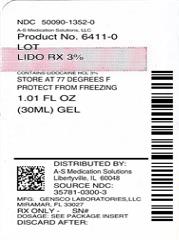
Lido Rx by A-S Medication Solutions LIDO RX- lidocaine gel
Lido Rx by
Drug Labeling and Warnings
Lido Rx by is a Prescription medication manufactured, distributed, or labeled by A-S Medication Solutions. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Lido see full prescribing information for safety and efficacy data and Initial U.S. Approval
INDICATIONS AND USAGE
These highlights do not include all the information needed to use Please see full prescription information (1)
LiDORx® 3% is an Amide type Local Anesthetic indicated for:
Relief of pain, soreness, abrasions, minor burns, insect bites and discomfort due to pruritus, pruritic eczemas, pruritus ani, pruritus vulvae, hemorrhoids, anal fissures, and similar conditions of the skin and mucous membranes. (1)DOSAGE AND ADMINISTRATION
Apply 1-4 pumps to the affected area three or four times daily not to exceed 16 pumps in twenty-four hours (24 Hrs) or as directed by a physician. As a topical anesthesic, apply an adequate amount for the desired procedure to the target area 10 minutes prior to initiation of procedure. (2)
CONTRAINDICATIONS
Traumatized mucosa, secondary bacterial infection of the area of proposed
application and known hypersensitivity to any of the components.
Lidocaine Hydrochloride USP is contraindicated in patients with a known
history of hypersensitivity to local anesthetics of the amide type. (4)WARNINGS AND PRECAUTIONS
For External Use Only. Avoid Contact with Eyes.
If irritation or sensitivity occurs or infection appears, discontinue use and institute appropriate therapy.
LiDORx® 3% should be used with caution in ill, elderly, debilitated patients and children who may be more sensitive to the systemic effects
of Lidocaine Hydrochloride USP.
Methemoglobinemia Warning: Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinernia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended. Signs and symptoms of methemoglobinemia may occur immediately or may be delayed some hours after exposure and are characterized by a cyanotic skin discoloration and abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue LiDORx® and any other oxidizing agents. Depending on the severity of the symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. More severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen. (5)ADVERSE REACTIONS
Most common adverse reactions are redness or swelling at the application site. Less common side effects, such as sluggishness, (6)
confusion, slow breathing, low blood pressure, or slow heartbeat, may occur. (6)
(6)
To report SUSPECTED ADVERSE REACTIONS, contact Gensco Pharma at 855-743-6726 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. (6)
DRUG INTERACTIONS
Prilocaine, Bupivacaine, Amyl nitrates/ sodium nitrate/ sodium thiosulfate, Dofetilide, Iomitapide, Beta-blockers (eg, atenolol), Cimetidine, or Class 1 antiarrhythmic drugs (ex. Mexiletine). Patients that are administered local anesthetics may be at increased risk of developing methemoglobinernia when concurrently exposed to the following oxidizing agents: Nitrates/Nitrites (nitroglycerin, nitroprusside, nitric oxide, nitrous oxide); Local anesthetics (benzocaine, lidocaine, bupivacaine, inepivacaine, tetracaine, prilocaine, procaine, articaine, ropivacaine); Antineoplastic agents (cyclophospharnide, flutamide, rasburicase, ifosfarnide, hydroxyurea); Antibiotics (dapsone, sulfonamides, nitrofurantoin, para-arninosalicvlic acid); Antimalarials (chloroquine, primaquine); Anticonvulsants (phenytoin, sodium valproate, phenobarbital); Other drugs (acetaminophen, metoclopramide, sulfa drugs (i.e., sulfasalazine), quinine).
This may not be a complete list of all interactions that may occur. Ask your health care provider if LiDORx® 3% may interact with other
medicines that you take. (7)Revised: 2/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
Indications
2. Dosage and Administration
2.1 Dosage for children
2.2 Administration
3. Dosage Form and Strength
CONTRAINDICATIONS
5. Warnings and Precautions
6. Adverse Reactions
6.1 Central Nervous System
6.2 Cardiovascular system
6.3 Allergic
7. Drug Interactions
7.1 Serious interactions:
7.2 General interactions:
DRUG INTERACTIONS:
Patients that are administered local anesthetics may be at increased risk of developing methemoglobinemia when concurrently exposed to the following oxidizing agents:
8. Use in Specific Populations
8.1 Use in Pregnancy
8.2 Labor and Delivery
8.4 Pediatric use
8.5 Geriatric use
9. Over Dosage
9.1 Management of local anesthetic emergencies
10. Description
10.1 Active Ingredients
10.2 Inactive Ingredients
11. Clinical Pharmacology
11.1 Mechanism of action
11.2 Onset and duration of anesthesia
11.3 Hemodynamics
11.4 Pharmacokinetics and metabolism
12. Non-Clinical Toxicity
13. How Supplied / Storage and Handling
- * Sections or subsections omitted from the full prescribing information are not listed.
-
Indications
Anesthetic for relief of pain at site of injury; relief of musculoskeletal pain
and soreness; pain from neuropathy; local medical procedures,
injections and vaccines; relief of pruritis, pruritic eczema, abrasions,
minor burns, insect bites, pain, soreness and discomfort due to pruritis
ani, pruritis vulvae, hemorrhoids, anal fissures and similar conditions of
the skin and mucous membranes. -
2. Dosage and Administration
Each pump of the LiDORx® 3% bottle (30mL Airless Pump bottle - NDC: 35781-0300-3) will deliver 0.25 mL of LiDORx® 3% enough to cover
a 2 inch by 2 inch area of skin. A single application should not exceed 4 pumps of the Airless bottle, equal to 1 gram of LiDORx® 3%, (30 mg of
Lidocaine Hydrochloride USP).
No more than 16 pumps of the Airless Pump bottle, approximately 4 grams of LiDORx® 3% (120 mg Lidocaine Hydrochloride USP,) should be
administered in any one day.
Although the incidence of adverse effects with LiDORx® 3% is quite low,caution should be exercised, particularly when employing large amounts,
since the incidence of adverse effects is directly proportional to the total dose of local anesthetic agent administered.2.1 Dosage for children
It is difficult to recommend a maximum dose of any drug for children since this varies as a function of age and weight. For children less
than ten years who have a normal lean body mass and a normal lean body development, the maximum dose may be determined by
the application of one of the standard pediatric drug formulas (e.g., Clark’s rule). For example a child of five years weighing 50 lbs., the
dose of lidocaine should not exceed 75-100 mg when calculated according to Clark’s rule. In any case, the maximum amount of
Lidocaine Hydrochloride USP administered should not exceed 4.3 mg/kg (2.0 mg/lb) of body weight.2.2 Administration
Apply 1-4 pumps to the affected area three or four times daily not to exceed 16 pumps in twenty-four hours (24 Hrs) or as directed by a
physician. As a topical anesthesic, apply an adequate amount for the desired procedure to the target area 10 minutes prior to initiation
of procedure. -
3. Dosage Form and Strength
LiDORx® 1% is a Topical Gel. Each gram of LiDORx® 1% contains 1% Lidocaine Hydrochloride USP (10mg). Lid10ml
LiDORx® 3% is a Topical Gel. Each gram of LiDORx® 3% contains 3% Lidocaine Hydrochloride USP (30mg). Lid30ml
LiDORx® 9% is a Topical Gel. Each gram of LiDORx® 9% contains 9% Lidocaine Hydrochloride USP (90mg). Lid90ml
-
CONTRAINDICATIONS
Lidocaine Hydrochloride USP is contraindicated in patients with a known history of hypersensitivity to local anesthetics of the amide type or to other components of LidoRx 3%.
Do not use LidoRx 3% on traumatized mucosa or in the presence of secondary bacterial infection of the area of proposed application.
-
5. Warnings and Precautions
If irritation or sensitivity occurs or infection appears, discontinue use and institute appropriate therapy. LiDORx® 3% Gel should be used with
caution in ill, elderly, debilitated patients and children who may be more sensitive to the systemic effects of Lidocaine Hydrochloride USP. In case
of accidental ingestion get medical help or contact poison control center right away.Methemoglobinemia: Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients
are at risk for methemoglobinernia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia,
cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites
are more susceptible to developing clinical manifestations of the condition. If local anesthetics must be used in these patients, close
monitoring for symptoms and signs of methemoglobinemia is recommended. Signs and symptoms of methemoglobinemia may
occur immediately or may be delayed some hours after exposure and are characterized by a cyanotic skin discoloration and abnormal
coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious
central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue LiDORx® and
any other oxidizing agents. Depending on the severity of the symptoms, patients may respond to supportive care, i.e., oxygen
therapy, hydration. More severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen -
6. Adverse Reactions
Adverse experiences following the administration of Lidocaine Hydrochloride USP are similar in nature to those observed with other amide local anesthetic agents. These adverse experiences are, in general, dose-related and may result from high plasma levels caused by excessive dosage or rapid absorption, or may result from a hypersensitivity, idiosyncrasy or diminished tolerance on the part of the patient.
Serious adverse experiences are generally systemic in nature. The following types are those most commonly reported:6.1 Central Nervous System
CNS manifestations are excitatory and/or depressant and may be characterized by lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. The excitatory manifestations may be very brief or may not occur at all, in which case the first manifestation of toxicity may be drowsiness merging into unconsciousness and respiratory arrest. Drowsiness following
the administration of Lidocaine Hydrochloride USP is usually an early sign of a high blood level of the drug and may occur as a
consequence of rapid absorption.6.2 Cardiovascular system
Cardiovascular manifestations are usually depressant and are characterized by bradycardia, hypotension, and cardiovascular collapse, which may lead to cardiac arrest.
6.3 Allergic
Allergic reactions are characterized by cutaneous lesions, urticaria, edema or anaphylactoid reactions. Allergic reactions may occur as a result of sensitivity either to the local anesthetic agent or to other components in the formulation. Allergic reactions as a result of sensitivity to Lidocaine Hydrochloride USP are extremely rare and, if they occur, should be managed by conventional means. The detection of sensitivity by skin testing is of doubtful value.
-
7. Drug Interactions
7.1 Serious interactions:
Antiarrhythmic Drugs: LiDORx® 3% should be used with caution in patients receiving Class I antiarrhythmic drugs (such as tocainide and mexiletine) since the toxic effects are additive and potentially synergistic.
Bupivacaine liposome: Lidocaine Hydrochloride USP increases toxicity of Bupivacaine by increasing the free (unencapsulated)bupiacaine.
Dofetilide: Lidocaine Hydrochloride USP increases effects of dofetilide thru pharmacodynamic synergism.
Lomitapide: Lidocaine Hydrochloride USP increases levels of lomitapide by affecting hepatic/intestinal enzymes CYP3A4 metabolism.7.2 General interactions:
DRUG INTERACTIONS:
Patients that are administered local anesthetics may be at increased risk of developing methemoglobinemia when concurrently exposed to the following oxidizing agents:
Class Examples Nitrates/Nitrites Nitroglycerin, Nitroprusside, nitric oxide, nitrous oxide Local anesthetics Benzocaine, Lidocaine, Bupivacaine, Mepivacaine, Letracaine, prilocaine, procaine, articaine, ropivacaine Antincoplastic agents cyclophosphosphamide,flutamide, rasburicase, ifosfamide, hydroxyurea Antibiotics Dapsone, sulfonamides, nitrofurantoin,paraaminosalicylic acid Antimalarials Chloroquine,primaquine Anticonvulsants phenytoin,sodium valproate,phenobarbital Other drugs acetaminophen, metoclopramide, sulfa drugs (i.e, Sulfasalazine), quinine Drugs metabolized via CYP3A4 enzyme: (ex. Antipsychotics, SSRIs, TCAs, many chemotherapeutics, calcium channel bockers, benzodiazopines) Lidocaine Hydrochloride USP may increase serum levels of many drugs metabolized by hepatic / intestinal CYP3A4 enzymes.
Drugs that affect hepatic CYP1A2 enzyme: (ex. Quinoline antibiotics, cimetidine, barbiturates, benzodiazepines, erythromycin) May increase serum Lidocaine Hydrochloride USP levels by decreasing Lidocaine Hydrochloride USP metabolism by CYP1A2 enzyme.
-
8. Use in Specific Populations
8.1 Use in Pregnancy
Teratogenic Effects. Pregnancy Category B. Reproduction studies have been performed in rats at doses up to 6.6 times the human dose and have revealed no evidence of harm to the fetus caused by Lidocaine Hydrochloride USP. There are, however, no adequate and well-controlled studies in pregnant women. Animal reproduction studies are not always predictive of human response. General consideration should be given to this fact before administering Lidocaine Hydrochloride USP to women of childbearing potential, especially during early pregnancy when maximum organogenesis takes place.
8.2 Labor and Delivery
Lidocaine Hydrochloride USP is not contraindicated in labor and delivery. Should LiDORx® 3% be used concomitantly with other products containing Lidocaine Hydrochloride USP, the total dose contributed by all formulations must be kept in mind. 8.3 Nursing Mothers: It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Lidocaine
Hydrochloride USP. is administered to a nursing woman.8.4 Pediatric use
Dosage in children should be reduced, commensurate with age, body weight and physical condition. Caution must be taken to avoid over dosage when applying LiDORx® 3% to large areas of injured or abraded skin, since the systemic absorption of Lidocaine Hydrochloride USP may be
increased under such conditions. -
9. Over Dosage
Acute emergencies from local anesthetics are generally related to high
plasma levels encountered during therapeutic use of local anesthetics.
(see ADVERSE REACTIONS, WARNINGS, and PRECAUTIONS).9.1 Management of local anesthetic emergencies
The first consideration is prevention, best accomplished by careful and constant monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic administration. At the first sign of change, oxygen should be administered. The first step in the management of convulsions consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, small increments of an ultra-short acting barbiturate (such as thiopental or thiamylal) or a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to use of local anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor as directed by the clinical situation (e.g., ephedrine). If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias and cardiac arrest. If cardiac arrest should occur, standard cardiopulmonary resuscitative measures should be instituted. Dialysis is of negligible value in the treatment of acute over dosage with Lidocaine Hydrochloride USP The oral LD50 of Lidocaine HCI USP in non-fasted female rats is 459 (346-773) mg/kg (as the salt) and 214 (159-324) mg/kg (as the salt) in fasted female rats.
- 10. Description
-
11. Clinical Pharmacology
11.1 Mechanism of action
LiDORx® 3% releases Lidocaine Hydrochloride USP from a mild acidic vehicle to stabilize the neuronal membrane by inhibiting the ionic fluxes required for initiation and conduction of impulses, thereby effecting local anesthetic action. A mild acidic vehicle lowers pH to increase protection against alkaline irritations and to provide a favorable environment for healing.
11.2 Onset and duration of anesthesia
LiDORx® 3% effects local, topical anesthesia. The onset is 3-5 minutes. Clinical testing has demonstrated the average onset of anesthesia occurs 5 to 10 minutes after application of LiDORx® 3%. In a study evaluating the onset and duration of anesthesia in 37 healthy volunteers the average time to anesthesia was 8 minutes and 40 seconds while duration of anesthesia in the majority of subjects was between 8-15 minutes (median 10 minutes and 46 seconds). There was considerable inter-subject variation that may be due to subject age and relative skin condition.
11.3 Hemodynamics
Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. These changes may be attributable to a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system.
11.4 Pharmacokinetics and metabolism
Lidocaine Hydrochloride USP may be absorbed following topical administration to mucous membranes or open wounds, its rate and extent of absorption depending upon the specific site of application, duration of exposure, concentration, and total dosage. In general, the rate of absorption of local anesthetic agents following topical application occurs most rapidly after intratracheal administration. Lidocaine Hydrochloride USP is also well-absorbed from the gastrointestinal tract, but little intact drug appears in the circulation because of biotransformation in the liver. Lidocaine Hydrochloride USP is metabolized rapidly by the liver, and metabolites and unchanged drug are excreted by the kidneys. Biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage, and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological actions of
these metabolites are similar to, but less potent than, those of Lidocaine Hydrochloride USP. Approximately 90% of Lidocaine Hydrochloride USP administered is excreted in the form of various metabolites, and less than 10% is excreted unchanged. The primary metabolite in urine is a conjugate of 4-hydroxy-2,6-dimethylaniline. The plasma binding of Lidocaine Hydrochloride USP is dependent on drug concentration, and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 μg of free base per mL, 60 to 80 percent of Lidocaine Hydrochloride USP is protein bound. Binding is also dependent on the plasma concentration of the alpha-l-acid glycoprotein. Lidocaine Hydrochloride USP crosses the blood-brain and placental barriers, presumably by passive diffusion. Studies of Lidocaine Hydrochloride USP metabolism following intravenous bolus injections have shown that the elimination half-life of this agent is typically 1.5 to 2.0 hours. Because of the rapid rate at which Lidocaine Hydrochloride USP is metabolized, any condition that affects liver function may alter Lidocaine Hydrochloride USP kinetics. The half-life may be prolonged two-fold or more in patients with liver dysfunction. Renal dysfunction does not affect Lidocaine Hydrochloride USP kinetics but may increase the accumulation of metabolites. Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of Lidocaine Hydrochloride USP required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6.0 μg free base per mL. In the rhesus monkey arterial blood levels
of 18-21 μg/mL have been shown to be threshold for convulsive activity. - 12. Non-Clinical Toxicity
- 13. How Supplied / Storage and Handling
-
14. Patient Counseling Information
Inform patients that use of local anesthetics may cause methemoglobinemiia, a serious condition that must be treated promptly. Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness or fatique.
What is LiDORx® 3%?
LiDORx® 3% is a topical gel containing 3% lidocaine HCl USP (30mg /gram of gel). Lidocaine Hydrochloride USP is a local anesthetic (numbing medication). It works by blocking nerve signals in your body. LiDORx® 3% (for use on the skin) is used to reduce pain or discomfort caused by skin irritations such as sunburn, insect bites, poison ivy, poison oak, poison sumac, and minor cuts, scratches, hemorrhoids, and burns. LiDORx® 3% may also be used for purposes not listed in this medication guide.
How do I use LiDORx® 3%?
Use exactly as prescribed by your doctor. Do not use in larger or smaller amounts or for longer than recommended. Follow the directions on your
prescription label. LiDORx® 3% is generally for use on the skin only. If your medication comes with patient instructions for safe and effective use, follow these directions carefully. Ask your doctor or pharmacist if you have any questions. Your body may absorb more of this medication if you use too much, if you apply it over large skin areas, or if you apply heat, bandages, or plastic wrap to treated skin areas. Skin that is cut or irritated may also absorb more topical medication than healthy skin. Use the smallest amount of this medication needed to numb the skin or relieve pain. Do not use large amounts of LiDORx® 3%, or cover treated skin areas with a bandage or plastic wrap without medical advice. Be
aware that many cosmetic procedures are performed without a medical doctor present. LiDORx® 3% may be applied with your finger tips or a
cotton swab. Follow your doctor’s instructions. Do not apply this medication to swollen skin areas or deep puncture wounds. Avoid using the medicine on skin that is raw or blistered, such as a severe burn or abrasion. Store at room temperature away from moisture and heat. Keep both used and unused LiDORx® 3% out of the reach of children or pets. The amount of Lidocaine Hydrochloride USP in the gel could be harmful to a child or pet who accidentally sucks on or swallows the gel. Seek emergency medical attention if this happens.What happens if I miss a dose?
Since LiDORx® 3% is used as needed, you may not be on a dosing schedule. If you are using the medication regularly, use the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not use extra medicine to make up the missed dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. LiDORx® 3% applied to the skin is not likely to cause an overdose unless you apply more than the recommended dose. Overdose may also occur if you apply heat, bandages, or plastic wrap to treated skin areas. Improper use of LiDORx® 3% may result in death. Overdose symptoms may include drowsiness, confusion, nervousness, ringing in your ears, blurred vision, feeling hot or cold, numbness, muscle twitches, uneven heartbeats, seizure (convulsions), slowed breathing, or respiratory failure (breathing stops).What should I avoid while using LiDORx® 3%?
Do not allow this medication to come into contact with your eyes. If it does, rinse with water. Avoid using other topical medications on the affected area unless directed by a physician.LiDORx® 3% side effects:
Get emergency medical help if you have any of these signs of an allergic reaction: hives; difficulty breathing; swelling of your face, lips, tongue, or throat.Use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Patients or caregivers should stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue.
Stop using LiDORx® 3% and call your doctor at once if you have any of these serious side effects:
uneven heartbeats;
drowsiness, confusion;
tremors, seizure (convulsions); or
blurred vision.
Less serious side effects include:
mild irritation, redness, or swelling where the medication isapplied; or
numbness in places where the medicine is accidentally applied.This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects
to FDA at 1-800-FDA-1088.PREGNANCY and BREAST-FEEDING:
It is not known if Lidocaine Hydrochloride USP can cause harm to the fetus. If you become pregnant, contact your doctor. You will need to discuss the benefits and risks of using LiDORx® 3% while you are pregnant. It is not known if Lidocaine Hydrochloride USP is found in breast milk after topical use. If you are or will be breast-feeding while you use LiDORx® 3%, check with your doctor. Discuss any possible risks to your baby. - Lidocaine
-
INGREDIENTS AND APPEARANCE
LIDO RX
lidocaine gelProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50090-1352(NDC:35781-0300) Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LIDOCAINE (UNII: 98PI200987) (LIDOCAINE - UNII:98PI200987) LIDOCAINE 30 mg in 1 g Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) CARBOMER COPOLYMER TYPE B (ALLYL PENTAERYTHRITOL CROSSLINKED) (UNII: 809Y72KV36) ISOPROPYL ALCOHOL (UNII: ND2M416302) PETROLATUM (UNII: 4T6H12BN9U) POLYSORBATE 20 (UNII: 7T1F30V5YH) TROLAMINE (UNII: 9O3K93S3TK) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50090-1352-0 1 in 1 CARTON 11/28/2014 1 28.5 g in 1 TUBE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date unapproved drug other 03/01/2013 Labeler - A-S Medication Solutions (830016429) Establishment Name Address ID/FEI Business Operations A-S Medication Solutions 830016429 RELABEL(50090-1352)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.