Metronidazole by Major Pharmaceuticals METRONIDAZOLE tablet
Metronidazole by
Drug Labeling and Warnings
Metronidazole by is a Prescription medication manufactured, distributed, or labeled by Major Pharmaceuticals. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
BOXED WARNING
(What is this?)
WARNING
Metronidazole has been shown to be carcinogenic in mice and rats (See PRECAUTIONS). Unnecessary use of the drug should be avoided. Its use should be reserved for the conditions described in the INDICATIONS AND USAGE section below. -
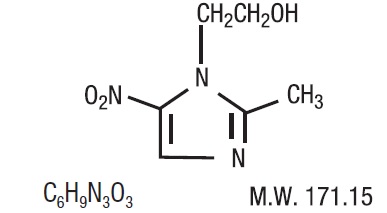
DESCRIPTION
Metronidazole tablets, USP 250 mg or 500 mg is an oral formulation of the synthetic nitroimidazole antimicrobial, 2-methyl-5-nitro-1H-imidazole-1-ethanol, which has the following structural formula:
Metronidazole tablets, USP contain 250 mg or 500 mg of metronidazole, USP. Inactive ingredients include colloidal silicon dioxide, crospovidone, hydrogenated vegetable oil and silicified microcrystalline cellulose.
FDA approved dissolution specifications differs from the USP.
-
CLINICAL PHARMACOLOGY
Absorption
Disposition of metronidazole in the body is similar for both oral and intravenous dosage forms. Following oral administration, metronidazole is well absorbed, with peak plasma concentrations occurring between one and two hours after administration.
Plasma concentrations of metronidazole are proportional to the administered dose. Oral administration of 250 mg, 500 mg, or 2,000 mg produced peak plasma concentrations of 6 mcg/mL, 12 mcg/mL, and 40 mcg/mL, respectively. Studies reveal no significant bioavailability differences between males and females; however, because of weight differences, the resulting plasma levels in males are generally lower.
Distribution
Metronidazole is the major component appearing in the plasma, with lesser quantities of metabolites also being present. Less than 20% of the circulating metronidazole is bound to plasma proteins. Metronidazole appears in cerebrospinal fluid, saliva, and breast milk in concentrations similar to those found in plasma. Bactericidal concentrations of metronidazole have also been detected in pus from hepatic abscesses.
Metabolism/Excretion
The major route of elimination of metronidazole and its metabolites is via the urine (60% to 80% of the dose), with fecal excretion accounting for 6% to 15% of the dose. The metabolites that appear in the urine result primarily from side-chain oxidation [1-(ß-hydroxyethyl)- 2-hydroxymethyl-5-nitroimidazole and 2-methyl-5-nitroimidazole-1-yl-acetic acid] and glucuronide conjugation, with unchanged metronidazole accounting for approximately 20% of the total. Both the parent compound and the hydroxyl metabolite possess in vitro antimicrobial activity.
Renal clearance of metronidazole is approximately 10 mL/min/1.73 m2. The average elimination half-life of metronidazole in healthy subjects is eight hours.
Renal Impairment
Decreased renal function does not alter the single-dose pharmacokinetics of metronidazole.
Subjects with end-stage renal disease (ESRD; CLCR= 8.1±9.1 mL/min) and who received a single intravenous infusion of metronidazole 500 mg had no significant change in metronidazole pharmacokinetics but had 2-fold higher Cmax of hydroxy-metronidazole and 5-fold higher Cmax of metronidazole acetate, compared to healthy subjects with normal renal function (CLCR= 126±16 mL/min). Thus, on account of the potential accumulation of metronidazole metabolites in ESRD patients, monitoring for metronidazole associated adverse events is recommended (see PRECAUTIONS).
Effect of Dialysis
Following a single intravenous infusion or oral dose of metronidazole 500 mg, the clearance of metronidazole was investigated in ESRD subjects undergoing hemodialysis or continuous ambulatory peritoneal dialysis (CAPD). A hemodialysis session lasting for 4 to 8 hours removed 40% to 65% of the administered metronidazole dose, depending on the type of dialyzer membrane used and the duration of the dialysis session. If the administration of metronidazole cannot be separated from the dialysis session, supplementation of metronidazole dose following hemodialysis should be considered (see DOSAGE AND ADMINISTRATION). A peritoneal dialysis session lasting for 7.5 hours removed approximately 10% of the administered metronidazole dose. No adjustment in metronidazole dose is needed in ESRD patients undergoing CAPD.
Hepatic Impairment
Following a single intravenous infusion of 500 mg metronidazole, the mean AUC24 of metronidazole was higher by 114% in patients with severe (Child-Pugh C) hepatic impairment, and by 54% and 53% in patients with mild (Child-Pugh A) and moderate (Child-Pugh B) hepatic impairment, respectively, compared to healthy control subjects. There were no significant changes in the AUC24 of hydroxyl-metronidazole in these hepatically impaired patients. A reduction in metronidazole dosage by 50% is recommended in patients with severe (Child- Pugh C) hepatic impairment (see DOSAGE AND ADMINISTRATION). No dosage adjustment is needed for patients with mild to moderate hepatic impairment. Patients with mild to moderate hepatic impairment should be monitored for metronidazole associated adverse events (see PRECAUTIONS and DOSAGE AND ADMINISTRATION).
Geriatric Patients
Following a single 500 mg oral or IV dose of metronidazole, subjects >70 years old with no apparent renal or hepatic dysfunction had a 40% to 80% higher mean AUC of hydroxy-metronidazole (active metabolite), with no apparent increase in the mean AUC of metronidazole (parent compound), compared to young healthy controls <40 years old. In geriatric patients, monitoring for metronidazole associated adverse events is recommended (see PRECAUTIONS).
Pediatric Patients
In one study, newborn infants appeared to demonstrate diminished capacity to eliminate metronidazole. The elimination half-life, measured during the first 3 days of life, was inversely related to gestational age. In infants whose gestational ages were between 28 and 40 weeks, the corresponding elimination half-lives ranged from 109 to 22.5 hours.
-
Microbiology
Mechanism of Action
Metronidazole, a nitroimidazole, exerts antibacterial effects in an anaerobic environment against most obligate anaerobes. Once metronidazole enters the organism by passive diffusion and activated in the cytoplasm of susceptible anaerobic bacteria, it is reduced; this process includes intracellular electron transport proteins such as ferredoxin, transfer of an electron to the nitro group of the metronidazole, and formation of a short-lived nitroso free radical. Because of this alteration of the metronidazole molecule, a concentration gradient is created and maintained which promotes the drug’s intracellular transport. The reduced form of metronidazole and free radicals can interact with DNA leading to inhibition of DNA synthesis and DNA degradation leading to death of the bacteria. The precise mechanism of action of metronidazole is unclear.
Resistance
A potential for development of resistance exists against metronidazole.
Resistance may be due to multiple mechanisms that include decreased uptake of the drug, altered reduction efficiency, overexpression of the efflux pumps, inactivation of the drug, and/ or increased DNA damage repair.
Metronidazole does not possess any clinically relevant activity against facultative anaerobes or obligate aerobes.
Antimicrobial Activity
Metronidazole has been shown to be active against most isolates of the following bacteria both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Gram-positive anaerobes
Clostridium species
Eubacterium species
Peptococcus species
Peptostreptococcus speciesGram-negative anaerobes
Bacteroides fragilis group (B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B.vulgatus)
Fusobacterium speciesProtozoal parasites
Entamoeba histolytica
Trichomonas vaginalisThe following in vitro data are available, but their clinical significance is unknown:
Metronidazole exhibits in vitro minimal inhibitory concentrations (MIC’s) of 8 mcg/mL or less against most (≥ 90%) isolates of the following bacteria; however, the safety and effectiveness of metronidazole in treating clinical infections due to these bacteria have not been established in adequate and well-controlled clinical trials.
Gram-negative anaerobes
Bacteroides fragilis group (B. caccae, B. uniformis)
Prevotella species (P. bivia, P. buccae, P. disiens)Susceptibility Testing
For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
-
INDICATIONS AND USAGE
Symptomatic Trichomoniasis. Metronidazole tablets are indicated for the treatment of T. vaginalis infection in females and males when the presence of the trichomonad has been confirmed by appropriate laboratory procedures (wet smears and/or cultures).
Asymptomatic Trichomoniasis. Metronidazole tablets are indicated in the treatment of asymptomatic T. vaginalis infection in females when the organism is associated with endocervicitis, cervicitis, or cervical erosion. Since there is evidence that presence of the trichomonad can interfere with accurate assessment of abnormal cytological smears, additional smears should be performed after eradication of the parasite.
Treatment of Asymptomatic Sexual Partners. T. vaginalis infection is a venereal disease. Therefore, asymptomatic sexual partners of treated patients should be treated simultaneously if the organism has been found to be present, in order to prevent reinfection of the partner. The decision as to whether to treat an asymptomatic male partner who has a negative culture or one for whom no culture has been attempted is an individual one. In making this decision, it should be noted that there is evidence that a woman may become reinfected if her sexual partner is not treated. Also, since there can be considerable difficulty in isolating the organism from the asymptomatic male carrier, negative smears and cultures cannot be relied upon in this regard. In any event, the sexual partner should be treated with metronidazole tablets in cases of reinfection.
Amebiasis. Metronidazole tablets are indicated in the treatment of acute intestinal amebiasis (amebic dysentery) and amebic liver abscess.
In amebic liver abscess, metronidazole tablet therapy does not obviate the need for aspiration or drainage of pus.
Anaerobic Bacterial Infections. Metronidazole tablets are indicated in the treatment of serious infections caused by susceptible anaerobic bacteria. Indicated surgical procedures should be performed in conjunction with metronidazole tablet therapy. In a mixed aerobic and anaerobic infection, antimicrobials appropriate for the treatment of the aerobic infection should be used in addition to metronidazole tablets.
INTRA-ABDOMINAL INFECTIONS, including peritonitis, intra-abdominal abscess, and liver abscess, caused by Bacteroides species including the B. fragilis group (B. fragilis, B. distasonis, B. ovatus, B. thetaiotaomicron, B. vulgatus), Clostridium species, Eubacterium species, Peptococcus species, and Peptostreptococcus species.
SKIN AND SKIN STRUCTURE INFECTIONS caused by Bacteroides species including the B. fragilis group, Clostridium species, Peptococcus species, Peptostreptococcus species, and Fusobacterium species.
GYNECOLOGIC INFECTIONS, including endometritis, endomyometritis, tubo-ovarian abscess, and postsurgical vaginal cuff infection, caused by Bacteroides species including the B. fragilis group, Clostridium species, Peptococcus species, Peptostreptococcus species, and Fusobacterium species.
BACTERIAL SEPTICEMIA caused by Bacteroides species including the B. fragilis group and Clostridium species.
BONE AND JOINT INFECTIONS, (as adjunctive therapy), caused by Bacteroides species including the B. fragilis group.
CENTRAL NERVOUS SYSTEM (CNS) INFECTIONS, including meningitis and brain abscess, caused by Bacteroides species including the B. fragilis group.
LOWER RESPIRATORY TRACT INFECTIONS, including pneumonia, empyema, and lung abscess, caused by Bacteroides species including the B. fragilis group.
ENDOCARDITIS caused by Bacteroides species including the B. fragilis group.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of metronidazole and other antibacterial drugs, metronidazole tablets should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
-
CONTRAINDICATIONS
Hypersensitivity
Metronidazole tablets are contraindicated in patients with a prior history of hypersensitivity to metronidazole or other nitroimidazole derivatives.
In patients with trichomoniasis, metronidazole tablets are contraindicated during the first trimester of pregnancy (see PRECAUTIONS).
Psychotic Reaction with Disulfiram
Use of oral metronidazole is associated with psychotic reactions in alcoholic patients who were using disulfiram concurrently. Do not administer metronidazole to patients who have taken disulfiram within the last two weeks (see PRECAUTIONS, Drug Interactions).
Interaction with Alcohol
Use of oral metronidazole is associated with a disulfiram-like reaction to alcohol, including abdominal cramps, nausea, vomiting, headaches, and flushing. Discontinue consumption of alcohol or products containing propylene glycol during and for at least three days after therapy with metronidazole (see PRECAUTIONS, Drug Interactions).
Cockayne Syndrome
Metronidazole Tablets are contraindicated in patients with Cockayne syndrome. Severe irreversible hepatotoxicity/acute liver failure with fatal outcomes have been reported after initiation of metronidazole in patients with Cockayne syndrome (see ADVERSE REACTIONS). -
WARNINGS
Hypersensitivity Reactions
Hypersensitivity reactions including severe cutaneous adverse reactions (SCARs) can be serious and potentially life threatening (seeADVERSE REACTIONS).
Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions (SCARs) including toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been reported with the use of metronidazole. Symptoms can be serious and potentially life threatening. If symptoms or signs of SCARs develop, discontinue metronidazole immediately and institute appropriate therapy.
Central and Peripheral Nervous System Effects
Encephalopathy and peripheral neuropathy: Cases of encephalopathy and peripheral neuropathy (including optic neuropathy) have been reported with metronidazole.
Encephalopathy has been reported in association with cerebellar toxicity characterized by ataxia, dizziness, and dysarthria. CNS lesions seen on MRI have been described in reports of encephalopathy. CNS symptoms are generally reversible within days to weeks upon discontinuation of metronidazole. CNS lesions seen on MRI have also been described as reversible.
Peripheral neuropathy, mainly of sensory type has been reported and is characterized by numbness or paresthesia of an extremity.
Convulsive seizures have been reported in patients treated with metronidazole.
Aseptic meningitis: Cases of aseptic meningitis have been reported with metronidazole. Symptoms can occur within hours of dose administration and generally resolve after metronidazole therapy is discontinued.
The appearance of abnormal neurologic signs and symptoms demands the prompt evaluation of the benefit/risk ratio of the continuation of therapy (see ADVERSE REACTIONS).
-
PRECAUTIONS
General
Hepatic Impairment
Patients with hepatic impairment metabolize metronidazole slowly, with resultant accumulation of metronidazole in the plasma. For patients with severe hepatic impairment (Child-Pugh C), a reduced dose of metronidazole is recommended. For patients with mild to moderate hepatic impairment, no dosage adjustment is needed but these patients should be monitored for metronidazole associated adverse events (seeCLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
Renal Impairment
Patients with end-stage renal disease may excrete metronidazole and metabolites slowly in the urine, resulting in significant accumulation of metronidazole metabolites. Monitoring for metronidazole associated adverse events is recommended (see CLINICAL PHARMACOLOGY).
Fungal Superinfections
Known or previously unrecognized candidiasis may present more prominent symptoms during therapy with metronidazole and requires treatment with a candidacidal agent.
Use in Patients with Blood Dyscrasias
Metronidazole is a nitroimidazole and should be used with caution in patients with evidence of or history of blood dyscrasia. A mild leukopenia has been observed during its administration; however, no persistent hematologic abnormalities attributable to metronidazole have been observed in clinical studies. Total and differential leukocyte counts are recommended before and after therapy.
Drug-Resistant Bacteria and Parasites
Prescribing metronidazole in the absence of a proven or strongly suspected bacterial or parasitic infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria and parasites.
Information for Patients
Interaction with Alcohol
Discontinue consumption of alcoholic beverages or products containing propylene glycol while taking metronidazole and for at least three days afterward because abdominal cramps, nausea, vomiting, headaches, and flushing may occur (see CONTRAINDICATIONS and PRECAUTIONS,Drug Interactions).
Treatment of Bacterial and Parasitic Infections
Patients should be counseled that metronidazole should only be used to treat bacterial and parasitic infections. Metronidazole does not treat viral infections (e.g., the common cold). When metronidazole is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by metronidazole in the future.
Severe Cutaneous Adverse Reactions
Advise patients that metronidazole may increase the risk of serious and sometimes fatal dermatologic reactions, including TEN, SJS and DRESS. Instruct the patient to be alert for skin rash, blisters, fever or other signs and symptoms of these hypersensitivity reactions. Advise patients to stop metronidazole tablets immediately if they develop any type of rash and seek medical attention.
Drug Interactions
Disulfiram
Psychotic reactions have been reported in alcoholic patients who are using metronidazole and disulfiram concurrently. Metronidazole should not be given to patients who have taken disulfiram within the last two weeks (see CONTRAINDICATIONS).
Alcoholic Beverages
Abdominal cramps, nausea, vomiting, headaches, and flushing may occur if alcoholic beverages or products containing propylene glycol are consumed during or following metronidazole therapy (see CONTRAINDICATIONS).
Warfarin and other Oral Anticoagulants
Metronidazole has been reported to potentiate the anticoagulant effect of warfarin and other oral coumarin anticoagulants, resulting in a prolongation of prothrombin time. When metronidazole is prescribed for patients on this type of anticoagulant therapy, prothrombin time and INR should be carefully monitored.
Lithium
In patients stabilized on relatively high doses of lithium, short-term metronidazole therapy has been associated with elevation of serum lithium and, in a few cases, signs of lithium toxicity. Serum lithium and serum creatinine levels should be obtained several days after beginning metronidazole to detect any increase that may precede clinical symptoms of lithium intoxication.
Busulfan
Metronidazole has been reported to increase plasma concentrations of busulfan, which can result in an increased risk for serious busulfan toxicity. Metronidazole should not be administered concomitantly with busulfan unless the benefit outweighs the risk. If no therapeutic alternatives to metronidazole are available, and concomitant administration with busulfan is medically needed, frequent monitoring of busulfan plasma concentration should be performed and the busulfan dose should be adjusted accordingly.
Drugs that Inhibit CYP450 Enzymes
The simultaneous administration of drugs that decrease microsomal liver enzyme activity, such as cimetidine, may prolong the half-life and decrease plasma clearance of metronidazole.
Drug/Laboratory Test Interactions
Metronidazole may interfere with certain types of determinations of serum chemistry values, such as aspartate aminotransferase (AST, SGOT), alanine aminotransferase (ALT, SGPT), lactate dehydrogenase (LDH), triglycerides, and glucose hexokinase. Values of zero may be observed. All of the assays in which interference has been reported involve enzymatic coupling of the assay to oxidation-reduction of nicotinamide adenine dinucleotide (NAD+
 NADH). Interference is due to the similarity in absorbance peaks of NADH (340 nm) and metronidazole (322 nm) at pH 7.
NADH). Interference is due to the similarity in absorbance peaks of NADH (340 nm) and metronidazole (322 nm) at pH 7.Carcinogenesis, Mutagenesis, Impairment of Fertility
Tumors affecting the liver, lungs, mammary, and lymphatic tissues have been detected in several studies of metronidazole in rats and mice, but not hamsters.
Pulmonary tumors have been observed in all six reported studies in the mouse, including one study in which the animals were dosed on an intermittent schedule (administration during every fourth week only). Malignant liver tumors were increased in male mice treated at approximately 1,500 mg/m2 (similar to the maximum recommended daily dose, based on body surface area comparisons). Malignant lymphomas and pulmonary neoplasms were also increased with lifetime feeding of the drug to mice. Mammary and hepatic tumors were increased among female rats administered oral metronidazole compared to concurrent controls. Two lifetime tumorigenicity studies in hamsters have been performed and reported to be negative.
Metronidazole has shown mutagenic activity in in vitro assay systems including the Ames test. Studies in mammals in vivo have failed to demonstrate a potential for genetic damage.
Metronidazole failed to produce any adverse effects on fertility or testicular function in male rats at doses up at 400 mg/kg/day (similar to the maximum recommended clinical dose, based on body surface area comparisons) for 28 days. However, rats treated at the same dose for 6 weeks or longer were infertile and showed severe degeneration of the seminiferous epithelium in the testes as well as marked decreases in testicular spermatid counts and epididymal sperm counts. Fertility was restored in most rats after an eight week, drug-free recovery period.
Pregnancy
Teratogenic Effects:
There are no adequate and well controlled studies of metronidazole in pregnant women. There are published data from case-control studies, cohort studies, and 2 meta-analyses that include more than 5,000 pregnant women who used metronidazole during pregnancy. Many studies included first trimester exposures. One study showed an increased risk of cleft lip, with or without cleft palate, in infants exposed to metronidazole in-utero; however, these findings were not confirmed. In addition, more than ten randomized placebo-controlled clinical trials enrolled more than 5,000 pregnant women to assess the use of antibiotic treatment (including metronidazole) for bacterial vaginosis on the incidence of preterm delivery. Most studies did not show an increased risk for congenital anomalies or other adverse fetal outcomes following metronidazole exposure during pregnancy. Three studies conducted to assess the risk of infant cancer following metronidazole exposure during pregnancy did not show an increased risk; however, the ability of these studies to detect such a signal was limited.
Metronidazole crosses the placental barrier and its effects on the human fetal organogenesis are not known. Reproduction studies have been performed in rats, rabbits, and mice at doses similar to the maximum recommended human dose based on body surface area comparisons.
There was no evidence of harm to the fetus due to metronidazole.Nursing Mothers
Metronidazole is present in human milk at concentrations similar to maternal serum levels, and infant serum levels can be close to or comparable to infant therapeutic levels. There are no data on the effects of metronidazole on milk production. Animal studies have shown the potential for tumorigenicity after oral metronidazole was administered chronically to rats and mice (see PRECAUTIONS, Carcinogenesis, Mutagenesis,
Impairment of Fertility). This drug is not intended to be administered chronically; therefore, the clinical relevance of the findings of the animal studies is unclear. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for metronidazole and any potential adverse effects on the breastfed infant from metronidazole or from the underlying maternal condition. Alternatively, a nursing mother may choose to pump and discard human milk for the duration of metronidazole therapy, and for 48 hours after the last dose and feed her infant stored human milk or formula.Geriatric Use
In elderly geriatric patients, monitoring for metronidazole associated adverse events is recommended (see CLINICAL PHARMACOLOGY,PRECAUTIONS). Decreased liver function in geriatric patients can result in increased concentrations of metronidazole that may necessitate adjustment of metronidazole dosage (see DOSAGE AND ADMINISTRATION).
-
ADVERSE REACTIONS
The following reactions have been reported during treatment with metronidazole:
Central Nervous System: The most serious adverse reactions reported in patients treated with metronidazole have been convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity. Since persistent peripheral neuropathy has been reported in some patients receiving prolonged administration of metronidazole, patients should be specifically warned about these reactions and should be told to stop the drug and report immediately to their physicians if any neurologic symptoms occur. In addition, patients have reported headache, syncope, dizziness, vertigo, incoordination, ataxia, tinnitus, hearing impairment, hearing loss, confusion, dysarthria, irritability, depression, weakness, and insomnia (see WARNINGS).
Gastrointestinal: The most common adverse reactions reported have been referable to the gastrointestinal tract, particularly nausea, sometimes accompanied by headache, anorexia, and occasionally vomiting; diarrhea; epigastric distress; and abdominal cramping and constipation.
Mouth: A sharp, unpleasant metallic taste is not unusual. Furry tongue, glossitis, and stomatitis have occurred; these may be associated with a sudden overgrowth of Candida which may occur during therapy.
Dermatologic: Dermatitis bullous, fixed drug eruption, erythematous rash and pruritus.
Hematopoietic: Reversible neutropenia (leukopenia); rarely, reversible thrombocytopenia.
Cardiovascular: QT prolongation has been reported, particularly when metronidazole was administered with drugs with the potential for prolonging the QT interval. Flattening of the T-wave may be seen in electrocardiographic tracings.
Hypersensitivity: Toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP) (see WARNINGS), urticaria, erythematous rash, flushing, nasal congestion, dryness of the mouth (or vagina or vulva), and fever.
Renal: Dysuria, cystitis, polyuria, incontinence, and a sense of pelvic pressure. Instances of darkened urine have been reported by approximately one patient in 100,000. Although the pigment which is probably responsible for this phenomenon has not been positively identified, it is almost certainly a metabolite of metronidazole and seems to have no clinical significance.
Hepatic: Cases of severe irreversible hepatotoxicity/acute liver failure, including cases with fatal outcomes with very rapid onset after initiation of systemic use of metronidazole, have been reported in patients with Cockayne syndrome (latency from drug start to signs of liver failure as short as 2 days) (seeCONTRAINDICATIONS).
Other: Proliferation of Candida in the vagina, dyspareunia, decrease of libido, proctitis, and fleeting joint pains sometimes resembling “serum sickness.” Rare cases of pancreatitis, which generally abated on withdrawal of the drug, have been reported.
Patients with Crohn’s disease are known to have an increased incidence of gastrointestinal and certain extraintestinal cancers. There have been some reports in the medical literature of breast and colon cancer in Crohn’s disease patients who have been treated with metronidazole at high doses for extended periods of time. A cause and effect relationship has not been established. Crohn’s disease is not an approved indication for metronidazole tablets.
To report SUSPECTED ADVERSE REACTIONS, contact Avet Pharmaceuticals Inc. at 1-866-901-DRUG (3784) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch -
OVERDOSAGE
Single oral doses of metronidazole, up to 15 g, have been reported in suicide attempts and accidental overdoses. Symptoms reported include nausea, vomiting, and ataxia.
Oral metronidazole has been studied as a radiation sensitizer in the treatment of malignant tumors. Neurotoxic effects, including seizures and peripheral neuropathy, have been reported after 5 to 7 days of doses of 6 to 10.4 g every other day.
Treatment of Overdosage: There is no specific antidote for metronidazole overdose; therefore, management of the patient should consist of symptomatic and supportive therapy.
-
DOSAGE AND ADMINISTRATION
Trichomoniasis:
In the Female:
One-day treatment − two grams of metronidazole tablets, given either as a single dose or in two divided doses of one gram each, given in the same day.Seven-day course of treatment - 250 mg three times daily for seven consecutive days. There is some indication from controlled comparative studies that cure rates as determined by vaginal smears and signs and symptoms, may be higher after a seven-day course of treatment than after a one-day treatment regimen.
The dosage regimen should be individualized. Single-dose treatment can assure compliance, especially if administered under supervision, in those patients who cannot be relied on to continue the seven-day regimen. A seven-day course of treatment may minimize reinfection by protecting the patient long enough for the sexual contacts to obtain appropriate treatment. Further, some patients may tolerate one treatment regimen better than the other.
Pregnant patients should not be treated during the first trimester (see CONTRAINDICATIONS). In pregnant patients for whom alternative treatment has been inadequate, the one-day course of therapy should not be used, as it results in higher serum levels which can reach the fetal circulation (seePRECAUTIONS,Pregnancy).
When repeat courses of the drug are required, it is recommended that an interval of four to six weeks elapse between courses and that the presence of the trichomonad be reconfirmed by appropriate laboratory measures. Total and differential leukocyte counts should be made before and after re-treatment.
In the Male: Treatment should be individualized as it is for the female.
Amebiasis
Adults:
For acute intestinal amebiasis (acute amebic dysentery):750 mg orally three times daily for 5 to 10 days.For amebic liver abscess: 500 mg or 750 mg orally three times daily for 5 to 10 days.
Pediatric patients: 35 to 50 mg/kg/24 hours, divided into three doses, orally for 10 days.
Anaerobic Bacterial Infections
In the treatment of most serious anaerobic infections, intravenous metronidazole is usually administered initially.
The usual adult oral dosage is 7.5 mg/kg every six hours (approx. 500 mg for a 70-kg adult). A maximum of 4 g should not be exceeded during a 24-hour period.
The usual duration of therapy is 7 to 10 days; however, infections of the bone and joint, lower respiratory tract, and endocardium may require longer treatment.
Dosage Adjustments
Patients with Severe Hepatic Impairment
For patients with severe hepatic impairment (Child-Pugh C), the dose of metronidazole tablets should be reduced by 50% (see CLINICAL PHARMACOLOGYand PRECAUTIONS).
Patients Undergoing Hemodialysis:
Hemodialysis removes significant amounts of metronidazole and its metabolites from systemic circulation. The clearance of metronidazole will depend on the type of dialysis membrane used, the duration of the dialysis session, and other factors. If the administration of metronidazole cannot be separated from the hemodialysis session, supplementation of metronidazole dosage following the hemodialysis session should be considered, depending on the patient’s clinical situation (see CLINICAL PHARMACOLOGY).
-
HOW SUPPLIED
Metronidazole tablets, USP 250 mg are white to off-white, round shaped tablets debossed with “MCR 104” on one side and plain on other side.
Cartons of 100 tablets (10 tablets per blister pack x 10), NDC: 0904-7156-61
Metronidazole tablets, USP 500 mg are white to off-white, oval shaped tablets debossed with “MCR 105” on one side and plain on other side.
Cartons of 100 tablets (10 tablets per blister pack x 10), NDC: 0904-7126-61
-
STORAGE AND HANDLING
Storage and Stability: Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
Protect from light.
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).Distributed by:
Avet Pharmaceuticals Inc.
East Brunswick, NJ 08816, USA.1-866-901-DRUG (3784)
Packaged and Distributed by:
MAJOR® PHARMACEUTICALS
Indianapolis, IN 46268 USA
Refer to package label for Distributor's NDC Number
Revised: 07/2024 200192
- Package/Label Display Panel
- Package/Label Display Panel
-
INGREDIENTS AND APPEARANCE
METRONIDAZOLE
metronidazole tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0904-7156(NDC:23155-651) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METRONIDAZOLE (UNII: 140QMO216E) (METRONIDAZOLE - UNII:140QMO216E) METRONIDAZOLE 250 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE, UNSPECIFIED (UNII: 2S7830E561) COTTONSEED OIL (UNII: H3E878020N) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color WHITE (White to Off-White) Score no score Shape ROUND Size 9mm Flavor Imprint Code MCR;104 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0904-7156-61 100 in 1 CARTON 11/29/2017 1 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205245 11/29/2017 METRONIDAZOLE
metronidazole tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0904-7126(NDC:23155-652) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METRONIDAZOLE (UNII: 140QMO216E) (METRONIDAZOLE - UNII:140QMO216E) METRONIDAZOLE 500 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) CROSPOVIDONE, UNSPECIFIED (UNII: 2S7830E561) COTTONSEED OIL (UNII: H3E878020N) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) Product Characteristics Color WHITE (White to Off-White) Score no score Shape OVAL (Oval) Size 16mm Flavor Imprint Code MCR;105 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0904-7126-61 100 in 1 CARTON 11/29/2017 1 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205245 11/29/2017 Labeler - Major Pharmaceuticals (191427277)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.