of bupropion. The mean systemic exposure (AUC) was approximately 13% higher in male volunteers compared to female volunteers.
Smokers
The effects of cigarette smoking on the pharmacokinetics of bupropion hydrochloride were studied in 34 healthy male and female volunteers; 17 were chronic cigarette smokers and 17 were nonsmokers. Following oral administration of a single 150-mg dose of bupropion, there was no statistically significant difference in Cmax, half-life, Tmax, AUC, or clearance of bupropion or its active metabolites between smokers and nonsmokers.
Drug Interactions
Potential for Other Drugs to Affect FORFIVO XL
In vitro studies indicate that bupropion is primarily metabolized to hydroxybupropion by CYP2B6. Therefore, the potential exists for drug interactions between FORFIVO XL and drugs that are inhibitors or inducers of CYP2B6. In addition, in vitro studies suggest that paroxetine, sertraline, norfluoxetine, fluvoxamine, and nelfinavir, inhibit the hydroxylation of bupropion.
Inhibitors of CYP2B6
Ticlopidine, Clopidogrel: In a study in healthy male volunteers, clopidogrel 75 mg once daily or ticlopidine 250 mg twice daily increased exposures (Cmax and AUC) of bupropion by 40% and 60% for clopidogrel and by 38% and 85% for ticlopidine, respectively. The exposures of hydroxybupropion were decreased.
Prasugrel: In healthy subjects, prasugrel increased bupropion Cmax and AUC values by 14% and 18%, respectively, and decreased Cmax and AUC values of hydroxybupropion by 32% and 24%, respectively.
Cimetidine: Following oral administration of bupropion 300 mg with and without cimetidine 800 mg in 24 healthy young male volunteers, the pharmacokinetics of bupropion and hydroxybupropion were unaffected. However, there were 16% and 32% increases in the AUC and Cmax, respectively, of the combined moieties of threohydrobupropion and erythrohydrobupropion.
Citalopram: Citalopram did not affect the pharmacokinetics of bupropion and its 3 metabolites.
Inducers of CYP2B6
Ritonavir and Lopinavir: In a healthy volunteer study, ritonavir 100 mg twice daily reduced the AUC and Cmax of bupropion by 22% and 21%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 23%, threohydrobupropion decreased by 38%, and erythrohydrobupropion decreased by 48%. In a second healthy volunteer study, ritonavir 600 mg twice daily decreased the AUC and the Cmax of bupropion by 66% and 62%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 78%, threohydrobupropion decreased by 50%, and erythrohydrobupropion decreased by 68%.
In another healthy volunteer study, lopinavir 400 mg/ritonavir 100 mg twice daily decreased bupropion AUC and Cmax by 57%. The AUC and Cmax of the hydroxybupropion metabolite were decreased by 50% and 31%, respectively.
Efavirenz: In a study of healthy volunteers, efavirenz 600 mg once daily for 2 weeks reduced the AUC and Cmax of bupropion by approximately 55% and 34%, respectively. The AUC of hydroxybupropion was unchanged, whereas Cmax of hydroxybupropion was increased by 50%.
Carbamazepine, Phenobarbital, Phenytoin: Although not systematically studied, these drugs may induce the metabolism of bupropion.
Potential for FORFIVO XL to Affect Other Drugs
Animal data indicated that bupropion may be an inducer of drug-metabolizing enzymes in humans. In a study of 8 healthy male volunteers, following a 14-day administration of bupropion 100 mg 3 times daily, there was no evidence of induction of its own metabolism. Nevertheless, there may be the potential for clinically important alterations of blood levels of coadministered drugs.
Drugs Metabolized by CYP2D6
In vitro, bupropion and hydroxybupropion are CYP2D6 inhibitors. In a clinical study of 15 male subjects (19 to 35 years of age) who were extensive metabolizers of CYP2D6, bupropion given as 150 mg twice daily followed by a single dose of 50 mg desipramine increased the Cmax, AUC, and t½ of desipramine by an average of approximately 2-, 5-, and 2-fold, respectively. The effect was present for at least 7 days after the last dose of bupropion. Concomitant use of bupropion with other drugs metabolized by CYP2D6 has not been formally studied.
Citalopram: Although citalopram is not primarily metabolized by CYP2D6, in one study bupropion increased the Cmax and AUC of citalopram by 30% and 40%, respectively.
Lamotrigine: Multiple oral doses of bupropion had no statistically significant effects on the single-dose pharmacokinetics of lamotrigine in 12 healthy volunteers.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime carcinogenicity studies were performed in rats and mice at doses up to 300 and 150 mg/kg/day bupropion hydrochloride, respectively. These doses are approximately 7 and 2 times the MRHD, respectively, on a mg/m2 basis. In the rat study there was an increase in nodular proliferative lesions of the liver at doses of 100 to 300 mg/kg/day of bupropion hydrochloride (approximately 2 to 7 times the MRHD on a mg/m2 basis); lower doses were not tested. The question of whether or not such lesions may be precursors of neoplasms of the liver is currently unresolved. Similar liver lesions were not seen in the mouse study, and no increase in malignant tumors of the liver and other organs was seen in either study.
Bupropion produced a positive response (2 to 3 times control mutation rate) in 2 of 5 strains in one Ames bacterial mutagenicity assay, but was negative in another. Bupropion produced an increase in chromosomal aberrations in 1 of 3 in vivo rat bone marrow cytogenetic studies.
A fertility study in rats at doses up to 300 mg/kg/day revealed no evidence of impaired fertility.
14 CLINICAL STUDIES
The efficacy of bupropion in the treatment of MDD was established with the immediate-release formulation of bupropion hydrochloride in two 4-week, placebo-controlled trials in adult inpatients with MDD and in one 6-week, placebo-controlled trial in adult outpatients with MDD. In the first study, the bupropion dose range was 300 to 600 mg/day administered in 3 divided doses; 78% of patients were treated with doses of 300 to 450 mg/day. The trial demonstrated the efficacy of bupropion as measured by the Hamilton Depression Rating Scale (HDRS) total score, the HDRS depressed mood item (item 1), and the Clinical Global Impressions-Severity Scale (CGI-S). The second study included 2 fixed doses of bupropion (300 and 450 mg/day) and placebo. This trial demonstrated the efficacy of bupropion for only the 450-mg dose. The efficacy results were significant for the HDRS total score and the CGI-S score, but not for HDRS item 1. In the third study, outpatients were treated with bupropion at 300 mg/day. This study demonstrated the efficacy of bupropion as measured by the HDRS total score, the HDRS item 1, the Montgomery-Asberg Depression Rating Scale (MADRS), the CGI-S score, and the CGI-Improvement Scale (CGI-I) score.
A longer-term, placebo-controlled, randomized withdrawal trial demonstrated the efficacy of bupropion hydrochloride sustained-release in the maintenance treatment of MDD. The trial included adult outpatients meeting DSM-IV criteria for MDD, recurrent type, who had responded during an 8-week open-label trial of bupropion 300 mg/day. Responders were randomized to continuation of bupropion at 300 mg/day or placebo, for up to 44 weeks of observation for relapse. Response during the open-label phase was defined as a CGI-I score of 1 (very much improved) or 2 (much improved) for each of the final 3 weeks. Relapse during the double-blind phase was defined as the investigator’s judgment that drug treatment was needed for worsening depressive symptoms. Patients in the bupropion group experienced significantly lower relapse rates over the subsequent 44 weeks compared to those in the placebo group.
Although there are no independent trials demonstrating the efficacy of bupropion extended-release in the acute treatment of MDD, studies have demonstrated similar bioavailability between the immediate-, sustained-, and extended-release formulations of bupropion hydrochloride under steady-state conditions (ie, the exposures [Cmax and AUC] for bupropion and its metabolites are similar among the 3 formulations). Further, it has been demonstrated that FORFIVO XL is bioequivalent to WELLBUTRIN XL.
16 HOW SUPPLIED/STORAGE AND HANDLING
FORFIVO XL Extended-Release Tablets, 450 mg of bupropion hydrochloride, are white to off-white, oblong-shaped tablets printed with the “Forfivo” logo on one side supplied in bottles of 30 tablets
(NDC: 49909-010-30).
Store at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Inform patients, their families, and their caregivers about the benefits and risks associated with treatment with FORFIVO XL and counsel them in its appropriate use.
A patient Medication Guide about “Antidepressant Medicines, Depression and Other Serious Mental Illnesses, and Suicidal Thoughts or Actions”, “Quitting Smoking, Quit-smoking Medications, Changes in Thinking and Behavior, Depression, and Suicidal Thoughts or Actions” and “What Other Important Information Should I Know about FORFIVO XL” is available for FORFIVO XL. Instruct patients, their families, and their caregivers to read the Medication Guide and assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Advise patients regarding the following issues and to alert their prescriber if these occur while taking FORFIVO XL.
Suicidal Thoughts and Behaviors
Instruct patients, their families, and/or their caregivers to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Advise families and caregivers of patients to observe for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient’s prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Neuropsychiatric Adverse Events and Suicide Risk in Smoking Cessation Treatment
Although FORFIVO XL is not indicated for smoking cessation treatment, it contains the same active ingredient as ZYBAN® which is approved for this use. Inform patients that some patients have experienced changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, hostility, agitation, anxiety, and panic, as well as suicidal ideation and suicide when attempting to quit smoking while taking bupropion. Instruct patients to discontinue FORFIVO XL and contact a healthcare professional if they experience such symptoms.
Severe Allergic Reactions
Educate patients on the symptoms of hypersensitivity and to discontinue FORFIVO XL if they have a severe allergic reaction.
Seizure
Instruct patients to discontinue and not restart FORFIVO XL if they experience a seizure while on treatment. Advise patients that the excessive use or the abrupt discontinuation of alcohol, benzodiazepines, antiepileptic drugs, or sedatives/hypnotics can increase the risk of seizure. Advise patients to avoid the use of alcohol.
Angle-closure Glaucoma
Patients should be advised that taking FORFIVO XL can cause mild pupillary dilation, which in susceptible individuals, can lead to an episode of angle-closure glaucoma. Pre-existing glaucoma is almost always open-angle glaucoma because angle-closure glaucoma, when diagnosed, can be treated definitively with iridectomy. Open-angle glaucoma is not a risk factor for angle-closure glaucoma. Patients may wish to be examined to determine whether they are susceptible to angle closure, and have a prophylactic procedure (eg, iridectomy), if they are susceptible [see Warnings and Precautions (5.7)].
Bupropion-containing Products
Educate patients that FORFIVO XL contains the same active ingredient (bupropion) found in ZYBAN, which is used as an aid to smoking cessation treatment, and that FORFIVO XL should not be used in combination with ZYBAN or any other medications that contain bupropion hydrochloride (such as WELLBUTRIN XL, the extended-release formulation; WELLBUTRIN SR®, the sustained-release formulation; WELLBUTRIN®, the immediate-release formulation; and APLENZIN®, a bupropion hydrobromide formulation). In addition, there are a number of generic bupropion hydrochloride products for the immediate-, sustained-, and extended-release formulations.
Potential for Cognitive and Motor Impairment
Advise patients that any CNS-active drug like FORFIVO XL tablets may impair their ability to perform tasks requiring judgment or motor and cognitive skills. Advise patients that until they are reasonably certain that FORFIVO XL tablets do not adversely affect their performance, they should refrain from driving an automobile or operating complex, hazardous machinery. FORFIVO XL treatment may lead to decreased alcohol tolerance.
Concomitant Medications
Counsel patients to notify their healthcare provider if they are taking or plan to take any prescription or over-the-counter drugs, because FORFIVO XL tablets and other drugs may affect each other’s metabolism.
Pregnancy
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during therapy.
Precautions for Nursing Mothers
Communicate with the patient and pediatric healthcare provider regarding the infant’s exposure to bupropion through human milk. Instruct patients to immediately contact the infant’s healthcare provider if they note any side effect in the infant that concerns them or is persistent.
Administration Information
Instruct patients to swallow FORFIVO XL tablets whole so that the release rate is not altered. Instruct patients that FORFIVO XL tablets should not be chewed, divided, or crushed. FORFIVO XL may be taken with or without food.
FORFIVO XL is a registered trademark of IntelGenx Corporation. All other products/brand names are trademarks of their respective owners.
Manufactured by:
Pillar5 Pharma, Inc.
Arnprior, Ontario, K7S 0C9
Canada
For:
Edgemont Pharmaceuticals, LLC
Austin, TX 78746
Rev. 05/2017
MEDICATION GUIDE
FORFIVO XL ®
Fore fye' voe Eks el
(bupropion hydrochloride extended-release tablets)
IMPORTANT: Be sure to read the three sections of this Medication Guide. The first section is about the risk of changes in thinking and behavior, depression and suicidal thoughts or actions with medicines used to quit smoking; the second section is about the risk of suicidal thoughts and actions with antidepressant medicines; and the third section is entitled “What Other Important Information Should I Know About FORFIVO XL?”
Antidepressant Medicines, Depression and Other Serious Mental Illnesses, and Suicidal Thoughts or Actions
This section of the Medication Guide is only about the risk of suicidal thoughts and actions with antidepressant medicines.
What is the most important information I should know about antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions?
- Antidepressant medicines may increase the risk of suicidal thoughts or actions in some children, teenagers, or young adults within the first few months of treatment.
- Depression or other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) bipolar illness (also called manic-depressive illness) or suicidal thoughts or actions.
-
How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
- o Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed.
- o Call your healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
- o Keep all follow-up visits with your healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call your healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling very agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
What else do I need to know about antidepressant medicines?
- Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms.
- Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.
- Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.
- Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member takes. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.
- It is not known if FORFIVO XL is safe and effective in children under the age of 18.
Quitting Smoking, Quit-Smoking Medications, Changes in Thinking and Behavior, Depression, and Suicidal Thoughts or Actions
This section of the Medication Guide is only about the risk of changes in thinking and behavior, depression and suicidal thoughts or actions with drugs used to quit smoking. Although FORFIVO XL is not a treatment for quitting smoking, it contains the same active ingredient (bupropion) as ZYBAN® which is used to help patients quit smoking. Talk to your healthcare provider or your family member’s healthcare provider about:
- all risks and benefits of quit-smoking medicines.
- all treatment choices for quitting smoking.
When you try to quit smoking, with or without bupropion you may have symptoms that may be due to nicotine withdrawal, including:
- urge to smoke
- depressed mood
- trouble sleeping
- irritability
- frustration
- anger
- feeling anxious
- difficulty concentrating
- restlessness
- decreased heart rate
- increased appetite
- weight gain
Some people have even experienced suicidal thoughts when trying to quit smoking without medication. Sometimes quitting smoking can lead to worsening of mental health problems that you already have, such as depression.
Some people have had serious side effects while taking bupropion help them quit smoking, including:
New or worse mental health problems, such as changes in behavior or thinking, aggression, hostility, agitation, depression, or suicidal thoughts or actions. Some people had these symptoms when they began taking bupropion, and others developed them after several weeks of treatment, or after stopping bupropion. These symptoms happened more often in people who had a history of mental health problems before taking bupropion than in people without a history of mental health problems.
Stop taking FORFIVO XL and call your healthcare provider right away if you, your family, or caregiver notice any of these symptoms. Work with your healthcare provider to decide whether you should continue to take FORFIVO XL. In many people, these symptoms went away after stopping bupropion, but in some people symptoms continued after stopping bupropion. It is important for you to follow-up with your healthcare provider until your symptoms go away. Before taking FORFIVO XL, tell your healthcare provider if you have ever had depression or other mental health problems. You should also tell your healthcare provider about any symptoms you had during other times you tried to quit smoking, with or without bupropion.
What Other Important Information Should I Know About FORFIVO XL?
-
Seizures: There is a chance of having a seizure (convulsion, fit) with FORFIVO XL, especially in people:
- o with certain medical problems.
- o who take certain medicines.
The chance of having seizures increases with higher doses of FORFIVO XL. For more information, see the sections “Who should not take FORFIVO XL?” and “What should I tell my healthcare provider before taking FORFIVO XL?” Tell your healthcare provider about all of your medical conditions and all the medicines you take. Do not take any other medicines while you are taking FORFIVO XL unless your healthcare provider has said it is okay to take them.
If you have a seizure while taking FORFIVO XL, stop taking the tablets and call your healthcare provider right away. Do not take FORFIVO XL again if you have a seizure.
- High blood pressure (hypertension). Some people get high blood pressure that can be severe, while taking FORFIVO XL. The chance of high blood pressure may be higher if you also use nicotine replacement therapy (such as a nicotine patch) to help you stop smoking (see the section of this Medication Guide called “How should I take FORFIVO XL?”).
-
Manic episodes. Some people may have periods of mania while taking FORFIVO XL, including:
- o Greatly increased energy
- o Severe trouble sleeping
- o Racing thoughts
- o Reckless behavior
- o Unusually grand ideas
- o Excessive happiness or irritability
- o Talking more or faster than usual
- If you have any of the above symptoms of mania, call your healthcare provider.
- Unusual thoughts or behaviors. Some patients have unusual thoughts or behaviors while taking FORFIVO XL, including delusions (believe you are someone else), hallucinations (seeing or hearing things that are not there), paranoia (feeling that people are against you), or feeling confused. If this happens to you, call your healthcare provider.
-
Visual problems.
- o eye pain
- o changes in vision
- o swelling or redness in or around the eye
- Only some people are at risk for these problems. You may want to undergo an eye examination to see if you are at risk and receive preventative treatment if you are.
- Severe allergic reactions. Some people can have severe allergic reactions to FORFIVO XL. Stop taking FORFIVO XL and call your healthcare provider right away if you get a rash, itching, hives, fever, swollen lymph glands, painful sores in the mouth or around the eyes, swelling of the lips or tongue, chest pain, or have trouble breathing. These could be signs of a serious allergic reaction.
What is FORFIVO XL?
FORFIVO XL is a prescription medicine used to treat adults with a certain type of depression called major depressive disorder.
Who should not take FORFIVO XL?
Do not take FORFIVO XL if you:
- have or had a seizure disorder or epilepsy.
- have or had an eating disorder such as anorexia nervosa or bulimia.
- are taking any other medicines that contain bupropion, including WELLBUTRIN,WELLBUTRIN SR, WELLBUTRIN XL, ZYBAN or APLENZIN®. Bupropion is the same active ingredient that is in FORFIVO XL.
- take medicines called sedatives (these make you sleepy), benzodiazepines, or anti-seizure medicines, and you stop taking them all of a sudden.
-
take a monoamine oxidase inhibitor (MAOI). Ask your healthcare provider or pharmacist if you are not sure if you take an MAOI, including the antibiotic linezolid.
- o do not take an MAOI within 2 weeks of stopping FORFIVO XL unless directed to do so by your healthcare provider.
- o do not start FORFIVO XL if you stopped taking an MAOI in the last 2 weeks unless directed to do so by your healthcare provider.
- are allergic to the active ingredient in FORFIVO XL, bupropion, or to any of the inactive ingredients. See the end of this Medication Guide for a complete list of ingredients in FORFIVO XL.
What should I tell my healthcare provider before taking FORFIVO XL?
Tell your healthcare provider if you have ever had depression, suicidal thoughts or actions, or other mental health problems. You should also tell your healthcare provider about any symptoms you had during other times you tried to quit smoking, with or without bupropion. See “Quitting Smoking, Quit-Smoking Medications, Changes in Thinking and Behavior, Depression, and Suicidal Thoughts or Actions.”
Tell your healthcare provider about your other medical conditions including if you:
- have liver problems, especially cirrhosis of the liver.
- have kidney problems.
- have, or have had, an eating disorder such as anorexia nervosa or bulimia.
- have had a head injury.
- have had a seizure (convulsion, fit).
- have a tumor in your nervous system (brain or spine).
- have had a heart attack, heart problems, or high blood pressure.
- are a diabetic taking insulin or other medicines to control your blood sugar.
- drink alcohol.
- abuse prescription medicines or street drugs.
- are pregnant or plan to become pregnant.
- are breastfeeding. FORFIVO XL passes into your milk in small amounts
Tell your healthcare provider about all the medicines you take, including prescription, over-the-counter medicines, vitamins, and herbal supplements. Many medicines increase your chances of having seizures or other serious side effects if you take them while you are taking FORFIVO XL.
How should I take FORFIVO XL?
- Take FORFIVO XL exactly as prescribed by your healthcare provider. Do not change your dose or stop taking FORFIVO XL without talking with your healthcare provider first.
- Swallow FORFIVO XL tablets whole. Do not chew, cut, or crush FORFIVO XL tablets. If you do, the medicine will be released into your body too quickly. If this happens you may be more likely to get side effects including seizures. Tell your healthcare provider if you cannot swallow tablets.
- You may take FORFIVO XL with or without food.
- If you miss a dose, do not take an extra dose to make up for the dose you missed. Wait and take your next dose at the regular time. This is very important. Too much FORFIVO XL can increase your chance of having a seizure.
- If you take too much FORFIVO XL, or overdose, call your local emergency room or poison control center right away.
Do not take any other medicines while taking FORFIVO XL unless your healthcare provider has told you it is okay.
What should I avoid while taking FORFIVO XL?
- Avoid using alcohol during treatment with FORFIVO XL.
- Do not drive a car or use heavy machinery until you know how FORFIVO XL affects you. FORFIVO XL can affect your ability to do these things safely.
What are possible side effects of FORFIVO XL?
FORFIVO XL can cause serious side effects. See the sections at the beginning of this Medication Guide for information about serious side effects of FORFIVO XL.
The most common side effects of FORFIVO XL include:
- trouble sleeping
- stuffy nose
- dry mouth
- dizziness
- feeling anxious
- nausea
- constipation
- joint aches
If you have nausea, take FORFIVO XL with food.
If you have trouble sleeping, do not take FORFIVO XL too close to bedtime.
Tell your healthcare provider right away about any side effects that bother you.
These are not all the possible side effects of FORFIVO XL. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store FORFIVO XL?
Store FORFIVO XL at room temperature between 68°F and 77°F (20°C to 25°C).
Keep FORFIVO XL and all medicines out of the reach of children.
General information about the safe and effective use of FORFIVO XL
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use FORFIVO XL for a condition for which it was not prescribed. Do not give FORFIVO XL to other people, even if they have the same symptoms you have. It may harm them.
If you take a urine drug screening test, FORFIVO XL may make the test result positive for amphetamines. If you tell the person giving you the drug screening test that you are taking FORFIVO XL, they can do a more specific drug screening test that should not have this problem.
This Medication Guide summarizes important information about FORFIVO XL. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about FORFIVO XL that is written for health professionals.
For more information about FORFIVO XL, go to www.forfivoxl.com or call 1-888-594-4332.
What are the ingredients in FORFIVO XL?
Active ingredient: bupropion hydrochloride.
Inactive ingredients: hydroxypropyl cellulose, hydrochloric acid, polyvinyl pyrrolidone and polyvinyl acetate blend, polyethylene oxide, stearic acid, colloidal silicon dioxide, magnesium stearate, hydroxypropylmethyl cellulose, triacetin, talc, methacrylic acid copolymer, polyethylene glycol 8000, titanium dioxide and carboxymethyl cellulose sodium. The tablets are printed with edible black ink.
FORFIVO XL is a registered trademark of IntelGenx Corporation. All other product/brand names are trademarks of their respective owners.
Rx only
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Pillar5 Pharma, Inc.
Arnprior, Ontario, K7S 0C9
Canada
For:
Edgemont Pharmaceuticals, LLC
Austin, TX 78746
Revised May 2017
PRINCIPAL DISPLAY PANEL
Bottle Label
NDC: 49909-010-30 Rx only
Forfivo XL®
(bupropion hydrochloride
extended-release tablets)
450 mg
30 Tablets
EDGEMONT
PHARMACEUTICALS
Each Tablet Contains:
Bupropion Hydrochloride, 450 mg
Extended-Release Tablet
USUAL DOSAGE:
Take 1 tablet daily or as directed by
physician. Consult package insert
for full prescribing information.
Storage: Store at 20°C to 25°C (68°F to 77°F)
[See USP Controlled Room Temperature].
WARNING: Do not use with other medicines
that contain bupropion hydrochloride or
bupropion hydrobromide.
KEEP THIS AND ALL MEDICATIONS
OUT OF REACH OF CHILDREN
Manufactured by:
Pillar5 Pharma Inc.
365 Madawaska Blvd.
Arnprior, Ontario K7S 0C9 CANADA
For:
Edgemont Pharmaceuticals, LLC.
Austin, TX 78746
FORFIVO XL is a trademark of IntelGenx Corp.
Medication Guide to be dispensed with
each prescription.
DO NOT USE if safety seal under cap is
broken or missing.
70119-05-3 Rev. 02
| FORFIVO
XL
bupropion hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
| Labeler - Edgemont Pharmaceuticals, LLC (802662739) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pillar5 Pharma, Inc. | 243904344 | MANUFACTURE(49909-010) | |