FENOFIBRATE tablet, coated
Fenofibrate by
Drug Labeling and Warnings
Fenofibrate by is a Prescription medication manufactured, distributed, or labeled by NuCare Pharmaceuticals,Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use FENOFIBRATE TABLETS safely and effectively. See full prescribing information for FENOFIBRATE TABLETS.
FENOFIBRATE tablets for oral use
Initial U.S. Approval: 1993RECENT MAJOR CHANGES
Warnings and Precautions, Hypersensitivity Reactions (5.9) 05/2018
INDICATIONS AND USAGE
Fenofibrate is a peroxisome proliferator receptor alpha (PPARα) activator indicated as an adjunct to diet:
- To reduce elevated LDL-C, Total-C, TG and Apo B, and to increase HDL-C in adult patients with primary hypercholesterolemia or mixed dyslipidemia ( 1.1).
- For treatment of adult patients with severe hypertriglyceridemia ( 1.2).
Limitations of Use: Fenofibrate was not shown to reduce coronary heart disease morbidity and mortality in patients with type 2 diabetes mellitus ( 5.1).
DOSAGE AND ADMINISTRATION
- Primary hypercholesterolemia or mixed dyslipidemia: Initial dose of 145 mg once daily ( 2.2).
- Severe hypertriglyceridemia: Initial dose of 48 to 145 mg once daily. Maximum dose is 145 mg ( 2.3).
- Renally impaired patients: Initial dose of 48 mg once daily ( 2.4).
- Geriatric patients: Select the dose on the basis of renal function ( 2.5).
- May be taken without regard to meals ( 2.1).
DOSAGE FORMS AND STRENGTHS
Oral Tablets: 48 mg and 145 mg ( 3).
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Myopathy and rhabdomyolysis have been reported in patients taking fenofibrate. Risks are increased during co-administration with a statin (with a significantly higher rate observed for gemfibrozil), particularly in elderly patients and patients with diabetes, renal failure, or hypothyroidism (5.2).
- Fenofibrate can increase serum transaminases. Monitor liver tests, including ALT, periodically during therapy (5.3).
- Fenofibrate can reversibly increase serum creatinine levels (5.4). Monitor renal function periodically in patients with renal impairment (8.6).
- Fenofibrate increases cholesterol excretion into the bile, leading to risk of cholelithiasis. If cholelithiasis is suspected, gallbladder studies are indicated (5.5).
- Use caution in concomitant treatment with oral coumarin anticoagulants. Adjust the dosage of coumarin anticoagulant to maintain the prothrombin time/INR at the desired level to prevent bleeding complications (5.6).
- Acute hypersensitivity reactions, including anaphylaxis and angioedema, and delayed hypersensitivity reactions, including severe cutaneous adverse drug reactions have been reported postmarketing. Some cases were life-threatening and required emergency treatment. Discontinue fenofibrate and treat patients appropriately if reactions occur (5.9).
ADVERSE REACTIONS
Adverse reactions > 2% and at least 1% greater than placebo: Abnormal liver tests, increased AST, increased ALT, increased CPK, and rhinitis ( 6).
To report SUSPECTED ADVERSE REACTIONS, contact Aurobindo Pharma USA, Inc. at 1-866-850-2876 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatchDRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 6/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Primary Hypercholesterolemia or Mixed Dyslipidemia
1.2 Severe Hypertriglyceridemia
1.3 Important Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 General Considerations
2.2 Primary Hypercholesterolemia or Mixed Dyslipidemia
2.3 Severe Hypertriglyceridemia
2.4 Impaired Renal Function
2.5 Geriatric Patients
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Mortality and Coronary Heart Disease Morbidity
5.2 Skeletal Muscle
5.3 Liver Function
5.4 Serum Creatinine
5.5 Cholelithiasis
5.6 Coumarin Anticoagulants
5.7 Pancreatitis
5.8 Hematologic Changes
5.9 Hypersensitivity Reactions
5.10 Venothromboembolic Disease
5.11 Paradoxical Decreases in HDL Cholesterol Levels
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Coumarin Anticoagulants
7.2 Immunosuppressants
7.3 Bile Acid Binding Resins
7.4 Colchicine
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Primary Hypercholesterolemia (Heterozygous Familial and Nonfamilial) and Mixed Dyslipidemia
14.2 Severe Hypertriglyceridemia
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Primary Hypercholesterolemia or Mixed Dyslipidemia
Fenofibrate tablets are indicated as adjunctive therapy to diet to reduce elevated low-density lipoprotein cholesterol (LDL-C), total cholesterol (Total-C), Triglycerides and apolipoprotein B (Apo B), and to increase high-density lipoprotein cholesterol (HDL-C) in adult patients with primary hypercholesterolemia or mixed dyslipidemia.
1.2 Severe Hypertriglyceridemia
Fenofibrate tablets are also indicated as adjunctive therapy to diet for treatment of adult patients with severe hypertriglyceridemia. Improving glycemic control in diabetic patients showing fasting chylomicronemia will usually obviate the need for pharmacologic intervention.
Markedly elevated levels of serum triglycerides (e.g., > 2,000 mg/dL) may increase the risk of developing pancreatitis. The effect of fenofibrate therapy on reducing this risk has not been adequately studied.1.3 Important Limitations of Use
Fenofibrate at a dose equivalent to 145 mg of fenofibrate tablets was not shown to reduce coronary heart disease morbidity and mortality in a large, randomized controlled trial of patients with type 2 diabetes mellitus [see Warnings and Precautions (5.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 General Considerations
Patients should be placed on an appropriate lipid-lowering diet before receiving fenofibrate tablets, and should continue this diet during treatment with fenofibrate tablets. Fenofibrate tablets can be given without regard to meals.
The initial treatment for dyslipidemia is dietary therapy specific for the type of lipoprotein abnormality. Excess body weight and excess alcoholic intake may be important factors in hypertriglyceridemia and should be addressed prior to any drug therapy. Physical exercise can be an important ancillary measure. Diseases contributory to hyperlipidemia, such as hypothyroidism or diabetes mellitus should be looked for and adequately treated. Estrogen therapy, thiazide diuretics and beta-blockers, are sometimes associated with massive rises in plasma triglycerides, especially in subjects with familial hypertriglyceridemia. In such cases, discontinuation of the specific etiologic agent may obviate the need for specific drug therapy of hypertriglyceridemia.
Lipid levels should be monitored periodically and consideration should be given to reducing the dosage of fenofibrate tablets if lipid levels fall significantly below the targeted range.
Therapy should be withdrawn in patients who do not have an adequate response after two months of treatment with the maximum recommended dose of 145 mg once daily.2.2 Primary Hypercholesterolemia or Mixed Dyslipidemia
The initial dose of fenofibrate tablets is 145 mg once daily.
2.3 Severe Hypertriglyceridemia
The initial dose is 48 to 145 mg per day. Dosage should be individualized according to patient response, and should be adjusted if necessary following repeat lipid determinations at 4 to 8 week intervals. The maximum dose is 145 mg once daily.
2.4 Impaired Renal Function
Treatment with fenofibrate tablets should be initiated at a dose of 48 mg per day in patients having mild to moderately impaired renal function, and increased only after evaluation of the effects on renal function and lipid levels at this dose. The use of fenofibrate tablets should be avoided in patients with severe renal impairment [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)] .
2.5 Geriatric Patients
Dose selection for the elderly should be made on the basis of renal function [see Use in Specific Populations (8.5)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Fenofibrate tablets are contraindicated in:
- patients with severe renal impairment, including those receiving dialysis [see Clinical Pharmacology (12.3)].
- patients with active liver disease, including those with primary biliary cirrhosis and unexplained persistent liver function abnormalities [see Warnings and Precautions (5.3)].
- patients with preexisting gallbladder disease [see Warnings and Precautions (5.5)] .
- nursing mothers [see Use in Specific Populations (8.3)].
- patients with known hypersensitivity to fenofibrate or fenofibric acid [see Warnings and Precautions (5.9)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Mortality and Coronary Heart Disease Morbidity
The effect of fenofibrate on coronary heart disease morbidity and mortality and non-cardiovascular mortality has not been established.
The Action to Control Cardiovascular Risk in Diabetes Lipid (ACCORD Lipid) trial was a randomized placebo-controlled study of 5518 patients with type 2 diabetes mellitus on background statin therapy treated with fenofibrate. The mean duration of follow-up was 4.7 years. Fenofibrate plus statin combination therapy showed a non-significant 8% relative risk reduction in the primary outcome of major adverse cardiovascular events (MACE), a composite of non-fatal myocardial infarction, non-fatal stroke, and cardiovascular disease death (hazard ratio [HR] 0.92, 95% CI 0.79 to 1.08) (p=0.32) as compared to statin monotherapy. In a gender subgroup analysis, the hazard ratio for MACE in men receiving combination therapy versus statin monotherapy was 0.82 (95% CI 0.69 to 0.99), and the hazard ratio for MACE in women receiving combination therapy versus statin monotherapy was 1.38 (95% CI 0.98 to 1.94) (interaction p=0.01). The clinical significance of this subgroup finding is unclear.
The Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study was a 5-year randomized, placebo-controlled study of 9795 patients with type 2 diabetes mellitus treated with fenofibrate. Fenofibrate demonstrated a non-significant 11% relative reduction in the primary outcome of coronary heart disease events (hazard ratio [HR] 0.89, 95% CI 0.75 to 1.05, p=0.16) and a significant 11% reduction in the secondary outcome of total cardiovascular disease events (HR 0.89 [0.8 to 0.99], p=0.04). There was a non-significant 11% (HR 1.11 [0.95, 1.29], p=0.18) and 19% (HR 1.19 [0.9, 1.57], p=0.22) increase in total and coronary heart disease mortality, respectively, with fenofibrate as compared to placebo.
Because of chemical, pharmacological, and clinical similarities between fenofibrate tablets, clofibrate, and gemfibrozil, the adverse findings in 4 large randomized, placebo-controlled clinical studies with these other fibrate drugs may also apply to fenofibrate.
In the Coronary Drug Project, a large study of post myocardial infarction of patients treated for 5 years with clofibrate, there was no difference in mortality seen between the clofibrate group and the placebo group. There was however, a difference in the rate of cholelithiasis and cholecystitis requiring surgery between the two groups (3% vs. 1.8%).
In a study conducted by the World Health Organization (WHO), 5000 subjects without known coronary artery disease were treated with placebo or clofibrate for 5 years and followed for an additional one year. There was a statistically significant, higher age − adjusted all-cause mortality in the clofibrate group compared with the placebo group (5.7% vs. 3.96%, p = < 0.01). Excess mortality was due to a 33% increase in non- cardiovascular causes, including malignancy, post-cholecystectomy complications, and pancreatitis. This appeared to confirm the higher risk of gallbladder disease seen in clofibrate-treated patients studied in the Coronary Drug Project.
The Helsinki Heart Study was a large (n=4081) study of middle-aged men without a history of coronary artery disease. Subjects received either placebo or gemfibrozil for 5 years, with a 3.5 year open extension afterward. Total mortality was numerically higher in the gemfibrozil randomization group but did not achieve statistical significance (p = 0.19, 95% confidence interval for relative risk G:P = 0.91 to 1.64). Although cancer deaths trended higher in the gemfibrozil group (p = 0.11), cancers (excluding basal cell carcinoma) were diagnosed with equal frequency in both study groups. Due to the limited size of the study, the relative risk of death from any cause was not shown to be different than that seen in the 9 year follow-up data from World Health Organization study (RR=1.29).
A secondary prevention component of the Helsinki Heart Study enrolled middle-aged men excluded from the primary prevention study because of known or suspected coronary heart disease. Subjects received gemfibrozil or placebo for 5 years. Although cardiac deaths trended higher in the gemfibrozil group, this was not statistically significant (hazard ratio 2.2, 95% confidence interval: 0.94 to 5.05). The rate of gallbladder surgery was not statistically significant between study groups, but did trend higher in the gemfibrozil group, (1.9% vs. 0.3%, p = 0.07).5.2 Skeletal Muscle
Fibrates increase the risk for myopathy and have been associated with rhabdomyolysis. The risk for serious muscle toxicity appears to be increased in elderly patients and in patients with diabetes, renal insufficiency, or hypothyroidism.
Myopathy should be considered in any patient with diffuse myalgias, muscle tenderness or weakness, and/or marked elevations of creatine phosphokinase (CPK) levels.
Patients should be advised to report promptly unexplained muscle pain, tenderness or weakness, particularly if accompanied by malaise or fever. CPK levels should be assessed in patients reporting these symptoms, and fenofibrate therapy should be discontinued if markedly elevated CPK levels occur or myopathy/myositis is suspected or diagnosed.
Data from observational studies indicate that the risk for rhabdomyolysis is increased when fibrates, in particular gemfibrozil, are co-administered with an HMG-CoA reductase inhibitor (statin). The combination should be avoided unless the benefit of further alterations in lipid levels is likely to outweigh the increased risk of this drug combination [see Clinical Pharmacology (12.3)].
Cases of myopathy, including rhabdomyolysis, have been reported with fenofibrates co-administered with colchicine, and caution should be exercised when prescribing fenofibrate with colchicine [see Drug Interactions (7.4)] .5.3 Liver Function
Fenofibrate at doses equivalent to 96 mg to 145 mg fenofibrate per day has been associated with increases in serum transaminases [AST (SGOT) or ALT (SGPT)]. In a pooled analysis of 10 placebo-controlled trials, increases to > 3 times the upper limit of normal occurred in 5.3% of patients taking fenofibrate versus 1.1% of patients treated with placebo.
When transaminase determinations were followed either after discontinuation of treatment or during continued treatment, a return to normal limits was usually observed. The incidence of increases in transaminases related to fenofibrate therapy appear to be dose related. In an 8-week dose-ranging study, the incidence of ALT or AST elevations to at least three times the upper limit of normal was 13% in patients receiving dosages equivalent to 96 mg to 145 mg fenofibrate per day and was 0% in those receiving dosages equivalent to 48 mg or less fenofibrate per day, or placebo. Hepatocellular, chronic active and cholestatic hepatitis associated with fenofibrate therapy have been reported after exposures of weeks to several years. In extremely rare cases, cirrhosis has been reported in association with chronic active hepatitis.
Baseline and regular periodic monitoring of liver function, including serum ALT (SGPT) should be performed for the duration of therapy with fenofibrate, and therapy discontinued if enzyme levels persist above three times the normal limit.5.4 Serum Creatinine
Elevations in serum creatinine have been reported in patients on fenofibrate. These elevations tend to return to baseline following discontinuation of fenofibrate. The clinical significance of these observations is unknown. Monitor renal function in patients with renal impairment taking fenofibrate. Renal monitoring should also be considered for patients taking fenofibrate at risk for renal insufficiency such as the elderly and patients with diabetes.
5.5 Cholelithiasis
Fenofibrate, like clofibrate and gemfibrozil, may increase cholesterol excretion into the bile, leading to cholelithiasis. If cholelithiasis is suspected, gallbladder studies are indicated. Fenofibrate therapy should be discontinued if gallstones are found.
5.6 Coumarin Anticoagulants
Caution should be exercised when coumarin anticoagulants are given in conjunction with fenofibrate because of the potentiation of coumarin-type anticoagulant effects in prolonging the Prothrombin Time/International Normalized Ratio (PT/INR). To prevent bleeding complications, frequent monitoring of PT/INR and dose adjustment of the anticoagulant are recommended until PT/INR has stabilized [see Drug Interactions (7.1)].
5.7 Pancreatitis
Pancreatitis has been reported in patients taking fenofibrate, gemfibrozil, and clofibrate. This occurrence may represent a failure of efficacy in patients with severe hypertriglyceridemia, a direct drug effect, or a secondary phenomenon mediated through biliary tract stone or sludge formation with obstruction of the common bile duct.
5.8 Hematologic Changes
Mild to moderate hemoglobin, hematocrit, and white blood cell decreases have been observed in patients following initiation of fenofibrate therapy. However, these levels stabilize during long-term administration. Thrombocytopenia and agranulocytosis have been reported in individuals treated with fenofibrate. Periodic monitoring of red and white blood cell counts are recommended during the first 12 months of fenofibrate administration.
5.9 Hypersensitivity Reactions
Anaphylaxis and angioedema have been reported postmarketing with fenofibrate. In some cases, reactions were life-threatening and required emergency treatment. If a patient develops signs or symptoms of an acute hypersensitivity reaction, advise them to seek immediate medical attention and discontinue fenofibrate. Severe cutaneous adverse drug reactions (SCAR), including Stevens-Johnson syndrome, toxic epidermal necrolysis, and Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), have been reported postmarketing, occurring days to weeks after initiation of fenofibrate. The cases of DRESS were associated with cutaneous reactions (such as rash or exfoliative dermatitis) and a combination of eosinophilia, fever, systemic organ involvement (renal, hepatic, or respiratory). Discontinue fenofibrate and treat patients appropriately if SCAR is suspected. Acute Hypersensitivity
Anaphylaxis and angioedema have been reported postmarketing with fenofibrate. In some cases, reactions were life-threatening and required emergency treatment. If a patient develops signs or symptoms of an acute hypersensitivity reaction, advise them to seek immediate medical attention and discontinue fenofibrate.
Delayed Hypersensitivity
Severe cutaneous adverse drug reactions (SCAR), including Stevens-Johnson syndrome, toxic epidermal necrolysis, and Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), have been reported postmarketing, occurring days to weeks after initiation of fenofibrate. The cases of DRESS were associated with cutaneous reactions (such as rash or exfoliative dermatitis) and a combination of eosinophilia, fever, systemic organ involvement (renal, hepatic, or respiratory). Discontinue fenofibrate and treat patients appropriately if SCAR is suspected.5.10 Venothromboembolic Disease
In the FIELD trial, pulmonary embolus (PE) and deep vein thrombosis (DVT) were observed at higher rates in the fenofibrate- than the placebo-treated group. Of 9,795 patients enrolled in FIELD, there were 4,900 in the placebo group and 4,895 in the fenofibrate group. For DVT, there were 48 events (1%) in the placebo group and 67 (1%) in the fenofibrate group (p = 0.074); and for PE, there were 32 (0.7%) events in the placebo group and 53 (1%) in the fenofibrate group (p = 0.022).
In the Coronary Drug Project, a higher proportion of the clofibrate group experienced definite or suspected fatal or nonfatal pulmonary embolism or thrombophlebitis than the placebo group (5.2% vs. 3.3% at five years; p < 0.01).5.11 Paradoxical Decreases in HDL Cholesterol Levels
There have been postmarketing and clinical trial reports of severe decreases in HDL cholesterol levels (as low as 2 mg/dL) occurring in diabetic and non-diabetic patients initiated on fibrate therapy. The decrease in HDL-C is mirrored by a decrease in apolipoprotein A1. This decrease has been reported to occur within 2 weeks to years after initiation of fibrate therapy. The HDL-C levels remain depressed until fibrate therapy has been withdrawn; the response to withdrawal of fibrate therapy is rapid and sustained. The clinical significance of this decrease in HDL-C is unknown. It is recommended that HDL-C levels be checked within the first few months after initiation of fibrate therapy. If a severely depressed HDL-C level is detected, fibrate therapy should be withdrawn, and the HDL-C level monitored until it has returned to baseline, and fibrate therapy should not be re-initiated.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Adverse events reported by 2% or more of patients treated with fenofibrate (and greater than placebo) during the double-blind, placebo-controlled trials, regardless of causality, are listed in Table 1 below. Adverse events led to discontinuation of treatment in 5% of patients treated with fenofibrate and in 3% treated with placebo. Increases in liver function tests were the most frequent events, causing discontinuation of fenofibrate treatment in 1.6% of patients in double-blind trials.
Table 1. Adverse Reactions Reported by 2% or More of Patients Treated with Fenofibrate and Greater than Placebo During the Double-Blind, Placebo-Controlled Trials. * Dosage equivalent to 145 mg fenofibrate.
** Significantly different from Placebo.BODY SYSTEM
Fenofibrate*
Placebo
Adverse Reaction
(N=439)
(N=365)
BODY AS A WHOLE
Abdominal Pain
4.6%
4.4%
Back Pain
3.4%
2.5%
Headache
3.2%
2.7%
DIGESTIVE
Nausea
2.3%
1.9%
Constipation
2.1%
1.4%
METABOLIC AND NUTRITIONAL DISORDERS
Abnormal Liver Function Tests
7.5%**
1.4%
Increased ALT
3%
1.6%
Increased CPK
3%
1.4%
Increased AST
3.4%**
0.5%
RESPIRATORY
Respiratory Disorder
6.2%
5.5%
Rhinitis
2.3%
1.1%
Urticaria was seen in 1.1% vs. 0%, and rash in 1.4% vs. 0.8% of fenofibrate and placebo patients respectively in controlled trials.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of fenofibrate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure: myalgia, rhabdomyolysis, pancreatitis, acute renal failure, muscle spasm, hepatitis, cirrhosis, anemia, arthralgia, decreases in hemoglobin, decreases in hematocrit, white blood cell decreases, asthenia, and severely depressed HDL-cholesterol levels. Photosensitivity reactions have occurred days to months after initiation; in some of these cases, patients reported a prior photosensitivity reaction to ketoprofen.
-
7 DRUG INTERACTIONS
7.1 Coumarin Anticoagulants
Potentiation of coumarin-type anticoagulant effects has been observed with prolongation of the PT/INR.
Caution should be exercised when coumarin anticoagulants are given in conjunction with fenofibrate. The dosage of the anticoagulants should be reduced to maintain the PT/INR at the desired level to prevent bleeding complications. Frequent PT/INR determinations are advisable until it has been definitely determined that the PT/INR has stabilized [see Warnings and Precautions (5.6)].7.2 Immunosuppressants
Immunosuppressants such as cyclosporine and tacrolimus can produce nephrotoxicity with decreases in creatinine clearance and rises in serum creatinine, and because renal excretion is the primary elimination route of fibrate drugs including fenofibrate, there is a risk that an interaction will lead to deterioration of renal function. The benefits and risks of using fenofibrate tablets with immunosuppressants and other potentially nephrotoxic agents should be carefully considered, and the lowest effective dose employed and renal function monitored.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Safety in pregnant women has not been established. There are no adequate and well controlled studies of fenofibrate in pregnant women. Fenofibrate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In female rats given oral dietary doses of 15, 75, and 300 mg/kg/day of fenofibrate from 15 days prior to mating through weaning, maternal toxicity was observed at 0.3 times the MRHD, based on body surface area comparisons; mg/m 2.
In pregnant rats given oral dietary doses of 14, 127, and 361 mg/kg/day from gestation day 6 to 15 during the period of organogenesis, adverse developmental findings were not observed at 14 mg/kg/day (less than 1 times the MRHD, based on body surface area comparisons; mg/m 2). At higher multiples of human doses evidence of maternal toxicity was observed.
In pregnant rabbits given oral gavage doses of 15, 150, and 300 mg/kg/day from gestation day 6 to 18 during the period of organogenesis and allowed to deliver, aborted litters were observed at 150 mg/kg/day (10 times the MRHD, based on body surface area comparisons: mg/m 2). No developmental findings were observed at 15 mg/kg/day (at less than 1 times the MRHD, based on body surface area comparisons; mg/m 2).
In pregnant rats given oral dietary doses of 15, 75, and 300 mg/kg/day from gestation day 15 through lactation day 21 (weaning), maternal toxicity was observed at less than 1 times the maximum recommended human dose (MRHD), based on body surface area comparisons; mg/m 2.8.3 Nursing Mothers
Fenofibrate should not be used in nursing mothers. A decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.5 Geriatric Use
Fenofibric acid is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Fenofibric acid exposure is not influenced by age. Since elderly patients have a higher incidence of renal impairment, dose selection for the elderly should be made on the basis of renal function [see Dosage and Administration (2.5) and Clinical Pharmacology (12.3)] . Elderly patients with normal renal function should require no dose modifications. Consider monitoring renal function in elderly patients taking fenofibrate.
8.6 Renal Impairment
The use of fenofibrate should be avoided in patients who have severe renal impairment [see Contraindications (4)]. Dose reduction is required in patients with mild to moderate renal impairment [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)]. Monitoring renal function in patients with renal impairment is recommended.
8.7 Hepatic Impairment
The use of fenofibrate has not been evaluated in subjects with hepatic impairment [see Contraindications (4) and Clinical Pharmacology (12.3 )].
-
10 OVERDOSAGE
There is no specific treatment for overdose with fenofibrate. General supportive care of the patient is indicated, including monitoring of vital signs and observation of clinical status, should an overdose occur. If indicated, elimination of unabsorbed drug should be achieved by emesis or gastric lavage; usual precautions should be observed to maintain the airway. Because fenofibric acid is highly bound to plasma proteins, hemodialysis should not be considered.
-
11 DESCRIPTION
Fenofibrate tablets USP, are a lipid regulating agent available as tablets for oral administration. Each tablet contains 48 mg or 145 mg of fenofibrate. The chemical name for fenofibrate is 2-[4-(4-chlorobenzoyl)phenoxy]-2-methyl-propanoic acid, 1-methylethyl ester with the following structural formula:
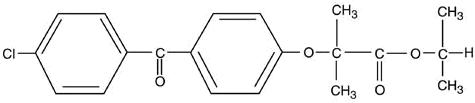
The molecular formula is C 20H 21O 4Cl and the molecular weight is 360.83; fenofibrate is insoluble in water. The melting point is 79 to 82°C. Fenofibrate USP is white or almost white, crystalline powder which is stable under ordinary conditions.
Inactive Ingredients
Each tablet contains crospovidone, hypromellose, magnesium stearate, microcrystalline cellulose, poloxamer, silicified microcrystalline cellulose, sodium lauryl sulfate and sucrose.
In addition individual tablets contain:
48 mg tablets
D&C Yellow No. 10 aluminium lake, FD&C Yellow No. 6 aluminium lake, FD&C Blue No. 2 aluminium lake, polyethylene glycol and titanium dioxide.
145 mg tablets
polyethylene glycol and titanium dioxide. -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The active moiety of fenofibrate is fenofibric acid. The pharmacological effects of fenofibric acid in both animals and humans have been extensively studied through oral administration of fenofibrate.
The lipid-modifying effects of fenofibric acid seen in clinical practice have been explained in vivo in transgenic mice and in vitro in human hepatocyte cultures by the activation of peroxisome proliferator activated receptor α (PPARα). Through this mechanism, fenofibrate increases lipolysis and elimination of triglyceride-rich particles from plasma by activating lipoprotein lipase and reducing production of apoprotein C-III (an inhibitor of lipoprotein lipase activity).
The resulting decrease in TG produces an alteration in the size and composition of LDL from small, dense particles (which are thought to be atherogenic due to their susceptibility to oxidation), to large buoyant particles. These larger particles have a greater affinity for cholesterol receptors and are catabolized rapidly. Activation of PPARα also induces an increase in the synthesis of apolipoproteins A-I, A-II and HDL-cholesterol.
Fenofibrate also reduces serum uric acid levels in hyperuricemic and normal individuals by increasing the urinary excretion of uric acid.12.2 Pharmacodynamics
A variety of clinical studies have demonstrated that elevated levels of total-C, LDL-C, and apo B, an LDL membrane complex, are associated with human atherosclerosis. Similarly, decreased levels of HDL-C and its transport complex, apolipoprotein A (apo AI and apo AII) are associated with the development of atherosclerosis. Epidemiologic investigations have established that cardiovascular morbidity and mortality vary directly with the level of total-C, LDL-C, and TG, and inversely with the level of HDL-C. The independent effect of raising HDL-C or lowering triglycerides (TG) on the risk of cardiovascular morbidity and mortality has not been determined.
Fenofibric acid, the active metabolite of fenofibrate, produces reductions in total cholesterol, LDL cholesterol, apolipoprotein B, total triglycerides and triglyceride rich lipoprotein (VLDL) in treated patients. In addition, treatment with fenofibrate results in increases in high density lipoprotein (HDL) and apolipoproteins apoAI and apoAII.12.3 Pharmacokinetics
Plasma concentrations of fenofibric acid after administration of three 48 mg or one 145 mg tablets are equivalent under fed conditions to one 200 mg micronized fenofibrate capsule.
Fenofibrate is a pro-drug of the active chemical moiety fenofibric acid. Fenofibrate is converted by ester hydrolysis in the body to fenofibric acid which is the active constituent measurable in the circulation.
Absorption
The absolute bioavailability of fenofibrate cannot be determined as the compound is virtually insoluble in aqueous media suitable for injection. However, fenofibrate is well absorbed from the gastrointestinal tract. Following oral administration in healthy volunteers, approximately 60% of a single dose of radiolabelled fenofibrate appeared in urine, primarily as fenofibric acid and its glucuronate conjugate, and 25% was excreted in the feces. Peak plasma levels of fenofibric acid occur within 6 to 8 hours after administration.
Exposure to fenofibric acid in plasma, as measured by C max and AUC, is not significantly different when a single 145 mg dose of fenofibrate is administered under fasting or nonfasting conditions.
Distribution
Upon multiple dosing of fenofibrate, fenofibric acid steady state is achieved within 9 days. Plasma concentrations of fenofibric acid at steady state are approximately double of those following a single dose. Serum protein binding was approximately 99% in normal and hyperlipidemic subjects.
Metabolism
Following oral administration, fenofibrate is rapidly hydrolyzed by esterases to the active metabolite, fenofibric acid; no unchanged fenofibrate is detected in plasma.
Fenofibric acid is primarily conjugated with glucuronic acid and then excreted in urine. A small amount of fenofibric acid is reduced at the carbonyl moiety to a benzhydrol metabolite which is, in turn, conjugated with glucuronic acid and excreted in urine.
In vivo metabolism data indicate that neither fenofibrate nor fenofibric acid undergo oxidative metabolism (e.g., cytochrome P450) to a significant extent.
Elimination
After absorption, fenofibrate is mainly excreted in the urine in the form of metabolites, primarily fenofibric acid and fenofibric acid glucuronide. After administration of radiolabelled fenofibrate, approximately 60% of the dose appeared in the urine and 25% was excreted in the feces.
Fenofibric acid is eliminated with a half-life of 20 hours, allowing once daily dosing.
Special Populations
Geriatrics
In elderly volunteers 77 to 87 years of age, the oral clearance of fenofibric acid following a single oral dose of fenofibrate was 1.2 L/h, which compares to 1.1 L/h in young adults. This indicates that a similar dosage regimen can be used in elderly with normal renal function, without increasing accumulation of the drug or metabolites [see Dosage and Administration (2.5) and Use in Specific Populations (8.5)] .
Pediatrics
The pharmacokinetics of fenofibrate has not been studied in pediatric populations.
Gender
No pharmacokinetic difference between males and females has been observed for fenofibrate.
Race
The influence of race on the pharmacokinetics of fenofibrate has not been studied, however fenofibrate is not metabolized by enzymes known for exhibiting inter-ethnic variability.
Renal Impairment
The pharmacokinetics of fenofibric acid was examined in patients with mild, moderate, and severe renal impairment. Patients with severe renal impairment (estimated glomerular filtration rate [eGFR] < 30 mL/min/1.73 m 2) showed 2.7-fold increase in exposure for fenofibric acid and increased accumulation of fenofibric acid during chronic dosing compared to that of healthy subjects. Patients with mild to moderate renal impairment (eGFR 30 to 59 mL/min/1.73 m 2) had similar exposure but an increase in the half-life for fenofibric acid compared to that of healthy subjects. Based on these findings, the use of fenofibrate should be avoided in patients who have severe renal impairment and dose reduction is required in patients having mild to moderate renal impairment [see Dosage and Administration (2.4)] .
Hepatic Impairment
No pharmacokinetic studies have been conducted in patients with hepatic impairment.
Drug-drug Interactions
In vitro studies using human liver microsomes indicate that fenofibrate and fenofibric acid are not inhibitors of cytochrome (CYP) P450 isoforms CYP3A4, CYP2D6, CYP2E1, or CYP1A2. They are weak inhibitors of CYP2C8, CYP2C19 and CYP2A6, and mild-to-moderate inhibitors of CYP2C9 at therapeutic concentrations.
Table 2 describes the effects of co-administered drugs on fenofibric acid systemic exposure.
Table 3 describes the effects of co-administered fenofibrate or fenofibric acid on other drugs.
Table 2. Effects of Co-Administered Drugs on Fenofibric Acid Systemic Exposure from Fenofibrate Administration 1 Fenofibrate oral tablet
2 Fenofibrate oral micronized capsule
Co-Administered Drug
Dosage Regimen of Co-Administered Drug
Dosage Regimen of Fenofibrate
Changes in Fenofibric Acid Exposure
AUC
C max
Lipid-lowering agents
Atorvastatin
20 mg once daily for 10 days
Fenofibrate 160 mg 1 once daily for 10 days
↓2%
↓4%
Pravastatin
40 mg as a single dose
Fenofibrate 3 x 67 mg 2 as a single dose
↓1%
↓2%
Fluvastatin
40 mg as a single dose
Fenofibrate 160 mg 1 as a single dose
↓2%
↓10%
Anti-diabetic agents
Glimepiride
1 mg as a single dose
Fenofibrate 145 mg 1 once daily for 10 days
↑1%
↓1%
Metformin
850 mg three times daily for 10 days
Fenofibrate 54 mg 1 three times daily for 10 days
↓9%
↓6%
Rosiglitazone
8 mg once daily for 5 days
Fenofibrate 145 mg 1 once daily for 14 days
↑10%
↑3%
Table 3. Effects of Fenofibrate Co-Administration on Systemic Exposure of Other Drugs 1 Fenofibrate oral tablet
2 Fenofibrate oral micronized capsule
Dosage Regimen of Fenofibrate
Dosage Regimen of Co-Administered Drug
Change in Co-Administered Drug Exposure
Analyte
AUC
C max
Lipid-lowering agents
Fenofibrate 160 mg 1 once daily for 10 days
Atorvastatin, 20 mg once daily for 10 days
Atorvastatin
↓17%
0%
Fenofibrate 3 x 67 mg 2 as a single dose
Pravastatin, 40 mg as a single dose
Pravastatin
↑13%
↑13%
3α-Hydroxyl-iso- pravastatin
↑26%
↑29%
Fenofibrate 160 mg 1 as a single dose
Fluvastatin, 40 mg as a single dose
(+)-3R, 5S- Fluvastatin
↑15%
↑16%
Anti-diabetic agents
Fenofibrate 145 mg 1 once daily for 10 days
Glimepiride, 1 mg as a single dose
Glimepiride
↑35%
↑18%
Fenofibrate 54 mg 1 three times daily for 10 days
Metformin, 850 mg three times daily for 10 days
Metformin
↑3%
↑6%
Fenofibrate 145 mg 1 once daily for 14 days
Rosiglitazone, 8 mg once daily for 5 days
Rosiglitazone
↑6%
↓1%
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two dietary carcinogenicity studies have been conducted in rats with fenofibrate. In the first 24-month study, Wistar rats were dosed with fenofibrate at 10, 45, and 200 mg/kg/day, approximately 0.3, 1, and 6 times the maximum recommended human dose (MRHD), based on body surface area comparisons (mg/m 2). At a dose of 200 mg/kg/day (at 6 times the MRHD), the incidence of liver carcinomas was significantly increased in both sexes. A statistically significant increase in pancreatic carcinomas was observed in males at 1 and 6 times the MRHD; an increase in pancreatic adenomas and benign testicular interstitial cell tumors was observed at 6 times the MRHD in males. In a second 24-month rat carcinogenicity study in a different strain of rats (Sprague-Dawley), doses of 10 and 60 mg/kg/day (0.3 and 2 times the MRHD) produced significant increases in the incidence of pancreatic acinar adenomas in both sexes and increases in testicular interstitial cell tumors in males at 2 times the MRHD.
A 117-week carcinogenicity study was conducted in rats comparing three drugs: fenofibrate 10 and 60 mg/kg/day (0.3 and 2 times the MRHD), clofibrate (400 mg/kg/day; 2 times the human dose), and gemfibrozil (250 mg/kg/day; 2 times the human dose, based on mg/m 2 surface area). Fenofibrate increased pancreatic acinar adenomas in both sexes. Clofibrate increased hepatocellular carcinoma and pancreatic acinar adenomas in males and hepatic neoplastic nodules in females. Gemfibrozil increased hepatic neoplastic nodules in males and females, while all three drugs increased testicular interstitial cell tumors in males.
In a 21-month study in CF-1 mice, fenofibrate 10, 45, and 200 mg/kg/day (approximately 0.2, 1, and 3 times the MRHD on the basis of mg/m 2 surface area) significantly increased the liver carcinomas in both sexes at 3 times the MRHD. In a second 18-month study at 10, 60, and 200 mg/kg/day, fenofibrate significantly increased the liver carcinomas in male mice and liver adenomas in female mice at 3 times the MRHD.
Electron microscopy studies have demonstrated peroxisomal proliferation following fenofibrate administration to the rat. An adequate study to test for peroxisome proliferation in humans has not been done, but changes in peroxisome morphology and numbers have been observed in humans after treatment with other members of the fibrate class when liver biopsies were compared before and after treatment in the same individual.
Mutagenesis: Fenofibrate has been demonstrated to be devoid of mutagenic potential in the following tests: Ames, mouse lymphoma, chromosomal aberration and unscheduled DNA synthesis in primary rat hepatocytes.
Impairment of Fertility: In fertility studies rats were given oral dietary doses of fenofibrate, males received 61 days prior to mating and females 15 days prior to mating through weaning which resulted in no adverse effect on fertility at doses up to 300 mg/kg/day (~10 times the MRHD, based on mg/m 2 surface area comparisons). -
14 CLINICAL STUDIES
14.1 Primary Hypercholesterolemia (Heterozygous Familial and Nonfamilial) and Mixed Dyslipidemia
The effects of fenofibrate at a dose equivalent to 145 mg fenofibrate tablets per day were assessed from four randomized, placebo-controlled, double-blind, parallel-group studies including patients with the following mean baseline lipid values: total-C 306.9 mg/dL; LDL-C 213.8 mg/dL; HDL-C 52.3 mg/dL; and triglycerides 191 mg/dL. Fenofibrate therapy lowered LDL-C, Total-C, and the LDL-C/HDL-C ratio. Fenofibrate therapy also lowered triglycerides and raised HDL-C (see Table 4).
Table 4. Mean Percent Change in Lipid Parameters at End of Treatment † † Duration of study treatment was 3 to 6 months.
* p = < 0.05 vs. PlaceboTreatment Group
Total-C
LDL-C
HDL-C
TG
Pooled Cohort
Mean baseline lipid values (n=646)
306.9 mg/dL
213.8 mg/dL
52.3 mg/dL
191 mg/dL
All FEN (n=361)
-18.7%*
-20.6%*
+11%*
-28.9%*
Placebo (n=285)
-0.4%
-2.2%
+0.7%
+7.7%
Baseline LDL-C > 160 mg/dL and TG < 150 mg/dL
Mean baseline lipid values (n=334)
307.7 mg/dL
227.7 mg/dL
58.1 mg/dL
101.7 mg/dL
All FEN (n=193)
-22.4%*
-31.4%*
+9.8%*
-23.5%*
Placebo (n=141)
+0.2%
-2.2%
+2.6%
+11.7%
Baseline LDL-C >160 mg/dL and TG ≥ 150 mg/dL
Mean baseline lipid values (n=242)
312.8 mg/dL
219.8 mg/dL
46.7 mg/dL
231.9 mg/dL
All FEN (n=126)
-16.8%*
-20.1%*
+14.6%*
-35.9%*
Placebo (n=116)
-3%
-6.6%
+2.3%
+0.9%
In a subset of the subjects, measurements of apo B were conducted. Fenofibrate treatment significantly reduced apo B from baseline to endpoint as compared with placebo (-25.1% vs. 2.4%, p < 0.0001, n=213 and 143 respectively).
14.2 Severe Hypertriglyceridemia
The effects of fenofibrate on serum triglycerides were studied in two randomized, double-blind, placebo- controlled clinical trials of 147 hypertriglyceridemic patients. Patients were treated for eight weeks under protocols that differed only in that one entered patients with baseline TG levels of 500 to 1500 mg/dL, and the other TG levels of 350 to 500 mg/dL. In patients with hypertriglyceridemia and normal cholesterolemia with or without hyperchylomicronemia, treatment with fenofibrate at dosages equivalent to fenofibrate 145 mg per day decreased primarily very low density lipoprotein (VLDL) triglycerides and VLDL cholesterol. Treatment of patients with elevated triglycerides often results in an increase of LDL-C (see Table 5).
Table 5. Effects of Fenofibrate in Patients With Severe Hypertriglyceridemia * =p < 0.05 vs. Placebo Study 1
Placebo
Fenofibrate
Baseline TG levels 350 to 499 mg/dL
N
Baseline (Mean)
Endpoint (Mean)
% Change (Mean)
N
Baseline (Mean)
Endpoint (Mean)
% Change (Mean)
Triglycerides
28
449
450
-0.5
27
432
223
-46.2*
VLDL Triglycerides
19
367
350
2.7
19
350
178
-44.1*
Total Cholesterol
28
255
261
2.8
27
252
227
-9.1*
HDL Cholesterol
28
35
36
4
27
34
40
19.6*
LDL Cholesterol
28
120
129
12
27
128
137
14.5
VLDL Cholesterol
27
99
99
5.8
27
92
46
-44.7*
Study 2
Placebo
Fenofibrate
Baseline TG levels 500 to 1500 mg/dL
N
Baseline (Mean)
Endpoint (Mean)
% Change (Mean)
N
Baseline (Mean)
Endpoint (Mean)
% Change (Mean)
Triglycerides
44
710
750
7.2
48
726
308
-54.5*
VLDL Triglycerides
29
537
571
18.7
33
543
205
-50.6*
Total Cholesterol
44
272
271
0.4
48
261
223
-13.8*
HDL Cholesterol
44
27
28
5
48
30
36
22.9*
LDL Cholesterol
42
100
90
-4.2
45
103
131
45*
VLDL Cholesterol
42
137
142
11
45
126
54
-49.4*
The effect of fenofibrate on cardiovascular morbidity and mortality has not been determined.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
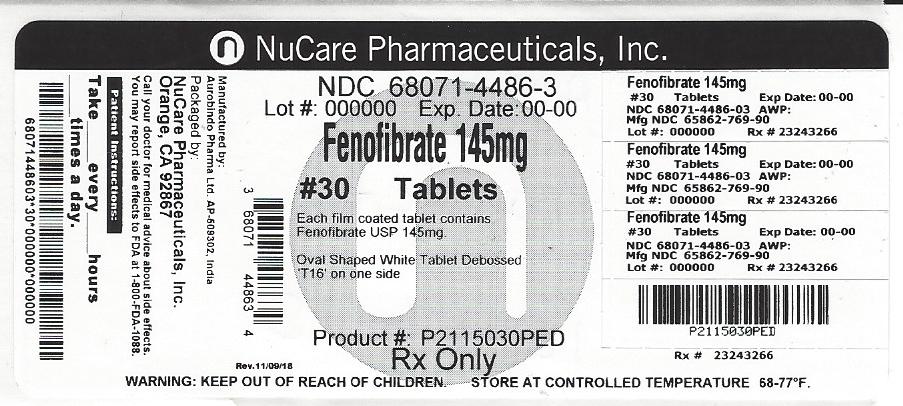
Fenofibrate Tablets USP, 145 mg are white colored, biconvex, oval shaped, coated tablets debossed with T 16 on one side and plain on other side.
NDC: 68071-4486-2 BOTTLES OF 20NDC: 68071-4486-3 BOTTLES OF 30
Storage
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Keep out of the reach of children. Protect from moisture. -
17 PATIENT COUNSELING INFORMATION
Patients should be advised:
- of the potential benefits and risks of fenofibrate.
- not to use fenofibrate if there is a known hypersensitivity to fenofibrate or fenofibric acid.
- of medications that should not be taken in combination with fenofibrate.
- that if they are taking coumarin anticoagulants, fenofibrate may increase their anti-coagulant effect, and increased monitoring may be necessary.
- to continue to follow an appropriate lipid-modifying diet while taking fenofibrate.
- to take fenofibrate once daily, without regard to food, at the prescribed dose, swallowing each tablet whole.
- to return for routine monitoring.
- to inform their physician of all medications, supplements, and herbal preparations they are taking and any change to their medical condition. Patients should also be advised to inform their physicians prescribing a new medication that they are taking fenofibrate.
- to inform their physician of any muscle pain, tenderness, or weakness; onset of abdominal pain; or any other new symptoms.
Distributed by:
Aurobindo Pharma USA, Inc.
279 Princeton-Hightstown Road
East Windsor, NJ 08520
Manufactured by:
Aurobindo Pharma Limited
Hyderabad-500 038, India
Revised: 06/2018 - PACKAGE LABEL-PRINCIPAL DISPLAY PANEL - )
-
INGREDIENTS AND APPEARANCE
FENOFIBRATE
fenofibrate tablet, coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68071-4486(NDC:65862-769) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FENOFIBRATE (UNII: U202363UOS) (FENOFIBRIC ACID - UNII:BGF9MN2HU1) FENOFIBRATE 145 mg Inactive Ingredients Ingredient Name Strength CROSPOVIDONE (UNII: 68401960MK) HYPROMELLOSE 2910 (3 MPA.S) (UNII: 0VUT3PMY82) HYPROMELLOSE 2910 (6 MPA.S) (UNII: 0WZ8WG20P6) HYPROMELLOSE 2910 (15 MPA.S) (UNII: 36SFW2JZ0W) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLOXAMER 407 (UNII: TUF2IVW3M2) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) SODIUM LAURYL SULFATE (UNII: 368GB5141J) SUCROSE (UNII: C151H8M554) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color white Score no score Shape OVAL (Biconvex) Size 18mm Flavor Imprint Code T;16 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68071-4486-2 20 in 1 BOTTLE; Type 0: Not a Combination Product 07/09/2018 2 NDC: 68071-4486-3 30 in 1 BOTTLE; Type 0: Not a Combination Product 07/09/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205118 05/05/2016 Labeler - NuCare Pharmaceuticals,Inc. (010632300) Establishment Name Address ID/FEI Business Operations NuCare Pharmaceuticals,Inc. 010632300 repack(68071-4486)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
 <
<