FEXOFENADINE HYDROCHLORIDE tablet, film coated
Fexofenadine Hydrochloride by
Drug Labeling and Warnings
Fexofenadine Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by NCS HealthCare of KY, Inc dba Vangard Labs. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Fexofenadine hydrochloride is a histamine H1-receptor antagonist with the chemical name (±)-4-[1 hydroxy-4-[4-(hydroxydiphenylmethyl)-1-piperidinyl]-butyl]-α,α-dimethyl benzeneacetic acid hydrochloride. It has the following chemical structure
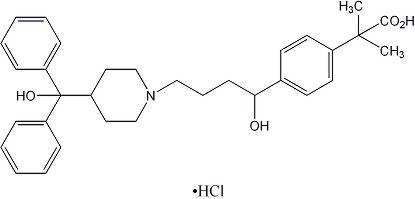
The molecular weight is 538.13 and the empirical formula is C32H39NO4HCl.
Fexofenadine hydrochloride is a white to off-white crystalline powder. It is freely soluble in methanol and ethanol, slightly soluble in chloroform and water, and insoluble in hexane. Fexofenadine hydrochloride is a racemate and exists as a zwitterion in aqueous media at physiological pH.
Fexofenadine hydrochloride is formulated as a tablet for oral administration. Each tablet contains 30, 60, or 180 mg fexofenadine hydrochloride (depending on the dosage strength) and the following excipients: croscarmellose sodium, magnesium stearate, microcrystalline cellulose, and pregelatinized starch. The aqueous tablet film coating is made from hypromellose, iron oxide blends, polyethylene glycol, povidone, silicone dioxide, and titanium dioxide.
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Fexofenadine hydrochloride, the major active metabolite of terfenadine, is an antihistamine with selective peripheral H1-receptor antagonist activity. Both enantiomers of fexofenadine hydrochloride displayed approximately equipotent antihistaminic effects. Fexofenadine hydrochloride inhibited antigen-induced bronchospasm in sensitized guinea pigs and histamine release from peritoneal mast cells in rats. The clinical significance of these findings is unknown. In laboratory animals, no anticholinergic or alpha1-adrenergic blocking effects were observed. Moreover, no sedative or other central nervous system effects were observed. Radiolabeled tissue distribution studies in rats indicated that fexofenadine does not cross the blood-brain barrier.
Pharmacokinetics
The pharmacokinetics of fexofenadine hydrochloride in subjects with seasonal allergic rhinitis and subjects with chronic urticaria were similar to those in healthy volunteers.
Absorption
Fexofenadine hydrochloride was rapidly absorbed following oral administration of a single dose of two 60 mg capsules to healthy male volunteers with a mean time to maximum plasma concentration occurring at 2.6 hours post-dose. After administration of a single 60 mg capsule to healthy volunteers, the mean maximum plasma concentration was 131 ng/mL. Following single dose oral administrations of either the 60 and 180 mg tablet to healthy adult male volunteers, mean maximum plasma concentrations were 142 and 494 ng/mL, respectively. The tablet formulations are bioequivalent to the capsule when administered at equal doses. Fexofenadine hydrochloride pharmacokinetics are linear for oral doses up to a total daily dose of 240 mg (120 mg twice daily). The administration of the 60 mg capsule contents mixed with applesauce did not have a significant effect on the pharmacokinetics of fexofenadine in adults.
Co-administration of 180 mg fexofenadine hydrochloride tablet with a high fat meal decreased the AUC and Cmax of fexofenadine by 21 and 20% respectively.
Distribution
Fexofenadine hydrochloride is 60% to 70% bound to plasma proteins, primarily albumin and α1-acid glycoprotein.
Metabolism
Approximately 5% of the total dose of fexofenadine hydrochloride was eliminated by hepatic metabolism.
Elimination
The mean elimination half-life of fexofenadine was 14.4 hours following administration of 60mg, twice daily, in healthy volunteers.
Human mass balance studies documented a recovery of approximately 80% and 11% of the [14C] fexofenadine hydrochloride dose in the feces and urine, respectively. Because the absolute bioavailability of fexofenadine hydrochloride has not been established, it is unknown if the fecal component represents primarily unabsorbed drug or the result of biliary excretion.
Special Populations
Pharmacokinetics in special populations (for renal, hepatic impairment, and age), obtained after a single dose of 80 mg fexofenadine hydrochloride, were compared to those from healthy volunteers in a separate study of similar design.
Geriatric Subjects
In older subjects (≥65 years old), peak plasma levels of fexofenadine were 99% greater than those observed in younger subjects (<65 years old). Mean fexofenadine elimination half-lives were similar to those observed in younger subjects.
Pediatric Subjects
Cross study comparisons indicated that fexofenadine area under the curve (AUC) following oral administration of a 60 mg dose of fexofenadine hydrochloride to 7–12 year old pediatric subjects with allergic rhinitis was 56% greater compared to healthy adult volunteers given the same dose. Plasma exposure in pediatric subjects given 30 mg fexofenadine hydrochloride is comparable to adults given 60 mg.
Renally Impaired
In subjects with mild to moderate (creatinine clearance 41–80 mL/min) and severe (creatinine clearance 11–40 mL/min) renal impairment, peak plasma levels of fexofenadine were 87% and 111% greater, respectively, and mean elimination half-lives were 59% and 72% longer, respectively, than observed in healthy volunteers. Peak plasma levels in subjects on dialysis (creatinine clearance ≤10 mL/min) were 82% greater and half-life was 31% longer than observed in healthy volunteers. Based on increases in bioavailability and half-life, a dose of 60 mg once daily is recommended as the starting dose in patients with decreased renal function. (See DOSAGE AND ADMINISTRATION).
Pharmacodynamics
Wheal and Flare
Human histamine skin wheal and flare studies following single and twice daily doses of 20 and 40 mg fexofenadine hydrochloride demonstrated that the drug exhibits an antihistamine effect by 1 hour, achieves maximum effect at 2 to 3 hours, and an effect is still seen at 12 hours. There was no evidence of tolerance to these effects after 28 days of dosing. The clinical significance of these observations is unknown.
Histamine skin wheal and flare studies in 7 to 12 year old subjects showed that following a single dose of 30 or 60 mg, antihistamine effect was observed at 1 hour and reached a maximum by 3 hours. Greater than 49% inhibition of wheal area, and 74% inhibition of flare area were maintained for 8 hours following the 30 and 60 mg dose.
Effects on QTc
In dogs (30 mg/kg/orally twice daily for 5 days) and rabbits (10 mg/kg, intravenously over 1 hour), fexofenadine hydrochloride did not prolong QTc. In dogs, the plasma fexofenadine concentration was approximately 9 times the therapeutic plasma concentrations in adults receiving the maximum recommended human daily oral dose of 180 mg. In rabbits, the plasma fexofenadine concentration was approximately 20 times the therapeutic plasma concentration in adults receiving the maximum recommended human daily oral dose of 180 mg. No effect was observed on calcium channel current, delayed K+ channel current, or action potential duration in guinea pig myocytes, Na+ current in rat neonatal myocytes, or on the delayed rectifier K+ channel cloned from human heart at concentrations up to 1 × 10-5 M of fexofenadine.
No statistically significant increase in mean QTc interval compared to placebo was observed in 714 subjects with seasonal allergic rhinitis given fexofenadine hydrochloride capsules in doses of 60 to 240 mg twice daily for 2 weeks. Pediatric subjects from 2 placebo- controlled trials (n=855) treated with up to 60 mg fexofenadine hydrochloride twice daily demonstrated no significant treatment- or dose-related increases in QTc. In addition, no statistically significant increase in mean QTc interval compared to placebo was observed in 40 healthy volunteers given fexofenadine hydrochloride as an oral solution at doses up to 400 mg twice daily for 6 days, or in 230 healthy volunteers given fexofenadine hydrochloride 240 mg once daily for 1 year. In subjects with chronic idiopathic urticaria, there were no clinically relevant differences for any ECG intervals, including QTc, between those treated with fexofenadine hydrochloride 180 mg once daily (n = 163) and those treated with placebo (n = 91) for 4 weeks.
-
CLINICAL STUDIES
Seasonal Allergic Rhinitis
Adults
In three 2-week, multicenter, randomized, double-blind, placebo-controlled trials in subjects 12 to 68 years of age with seasonal allergic rhinitis (n=1634), fexofenadine hydrochloride 60 mg twice daily significantly reduced total symptom scores (the sum of the individual scores for sneezing, rhinorrhea, itchy nose/palate/throat, itchy/watery/red eyes) compared to placebo. Statistically significant reductions in symptom scores were observed following the first 60 mg dose, with the effect maintained throughout the 12-hour interval. In these studies, there was no additional reduction in total symptom scores with higher doses of fexofenadine hydrochloride up to 240 mg twice daily.
In one 2-week, multicenter, randomized, double-blind clinical trial in subjects 12 to 65 years of age with seasonal allergic rhinitis (n=863), fexofenadine hydrochloride 180 mg once daily significantly reduced total symptom scores (the sum of the individual scores for sneezing, rhinorrhea, itchy nose/palate/throat, itchy/watery/red eyes) compared to placebo. Although the number of subjects in some of the subgroups was small, there were no significant differences in the effect of fexofenadine hydrochloride across subgroups of subjects defined by gender, age, and race. Onset of action for reduction in total symptom scores, excluding nasal congestion, was observed at 60 minutes compared to placebo following a single 60 mg fexofenadine hydrochloride dose administered to subjects with seasonal allergic rhinitis who were exposed to ragweed pollen in an environmental exposure unit. In 1 clinical trial conducted with fexofenadine hydrochloride 60 mg capsules, and in 1 clinical trial conducted with fexofenadine hydrochloride/pseudoephedrine hydrochloride extended release tablets, onset of action was seen within 1 to 3 hours.
Pediatrics
Two 2-week multicenter, randomized, placebo-controlled, double-blind trials in 877 pediatric subjects 6 to 11 years of age with seasonal allergic rhinitis were conducted at doses of 15, 30, and 60 mg twice daily. In 1 of these 2 studies, conducted in 411 pediatric subjects, all 3 doses of fexofenadine hydrochloride significantly reduced total symptom scores (the sum of the individual scores for sneezing, rhinorrhea, itchy nose/palate/throat, itchy/watery/red eyes) compared to placebo, however, a dose-response relationship was not seen. The 60 mg twice daily dose did not provide any additional benefit over the 30 mg twice daily dose. Furthermore, exposure in pediatric subjects given 30 mg fexofenadine hydrochloride is comparable to adults given 60 mg (see CLINICAL PHARMACOLOGY).
Three clinical safety studies in 845 children aged 6 months to 5 years with allergic rhinitis comparing 15 mg twice daily (n=85) and 30 mg twice daily (n=330) of an experimental formulation of fexofenadine to placebo (n=430) have been conducted. In general, fexofenadine hydrochloride was well tolerated in these studies. No unexpected adverse events were seen given the known safety profile of fexofenadine and likely adverse reactions for this patient population. (See PRECAUTIONS Pediatric Use and ADVERSE REACTIONS.)
Chronic Idiopathic Urticaria
Two 4-week multicenter, randomized, double-blind, placebo-controlled clinical trials compared four different doses of fexofenadine hydrochloride tablet (20, 60, 120, and 240 mg twice daily) to placebo in subjects aged 12 to 70 years with chronic idiopathic urticaria (n=726). Efficacy was demonstrated by a significant reduction in mean pruritus scores (MPS), mean number of wheals (MNW), and mean total symptom scores (MTSS, the sum of the MPS and MNW score). Although all 4 doses were significantly superior to placebo, symptom reduction was greater and efficacy was maintained over the entire 4-week treatment period with fexofenadine hydrochloride doses of ≥60 mg twice daily. However, no additional benefit of the 120 or 240 mg fexofenadine hydrochloride twice daily dose was seen over the 60 mg twice daily dose in reducing symptom scores. There were no significant differences in the effect of fexofenadine hydrochloride across subgroups of subjects defined by gender, age, weight, and race.
In one 4-week, multicenter, randomized, double-blind, placebo-controlled clinical trial in subjects 12 years of age and older with chronic idiopathic urticaria (n=259), fexofenadine hydrochloride 180 mg once daily significantly reduced the mean number of wheals (MNW), the mean pruritus score (MPS), and the mean total symptom score (MTSS, the sum of the MPS and MNW scores). Similar reductions were observed for mean number of wheals and mean pruritus score at the end of the 24-hour dosing interval. Symptom reduction was greater with fexofenadine hydrochloride 180 mg than with placebo. Improvement was demonstrated within 1 day of treatment with fexofenadine hydrochloride 180 mg and was maintained over the entire 4-week treatment period. There were no significant differences in the effect of fexofenadine hydrochloride across subgroups of subjects defined by gender, age, and race.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
-
PRECAUTIONS
Information for Patients
Patients taking Fexofenadine Hydrochloride Tablets should receive the following information:
Fexofenadine Hydrochloride Tablets are prescribed for the relief of symptoms of seasonal allergic rhinitis or for the relief of symptoms of chronic idiopathic urticaria (hives). Patients should be instructed to take Fexofenadine Hydrochloride Tablets only as prescribed. Do not exceed the recommended dose. If any untoward effects occur while taking Fexofenadine Hydrochloride Tablets, discontinue use and consult the doctor.
The product should not be used by patients who are hypersensitive to it or to any of its ingredients.
Patients should be told that this product should be used in pregnancy or lactation only if the potential benefit justifies the potential risk to the fetus or nursing infant.
Patients should be advised to take the tablet with water. Patients should also be advised to store the medication in a tightly closed container in a cool, dry place, away from children.
Drug Interaction with Erythromycin and Ketoconazole
Fexofenadine has been shown to exhibit minimal (ca. 5%) metabolism. However, co-administration of fexofenadine hydrochloride with either ketoconazole or erythromycin led to increased plasma concentrations of fexofenadine. Fexofenadine had no effect on the pharmacokinetics of either erythromycin or ketoconazole. In 2 separate studies, fexofenadine hydrochloride 120 mg twice daily (240 mg total daily dose) was co-administered with either erythromycin 500 mg every 8 hours or ketoconazole 400 mg once daily under steady-state conditions to healthy volunteers (n=24, each study). No differences in adverse events or QTc interval were observed when subjects were administered fexofenadine hydrochloride alone or in combination with either erythromycin or ketoconazole. The findings of these studies are summarized in the following table:
Effects on steady-state fexofenadine pharmacokinetics after 7 days of co-administration with fexofenadine hydrochloride 120 mg every 12 hours (two times the recommended twice daily dose) in healthy volunteers (n=24) Concomitant Drug CmaxSS
(Peak plasma concentration)AUCss(0–12h)
(Extent of systemic exposure)Erythromycin +82% +109% (500 mg every 8 hrs) Ketoconazole +135% +164% (400 mg once daily) The changes in plasma levels were within the range of plasma levels achieved in adequate and well-controlled clinical trials.
The mechanism of these interactions has been evaluated in in vitro, in situ, and in vivo animal models. These studies indicate that ketoconazole or erythromycin co-administration enhances fexofenadine gastrointestinal absorption. This observed increase in the bioavailability of fexofenadine may be due to transport-related effects, such as p-glycoprotein. In vivo animal studies also suggest that in addition to enhancing absorption, ketoconazole decreases fexofenadine gastrointestinal secretion, while erythromycin may also decrease biliary excretion.
Drug Interactions with Antacids
Administration of 120 mg of fexofenadine hydrochloride (2 × 60 mg capsule) within 15 minutes of an aluminum and magnesium containing antacid (Maalox®) decreased fexofenadine AUC by 41% and Cmax by 43%. Fexofenadine hydrochloride should not be taken closely in time with aluminum and magnesium containing antacids.
Interactions with Fruit Juices
Fruit juices such as grapefruit, orange and apple may reduce the bioavailability and exposure of fexofenadine. This is based on the results from 3 clinical studies using histamine induced skin wheals and flares coupled with population pharmacokinetic analysis. The size of wheal and flare were significantly larger when fexofenadine hydrochloride was administered with either grapefruit or orange juices compared to water. Based on the literature reports, the same effects may be extrapolated to other fruit juices such as apple juice. The clinical significance of these observations is unknown. In addition, based on the population pharmacokinetics analysis of the combined data from grapefruit and orange juices studies with the data from a bioequivalence study, the bioavailability of fexofenadine was reduced by 36%. Therefore, to maximize the effects of fexofenadine, it is recommended that Fexofenadine hydrochloride should be taken with water (see Dosage and Administration).
CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
The carcinogenic potential and reproductive toxicity of fexofenadine hydrochloride were assessed using terfenadine studies with adequate fexofenadine hydrochloride exposure (based on plasma area-under-the-concentration vs. time [AUC] values). No evidence of carcinogenicity was observed in an 18-month study in mice and in a 24-month study in rats at oral doses up to 150 mg/kg of terfenadine (which led to fexofenadine exposures that were approximately 3 and 5 times the exposure from the maximum recommended human daily oral dose of fexofenadine hydrochloride in adults [180 mg] and children [60 mg] respectively .
In in vitro (Bacterial Reverse Mutation, CHO/HGPRT Forward Mutation, and Rat Lymphocyte Chromosomal Aberration assays) and in vivo (Mouse Bone Marrow Micronucleus assay) tests, fexofenadine hydrochloride revealed no evidence of mutagenicity.
In rat dietary fertility studies, dose-related reductions in implants and increases in postimplantation losses were observed at an oral dose of 150 mg/kg of terfenadine (which led to fexofenadine hydrochloride exposures that were approximately 3 times the exposure of the maximum recommended human daily oral dose of 180 mg fexofenadine hydrochloride). In mice, fexofenadine hydrochloride produced no effect on male or female fertility at average dietary doses up to 4438 mg/kg (approximately 10 times the maximum recommended human daily oral dose of fexofenadine hydrochloride 180 mg based on comparison of AUCs).
PREGNANCY
Teratogenic Effects
Category C.
There was no evidence of teratogenicity in rats or rabbits at oral doses of terfenadine up to 300 mg/kg (which led to fexofenadine exposures that were approximately 3 and 30 times, respectively, the exposure from the maximum recommended human daily oral dose of fexofenadine hydrochloride of 180 mg based on comparison of AUCs).
In mice, no adverse effects and no teratogenic effects during gestation were observed with fexofenadine at dietary doses up to 3730 mg/kg (approximately 15 times the maximum recommended human daily oral dose of fexofenadine hydrochloride 180 mg based on comparison of AUCs).
There are no adequate and well controlled studies in pregnant women. Fexofenadine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects
Dose-related decreases in pup weight gain and survival were observed in rats exposed to an oral dose of 150 mg/kg of terfenadine (approximately 3 times the maximum recommended human daily oral dose of fexofenadine hydrochloride of 180 mg in adults based on comparison of fexofenadine hydrochloride AUCs).
NURSING MOTHERS
It is not known if fexofenadine is excreted in human milk. There are no adequate and well-controlled studies in women during lactation. Because many drugs are excreted in human milk, caution should be exercised when fexofenadine hydrochloride is administered to a nursing woman.
PEDIATRIC USE
The recommended dose in patients 6 to 11 years of age is based on cross-study comparison of the pharmacokinetics of fexofenadine hydrochloride in adults and pediatric subjects and on the safety profile of fexofenadine hydrochloride in both adult and pediatric subjects at doses equal to or higher than the recommended doses.
The safety of fexofenadine hydrochloride tablets at a dose of 30 mg twice daily has been demonstrated in 438 pediatric subjects 6 to 11 years of age in two placebo-controlled 2-week seasonal allergic rhinitis trials. The safety of fexofenadine hydrochloride for the treatment of chronic idiopathic urticaria in subjects 6 to 11 years of age is based on cross-study comparison of the pharmacokinetics of fexofenadine hydrochloride in adult and pediatric subjects and on the safety profile of fexofenadine in both adult and pediatric subjects at doses equal to or higher than the recommended dose.
The effectiveness of fexofenadine hydrochloride for the treatment of seasonal allergic rhinitis in subjects 6 to 11 years of age was demonstrated in 1 trial (n=411) in which fexofenadine hydrochloride tablets 30 mg twice daily significantly reduced total symptom scores compared to placebo, along with extrapolation of demonstrated efficacy in subjects aged 12 years and above, and the pharmacokinetic comparisons in adults and children. The effectiveness of fexofenadine hydrochloride for the treatment of chronic idiopathic urticaria in patients 6 to 11 years of age is based on an extrapolation of the demonstrated efficacy of fexofenadine hydrochloride in adults with this condition and the likelihood that the disease course, pathophysiology and the drug's effect are substantially similar in children to that of adult patients.
Three clinical safety studies comparing 15 mg twice daily (n=85) and 30 mg twice daily (n=330) of an experimental formulation of fexofenadine to placebo (n=430) have been conducted in pediatric subjects aged 6 months to 5 years. In general, fexofenadine hydrochloride was well tolerated in these studies. No unexpected adverse events were seen given the known safety profile of fexofenadine and likely adverse reactions for this patient population. (See ADVERSE REACTIONS and CLINICAL PHARMACOLOGY.)
The safety and effectiveness of fexofenadine hydrochloride in pediatric patients under 6 years of age have not been established.
GERIATRIC USE
Clinical studies of fexofenadine hydrochloride tablets and capsules did not include sufficient numbers of subjects aged 65 years and over to determine whether this population responds differently from younger subjects. Other reported clinical experience has not identified differences in responses between the geriatric and younger subjects. This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function. (See CLINICAL PHARMACOLOGY).
-
ADVERSE REACTIONS
Seasonal Allergic Rhinitis
Adults
In placebo-controlled seasonal allergic rhinitis clinical trials in subjects 12 years of age and older, which included 2461 subjects receiving fexofenadine hydrochloride capsules at doses of 20 mg to 240 mg twice daily, adverse events were similar in fexofenadine hydrochloride- and placebo-treated subjects. All adverse events that were reported by greater than 1% of subjects who received the recommended daily dose of fexofenadine hydrochloride (60 mg capsules twice daily), and that were more common with fexofenadine hydrochloride than placebo, are listed in Table 1.
In a placebo-controlled clinical study in the United States, which included 570 subjects aged 12 years and older receiving fexofenadine hydrochloride tablets at doses of 120 or 180 mg once daily, adverse events were similar in fexofenadine hydrochloride- and placebo-treated subjects. Table 1 also lists adverse experiences that were reported by greater than 2% of subjects treated with fexofenadine hydrochloride tablets at doses of 180 mg once daily and that were more common with fexofenadine hydrochloride than placebo.
The incidence of adverse events, including drowsiness, was not dose-related and was similar across subgroups defined by age, gender, and race.
Table 1 Adverse experiences in subjects aged 12 years and older reported in placebo-controlled seasonal allergic rhinitis clinical trials in the United States Twice- daily dosing with fexofenadine capsules
at rates of greater than 1%Adverse experience Fexofenadine 60 mg
Twice Daily
(n=679)Placebo
Twice Daily
(n=671)Viral Infection (cold, flu) 2.5% 1.5% Nausea 1.6% 1.5% Dysmenorrhea 1.5% 0.3% Drowsiness 1.3% 0.9% Dyspepsia 1.3% 0.6% Fatigue 1.3% 0.9% Once daily dosing with fexofenadine hydrochloride tablets
at rates of greater than 2%Adverse experience Fexofenadine 180 mg
Once Daily
(n=283)Placebo
(n=293)Headache 10.6% 7.5% Upper Respiratory Tract Infection 3.2% 3.1% Back Pain 2.8% 1.4% The frequency and magnitude of laboratory abnormalities were similar in fexofenadine hydrochloride- and placebo-treated subjects.
Pediatrics
Table 2 lists adverse experiences in subjects aged 6 to 11 years of age which were reported by greater than 2% of subjects treated with fexofenadine hydrochloride tablets at a dose of 30 mg twice daily in placebo-controlled seasonal allergic rhinitis studies in the United States and Canada that were more common with fexofenadine hydrochloride than placebo.
Table 2 Adverse experiences reported in placebo-controlled seasonal allergic rhinitis studies in pediatric subjects aged 6 to 11 in the United States and Canada at rates of greater than 2% Adverse experience Fexofenadine 30 mg
Twice Daily
(n=209)Placebo
(n=229)Headache 7.2% 6.6% Accidental Injury 2.9% 1.3% Coughing 3.8% 1.3% Fever 2.4% 0.9% Pain 2.4% 0.4% Otitis Media 2.4% 0.0% Upper Respiratory Tract Infection 4.3% 1.7% Three clinical safety studies in 845 children aged 6 months to 5 years comparing 15 mg twice daily (n=85) and 30 mg twice daily (n=330) of an experimental formulation of fexofenadine to placebo (n=430) have been conducted. In general, fexofenadine hydrochloride was well tolerated in these studies. No unexpected adverse events were seen given the known safety profile of fexofenadine and likely adverse reactions for this patient population. (See PRECAUTIONS Pediatric Use.)
Chronic Idiopathic Urticaria
Adverse events reported by subjects 12 years of age and older in placebo-controlled chronic idiopathic urticaria studies were similar to those reported in placebo-controlled seasonal allergic rhinitis studies. In placebo-controlled chronic idiopathic urticaria clinical trials, which included 726 subjects 12 years of age and older receiving fexofenadine hydrochloride tablets at doses of 20 to 240 mg twice daily, adverse events were similar in fexofenadine hydrochloride- and placebo-treated patients. Table 3 lists adverse experiences in subjects aged 12 years and older which were reported by greater than 2% of subjects treated with fexofenadine hydrochloride 60 mg tablets twice daily in controlled clinical studies in the United States and Canada and that were more common with fexofenadine hydrochloride than placebo.
In a placebo-controlled clinical study in the United States, which included 167 subjects aged 12 years and older receiving fexofenadine hydrochloride 180 mg tablets, adverse events were similar in fexofenadine hydrochloride- and placebo-treated subjects. Table 3 also lists adverse experiences that were reported by greater than 2% of subjects treated with fexofenadine hydrochloride tablets at doses of 180 mg once daily and that were more common with fexofenadine hydrochloride than placebo.
The safety of fexofenadine hydrochloride in the treatment of chronic idiopathic urticaria in pediatric patients 6 to 11 years of age is based on the safety profile of fexofenadine hydrochloride in adults and adolescent patients at doses equal to or higher than the recommended dose (see Pediatric Use).
Table 3 Adverse experiences reported in subjects 12 years of age and older in placebo-controlled chronic idiopathic urticaria studies Twice-daily dosing with fexofenadine hydrochloride in studies
in the United States and Canada at rates of greater than 2%Adverse experience Fexofenadine 60 mg
Twice Daily
(n=191)Placebo
(n=183)Dyspepsia 4.7% 4.4% Myalgia 2.6% 2.2% Back Pain 2.1% 1.1% Dizziness 2.1% 1.1% Pain in extremity 2.1% 0.0% Once-daily dosing with fexofenadine hydrochloride in a study
in the United States at rates of greater than 2%Adverse experience Fexofenadine 180 mg
Once Daily
(n=167)Placebo
(n=92)Headache 4.8% 3.3% Nasopharyngitis 2.4% 2.2% Upper respiratory tract infection 2.4% 2.2% Events that have been reported during controlled clinical trials involving seasonal allergic rhinitis and chronic idiopathic urticaria subjects with incidences less than 1% and similar to placebo and have been rarely reported during postmarketing surveillance include: insomnia, nervousness, and sleep disorders or paroniria. In rare cases, rash, urticaria, pruritus and hypersensitivity reactions with manifestations such as angioedema, chest tightness, dyspnea, flushing and systemic anaphylaxis have been reported.
-
OVERDOSAGE
Reports of fexofenadine hydrochloride overdose have been infrequent and contain limited information. However, dizziness, drowsiness, and dry mouth have been reported. Single doses of fexofenadine hydrochloride up to 800 mg (6 healthy volunteers at this dose level), and doses up to 690 mg twice daily for 1 month (3 healthy volunteers at this dose level) or 240 mg once daily for 1 year (234 healthy volunteers at this dose level) were administered without the development of clinically significant adverse events as compared to placebo.
In the event of overdose, consider standard measures to remove any unabsorbed drug. Symptomatic and supportive treatment is recommended. Following administration of terfenadine, hemodialysis did not effectively remove fexofenadine, the major active metabolite of terfenadine, from blood (up to 1.7% removed).
No deaths occurred at oral doses of fexofenadine hydrochloride up to 5000 mg/kg in mice (110 times the maximum recommended human daily oral dose in adults and 200 times the maximum recommended human daily oral dose in children based on mg/m2) and up to 5000 mg/kg in rats (230 times the maximum recommended human daily oral dose in adults and 400 times the maximum recommended human daily oral dose in children based on mg/m2). Additionally, no clinical signs of toxicity or gross pathological findings were observed. In dogs, no evidence of toxicity was observed at oral doses up to 2000 mg/kg (300 times the maximum recommended human daily oral dose in adults and 530 times the maximum recommended human daily oral dose in children based on mg/m2).
-
DOSAGE AND ADMINISTRATION
Seasonal Allergic Rhinitis
Adults and Children 12 Years and Older
The recommended dose of Fexofenadine Hydrochloride Tablets is 60 mg twice daily, or 180 mg once daily with water. A dose of 60 mg once daily is recommended as the starting dose in patients with decreased renal function (see CLINICAL PHARMACOLOGY).
Children 6 to 11 Years
The recommended dose of Fexofenadine Hydrochloride Tablets is 30 mg twice daily with water. A dose of 30 mg once daily is recommended as the starting dose in pediatric patients with decreased renal function (see CLINICAL PHARMACOLOGY).
Chronic Idiopathic Urticaria
Adults and Children 12 Years and Older
The recommended dose of Fexofenadine Hydrochloride Tablets is 60 mg twice daily or 180 mg once daily with water. A dose of 60 mg once daily is recommended as the starting dose in patients with decreased renal function (see CLINICAL PHARMACOLOGY).
Children 6 to 11 Years
The recommended dose of Fexofenadine Hydrochloride Tablets is 30 mg twice daily with water. A dose of 30 mg once daily is recommended as the starting dose in pediatric patients with decreased renal function (see CLINICAL PHARMACOLOGY).
-
HOW SUPPLIED
Fexofenadine Hydrochloride Tablets 60 mg are available in blisterpacks of 30 (NDC: 0615-5620-39).
Fexofenadine Hydrochloride Tablets 180 mg are available in blisterpacks of 30 (NDC: 0615-5619-39)
Fexofenadine Hydrochloride Tablets are coated with a peach colored film coating. Tablets have the following unique identifiers: 30 mg tablets have 03 on one side, 60 mg tablets have 06 on one side, and 180 mg tablets have 018 on one side.
Store Fexofenadine Hydrochloride Tablets at controlled room temperature 20–25°C (68–77°F). (See USP Controlled Room Temperature). Fexofenadine Hydrochloride Tablets should be protected from excessive moisture.
- SPL UNCLASSIFIED SECTION
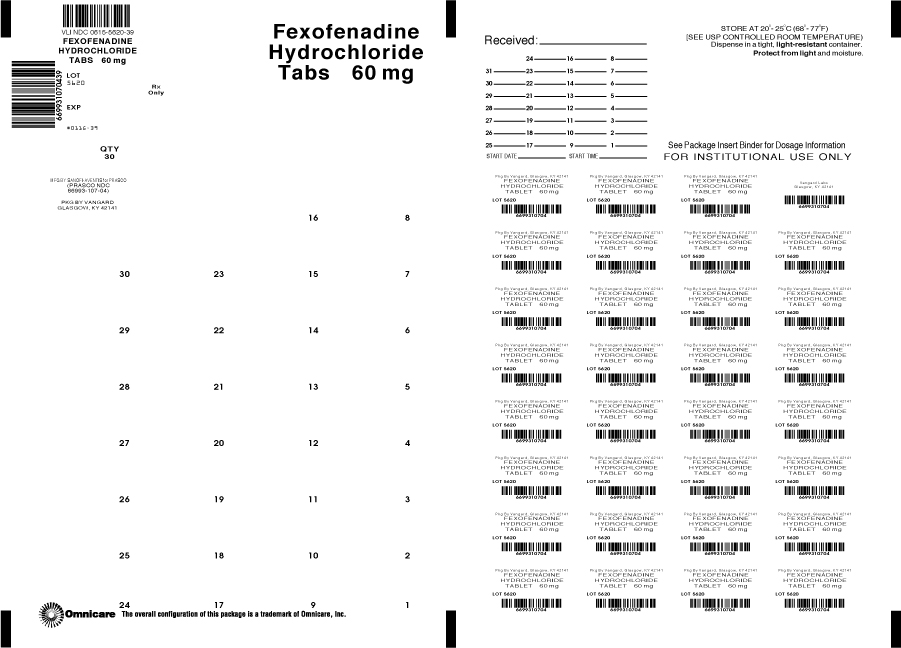
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FEXOFENADINE HYDROCHLORIDE
fexofenadine hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0615-5620(NDC: 66993-107) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FEXOFENADINE HYDROCHLORIDE (UNII: 2S068B75ZU) (FEXOFENADINE - UNII:E6582LOH6V) FEXOFENADINE HYDROCHLORIDE 60 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) HYPROMELLOSES (UNII: 3NXW29V3WO) FERROUS OXIDE (UNII: G7036X8B5H) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POVIDONE (UNII: FZ989GH94E) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color ORANGE (Peach) Score no score Shape OVAL (OVAL) Size 12mm Flavor Imprint Code 06 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0615-5620-39 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 04/14/2006 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020872 02/25/2000 FEXOFENADINE HYDROCHLORIDE
fexofenadine hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0615-5619(NDC: 66993-109) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FEXOFENADINE HYDROCHLORIDE (UNII: 2S068B75ZU) (FEXOFENADINE - UNII:E6582LOH6V) FEXOFENADINE HYDROCHLORIDE 180 mg Inactive Ingredients Ingredient Name Strength CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) HYPROMELLOSES (UNII: 3NXW29V3WO) FERROUS OXIDE (UNII: G7036X8B5H) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POVIDONE (UNII: FZ989GH94E) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color ORANGE (Peach) Score no score Shape OVAL (OVAL) Size 17mm Flavor Imprint Code 018 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0615-5619-39 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 01/17/2008 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020872 02/25/2000 Labeler - NCS HealthCare of KY, Inc dba Vangard Labs (050052943) Establishment Name Address ID/FEI Business Operations NCS HealthCare of KY, Inc dba Vangard Labs 050052943 REPACK(0615-5620, 0615-5619)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.