These highlights do not include all the information needed to use THYQUIDITYTM safely and effectively. See full prescribing information for THYQUIDITYTM . THYQUIDITYTM (levothyroxine sodium) oral solution Initial U.S. Approval: 2000
THYQUIDITY by
Drug Labeling and Warnings
THYQUIDITY by is a Prescription medication manufactured, distributed, or labeled by VistaPharm, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
THYQUIDITY- levothyroxine sodium solution
VistaPharm, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use THYQUIDITYTM safely and effectively. See full prescribing information for THYQUIDITYTM.
THYQUIDITYTM (levothyroxine sodium) oral solution Initial U.S. Approval: 2000 WARNING: NOT FOR TREATMENT OF OBESITY OR FOR WEIGHT LOSSSee full prescribing information for complete boxed warningINDICATIONS AND USAGETHYQUIDITY is levothyroxine sodium (T4) indicated for:
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSOral Solution: 100 mcg per 5 mL (20 mcg per mL) in 100 mL bottles (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSAdverse reactions associated with THYQUIDITY therapy are primarily those of hyperthyroidism due to therapeutic overdosage: arrhythmias, myocardial infarction, dyspnea, muscle spasm, headache, nervousness, irritability, insomnia, tremors, muscle weakness, increased appetite, weight loss, diarrhea, heat intolerance, menstrual irregularities, and skin rash. (6) To report SUSPECTED ADVERSE REACTIONS, contact Vertice Specialty Group, a division of VistaPharm, Inc., at 1-800-470-6233 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSSee full prescribing information for drugs that affect thyroid hormone pharmacokinetics (e.g., absorption, synthesis, secretion, metabolism, protein binding, and target tissue response) and may alter the therapeutic response to THYQUIDITY. (7) See 17 for PATIENT COUNSELING INFORMATION. Revised: 9/2022 |
FULL PRESCRIBING INFORMATION
WARNING: NOT FOR TREATMENT OF OBESITY OR FOR WEIGHT LOSS
Thyroid hormones, including THYQUIDITY, either alone or with other therapeutic agents, should not be used for the treatment of obesity or for weight loss.
In euthyroid patients, doses within the range of daily hormonal requirements are ineffective for weight reduction.
Larger doses may produce serious or even life threatening manifestations of toxicity, particularly when given in association with sympathomimetic amines such as those used for their anorectic effects [see Adverse Reactions (6), Drug Interactions (7.7), and Overdosage (10)].
1 INDICATIONS AND USAGE
Hypothyroidism
THYQUIDITY is indicated as a replacement therapy in primary (thyroidal), secondary (pituitary), and tertiary (hypothalamic) congenital or acquired hypothyroidism.
Pituitary Thyrotropin (Thyroid-Stimulating Hormone, TSH) Suppression
THYQUIDITY is indicated as an adjunct to surgery and radioiodine therapy in the management of thyrotropin-dependent well-differentiated thyroid cancer.
Limitations of Use:
- THYQUIDITY is not indicated for suppression of benign thyroid nodules and nontoxic diffuse goiter in iodine-sufficient patients as there are no clinical benefits and overtreatment with THYQUIDITY may induce hyperthyroidism [see Warnings and Precautions (5.4)].
- THYQUIDITY is not indicated for treatment of hypothyroidism during the recovery phase of subacute thyroiditis.
2 DOSAGE AND ADMINISTRATION
2.1 General Administration Information
Administer THYQUIDITY as a single daily oral dose, on an empty stomach, one-half to one hour before breakfast.
Administer THYQUIDITY at least 4 hours before or after drugs known to interfere with THYQUIDITY absorption [see Drug Interactions (7.1)].
Evaluate the need for dose adjustments when regularly administering within one hour of certain foods that may affect THYQUIDITY absorption [see Drug Interactions (7.9) and Clinical Pharmacology (12.3)].
Administer THYQUIDITY directly to the mouth using a calibrated oral syringe provided by the pharmacy. A household teaspoon or tablespoon is not an adequate measuring device.
2.2 General Principles of Dosing
The dose of THYQUIDITY for hypothyroidism or pituitary TSH suppression depends on a variety of factors including: the patient's age, body weight, cardiovascular status, concomitant medical conditions (including pregnancy), concomitant medications, co-administered food and the specific nature of the condition being treated [see Dosage and Administration (2.3), Warnings and Precautions (5), and Drug Interactions (7)]. Dosing must be individualized to account for these factors and dose adjustments made based on periodic assessment of the patient's clinical response and laboratory parameters [see Dosage and Administration (2.4)].
The peak therapeutic effect of a given dose of THYQUIDITY may not be attained for 4 to 6 weeks.
2.3 Dosing in Specific Patient Populations
Primary Hypothyroidism in Adults and in Adolescents in Whom Growth and Puberty are Complete
Start THYQUIDITY at the full replacement dose in otherwise healthy, non-elderly individuals who have been hypothyroid for only a short time (such as a few months). The average full replacement dose of THYQUIDITY is approximately 1.6 mcg per kg per day (for example: 100 to 125 mcg per day for a 70 kg adult).
Adjust the dose by 12.5 to 25 mcg increments every 4 to 6 weeks until the patient is clinically euthyroid and the serum TSH returns to normal. Doses greater than 200 mcg per day are seldom required. An inadequate response to daily doses of greater than 300 mcg per day is rare and may indicate poor compliance, malabsorption, drug interactions, or a combination of these factors.
For elderly patients or patients with underlying cardiac disease, start with a dose of 12.5 to 25 mcg per day. Increase the dose every 6 to 8 weeks, as needed, until the patient is clinically euthyroid and the serum TSH returns to normal. The full replacement dose of THYQUIDITY may be less than 1 mcg per kg per day in elderly patients.
In patients with severe longstanding hypothyroidism, start with a dose of 12.5 to 25 mcg per day. Adjust the dose in 12.5 to 25 mcg increments every 2 to 4 weeks until the patient is clinically euthyroid and the serum TSH level is normalized.
Secondary or Tertiary Hypothyroidism
Start THYQUIDITY at the full replacement dose in otherwise healthy, non-elderly individuals. Start with a lower dose in elderly patients, patients with underlying cardiovascular disease or patients with severe longstanding hypothyroidism as described above. Serum TSH is not a reliable measure of THYQUIDITY dose adequacy in patients with secondary or tertiary hypothyroidism and should not be used to monitor therapy. Use the serum free-T4 level to monitor adequacy of therapy in this patient population. Titrate THYQUIDITY dosing per above instructions until the patient is clinically euthyroid and the serum free-T4 level is restored to the upper half of the normal range.
Pediatric Dosage - Congenital or Acquired Hypothyroidism
The recommended daily dose of THYQUIDITY in pediatric patients with hypothyroidism is based on body weight and changes with age as described in Table 1. Start THYQUIDITY at the full daily dose in most pediatric patients. Start at a lower starting dose in newborns (0-3 months) at risk for cardiac failure and in children at risk for hyperactivity (see below). Monitor for clinical and laboratory response [see Dosage and Administration (2.4)].
Table 1. THYQUIDITY Dosing Guidelines for Pediatric Hypothyroidism
|
AGE |
Daily Dose Per Kg Body Weighta |
|
0-3 months |
10-15 mcg/kg/day |
|
3-6 months |
8-10 mcg/kg/day |
|
6-12 months |
6-8 mcg/kg/day |
|
1-5 years |
5-6 mcg/kg/day |
|
6-12 years |
4-5 mcg/kg/day |
|
Greater than 12 years but growth and puberty incomplete |
2-3 mcg/kg/day |
|
Growth and puberty complete |
1.6 mcg/kg/day |
|
a. The dose should be adjusted based on clinical response and laboratory parameters [see Dosage and Administration (2.4) and Use in Specific Populations (8.4)]. |
|
Newborns (0-3 months) at risk for cardiac failure: Consider a lower starting dose in newborns at risk for cardiac failure. Increase the dose every 4 to 6 weeks as needed based on clinical and laboratory response.
Children at risk for hyperactivity: To minimize the risk of hyperactivity in children, start at one-fourth the recommended full replacement dose, and increase on a weekly basis by one-fourth the full recommended replacement dose until the full recommended replacement dose is reached.
Pregnancy
Pre-existing Hypothyroidism: THYQUIDITY dose requirements may increase during pregnancy. Measure serum TSH and free-T4 as soon as pregnancy is confirmed and, at a minimum, during each trimester of pregnancy. In patients with primary hypothyroidism, maintain serum TSH in the trimester-specific reference range. For patients with serum TSH above the normal trimester- specific range, increase the dose of THYQUIDITY by 12.5 to 25 mcg/day and measure TSH every 4 weeks until a stable THYQUIDITY dose is reached and serum TSH is within the normal trimester-specific range. Reduce THYQUIDITY dosage to pre-pregnancy levels immediately after delivery and measure serum TSH levels 4 to 8 weeks postpartum to ensure THYQUIDITY dose is appropriate.
New Onset Hypothyroidism: Normalize thyroid function as rapidly as possible. Evaluate serum TSH every 4 weeks and adjust THYQUIDITY dosage until a serum TSH is within the normal trimester specific range [see Use in Specific Populations (8.1)].
TSH Suppression in Well-differentiated Thyroid Cancer
Generally, TSH is suppressed to below 0.1 mIU per liter, and this usually requires a THYQUIDITY dose of greater than 2 mcg per kg per day. However, in patients with high-risk tumors, the target level for TSH suppression may be lower.
2.4 Monitoring TSH and/or Thyroxine (T4) Levels
Assess the adequacy of therapy by periodic assessment of laboratory tests and clinical evaluation. Persistent clinical and laboratory evidence of hypothyroidism, despite an apparent adequate replacement dose of THYQUIDITY, may be evidence of inadequate absorption, poor compliance, drug interactions, or a combination of these factors.
Adults
In adult patients with primary hypothyroidism, monitor serum TSH levels after an interval of 6 to 8 weeks after any change in dose. In patients on a stable and appropriate replacement dose, evaluate clinical and biochemical response every 6 to 12 months and whenever there is a change in the patient’s clinical status.
Pediatrics
In patients with congenital hypothyroidism, assess the adequacy of replacement therapy by measuring both serum TSH and total or free-T4. Monitor TSH and total or free-T4 in children as follows: 2 and 4 weeks after the initiation of treatment, 2 weeks after any change in dosage, and then every 3 to 12 months thereafter following dose stabilization until growth is completed. Poor compliance or abnormal values may necessitate more frequent monitoring. Perform routine clinical examination, including assessment of development, mental and physical growth, and bone maturation, at regular intervals.
Although the general aim of therapy is to normalize the serum TSH level, TSH may not normalize in some patients due to in utero hypothyroidism causing a resetting of pituitary-thyroid feedback. Failure of the serum T4 to increase into the upper half of the normal range within 2 weeks of initiation of THYQUIDITY therapy and/or of the serum TSH to decrease below 20 mIU per liter within 4 weeks may indicate the child is not receiving adequate therapy. Assess compliance, dose of medication administered, and method of administration prior to increasing the dose of THYQUIDITY [see Warnings and Precautions (5.4) and Use in Specific Populations (8.4)].
Secondary and Tertiary Hypothyroidism
Monitor serum free-T4 levels and maintain in the upper half of the normal range in these patients.
3 DOSAGE FORMS AND STRENGTHS
Oral Solution: 100 mcg per 5 mL (20 mcg per mL) clear, colorless to nearly colorless solution in 100 mL bottles
THYQUIDITY is to be used with a calibrated oral syringe provided by the pharmacy.
4 CONTRAINDICATIONS
THYQUIDITY is contraindicated in patients with:
- Uncorrected adrenal insufficiency [see Warnings and Precautions (5.3)].
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Adverse Reactions in the Elderly and in Patients with Underlying Cardiovascular Disease
Over-treatment with levothyroxine may cause an increase in heart rate, cardiac wall thickness, and cardiac contractility and may precipitate angina or arrhythmias, particularly in patients with cardiovascular disease and in elderly patients. Initiate THYQUIDITY therapy in this population at lower doses than those recommended in younger individuals or in patients without cardiac disease [see Dosage and Administration (2.3), Use in Specific Populations (8.5)].
Monitor for cardiac arrhythmias during surgical procedures in patients with coronary artery disease receiving suppressive THYQUIDITY therapy. Monitor patients receiving concomitant THYQUIDITY and sympathomimetic agents for signs and symptoms of coronary insufficiency.
If cardiac symptoms develop or worsen, reduce the THYQUIDITY dose or withhold for one week and restart at a lower dose.
5.2 Myxedema Coma
Myxedema coma is a life-threatening emergency characterized by poor circulation and hypometabolism, and may result in unpredictable absorption of levothyroxine sodium from the gastrointestinal tract. Use of oral thyroid hormone drug products is not recommended to treat myxedema coma. Administer thyroid hormone products formulated for intravenous administration to treat myxedema coma.
5.3 Acute Adrenal Crisis in Patients with Concomitant Adrenal Insufficiency
Thyroid hormone increases metabolic clearance of glucocorticoids. Initiation of thyroid hormone therapy prior to initiating glucocorticoid therapy may precipitate an acute adrenal crisis in patients with adrenal insufficiency. Treat patients with adrenal insufficiency with replacement glucocorticoids prior to initiating treatment with THYQUIDITY [see Contraindications (4)].
5.4 Prevention of Hyperthyroidism or Incomplete Treatment of Hypothyroidism
THYQUIDITY has a narrow therapeutic index. Over- or undertreatment with THYQUIDITY may have negative effects on growth and development, cardiovascular function, bone metabolism, reproductive function, cognitive function, emotional state, gastrointestinal function, and glucose and lipid metabolism [see Use in Specific Populations - Pediatric Use (8.4)]. Titrate the dose of THYQUIDITY carefully and monitor response to titration to avoid these effects [see Dosage and Administration (2.4)]. Monitor for the presence of drug or food interactions when using THYQUIDITY and adjust the dose as necessary [see Drug Interactions (7.9) and Clinical Pharmacology (12.3)].
5.5 Worsening of Diabetic Control
Addition of levothyroxine therapy in patients with diabetes mellitus may worsen glycemic control and result in increased antidiabetic agent or insulin requirements. Carefully monitor glycemic control after starting, changing, or discontinuing THYQUIDITY [see Drug Interactions (7.2)].
5.6 Decreased Bone Mineral Density Associated with Thyroid Hormone Over-Replacement
Increased bone resorption and decreased bone mineral density may occur as a result of levothyroxine over-replacement, particularly in post-menopausal women. The increased bone resorption may be associated with increased serum levels and urinary excretion of calcium and phosphorous, elevations in bone alkaline phosphatase, and suppressed serum parathyroid hormone levels. Administer the minimum dose of THYQUIDITY that achieves the desired clinical and biochemical response to mitigate this risk.
6 ADVERSE REACTIONS
Adverse reactions associated with THYQUIDITY therapy are primarily those of hyperthyroidism due to therapeutic overdosage [see Warnings and Precautions (5), Overdosage (10)]. They include the following:
- General: fatigue, increased appetite, weight loss, heat intolerance, fever, excessive sweating
- Central nervous system: headache, hyperactivity, nervousness, anxiety, irritability, emotional lability, insomnia
- Musculoskeletal: tremors, muscle weakness, muscle spasm
- Cardiovascular: palpitations, tachycardia, arrhythmias, increased pulse and blood pressure, heart failure, angina, myocardial infarction, cardiac arrest
- Respiratory: dyspnea
- Gastrointestinal: diarrhea, vomiting, abdominal cramps, elevations in liver function tests
- Dermatologic: hair loss, flushing, rash
- Endocrine: decreased bone mineral density
- Reproductive: menstrual irregularities, impaired fertility
Seizures have been reported rarely with the institution of levothyroxine therapy.
Adverse Reactions in Children
Pseudotumor cerebri and slipped capital femoral epiphysis have been reported in children receiving levothyroxine therapy. Overtreatment may result in craniosynostosis in infants and premature closure of the epiphyses in children with resultant compromised adult height.
Hypersensitivity Reactions
Hypersensitivity reactions to inactive ingredients have occurred in patients treated with thyroid hormone products. These include urticaria, pruritus, skin rash, flushing, angioedema, various gastrointestinal symptoms (abdominal pain, nausea, vomiting and diarrhea), fever, arthralgia, serum sickness, and wheezing. Hypersensitivity to levothyroxine itself is not known to occur.
7 DRUG INTERACTIONS
7.1 Drugs Known to Affect Thyroid Hormone Pharmacokinetics
Many drugs can exert effects on thyroid hormone pharmacokinetics (e.g., absorption, synthesis, secretion, metabolism, protein binding, and target tissue response) and may alter the therapeutic response to THYQUIDITY (see Tables 2-5 below).
Table 2. Drugs That May Decrease T4 Absorption (Hypothyroidism)
|
Potential impact: Concurrent use may reduce the efficacy of THYQUIDITY by binding and delaying or preventing absorption, potentially resulting in hypothyroidism. |
|
|
Drug or Drug Class |
Effect |
|
Calcium Carbonate Ferrous Sulfate |
Calcium carbonate may form an insoluble chelate with levothyroxine, and ferrous sulfate likely forms a ferric- thyroxine complex. Administer THYQUIDITY at least 4 hours apart from these agents. |
|
Orlistat |
Monitor patients treated concomitantly with orlistat and THYQUIDITY for changes in thyroid function. |
|
Bile Acid Sequestrants -Colesevelam -Cholestyramine -Colestipol Ion Exchange Resins -Kayexalate -Sevelamer |
Bile acid sequestrants and ion exchange resins are known to decrease levothyroxine absorption. Administer THYQUIDITY at least 4 hours prior to these drugs or monitor TSH levels. |
|
Other drugs: Proton Pump Inhibitors Sucralfate Antacids - Aluminum & Magnesium Hydroxides - Simethicone |
Gastric acidity is an essential requirement for adequate absorption of levothyroxine. Sucralfate, antacids and proton pump inhibitors may cause hypochlorhydria, affect intragastric pH, and reduce levothyroxine absorption. Monitor patients appropriately. |
Table 3. Drugs That May Alter T4 and Triiodothyronine (T3) Serum Transport Without Affecting Free Thyroxine (FT4) Concentration (Euthyroidism)
|
Drug or Drug Class |
Effect |
|
Clofibrate Estrogen-containing oral contraceptives Estrogens (oral) Heroin / Methadone 5-Fluorouracil Mitotane Tamoxifen |
These drugs may increase serum thyroxine-binding globulin (TBG) concentration. |
|
Androgens / Anabolic Steroids Asparaginase Glucocorticoids Slow-Release Nicotinic Acid |
These drugs may decrease serum TBG concentration. |
|
Potential impact (below): Administration of these agents with THYQUIDITY results in an initial transient increase in FT4. Continued administration results in a decrease in serum T4 and normal FT4 and TSH concentrations. |
|
|
Salicylates (> 2 g/day) |
Salicylates inhibit binding of T4 and T3 to TBG and transthyretin. An initial increase in serum FT4 is followed by return of FT4 to normal levels with sustained therapeutic serum salicylate concentrations, although total T4 levels may decrease by as much as 30%. |
|
Other drugs: Carbamazepine Furosemide (> 80 mg IV) Heparin Hydantoins Non-Steroidal Anti-inflammatory Drugs -Fenamates |
These drugs may cause protein-binding site displacement. Furosemide has been shown to inhibit the protein binding of T4 to TBG and albumin, causing an increase free T4 fraction in serum. Furosemide competes for T4-binding sites on TBG, prealbumin, and albumin, so that a single high dose can acutely lower the total T4 level. Phenytoin and carbamazepine reduce serum protein binding of levothyroxine, and total and free T4 may be reduced by 20% to 40%, but most patients have normal serum TSH levels and are clinically euthyroid. Closely monitor thyroid hormone parameters. |
Table 4. Drugs That May Alter Hepatic Metabolism of T4 (Hypothyroidism)
|
Potential impact: Stimulation of hepatic microsomal drug-metabolizing enzyme activity may cause increased hepatic degradation of levothyroxine, resulting in increased THYQUIDITY requirements. |
|
|
Drug or Drug Class |
Effect |
|
Phenobarbital Rifampin |
Phenobarbital has been shown to reduce the response to thyroxine. Phenobarbital increases L-thyroxine metabolism by inducing uridine 5’-diphospho-glucuronosyltransferase (UGT) and leads to a lower T4 serum levels. Changes in thyroid status may occur if barbiturates are added or withdrawn from patients being treated for hypothyroidism. Rifampin has been shown to accelerate the metabolism of levothyroxine. |
Table 5. Drugs That May Decrease Conversion of T4 to T3
|
Potential impact: Administration of these enzyme inhibitors decreases the peripheral conversion of T4 to T3, leading to decreased T3 levels. However, serum T4 levels are usually normal but may occasionally be slightly increased. |
|
|
Drug or Drug Class |
Effect |
|
Beta-adrenergic antagonists (e.g., Propranolol > 160 mg/day) |
In patients treated with large doses of propranolol (> 160 mg/day), T3 and T4 levels change, TSH levels remain normal, and patients are clinically euthyroid. Actions of particular beta-adrenergic antagonists may be impaired when the hypothyroid patient is converted to the euthyroid state. |
|
Glucocorticoids (e.g., Dexamethasone > 4 mg/day) |
Short-term administration of large doses of glucocorticoids may decrease serum T3 concentrations by 30% with minimal change in serum T4 levels. However, long-term glucocorticoid therapy may result in slightly decreased T3 and T4 levels due to decreased TBG production (See above). |
|
Other drugs: Amiodarone |
Amiodarone inhibits peripheral conversion of levothyroxine (T4) to triiodothyronine (T3) and may cause isolated biochemical changes (increase in serum free-T4, and decrease or normal free-T3) in clinically euthyroid patients. |
7.2 Antidiabetic Therapy
Addition of THYQUIDITY therapy in patients with diabetes mellitus may worsen glycemic control and result in increased antidiabetic agent or insulin requirements. Carefully monitor glycemic control, especially when thyroid therapy is started, changed, or discontinued [see Warnings and Precautions (5.5)].
7.3 Oral Anticoagulants
THYQUIDITY increases the response to oral anticoagulant therapy. Therefore, a decrease in the dose of anticoagulant may be warranted with correction of the hypothyroid state or when the THYQUIDITY dose is increased. Closely monitor coagulation tests to permit appropriate and timely dosage adjustments.
7.4 Digitalis Glycosides
THYQUIDITY may reduce the therapeutic effects of digitalis glycosides. Serum digitalis glycoside levels may decrease when a hypothyroid patient becomes euthyroid, necessitating an increase in the dose of digitalis glycosides.
7.5 Antidepressant Therapy
Concurrent use of tricyclic (e.g., amitriptyline) or tetracyclic (e.g., maprotiline) antidepressants and THYQUIDITY may increase the therapeutic and toxic effects of both drugs, possibly due to increased receptor sensitivity to catecholamines. Toxic effects may include increased risk of cardiac arrhythmias and central nervous system stimulation. THYQUIDITY may accelerate the onset of action of tricyclics. Administration of sertraline in patients stabilized on THYQUIDITY may result in increased THYQUIDITY requirements.
7.6 Ketamine
Concurrent use of ketamine and THYQUIDITY may produce marked hypertension and tachycardia. Closely monitor blood pressure and heart rate in these patients
7.7 Sympathomimetics
Concurrent use of sympathomimetics and THYQUIDITY may increase the effects of sympathomimetics or thyroid hormone. Thyroid hormones may increase the risk of coronary insufficiency when sympathomimetic agents are administered to patients with coronary artery disease.
7.8 Tyrosine-Kinase Inhibitors
Concurrent use of tyrosine-kinase inhibitors such as imatinib may cause hypothyroidism. Closely monitor TSH levels in such patients.
7.9 Drug-Food Interactions
Consumption of certain foods may affect THYQUIDITY absorption thereby necessitating adjustments in dosing [see Dosage and Administration (2.1)]. Soybean products, such as infant formula and soybean flour, cottonseed meal, walnuts, and dietary fiber may bind and decrease the absorption of THYQUIDITY from the gastrointestinal tract. Grapefruit juice may delay the absorption of levothyroxine and reduce its bioavailability.
7.10 Drug-Laboratory Test Interactions
Consider changes in TBG concentration when interpreting T4 and T3 values. Measure and evaluate unbound (free) hormone and/or determine the free-T4 index (FT4I) in this circumstance. Pregnancy, infectious hepatitis, estrogens, estrogen-containing oral contraceptives, and acute intermittent porphyria increase TBG concentration. Nephrosis, severe hypoproteinemia, severe liver disease, acromegaly, androgens, and corticosteroids decrease TBG concentration. Familial hyper- or hypo-thyroxine binding globulinemias have been described, with the incidence of TBG deficiency approximating 1 in 9000.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Prolonged experience with levothyroxine use in pregnant women, including data from post-marketing studies, to maintain a euthyroid state have not reported increased rates of major birth defects, miscarriages, or adverse maternal or fetal outcomes. There are risks to the mother and fetus associated with untreated hypothyroidism in pregnancy. Since TSH levels may increase during pregnancy, TSH should be monitored and THYQUIDITY dosage adjusted during pregnancy (see Clinical Considerations). There are no animal studies conducted with levothyroxine during pregnancy. THYQUIDITY should not be discontinued during pregnancy and hypothyroidism diagnosed during pregnancy should be promptly treated.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Maternal hypothyroidism during pregnancy is associated with a higher rate of complications, including spontaneous abortion, gestational hypertension, pre-eclampsia, stillbirth, and premature delivery. Untreated maternal hypothyroidism may have an adverse effect on fetal neurocognitive development.
Dose Adjustments During Pregnancy and the Postpartum Period
Pregnancy may increase THYQUIDITY requirements. Serum TSH levels should be monitored and the THYQUIDITY dosage adjusted during pregnancy to maintain TSH within normal trimester specific ranges. Since postpartum TSH levels are similar to preconception values, the THYQUIDITY dosage should return to the pre-pregnancy dose immediately after delivery [see Dosage and Administration (2.3)].
8.2 Lactation
Risk Summary
Limited published studies report that levothyroxine is present in human milk. No adverse effects on the breastfed infant have been reported and there is no information on the effects of levothyroxine on milk production. Adequate levothyroxine treatment during lactation may normalize milk production in hypothyroid lactating mothers with low milk supply. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for THYQUIDITY and any potential adverse effects on the breastfed infant from THYQUIDITY or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of THYQUIDITY has been established for the treatment of congenital hypothyroidism and acquired hypothyroidism in pediatric patients down to birth [see Adverse Reactions (6)].
Glycerol has the potential to cause gastrointestinal irritation resulting in vomiting and/or osmotic diarrhea. Patients in the first 3 months of life may be particularly susceptible to serious fluid and electrolyte complications from glycerol-induced gastrointestinal irritation. Closely monitor patients from birth to 3 months of age receiving THYQUIDITY for signs and symptoms of gastrointestinal irritation.
Congenital Hypothyroidism [see Dosage and Administration (2.3, 2.4)]
Rapid restoration of normal serum T4 concentrations is essential for preventing the adverse effects of congenital hypothyroidism on intellectual development as well as on overall physical growth and maturation. Therefore, initiate THYQUIDITY therapy immediately upon diagnosis. Levothyroxine is generally continued for life in these patients.
Closely monitor patients during the first 2 weeks of THYQUIDITY therapy for cardiac overload, arrhythmias, and aspiration from avid suckling.
Closely monitor patients to avoid undertreatment or overtreatment. Undertreatment may have deleterious effects on intellectual development and linear growth. Overtreatment is associated with craniosynostosis in infants, may adversely affect the tempo of brain maturation, and may accelerate the bone age and result in premature epiphyseal closure and compromised adult stature.
Acquired Hypothyroidism in Pediatric Patients
Closely monitor patients to avoid undertreatment and overtreatment. Undertreatment may result in poor school performance due to impaired concentration and slowed mentation and in reduced adult height. Overtreatment may accelerate the bone age and result in premature epiphyseal closure and compromised adult stature.
Treated children may manifest a period of catch-up growth, which may be adequate in some cases to normalize adult height. In children with severe or prolonged hypothyroidism, catch-up growth may not be adequate to normalize adult height.
8.5 Geriatric Use
Because of the increased prevalence of cardiovascular disease among the elderly, initiate THYQUIDITY at less than the full replacement dose [see Warnings and Precautions (5.1) and Dosage and Administration (2.3)]. Atrial arrhythmias can occur in elderly patients. Atrial fibrillation is the most common of the arrhythmias observed with levothyroxine overtreatment in the elderly.
10 OVERDOSAGE
The signs and symptoms of overdosage are those of hyperthyroidism [see Warnings and Precautions (5) and Adverse Reactions (6)]. In addition, confusion and disorientation may occur. Cerebral embolism, shock, coma, and death have been reported. Seizures occurred in a 3-year old child ingesting 3.6 mg of levothyroxine. Symptoms may not necessarily be evident or may not appear until several days after ingestion of levothyroxine sodium.
Reduce the THYQUIDITY dose or discontinue temporarily if signs or symptoms of overdosage occur. Initiate appropriate supportive treatment as dictated by the patient’s medical status. For current information on the management of poisoning or overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org.
11 DESCRIPTION
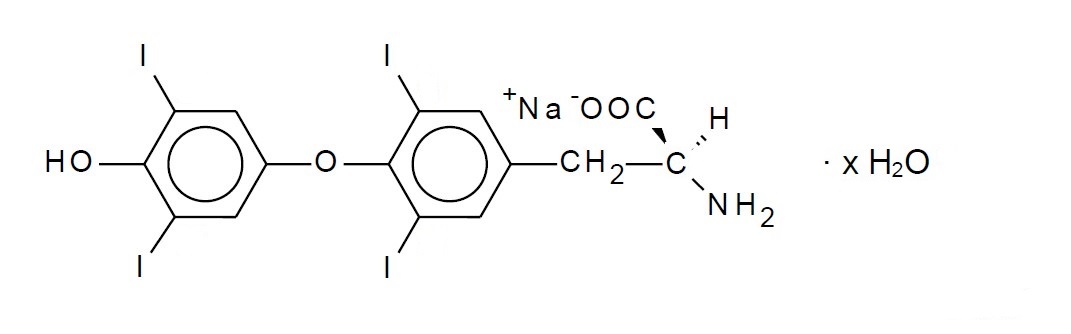
THYQUIDITY (levothyroxine sodium) oral solution contains synthetic L-3,3',5,5'-tetraiodothyronine sodium salt [levothyroxine (T4) sodium]. Synthetic T4 is chemically identical to that produced in the human thyroid gland, and is very slightly soluble in water. Levothyroxine (T4) sodium hydrate has an empirical formula of C15H10I4NNaO4 xH2O, molecular weight of 798.85 (anhydrous), and structural formula as shown:
THYQUIDITY oral solution is supplied in the following strength: 100 mcg per 5 mL (20 mcg per mL). THYQUIDITY oral solution contains the inactive ingredients citric acid monohydrate, glycerin, methylparaben sodium, sodium hydroxide and purified water.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Thyroid hormones exert their physiologic actions through control of DNA transcription and protein synthesis. Triiodothyronine (T3) and L-thyroxine (T4) diffuse into the cell nucleus and bind to thyroid receptor proteins attached to DNA. This hormone nuclear receptor complex activates gene transcription and synthesis of messenger RNA and cytoplasmic proteins.
The physiological actions of thyroid hormones are produced predominantly by T3, the majority of which (approximately 80%) is derived from T4 by deiodination in peripheral tissues.
12.2 Pharmacodynamics
Oral levothyroxine sodium is a synthetic T4 hormone that exerts the same physiologic effect as endogenous T4, thereby maintaining normal T4 levels when a deficiency is present.
12.3 Pharmacokinetics
Absorption
Absorption of orally administered T4 from the gastrointestinal tract ranges from 40% to 80%. The majority of the THYQUIDITY dose is absorbed from the jejunum and upper ileum. T4 absorption is increased by fasting, and decreased in malabsorption syndromes and by certain foods such as soybeans. Dietary fiber decreases bioavailability of T4. Absorption may also decrease with age. In addition, many drugs and foods affect T4 absorption [see Drug Interactions (7)].
Distribution
Circulating thyroid hormones are greater than 99% bound to plasma proteins, including thyroxine-binding globulin (TBG), thyroxine-binding prealbumin (TBPA), and thyroxine-binding albumin (TBA), whose capacities and affinities vary for each hormone. The higher affinity of both TBG and TBPA for T4 partially explains the higher serum levels, slower metabolic clearance, and longer half-life of T4 compared to T3. Protein-bound thyroid hormones exist in reverse equilibrium with small amounts of free hormone. Only unbound hormone is metabolically active. Many drugs and physiologic conditions affect the binding of thyroid hormones to serum proteins [see Drug Interactions (7)]. Thyroid hormones do not readily cross the placental barrier [see Use in Specific Populations (8.1)].
Elimination
Metabolism
T4 is slowly eliminated (see Table 6). The major pathway of thyroid hormone metabolism is through sequential deiodination. Approximately 80% of circulating T3 is derived from peripheral T4 by monodeiodination. The liver is the major site of degradation for both T4 and T3, with T4 deiodination also occurring at a number of additional sites, including the kidney and other tissues. Approximately 80% of the daily dose of T4 is deiodinated to yield equal amounts of T3 and reverse T3 (rT3). T3 and rT3 are further deiodinated to diiodothyronine. Thyroid hormones are also metabolized via conjugation with glucuronides and sulfates and excreted directly into the bile and gut where they undergo enterohepatic recirculation.
Excretion
Thyroid hormones are primarily eliminated by the kidneys. A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. Approximately 20% of T4 is eliminated in the stool. Urinary excretion of T4 decreases with age.
Table 6. Pharmacokinetic Parameters of Thyroid Hormones in Euthyroid Patients
|
Hormone |
Ratio in Thyroglobulin |
Biologic Potency |
Half-Life (days) |
Protein Binding (%)a |
|
Levothyroxine (T4) |
10 - 20 |
1 |
6-7b |
99.96 |
|
Liothyronine (T3) |
1 |
4 |
≤ 2 |
99.5 |
|
aIncludes TBG, TBPA, and TBA b3 to 4 days in hyperthyroidism, 9 to 10 days in hypothyroidism |
||||
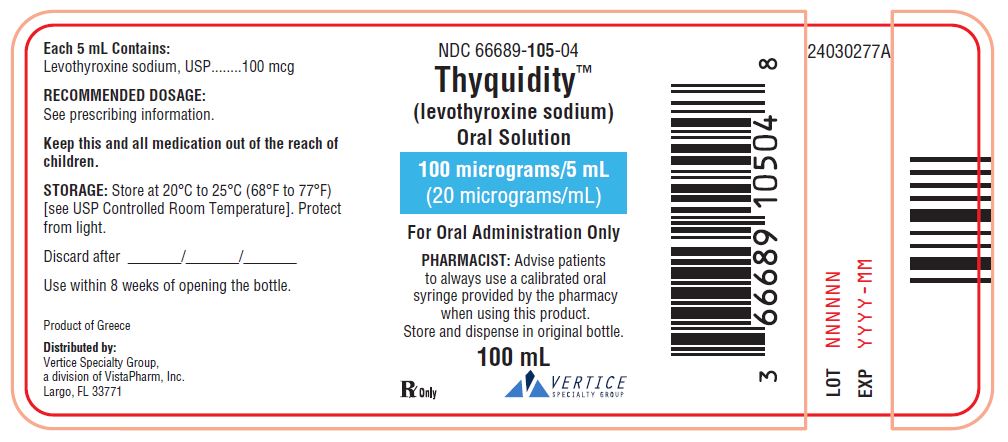
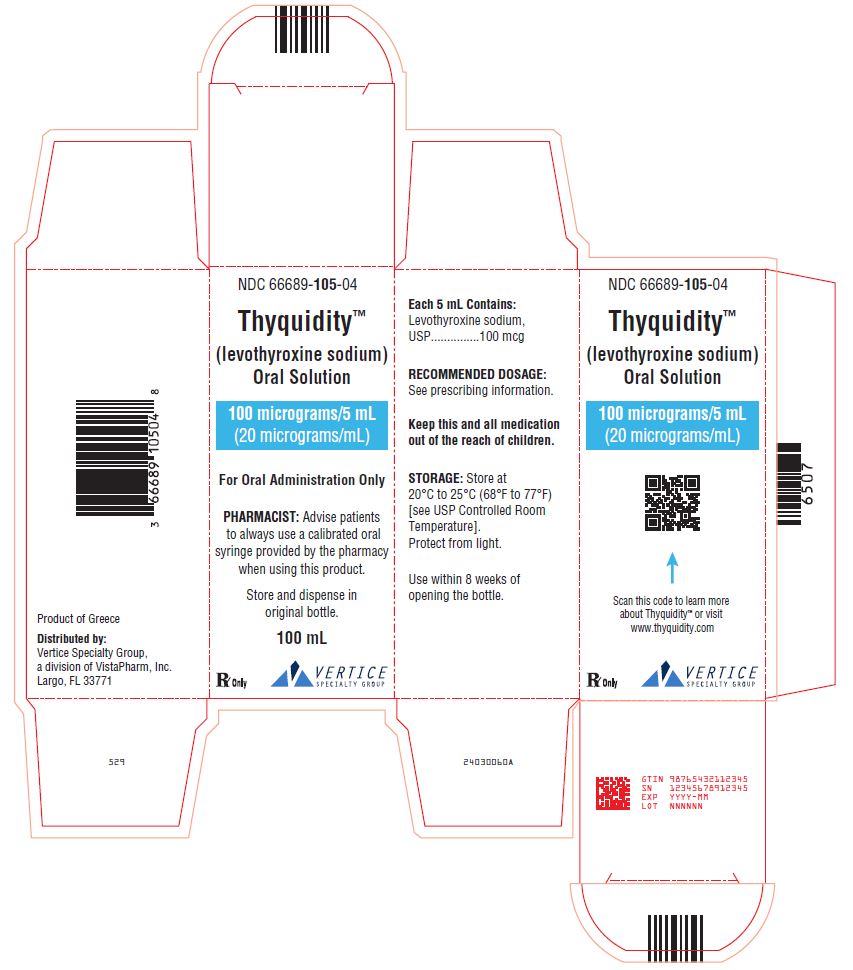
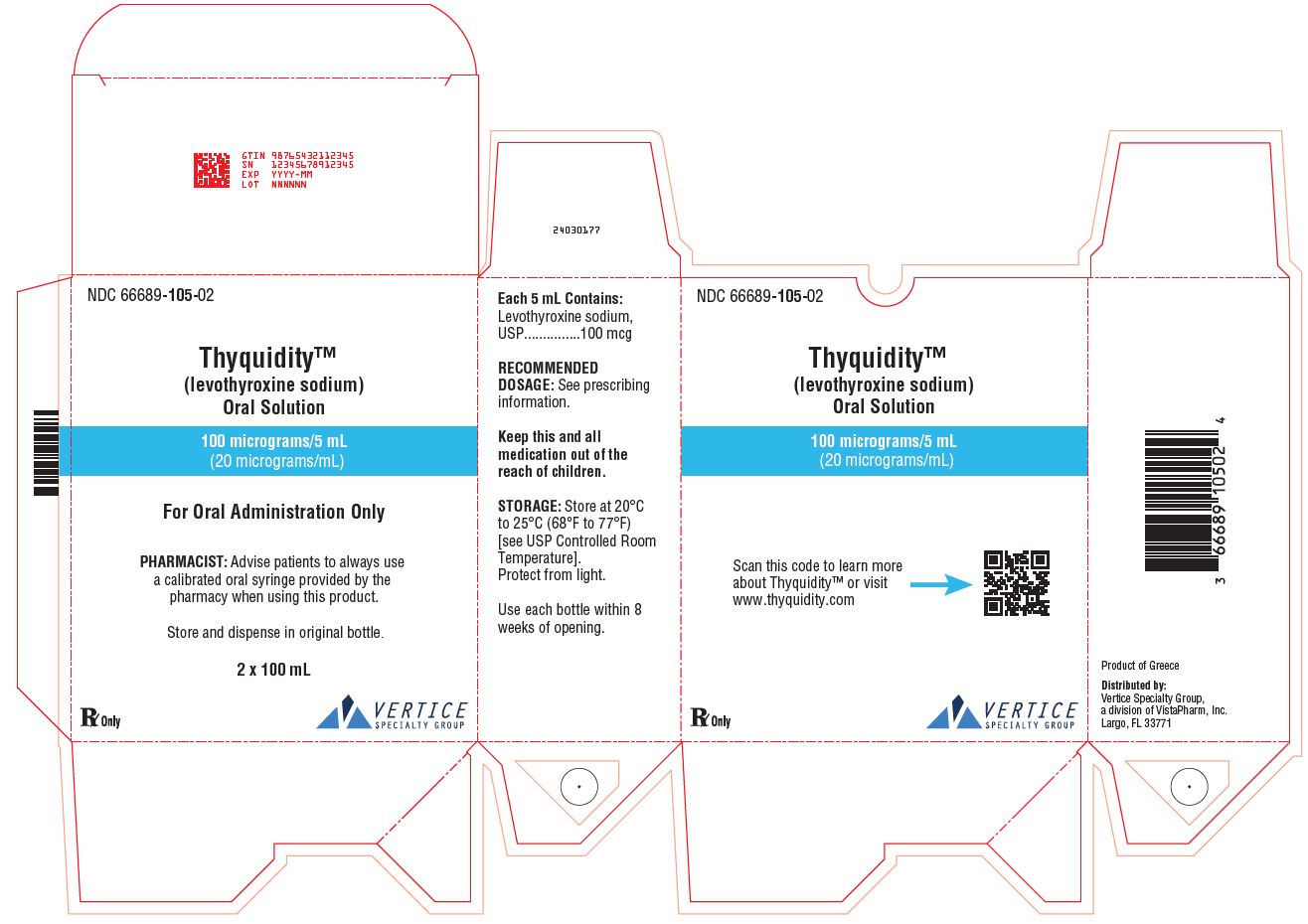
16 HOW SUPPLIED/STORAGE AND HANDLING
THYQUIDITY (levothyroxine sodium) oral solution, 100 mcg per 5 mL (20 mcg per mL) is a clear, colorless to nearly colorless solution supplied in a 100 mL amber glass bottle with a child-resistant closure as follows:
NDC: 66689-105-04: 1 x 100 mL bottle
NDC: 66689-105-02: 2 x 100 mL bottles (NDC: 66689-105-04)
The pharmacy will provide a calibrated oral syringe to accurately measure the prescribed dose.
Storage Conditions
Store at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature]. Protect from light.
Store and dispense in original bottle. Use within 8 weeks of opening the bottle.
17 PATIENT COUNSELING INFORMATION
Inform the patient of the following information to aid in the safe and effective use of THYQUIDITY:
Dosing and Administration
- Instruct patients to take THYQUIDITY only as directed by their healthcare provider.
- Instruct patients to take THYQUIDITY once daily, preferably on an empty stomach, one-half to one hour before breakfast.
- Instruct patients to always use a calibrated oral syringe provided by the pharmacy when administering THYQUIDITY to ensure that the dose is measured and administered accurately.
- Inform patients that agents such as iron and calcium supplements and antacids can decrease the absorption of levothyroxine. Instruct patients not to take THYQUIDITY within 4 hours of these agents.
- Instruct patients to notify their healthcare provider if they are pregnant or breastfeeding or are thinking of becoming pregnant while taking THYQUIDITY.
Important Information
- Inform patients that it may take several weeks before they notice an improvement in symptoms.
- Inform patients that the levothyroxine in THYQUIDITY is intended to replace a hormone that is normally produced by the thyroid gland. Generally, replacement therapy is to be taken for life.
- Inform patients that THYQUIDITY should not be used as a primary or adjunctive therapy in a weight control program.
- Instruct patients to notify their healthcare provider if they are taking any other medications, including prescription and over-the-counter preparations.
- Instruct patients to notify their physician of any other medical conditions they may have, particularly heart disease, diabetes, clotting disorders, and adrenal or pituitary gland problems, as the dose of medications used to control these other conditions may need to be adjusted while they are taking THYQUIDITY. If they have diabetes, instruct patients to monitor their blood and/or urinary glucose levels as directed by their physician and immediately report any changes to their physician. If patients are taking anticoagulants, their clotting status should be checked frequently.
- Instruct patients to notify their physician or dentist that they are taking THYQUIDITY prior to any surgery.
Adverse Reactions
- Instruct patients to notify their healthcare provider if they experience any of the following symptoms: rapid or irregular heartbeat, chest pain, shortness of breath, leg cramps, headache, nervousness, irritability, sleeplessness, tremors, change in appetite, weight gain or loss, vomiting, diarrhea, excessive sweating, heat intolerance, fever, changes in menstrual periods, hives or skin rash, or any other unusual medical event.
- Inform patients that partial hair loss may occur rarely during the first few months of THYQUIDITY therapy, but this is usually temporary.
Distributed by:

Vertice Specialty Group,
a division of VistaPharm, Inc.
Largo, FL 33771
For more information go to www.thyquidity.com
24030173B
PRINCIPAL DISPLAY PANEL - BOTTLE
NDC 66689-105-04
ThyquidityTM
(levothyroxine sodium)
Oral Solution
100 micrograms/5 mL
(20 micrograms/mL)
For Oral Administration Only
PHARMACIST: Advise patients
to always use a calibrated oral
syringe provided by the pharmacy
when using this product.
Store and dispense in original bottle.
100 mL
Rx Only Vertice Specialty Group
PRINCIPAL DISPLAY PANEL - CARTON
NDC 66689-105-04
ThyquidityTM
(levothyroxine sodium)
Oral Solution
100 micrograms/5 mL
(20 micrograms/mL)
For Oral Administration Only
PHARMACIST: Advise patients
to always use a calibrated oral
syringe provided by the pharmacy
when using this product.
Store and dispense in
original bottle.
100 mL
Rx Only Vertice Specialty Group
PRINCIPAL DISPLAY PANEL - CARTON - 2 x 100 mL
NDC 66689-105-02
ThyquidityTM
(levothyroxine sodium)
Oral Solution
100 micrograms/5 mL
(20 micrograms/mL)
For Oral Administration Only
PHARMACIST: Advise patients to always use
a calibrated oral syringe provided by the
pharmacy when using this product.
Store and dispense in original bottle.
2 x 100 mL
Rx Only Vertice Specialty Group
| THYQUIDITY
levothyroxine sodium solution |
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
| Labeler - VistaPharm, Inc. (116743084) |
Trademark Results [THYQUIDITY]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 THYQUIDITY 88945650 not registered Live/Pending |
VistaPharm, Inc. 2020-06-03 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.