PHENYLEPHRINE HYDROCHLORIDE INJECTION, SOLUTION injection, solution
phenylephrine hydrochloride injection, solution by
Drug Labeling and Warnings
phenylephrine hydrochloride injection, solution by is a Prescription medication manufactured, distributed, or labeled by Dr. Reddy's Laboratories Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Phenylephrine Hydrochloride in 0.9% Sodium Chloride Injection safely and effectively. See full prescribing information for Phenylephrine Hydrochloride Injection.
PHENYLEPHRINE HYDROCHLORIDE IN SODIUM CHLORIDE injection, for intravenous use
Initial U.S. Approval: 2012INDICATIONS AND USAGE
Phenylephrine Hydrochloride in 0.9% Sodium Chloride Injection is an alpha-1 adrenergic receptor agonist indicated for increasing blood pressure in adults with clinically important hypotension resulting primarily from vasodilation, in the setting of anesthesia (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
njection: 20 mg in 250 mL (80 mcg/mL) of phenylephrine hydrochloride (equivalent to 16.4 mg of phenylephrine base per 250 mL) in 0.9% Sodium Chloride, supplied in a ready-to-use, single-dose intravenous solution bag (3, 11, 16) (3)
CONTRAINDICATIONS
- Hypersensitivity to it or any of its components (4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
Most common adverse reactions: nausea and vomiting, headache, nervousness (6)
To report SUSPECTED ADVERSE REACTIONS, contact Dr. Reddy’s Laboratories Inc., at 1-888-375-3784 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Agonistic effects with monoamine oxidase inhibitors (MAOI), β-adrenergic blocking agents, α-2 adrenergic agonists, steroids, tricyclic antidepressants, norepinephrine transport inhibitors, ergot alkaloids, centrally-acting sympatholytic agents and atropine sulfate (7.1)
- Antagonistic effects on and by α-adrenergic blocking agents (7.2)
Revised: 6/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Administration Instructions
2.2 Recommended Dosage
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Exacerbation of Angina, Heart Failure, or Pulmonary Arterial Hypertension
5.2 Bradycardia
5.3 Risk in Patients with Autonomic Dysfunction
5.4 Skin and Subcutaneous Necrosis
5.5 Pressor Effect with Concomitant Oxytocic Drugs
5.6 Peripheral and Visceral Ischemia
5.7 Renal Toxicity
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 Agonists
7.2 Antagonists
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 General Administration Instructions
During Phenylephrine Hydrochloride in 0.9% Sodium Chloride Injection, 80 mcg/mL (20 mg/250 mL) administration:
- Correct intravascular volume depletion.
- Correct acidosis. Acidosis may reduce the effectiveness of phenylephrine
Phenylephrine Hydrochloride in 0.9% Sodium Chloride Injection, 80 mcg/mL (20 mg/250 mL) is supplied as a premixed, ready to administer product that requires no further dilution prior to infusion.
Parenteral drug products should be inspected for particulate matter and discoloration prior to administration. Do not use if the solution is coloured or cloudy, or if it contains particulate matter.
Discard any unused portion.
2.2 Recommended Dosage
In adult patients undergoing surgical procedures with either neuraxial anesthesia or general anesthesia:
- 50 mcg to 250 mcg by intravenous bolus administration. The most frequently reported initial bolus dose is 50 mcg or 100 mcg.
- 0.5 mcg/kg/min to 1.4 mcg/kg/min by intravenous continuous infusion, titrated to blood pressure goal. Do not exceed 200 mcg/min.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Exacerbation of Angina, Heart Failure, or Pulmonary Arterial Hypertension
Because of its pressor effects, phenylephrine hydrochloride can precipitate angina in patients with severe arteriosclerosis or history of angina, exacerbate underlying heart failure, and increase pulmonary arterial pressure.
5.2 Bradycardia
Phenylephrine hydrochloride can cause severe bradycardia and decreased cardiac output.
5.3 Risk in Patients with Autonomic Dysfunction
The pressor response to adrenergic drugs, including phenylephrine, can be increased in patients with autonomic dysfunction, as may occur with spinal cord injuries.
5.4 Skin and Subcutaneous Necrosis
Extravasation of phenylephrine can cause necrosis or sloughing of tissue. Avoid extravasation by checking infusion site for free flow.
5.5 Pressor Effect with Concomitant Oxytocic Drugs
Oxytocic drugs potentiate the pressor effect of sympathomimetic pressor amines including phenylephrine hydrochloride [see Drug Interactions (7.1)], with the potential for hemorrhagic stroke.
-
6 ADVERSE REACTIONS
The following adverse reactions associated with the use of phenylephrine hydrochloride were identified in the literature. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate their frequency reliably or to establish a causal relationship to drug exposure.
Cardiac disorders: Bradycardia, AV block, ventricular extrasystoles, myocardial ischemia
Gastrointestinal disorders: Nausea, vomiting
General disorders and administrative site conditions: Chest pain, extravasation
Nervous system disorders: Headache, nervousness, paresthesia, tremor
Psychiatric disorders: Excitability
Respiratory: Pulmonary edema, rales
Skin and subcutaneous tissue disorders: Diaphoresis, pallor, piloerection, skin blanching, skin necrosis with extravasation
Vascular disorders: Hypertensive crisis
-
7 DRUG INTERACTIONS
7.1 Agonists
The pressor effect of phenylephrine hydrochloride is increased in patients receiving:
- Monoamine oxidase inhibitors (MAOI), such as selegiline.
- Oxytocin and oxytocic drugs
- β-adrenergic blockers
- α-2 adrenergic agonists, such as clonidine
- Steroids
- Tricyclic antidepressants
- Norepinephrine transport inhibitors, such as atomoxetine
- Ergot alkaloids, such as methylergonovine maleate
- Centrally-acting sympatholytic agents, such as guanfacine or reserpine
- Atropine sulfate
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Data from randomized controlled trials and meta-analyses with phenylephrine hydrochloride injection use in pregnant women during caesarean section have not established a drug-associated risk of major birth defects and miscarriage. These studies have not identified an adverse effect on maternal outcomes or infant Apgar scores [see Data]. There are no data on the use of phenylephrine during the first or second trimester. In animal reproduction and development studies in normotensive animals, evidence of fetal malformations was noted when phenylephrine was administered during organogenesis via a 1-hour infusion at 1.2 times a human daily dose (HDD) of 10 mg/60 kg/day. Decreased pup weights were noted in offspring of pregnant rats treated with 2.9 times the HDD [See Data].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryofetal Risk
Untreated hypotension associated with spinal anesthesia for cesarean section is associated with an increase in maternal nausea and vomiting. A sustained decrease in uterine blood flow due to maternal hypotension may result in fetal bradycardia and acidosis.
Data
Human Data
Published randomized controlled trials over several decades, which compared the use of phenylephrine injection to other similar agents in pregnant women during cesarean section, have not identified adverse maternal or infant outcomes. At recommended doses, phenylephrine does not appear to affect fetal heart rate or fetal heart variability to a significant degree.
There are no studies on the safety of phenylephrine injection exposure during the period of organogenesis, and therefore, it is not possible to draw any conclusions on the risk of birth defects following exposure to phenylephrine injection during pregnancy. In addition, there are no data on the risk of miscarriage following fetal exposure to phenylephrine injection.
Animal Data
No clear malformations or fetal toxicity were reported when normotensive pregnant rabbits were treated with phenylephrine via continuous intravenous infusion over 1 hour (0.5 mg/kg/day; approximately equivalent to a HDD based on body surface area) from Gestation Day 7 to 19. At this dose, which demonstrated no maternal toxicity, there was evidence of developmental delay (altered ossification of sternebra).
In a non-GLP dose range-finding study in normotensive pregnant rabbits, fetal lethality and cranial, paw, and limb malformations were noted following treatment with 1.2 mg/kg/day of phenylephrine via continuous intravenous infusion over 1 hour (2.3-times the HDD). This dose was clearly maternally toxic (increased mortality and significant body weight loss). An increase in the incidence of limb malformation (hyperextension of the forepaw) coincident with high fetal mortality was noted in a single litter at 0.6 mg/kg/day (1.2-times the HDD) in the absence of maternal toxicity.
No malformations or embryo-fetal toxicity were reported when normotensive pregnant rats were treated with up to 3 mg/kg/day phenylephrine via continuous intravenous infusion over 1 hour (2.9-times the HDD) from Gestation Day 6 to 17. This dose was associated with some maternal toxicity (decreased food consumption and body weights).
Decreased pup weights were reported in a pre- and postnatal development toxicity study in which normotensive pregnant rats were administered phenylephrine via continuous intravenous infusion over 1 hour (0.3, 1.0, or 3.0 mg/kg/day; 0.29, 1, or 2.9 times the HDD) from Gestation Day 6 through Lactation Day 21). No adverse effects on growth and development (learning and memory, sexual development, and fertility) were noted in the offspring of pregnant rats at any dose tested. Maternal toxicities (mortality late in gestation and during lactation period, decreased food consumption and body weight) occurred at 1 and 3 mg/kg/day of phenylephrine (equivalent to and 2.9 times the HDD, respectively).
8.2 Lactation
Risk Summary
There are no data on the presence of Phenylephrine Hydrochloride Injection or its metabolite in human or animal milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for phenylephrine hydrochloride injection and any potential adverse effects on the breastfed infant from phenylephrine hydrochloride injection or from the underlying maternal condition.
8.5 Geriatric Use
Clinical studies of phenylephrine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
10 OVERDOSAGE
Overdose of Phenylephrine Hydrochloride Injection, 80 mcg/mL (20 mg/250 mL) can cause a rapid rise in blood pressure. Symptoms of overdose include headache, vomiting, hypertension, reflex bradycardia, and cardiac arrhythmias including ventricular extrasystoles and ventricular tachycardia, and may cause a sensation of fullness in the head and tingling of the extremities.
Consider using an α-adrenergic antagonist.
-
11 DESCRIPTION
Phenylephrine Hydrochloride in 0.9% Sodium Chloride Injection, 80 mcg/mL (20 mg/250 mL), an alpha-1 adrenergic receptor agonist, contains the active pharmaceutical ingredient phenylephrine in the form of hydrochloride salt. Phenylephrine is a synthetic sympathomimetic agent in sterile form for parenteral injection. Phenylephrine hydrochloride chemical name is (-)-m-Hydroxy-α-[(methylamino) methyl]benzyl alcohol hydrochloride and has the following structural formula:
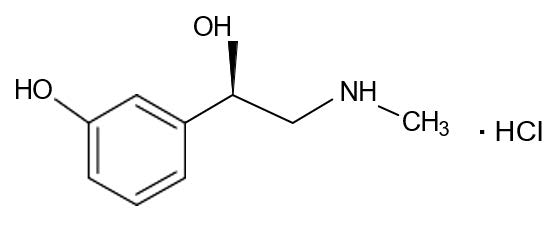
Phenylephrine hydrochloride is very soluble in water, freely soluble in ethanol, and insoluble in chloroform and ethyl ether. Phenylephrine hydrochloride is sensitive to light.
Phenylephrine Hydrochloride Injection, USP 80 mcg/mL (20 mg/250 mL, equivalent to 16.4 mg of phenylephrine base per 250 ml) is a clear and colorless sterile aqueous solution, essentially free of visible foreign matter. It is a ready-to-use solution intended for intravenous administration.
Each mL contains: 0.08 mg of Phenylephrine Hydrochloride and 9.04 mg of Sodium Chloride in Water for Injection. Phenylephrine Hydrochloride Injection, USP 80 mcg/mL. Hydrochloric acid is added as needed to adjust pH (pH range is 3.0 to 5.0).
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
Phenylephrine is the active moiety. Metabolites are inactive at both the α-1 and α-2 adrenergic receptors. Following parenteral administration of phenylephrine hydrochloride, increases in systolic blood pressure, diastolic blood pressure, mean arterial blood pressure, and total peripheral vascular resistance are observed. The onset of blood pressure increase following an intravenous bolus phenylephrine hydrochloride administration is rapid and the effect may persist for up to 20 minutes. As mean arterial pressure increases following parenteral doses, vagal activity also increases, resulting in reflex bradycardia.
Most vascular beds are constricted, including renal, splanchnic, and hepatic.
12.3 Pharmacokinetics
Following an intravenous infusion of phenylephrine hydrochloride, the effective half-life was approximately 5 minutes. The steady-state volume of distribution (340 L) exceeded the body volume by a factor of 5, suggesting a high distribution into certain organ compartments. The average total serum clearance (2095 mL/min) was close to one-third of the cardiac output.
A mass balance study showed that phenylephrine is extensively metabolized by the liver with only 12% of the dose excreted unchanged in the urine. Deamination by monoamino oxidase is the primary metabolic pathway resulting in the formation of the major metabolite (m-hydroxymandelic acid) which accounts for 57% of the total administered dose.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
Carcinogenesis:
Long-term animal studies that evaluated the carcinogenic potential of orally administered phenylephrine hydrochloride in F344/N rats and B6C3F1 mice were completed by the National Toxicology Program using the dietary route of administration. There was no evidence of carcinogenicity in mice administered approximately 270 mg/kg/day (131-times the human daily dose (HDD) of 10 mg/day based on body surface area) or rats administered approximately 50 mg/kg/day (48-times the HDD based on body surface area comparisons).
Mutagenesis:
Phenylephrine hydrochloride tested negative in the in vitro bacterial reverse mutation assay (S. typhimurium strains TA98, TA100, TA1535 and TA1537), the in vitro chromosomal aberrations assay, the in vitro sister chromatid exchange assay, and the in vivo rat micronucleus assay. Positive results were reported in only one of two replicates of the in vitro mouse lymphoma assay.
Impairment of Fertility:
No adverse effects on fertility or early embryonic development were noted when phenylephrine hydrochloride was administered at doses of 50 mcg, 100 mcg, or 200 mcg/kg/day (up to 0.2 times HDD of 10 mg/60 kg/day based on body surface area) via single daily bolus injection for 28 days prior to mating to male rats or for 14 days prior to mating through Gestation Day 7 to female rats.
-
14 CLINICAL STUDIES
Increases in systolic and mean blood pressure following administration of phenylephrine were observed in 42 literature-based studies in the perioperative setting, including 26 studies where phenylephrine was used in lowrisk (ASA 1 and 2) pregnant women undergoing neuraxial anesthesia during cesarean delivery, 3 studies in non-obstetric surgery under neuraxial anesthesia, and 13 studies in patients undergoing surgery under general anesthesia.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Phenylephrine Hydrochloride in 0.9% Sodium Chloride Injection is a clear, colorless solution supplied in a readyto- use single dose 250 mL infusion bag as follows:
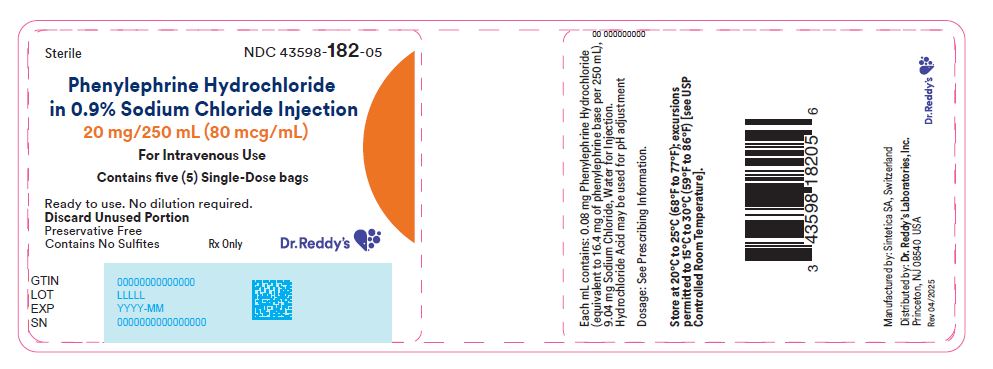
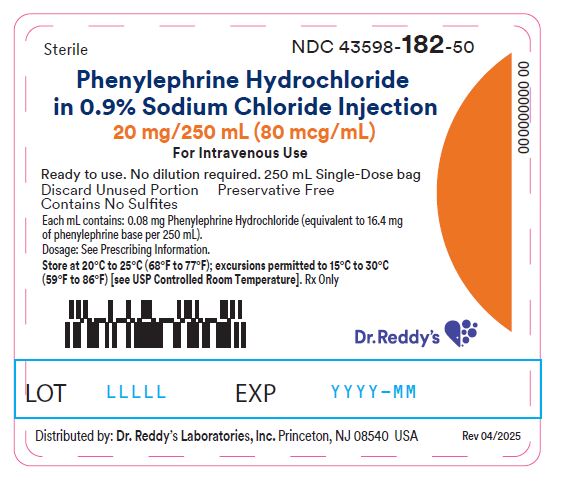
Unit of Sale Strength Each NDC: 43598-182-05
Pack of 5 intravenous solution bags in a
cardboard box
(20 mg/250 mL)80 mcg/mL NDC: 43598-182-50
250 mL intravenous solution bagStore at 20°C to 25°C (68°F to 77°F), excursions permitted to 15°C to 30°C (59°F to 86°F) [See USP Controlled Room Temperature].
Discard any unused portion.
- SPL UNCLASSIFIED SECTION
- Principle Display Panel
-
INGREDIENTS AND APPEARANCE
PHENYLEPHRINE HYDROCHLORIDE INJECTION, SOLUTION
phenylephrine hydrochloride injection, solution injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 43598-182 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHENYLEPHRINE (UNII: 1WS297W6MV) (PHENYLEPHRINE - UNII:1WS297W6MV) PHENYLEPHRINE 80 ug in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) NITROGEN (UNII: N762921K75) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 43598-182-05 5 in 1 CARTON 07/01/2025 1 NDC: 43598-182-50 250 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA216830 07/01/2025 Labeler - Dr. Reddy's Laboratories Inc. (802315887)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.