SANCUSO- granisetron patch
SANCUSO by
Drug Labeling and Warnings
SANCUSO by is a Prescription medication manufactured, distributed, or labeled by Cumberland Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SANCUSO safely and effectively. See full prescribing information for SANCUSO.
SANCUSO (granisetron transdermal system)
Initial U.S. Approval: 2008INDICATIONS AND USAGE
SANCUSO is a serotonin-3 (5-HT3) receptor antagonist indicated for the prevention of nausea and vomiting in adults receiving moderately and/or highly emetogenic chemotherapy for up to 5 consecutive days. (1)
DOSAGE AND ADMINISTRATION
The recommended dosage is a single transdermal system applied to the upper outer arm a minimum of 24 hours, up to a maximum of 48 hours, before chemotherapy. The transdermal system should be worn at minimum, 24 hours after chemotherapy is finished. The transdermal system can be worn for up to 7 days. (2)
DOSAGE FORMS AND STRENGTHS
Transdermal System: 3.1 mg per 24 hours. (3)
CONTRAINDICATIONS
Known hypersensitivity to granisetron or to any of the components of the transdermal system (4)
WARNINGS AND PRECAUTIONS
-
Progressive Ileus and Gastric Distention: Granisetron may mask a progressive ileus and/or gastric distention; consider before use in patients with abdominal surgery.
Monitor for decreased bowel activity, particularly in patients with risk factors for gastrointestinal obstruction. (5.1) - Serotonin Syndrome: Serotonin syndrome has been reported with 5-HT3 receptor antagonists alone but particularly with concomitant use of serotonergic drugs. If such symptoms occur, discontinue SANCUSO and initiate supportive treatment. If concomitant use of SANCUSO with other serotonergic drugs is clinically warranted, patients should be aware of a potential increased risk of serotonin syndrome. (5.2, 7.1)
- Skin Reactions: Mild application site reactions have occurred; remove SANCUSO transdermal system if severe reactions or a generalized skin reaction occur. (5.3)
- Increased Drug Exposure with Use of External Heat Sources: Avoid exposing SANCUSO transdermal system and surrounding area to direct external heat sources, such as heating pads (5.4).
- Phototoxicity with Ultraviolet Light Exposure: Avoid direct exposure of application site to natural or artificial sunlight, including sunlamps, by covering with clothing throughout the period of wear and for 10 days after removal. (5.5)
ADVERSE REACTIONS
The most common adverse reaction (≥ 3%) is constipation. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Cumberland Pharmaceuticals Inc. at 1-877-484-2700 (X 225) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2024
-
Progressive Ileus and Gastric Distention: Granisetron may mask a progressive ileus and/or gastric distention; consider before use in patients with abdominal surgery.
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Progressive Ileus and Gastric Distention
5.2 Serotonin Syndrome
5.3 Skin Reactions
5.4 Increased Drug Exposure with Use of External Heat Sources
5.5 Phototoxicity with Ultraviolet Light Exposure
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Serotonergic Drugs
7.2 Concomitant Use Medications
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment or Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.3 Phototoxicity
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
The recommended dosage is a single transdermal system applied to the upper outer arm a minimum of 24 hours, up to a maximum of 48 hours, before chemotherapy. The transdermal system should be worn at minimum, 24 hours after chemotherapy is finished. The transdermal system can be worn for up to 7 days.
Application and Removal Instructions
- Each transdermal system releases 3.1 mg of granisetron per 24 hours for up to 7 days.
- Each transdermal system is packed in a pouch and should be applied directly after the pouch has been opened.
- Only wear one transdermal system at any time.
- Do not cut the transdermal system.
- Open the pouch and apply the transdermal system to clean, dry, nearly hairless, intact healthy skin on the upper outer arm.
- Do not place SANCUSO transdermal system on skin that is red, irritated, or damaged.
- Do not apply a heat pad or heat lamp over or in vicinity of the transdermal system and avoid extended exposure to heat [see Warnings and Precautions (5.4)].
- Cover the application site of the transdermal system with clothing, if there is a risk of exposure to direct natural or artificial sunlight throughout the period of wear and for 10 days following its removal [see Warnings and Precautions (5.5)].
- After the transdermal system is applied, wash hands thoroughly.
- Remove the transdermal system by peeling off gently from the skin.
- Upon removal, fold the transdermal system in half with the sticky side together, and discard in the household trash in a manner that prevents accidental contact or ingestion by children, pets or others.
- SANCUSO contains granisetron. Do not use other granisetron-containing products with SANCUSO.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
SANCUSO is contraindicated in patients with known hypersensitivity to granisetron or to any of the components of the transdermal system [see Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Progressive Ileus and Gastric Distention
SANCUSO may mask a progressive ileus and/or gastric distention. This should be particularly considered before use of SANCUSO in patients who have had recent abdominal surgery. Monitor for decreased bowel activity, particularly in patients with risk factors for gastrointestinal obstruction.
5.2 Serotonin Syndrome
The development of serotonin syndrome has been reported with 5-HT3 receptor antagonists. Most reports have been associated with concomitant use of serotonergic drugs (e.g., selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors, mirtazapine, fentanyl, lithium, tramadol, and intravenous methylene blue). Some of the reported cases were fatal. Serotonin syndrome occurring with overdose of another 5-HT3 receptor antagonist alone has also been reported. The majority of reports of serotonin syndrome related to 5-HT3 receptor antagonist use occurred in a post-anesthesia care unit or an infusion center.
Symptoms associated with serotonin syndrome may include the following combination of signs and symptoms: mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, with or without gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome, especially with concomitant use of SANCUSO and other serotonergic drugs. If symptoms of serotonin syndrome occur, discontinue SANCUSO and initiate supportive treatment. Patients should be informed of the increased risk of serotonin syndrome, especially if SANCUSO is used concomitantly with other serotonergic drugs. [see Drug Interactions (7)].
5.3 Skin Reactions
In clinical trials with SANCUSO, application site reactions were reported that were generally mild in intensity and did not lead to discontinuation of use. The incidence of reactions was comparable with placebo.
If severe reactions, or a generalized skin reaction occur (e.g., allergic rash, including erythematous, macular, papular rash or pruritus), remove the SANCUSO transdermal system.
5.4 Increased Drug Exposure with Use of External Heat Sources
Prolonged exposure to heat results in increasing plasma concentrations of granisetron during the period of heat exposure [see Clinical Pharmacology (12.3)]. Do not apply a heat pad or heat lamp over or in the vicinity of the SANCUSO transdermal system and avoid extended exposure to heat [see Dosage and Administration (2)].
5.5 Phototoxicity with Ultraviolet Light Exposure
Granisetron may be affected by direct natural or artificial sunlight, including sunlamps. An in vitro study using Chinese hamster ovary cells suggests that granisetron has the potential for photogenotoxicity [see Nonclinical Toxicology (13.3)]. To avoid a potential skin reaction, advise patients to cover the application site of the transdermal system with clothing if there is a risk of exposure to direct natural or artificial sunlight throughout the period of wear and for 10 days following its removal.
-
6 ADVERSE REACTIONS
The following are serious or otherwise clinically significant adverse reactions reported in other sections of labeling:
- Progressive ileus and gastric distention [see Warnings and Precautions (5.1)]
- Serotonin syndrome [see Warnings and Precautions (5.2)]
- Skin reactions [see Warnings and Precautions (5.3)]
- Increased drug exposure with use of external heat sources [see Warnings and Precautions (5.4)]
- Phototoxicity with ultraviolet light exposure [se Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of SANCUSO was evaluated in a total of 404 patients undergoing chemotherapy who participated in two double-blind, comparator studies with transdermal system treatment durations of up to 7 days. The control groups included a total of 406 patients who received a daily dose of 2 mg oral granisetron, for 1 to 5 days.
Adverse reactions occurred in 9% (35/404) of patients receiving SANCUSO and 7% (29/406) of patients receiving oral granisetron. The most common adverse reaction was constipation that occurred in 5% of patients in the SANCUSO group and 3% of patients in the oral granisetron group.
Table 1 lists the adverse reactions that occurred in at least 3% of patients treated with SANCUSO or oral granisetron.
Table 1: Incidence of Adverse Reactions in Double-Blind, Active Comparator Controlled Studies in Cancer Patients Receiving Chemotherapy (³ 3% in either group) SANCUSO Transdermal System Oral granisetron Body System N=404 N=406 Preferred Term (%) (%) Gastrointestinal disorders Constipation 5 3 Nervous system disorders Headache 1 3 5-HT3 receptor antagonists, such as granisetron, may be associated with arrhythmias or ECG abnormalities. Three ECGs were performed on 588 patients in a randomized, parallel group, double-blind, double-dummy study: at baseline before treatment, the first day of chemotherapy, and 5 to 7 days after starting chemotherapy. QTcF prolongation greater than 450 milliseconds was seen in a total of 11 (1.9%) patients after receiving granisetron, 8 (2.7%) on oral granisetron, and 3 (1.1%) on the transdermal system. No new QTcF prolongation greater than 480 milliseconds was observed in any patient in this study. No arrhythmias were detected in this study.
Adverse reactions reported in clinical trials with other formulations of granisetron include the following:
Gastrointestinal: abdominal pain, diarrhea, constipation, elevation of ALT and AST levels, nausea and vomiting
Cardiovascular: hypertension, hypotension, angina pectoris, atrial fibrillation and syncope have been observed rarely
Central Nervous System: dizziness, insomnia, headache, anxiety, somnolence and asthenia
Hypersensitivity: rare cases of hypersensitivity reactions, sometimes severe (e.g. anaphylaxis, shortness of breath, hypotension, urticaria) have been reported
Other: fever; events often associated with chemotherapy have also been reported: leucopenia, decreased appetite, anemia, alopecia, thrombocytopenia.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of SANCUSO. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General Disorders and Administration Site Conditions: Application site reactions (pain, pruritus, erythema, rash, irritation, vesicles, burn, discoloration, urticaria) [see Warnings and Precautions (5.3)]; transdermal system non-adhesion.
Cardiac Disorders: bradycardia, chest pain, palpitations, sick sinus syndrome
-
7 DRUG INTERACTIONS
7.1 Serotonergic Drugs
Serotonin syndrome (including altered mental status, autonomic instability, and neuromuscular symptoms) has been described following the concomitant use of 5-HT3 receptor antagonists and other serotonergic drugs, including selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs). Monitor for the emergence of serotonin syndrome. If symptoms occur, discontinue SANCUSO and initiate supportive treatment [see Warnings and Precautions (5.4)].
7.2 Concomitant Use Medications
There have been no definitive drug-drug interaction studies to examine pharmacokinetic or pharmacodynamic interaction with other drugs. However, in humans, granisetron hydrochloride injection has been safely administered with drugs representing benzodiazepines, neuroleptics and anti-ulcer medications commonly prescribed with antiemetic treatments. Granisetron hydrochloride injection also does not appear to interact with emetogenic cancer therapies. In agreement with these data, no clinically relevant drug interactions have been reported in clinical studies with SANCUSO.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available published data and postmarketing reports with granisetron use in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. In a published ex vivo human placental perfusion model, no transplacental passage of granisetron was detected at a concentration (5 ng/mL) that mimics the plasma concentration achieved following transdermal application of SANCUSO. In animal reproduction studies, no adverse developmental effects were observed in pregnant rats and rabbits administered granisetron hydrochloride during organogenesis at intravenous doses up to 24 times and 16 times, respectively, the maximum recommended human dose delivered by the SANCUSO transdermal system, based on body surface area (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risks of major birth defects and miscarriage in clinically recognized pregnancies are 2-4% and 15-20%, respectively.
In animal reproduction studies, no adverse developmental effects were observed in pregnant rats and rabbits administered granisetron hydrochloride at intravenous doses up to 24 times and 16 times, respectively, the maximum recommended human dose delivered by the SANCUSO transdermal system, based on body surface area (see Data).
Data
Animal Data
Reproduction studies with granisetron hydrochloride have been performed in pregnant rats at intravenous doses up to 9 mg/kg/day (54 mg/m2/day, about 24 times the recommended human dose delivered by the SANCUSO transdermal system, based on body surface area) and oral doses up to 125 mg/kg/day (750 mg/m2/day, about 326 times the recommended human dose with SANCUSO based on body surface area). Reproduction studies have been performed in pregnant rabbits at intravenous doses up to 3 mg/kg/day (36 mg/m2/day, about 16 times the human dose with SANCUSO based on body surface area) and at oral doses up to 32 mg/kg/day (384 mg/m2/day, about 167 times the human dose with SANCUSO based on body surface area). These studies did not reveal any harm to the fetus due to granisetron.
8.2 Lactation
Risk Summary
There are no data on the presence of granisetron in human milk, the effects on the breastfed child, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for SANCUSO and any potential adverse effects on the breastfed child from SANCUSO or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of SANCUSO have not been established in pediatric patients.
8.5 Geriatric Use
Clinical studies of SANCUSO did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, cautious treatment selection for an elderly patient is prudent because of the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment or Hepatic Impairment
Although no studies have been performed to investigate the pharmacokinetics of SANCUSO in patients with renal or hepatic impairment, pharmacokinetic information is available for intravenous granisetron [see Clinical Pharmacology (12.3)]. No dosage adjustment is recommended for renal or hepatic impairment.
- 10 OVERDOSAGE
-
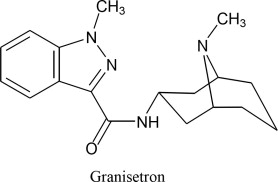
11 DESCRIPTION
SANCUSO contains granisetron, which is a serotonin-3 (5-HT3) receptor antagonist. Chemically it is 1-methyl-N-[(1R,3r,5S)-9-methyl-9-azabicyclo[3.3.1]non-3-yl]-1H-indazole-3-carboxamide with a molecular weight of 312.4. Its empirical formula is C18H24N4O, while its chemical structure is:
Granisetron is a white to off-white solid that is insoluble in water. The inactive ingredients are acrylate-vinylacetate copolymer, polyester, titanium dioxide, polyamide resin and polyethylene wax. SANCUSO is a 52 cm2 thin, translucent, matrix-type transdermal system that is rectangular- shaped with rounded corners, consisting of a backing (polyester), the drug matrix (acrylate- vinylacetate copolymer) and a release liner (siliconized polyester).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Granisetron is a selective 5-hydroxytryptamine3 (5-HT3) receptor antagonist with little or no affinity for other serotonin receptors, including 5-HT1, 5-HT1A, 5-HT1B/C, 5-HT2; for alpha1-, alpha2-, or beta-adrenoreceptors; for dopamine-D2; or for histamine-H1; benzodiazepine; picrotoxin or opioid receptors.
Serotonin receptors of the 5-HT3 type are located peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone of the area postrema. During chemotherapy that induces vomiting, mucosal enterochromaffin cells release serotonin, which stimulates 5-HT3 receptors. This evokes vagal afferent discharge, inducing vomiting. Animal studies demonstrate that, in binding to 5-HT3 receptors, granisetron blocks serotonin stimulation and subsequent vomiting after emetogenic stimuli such as cisplatin. In the ferret animal model, a single granisetron injection prevented vomiting due to high-dose cisplatin or arrested vomiting within 5 to 30 seconds.
12.2 Pharmacodynamics
The effect of granisetron on QTc prolongation was evaluated in a randomized, single-blind, positive (moxifloxacin 400 mg) - and placebo controlled parallel study in healthy subjects. A total of 120 subjects were administered SANCUSO transdermal system (n=60) or intravenous granisetron (10 mcg/kg over 30 seconds; n=60). In a study with demonstrated ability to detect small effects, the upper bound of the 90% confidence interval for the largest placebo adjusted, baseline corrected QTc based on Fridericia correction method (QTcF) for SANCUSO was below 10 ms. This study suggests that SANCUSO does not have significant effects on QT prolongation.
No evidence of an effect on plasma prolactin or aldosterone concentrations has been found in studies using granisetron.
The effect on oro-cecal transit time following application of SANCUSO has not been studied. Granisetron hydrochloride injection exhibited no effect on oro-cecal transit time in healthy subjects given a single intravenous infusion of 50 mcg/kg or 200 mcg/kg. Single and multiple oral doses of granisetron hydrochloride slowed colonic transit in healthy subjects.
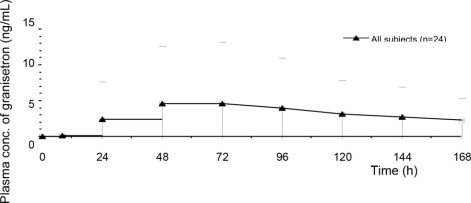
12.3 Pharmacokinetics
Absorption
Granisetron crosses intact skin into the systemic circulation by a passive diffusion process.
Following a 7-day application of SANCUSO transdermal system in 24 healthy subjects, high inter- subject variability in systemic exposure was observed. Maximal concentration was reached at approximately 48 hours (range: 24-168 hours) following application. Mean Cmax was 5 ng/mL (CV: 170%) and mean AUC0-168hr was 527 ng-hr/mL (CV: 173%).
Mean Plasma Concentration of Granisetron (mean ± SD)
Based on the measure of residual content of the transdermal system after removal, approximately 66% (SD: ± 10.9) of granisetron is delivered following transdermal system application for 7 days.
Following consecutive application of two SANCUSO transdermal systems, each for seven days, granisetron plasma concentrations were maintained over the study period with evidence of minimal accumulation. The mean plasma concentration at 24 hours after the second transdermal system application was 1.5-fold higher due to residual granisetron from the first transdermal system. As the plasma concentration increased after the second transdermal system application, the difference decreased and the mean plasma concentration at 48 hours was 1.3-fold higher after application of the second transdermal system compared to that after application of the first transdermal system.
In a study designed to assess the effect of heat on the transdermal delivery of granisetron from SANCUSO in healthy subjects, a heat pad generating an average temperature of 42°C (107.6°F) was applied over the transdermal system for 4 hours each day over the 5 day period of wear. The application of the heat pad was associated with an increase in plasma granisetron concentrations during the period of heat pad application. The elevated plasma concentration declined after removal of the heat pad. Mean Cmax with intermittent heat exposure was 6% higher than without heat. Mean partial AUCs over 6 hours with 4 hour of heat application (AUC0-6, AUC24-30, and AUC48-54) were 4.9, 1.4, and 1.1 fold higher, respectively, with heat pad than without heat pad [see Dosage and Administration (2), Warnings and Precautions (5.4)].
Distribution
Plasma protein binding is approximately 65%. Granisetron distributes freely between plasma and red blood cells.
Elimination
Metabolism
Granisetron metabolism involves N-demethylation and aromatic ring oxidation followed by conjugation. In vitro liver microsomal studies show that granisetron's major route of metabolism is inhibited by ketoconazole, suggestive of metabolism mediated by the cytochrome P-450 3A subfamily. Animal studies suggest that some of the metabolites may also have 5-HT3 receptor antagonist activity.
Use in Specific Populations
Geriatric Patients
Following application of SANCUSO transdermal system in healthy subjects, mean AUC0-z, Cmax, and Cavg were 17%, 15%, and 16% higher, respectively in male and female elderly subjects (≥ 65 years) compared to younger subjects (aged 18-45 years inclusive). These pharmacokinetic parameters were largely overlapped between the two age groups with high variability (CV: >50%).
Following a single 40 mcg/kg intravenous dose of granisetron hydrochloride in elderly subjects (mean age 71 years), lower clearance and longer half-life were observed compared to younger healthy subjects.
Male and Female Patients
There is evidence to suggest that female subjects had higher granisetron concentrations than males following transdermal system application. However, no statistically significant difference in clinical efficacy outcome was observed between males and females.
Racial or Ethnic Groups
The pharmacokinetic profile of granisetron from SANCUSO was assessed in healthy Japanese males. Following the application of a single 6-day SANCUSO 52 cm2 transdermal system, in healthy male Japanese subjects, mean Cmax, AUC(0-144), and AUC(0-∞) values were 5.02 ng/mL (CV: 66%), 492 ng.hr/mL (CV: 72%), and 562 ng.hr/mL (CV: 60%), respectively, and a median tmax value was 48 hours.
Patients with Renal Impairment
Total clearance of granisetron was not affected in patients with severe renal failure who received a single 40 mcg/kg intravenous dose of granisetron hydrochloride.
Patients with Hepatic Impairment
In patients with hepatic impairment due to neoplastic liver involvement, total plasma clearance following a single 40 mcg/kg intravenous dose of granisetron hydrochloride was approximately halved compared to patients without hepatic impairment. Given the wide variability in pharmacokinetic parameters of granisetron and the good tolerance of doses well above the recommended dose, dose adjustment in patients with hepatic functional impairment is not necessary.
Body Mass Index
In a clinical study designed to assess granisetron exposure from SANCUSO in subjects with differing levels of body fat, using body mass index (BMI) as a surrogate measure for subcutaneous fat, no significant differences were seen in the plasma pharmacokinetics of SANCUSO in male and female subjects with low BMI [<19.5 kg/m2 (males), <18.5 kg/m2 (females)] and high BMI (30.0 to 39.9 kg/m2 inclusive) compared to a control group (BMI 20.0 to 24.9 kg/m2 inclusive).
Drug Interaction Studies
Because granisetron is metabolized by hepatic cytochrome P-450 drug-metabolizing enzymes (CYP1A1 and CYP3A4), inducers or inhibitors of these enzymes may change the clearance and hence, the half-life of granisetron. In addition, the activity of the cytochrome P-450 subfamily 3A4 (involved in the metabolism of some of the main narcotic analgesic agents) is not modified by granisetron hydrochloride in vitro. In in vitro human microsomal studies, ketoconazole inhibited ring oxidation of granisetron hydrochloride. However, the clinical significance of in vivo pharmacokinetic interactions with ketoconazole is not known. In a human pharmacokinetic study, hepatic enzyme induction with phenobarbital resulted in a 25% increase in total plasma clearance of intravenous granisetron hydrochloride. The clinical significance of this change is not known.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 24-month carcinogenicity study, rats were treated orally with granisetron 1, 5 or 50 mg/kg/day (6, 30 or 300 mg/m2/day). The 50 mg/kg/day dose was reduced to 25 mg/kg/day (150 mg/m2/day) during week 59 due to toxicity. For a 50 kg person of average height (1.46 m2 body surface area), these doses represent about 2.6, 13, and 65 times the recommended clinical dose (3.1 mg/day, 2.3 mg/m2/day, delivered by the SANCUSO transdermal system, on a body surface area basis). There was a statistically significant increase in the incidence of hepatocellular carcinomas and adenomas in males treated with 5 mg/kg/day (30 mg/m2/day, about 13 times the recommended human dose with SANCUSO, on a body surface area basis) and above, and in females treated with 25 mg/kg/day (150 mg/m2/day, about 65 times the recommended human dose with SANCUSO, on a body surface area basis). No increase in liver tumors was observed at a dose of 1 mg/kg/day (6 mg/m2/day, about 2.6 times the recommended human dose with SANCUSO, on a body surface area basis) in males and 5 mg/kg/day (30 mg/m2/day, about 13 times the recommended human dose with SANCUSO, on a body surface area basis) in females.
In a 12-month oral toxicity study, treatment with granisetron 100 mg/kg/day (600 mg/m2/day, about 261 times the recommended human dose with SANCUSO, on a body surface area basis) produced hepatocellular adenomas in male and female rats while no such tumors were found in the control rats. A 24-month mouse carcinogenicity study of granisetron did not show a statistically significant increase in tumor incidence, but the study was not conclusive.
Because of the tumor findings in rat studies, SANCUSO should be prescribed only at the dose and for the indication recommended [see Indications and Usage (1), Dosage and Administration (2)].
Granisetron was not mutagenic in an in vitro Ames test and mouse lymphoma cell forward mutation assay, and in vivo mouse micronucleus test and in vitro and ex vivo rat hepatocyte UDS assays. It, however, produced a significant increase in UDS in HeLa cells in vitro and a significant increased incidence of cells with polyploidy in an in vitro human lymphocyte chromosomal aberration test.
Granisetron at subcutaneous doses up to 6 mg/kg/day (36 mg/m2/day, about 16 times the recommended human dose of SANCUSO, on a body surface area basis), and oral doses up to 100 mg/kg/day (600 mg/m2/day, about 261 times the recommended human dose of SANCUSO, on a body surface area basis) was found to have no effect on fertility and reproductive performance of male and female rats.
13.3 Phototoxicity
When tested for potential photogenotoxicity in vitro in a Chinese hamster ovary (CHO) cell line, at 200 and 300 mcg/mL, granisetron increased the percentage of cells with chromosomal aberration following photoirradiation [see Warnings and Precautions (5.5)].
Granisetron was not phototoxic when tested in vitro in a mouse fibroblast cell line. When tested in vivo in guinea-pigs, SANCUSO transdermal system did not show any potential for photoirritation or photosensitivity. No phototoxicity studies have been performed in humans.
-
14 CLINICAL STUDIES
The effectiveness of SANCUSO in the prevention of chemotherapy-induced nausea and vomiting (CINV) was evaluated in a randomized, parallel group, double-blind, double-dummy study conducted in the U.S. and abroad. The study compared the efficacy, tolerability and safety of SANCUSO transdermal system with that of 2 mg oral granisetron once daily in the prevention of nausea and vomiting in a total of 641 patients receiving multi-day chemotherapy.
The population randomized into the trial included 48% males and 52% females aged 16 to 86 years receiving moderately emetogenic (ME) or highly emetogenic (HE) multi-day chemotherapy. Seventy-eight (78%) of patients were White, 12% Asian, 10% Hispanic/Latino and 0% Black.
SANCUSO was applied 24 to 48 hours before the first dose of chemotherapy and kept in place for 7 days. Oral granisetron was administered daily for the duration of the chemotherapy regimen, 1hour before each dose of chemotherapy. Efficacy was assessed from the first administration until 24 hours after the start of the last day's administration of the chemotherapy regimen.
The primary endpoint of the trial was the proportion of patients achieving no vomiting and/or retching, no more than mild nausea and no rescue medication from the first administration until 24 hours after the start of the last day's administration of multi-day chemotherapy. Using this definition, the effect of SANCUSO was established in 60.2% of patients in the SANCUSO arm and 64.8% of patients receiving oral granisetron (difference -4.89%; 95% confidence interval – 12.91% to +3.13%).
An assessment of transdermal system adhesion in 621 patients receiving either active or placebo transdermal system showed that less than 1% of transdermal systems became detached over the course of the 7 day period of transdermal system application.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
SANCUSO (granisetron transdermal system) is a 52 cm2 thin, translucent, rectangular-shaped transdermal system with rounded corners imprinted on one side with "Granisetron 3.1 mg/24 hours". The transdermal system releases 3.1 mg of granisetron per 24 hours for up to 7 days.
Each SANCUSO transdermal system is packaged in a separate sealed foil-lined plastic pouch supplied in packages of 1 (NDC: 66220-637-31) transdermal system.
Store at 20°-25°C (68°-77°F); excursions permitted between 15°-30°C (59°-86°F). [see USP Controlled Room Temperature].
SANCUSO should be stored in the original packaging.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Progressive Ileus and Gastric Distention
Advise the patient to report new or worsening constipation to their healthcare provider and seek immediate medical care if symptoms of an ileus (pain or swelling in their abdomen) occur [see Warnings and Precautions (5.1)].
Serotonin Syndrome
Advise the patient of the possibility of serotonin syndrome with concomitant use of SANCUSO and another serotonergic agent such as medications to treat depression and migraines. Advise the patient to seek immediate medical attention if the following symptoms occur: changes in mental status, autonomic instability, neuromuscular symptoms, with or without gastrointestinal symptoms [see Warnings and Precautions (5.2)].
Skin Reactions
Instruct the patient remove the transdermal system if they have a severe skin reaction, or a generalized skin reaction (e.g. allergic rash, including erythematous, macular, papular rash or pruritus) [see Warnings and Precautions (5.3)].
Increased Drug Exposure with Use of External Heat Sources
Advise the patient to avoid prolonged exposure to heat and not to apply a heat pad or heat lamp over or near the SANCUSO transdermal system and avoid extended exposure to heat [see Warnings and Precautions (5.4)].
Phototoxicity with Ultraviolet Light Exposure
Advise the patient to avoid direct sunlight or exposure to sunlamps and to cover the application site of the transdermal system with clothing, if there is a risk of exposure to sunlight or sunlamps throughout the period of wear and for 10 days following its removal [see Warnings and Precautions (5.5)].
Application and Removal Instructions
Instruct the patient on how to apply and remove the transdermal system:
- Only wear one transdermal system at any time.
- Do not cut the transdermal system.
- Apply the transdermal system to clean, dry, nearly hairless, intact healthy skin on the upper outer arm.
- After the transdermal system is applied, wash hands thoroughly.
- Remove the transdermal system by peeling off gently from the skin.
- Upon removal, fold the used transdermal system in half with the sticky side together, and discard in household trash in a manner that prevents accidental contact or ingestion by children, pets or others.
- SANCUSO contains granisetron. Do not use other granisetron-containing products with SANCUSO [see Dosage and Administration (2)].
Manufactured by:
Kindeva Drug Delivery L.P.
Northridge, CA 91324Manufactured for:
Cumberland Pharmaceuticals Inc.
Nashville, TN 37203US Patent Number 7608282
SANCUSO® is a registered trademark of Cumberland Pharmaceuticals Inc. -
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration
Revised: 07/2024
Patient Information
SANCUSO® [san-KOO-so]
(granisetron transdermal system)
for transdermal useImportant: For skin use only. Read the Patient Information that comes with SANCUSO before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment. If you have any questions about SANCUSO, ask your healthcare provider. What is SANCUSO?
SANCUSO is a prescription medicine used to prevent nausea and vomiting in adults receiving anti-cancer (chemotherapy) treatment that causes moderate or severe vomiting.
SANCUSO is a skin patch (transdermal system) that slowly releases the medicine into your bloodstream while you wear the transdermal system.
It is not known if SANCUSO is safe and effective in children.Who should not use SANCUSO?
Do not use SANCUSO if you are allergic to granisetron or any of the ingredients in SANCUSO. See the end of this leaflet for a list of ingredients in SANCUSO.What should I tell my healthcare provider before using SANCUSO? Before using SANCUSO, tell your healthcare provider about all of your medical conditions, including if you:
- have pain or swelling in your stomach area (abdomen).
- are pregnant. It is not known if SANCUSO will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed. It is not known if SANCUSO passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements. Other medicines may affect how SANCUSO works. SANCUSO may also affect how other medicines work. SANCUSO contains granisetron. Do not take other granisetron containing products with SANCUSO.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.How should I use SANCUSO?
- Read the Instructions for Use that comes with SANCUSO transdermal system.
- Use SANCUSO exactly as your healthcare provider tells you to.
What should I avoid while using SANCUSO?
Do not apply any heat source over or near the SANCUSO transdermal system.
- A heating pad or heat lamp should not be used where the transdermal system is applied.
- You should avoid long periods of exposure to heat because heat can increase the amount of SANCUSO in your blood.
- Avoid sunlight and artificial sunlight. The medicine in SANCUSO may not work as well and may affect your skin if exposed to direct sunlight or artificial sunlight from sunlamps or tanning beds.
- Keep the transdermal system covered with clothing if you will be in direct sunlight or artificial sunlight.
- Keep the skin where SANCUSO was applied covered for another 10 days after the transdermal system is taken off to protect from exposure to direct sunlight or artificial sunlight.
What are the possible side effects of SANCUSO?
SANCUSO may cause serious side effects, including:
- Using SANCUSO may make it harder to identify certain stomach (abdomen) and bowel problems that are from other causes. Tell your healthcare provider if you have any abdominal pain or swelling while using SANCUSO.
-
Serotonin Syndrome. A potentially life-threatening problem called serotonin syndrome can happen if you use SANCUSO with certain medicines. Call your healthcare provider or go to the nearest hospital emergency room right away if you have any of the following signs and symptoms of serotonin syndrome:
- agitation
- seeing or hearing things that are not real (hallucinations)
- confusion
- coma
- fast heart beat
- changes in blood pressure
- dizziness
- sweating
- flushing
- high body temperature (hyperthermia)
- shaking (tremors), stiff muscles, or muscle twitching
- loss of coordination
- seizures
- nausea, vomiting, diarrhea
- Skin reactions. Skin reactions can happen at the transdermal system application site or outside the transdermal system application site. Tell your healthcare provider if you get any redness, rashes, bumps, blisters or itching at or near the transdermal system application site, and especially if they spread outside the place where the transdermal system was applied or if they appear outside the transdermal system application site. You may need to stop using SANCUSO.
The most common side effects of SANCUSO include:
- constipation
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of SANCUSO. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store SANCUSO?
- Store SANCUSO at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep SANCUSO in the original package it comes in.
Keep SANCUSO out of the reach of children. General information about the safe and effective use of SANCUSO.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use SANCUSO for a condition for which it was not prescribed. Do not give SANCUSO to other people, even if they have the same symptoms that you have. It may harm them. This Patient Information leaflet summarizes the most important information about SANCUSO. You can ask your pharmacist or healthcare provider for information about SANCUSO that is written for health professionals.Manufactured by:
Kindeva Drug Delivery L.P.
Northridge, CA 91324
Manufactured for:
Cumberland Pharmaceuticals Inc.
Nashville, TN 37203
For more information, go to www.sancuso.com or call 1-877-683-6110. -
INSTRUCTIONS FOR USE
Instructions for Use SANCUSO® [san-KOO-so] (granisetron transdermal system) for transdermal use
Read this Instructions for Use before you start using SANCUSO transdermal system and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
Important Information:
- SANCUSO is for skin use only (transdermal system).
- Avoid exposing the SANCUSO transdermal system application site to direct heat sources such as a heating pad or heat lamp.
- Avoid exposing the SANCUSO transdermal system to direct sunlight or artificial light such as a sunlamp or tanning bed.
- Keep the SANCUSO transdermal system covered with clothing if you will be in sunlight or artificial sunlight.
- Keep the skin where the SANCUSO transdermal system was applied covered for another 10 days after the SANCUSO transdermal system is taken off, to protect from exposure to direct sunlight or artificial sunlight.
- Skin reactions can happen at the SANCUSO transdermal system application site or outside the SANCUSO transdermal system application site. Tell your healthcare provider if you get any redness, rashes, bumps, blisters or itching at the SANCUSO transdermal system application site, and especially if they spread outside the place where the SANCUSO transdermal system was applied or if they appear outside the SANCUSO transdermal system application site. You may need to stop using the SANCUSO transdermal system.
How should I store the SANCUSO transdermal system?
- Store the SANCUSO transdermal system at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep the SANCUSO transdermal system in the original package it comes in.
- Do not open the package until you are ready to apply the SANCUSO transdermal system.
Supplies:
- SANCUSO transdermal system
- surgical or medical adhesive tape (not included)
When do I apply the SANCUSO transdermal system?
- Use the SANCUSO transdermal system exactly as your healthcare provider tells you to.
- Apply the SANCUSO transdermal system at least 1 day (24 hours) or up to 2 days (48 hours) before your scheduled anti-cancer (chemotherapy) treatment.
- Wear the SANCUSO transdermal system all the time during your chemotherapy treatment.
- Wait at least 1 day (24 hours) after your chemotherapy treatment is finished to remove the SANCUSO transdermal system.
- The SANCUSO transdermal system may be worn for up to 7 days.
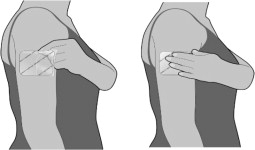
Where do I apply the SANCUSO transdermal system?
- SANCUSO transdermal system should only be applied to the outside of the upper arm.
- Apply the SANCUSO transdermal system to a clean, dry, nearly hairless, healthy area of skin on the outside part of your upper arm. If there is hair, do not shave. Instead, clip hair as close to the skin as possible.
- The area you choose should not be oily or recently shaved. The SANCUSO transdermal system should not be placed on skin that is red, irritated, or damaged (cut or scraped).
- Do not apply the SANCUSO transdermal system to areas that have been treated with creams, oils, lotions, powders or other skin products that could keep the SANCUSO transdermal system from sticking well to your skin.
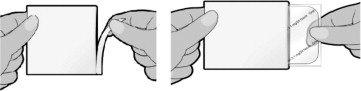
How do I apply the SANCUSO transdermal system?
The SANCUSO transdermal system comes inside a pouch which is inside the carton.
- Do not remove the SANCUSO transdermal system from the pouch until you are ready to use it.
- Do not cut the SANCUSO transdermal system into pieces.
- Remove the pouch from the carton.
- Tear the pouch open at the notch provided, and remove the SANCUSO transdermal system. Each pouch contains one SANCUSO transdermal system stuck onto a stiff (rigid) plastic film.
- The unprinted, sticky side of the SANCUSO transdermal system is covered by a 2-piece stiff (rigid) plastic film. Bend the transdermal system in the middle. Slowly peel 1-half of the stiff (rigid) plastic film. Be careful not to stick the SANCUSO transdermal system to itself. Do not touch the sticky side of the SANCUSO transdermal system.
- While holding the other half of the stiff (rigid) plastic film, apply the sticky half of the SANCUSO transdermal system to your skin. Remove the second half of the stiff (rigid) plastic film and press the whole SANCUSO transdermal system firmly in place and smooth it down with your fingers. Press firmly making sure the SANCUSO transdermal system sticks well to the skin, especially around the edges.
- Wash your hands with soap and water right away after applying the SANCUSO transdermal system to remove any medicine that may have stuck to your fingers.
- Keep the SANCUSO transdermal system in place for the whole time you are receiving your chemotherapy treatment. Remove the SANCUSO transdermal system at least 1 day (24 hours) after your chemotherapy treatment is finished. The SANCUSO transdermal system can be worn for up to 7 days, depending on the number of days your chemotherapy treatment lasts.
- Do not re-use the SANCUSO transdermal system after you remove it. See the instructions below on the right way to remove and throw away the SANCUSO transdermal system.
What do I do if the SANCUSO transdermal system does not stick well?
If the SANCUSO transdermal system does not stick well or the edges lift off the skin, you may apply pieces of surgical or medical adhesive tape on each lifted edge to keep the SANCUSO transdermal system in place. Only place pieces of the surgical or medical adhesive tape on the edges of the SANCUSO transdermal system. Do not completely cover the SANCUSO transdermal system with surgical or medical adhesive tape and do not wrap completely around your arm. If the SANCUSO transdermal system comes more than half off or it becomes damaged (e.g. rips), contact your healthcare provider.
Can I bathe or shower while wearing the SANCUSO transdermal system?
You can continue to shower and wash normally while wearing the SANCUSO transdermal system.
It is not known how other activities, for example swimming, strenuous exercise or using a sauna or whirlpool, may affect the SANCUSO transdermal system. Avoid these activities while wearing the SANCUSO transdermal system.
How do I remove and dispose of the SANCUSO transdermal system?
- When you remove the SANCUSO transdermal system, peel it off gently.
- The used SANCUSO transdermal system will still contain some of the medicine. After removing the used SANCUSO transdermal system, fold it in half so that the sticky side sticks to itself. Throw away the used SANCUSO transdermal system in the trash right away so that children and pets cannot reach it.
- If any adhesive (glue) remains on your skin after you remove the SANCUSO transdermal system, wash the area with soap and water to remove it. Do not use alcohol or other dissolving liquids, such as nail polish remover. These may cause skin irritation.
- Wash your hands with soap and water after handling the SANCUSO transdermal system.
- You may see mild redness on the skin where the SANCUSO transdermal system is removed. This redness should go away within 3 days. If redness continues, tell your healthcare provider.
What are the ingredients in the SANCUSO transdermal system?
Active ingredient: granisetron.
Inactive ingredients: acrylate-vinylacetate copolymer, polyester, titanium dioxide, polyamide resin and polyethylene wax. This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured by:
Kindeva Drug Delivery L.P.
Northridge, CA 91324Manufactured for:
Cumberland Pharmaceuticals Inc., Nashville, TN 37203Revised: 07/2024
-
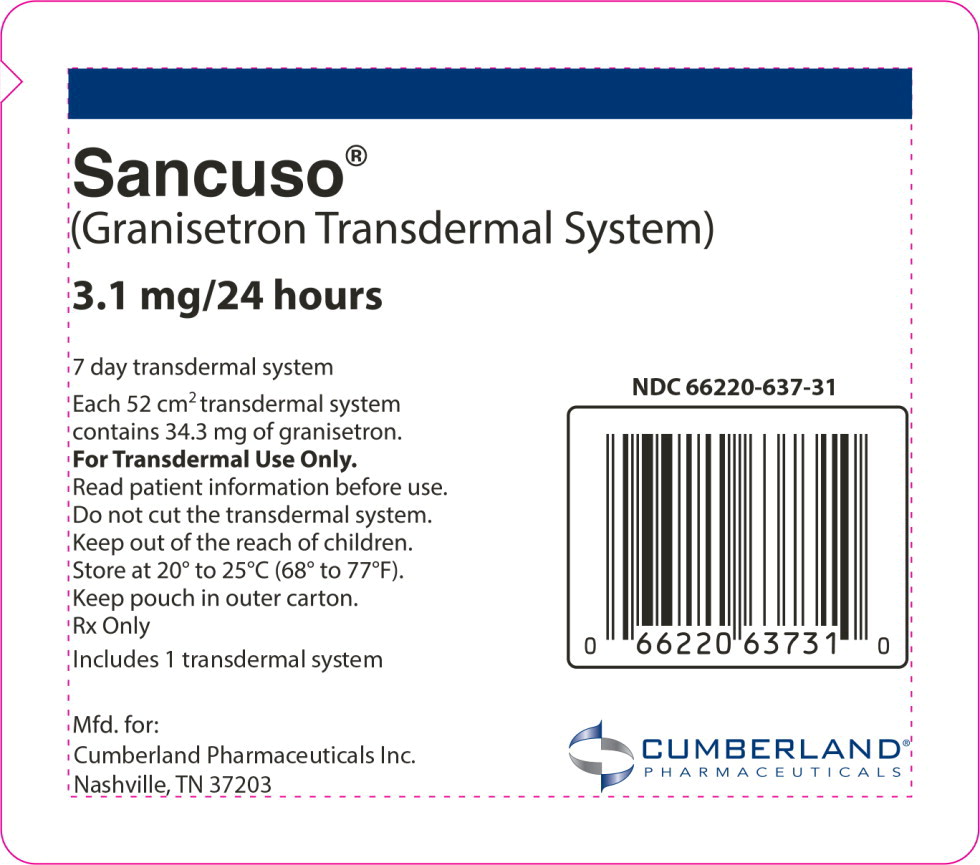
PRINCIPAL DISPLAY PANEL
Principal Display Panel – 168 h Pouch Label
Sancuso®
(Granisetron Transdermal System)
3.1 mg/24 hours
NDC: 66220-637-31
7 day transdermal system
Each 52 cm2 transdermal system
contains 34.3 mg of granisetron.For Transdermal Use Only.
Read patient information before use.
Do not cut the transdermal system.
Keep out of the reach of children.
Store at 20° to 25°C (68° to 77°F).
Keep pouch in outer carton.
Rx OnlyIncludes 1 transdermal system
Mfd. for:
Cumberland Pharmaceuticals Inc.
Nashville, TN 37203
CUMBERLAND®
PHARMACEUTICALS -
INGREDIENTS AND APPEARANCE
SANCUSO
granisetron patchProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 66220-637 Route of Administration TRANSDERMAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength granisetron (UNII: WZG3J2MCOL) (granisetron - UNII:WZG3J2MCOL) granisetron 3.1 mg in 24 h Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 66220-637-31 168 h in 1 POUCH; Type 0: Not a Combination Product 07/16/2024 2 NDC: 66220-637-72 168 h in 1 POUCH; Type 0: Not a Combination Product 07/16/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA022198 07/16/2024 Labeler - Cumberland Pharmaceuticals Inc. (069532880)
Trademark Results [SANCUSO]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SANCUSO 79064017 3744866 Live/Registered |
Kyowa Kirin, Inc. 2008-12-19 |
 SANCUSO 76460343 2814630 Live/Registered |
STRAKAN INTERNATIONAL S.A. 2002-10-17 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.