CLINDAMYCIN PALMITATE HYDROCHLORIDE solution
Clindamycin Palmitate Hydrochloride by
Drug Labeling and Warnings
Clindamycin Palmitate Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Marlex Pharmaceuticals Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
CLINDAMYCIN PALMITATE HYDROCHLORIDE- clindamycin palmitate
hydrochloride powder, for solution
Marlex Pharmaceuticals Inc. of New Castle, Delaware----------
Clindamycin Palmitate Hydrochloride for Oral Solution, USP (Pediatric)
To reduce the development of drug-resistant bacteria and maintain the effectiveness of clindamycin palmitate hydrochloride (HCl) for oral solution, USP (pediatric) and other antibacterial drugs, clindamycin palmitate HCl for oral solution, USP (pediatric) should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
Not for Injection
-
BOXED WARNING
(What is this?)
WARNING
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including clindamycin and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C.difficile.
Because clindamycin therapy has been associated with severe colitis which may end fatally, it should be reserved for serious infections where less toxic antimicrobial agents are inappropriate, as described in the INDICATIONS AND USAGE section. It should not be used in patients with nonbacterial infections such as most upper respiratory tract infections.
C.difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C.difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C.difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C.difficile, and surgical evaluation should be instituted as clinically indicated.
-
DESCRIPTION
Clindamycin palmitate hydrochloride is a water soluble hydrochloride salt of the ester of clindamycin and palmitic acid. Clindamycin is a semisynthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent compound lincomycin.
The structural formula is represented below:
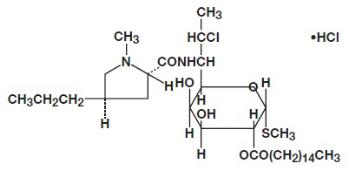
The chemical name for clindamycin palmitate hydrochloride is Methyl 7-chloro-6, 7, 8-trideoxy-6-(1-methyl-trans-4propyl-L-2-pyrrolidinecarboxamido)-1-threo-a-D-galacto-octopyranoside 2-palmitate monohydrochloride. Clindamycin palmitate HCl for oral solution, USP (pediatric) contains clindamycin palmitate hydrochloride granules for reconstitution. Each 5 mL contains the equivalent of 75 mg clindamycin.
Inactive ingredients: artificial cherry flavor, dextrin, ethylparaben, poloxamer 188, sucrose.
-
CLINICAL PHARMACOLOGY
Microbiology
Although clindamycin palmitate HCl is inactive in vitro, rapid in vivo hydrolysis converts this compound to the antibacterially active clindamycin.
Clindamycin has been shown to have in vitro activity against isolates of the following organisms:
Aerobic gram positive cocci, including:
Staphylococcus aureus (penicillinase and non-penicillinase producing strains). When tested by in vitro methods some staphylococcal strains originally resistant to erythromycin rapidly develop resistance to clindamycin.
Staphylococcus epidermidis (penicillinase and non-penicillinase producing strains). When tested by in vitro methods some staphylococcal strains originally resistant to erythromycin rapidly develop resistance to clindamycin.
Streptococci (except Streptococcus faecalis)
Pneumococci
Anaerobic gram negative bacilli, including:
Bacteroides species (including Bacteroides fragilis group and Bacteroides melaninogenicus group)
Fusobacterium species
Anaerobic gram positive nonsporeforming bacilli, including:
Propionibacterium
Eubacterium
Actinomyces species
Anaerobic and microaerophilic gram positive cocci, including:
Peptococcus species
Peptostreptococcus species
Microaerophilic streptococci
Clostridia: Clostridia are more resistant than most anaerobes to clindamycin.
Most Clostridium perfringens are susceptible, but other species, e.g., Clostridium sporogenes and
Most Clostridium perfringens are susceptible, but other species, e.g., Clostridium sporogenes and
Clostridium tertium are frequently resistant to clindamycin. Susceptibility testing should be done.
Cross resistance has been demonstrated between clindamycin and lincomycin.
Antagonism has been demonstrated between clindamycin and erythromycin.
Human Pharmacology
Blood level studies comparing clindamycin palmitate HCl with clindamycin hydrochloride show that both drugs reach their peak active serum levels at the same time, indicating a rapid hydrolysis of the palmitate to the clindamycin.
Clindamycin is widely distributed in body fluids and tissues (including bones). Approximately 10% of the biological activity is excreted in the urine. The average serum half-life after doses of clindamycin palmitate HCl is approximately two hours in pediatric patients.
Serum half-life of clindamycin is increased slightly in patients with markedly reduced renal function. Hemodialysis and peritoneal dialysis are not effecting in removing clindamycin from the serum.
Serum level studies with clindamycin palmitate HCl in normal pediatric patients weighing 50 to 100 lbs given 2, 3 or 4 mg/kg every 6 hours (8, 12 or 16 mg/kg/day) demonstrated mean peak clindamycin serum levels of 1.24, 2.25 and 2.44 mcg/mL respectively, one hour after the first dose. By the fifth dose, the 6-hour serum concentration had reached equilibrium. Peak serum concentrations after this time would be about 2.46, 2.98 and 3.79 mcg/mL with doses of 8, 12 and 16 mg/kg/day, respectively.
Serum levels have been uniform and predictable from person to person and dose to dose. Multiple-dose studies in neonates and infants up to 6 months of age show that the drug does not accumulate in the serum and is excreted rapidly. Serum levels exceed the MICs for most indicated organisms for at least six hours following administration of the usually recommended doses of clindamycin palmitate HCl in adults and pediatric patients.
No significant levels of clindamycin are attained in the cerebrospinal fluid, even in the presence of inflamed meninges.
Pharmacokinetic studies in elderly volunteers (61 to 79 years) and younger adults (18 to 39 years) indicate that age alone does not alter clindamycin pharmacokinetics (clearance, elimination half-life, volume of distribution, and area under the serum concentration-time curve) after IV administration of clindamycin phosphate.
After oral administration of clindamycin hydrochloride, elimination half-life is increased to approximately 4.0 hours (range 3.4 to 5.1 h) in the elderly compared to 3.2 hours (range 2.1 to 4.2 h) in younger adults; administration of clindamycin palmitate HCl resulted in a similar elimination half-life value of about 4.5 hours in elderly subjects. However, the extent of absorption is not different between age groups and no dosage alteration is necessary for the elderly with normal hepatic function and normal (age-adjusted) renal function.
-
INDICATIONS AND USAGE
Clindamycin palmitate HCl for oral solution, USP (pediatric) is indicated in the treatment of serious infections cause by susceptible anaerobic bacteria.
Clindamycin is also indicated in the treatment of serious infections due to susceptible strains of streptococci, pneumococci and staphylococci. Its use should be reserved for penicillin-allergic patients or other patients for whom, in the judgment of the physician, a penicillin is inappropriate. Because of the risk of colitis, as described in the WARNING box, before selecting clindamycin the physician should consider the nature of the infection and the suitability of less toxic alternatives (e.g., erythromycin).
Anaerobes: Serious respiratory tract infections such as empyema, anaerobic pneumonitis and lung abscess; serious skin and soft tissue infections; septicemia; intra-abdominal infections such as peritonitis and intra-abdominal abscess (typically resulting from anaerobic organisms resident in the normal gastrointestinal tract); infections of the female pelvis and genital tract such as endometritis, nongonococcal tubo-ovarian abscess, pelvic cellulitis and postsurgical vaginal cuff infection.
Streptococci: Serious respiratory tract infections; serious skin and soft tissue infections.
Staphylococci: Serious respiratory tract infections; serious skin and soft tissue infections.
Pneumococci: Serious respiratory tract infections.
Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to clindamycin.
In Vitro Susceptibility Testing
A standardized disk testing procedure is recommended for determining susceptibility of aerobic bacteria to clindamycin. A description is contained in the clindamycin palmitate HCl susceptibility disk insert. Using this method, the laboratory can designate isolates as resistant, intermediate, or susceptible.
Tube or agar dilution methods may be used for both anaerobic and aerobic bacteria. When the directions in the clindamycin palmitate HCl susceptibility powder insert are followed, an MIC (minimal inhibitory concentration) of 1.6 mcg/mL may be considered susceptible; MICs of 1.6 to 4.8 mcg/mL may be considered intermediate and MICs greater than 4.8 mcg/mL may be considered resistant.
Clindamycin palmitate HCl susceptibility disks 2 mcg. See package insert for use.
Clindamycin palmitate HCl susceptibility powder 20 mg. See package insert for use.
For anaerobic bacteria the minimal inhibitory concentration (MIC) of clindamycin can be determined by agar dilution and broth dilution (including microdilution) techniques. If MICs are not determined routinely, the disk broth method is recommended for routine use. THE KIRBY-BAUER DISK
DIFFUSION METHOD AND ITS INTERPRETIVE STANDARDS ARE NOT RECOMMENDED FOR ANAEROBES.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of clindamycin palmitate HCl for oral solution, USP (pediatric) and other antibacterial drugs, clindamycin palmitate HCl for oral solution, USP (pediatric) should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
- CONTRAINDICATIONS
-
WARNINGS
See WARNING box.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including clindamycin palmitate HCl, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
A careful inquiry should be made concerning previous sensitivities to drugs and other allergens.
Usage in Meningitis: Since clindamycin does not diffuse adequately into the cerebrospinal fluid, the drug should not be used in the treatment of meningitis.
-
PRECAUTIONS
General
Review of experience to date suggests that a subgroup of older patients with associated severe illness may tolerate diarrhea less well. When clindamycin is indicated in these patients, they should be carefully monitored for change in bowel frequency.
Clindamycin palmitate HCl should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
Clindamycin palmitate HCl should be prescribed with caution in atopic individuals.
Indicated surgical procedures should be performed in conjunction with antibiotic therapy.
The use of clindamycin palmitate HCl occasionally results in overgrowth of non-susceptible organisms particularly yeasts. Should superinfections occur, appropriate measures should be taken as indicated by the clinical situation.
Clindamycin dosage modification may not be necessary in patients with renal disease. In patients with moderate to severe liver disease, prolongation of clindamycin half-life has been found. However, it was postulated from studies that when given every eight hours, accumulation should rarely occur.
Therefore, dosage modification in patients with liver disease may not be necessary. However, periodic liver enzyme determinations should be made when treating patients with severe liver disease.
Prescribing clindamycin palmitate HCl in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs including clindamycin palmitate HCl should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When clindamycin palmitate HCl is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by clindamycin palmitate HCl or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Laboratory Tests
During prolonged therapy, periodic liver and kidney function tests and blood counts should be performed.
Drug Interactions
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents.
Antagonism has been demonstrated between clindamycin and erythromycin in vitro. Because of possible clinical significance, these two drugs should not be administered concurrently.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term studies in animals have not been performed with clindamycin to evaluate carcinogenic potential. Genotoxicity tests performed included a rat micronucleus test and an Ames Salmonella reversion test. Both tests were negative.
Fertility studies in rats treated orally with up to 300mg/kg/day (approximately 1.6 times the highest recommended adult human oral dose based on mg/m²) revealed no effects on fertility or mating ability.
Pregnancy:
Teratogenic Effects
Pregnancy Category B
Reproduction studies performed in rats and mice using oral doses of clindamycin up to 600mg/kg/day (3.2 and 1.6 times the highest recommended adult human oral dose based on mg/m², respectively) or subcutaneous doses of clindamycin up to 250mg/kg/day (1.3 and 0.7 times the highest recommended adult human oral dose based on mg/ m², respectively) revealed no evidence of teratogenicity.
There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of the human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Clindamycin has been reported to appear in breast milk in the range of 0.7 to 3.8 mcg/mL.
Pediatric Use
When clindamycin palmitate HCl is administered to the pediatric population (birth to 16 years), appropriate monitoring of organ system functions is desirable.
Geriatric Use
Clinical studies of clindamycin did not include sufficient numbers of patients age 65 and over to determine whether they respond differently from younger patients. However, other reported clinical experience indicates that antibiotic-associated colitis and diarrhea (due to Clostridium difficile) seen in association with most antibiotics occur more frequently in the elderly (>60 years) and may be more sever. These patients should be carefully monitored for the development of diarrhea.
Pharmacokinetic studies with clindamycin have shown no clinically important differences between young subjects (18 to 39 years) and elderly subjects (61 to 79 years) with normal hepatic function and normal (age-adjusted) renal function after oral or intravenous administration.
-
ADVERSE REACTIONS
The following reactions have been reported with the use of clindamycin.
Gastrointestinal: Abdominal pain, pseudomembranous colitis, esophagitis, nausea, vomiting and diarrhea (see WARNING box). The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment (see WARNINGS).
Hypersensitivity Reactions:
Generalized mild to moderate morbilliform-like (maculopapular) skin rashes are the most frequently reported adverse reactions. Vesiculobullous rashes, as well as urticaria, have been observed during drug therapy. Rare instances of erythema multiforme, some resembling Stevens-Johnson syndrome, and a few cases of anaphylactoid reactions have also been reported.
Skin and Mucous Membranes: Pruritus, vaginitis, and rare instances of exfoliative dermatitis have been reported. (See Hypersensitivity Reactions.)
Liver: Jaundice and abnormalities in liver function tests have been observed during clindamycin therapy.
Renal: Although no direct relationship of clindamycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed in rare instances.
Hematopoietic: Transient neutropenia (leukopenia) and eosinophilia have been reported. Reports of agranulocytosis and thrombocytopenia have been made. No direct etiologic relationship to concurrent clindamycin therapy could be made in any of the foregoing.
Musculoskeletal: Rare instances of polyarthritis have been reported.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
If significant diarrhea occurs during therapy, this antibiotic should be discontinued (see WARNING box).
Concomitant administration of food does not adversely affect the absorption of clindamycin palmitate HCl contained in clindamycin palmitate HCl for oral solution, USP (pediatric).
Serious infections: 8 to 12mg/kg/day (4 to 6 mg/lb/day) divided into 3 or 4 equal doses.
Severe infections: 13 to 16mg/kg/day (6.5 to 8 mg/lb/day) divided into 3 or 4 equal doses.
More severe infections: 17 to 25 mg/kg/day (8.5 to 12.5 mg/lb/day) divided into 3 or 4 equal doses.
In pediatric patients weighing 10 kg or less, ½ teaspoon (37.5 mg) three times a day should be considered the minimum recommended dose.
Serious infections due to anaerobic bacteria are usually treated with clindamycin injection. However, in clinically appropriate circumstances, the physician may elect to initiate treatment or continue treatment with clindamycin palmitate HCl for oral solution, USP (pediatric).
NOTE: In cases of β-hemolytic streptococcal infections, treatment should be continued for at least 10 days.
Reconstitution Instructions: When reconstituted with water as follows, each 5 mL (teaspoon) of solution contains clindamycin palmitate HCl equivalent to 75 mg clindamycin.
Reconstitute bottles of 100 mL with 75 mL of water. Add a large portion of the water and shake vigorously; add the remainder of the water and shake until the solution is uniform.
Storage Conditions: Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Do NOT refrigerate the reconstituted solution; when chilled, the solution may thicken and be difficult to pour. The solution is stable for 2 weeks at room temperature.
-
HOW SUPPLIED
Clindamycin palmitate HCl for oral solution, USP (pediatric) is a white to off-white powder forming a clear colorless cherry flavored solution upon constitution with water.
When reconstituted as directed, each bottle yields 100mL of solution containing 75mg of clindamycin per 5mL (NDC: 10135-569-19).
Storage Conditions: Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
-
ANIMAL TOXICOLOGY
One year oral toxicity studies in Spartan Sprague-Dawley rats and beagle dogs at dose levels up to 300 mg/kg/day (approximately 1.6 and 5.4 times the highest recommended adult human oral dose based on mg/m, respectively) have shown clindamycin to be well tolerated. No appreciable difference in pathological findings has been observed between groups of animals treated with clindamycin and comparable control groups. Rats receiving clindamycin hydrochloride at 600 mg/kg/day (approximately 3.2 times the highest recommended adult human oral dose based on mg/m ) for 6 months tolerated the drug well; however, dogs dosed at this level (approximately 10.8 times the highest recommended adult human oral dose based on mg/m ) vomited, would not eat, and lost weight.
Rx only
-
References
1. Smith RB, Phillips JP: Evaluation of CLEOCIN HCl and CLEOCIN Phosphate in an Aged Population. Upjohn TR 8147-82-9122-021, December 1982.
2. Bauer AW, Kirby WMM, Sherris JC, Turck M: Antibiotic susceptibility testing by a standardized single disk method. Am J. Clin. Path., 45:493–496, 1966.
Standardized Disk Susceptibility Test, Federal Register, 37:20527-29, 1972.
Trademarks are the property of their respective owners.
Manufactured for:
Marlex Pharmaceuticals, Inc.
New Castle, DE 19720Distributed by:
Marlex Pharmaceuticals, Inc.
New Castle, DE 19720
Rev. 08/15 - PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
CLINDAMYCIN PALMITATE HYDROCHLORIDE
clindamycin palmitate hydrochloride solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 10135-569 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN PALMITATE HYDROCHLORIDE (UNII: VN9A8JM7M7) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN 75 mg in 5 mL Inactive Ingredients Ingredient Name Strength ICODEXTRIN (UNII: 2NX48Z0A9G) ETHYLPARABEN (UNII: 14255EXE39) POLOXAMER 188 (UNII: LQA7B6G8JG) SUCROSE (UNII: C151H8M554) Product Characteristics Color WHITE (white to off-white) Score Shape Size Flavor CHERRY Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 10135-569-19 1 in 1 BOX 08/01/2015 1 100 mL in 1 BOTTLE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA203513 08/01/2015 Labeler - Marlex Pharmaceuticals Inc (782540215)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
