VEMLIDY- tenofovir alafenamide tablet
VEMLIDY by
Drug Labeling and Warnings
VEMLIDY by is a Prescription medication manufactured, distributed, or labeled by Gilead Sciences, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use VEMLIDY safely and effectively. See full prescribing information for VEMLIDY.
VEMLIDY® (tenofovir alafenamide) tablets, for oral use
Initial U.S. Approval: 2015WARNING: POSTTREATMENT SEVERE ACUTE EXACERBATION OF HEPATITIS B
See full prescribing information for complete boxed warning.
Discontinuation of anti-hepatitis B therapy may result in severe acute exacerbations of hepatitis B. Hepatic function should be monitored closely in patients who discontinue VEMLIDY. If appropriate, resumption of anti-hepatitis B therapy may be warranted. (5.1)
RECENT MAJOR CHANGES
Dosage and Administration Dosage in Patients with Renal Impairment (2.3) 02/2019 INDICATIONS AND USAGE
VEMLIDY is a hepatitis B virus (HBV) nucleoside analog reverse transcriptase inhibitor and is indicated for the treatment of chronic hepatitis B virus infection in adults with compensated liver disease. (1)
DOSAGE AND ADMINISTRATION
- Testing: Prior to initiation of VEMLIDY, test patients for HIV infection. VEMLIDY alone should not be used in patients with HIV infection. Prior to or when initiating VEMLIDY, and during treatment on a clinically appropriate schedule, assess serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients. Also assess serum phosphorus in patients with chronic kidney disease. (2.1)
- Recommended dosage: 25 mg (one tablet) taken orally once daily with food. (2.2)
- Renal Impairment: VEMLIDY is not recommended in patients with estimated creatinine clearance below 15 mL per minute who are not receiving chronic hemodialysis. In patients on chronic hemodialysis, on hemodialysis days, administer VEMLIDY after hemodialysis. (2.3)
- Hepatic Impairment: VEMLIDY is not recommended in patients with decompensated (Child-Pugh B or C) hepatic impairment. (2.4)
DOSAGE FORMS AND STRENGTHS
Tablets: 25 mg of tenofovir alafenamide. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- HBV and HIV-1 coinfection: VEMLIDY alone is not recommended for the treatment of HIV-1 infection. HIV-1 resistance may develop in these patients. (5.2)
- New onset or worsening renal impairment: Prior to or when initiating VEMLIDY, and during treatment on a clinically appropriate schedule, assess serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients. Also assess serum phosphorus in patients with chronic kidney disease. (5.3)
- Lactic acidosis/severe hepatomegaly with steatosis: Discontinue treatment in patients who develop symptoms or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity. (5.4)
ADVERSE REACTIONS
Most common adverse reaction (incidence greater than or equal to 10%, all grades) is headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Gilead Sciences, Inc. at 1-800-GILEAD-5 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
VEMLIDY is a substrate of P-glycoprotein (P-gp) and BCRP. Drugs that strongly affect P-gp and BCRP activity may lead to changes in VEMLIDY absorption. Consult the full prescribing information prior to and during treatment for potential drug-drug interactions. (7)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 2/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: POSTTREATMENT SEVERE ACUTE EXACERBATION OF HEPATITIS B
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Testing Prior to Initiation of VEMLIDY
2.2 Recommended Dosage in Adults
2.3 Dosage in Patients with Renal Impairment
2.4 Dosage in Patients with Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Severe Acute Exacerbation of Hepatitis B after Discontinuation of Treatment
5.2 Risk of Development of HIV-1 Resistance in Patients Coinfected with HBV and HIV-1
5.3 New Onset or Worsening Renal Impairment
5.4 Lactic Acidosis/Severe Hepatomegaly with Steatosis
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect VEMLIDY
7.2 Drugs Affecting Renal Function
7.3 Established and Other Potentially Significant Interactions
7.4 Drugs without Clinically Significant Interactions with VEMLIDY
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Description of Clinical Trials
14.2 Clinical Trials in Adults with Chronic Hepatitis B Virus Infection and Compensated Liver Disease
14.3 Clinical Trials in Virologically Suppressed Adults with Chronic Hepatitis B Virus Infection Who Switched to VEMLIDY
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: POSTTREATMENT SEVERE ACUTE EXACERBATION OF HEPATITIS B
Discontinuation of anti-hepatitis B therapy, including VEMLIDY, may result in severe acute exacerbations of hepatitis B. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue anti-hepatitis B therapy, including VEMLIDY. If appropriate, resumption of anti-hepatitis B therapy may be warranted [see Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
VEMLIDY is indicated for the treatment of chronic hepatitis B virus (HBV) infection in adults with compensated liver disease [see Clinical Studies (14)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Testing Prior to Initiation of VEMLIDY
Prior to initiation of VEMLIDY, patients should be tested for HIV-1 infection. VEMLIDY alone should not be used in patients with HIV-1 infection [see Warnings and Precautions (5.2)].
Prior to or when initiating VEMLIDY, and during treatment with VEMLIDY on a clinically appropriate schedule, assess serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients. In patients with chronic kidney disease, also assess serum phosphorus [see Warnings and Precautions (5.3)].
2.2 Recommended Dosage in Adults
The recommended dosage of VEMLIDY is 25 mg (one tablet) taken orally once daily with food [see Clinical Pharmacology (12.3)].
2.3 Dosage in Patients with Renal Impairment
No dosage adjustment of VEMLIDY is required in patients with estimated creatinine clearance greater than or equal to 15 mL per minute, or in patients with end stage renal disease (ESRD; estimated creatinine clearance below 15 mL per minute) who are receiving chronic hemodialysis. On days of hemodialysis, administer VEMLIDY after completion of hemodialysis treatment.
VEMLIDY is not recommended in patients with ESRD who are not receiving chronic hemodialysis [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.4 Dosage in Patients with Hepatic Impairment
No dosage adjustment of VEMLIDY is required in patients with mild hepatic impairment (Child-Pugh A). VEMLIDY is not recommended in patients with decompensated (Child-Pugh B or C) hepatic impairment [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)].
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Severe Acute Exacerbation of Hepatitis B after Discontinuation of Treatment
Discontinuation of anti-hepatitis B therapy, including VEMLIDY, may result in severe acute exacerbations of hepatitis B. Patients who discontinue VEMLIDY should be closely monitored with both clinical and laboratory follow-up for at least several months after stopping treatment. If appropriate, resumption of anti-hepatitis B therapy may be warranted.
5.2 Risk of Development of HIV-1 Resistance in Patients Coinfected with HBV and HIV-1
Due to the risk of development of HIV-1 resistance, VEMLIDY alone is not recommended for the treatment of HIV-1 infection. The safety and efficacy of VEMLIDY have not been established in patients coinfected with HBV and HIV-1. HIV antibody testing should be offered to all HBV-infected patients before initiating therapy with VEMLIDY, and, if positive, an appropriate antiretroviral combination regimen that is recommended for patients coinfected with HIV-1 should be used.
5.3 New Onset or Worsening Renal Impairment
Renal impairment, including cases of acute renal failure and Fanconi syndrome (renal tubular injury with severe hypophosphatemia), has been reported with the use of tenofovir prodrugs in both animal toxicology studies and human trials. In clinical trials of VEMLIDY, there have been no cases of Fanconi syndrome or Proximal Renal Tubulopathy (PRT).
Patients taking tenofovir prodrugs who have impaired renal function and those taking nephrotoxic agents, including non-steroidal anti-inflammatory drugs, are at increased risk of developing renal-related adverse reactions [see Drug Interactions (7.2)].
Prior to or when initiating VEMLIDY, and during treatment with VEMLIDY on a clinically appropriate schedule, assess serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients. In patients with chronic kidney disease, also assess serum phosphorus. Discontinue VEMLIDY in patients who develop clinically significant decreases in renal function or evidence of Fanconi syndrome.
5.4 Lactic Acidosis/Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogs, including tenofovir disoproxil fumarate (TDF), another prodrug of tenofovir, alone or in combination with other antiretrovirals. Treatment with VEMLIDY should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in other sections of the labeling:
- Severe Acute Exacerbation of Hepatitis B [see Warnings and Precautions (5.1)]
- New Onset or Worsening of Renal Impairment [see Warnings and Precautions (5.3)]
- Lactic Acidosis/Severe Hepatomegaly with Steatosis [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse Reactions in Adult Subjects with Chronic Hepatitis B and Compensated Liver Disease
The safety assessment of VEMLIDY was based on pooled data through the Week 96 data analysis from 1298 subjects in two randomized, double-blind, active-controlled trials, Trial 108 and Trial 110, in adult subjects with chronic hepatitis B and compensated liver disease. A total of 866 subjects received VEMLIDY 25 mg once daily [see Clinical Studies (14.2)]. Further safety assessment was based on pooled data from Trials 108 and 110 from subjects who continued to receive their original blinded treatment through Week 120 and additionally from subjects who received open-label VEMLIDY from Week 96 through Week 120 (n = 361 remained on VEMLIDY; n = 180 switched from TDF to VEMLIDY at Week 96).
Based on the Week 96 analysis, the most common adverse reaction (all Grades) reported in at least 10% of subjects in the VEMLIDY group was headache. The proportion of subjects who discontinued treatment with VEMLIDY or TDF due to adverse reactions of any severity was 1.5% and 0.9%, respectively. Table 1 displays the frequency of the adverse reactions (all Grades) greater than or equal to 5% in the VEMLIDY group.
Table 1 Adverse Reactions* (All Grades) Reported in ≥5% of Subjects with Chronic HBV Infection and Compensated Liver Disease in Trials 108 and 110 (Week 96 analysis†) VEMLIDY
(N=866)TDF
(N=432)- * Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
- † Double-blind phase.
- ‡ Grouped term including abdominal pain upper, abdominal pain, abdominal pain lower, and abdominal tenderness.
Headache 12% 10% Abdominal pain‡ 9% 6% Cough 8% 8% Back pain 6% 6% Fatigue 6% 5% Nausea 6% 6% Arthralgia 5% 6% Diarrhea 5% 5% Dyspepsia 5% 5% Additional adverse reactions occurring in less than 5% of subjects in Trials 108 and 110 included vomiting, rash, and flatulence.
The safety profile of VEMLIDY in subjects who continued to receive blinded treatment through Week 120 was similar to that at Week 96. The safety profile of VEMLIDY in subjects who remained on VEMLIDY in the open-label phase through Week 120 was similar to that in subjects who switched from TDF to VEMLIDY at Week 96.
Renal Laboratory Tests
In a pooled analysis of Trials 108 and 110 in adult subjects with chronic hepatitis B and a median baseline estimated creatinine clearance between 106 and 105 mL per minute (for the VEMLIDY and TDF groups, respectively), mean serum creatinine increased by less than 0.1 mg/dL and median serum phosphorus decreased by 0.1 mg/dL in both treatment groups at Week 96. Median change from baseline to Week 96 in estimated creatinine clearance was -1.2 mL per minute in the VEMLIDY group and -4.8 mL per minute in those receiving TDF.
In subjects who remained on blinded treatment beyond Week 96 in Trials 108 and 110, change from baseline in renal laboratory parameter values in each group at Week 120 were similar to those at Week 96. In the open-label phase, median change in eGFR from Week 96 to Week 120 was -0.6 mL per minute in subjects who remained on VEMLIDY and 1.8 mL per minute in those who switched from TDF to VEMLIDY at Week 96. Mean serum creatinine and median serum phosphorus values at Week 120 were similar to those at Week 96 in subjects who remained on VEMLIDY and in subjects who switched from TDF to VEMLIDY.
The long-term clinical significance of these renal laboratory changes on adverse reaction frequencies between VEMLIDY and TDF is not known.
Bone Mineral Density Effects
In a pooled analysis of Trials 108 and 110, the mean percentage change in bone mineral density (BMD) from baseline to Week 96 as assessed by dual-energy X-ray absorptiometry (DXA) was -0.7% with VEMLIDY compared to -2.6% with TDF at the lumbar spine and -0.3% compared to -2.5% at the total hip. BMD declines of 5% or greater at the lumbar spine were experienced by 11% of VEMLIDY subjects and 25% of TDF subjects at Week 96. BMD declines of 7% or greater at the femoral neck were experienced by 5% of VEMLIDY subjects and 13% of TDF subjects at Week 96.
In subjects who remained on blinded treatment beyond Week 96 in Trials 108 and 110, mean percentage change in BMD in each group at Week 120 was similar to that at Week 96. In the open-label phase, mean percentage change in BMD from Week 96 to Week 120 in subjects who remained on VEMLIDY was 0.6% at the lumbar spine and 0% at the total hip, compared to 1.7% at the lumbar spine and 0.6% at the total hip in those who switched from TDF to VEMLIDY.
The long-term clinical significance of these BMD changes is not known.
Laboratory Abnormalities
The frequency of laboratory abnormalities (Grades 3–4) occurring in at least 2% of subjects receiving VEMLIDY in Trials 108 and 110 are presented in Table 2.
Table 2 Laboratory Abnormalities (Grades 3–4) Reported in ≥2% of Subjects with Chronic HBV Infection and Compensated Liver Disease in Trials 108 and 110 (Week 96 analysis*) Laboratory Parameter Abnormality† VEMLIDY
(N=866)TDF
(N=432)ULN=Upper Limit of Normal - * Double-blind phase
- † Frequencies are based on treatment-emergent laboratory abnormalities.
ALT (>5 × ULN) 8% 10% LDL-cholesterol (fasted) (>190 mg/dL) 6% 1% Glycosuria (≥3+) 5% 2% AST (>5 × ULN) 3% 5% Creatine Kinase (≥10 × ULN) 3% 3% Serum Amylase (>2.0 × ULN) 3% 3% The overall incidence of blinded treatment ALT flares (defined as confirmed serum ALT greater than 2 × baseline and greater than 10 × ULN at 2 consecutive postbaseline visits, with or without associated symptoms) was similar between VEMLIDY (0.6%) and TDF (0.9%) through Week 96. ALT flares generally were not associated with coincident elevations in bilirubin, occurred within the first 12 weeks of treatment, and resolved without recurrence.
Based on the Week 120 analysis, the frequencies of lab abnormalities in subjects who remained on VEMLIDY in the open-label phase were similar to those in subjects who switched from TDF to VEMLIDY at Week 96.
Amylase and Lipase Elevations and Pancreatitis
At Week 96, in Trials 108 and 110, eight subjects treated with VEMLIDY with elevated amylase levels had associated symptoms, such as nausea, low back pain; abdominal tenderness, pain, and distension; and biliary pancreatitis and pancreatitis. Of these eight, two subjects discontinued VEMLIDY due to elevated amylase and/or lipase; one subject experienced recurrence of adverse events when VEMLIDY was restarted. No subject treated with TDF had associated symptoms or discontinued treatment.
From Week 96 to Week 120, one additional subject who continued open-label VEMLIDY and none of the subjects who switched from TDF to VEMLIDY had elevated amylase levels and associated symptoms.
Serum Lipids
Changes from baseline in total cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, and total cholesterol to HDL ratio among subjects treated with VEMLIDY and TDF in Trials 108 and 110 are presented in Table 3.
Table 3 Lipid Abnormalities: Mean Change from Baseline in Lipid Parameters in Patients with Chronic HBV Infection and Compensated Liver Disease in Trials 108 and 110 (Week 96 analysis) VEMLIDY
(N=866)TDF
(N=432)Baseline Week 96 Baseline Week 96 mg/dL Change* mg/dL Change* - * The change from baseline is the mean of within-subject changes from baseline for subjects with both baseline and Week 96 values.
Total Cholesterol (fasted) 188
[n=835]-1
[n=742]193
[n=423]-25
[n=368]HDL-Cholesterol (fasted) 60
[n=835]-5
[n=740]61
[n=423]-12
[n=368]LDL-Cholesterol (fasted) 116
[n=835]+7
[n=741]120
[n=423]-10
[n=368]Triglycerides (fasted) 102
[n=836]+13
[n=743]102
[n=423]-7
[n=368]Total Cholesterol to HDL ratio 3
[n=835]0
[n=740]3
[n=423]0
[n=368]In the open-label phase, lipid parameters at Week 120 in subjects who remained on VEMLIDY were similar to those at Week 96. In subjects who switched from TDF to VEMLIDY, mean change from Week 96 to Week 120 in total cholesterol was 23 mg/dL, HDL-cholesterol was 5 mg/dL, LDL-cholesterol was 16 mg/dL, triglycerides was 30 mg/dL, and total cholesterol to HDL ratio was 0 mg/dL.
Adverse Reactions in Virologically Suppressed Adult Subjects with Chronic Hepatitis B
The safety of VEMLIDY in virologically suppressed adults is based on Week 48 data from a randomized, double-blind, active-controlled trial (Trial 4018) in which subjects taking TDF at baseline were randomized to switch to VEMLIDY (N=243) or to continue their TDF treatment (N=245). Adverse reactions observed with VEMLIDY in Trial 4018 were similar to those in Trials 108 and 110 [see Clinical Studies (14.3)].
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of VEMLIDY. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Skin and Subcutaneous Tissue Disorders
Angioedema, urticaria
-
7 DRUG INTERACTIONS
7.1 Potential for Other Drugs to Affect VEMLIDY
VEMLIDY is a substrate of P-glycoprotein (P-gp) and BCRP. Drugs that strongly affect P-gp and BCRP activity may lead to changes in tenofovir alafenamide absorption (see Table 4). Drugs that induce P-gp activity are expected to decrease the absorption of tenofovir alafenamide, resulting in decreased plasma concentrations of tenofovir alafenamide, which may lead to loss of therapeutic effect of VEMLIDY. Coadministration of VEMLIDY with other drugs that inhibit P-gp and BCRP may increase the absorption and plasma concentration of tenofovir alafenamide.
7.2 Drugs Affecting Renal Function
Because tenofovir is primarily excreted by the kidneys by a combination of glomerular filtration and active tubular secretion, coadministration of VEMLIDY with drugs that reduce renal function or compete for active tubular secretion may increase concentrations of tenofovir and other renally eliminated drugs and this may increase the risk of adverse reactions. Some examples of drugs that are eliminated by active tubular secretion include, but are not limited to, acyclovir, cidofovir, ganciclovir, valacyclovir, valganciclovir, aminoglycosides (e.g., gentamicin), and high-dose or multiple NSAIDs [see Warnings and Precautions (5.3)].
7.3 Established and Other Potentially Significant Interactions
Table 4 provides a listing of established or potentially clinically significant drug interactions. The drug interactions described are based on studies conducted with tenofovir alafenamide or are predicted drug interactions that may occur with VEMLIDY [For magnitude of interaction, see Clinical Pharmacology (12.3)]. Information regarding potential drug-drug interactions with HIV antiretrovirals is not provided (see the prescribing information for emtricitabine/tenofovir alafenamide for interactions with HIV antiretrovirals). The table includes potentially significant interactions but is not all inclusive.
Table 4 Established and Other Potentially Significant Drug Interactions* Concomitant Drug Class:
Drug NameEffect on Concentration† Clinical Comment - * This table is not all inclusive.
- † ↓ = decrease.
- ‡ Indicates that a drug interaction study was conducted.
- § P-gp inducer
Anticonvulsants:
Carbamazepine‡§
Oxcarbazepine§
Phenobarbital§
Phenytoin§↓ tenofovir alafenamide When coadministered with carbamazepine, the tenofovir alafenamide dose should be increased to two tablets once daily.
Coadministration of VEMLIDY with oxcarbazepine, phenobarbital, or phenytoin is not recommended.Antimycobacterials:
Rifabutin§
Rifampin§
Rifapentine§↓ tenofovir alafenamide
Coadministration of VEMLIDY with rifabutin, rifampin or rifapentine is not recommended.
Herbal Products:
St. John's wort§
(Hypericum perforatum)↓ tenofovir alafenamide Coadministration of VEMLIDY with St. John's wort is not recommended. 7.4 Drugs without Clinically Significant Interactions with VEMLIDY
Based on drug interaction studies conducted with VEMLIDY, no clinically significant drug interactions have been observed with: ethinyl estradiol, ledipasvir/sofosbuvir, midazolam, norgestimate, sertraline, sofosbuvir, sofosbuvir/velpatasvir, and sofosbuvir/velpatasvir/voxilaprevir.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to VEMLIDY during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Available data from the APR show no significant difference in the overall risk of birth defects for tenofovir alafenamide (TAF) compared with the background rate for major birth defects of 2.7% in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP) (see Data). The rate of miscarriage is not reported in the APR. The estimated background rate of miscarriage in clinically recognized pregnancies in the U.S. general population is 15% to 20%.
In animal studies, no adverse developmental effects were observed when tenofovir alafenamide was administered during the period of organogenesis at exposure equal to or 51 times (rats and rabbits, respectively) the tenofovir alafenamide exposure at the recommended daily dose of VEMLIDY (see Data). No adverse effects were observed in the offspring when TDF was administered through lactation at tenofovir exposures of approximately 12 times the exposure at the recommended daily dosage of VEMLIDY.
Data
Human Data
Based on prospective reports to the APR of exposures to TAF-containing regimens during pregnancy resulting in live births (including over 200 exposed in the first trimester and over 80 exposed in the second/third trimester), the prevalence of birth defects in live births was 5.2% (95% CI: 2.7% to 8.8%) and 1.2% (95% CI: 0% to 6.5%) following first and second/third trimester exposure, respectively, to TAF-containing regimens. Methodologic limitations of the APR include the use of MACDP as the external comparator group. The MACDP population is not disease-specific, evaluates women and infants from a limited geographic area, and does not include outcomes for births that occurred at <20 weeks gestation.
Animal Data
Embryonic fetal development studies performed in rats and rabbits revealed no evidence of impaired fertility or harm to the fetus. The embryo-fetal NOAELs (no observed adverse effect level) in rats and rabbits occurred at tenofovir alafenamide exposures similar to and 51 times higher than, respectively, the exposure in humans at the recommended daily dose. Tenofovir alafenamide is rapidly converted to tenofovir; the observed tenofovir exposure in rats and rabbits were 54 (rats) and 85 (rabbits) times higher than human tenofovir exposures at the recommended daily dose.
Tenofovir alafenamide was administered orally to pregnant rats (25, 100, or 250 mg/kg/day) and rabbits (10, 30, or 100 mg/kg/day) through organogenesis (on gestation days 6 through 17, and 7 through 20, respectively). No adverse embryo-fetal effects were observed in rats and rabbits at tenofovir alafenamide exposures approximately similar to (rats) and 51 (rabbits) times higher than the exposure in humans at the recommended daily dose of VEMLIDY. Tenofovir alafenamide is rapidly converted to tenofovir; the observed tenofovir exposures in rats and rabbits were 54 (rats) and 85 (rabbits) times higher than human tenofovir exposures at the recommended daily dose. Since tenofovir alafenamide is rapidly converted to tenofovir and a lower tenofovir exposure in rats and mice was observed after tenofovir alafenamide administration compared to TDF, another prodrug for tenofovir administration, a pre/postnatal development study in rats was conducted only with TDF. Doses up to 600 mg/kg/day were administered through lactation; no adverse effects were observed in the offspring on gestation day 7 [and lactation day 20] at tenofovir exposures of approximately 12 [18] times higher than the exposures in humans at the recommended daily dose of VEMLIDY.
8.2 Lactation
Risk Summary
It is not known whether VEMLIDY and its metabolites are present in human breast milk, affect human milk production, or have effects on the breastfed infant. Tenofovir has been shown to be present in the milk of lactating rats and rhesus monkeys after administration of TDF (see Data). It is not known if tenofovir alafenamide can be present in animal milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for VEMLIDY and any potential adverse effects on the breastfed infant from VEMLIDY or from the underlying maternal condition.
Data
Animal Data
Studies in rats and monkeys have demonstrated that tenofovir is secreted in milk. Tenofovir was excreted into the milk of lactating rats following oral administration of TDF (up to 600 mg/kg/day) at up to approximately 24% of the median plasma concentration in the highest dosed animals at lactation day 11 (see Data 8.1). Tenofovir was excreted into the milk of lactating monkeys following a single subcutaneous (30 mg/kg) dose of tenofovir at concentrations up to approximately 4% of plasma concentration, resulting in exposure (AUC) of approximately 20% of plasma exposure.
8.4 Pediatric Use
Safety and effectiveness of VEMLIDY in pediatric patients less than 18 years of age have not been established.
8.5 Geriatric Use
Clinical trials of VEMLIDY did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, treatment of an elderly patient should be done with caution; the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy should be considered.
8.6 Renal Impairment
No dosage adjustment of VEMLIDY is required in patients with mild, moderate, or severe renal impairment, or in patients with ESRD (estimated creatinine clearance below 15 mL per minute) who are receiving chronic hemodialysis. On days of hemodialysis, administer VEMLIDY after completion of hemodialysis treatment [see Dosage and Administration (2.3)].
The pharmacokinetics and safety of tenofovir alafenamide were studied in HIV-1 infected adults with ESRD (estimated creatinine clearance below 15 mL per minute by Cockcroft-Gault method) receiving chronic hemodialysis in an open-label trial of 55 subjects who received elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide 150/150/200/10 mg. Tenofovir alafenamide 10 mg, given in this combination, achieves similar exposures as tenofovir alafenamide 25 mg alone [see Clinical Pharmacology (12.3)]. The safety profile of subjects in this trial was consistent with that expected in patients with ESRD on chronic hemodialysis and HIV-1 infection.
VEMLIDY is not recommended in patients with ESRD (estimated creatinine clearance below 15 mL per minute by Cockcroft-Gault method) who are not receiving chronic hemodialysis as the safety of VEMLIDY has not been established in this population [see Dosage and Administration (2.3), and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
No dosage adjustment of VEMLIDY is required in patients with mild hepatic impairment (Child-Pugh A). The safety and efficacy of VEMLIDY in patients with decompensated cirrhosis (Child-Pugh B or C) have not been established; therefore, VEMLIDY is not recommended in patients with decompensated (Child-Pugh B or C) hepatic impairment [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
If overdose occurs, monitor patient for evidence of toxicity. Treatment of overdosage with VEMLIDY consists of general supportive measures including monitoring of vital signs as well as observation of the clinical status of the patient. Tenofovir is efficiently removed by hemodialysis with an extraction coefficient of approximately 54%.
-
11 DESCRIPTION
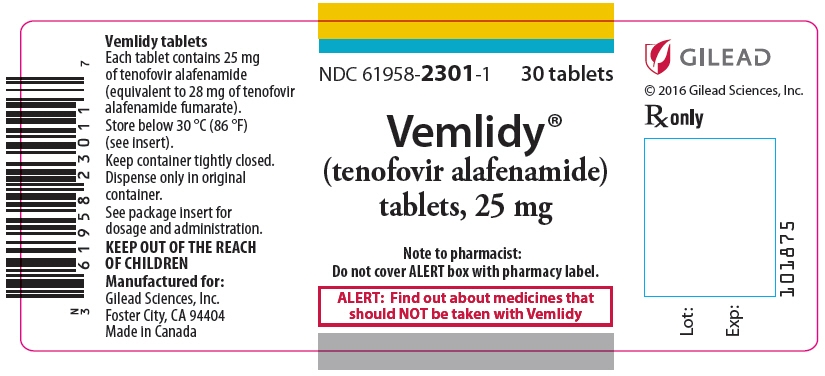
VEMLIDY is a tablet containing tenofovir alafenamide for oral administration. Tenofovir alafenamide, a hepatitis B virus (HBV) nucleoside analog reverse transcriptase inhibitor, is converted in vivo to tenofovir, an acyclic nucleoside phosphonate (nucleotide) analog of adenosine 5′-monophosphate.
Each tablet contains 25 mg of tenofovir alafenamide (equivalent to 28 mg of tenofovir alafenamide fumarate). The tablets include the following inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. The tablets are film coated with a coating material containing: iron oxide yellow, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
The chemical name of tenofovir alafenamide fumarate drug substance is L-alanine, N-[(S)-[[(1R)-2-(6-amino-9H-purin-9-yl)-1-methylethoxy]methyl]phenoxyphosphinyl]-, 1-methylethyl ester, (2E)-2-butenedioate (2:1).
It has an empirical formula of C21H29O5N6P∙½(C4H4O4) and a formula weight of 534.50. It has the following structural formula:
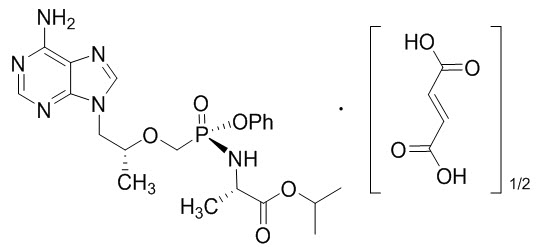
Tenofovir alafenamide fumarate is a white to off-white or tan powder with a solubility of 4.7 mg per mL in water at 20 °C.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tenofovir alafenamide is an antiviral drug against the hepatitis B virus [see Microbiology (12.4)].
12.3 Pharmacokinetics
The pharmacokinetic properties of VEMLIDY are provided in Table 5. The multiple dose PK parameters of tenofovir alafenamide and its metabolite tenofovir are provided in Table 6.
Table 5 Pharmacokinetic Properties of VEMLIDY Tenofovir Alafenamide CES1 = carboxylesterase 1; PBMCs = peripheral blood mononuclear cells. - * Values refer to geometric mean ratio in AUClast [fed/fasted] and (90% confidence interval). High fat meal = ~800 kcal, 50% fat.
- † In vivo, TAF is hydrolyzed within cells to form tenofovir (major metabolite), which is phosphorylated to the active metabolite, tenofovir diphosphate. In vitro studies have shown that TAF is metabolized to tenofovir by CES1 in hepatocytes, and by cathepsin A in PBMCs and macrophages.
- ‡ t1/2 values refer to median terminal plasma half-life.
- § Dosing in mass balance study: TAF 25 mg (single dose administration of [14C] TAF).
Absorption Tmax (h) 0.48 Effect of high fat meal (relative to fasting): AUClast Ratio* 1.65 (1.51, 1.81) Distribution % Bound to human plasma proteins 80% Source of protein binding data Ex vivo Blood-to-plasma ratio 1.0 Metabolism Metabolism† CES1 (hepatocytes)
Cathepsin A (PBMCs)
CYP3A (minimal)Elimination Major route of elimination Metabolism (>80% of oral dose) t1/2 (h)‡ 0.51 % Of dose excreted in urine§ <1 % Of dose excreted in feces§ 31.7 Table 6 Multiple Dose PK Parameters of Tenofovir Alafenamide and its Metabolite Tenofovir Following Oral Administration in Adults with Chronic Hepatitis B Parameter Mean (CV%) Tenofovir Alafenamide* Tenofovir* CV = coefficient of variation; NA = not applicable - * From Intensive PK analyses in Trial 108 and Trial 110; N = 8.
Cmax
(microgram per mL)0.27 (63.3) 0.03 (24.6) AUCtau
(microgram∙hour per mL)0.27 (47.8) 0.40 (35.2) Ctrough (microgram per mL) NA 0.01 (39.6) Specific Populations
Geriatric Patients, Race, and Gender
Limited data in subjects aged 65 years and over suggest a lack of clinically relevant differences in tenofovir alafenamide or tenofovir pharmacokinetics. No clinically relevant differences in tenofovir alafenamide or tenofovir pharmacokinetics due to race or gender have been identified [see Use in Specific Populations (8.5)].
Patients with Renal Impairment
In a Phase 1, open-label study, tenofovir alafenamide and tenofovir systemic exposures (AUCinf) were evaluated in subjects with severe renal impairment and in subjects with normal renal function (Table 7). In an open-label trial of elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide 150/150/200/10 mg, tenofovir alafenamide and tenofovir AUC was evaluated in a subset of virologically suppressed HIV-1 infected subjects with ESRD receiving chronic hemodialysis (Table 7) [see Use in Specific Populations (8.6)].
Table 7 Pharmacokinetics of Tenofovir Alafenamide and its Metabolite Tenofovir in Subjects with Renal Impairment as Compared to Subjects with Normal Renal Function AUC (mcg∙hour per mL)
Mean (CV%)Estimated Creatinine Clearance* ≥90 mL per minute
25 mg TAF
(N=13)†15–29 mL per minute
25 mg TAF
(N=14)†<15 mL per minute
10 mg TAF‡
(N=12)§- * By Cockcroft-Gault method.
- † PK assessed on a single dose of TAF 25 mg in subjects with severe renal impairment and healthy subjects.
- ‡ Exposures from TAF 25 mg = exposures from TAF 10 mg as part of elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide.
- § PK assessed prior to hemodialysis following 3 consecutive daily doses of elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide in HIV-infected subjects.
- ¶ AUCinf.
- # AUClast.
- Þ AUCtau.
- ß N=10.
Tenofovir alafenamide 0.27 (49.2)¶ 0.51 (47.3)¶ 0.23 (53.2)# Tenofovir 0.34 (27.2)¶ 2.07 (47.1)¶ 8.72 (39.4)Þ,ß Drug Interaction Studies
[see Drug Interactions (7)]
The effects of coadministered drugs on the exposure of tenofovir alafenamide are shown in Table 8. The effects of tenofovir alafenamide on the exposure of coadministered drugs are shown in Table 9 [For information regarding clinical recommendations, see Drug Interactions (7)]. Information regarding potential drug-drug interactions with HIV antiretrovirals is not provided (see the prescribing information for emtricitabine/tenofovir alafenamide for interactions with HIV antiretrovirals).
Table 8 Drug Interactions: Changes in Pharmacokinetic Parameters for Tenofovir Alafenamide in the Presence of the Coadministered Drug* Coadministered Drug Dose of Coadministered Drug (mg) Tenofovir Alafenamide (mg) N Geometric Mean Ratio of TAF Pharmacokinetic Parameters (90% CI)†;
No effect = 1.00Cmax AUC Cmin NC = not calculated - * All interaction studies conducted in healthy subjects.
- † All no effect boundaries are 70%–143%.
- ‡ Study conducted with emtricitabine/tenofovir alafenamide.
- § A representative inhibitor of P-glycoprotein.
- ¶ Study conducted with emtricitabine/rilpivirine/tenofovir alafenamide.
- # Study conducted with elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide.
- Þ Study conducted with additional voxilaprevir 100 mg to achieve voxilaprevir exposures expected in HCV-infected patients.
Carbamazepine 300 twice daily 25 once daily‡ 26 0.43
(0.36, 0.51)0.45
(0.40, 0.51)NC Cobicistat§ 150 once daily 8 once daily 12 2.83
(2.20, 3.65)2.65
(2.29, 3.07)NC Ledipasvir/ Sofosbuvir 90/400 once daily 25 once daily¶ 42 1.03
(0.94, 1.14)1.32
(1.25, 1.40)NC Sertraline 50 single dose 10 once daily# 19 1.00
(0.86, 1.16)0.96
(0.89, 1.03)NC Sofosbuvir/ Velpatasvir/ Voxilaprevir 400/100/100+ 100 voxilaprevirÞ once daily 25 once daily¶ 30 1.32
(1.17, 1.48)1.52
(1.43, 1.61)NC Table 9 Drug Interactions: Changes in Pharmacokinetic Parameters for Coadministered Drug in the Presence of Tenofovir Alafenamide* Coadministered Drug Dose of Coadministered Drug (mg) Tenofovir Alafenamide (mg) N Geometric Mean Ratio of Coadministered Drug Pharmacokinetic Parameters (90% CI)†;
No effect = 1.00Cmax AUC Cmin NC = not calculated - * All interaction studies conducted in healthy subjects.
- † All no effect boundaries are 70%–143%.
- ‡ Study conducted with emtricitabine/rilpivirine/tenofovir alafenamide.
- § The predominant circulating nucleoside metabolite of sofosbuvir.
- ¶ A sensitive CYP3A4 substrate.
- # Study conducted with emtricitabine/tenofovir alafenamide.
- Þ Study conducted with elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide.
- ß Study conducted with emtricitabine/rilpivirine/tenofovir alafenamide.
- à Study conducted with additional voxilaprevir 100 mg to achieve voxilaprevir exposures expected in HCV-infected patients.
Ledipasvir 90 ledipasvir / 400 sofosbuvir once daily 25 once daily‡ 41 1.01
(0.97, 1.05)1.02
(0.97, 1.06)1.02
(0.98, 1.07)Sofosbuvir 0.96
(0.89, 1.04)1.05
(1.01, 1.09)NC GS-331007§ 1.08
(1.05, 1.11)1.08
(1.06, 1.10)1.10
(1.07, 1.12)Midazolam¶ 2.5 single dose orally 25 once daily
18
1.02
(0.92, 1.13)1.13
(1.04, 1.23)NC 1 single dose IV 0.99
(0.89, 1.11)1.08
(1.04, 1.14)NC Norelgestromin norgestimate 0.180/0.215/0.250 once daily / ethinyl estradiol 0.025 once daily 25 once daily# 29 1.17
(1.07, 1.26)1.12
(1.07, 1.17)1.16
(1.08, 1.24)Norgestrel 1.10
(1.02, 1.18)1.09
(1.01, 1.18)1.11
(1.03, 1.20)Ethinyl estradiol 1.22
(1.15, 1.29)1.11
(1.07, 1.16)1.02
(0.93, 1.12)Sertraline 50 single dose 10 once dailyÞ 19 1.14
(0.94, 1.38)0.93
(0.77, 1.13)NC Sofosbuvir 400 once daily 25 once dailyß 30 0.95
(0.86, 1.05)1.01
(0.97, 1.06)NC GS-331007§ 1.02
(0.98, 1.06)1.04
(1.01, 1.06)NC Velpatasvir 100 once daily 1.05
(0.96, 1.16)1.01
(0.94, 1.07)1.01
(0.95, 1.09)Voxilaprevir 100+100à once daily 0.96
(0.84, 1.11)0.94
(0.84, 1.05)1.02
(0.92, 1.12)12.4 Microbiology
Mechanism of Action
Tenofovir alafenamide is a phosphonamidate prodrug of tenofovir (2'-deoxyadenosine monophosphate analog). Tenofovir alafenamide as a lipophilic cell-permeant compound enters primary hepatocytes by passive diffusion and by the hepatic uptake transporters OATP1B1 and OATP1B3. Tenofovir alafenamide is then converted to tenofovir through hydrolysis primarily by carboxylesterase 1 (CES1) in primary hepatocytes. Intracellular tenofovir is subsequently phosphorylated by cellular kinases to the pharmacologically active metabolite tenofovir diphosphate. Tenofovir diphosphate inhibits HBV replication through incorporation into viral DNA by the HBV reverse transcriptase, which results in DNA chain-termination.
Tenofovir diphosphate is a weak inhibitor of mammalian DNA polymerases that include mitochondrial DNA polymerase γ and there is no evidence of toxicity to mitochondria in cell culture.
Antiviral Activity in Cell Culture
The antiviral activity of tenofovir alafenamide was assessed in a transient transfection assay using HepG2 cells against a panel of HBV clinical isolates representing genotypes A-H. The EC50 (50% effective concentration) values for tenofovir alafenamide ranged from 34.7 to 134.4 nM, with an overall mean EC50 value of 86.6 nM. The CC50 (50% cytotoxicity concentration) values in HepG2 cells were greater than 44,400 nM. In cell culture combination antiviral activity studies of tenofovir with the HBV nucleoside reverse transcriptase inhibitors entecavir, lamivudine, and telbivudine, no antagonistic activity was observed.
Resistance in Clinical Trials
Genotypic resistance analysis was performed on paired baseline and on-treatment HBV isolates for subjects who either experienced virologic breakthrough (2 consecutive visits with HBV DNA greater than or equal to 69 IU/mL [400 copies/mL] after having been less than 69 IU/mL, or 1.0-log10 or greater increase in HBV DNA from nadir) through Week 48, or had HBV DNA greater than or equal to 69 IU/mL at early discontinuation at or after Week 24.
In a pooled analysis of treatment-naïve and treatment-experienced subjects receiving VEMLIDY in Trials 108 and 110 [see Clinical Studies (14.2)], treatment-emergent amino acid substitutions in the HBV reverse transcriptase domain, all occurring at polymorphic positions, were observed in some HBV isolates evaluated (5/20); however, no specific substitutions occurred at a sufficient frequency to be associated with resistance to VEMLIDY.
In virologically suppressed subjects receiving VEMLIDY in Trial 4018 [see Clinical Studies (14.3)], no subjects qualified for resistance analysis through 48 weeks of VEMLIDY treatment.
Cross-Resistance
The antiviral activity of tenofovir alafenamide was evaluated against a panel of isolates containing substitutions associated with HBV nucleoside reverse transcriptase inhibitor resistance in a transient transfection assay using HepG2 cells. HBV isolates expressing the lamivudine resistance-associated substitutions rtM204V/I (±rtL180M±rtV173L) and expressing the entecavir resistance-associated substitutions rtT184G, rtS202G, or rtM250V in the presence of rtL180M and rtM204V showed less than 2-fold reduced susceptibility (within the inter-assay variability) to tenofovir alafenamide. HBV isolates expressing the rtA181T, rtA181V, or rtN236T single substitutions associated with resistance to adefovir also had less than 2-fold changes in EC50 values; however, the HBV isolate expressing the rtA181V plus rtN236T double substitutions exhibited reduced susceptibility (3.7-fold) to tenofovir alafenamide. The clinical relevance of these substitutions is not known.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Since tenofovir alafenamide is rapidly converted to tenofovir and a lower tenofovir exposure in rats and mice was observed after tenofovir alafenamide administration compared to TDF administration, carcinogenicity studies were conducted only with TDF. Long-term oral carcinogenicity studies of TDF in mice and rats were carried out at exposures up to approximately 10 times (mice) and 4 times (rats) those observed in humans at the 300 mg therapeutic dose of TDF for chronic hepatitis B. The tenofovir exposure in these studies was approximately 151 times (mice) and 50 times (rat) those observed in humans after administration of VEMLIDY treatment. At the high dose in female mice, liver adenomas were increased at tenofovir exposures approximately 151 times those observed after VEMLIDY administration in humans. In rats, the study was negative for carcinogenic findings.
Tenofovir alafenamide was not genotoxic in the reverse mutation bacterial test (Ames test), mouse lymphoma or rat micronucleus assays.
There were no effects on fertility, mating performance or early embryonic development when tenofovir alafenamide was administered to male rats at a dose equivalent to 155 times the human dose based on body surface area comparisons for 28 days prior to mating and to female rats for 14 days prior to mating through Day 7 of gestation.
13.2 Animal Toxicology and/or Pharmacology
Minimal to slight infiltration of mononuclear cells in the posterior uvea was observed in dogs with similar severity after three- and nine-month administration of tenofovir alafenamide; reversibility was seen after a three-month recovery period. At the NOAEL for eye toxicity, the systemic exposure in dogs was 5 (tenofovir alafenamide) and 14 (tenofovir) times the exposure seen in humans at the recommended daily VEMLIDY dosage.
-
14 CLINICAL STUDIES
14.1 Description of Clinical Trials
The efficacy and safety of VEMLIDY were evaluated in the trials summarized in Table 10.
Table 10 Trials Conducted with VEMLIDY in Adults with Chronic HBV Infection Trial Population Trial Arms (N) Primary Endpoint (Week) TE = treatment-experienced, TN = treatment-naive - * Randomized, double blind, active controlled trial.
- † HBV DNA <20 IU/mL at screening.
Trial 108*
(NCT01940341)HBeAg-negative TN and TE adults with compensated liver disease VEMLIDY (285)
TDF (140)48 Trial 110*
(NCT01940471)HBeAg-positive TN and TE adults with compensated liver disease VEMLIDY (581)
TDF(292)48 Trial 4018*
(NCT02979613)HBeAg-negative and HBeAg-positive virologically suppressed† adults with compensated liver disease VEMLIDY (243)
TDF (245)48 14.2 Clinical Trials in Adults with Chronic Hepatitis B Virus Infection and Compensated Liver Disease
The efficacy and safety of VEMLIDY in the treatment of adults with chronic hepatitis B virus infection with compensated liver disease are based on 48-week data from two randomized, double-blind, active-controlled trials, Trial 108 (N=425) and Trial 110 (N=873). In both trials, besides trial treatment, subjects were not allowed to receive other nucleosides, nucleotides, or interferon.
In Trial 108, HBeAg-negative treatment-naïve and treatment-experienced subjects with compensated liver disease (no evidence of ascites, hepatic encephalopathy, variceal bleeding, INR <1.5× ULN, total bilirubin <2.5× ULN, and albumin >3.0 mg/dL) were randomized in a 2:1 ratio to receive VEMLIDY 25 mg (N=285) once daily or TDF 300 mg (N=140) once daily for 48 weeks. The mean age was 46 years, 61% were male, 72% were Asian, 25% were White, 2% were Black, and 1% were other races. 24%, 38%, and 31% had HBV genotype B, C, and D, respectively. 21% were treatment experienced [previous treatment with oral antivirals, including entecavir (N=41), lamivudine (N=42), TDF (N=21), or other (N=18)]. At baseline, mean plasma HBV DNA was 5.8 log10 IU/mL, mean serum ALT was 94 U/L, and 9% of subjects had a history of cirrhosis.
In Trial 110, HBeAg-positive treatment-naïve and treatment-experienced subjects with compensated liver disease were randomized in a 2:1 ratio to receive VEMLIDY 25 mg (N=581) once daily or TDF 300 mg (N=292) once daily for 48 weeks. The mean age was 38 years, 64% were male, 82% were Asian, 17% were White, and 1% were Black or other races. 17%, 52%, and 23% had HBV genotype B, C, and D, respectively. 26% were treatment experienced [previous treatment with oral antivirals, including adefovir (N=42), entecavir (N=117), lamivudine (N=84), telbivudine (N=25), TDF (N=70), or other (n=17)]. At baseline, mean plasma HBV DNA was 7.6 log10 IU/mL, mean serum ALT was 120 U/L, and 7% of subjects had a history of cirrhosis.
In both trials, randomization was stratified on prior treatment history (nucleoside naïve or experienced) and baseline HBV DNA (<7, ≥7 to <8, and ≥8 log10 IU/mL in Trial 108; and <8 and ≥8 log10 IU/mL in Trial 110). The efficacy endpoint in both trials was the proportion of subjects with plasma HBV DNA levels below 29 IU/mL at Week 48. Additional efficacy endpoints include the proportion of subjects with ALT normalization, HBsAg loss and seroconversion, and HBeAg loss and seroconversion in Trial 110.
Treatment outcomes of Trials 108 and 110 at Week 48 are presented in Table 11 and Table 12.
Table 11 Trials 108 and 110: HBV DNA Virologic Outcome at Week 48* in Patients with Chronic HBV Infection and Compensated Liver Disease Trial 108 (HBeAg-Negative) Trial 110 (HBeAg-Positive) VEMLIDY
(N=285)TDF
(N=140)VEMLIDY
(N=581)TDF
(N=292)- * Missing = failure analysis
- † Adjusted by baseline plasma HBV DNA categories and oral antiviral treatment status strata.
- ‡ Treatment-naïve subjects received <12 weeks of oral antiviral treatment with any nucleoside or nucleotide analog including TDF or VEMLIDY.
- § Includes subjects who discontinued due to lack of efficacy, adverse event or death, for reasons other than an AE, death or lack or loss of efficacy, e.g., withdrew consent, loss to follow-up, etc., or missing data during Week 48 window but still on study drug.
HBV DNA
<29 IU/mL94% 93% 64% 67% Treatment Difference† 1.8% (95% CI = -3.6% to 7.2%) -3.6% (95% CI = -9.8% to 2.6%) HBV DNA ≥ 29 IU/mL 2% 3% 31% 30% Baseline HBV DNA <7 log10 IU/mL 96% (221/230) 92% (107/116) N/A N/A ≥7 log10 IU/mL 85% (47/55) 96% (23/24) Baseline HBV DNA <8 log10 IU/mL N/A N/A 82% (254/309) 82% (123/150) ≥8 log10 IU/mL 43% (117/272) 51% (72/142) Nucleoside Naïve‡ 94% (212/225) 93% (102/110) 68% (302/444) 70% (156/223) Nucleoside Experienced 93% (56/60) 93% (28/30) 50% (69/137) 57% (39/69) No Virologic Data at Week 48§ 4% 4% 5% 3% In Trial 108, the proportion of subjects with cirrhosis who achieved HBV DNA <29 IU/mL at Week 48 was 92% (22/24) in the VEMLIDY group and 93% (13/14) in the TDF group. The corresponding proportions in Trial 110 were 63% (26/41) and 67% (16/24) in the VEMLIDY and TDF groups, respectively.
Table 12 Additional Efficacy Parameters at Week 48* Trial 108 (HBeAg-Negative) Trial 110 (HBeAg-Positive) VEMLIDY
(N=285)TDF
(N=140)VEMLIDY
(N=581)TDF
(N=292)N/A = not applicable - * Missing = failure analysis
- † The population used for analysis of ALT normalization included only subjects with ALT above upper limit of normal (ULN) of the central laboratory range (>43 U/L for males aged 18 to <69 years and >35 U/L for males ≥69 years; >34 U/L for females 18 to <69 years and >32 U/L for females ≥69 years) at baseline.
- ‡ The population used for analysis of ALT normalization included only subjects with ALT above ULN of the 2016 American Association of the Study of Liver Diseases (AASLD) criteria (>30 U/L males and >19 U/L females) at baseline.
- § The population used for serology analysis included only subjects with antigen (HBeAg) positive and anti-body (HBeAb) negative or missing at baseline.
ALT Normalized ALT (Central Lab)† 83% 75% 72% 67% Normalized ALT (AASLD)‡ 50% 32% 45% 36% Serology HBeAg Loss / Seroconversion§ N/A N/A 14% / 10% 12% / 8% HBsAg Loss / Seroconversion 0 / 0 0 / 0 1% / 1% <1% / 0 14.3 Clinical Trials in Virologically Suppressed Adults with Chronic Hepatitis B Virus Infection Who Switched to VEMLIDY
The efficacy and safety of switching from TDF to VEMLIDY in virologically suppressed adults with chronic hepatitis B virus infection is based on 48-week data from a randomized, double-blind, active-controlled trial, Trial 4018 (N=488). Subjects must have been taking TDF 300 mg once daily for at least 12 months, with HBV DNA less than the Lower Limit of Quantitation by local laboratory assessment for at least 12 weeks prior to screening and HBV DNA <20 IU/mL at screening. Subjects were stratified by HBeAg status (HBeAg-positive or HBeAg-negative) and age (≥50 or <50 years) and randomized in a 1:1 ratio to either switch to VEMLIDY 25 mg once daily (N=243) or stay on TDF 300 mg once daily (N=245). The mean age was 51 years (22% were ≥60 years), 71% were male, 82% were Asian, 14% were White, and 68% were HBeAg-negative. At baseline, median duration of prior TDF treatment was 220 and 224 weeks in the VEMLIDY and TDF groups, respectively. At baseline, mean serum ALT was 27 U/L, and 16% of patients had a history of cirrhosis.
The primary efficacy endpoint was the proportion of subjects with plasma HBV DNA levels ≥20 IU/mL at Week 48. Additional efficacy endpoints in Trial 4018 included the proportion of subjects with HBV DNA <20 IU/mL, ALT normal and normalization, HBsAg loss and seroconversion, and HBeAg loss and seroconversion.
Treatment outcomes of Trial 4018 at Week 48 are presented in Table 13 and Table 14.
Table 13 Trial 4018: HBV DNA Virologic Outcome at Week 48* in Virologically Suppressed Subjects with Chronic HBV Infection VEMLIDY
(N=243)TDF
(N=245)- * Week 48 window was between Day 295 and Day 378 (inclusive).
- † No subject discontinued treatment due to lack of efficacy.
- ‡ Adjusted by baseline age groups (< 50, ≥ 50 years) and baseline HBeAg status strata.
- § Includes subjects who discontinued for reasons other than an AE, death, or lack of efficacy, e.g., withdrew consent, loss to follow-up, etc.
HBV DNA ≥20 IU/mL† <1% <1% Treatment Difference‡ 0.0% (95% CI = -1.9% to 2.0%) HBV DNA <20 IU/mL 96% 96% Treatment Difference‡ 0.0% (95% CI = -3.7% to 3.7%) No Virologic Data at Week 48 3% 3% Discontinued Study Drug Due to AE or Death and Last Available HBV DNA <20 IU/mL 1% 0 Discontinued Study Drug Due to Other Reasons§and Last Available HBV DNA <20 IU/mL 2% 3% Table 14 Additional Efficacy Parameters at Week 48* (Trial 4018) VEMLIDY
(N=243)TDF
(N=245)- * Missing = failure analysis
- † The population used for analysis of ALT normalization included only subjects with ALT above upper limit of normal (ULN) of the central laboratory range (>43 U/L for males 18 to <69 years and >35 U/L for males ≥69 years; >34 U/L for females 18 to <69 years and >32 U/L for females ≥69 years) at baseline.
- ‡ Proportion of subjects at Week 48: VEMLIDY, 16/32; TDF, 7/19.
- § The population used for analysis of ALT normalization included only subjects with ALT above ULN of the 2018 American Association of the Study of Liver Diseases (AASLD) criteria (35 U/L males and 25 U/L females) at baseline.
- ¶ Proportion of subjects at Week 48: VEMLIDY, 26/52; TDF, 14/53.
- # The population used for serology analysis included only subjects with antigen (HBeAg) positive and anti-body (HBeAb) negative or missing at baseline.
ALT Normal ALT (Central Lab) 89% 85% Normal ALT (AASLD) 79% 75% Normalized ALT (Central Lab)†,‡ 50% 37% Normalized ALT (AASLD)§,¶ 50% 26% Serology HBeAg Loss / Seroconversion# 8% / 3% 6% / 0 HBsAg Loss / Seroconversion 0 / 0 2% / 0 -
16 HOW SUPPLIED/STORAGE AND HANDLING
VEMLIDY tablets containing 25 mg of tenofovir alafenamide are yellow, round, film-coated, debossed with "GSI" on one side and "25" on the other side. Each bottle contains 30 tablets (NDC: 61958-2301-1), a silica gel desiccant, polyester coil, and is closed with a child-resistant closure.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Severe Acute Exacerbation of Hepatitis after Discontinuation of Treatment
Inform patients that discontinuation of anti-hepatitis B therapy, including VEMLIDY, may result in severe acute exacerbations of hepatitis B. Advise the patient to not discontinue VEMLIDY without first informing their healthcare provider [see Warnings and Precautions (5.1)].
Risk of Development of HIV-1 Resistance in Patients with HIV-1 Coinfection
Inform patients that if they have or develop HIV infection and are not receiving effective HIV treatment, VEMLIDY may increase the risk of development of resistance to HIV medication [see Dosage and Administration (2.1) and Warnings and Precautions (5.2)].
New Onset or Worsening Renal Impairment
Advise patients that renal impairment, including cases of acute renal failure, has been reported in association with the use of tenofovir prodrugs [see Warnings and Precautions (5.3)].
Lactic Acidosis and Severe Hepatomegaly
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with use of drugs similar to VEMLIDY. Advise patients to contact their healthcare provider immediately and stop VEMLIDY if they develop clinical symptoms suggestive of lactic acidosis or pronounced hepatotoxicity [see Warnings and Precautions (5.4)].
Drug Interactions
Advise patients to report to their healthcare provider the use of any other prescription or non-prescription medication or herbal products including St. John's wort, as VEMLIDY may interact with other drugs [see Drug Interactions (7)].
Missed Dosage
Inform patients that it is important to take VEMLIDY on a regular dosing schedule with food and to avoid missing doses, as it can result in development of resistance [see Dosage and Administration (2.2)].
Pregnancy Registry
Inform patients that there is an antiretroviral pregnancy registry to monitor fetal outcomes of pregnant women exposed to VEMLIDY [see Use in Specific Populations (8.1)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration. Revised: 02/2020 Patient Information
VEMLIDY® (VEM-lih-dee)
(tenofovir alafenamide)
tabletsWhat is the most important information I should know about VEMLIDY?
VEMLIDY can cause serious side effects, including:-
Worsening of hepatitis B infection. Your hepatitis B (HBV) infection may become worse (flare-up) if you take VEMLIDY and then stop taking it. A "flare-up" is when your HBV infection suddenly returns in a worse way than before.
- Do not run out of VEMLIDY. Refill your prescription or talk to your healthcare provider before your VEMLIDY is all gone.
- Do not stop taking VEMLIDY without first talking to your healthcare provider.
- If you stop taking VEMLIDY, your healthcare provider will need to check your health often and do blood tests regularly for several months to check your HBV infection. Tell your healthcare provider about any new or unusual symptoms you may have after you stop taking VEMLIDY.
What is VEMLIDY?
VEMLIDY is a prescription medicine used to treat chronic (long-lasting) hepatitis B virus (HBV) in adults with stable (compensated) liver disease.- VEMLIDY may lower the amount of HBV in your body.
- VEMLIDY may improve the condition of your liver.
What should I tell my healthcare provider before taking VEMLIDY?
Before you take VEMLIDY, tell your healthcare provider about all of your medical conditions, including if you:- have HIV-1 infection. Your healthcare provider may test you for HIV-1 infection before you start VEMLIDY. If you have both HBV and HIV-1, and you only take VEMLIDY, the HIV-1 virus may develop resistance and become harder to treat.
- have end stage renal disease (ESRD).
- are pregnant or plan to become pregnant. It is not known if VEMLIDY will harm your unborn baby. Tell your healthcare provider if you become pregnant during treatment with VEMLIDY.
Pregnancy Registry: There is a pregnancy registry for women who take antiviral medicines during pregnancy. The purpose of this registry is to collect information about the health of you and your baby. Talk with your healthcare provider about how you can take part in this registry. - are breastfeeding or plan to breastfeed. It is not known if VEMLIDY passes into your breast milk. Talk with your healthcare provider about the best way to feed your baby.
Some medicines may affect how VEMLIDY works.- Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine. You can ask your healthcare provider or pharmacist for a list of medicines that interact with VEMLIDY.
- Do not start a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take VEMLIDY with other medicines.
How should I take VEMLIDY? - Take VEMLIDY exactly as your healthcare provider tells you to take it.
- Take VEMLIDY 1 time each day.
- Take VEMLIDY with food.
- If you are on dialysis, on your dialysis days, take your daily dose of VEMLIDY following dialysis.
- Do not change your dose or stop taking VEMLIDY without first talking with your healthcare provider. Stay under a healthcare provider's care when taking VEMLIDY.
- Do not miss a dose of VEMLIDY.
- If you take too much VEMLIDY, call your healthcare provider or go to the nearest hospital emergency room right away.
- When your VEMLIDY supply starts to run low, get more from your healthcare provider or pharmacy. This is very important because your HBV infection may get worse (flare-up) if you stop taking VEMLIDY.
What are the possible side effects of VEMLIDY?
VEMLIDY may cause serious side effects, including:- See "What is the most important information I should know about VEMLIDY?"
- New or worse kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys when starting and during treatment with VEMLIDY. Your healthcare provider may tell you to stop taking VEMLIDY if you develop new or worse kidney problems.
- Too much lactic acid in your blood (lactic acidosis). Too much lactic acid is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
- Severe liver problems. In rare cases, severe liver problems can happen that can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark "tea-colored" urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
These are not all the possible side effects of VEMLIDY. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store VEMLIDY? - Store VEMLIDY below 86 °F (30 °C).
- Keep VEMLIDY in its original container.
- Keep the container tightly closed.
- VEMLIDY comes in a child-resistant package.
General information about the safe and effective use of VEMLIDY.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use VEMLIDY for a condition for which it was not prescribed. Do not give VEMLIDY to other people, even if they have the same symptoms you have. It may harm them. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about VEMLIDY that is written for health professionals.What are the ingredients in VEMLIDY?
Active ingredients: tenofovir alafenamide
Inactive ingredients: croscarmellose sodium, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. The tablets are film-coated with a coating material containing: iron oxide yellow, polyethylene glycol, polyvinyl alcohol, talc, and titanium dioxide.
Manufactured and distributed by: Gilead Sciences, Inc. Foster City, CA 94404
VEMLIDY is a registered trademark of Gilead Sciences, Inc., or its related companies. © 2020 Gilead Sciences, Inc. All rights reserved.
208464-GS-004
For more information, call 1-800-445-3235 or go to www.VEMLIDY.com. -
Worsening of hepatitis B infection. Your hepatitis B (HBV) infection may become worse (flare-up) if you take VEMLIDY and then stop taking it. A "flare-up" is when your HBV infection suddenly returns in a worse way than before.
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
VEMLIDY
tenofovir alafenamide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61958-2301 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TENOFOVIR ALAFENAMIDE FUMARATE (UNII: FWF6Q91TZO) (TENOFOVIR ANHYDROUS - UNII:W4HFE001U5) TENOFOVIR ALAFENAMIDE 25 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYETHYLENE GLYCOL 3350 (UNII: G2M7P15E5P) TALC (UNII: 7SEV7J4R1U) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color yellow Score no score Shape ROUND Size 8mm Flavor Imprint Code GSI;25 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61958-2301-1 30 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 11/10/2016 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA208464 11/10/2016 Labeler - Gilead Sciences, Inc. (185049848)
Trademark Results [VEMLIDY]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 VEMLIDY 86765021 5001852 Live/Registered |
Gilead Sciences Ireland UC 2015-09-22 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.