BETOPTIC S- betaxolol hydrochloride suspension/ drops
Drug Labeling and Warnings
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use BETOPTIC S safely and effectively. See full prescribing information for BETOPTIC S.
BETOPTIC S® Ophthalmic Suspension 0.25% as base, sterile topical ophthalmic drops
Initial U.S. Approval: 1985INDICATIONS AND USAGE
BETOPTIC S Ophthalmic Suspension 0.25% is a beta-adrenergic receptor inhibitor indicated for the treatment of elevated intraocular pressure (IOP) in patients with chronic open-angle glaucoma or ocular hypertension (1).
DOSAGE AND ADMINISTRATION
- Instill one drop in the affected eye(s) twice daily (2)
DOSAGE FORMS AND STRENGTHS
- Bottles filled with 10 and 15 mL of 0.25% sterile ophthalmic suspension (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Same adverse reactions found with systemic administration of beta-adrenergic receptor inhibitors may occur with topical ophthalmic administration (5.1)
- Treatment should be discontinued at the first signs of cardiac failure (5.2)
- Beta-adrenergic receptor inhibitors may mask the signs and symptoms of acute hypoglycemia and should be administered with caution in diabetic patients subject to hypoglycemia (5.3)
- Beta-adrenergic receptor inhibitors may mask certain clinical signs (e.g., tachycardia) or hyperthyroidism (5.4)
ADVERSE REACTIONS
The most frequent adverse reaction is transient ocular discomfort (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Alcon Laboratories, Inc. at 1-800-757-9195 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 General
5.2 Cardiac Failure
5.3 Diabetes Mellitus
5.4 Thyrotoxicosis
5.5 Muscle Weakness
5.6 Surgical Anesthesia
5.7 Bronchospasm and Obstructive Pulmonary Disease
5.8 Atopy/Anaphylaxis
5.9 Angle-Closure Glaucoma
5.10 Vascular Insufficiency
5.11 Bacterial Keratitis
5.12 Choroidal Detachment
5.13 Contact Lens Wear
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Additional Potential Adverse Reactions Associated with Betaxolol
7 DRUG INTERACTIONS
7.1 Oral Beta-Adrenergic Receptor Inhibitors
7.2 Catecholamine-Depleting Drugs
7.3 Concomitant Adrenergic Psychotropic Drugs
7.4 Calcium Antagonists, Antiarrhythmics and Digitalis
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
- 2 DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 General
As with many topically applied ophthalmic drugs, this drug is absorbed systemically. The same adverse reactions found with systemic administration of beta-adrenergic receptor inhibitors may occur with topical administration. For example, severe respiratory reactions and cardiac reactions, including death due to bronchospasm in patients with asthma, and death due to cardiac failure, have been reported with topical application of beta-adrenergic receptor inhibitors.
5.2 Cardiac Failure
BETOPTIC S Ophthalmic Suspension 0.25% has been shown to have a minor effect on heart rate and blood pressure in clinical studies. Caution should be used in treating patients with a history of cardiac failure or heart block. Treatment with BETOPTIC S Ophthalmic Suspension 0.25% should be discontinued at the first signs of cardiac failure.
5.3 Diabetes Mellitus
Beta-adrenergic receptor inhibitors should be administered with caution in patients subject to hypoglycemia or to diabetic patients (especially those with labile diabetes) who are receiving insulin or oral hypoglycemic agents.
Beta-adrenergic receptor inhibitors may mask the signs and symptoms of acute hypoglycemia.5.4 Thyrotoxicosis
Beta-adrenergic receptor inhibitors may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta-adrenergic receptor inhibitors, which might precipitate a thyroid storm.
5.5 Muscle Weakness
Beta-adrenergic receptor inhibitors have been reported to potentiate muscle weakness consistent with certain myasthenic symptoms (e.g., diplopia, ptosis and generalized weakness).
5.6 Surgical Anesthesia
The necessity or desirability of withdrawal of beta-adrenergic receptor inhibitors prior to major surgery is controversial. Beta-adrenergic receptor inhibitors impair the ability of the heart to respond to beta adrenergically mediated reflex stimuli. This may augment the risk of general anesthesia in surgical procedures. Some patients receiving beta-adrenergic receptor inhibitors have experienced protracted, severe hypotension during anesthesia. Difficulty in restarting and maintaining the heartbeat has also been reported. In patients undergoing elective surgery, consider gradual withdrawal of beta-adrenergic receptor inhibitors. If necessary during surgery, the effects of beta-adrenergic receptor inhibitors may be reversed by sufficient doses of adrenergic agonists.
5.7 Bronchospasm and Obstructive Pulmonary Disease
Caution should be exercised in the treatment of glaucoma patients with excessive restriction of pulmonary function. There have been reports of asthmatic attacks and pulmonary distress during betaxolol treatment. Although re-challenges of some such patients with ophthalmic betaxolol has not adversely affected pulmonary function test results, the possibility of adverse pulmonary effects in patients sensitive to beta-adrenergic receptor inhibitors cannot be ruled out.
5.8 Atopy/Anaphylaxis
While taking beta-adrenergic receptor inhibitors, patients with a history of atopy or a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated accidental, diagnostic, or therapeutic challenge with such allergens. Such patients may be unresponsive to the usual doses of epinephrine used to treat anaphylactic reactions.
5.9 Angle-Closure Glaucoma
In patients with angle-closure glaucoma, the immediate treatment objective is to reopen the angle. This may require constricting the pupil. Betaxolol has little or no effect on the pupil and should not be used alone in the treatment of angle-closure glaucoma.
5.10 Vascular Insufficiency
Because of potential effects of beta-adrenergic receptor inhibitors on blood pressure and pulse, these inhibitors should be used with caution in patients with vascular insufficiency. If signs or symptoms suggesting reduced cerebral blood flow or Raynaud’s phenomenon develop following initiation of therapy with BETOPTIC S Ophthalmic Suspension 0.25%, alternative therapy should be considered.
5.11 Bacterial Keratitis
Bacterial keratitis may occur with use of multiple dose containers of topical ophthalmic products when these containers are inadvertently contaminated by patients who, in most cases, had a concurrent corneal disease or a disruption of the ocular epithelial surface. Instruct patients on appropriate instillation techniques [see Patient Counseling Information (17)].
5.12 Choroidal Detachment
Choroidal detachment after filtration procedures has been reported with the administration of aqueous suppressant therapy.
5.13 Contact Lens Wear
The preservative in BETOPTIC S Ophthalmic Suspension 0.25%, benzalkonium chloride, may be absorbed by soft contact lenses. Contact lenses should be removed during instillation of BETOPTIC S Ophthalmic Suspension 0.25% but may be reinserted 15 minutes after instillation [see Patient Counseling Information (17)].
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials, the most frequent adverse reaction associated with the use of BETOPTIC S Ophthalmic Suspension 0.25% has been transient ocular discomfort. The following other adverse reactions have been reported in small numbers of patients:
Ocular: blurred vision, corneal punctate keratitis, foreign body sensation, photophobia, tearing, itching, dryness of eyes, erythema, inflammation, discharge, ocular pain, decreased visual acuity and crusty lashes.
Systemic adverse reactions include:
Cardiovascular: Bradycardia, heart block and congestive failure.
Pulmonary: Pulmonary distress characterized by dyspnea, bronchospasm, thickened bronchial secretions, asthma and respiratory failure.
Central Nervous System: Insomnia, dizziness, vertigo, headaches, depression, lethargy, and increase in signs and symptoms of myasthenia gravis.
Other: Hives, toxic epidermal necrolysis, hair loss and glossitis. Perversions of taste and smell have been reported.
In a 3-month, double-masked, active-controlled, multicenter study in pediatric patients, the adverse reaction profile of BETOPTIC S Ophthalmic Suspension 0.25% was comparable to that seen in adult patients.
-
7 DRUG INTERACTIONS
7.1 Oral Beta-Adrenergic Receptor Inhibitors
Patients who are receiving a beta-adrenergic receptor inhibitor orally and BETOPTIC S Ophthalmic Suspension 0.25% should be observed for a potential additive effect either on the IOP or on the known systemic effects of beta blockade.
7.2 Catecholamine-Depleting Drugs
Close observation of the patient is recommended when a beta-adrenergic receptor inhibitor is administered to patients receiving catecholamine-depleting drugs such as reserpine, because of possible additive effects and the production of hypotension and/or bradycardia which may result in vertigo, syncope, or postural hypotension.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C: Reproduction, teratology, and peri- and postnatal studies have been conducted with orally administered betaxolol HCl in rats and rabbits. There was evidence of drug related postimplantation loss in rabbits and rats at dose levels above 12 mg/kg and 128 mg/kg, respectively. Betaxolol HCl was not shown to be teratogenic, however, and there were no other adverse effects on reproduction at subtoxic dose levels. There are no adequate and well-controlled studies in pregnant women.
BETOPTIC S Ophthalmic Suspension 0.25% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
8.3 Nursing Mothers
It is not known whether betaxolol HCl is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when BETOPTIC S Ophthalmic Suspension 0.25% is administered to nursing women.
-
10 OVERDOSAGE
No information is available on overdosage in humans. The oral LD50 of the drug ranged from 350 - 920 mg/kg in mice and 860 - 1050 mg/kg in rats. The symptoms which might be expected with an overdose of a systemically administered beta-adrenergic receptor inhibitor are bradycardia, hypotension, bronchospasm and acute cardiac failure.
A topical overdose of BETOPTIC S Ophthalmic Suspension 0.25% may be flushed from the eye(s) with warm tap water. If overdose occurs, treatment should be symptomatic and supportive.
-
11 DESCRIPTION
BETOPTIC S Ophthalmic Suspension 0.25% contains betaxolol hydrochloride, a cardioselective beta-adrenergic receptor inhibitor, in a sterile resin suspension formulation. Betaxolol hydrochloride is a white, crystalline powder, with a molecular weight of 343.89. The chemical structure is presented below.
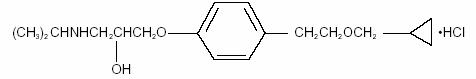
Empirical Formula: C18H29NO3HCl
Chemical Name:
(±)-1-[p-[2-(cyclopropylmethoxy) ethyl]phenoxy]-3-(isopropylamino)-2-propanol hydrochloride.Each mL of BETOPTIC S Ophthalmic Suspension 0.25% contains: Active: betaxolol HCl 2.8 mg equivalent to 2.5 mg of betaxolol base. Preservative: benzalkonium chloride 0.01%. Inactives: mannitol, poly (styrene-divinyl benzene) sulfonic acid, carbomer 934P, edetate disodium, hydrochloric acid or sodium hydroxide (to adjust pH) and purified water.
BETOPTIC S Ophthalmic Suspension 0.25% has pH of approximately 7.6 and an osmolality of approximately 290 mOsmol/kg.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Betaxolol HCl, a cardioselective (beta-1-adrenergic) receptor inhibitor, does not have significant membrane-stabilizing (local anesthetic) activity and is devoid of intrinsic sympathomimetic action. Orally administered beta-adrenergic receptor inhibitors reduce cardiac output in healthy subjects and patients with heart disease. In patients with severe impairment of myocardial function, beta-adrenergic receptor antagonists may inhibit the sympathetic stimulatory effect necessary to maintain adequate cardiac function.
When instilled in the eye, BETOPTIC S Ophthalmic Suspension 0.25% has the action of reducing elevated IOP, whether or not accompanied by glaucoma. Ophthalmic betaxolol has minimal effect on pulmonary and cardiovascular parameters.
Elevated IOP presents a major risk factor in glaucomatous field loss. The higher the level of IOP, the greater the likelihood of optic nerve damage and visual field loss. Betaxolol has the action of reducing elevated as well as normal IOP and the mechanism of ocular hypotensive action appears to be a reduction of aqueous production as demonstrated by tonography and aqueous fluorophotometry.
12.2 Pharmacodynamics
The onset of action with betaxolol can generally be noted within 30 minutes and the maximum effect can usually be detected 2 hours after topical administration. A single dose provides a 12-hour reduction in IOP. In some patients, the IOP lowering responses to BETOPTIC S may require a few weeks to stabilize. As with any new medication, careful monitoring of patients is advised.
Ophthalmic betaxolol solution at 1% (one drop in each eye) was compared to placebo in a crossover study challenging nine patients with reactive airway disease. Betaxolol HCl had no significant effect on pulmonary function as measured by Forced Expiratory Volume in 1 second (FEV1), Forced Vital Capacity (FVC), FEV1/FVC and was not significantly different from placebo. The action of isoproterenol, a beta stimulant, administered at the end of the study was not inhibited by ophthalmic betaxolol.
No evidence of cardiovascular beta adrenergic-blockade during exercise was observed with betaxolol in a double-masked, crossover study in 24 normal subjects comparing ophthalmic betaxolol and placebo for effects on blood pressure and heart rate.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime studies with betaxolol HCl have been completed in mice at oral doses of 6, 20 or 60 mg/kg/day and in rats at 3, 12 or 48 mg/kg/day; betaxolol HCl demonstrated no carcinogenic effect. Higher dose levels were not tested.
In a variety of in vitro and in vivo bacterial and mammalian cell assays, betaxolol HCl was nonmutagenic.
- 14 CLINICAL STUDIES
-
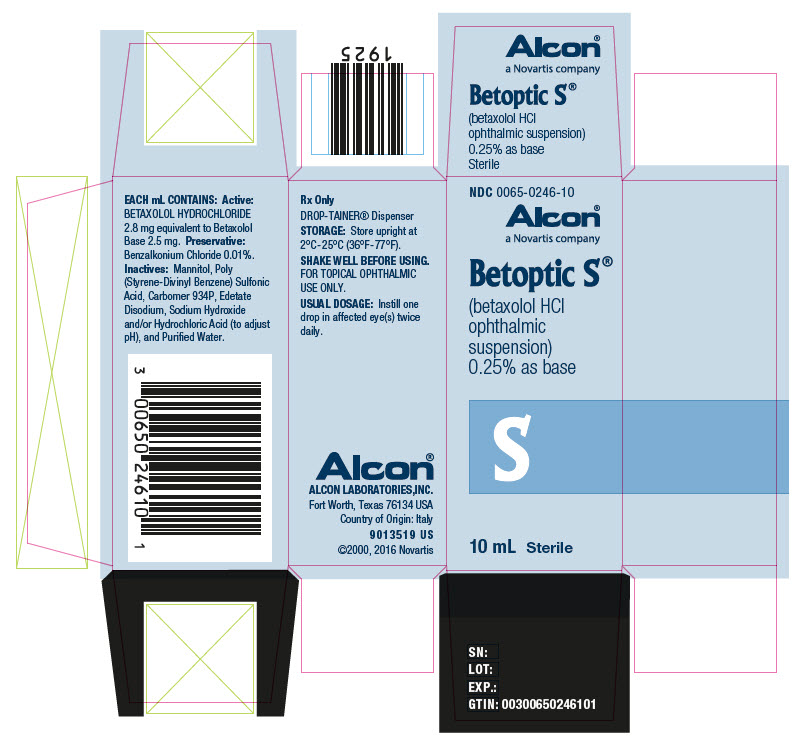
16 HOW SUPPLIED/STORAGE AND HANDLING
BETOPTIC S Ophthalmic Suspension 0.25% is supplied as follows: 10 and 15 mL in plastic ophthalmic DROP-TAINER® dispensers. Tamper evidence is provided with a shrink band around the closure and neck area of the DROP-TAINER® package.
10 mL NDC 0065-0246-10
15 mL NDC 0065-0246-15Storage and Handling
Store upright at 2°C - 25°C (36°F - 77°F).
Shake well before using. -
17 PATIENT COUNSELING INFORMATION
Avoiding Contamination of the Product
Instruct patients to avoid allowing the tip of the dispensing container to contact the eye(s) or surrounding structures. Also instruct patients that ocular solutions, if handled improperly, could become contaminated by common bacteria known to cause ocular infections. Serious damage to the eye(s) and subsequent loss of vision may result from using contaminated solutions.Intercurrent Ocular Conditions
Advise patients that if they have ocular surgery or develop an intercurrent ocular condition (e.g., trauma or infection), they should immediately seek their physician’s advice concerning the continued use of the present multidose container.Concomitant Topical Ocular Therapy
Advise patients requiring concomitant topical ophthalmic medications to administer these at least 10 minutes before instilling BETOPTIC S Suspension.Temporary Blurred Vision
Vision may be temporarily blurred following dosing with BETOPTIC S Ophthalmic Suspension 0.25%. Care should be exercised in operating machinery or driving a motor vehicle.Contact Lens Wear
The preservative in BETOPTIC S Ophthalmic Suspension 0.25%, benzalkonium chloride, may be absorbed by soft contact lenses. Remove contact lenses during instillation of BETOPIC S Ophthalmic Suspension 0.25%. Contact lenses may be reinserted 15 minutes after instillation.© 2003, 2007- 2009, 2016 Novartis
Distributed by:
Alcon Laboratories, Inc.
Fort Worth, Texas 76134
Alcon®
a Novartis company
T2017-21
March 2017
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
BETOPTIC S
betaxolol hydrochloride suspension/ dropsProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0065-0246 Route of Administration OPHTHALMIC Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Betaxolol Hydrochloride (UNII: 6X97D2XT0O) (Betaxolol - UNII:O0ZR1R6RZ2) Betaxolol Hydrochloride 2.8 mg in 1 mL Inactive Ingredients Ingredient Name Strength Mannitol (UNII: 3OWL53L36A) Edetate Disodium (UNII: 7FLD91C86K) Hydrochloric Acid (UNII: QTT17582CB) Sodium Hydroxide (UNII: 55X04QC32I) Benzalkonium Chloride (UNII: F5UM2KM3W7) Water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0065-0246-10 1 in 1 CARTON 01/15/1996 1 10 mL in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 2 NDC: 0065-0246-15 1 in 1 CARTON 01/15/1996 2 15 mL in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA019845 01/15/1996 Labeler - Alcon Laboratories, Inc. (008018525)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.