PROQUAD- measles, mumps, rubella and varicella virus vaccine live injection, powder, lyophilized, for suspension
ProQuad by
Drug Labeling and Warnings
ProQuad by is a Other medication manufactured, distributed, or labeled by Merck Sharp & Dohme Corp.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ProQuad safely and effectively. See full prescribing information for ProQuad.
ProQuad®
Measles, Mumps, Rubella and Varicella Virus Vaccine Live
Suspension for subcutaneous injection
Initial U.S. Approval: 2005RECENT MAJOR CHANGES
Warnings and Precautions Risk of Vaccine Virus Transmission (5.8) 03/2020 INDICATIONS AND USAGE
ProQuad is a vaccine indicated for active immunization for the prevention of measles, mumps, rubella, and varicella in children 12 months through 12 years of age. (1)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
- History of anaphylactic reaction to neomycin or hypersensitivity to gelatin or any other component of the vaccine. (4.1)
- Primary or acquired immunodeficiency states. (4.2)
- Family history of congenital or hereditary immunodeficiency. (4.2)
- Immunosuppressive therapy. (4.2, 7.3)
- Active untreated tuberculosis or febrile illness (>101.3°F or >38.5°C). (4.3)
- Pregnancy. (4.4, 8.1, 17)
WARNINGS AND PRECAUTIONS
- Administration of ProQuad (dose 1) to children 12 to 23 months old who have not been previously vaccinated against measles, mumps, rubella, or varicella, nor had a history of the wild-type infections, is associated with higher rates of fever and febrile seizures at 5 to 12 days after vaccination when compared to children vaccinated with M-M-R® II and VARIVAX® administered separately. (5.1, 6.1, 6.3)
- Use caution when administering ProQuad to children with a history of cerebral injury or seizures or any other condition in which stress due to fever should be avoided. (5.2)
- Use caution when administering ProQuad to children with anaphylaxis or immediate hypersensitivity to eggs (5.3) or contact hypersensitivity to neomycin. (5.4)
- Use caution when administering ProQuad to children with thrombocytopenia. (5.5)
- Avoid close contact with high-risk individuals susceptible to varicella because of possible transmission of varicella vaccine virus. (5.8)
- Defer vaccination for at least 3 months following blood or plasma transfusions, or administration of immune globulins (IG). (5.9, 7.1)
- Avoid using salicylates for 6 weeks after vaccination with ProQuad. (5.10, 7.2, 17)
- Avoid pregnancy for 3 months following vaccination with measles, mumps, rubella, and/or varicella vaccines. (8.1, 17)
ADVERSE REACTIONS
- The most frequent vaccine-related adverse events reported in ≥5% of subjects vaccinated with ProQuad were:
- injection-site reactions (pain/tenderness/soreness, erythema, and swelling)
- fever
- irritability. (6.1)
- Systemic vaccine-related adverse events that were reported at a significantly greater rate in recipients of ProQuad than in recipients of the component vaccines administered concomitantly were:
- fever
- measles-like rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877-888-4231 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov.
DRUG INTERACTIONS
- Tuberculin testing should be administered anytime before, simultaneously with, or at least 4 to 6 weeks after ProQuad. (7.4)
- ProQuad may be administered concomitantly with Haemophilus influenzae type b conjugate vaccine and/or hepatitis B vaccine at separate injection sites. (7.5)
- ProQuad may be administered concomitantly with pneumococcal 7-valent conjugate vaccine and/or hepatitis A vaccine (inactivated) at separate injection sites. (7.5)
USE IN SPECIFIC POPULATIONS
Pregnancy: Do not administer ProQuad to females who are pregnant. Pregnancy should be avoided for 3 months following vaccination with ProQuad. (4.4, 8.1, 17)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose and Schedule
2.2 Preparation for Administration
2.3 Method of Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Immunosuppression
4.3 Concurrent Illness
4.4 Pregnancy
5 WARNINGS AND PRECAUTIONS
5.1 Fever and Febrile Seizures
5.2 History of Cerebral Injury or Seizures
5.3 Hypersensitivity to Eggs
5.4 Contact Hypersensitivity to Neomycin
5.5 Thrombocytopenia
5.6 Use for Post-Exposure Prophylaxis
5.7 Use in HIV-Infected Children
5.8 Risk of Vaccine Virus Transmission
5.9 Immune Globulins and Transfusions
5.10 Salicylate Therapy
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
6.3 Post-Marketing Observational Safety Surveillance Study
7 DRUG INTERACTIONS
7.1 Immune Globulins and Transfusions
7.2 Salicylates
7.3 Corticosteroids and Immunosuppressive Drugs
7.4 Drug/Laboratory Test Interactions
7.5 Use with Other Vaccines
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.6 Persistence of Antibody Responses after Vaccination
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose and Schedule
FOR SUBCUTANEOUS ADMINISTRATION ONLY
Each 0.5-mL dose of ProQuad is administered subcutaneously.
The first dose is usually administered at 12 to 15 months of age but may be given anytime through 12 years of age.
If a second dose of measles, mumps, rubella, and varicella vaccine is needed, ProQuad may be used. This dose is usually administered at 4 to 6 years of age. At least 1 month should elapse between a dose of a measles-containing vaccine such as M-M-R® II (measles, mumps, and rubella virus vaccine live) and a dose of ProQuad. At least 3 months should elapse between a dose of varicella-containing vaccine and ProQuad.
2.2 Preparation for Administration
CAUTION: Preservatives, antiseptics, detergents, and other anti-viral substances may inactivate the vaccine. Use only sterile syringes that are free of preservatives, antiseptics, detergents, and other anti-viral substances for reconstitution and injection of ProQuad.
Withdraw the entire volume of the supplied diluent into a syringe. Use only the diluent supplied with the vaccine since it is free of preservatives or other anti-viral substances.
Inject the entire content of the syringe into the vial containing the powder. Gently agitate to dissolve completely.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Visually inspect the vaccine before and after reconstitution prior to administration. Before reconstitution, the lyophilized vaccine is a white to pale yellow compact crystalline plug. ProQuad, when reconstituted, is a clear pale yellow to light pink liquid.
Withdraw the entire amount of the reconstituted vaccine from the vial into the same syringe, inject the entire volume, and discard vial.
TO MINIMIZE LOSS OF POTENCY, THE VACCINE SHOULD BE ADMINISTERED IMMEDIATELY AFTER RECONSTITUTION. IF NOT USED IMMEDIATELY, THE RECONSTITUTED VACCINE MAY BE STORED AT ROOM TEMPERATURE, PROTECTED FROM LIGHT, FOR UP TO 30 MINUTES. DISCARD RECONSTITUTED VACCINE IF IT IS NOT USED WITHIN 30 MINUTES.
2.3 Method of Administration
Inject the vaccine subcutaneously into the outer aspect of the deltoid region of the upper arm or into the higher anterolateral area of the thigh.
Use With Other Vaccines
Use different injection sites to administer each vaccine if other vaccines are administered concomitantly. [See Drug Interactions (7.5).]
-
3 DOSAGE FORMS AND STRENGTHS
ProQuad is a suspension for injection supplied as a 0.5-mL single dose vial of lyophilized vaccine to be reconstituted using the sterile diluent supplied [see How Supplied/Storage and Handling (16)].
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Do not administer ProQuad to individuals with a history of anaphylactic reactions to neomycin. If vaccination with ProQuad is medically necessary for such individuals, they are advised to consult an allergist or immunologist and should receive ProQuad only in settings where anaphylactic reactions can be appropriately managed.
Do not administer ProQuad to individuals with a history of hypersensitivity to gelatin or any other component of the vaccine or following previous vaccination with ProQuad, VARIVAX® (varicella virus vaccine live), or any measles-, mumps-, or rubella-containing vaccine [see Description (11) and Warnings and Precautions (5) for exceptions].
4.2 Immunosuppression
Do not administer ProQuad to individuals with blood dyscrasias, leukemia, lymphomas of any type, or other malignant neoplasms affecting the bone marrow or lymphatic system; or to individuals on immunosuppressive therapy (including high-dose systemic corticosteroids) [see Drug Interactions (7.3)]. Vaccination with a live, attenuated vaccine, such as varicella, can result in a more extensive vaccine-associated rash or disseminated disease in individuals on immunosuppressive drugs. ProQuad may be used by individuals who are receiving topical corticosteroids or low-dose corticosteroids, as are commonly used for asthma prophylaxis or in patients who are receiving corticosteroids as replacement therapy, e.g., for Addison's disease.
Do not administer ProQuad to individuals with primary and acquired immunodeficiency states, including AIDS or other clinical manifestations of infection with human immunodeficiency viruses; cellular immune deficiencies; and hypogammaglobulinemic and dysgammaglobulinemic states. Measles inclusion body encephalitis, pneumonitis, and death as a direct consequence of disseminated measles vaccine virus infection have been reported in severely immunocompromised individuals inadvertently vaccinated with measles-containing vaccine. In addition, disseminated varicella vaccine virus infection has been reported in children with underlying immunodeficiency disorders who were inadvertently vaccinated with a varicella-containing vaccine {1}.
Do not administer ProQuad to individuals with a family history of congenital or hereditary immunodeficiency, unless the immune competence of the potential vaccine recipient is demonstrated.
4.3 Concurrent Illness
Do not administer ProQuad to individuals with active untreated tuberculosis or to individuals with an active febrile illness with fever >101.3°F (>38.5°C).
4.4 Pregnancy
Do not administer ProQuad to individuals who are pregnant because the effects of the vaccine on fetal development are unknown. If vaccination of postpubertal females is undertaken, pregnancy should be avoided for three months following administration of ProQuad [see Use in Specific Populations (8.1) and Patient Counseling Information (17)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Fever and Febrile Seizures
Administration of ProQuad (dose 1) to children 12 to 23 months old who have not been previously vaccinated against measles, mumps, rubella, or varicella, nor had a history of the wild-type infections, is associated with higher rates of fever and febrile seizures at 5 to 12 days after vaccination when compared to children vaccinated with dose 1 of both M-M-R II and VARIVAX administered separately [see Adverse Reactions (6.3)].
5.2 History of Cerebral Injury or Seizures
Exercise caution when administering ProQuad to persons with a history of cerebral injury, individual or family history of convulsions, or any other condition in which stress due to fever should be avoided. Healthcare providers should be alert to the temperature elevations that may occur following vaccination.
5.3 Hypersensitivity to Eggs
Live measles vaccine and live mumps vaccine are produced in chick embryo cell culture. Persons with a history of anaphylactic or other immediate hypersensitivity reactions (e.g., hives, swelling of the mouth and throat, difficulty breathing, hypotension, or shock) subsequent to egg ingestion may be at an enhanced risk of immediate-type hypersensitivity reactions after receiving vaccines containing traces of chick embryo antigen. Carefully evaluate the potential risk-to-benefit ratio before considering vaccination in such cases. Such individuals may be vaccinated with extreme caution; adequate treatment should be readily available should a reaction occur [see Contraindications (4.1)] {2}.
Children with egg allergy are at low risk for anaphylactic reactions to measles-containing vaccines (including M-M-R II), and skin testing of children allergic to eggs is not predictive of reactions to M-M-R II vaccine. Persons with allergies to chickens or feathers are not at increased risk of reaction to the vaccine {2}.
5.4 Contact Hypersensitivity to Neomycin
Most often, neomycin allergy manifests as a contact dermatitis, which is not a contraindication to receiving measles-, mumps-, rubella-, or varicella-containing vaccine.
5.5 Thrombocytopenia
Carefully evaluate the potential risk-to-benefit ratio before considering vaccination with ProQuad in children with thrombocytopenia or in those who experienced thrombocytopenia after vaccination with a previous dose of measles, mumps, rubella, and/or varicella vaccine. No clinical data are available regarding the development or worsening of thrombocytopenia in individuals vaccinated with ProQuad. Cases of thrombocytopenia have been reported after primary vaccination with measles vaccine; measles, mumps, and rubella vaccine; after varicella vaccination; and following re-vaccination with measles vaccine or M-M-R II [see Adverse Reactions (6.2)].
5.6 Use for Post-Exposure Prophylaxis
The safety and efficacy of ProQuad for use after exposure to measles, mumps, rubella, or varicella have not been established.
5.7 Use in HIV-Infected Children
The safety and efficacy of ProQuad for use in children known to be infected with human immunodeficiency viruses have not been established.
5.8 Risk of Vaccine Virus Transmission
Post-licensing experience suggests that transmission of varicella vaccine virus (Oka/Merck) resulting in varicella infection including disseminated disease may occur rarely between vaccine recipients (who develop or do not develop a varicella-like rash) and contacts susceptible to varicella including healthy as well as high-risk individuals.
High-risk individuals susceptible to varicella include:
- Immunocompromised individuals;
- Pregnant women without documented positive history of varicella (chickenpox) or laboratory evidence of prior infection;
- Newborn infants of mothers without documented positive history of varicella or laboratory evidence of prior infection and all newborn infants born at <28 weeks gestation regardless of maternal varicella immunity.
Vaccine recipients should attempt to avoid, to the extent possible, close association with high-risk individuals susceptible to varicella for up to 6 weeks following vaccination. In circumstances where contact with high-risk individuals susceptible to varicella is unavoidable, the potential risk of transmission of the varicella vaccine virus should be weighed against the risk of acquiring and transmitting wild-type varicella virus.
Excretion of small amounts of the live, attenuated rubella virus from the nose or throat has occurred in the majority of susceptible individuals 7 to 28 days after vaccination. There is no confirmed evidence to indicate that such virus is transmitted to susceptible persons who are in contact with the vaccinated individuals. Consequently, transmission through close personal contact, while accepted as a theoretical possibility, is not regarded as a significant risk. However, transmission of the rubella vaccine virus to infants via breast milk has been documented [see Use in Specific Populations (8.2)].
There are no reports of transmission of the more attenuated Enders' Edmonston strain of measles virus or the Jeryl Lynn™ strain of mumps virus from vaccine recipients to susceptible contacts.
5.9 Immune Globulins and Transfusions
Immune globulins (IG) administered concomitantly with ProQuad contain antibodies that may interfere with vaccine virus replication and decrease the expected immune response. Vaccination should be deferred for at least 3 months following blood or plasma transfusions, or administration of IG.
The appropriate suggested interval between transfusion or IG administration and vaccination will vary with the type of transfusion or indication for, and dose of, IG (e.g., 5 months for Varicella Zoster Immune Globulin [VZIG]) {2}. Following administration of ProQuad, any IG including VZIG should not be given for 1 month thereafter unless its use outweighs the benefits of vaccination {2}. [See Drug Interactions (7.1).]
5.10 Salicylate Therapy
Avoid the use of salicylates (aspirin) or salicylate-containing products in children and adolescents 12 months through 12 years of age, for six weeks following vaccination with ProQuad due to the association of Reye syndrome with aspirin therapy and wild-type varicella infection. [See Drug Interactions (7.2) and Patient Counseling Information (17).]
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. Vaccine-related adverse reactions reported during clinical trials were assessed by the study investigators to be possibly, probably, or definitely vaccine-related and are summarized below.
Children 12 Through 23 Months of Age Who Received a Single Dose of ProQuad
ProQuad was administered to 4497 children 12 through 23 months of age involved in 4 randomized clinical trials without concomitant administration with other vaccines. The safety of ProQuad was compared with the safety of M-M-R II and VARIVAX given concomitantly (N=2038) at separate injection sites. The safety profile for ProQuad was similar to the component vaccines. Children in these studies were monitored for up to 42 days postvaccination using vaccination report card-aided surveillance. Safety follow-up was obtained for 98% of children in each group. Few subjects (<0.1%) who received ProQuad discontinued the study due to an adverse reaction. The race distribution of the study subjects across these studies following a first dose of ProQuad was as follows: 65.2% White; 13.1% African-American; 11.1% Hispanic; 5.8% Asian/Pacific; 4.5% other; and 0.2% American Indian. The racial distribution of the control group was similar to that of the group who received ProQuad. The gender distribution across the studies following a first dose of ProQuad was 52.5% male and 47.5% female. The gender distribution of the control group was similar to that of the group who received ProQuad. Vaccine-related injection-site and systemic adverse reactions observed among recipients of ProQuad or M-M-R II and VARIVAX at a rate of at least 1% are shown in Table 1. Systemic vaccine-related adverse reactions that were reported at a significantly greater rate in individuals who received a first dose of ProQuad than in individuals who received first doses of M-M-R II and VARIVAX concomitantly at separate injection sites were fever (≥102°F [≥38.9°C] oral equivalent or abnormal) (21.5% versus 14.9%, respectively, risk difference 6.6%, 95% CI: 4.6, 8.5), and measles-like rash (3.0% versus 2.1%, respectively, risk difference 1.0%, 95% CI: 0.1, 1.8). Both fever and measles-like rash usually occurred within 5 to 12 days following the vaccination, were of short duration, and resolved with no long-term sequelae. Pain/tenderness/soreness at the injection site was reported at a statistically lower rate in individuals who received ProQuad than in individuals who received M-M-R II and VARIVAX concomitantly at separate injection sites (22.0% versus 26.8%, respectively, risk difference -4.8%, 95% CI: -7.1, -2.5). The only vaccine-related injection-site adverse reaction that was more frequent among recipients of ProQuad than recipients of M-M-R II and VARIVAX was rash at the injection site (2.4% versus 1.6%, respectively, risk difference 0.9%, 95% CI: 0.1, 1.5).
Table 1: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad Dose 1 or M-M-R II and VARIVAX at 12 to 23 Months of Age (0 to 42 Days Postvaccination) ProQuad
(N=4497)M-M-R II and VARIVAX
(N=2038)Adverse Reactions (n=4424)
%(n=1997)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * Injection-site adverse reactions for M-M-R II and VARIVAX are based on occurrence with either of the vaccines administered.
- † Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 0 to 4 postvaccination.
- ‡ Temperature reported as elevated (≥102°F, oral equivalent) or abnormal.
Injection Site* Pain/tenderness/soreness† 22.0 26.7 Erythema† 14.4 15.8 Swelling† 8.4 9.8 Ecchymosis 1.5 2.3 Rash 2.3 1.5 Systemic Fever†,‡ 21.5 14.9 Irritability 6.7 6.7 Measles-like rash† 3.0 2.1 Varicella-like rash† 2.1 2.2 Rash (not otherwise specified) 1.6 1.4 Upper respiratory infection 1.3 1.1 Viral exanthema 1.2 1.1 Diarrhea 1.2 1.3 Rubella-like rashes were observed in <1% of subjects following a first dose of ProQuad.
In these clinical trials, two cases of herpes zoster were reported among 2108 healthy subjects 12 through 23 months of age who were vaccinated with their first dose of ProQuad and followed for 1 year. Both cases were unremarkable and no sequelae were reported.
Children 15 to 31 Months of Age Who Received a Second Dose of ProQuad
In 5 clinical trials, 2780 healthy children were vaccinated with ProQuad (dose 1) at 12 to 23 months of age and then administered a second dose approximately 3 to 9 months later. The race distribution of the study subjects across these studies following a second dose of ProQuad was as follows: 64.4% White; 14.1% African-American; 12.0% Hispanic; 5.9% other; 3.5% Asian/Pacific; and 0.1% American Indian. The gender distribution across the studies following a second dose of ProQuad was 51.5% male and 48.5% female. Children in these open-label studies were monitored for at least 28 days postvaccination using vaccination report card-aided surveillance. Safety follow-up was obtained for approximately 97% of children overall. Vaccine-related injection-site and systemic adverse reactions observed after Dose 1 and 2 of ProQuad at a rate of at least 1% are shown in Table 2. In these trials, the overall rates of systemic adverse reactions after ProQuad (dose 2) were comparable to, or lower than, those seen with the first dose. In the subset of children who received both ProQuad dose 1 and dose 2 in these trials (N=2408) with follow-up for fever, fever ≥102.2°F (≥38.9°C) was observed significantly less frequently days 1 to 28 after the second dose (10.8%) than after the first dose (19.1%) (risk difference 8.3%, 95% CI: 6.4, 10.3). Fevers ≥102.2°F (≥38.9°C) days 5 to 12 after vaccinations were also reported significantly less frequently after dose 2 (3.9%) than after dose 1 (13.6%) (risk difference 9.7%, 95% CI: 8.1, 11.3). In the subset of children who received both doses and for whom injection-site reactions were reported (N=2679), injection-site erythema was noted significantly more frequently after ProQuad (dose 2) as compared to ProQuad (dose 1) (12.6% and 10.8%, respectively, risk difference -1.8, 95% CI: -3.3, -0.3); however, pain and tenderness at the injection site was significantly lower after dose 2 (16.1%) as compared with after dose 1 (21.9%) (risk difference, 5.8%, 95% CI: 4.1, 7.6). Two children had febrile seizures after ProQuad (dose 2); both febrile seizures were thought to be related to a concurrent viral illness [see Adverse Reactions (6.3) and Clinical Studies (14)]. These studies were not designed or statistically powered to detect a difference in rates of febrile seizure between recipients of ProQuad as compared to M-M-R II and VARIVAX. The risk of febrile seizure has not been evaluated in a clinical study comparing the incidence rate after ProQuad (dose 2) with the incidence rate after concomitant M-M-R II (dose 2) and VARIVAX (dose 2). [See Adverse Reactions (6.1), Children 4 to 6 Years of Age Who Received ProQuad After Primary Vaccination with M-M-R II and VARIVAX.]
Table 2: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad Dose 1 at 12 to 23 Months of Age and Dose 2 at 15 to 31 Months of Age (1 to 28 Days Postvaccination) ProQuad
Dose 1ProQuad
Dose 2Adverse Reactions (N=3112)
(n=3019)
%(N=2780)
(n=2695)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 1 to 5 postvaccination.
- † Temperature reported as elevated or abnormal.
Injection-Site Pain/tenderness/soreness* 21.4 15.9 Erythema* 10.7 12.4 Swelling* 8.0 8.5 Injection-site bruising 1.1 0.0 Systemic Fever*,† 20.4 8.3 Irritability 6.0 2.4 Measles-like/Rubella-like rash 4.3 0.9 Varicella-like/Vesicular rash 1.5 0.1 Diarrhea 1.3 0.6 Upper respiratory infection 1.3 1.4 Rash (not otherwise specified) 1.2 0.6 Rhinorrhea 1.1 1.0 Children 4 to 6 Years of Age Who Received ProQuad After Primary Vaccination with M-M-R II and VARIVAX
In a double-blind clinical trial, 799 healthy 4- to 6-year-old children who received M-M-R II and VARIVAX at least 1 month prior to study entry were randomized to receive ProQuad and placebo (N=399), M-M-R II and placebo concomitantly (N=205) at separate injection sites, or M-M-R II and VARIVAX (N=195) concomitantly at separate injection sites [see Clinical Studies (14)]. Children in these studies were monitored for up to 42 days postvaccination using vaccination report card-aided surveillance. Safety follow-up was obtained for >98% of children in each group. The race distribution of the study subjects following a dose of ProQuad was as follows: 78.4% White; 12.3% African-American; 3.8% Hispanic; 3.5% other; and 2.0% Asian/Pacific. The gender distribution following a dose of ProQuad was 52.1% male and 47.9% female. Injection-site and systemic adverse reactions observed after Dose 1 and 2 of ProQuad at a rate of at least 1% are shown in Table 3. [See Clinical Studies (14).]
Table 3: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Previously Vaccinated with M-M-R II and VARIVAX Who Received ProQuad + Placebo, M-M-R II + Placebo, or M-M-R II + VARIVAX at 4 to 6 Years of Age (1 to 43 Days Postvaccination)
Adverse ReactionsProQuad + Placebo
(N=399)
(n=397)
%M-M-R II + Placebo
(N=205)
(n=205)
%M-M-R II + VARIVAX
(N=195)
(n=193)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 1 to 5 postvaccination.
- † Temperature reported as elevated (≥102°F, oral equivalent) or abnormal.
Systemic Fever*,† 2.5 2.0 4.1 Cough 1.3 0.5 0.5 Irritability 1.0 0.5 1.0 Headache 0.8 1.5 1.6 Rhinorrhea 0.5 1.0 0.5 Nasopharyngitis 0.3 1.0 1.0 Vomiting 0.3 1.0 0.5 Upper respiratory infection 0.0 0.0 1.0 ProQuad
%Placebo
%M-M-R II
%Placebo
%M-M-R II
%VARIVAX
%Injection-Site Pain* 41.1 34.5 36.6 34.1 35.2 36.8 Erythema* 24.4 13.4 15.6 14.1 14.5 15.5 Swelling* 15.6 8.1 10.2 8.8 7.8 10.9 Bruising 3.5 3.8 2.4 3.4 1.6 2.1 Rash 1.5 1.3 0.0 0.0 0.5 0.0 Pruritus 1.0 0.3 0.0 0.0 0.0 1.0 Nodule 0.0 0.0 0.0 0.0 0.0 1.0 Safety in Trials That Evaluated Concomitant Use with Other Vaccines
ProQuad Administered with Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine
In an open-label clinical trial, 1434 children were randomized to receive ProQuad given with diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (DTaP) and Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccine concomitantly (N=949) or non-concomitantly with ProQuad given first and the other vaccines 6 weeks later (N=485). No clinically significant differences in adverse events were reported between treatment groups [see Clinical Studies (14)]. The race distribution of the study subjects who received ProQuad was as follows: 70.7% White; 10.9% Asian/Pacific; 10.7% African-American; 4.5% Hispanic; 3.0% other; and 0.2% American Indian. The gender distribution of the study subjects who received ProQuad was 53.6% male and 46.4% female.
ProQuad Administered with Pneumococcal 7-valent Conjugate Vaccine and/or Hepatitis A Vaccine, Inactivated
In an open-label clinical trial, 1027 healthy children 12 to 23 months of age were randomized to receive ProQuad (dose 1) and pneumococcal 7-valent conjugate vaccine (dose 4) concomitantly (N=510) or non-concomitantly at different clinic visits (N=517). The race distribution of the study subjects was as follows: 65.2% White; 15.1% African-American; 10.0% Hispanic; 6.6% other; and 3.0% Asian/Pacific. The gender distribution of the study subjects was 54.5% male and 45.5% female. Injection-site and systemic adverse reactions observed among recipients of ProQuad administered concomitantly or non-concomitantly with pneumococcal 7-valent conjugate vaccine at a rate of at least 1% are shown in Table 4. No clinically significant differences in adverse reactions were reported between the concomitant and non-concomitant treatment groups [see Clinical Studies (14)].
Table 4: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad (dose 1) Concomitantly or Non-Concomitantly with PCV7* (dose 4) at the First Visit (1 to 28 Days Postvaccination)
Adverse ReactionsProQuad + PCV7
(N=510)
(n=498)
%PCV7
(N=258)
(n=250)
%ProQuad
(N=259)
(n=255)
%N/A = Not applicable.
N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * PCV7 = Pneumococcal 7-valent conjugate vaccine, dose 4.
- † Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 1 to 5 postvaccination.
- ‡ Temperature reported as elevated (≥102°F, oral equivalent) or abnormal.
Injection-Site - ProQuad Pain† 24.9 N/A 24.7 Erythema† 12.4 N/A 11.0 Swelling† 10.8 N/A 7.5 Bruising 2.0 N/A 1.6 Injection-Site - PCV7 Pain† 30.5 29.6 N/A Erythema† 21.1 24.4 N/A Swelling† 17.9 20.0 N/A Bruising 1.6 1.2 N/A Systemic Fever†,‡ 15.5 10.0 15.3 Measles-like rash 4.4 0.8 5.1 Irritability 3.8 3.6 3.5 Upper respiratory infection 1.6 0.8 1.2 Varicella-like/vesicular rash 1.6 0.0 1.2 Diarrhea 0.8 1.2 1.2 Vomiting 0.6 0.8 1.2 Rash 0.4 0.0 1.2 Somnolence 0.0 0.0 1.2 In an open-label clinical trial, 699 healthy children 12 to 23 months of age were randomized to receive 2 doses of VAQTA® (hepatitis A vaccine, inactivated) (N=352) or 2 doses of VAQTA concomitantly with 2 doses of ProQuad (N=347) at least 6 months apart. An additional 1101 subjects received 2 doses of VAQTA alone at least 6 months apart (non-randomized), resulting in 1453 subjects receiving 2 doses of VAQTA alone (1101 non-randomized and 352 randomized) and 347 subjects receiving 2 doses of VAQTA concomitantly with ProQuad (all randomized). The race distribution of the study subjects following a dose of ProQuad was as follows: 47.3% White; 42.7% Hispanic; 5.5% other; 2.9% African-American; and 1.7% Asian/Pacific. The gender distribution of the study subjects following a dose of ProQuad was 49.3% male and 50.7% female. Vaccine-related injection-site adverse reactions (days 1 to 5 postvaccination) and systemic adverse events (days 1 to 14 post VAQTA and days 1 to 28 post ProQuad vaccination) observed among recipients of VAQTA and ProQuad administered concomitantly with VAQTA at a rate of at least 1% are shown in Tables 5 and 6, respectively. In addition, among the randomized cohort, in the 14 days after each vaccination, the rates of fever (including all vaccine- and non-vaccine-related reports) were significantly higher in subjects who received ProQuad with VAQTA concomitantly after dose 1 (22.0%) as compared to subjects given dose 1 of VAQTA without ProQuad (10.8%). However, rates of fever were not significantly higher in subjects who received ProQuad with VAQTA concomitantly after dose 2 (12.5%) as compared to subjects given dose 2 of VAQTA without ProQuad (9.4%). In post-hoc analyses, these rates were significantly different for dose 1 (relative risk (RR) 2.03 [95% CI: 1.42, 2.94]), but not dose 2 (RR 1.32 [95% CI: 0.82, 2.13]). Rates of injection-site adverse reactions and other systemic adverse events were lower following a second dose than following the first dose of both vaccines given concomitantly.
Table 5: Vaccine-Related Injection-Site Adverse Reactions Reported in ≥1% of Children Who Received VAQTA or ProQuad Concomitantly with VAQTA 1 to 5 Days After Vaccination with VAQTA or VAQTA and ProQuad Dose 1 Dose 2
Adverse ReactionsVAQTA
(N=1453)
(n=1412)
%ProQuad + VAQTA
(N=347)
(n=328)
%VAQTA
(N=1301)
(n=1254)
%ProQuad + VAQTA
(N=292)
(n=264)
%N/A = Not applicable.
N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 1 to 5 postvaccination.
Injection-Site - VAQTA Pain/tenderness* 29.2 27.1 30.1 25.0 Erythema* 13.5 12.5 14.3 11.7 Swelling* 7.1 9.1 9.0 8.0 Injection-site bruising 1.9 2.4 1.0 0.8 Injection-Site - ProQuad Pain/tenderness* N/A 30.5 N/A 26.2 Erythema* N/A 13.4 N/A 12.9 Swelling* N/A 6.7 N/A 6.5 Injection-site bruising N/A 1.5 N/A 0.4 Table 6: Vaccine-Related Systemic Adverse Reactions Reported in ≥1% of Children Who Received VAQTA* or ProQuad Concomitantly with VAQTA 1 to 14 Days After VAQTA or Vaccination with ProQuad and VAQTA and 1 to 28 Days After Vaccination with ProQuad and VAQTA Adverse Reactions Dose 1 Dose 2 Days 1 to 14 Days 1 to 28 Days 1 to 14 Days 1 to 28 VAQTA†
(N=1453)
(n=1412)
%ProQuad + VAQTA†
(N=347)
(n=328)
%ProQuad + VAQTA
(N=347)
(n=328)
%VAQTA
(N=1301)
(n=1254)
%ProQuad + VAQTA†
(N=292)
(n=264)
%ProQuad + VAQTA†
(N=291)
(n=263)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * Systemic adverse events for subjects given VAQTA alone were collected for 14 days postvaccination.
- † Safety follow-up for systemic adverse reactions was 14 days for VAQTA and 28 days for ProQuad + VAQTA.
- ‡ Designates a solicited adverse reaction.
- § Temperature reported as elevated or abnormal.
Fever‡,§ 5.7 14.9 15.2 4.1 8.0 8.4 Irritability 5.8 7.0 7.3 3.5 5.3 5.3 Measles-like rash 0.0 3.4 3.4 0.0 1.1 1.1 Rhinorrhea 0.6 2.7 3.0 0.6 1.1 2.7 Diarrhea 1.5 1.8 2.4 1.7 0.4 0.8 Cough 0.6 2.1 2.1 0.2 0.8 1.5 Vomiting 1.1 0.3 0.9 0.6 0.8 1.1 In an open-label clinical trial, 653 children 12 to 23 months of age were randomized to receive a first dose of ProQuad with VAQTA and pneumococcal 7-valent conjugate vaccine concomitantly (N=330) or a first dose of ProQuad and pneumococcal 7-valent conjugate vaccine concomitantly and then vaccinated with VAQTA 6 weeks later (N=323). Approximately 6 months later, subjects received either the second doses of ProQuad and VAQTA concomitantly or the second doses of ProQuad and VAQTA separately. The race distribution of the study subjects was as follows: 60.3% White; 21.6% African-American; 9.5% Hispanic; 7.2% other; 1.1% Asian/Pacific; and 0.3% American Indian. The gender distribution of the study subjects was 50.7% male and 49.3% female. Vaccine-related injection-site and systemic adverse reactions observed among recipients of concomitant ProQuad, VAQTA, and pneumococcal 7-valent conjugate vaccine and ProQuad and pneumococcal 7-valent conjugate vaccine at a rate of at least 1% are shown in Tables 7 and 8. In the 28 days after vaccination with the first dose of ProQuad, the rates of fever (including all vaccine- and non-vaccine-related reports) were comparable in subjects who received the 3 vaccines together (38.6%) as compared with subjects given ProQuad and pneumococcal 7-valent conjugate vaccine (42.7%). The rates of fever in the 28 days following the second dose of ProQuad were also comparable in subjects who received ProQuad and VAQTA together (17.4%) as compared with subjects given ProQuad separately from VAQTA (17.0%). In a post-hoc analysis, these differences were not statistically significant after ProQuad (dose 1) (RR 0.90 [95% CI: 0.75, 1.09]) nor after dose 2 (RR 1.02 [95% CI: 0.70, 1.51]). No clinically significant differences in adverse reactions were reported among treatment groups [see Clinical Studies (14)].
Table 7: Vaccine-Related Injection-Site Adverse Reactions Reported in ≥1% of Children Who Received ProQuad + VAQTA + PCV7* Concomitantly or VAQTA Alone Followed by ProQuad + PCV7 Concomitantly (1 to 5 Days After a Dose of ProQuad) Adverse Reactions Dose 1 Dose 2 VAQTA + ProQuad + PCV7
(N=330)
(n=311)
%VAQTA Alone Followed by ProQuad + PCV7
(N=323)
(n=302)
%VAQTA + ProQuad
(N=273)
(n=265)
%VAQTA Alone Followed by ProQuad
(N=240)
(n=230)
%N/A = Not applicable.
N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * PCV7 = Pneumococcal 7-valent conjugate vaccine.
- † Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 1 to 5 postvaccination at each vaccine injection site.
Injection-Site - ProQuad Pain/tenderness† 21.2 24.2 18.1 17.0 Erythema† 13.5 11.9 10.6 13.0 Swelling† 7.4 10.9 8.3 11.7 Bruising 1.9 1.3 0.8 0.4 Injection-Site - VAQTA Pain/tenderness† 20.6 15.3 17.5 20.3 Erythema† 9.6 11.7 9.1 12.7 Swelling† 6.8 9.5 6.1 7.6 Bruising 1.3 1.1 1.1 1.6 Rash 1.0 0.0 0.4 0.4 Injection-Site - PCV7 Pain/tenderness† 25.4 27.6 N/A N/A Erythema† 16.4 16.6 N/A N/A Swelling† 13.2 14.3 N/A N/A Bruising 0.6 1.7 N/A N/A Table 8: Vaccine-Related Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad + VAQTA + PCV7* Concomitantly, or VAQTA Alone Followed by ProQuad + PCV7 Concomitantly (1 to 28 Days After a Dose of ProQuad) Adverse Reactions Dose 1 Dose 2 VAQTA + ProQuad + PCV7
(N=330)
(n=311)
%VAQTA Alone Followed by ProQuad + PCV7
(N=323)
(n=302)
%VAQTA + ProQuad
(N=273)
(n=265)
%VAQTA Alone Followed by ProQuad
(N=240)
(n=230)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- * PCV7 = Pneumococcal 7-valent conjugate vaccine.
- † Designates a solicited adverse reaction.
- ‡ Temperature reported as elevated or abnormal.
Fever†,‡ 26.4 27.2 9.1 9.6 Irritability 4.8 6.3 1.9 1.3 Measles-like rash† 2.3 4.0 0.0 0.0 Varicella-like rash† 1.0 1.7 0.0 0.0 Rash (not otherwise specified) 1.3 1.3 0.0 0.9 Diarrhea 1.3 1.3 0.4 1.3 Upper respiratory infection 1.0 1.3 1.1 0.9 Viral infection 1.0 0.7 0.0 0.0 Rhinorrhea 0.0 0.7 1.1 0.0 6.2 Post-Marketing Experience
The following adverse events have been identified during post-approval use of either the components of ProQuad or ProQuad. Because the events are in some cases described in the literature or reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Subacute sclerosing panencephalitis (see below), encephalitis (see below), aseptic meningitis (see below), meningitis, measles, atypical measles, pneumonia, respiratory infection, infection, varicella (vaccine strain), influenza, herpes zoster, orchitis, epididymitis, cellulitis, skin infection, retinitis, bronchitis, parotitis, sinusitis, impetigo, herpes simplex, candidiasis, rhinitis.
Although not reported following vaccination with ProQuad, cases of encephalitis or meningitis caused by vaccine strain varicella virus have been reported in immunocompetent individuals previously vaccinated with VARIVAX (same varicella vaccine strain as in ProQuad) months to years after vaccination. Reported cases were commonly associated with preceding or concurrent herpes zoster rash (see below).
Blood and the lymphatic system disorders
Aplastic anemia, thrombocytopenia, regional lymphadenopathy, lymphadenitis.
Immune system disorders
Anaphylaxis and related phenomena such as angioneurotic edema, facial edema, and peripheral edema, anaphylactoid reaction.
Psychiatric disorders
Agitation, apathy, nervousness.
Nervous system disorders
Measles inclusion body encephalitis [see Contraindications (4.2)], acute disseminated encephalomyelitis, transverse myelitis, cerebrovascular accident, encephalopathy (see below), Guillain-Barré syndrome, optic neuritis, Bell's palsy, polyneuropathy, ataxia, hypersomnia, afebrile convulsions or seizures, febrile seizure, headache, syncope, dizziness, tremor, paraesthesia.
Eye disorders
Necrotizing retinitis (in immunocompromised individuals), retrobulbar neuritis, ocular palsies, edema of the eyelid, irritation eye.
Ear and labyrinth disorders
Nerve deafness, ear pain.
Vascular disorders
Extravasation blood.
Respiratory, thoracic and mediastinal disorders
Pneumonitis [see Contraindications (4.3)], pulmonary congestion, wheezing, bronchial spasm, epistaxis, sore throat.
Gastrointestinal disorders
Hematochezia, abdominal pain, mouth ulcer.
Skin and subcutaneous tissue disorders
Stevens-Johnson syndrome, Henoch-Schönlein purpura, erythema multiforme, acute hemorrhagic edema of infancy, purpura, skin induration, panniculitis, pruritus.
Musculoskeletal, connective tissue and bone disorders
Arthritis and/or arthralgia (usually transient and rarely chronic, see below); pain of the hip, leg, or neck; myalgia; musculoskeletal pain.
General disorders and administration site conditions
Injection-site complaints (burning and/or stinging of short duration, edema/swelling, hive-like rash, discoloration, hematoma, induration, lump, vesicles, wheal and flare), varicella-like rash, warm to touch, stiffness, warm sensation, inflammation, injection-site hemorrhage, injection-site injury.
Deaths have been reported following vaccination with measles, mumps, and rubella vaccines; however, a causal relationship has not been established in healthy individuals. Death as a direct consequence of disseminated measles vaccine virus infection has been reported in severely immunocompromised individuals in whom a measles-containing vaccine is contraindicated and who were inadvertently vaccinated. However, there were no deaths or permanent sequelae reported in a published post-marketing surveillance study in Finland involving 1.5 million children and adults who were vaccinated with M-M-R II during 1982 to 1993 {3}.
Encephalitis and encephalopathy have been reported approximately once for every 3 million doses of M-M-R II or measles-, mumps-, and rubella-containing vaccine administered since licensure of these vaccines.
The risk of serious neurological disorders following live measles virus vaccine administration remains less than the risk of encephalitis and encephalopathy following infection with wild-type measles (1 per 1000 reported cases) {4,5}.
In severely immunocompromised individuals who have been inadvertently vaccinated with measles-containing vaccine; measles inclusion body encephalitis, pneumonitis, and fatal outcome as a direct consequence of disseminated measles vaccine virus infection have been reported [see Contraindications (4.2)]. In this population, disseminated mumps and rubella vaccine virus infection have also been reported.
Recipients of rubella vaccine may develop chronic joint symptoms. Arthralgia and/or arthritis, and polyneuritis after wild-type rubella virus infection vary in frequency and severity with age and gender, being greatest in adult females and least in pre-pubertal children. Following vaccination in children, reactions in joints are uncommon (0 to 3%) and of brief duration. In women, incidence rates for arthritis and arthralgia are higher than those seen in children (12 to 26%), and the reactions tend to be more marked and of longer duration (e.g., months or years). In adolescent girls, the reactions appear to be intermediate in incidence between those seen in children and adult women.
Chronic arthritis has been associated with wild-type rubella infection and has been related to persistent virus and/or viral antigen isolated from body tissues. Chronic joint symptoms have been reported following administration of rubella-containing vaccine.
There have been reports of subacute sclerosing panencephalitis (SSPE) in children who did not have a history of infection with wild-type measles but did receive measles vaccine. Some of these cases may have resulted from unrecognized measles in the first year of life or possibly from the measles vaccination. Based on estimated measles vaccine distribution in the United States (US), the association of SSPE cases to measles vaccination is about one case per million vaccine doses distributed. The association with wild-type measles virus infection is 6 to 22 cases of SSPE per million cases of measles. The results of a retrospective case-controlled study suggest that the overall effect of measles vaccine has been to protect against SSPE by preventing measles with its inherent higher risk of SSPE.
Cases of aseptic meningitis have been reported to Vaccine Adverse Event Reporting System (VAERS) following measles, mumps, and rubella vaccination. Although a causal relationship between other strains of mumps vaccine and aseptic meningitis has been shown, there is no evidence to link Jeryl Lynn™ mumps vaccine to aseptic meningitis.
Cases of thrombocytopenia have been reported after use of measles vaccine; measles, mumps, and rubella vaccine; and after varicella vaccination. Post-marketing experience with live measles, mumps, and rubella vaccine indicates that individuals with current thrombocytopenia may develop more severe thrombocytopenia following vaccination. In addition, individuals who experienced thrombocytopenia following the first dose of a live measles, mumps, and rubella vaccine may develop thrombocytopenia with repeat doses. Serologic testing for antibody to measles, mumps, or rubella should be considered in order to determine if additional doses of vaccine are needed [see Warnings and Precautions (5.5)].
The reported rate of zoster in recipients of VARIVAX appears not to exceed that previously determined in a population-based study of healthy children who had experienced wild-type varicella {6}. In clinical trials, 8 cases of herpes zoster were reported in 9454 vaccinated individuals 12 months to 12 years of age during 42,556 person-years of follow-up. This resulted in a calculated incidence of at least 18.8 cases per 100,000 person-years. All 8 cases reported after VARIVAX were mild and no sequelae were reported. The long-term effect of VARIVAX on the incidence of herpes zoster is unknown at present.
The vaccine virus (Oka/Merck strain) contained in ProQuad may establish latency of varicella zoster virus in immunocompetent individuals, with the potential for later development of herpes zoster [see Adverse Reactions (6.2), Infections and Infestations].
6.3 Post-Marketing Observational Safety Surveillance Study
Safety was evaluated in an observational study that included 69,237 children vaccinated with ProQuad 12 months to 12 years old. A historical comparison group included 69,237 age-, gender-, and date-of-vaccination (day and month) matched subjects who were given M-M-R II and VARIVAX concomitantly. The primary objective was to assess the incidence of febrile seizures occurring within various time intervals after vaccination in 12- to 60-month-old children who had neither been vaccinated against measles, mumps, rubella, or varicella, nor had a history of the wild-type infections (N=31,298 vaccinated with ProQuad, including 31,043 who were 12 to 23 months old). The incidence of febrile seizures was also assessed in a historical control group of children who had received their first vaccination with M-M-R II and VARIVAX concomitantly (N=31,298, including 31,019 who were 12 to 23 months old). The secondary objective was to assess the general safety of ProQuad in the 30-day period after vaccination in children 12 months to 12 years old.
In pre-licensure clinical studies, an increase in fever was observed 5 to 12 days after vaccination with ProQuad (dose 1) compared to M-M-R II and VARIVAX (dose 1) given concomitantly. In the post-marketing observational surveillance study, results from the primary safety analysis revealed an approximate two-fold increase in the risk of febrile seizures in the same 5 to 12 day timeframe after vaccination with ProQuad (dose 1). The incidence of febrile seizures 5 to 12 days after ProQuad (dose 1) (0.70 per 1000 children) was higher than that in children receiving M-M-R II and VARIVAX concomitantly (0.32 per 1000 children) [RR 2.20, 95% confidence interval (CI): 1.04, 4.65]. The incidence of febrile seizures 0 to 30 days after ProQuad (dose 1) (1.41 per 1000 children) was similar to that observed in children receiving M-M-R II and VARIVAX concomitantly [RR 1.10 (95% CI: 0.72, 1.69)]. See Table 9. General safety analyses revealed that the risks of fever (RR=1.89; 95% CI: 1.67, 2.15) and skin eruption (RR=1.68; 95% CI: 1.07, 2.64) were significantly higher after ProQuad (dose 1) compared with those who received concomitant first doses of M-M-R II and VARIVAX, respectively. All medical events that resulted in hospitalization or emergency room visits were compared between the group given ProQuad and the historical comparison group, and no other safety concerns were identified in this study.
Table 9: Confirmed Febrile Seizures Days 5 to 12 and 0 to 30 After Vaccination with ProQuad (dose 1) Compared to Concomitant Vaccination with M-M-R II and VARIVAX (dose 1) in Children 12 to 60 Months of Age Time Period ProQuad cohort (N=31,298) MMR+V cohort (N=31,298) Relative risk (95% CI) n Incidence per 1000 n Incidence per 1000 5 to 12 Days 22 0.70 10 0.32 2.20 (1.04, 4.65) 0 to 30 Days 44 1.41 40 1.28 1.10 (0.72, 1.69) In this observational post-marketing study, no case of febrile seizure was observed during the 5 to 12 day postvaccination time period among 26,455 children who received ProQuad as a second dose of M-M-R II and VARIVAX. In addition, detailed general safety data were available from more than 25,000 children who received ProQuad as a second dose of M-M-R II and VARIVAX, most of them (95%) between 4 and 6 years of age, and an analysis of these data by an independent, external safety monitoring committee did not identify any specific safety concern.
-
7 DRUG INTERACTIONS
7.1 Immune Globulins and Transfusions
Immune globulins (IG) administered concomitantly with ProQuad contain antibodies that may interfere with vaccine virus replication and decrease the expected immune response. Vaccination should be deferred for at least 3 months following blood or plasma transfusions, or administration of IG.
The appropriate suggested interval between transfusion or IG administration and vaccination will vary with the type of transfusion or indication for, and dose of, IG (e.g., 5 months for Varicella Zoster Immune Globulin [VZIG]) {2}. Following administration of ProQuad, any IG including VZIG should not be given for 1 month thereafter unless its use outweighs the benefits of vaccination {2}. [See Warnings and Precautions (5.9).]
7.2 Salicylates
Reye syndrome has been reported following the use of salicylates during wild-type varicella infection. Vaccine recipients should avoid use of salicylates for 6 weeks after vaccination with ProQuad. [See Warnings and Precautions (5.10) and Patient Counseling Information (17).]
7.3 Corticosteroids and Immunosuppressive Drugs
ProQuad may be used in individuals who are receiving topical corticosteroids or low-dose corticosteroids for asthma prophylaxis or replacement therapy, e.g., for Addison's disease. ProQuad should not be given to individuals receiving immunosuppressive doses of corticosteroids or other immunosuppressive drugs. Vaccination with a live, attenuated vaccine, such as varicella or measles, can result in a more extensive vaccine-associated rash or disseminated disease in individuals on immunosuppressive drugs [see Contraindications (4.2)].
7.4 Drug/Laboratory Test Interactions
Live, attenuated measles, mumps, and rubella virus vaccines given individually may result in a temporary depression of tuberculin skin sensitivity. Therefore, if a tuberculin test is to be done, it should be administered either any time before, simultaneously with, or at least 4 to 6 weeks after ProQuad.
7.5 Use with Other Vaccines
At least 1 month should elapse between a dose of a measles-containing vaccine such as M-M-R II and a dose of ProQuad, and at least 3 months should elapse between administration of 2 doses of ProQuad or varicella-containing vaccines.
ProQuad may be administered concomitantly with Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant). Additionally, ProQuad may be administered concomitantly with pneumococcal 7-valent conjugate vaccine, and/or hepatitis A (inactivated) vaccines. [See Clinical Studies (14).]
There are no data regarding the administration of ProQuad with inactivated poliovirus vaccine or with other live virus vaccines.
There are insufficient data to support concomitant vaccination with diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed. [See Clinical Studies (14).]
Children under treatment for tuberculosis have not experienced exacerbation of the disease when vaccinated with live measles virus vaccine; no studies have been reported to date of the effect of measles virus vaccines on children with untreated tuberculosis.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
ProQuad vaccine contains live attenuated measles, mumps, rubella and varicella viruses. The vaccine is contraindicated for use in pregnant women because infection during pregnancy with the wild-type viruses is associated with maternal and fetal adverse outcomes.
For women who are inadvertently vaccinated when pregnant or who become pregnant within 3 months of administration of ProQuad, the healthcare provider should be aware of the following: (1) Reports have indicated that contracting wild-type measles during pregnancy enhances fetal risk. Increased rates of spontaneous abortion, stillbirth, congenital defects, and prematurity have been observed subsequent to infection with wild-type measles during pregnancy. There are no adequate studies of the attenuated (vaccine) strain of measles virus in pregnancy; (2) Mumps infection during the first trimester of pregnancy may increase the rate of spontaneous abortion. Although mumps vaccine virus has been shown to infect the placenta and fetus, there is no evidence that it causes congenital malformations in humans {7}; (3) In a 10-year survey involving over 700 pregnant women who received rubella vaccine within 3 months before or after conception (of whom 189 received the Wistar RA 27/3 strain), none of the newborns had abnormalities compatible with congenital rubella syndrome {8}; and (4) Wild-type varicella, if acquired during pregnancy, can sometimes cause congenital varicella syndrome.
Available data on inadvertent administration of ProQuad to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
There are no relevant animal data.
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4%, and 15% to 20%, respectively {9,10}.
8.2 Lactation
Risk Summary
It is not known whether varicella, measles, or mumps vaccine virus is excreted in human milk. Studies have shown that lactating postpartum women vaccinated with live rubella vaccine may secrete the virus in breast milk and transmit it to breastfed infants. {11,12} [See Warnings and Precautions (5.8).]
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ProQuad, and any potential adverse effects on the breastfed child from ProQuad or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
Do not administer ProQuad to infants younger than 12 months of age or to children 13 years and older. Safety and effectiveness of ProQuad in infants younger than 12 months of age and in children 13 years and older have not been studied. ProQuad is not approved for use in persons in these age groups. [See Adverse Reactions (6) and Clinical Studies (14).]
-
11 DESCRIPTION
ProQuad (Measles, Mumps, Rubella and Varicella Virus Vaccine Live) is a combined, attenuated, live virus vaccine containing measles, mumps, rubella, and varicella viruses. ProQuad is a sterile lyophilized preparation of (1) the components of M-M-R II (Measles, Mumps, and Rubella Virus Vaccine Live): Measles Virus Vaccine Live, a more attenuated line of measles virus, derived from Enders' attenuated Edmonston strain and propagated in chick embryo cell culture; Mumps Virus Vaccine Live, the Jeryl Lynn™ (B level) strain of mumps virus propagated in chick embryo cell culture; Rubella Virus Vaccine Live, the Wistar RA 27/3 strain of live attenuated rubella virus propagated in WI-38 human diploid lung fibroblasts; and (2) Varicella Virus Vaccine Live (Oka/Merck), the Oka/Merck strain of varicella-zoster virus propagated in MRC-5 cells. The cells, virus pools, bovine serum, and recombinant human albumin used in manufacturing are all tested to provide assurance that the final product is free of potential adventitious agents.
ProQuad, when reconstituted as directed, is a sterile suspension for subcutaneous administration. Each 0.5-mL dose contains not less than 3.00 log10 TCID50 of measles virus; 4.30 log10 TCID50 of mumps virus; 3.00 log10 TCID50 of rubella virus; and a minimum of 3.99 log10 PFU of Oka/Merck varicella virus.
Each 0.5-mL dose of the vaccine contains no more than 21 mg of sucrose, 11 mg of hydrolyzed gelatin, 2.4 mg of sodium chloride, 1.8 mg of sorbitol, 0.40 mg of monosodium L-glutamate, 0.34 mg of sodium phosphate dibasic, 0.31 mg of recombinant human albumin, 0.17 mg of sodium bicarbonate, 72 mcg of potassium phosphate monobasic, 60 mcg of potassium chloride; 36 mcg of potassium phosphate dibasic; residual components of MRC-5 cells including DNA and protein; <16 mcg of neomycin, bovine calf serum (0.5 mcg), and other buffer and media ingredients. The product contains no preservative.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
ProQuad has been shown to induce measles-, mumps-, rubella-, and varicella-specific immunity, which is thought to be the mechanism by which it protects against these four childhood diseases.
The efficacy of ProQuad was established through the use of immunological correlates for protection against measles, mumps, rubella, and varicella. Results from efficacy studies or field effectiveness studies that were previously conducted for the component vaccines were used to define levels of serum antibodies that correlated with protection against measles, mumps, and rubella. Also, in previous studies with varicella vaccine, antibody responses against varicella virus ≥5 gpELISA units/mL in a glycoprotein enzyme-linked immunosorbent assay (gpELISA) (not commercially available) similarly correlated with long-term protection. In these efficacy studies, the clinical endpoint for measles and mumps was a clinical diagnosis of either disease confirmed by a 4-fold or greater rise in serum antibody titers between either postvaccination or acute and convalescent titers; for rubella, a 4-fold or greater rise in antibody titers with or without clinical symptoms of rubella; and for varicella, varicella-like rash that occurred >42 days postvaccination and for which varicella was not excluded by either viral cultures of the lesion or serological tests. Specific laboratory evidence of varicella either by serology or culture was not required to confirm the diagnosis of varicella. Clinical studies with a single dose of ProQuad have shown that vaccination elicited rates of antibody responses against measles, mumps, and rubella that were similar to those observed after vaccination with a single dose of M-M-R II [see Clinical Studies (14)] and seroresponse rates for varicella virus were similar to those observed after vaccination with a single dose of VARIVAX [see Clinical Studies (14)]. The duration of protection from measles, mumps, rubella, and varicella infections after vaccination with ProQuad is unknown.
12.6 Persistence of Antibody Responses after Vaccination
The persistence of antibody at 1 year after vaccination was evaluated in a subset of 2107 children enrolled in the clinical trials. Antibody was detected in 98.9% (1722/1741) for measles, 96.7% (1676/1733) for mumps, 99.6% (1796/1804) for rubella, and 97.5% (1512/1550) for varicella (≥5 gpELISA units/mL) of vaccinees following a single dose of ProQuad.
Experience with M-M-R II demonstrates that antibodies to measles, mumps, and rubella viruses are still detectable in most individuals 11 to 13 years after primary vaccination {13}. Varicella antibodies were present for up to ten years postvaccination in most of the individuals tested who received 1 dose of VARIVAX.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
Formal studies to evaluate the clinical efficacy of ProQuad have not been performed.
Efficacy of the measles, mumps, rubella, and varicella components of ProQuad was previously established in a series of clinical studies with the monovalent vaccines. A high degree of protection from infection was demonstrated in these studies {14-21}.
Immunogenicity in Children 12 Months to 6 Years of Age
Prior to licensure, immunogenicity was studied in 5845 healthy children 12 months to 6 years of age with a negative clinical history of measles, mumps, rubella, and varicella who participated in 5 randomized clinical trials. The immunogenicity of ProQuad was similar to that of its individual component vaccines (M-M-R II and VARIVAX), which are currently used in routine vaccination.
The presence of detectable antibody was assessed by an appropriately sensitive enzyme-linked immunosorbent assay (ELISA) for measles, mumps (wild-type and vaccine-type strains), and rubella, and by gpELISA for varicella. For evaluation of vaccine response rates, a positive result in the measles ELISA corresponded to measles antibody concentrations of ≥255 mIU/mL when compared to the WHO II (66/202) Reference Immunoglobulin for Measles.
Children were positive for mumps antibody if the antibody level was ≥10 ELISA units/mL. A positive result in the rubella ELISA corresponded to concentrations of ≥10 IU rubella antibody/mL when compared to the WHO International Reference Serum for Rubella; children with varicella antibody levels ≥5 gpELISA units/mL were considered to be seropositive since a response rate based on ≥5 gpELISA units/mL has been shown to be highly correlated with long-term protection.
Immunogenicity in Children 12 to 23 Months of Age After a Single Dose
In 4 randomized clinical trials, 5446 healthy children 12 to 23 months of age were administered ProQuad, and 2038 children were vaccinated with M-M-R II and VARIVAX given concomitantly at separate injection sites. Subjects enrolled in each of these trials had a negative clinical history, no known recent exposure, and no vaccination history for varicella, measles, mumps, and rubella. Children were excluded from study participation if they had an immune impairment or had a history of allergy to components of the vaccine(s). Except for in 1 trial [see ProQuad Administered with Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine below], no concomitant vaccines were permitted during study participation. The race distribution of the study subjects across these studies following a first dose of ProQuad was as follows: 66.3% White; 12.7% African-American; 9.9% Hispanic; 6.7% Asian/Pacific; 4.2% other; and 0.2% American Indian. The gender distribution of the study subjects across these studies following a first dose of ProQuad was 52.6% male and 47.4% female. A summary of combined immunogenicity results 6 weeks following administration of a single dose of ProQuad or M-M-R II and VARIVAX is shown in Table 10. These results were similar to the immune response rates induced by concomitant administration of single doses of M-M-R II and VARIVAX at separate injection sites (lower bound of the 95% CI for the risk difference in measles, mumps, and rubella seroconversion rates were >-5.0 percentage points and the lower bound of the 95% CI for the risk difference in varicella seroprotection rates was either >-15 percentage points [one study] or >-10.0 percentage points [three studies]).
Table 10: Summary of Combined Immunogenicity Results 6 Weeks Following the Administration of a Single Dose of ProQuad (Varicella Virus Potency ≥3.97 log10 PFU) or M-M-R II and VARIVAX (Per-Protocol Population) Group Antigen n Observed Response Rate
(95% CI)Observed GMT
(95% CI)n = Number of per-protocol subjects with evaluable serology.
CI = Confidence interval.
GMT = Geometric mean titer.
ELISA = Enzyme-linked immunosorbent assay.
PFU = Plaque-forming units.
OD = Optical density.- * Includes ProQuad + Placebo followed by ProQuad (Visit 1) (Protocol 009), ProQuad Middle and High Doses (Visit 1) (Protocol 011), ProQuad (Lot 1, Lot 2, Lot 3) (Protocol 012), both the Concomitant and Non-concomitant groups (Protocol 013).
- † The mumps antibody response was assessed by a vaccine-strain ELISA in Protocols 009 and 011 and by a wild-type ELISA in Protocols 012 and 013. In the former assay, the serostatus was based on the OD cutoff of the assay. In the latter assay, 10 mumps ELISA units was used as the serostatus cutoff.
ProQuad
(N=5446*)Varicella 4381 91.2%
(90.3%, 92.0%)15.5
(15.0, 15.9)Measles 4733 97.4%
(96.9%, 97.9%)3124.9
(3038.9, 3213.3)Mumps
(OD cutoff)†973 98.8%
(97.9%, 99.4%)105.3
(98.0, 113.1)Mumps (wild-type ELISA)† 3735 95.8%
(95.1%, 96.4%)93.1
(90.2, 96.0)Rubella 4773 98.5%
(98.1%, 98.8%)91.8
(89.6, 94.1)M-M-R II + VARIVAX
(N=2038*)Varicella 1417 94.1%
(92.8%, 95.3%)16.6
(15.9, 17.4)Measles 1516 98.2%
(97.4%, 98.8%)2239.6
(2138.3, 2345.6)Mumps
(OD cutoff)†501 99.4%
(98.3%, 99.9%)87.5
(79.7, 96.0)Mumps (wild-type ELISA)† 1017 98.0%
(97.0%, 98.8%)90.8
(86.2, 95.7)Rubella 1528 98.5%
(97.7%, 99.0%)102.2
(97.8, 106.7)Immunogenicity in Children 15 to 31 Months of Age After a Second Dose of ProQuad
In 2 of the 4 randomized clinical trials described above, a subgroup (N=1035) of the 5446 children administered a single dose of ProQuad were administered a second dose of ProQuad approximately 3 to 9 months after the first dose. Children were excluded from receiving a second dose of ProQuad if they were recently exposed to or developed varicella, measles, mumps, and/or rubella prior to receipt of the second dose. No concomitant vaccines were administered to these children. The race distribution across these studies following a second dose of ProQuad was as follows: 67.3% White; 14.3% African-American; 8.3% Hispanic; 5.4% Asian/Pacific; 4.4% other; 0.2% American Indian; and 0.10% mixed. The gender distribution of the study subjects across these studies following a second dose of ProQuad was 50.4% male and 49.6% female. A summary of immune responses following a second dose of ProQuad is presented in Table 11. Results from this study showed that 2 doses of ProQuad administered at least 3 months apart elicited a positive antibody response to all four antigens in greater than 98% of subjects. The geometric mean titers (GMTs) following the second dose of ProQuad increased approximately 2-fold each for measles, mumps, and rubella, and approximately 41-fold for varicella.
Table 11: Summary of Immune Response to a First and Second Dose of ProQuad in Subjects <3 Years of Age Who Received ProQuad with a Varicella Virus Dose ≥3.97 Log10 PFU* Dose 1
N=1097Dose 2
N=1097Serostatus Cutoff/ Observed Response Rate Observed GMT Observed Response Rate Observed GMT Antigen Response Criteria n (95% CI) (95% CI) n (95% CI) (95% CI) ProQuad (Middle Dose) = ProQuad containing a varicella virus dose of 3.97 log10 PFU.
ProQuad (High Dose) = ProQuad containing a varicella virus dose of 4.25 log10 PFU.
ELISA = Enzyme-linked immunosorbent assay.
gpELISA = Glycoprotein enzyme-linked immunosorbent assay.
N = Number vaccinated at baseline.
n = Number of subjects who were per-protocol Postdose 1 and Postdose 2 and satisfied the given prevaccination serostatus cutoff.
CI = Confidence interval.
GMT = Geometric mean titer.
PFU = Plaque-forming units.- * Includes the following treatment groups: ProQuad + Placebo followed by ProQuad (Visit 1) (Protocol 009) and ProQuad (Middle and High Dose) (Protocol 011).
- † Samples from Protocols 009 and 011 were assayed in the legacy format Measles ELISA, which reported antibody titers in Measles ELISA units. To convert titers from ELISA units to mIU/mL, titers for these 2 protocols were divided by 0.1025. The lowest measurable titer postvaccination is 207.5 mIU/mL. The response rate for measles in the legacy format is the percent of subjects with a negative baseline measles antibody titer, as defined by the optical density (OD) cutoff, with a postvaccination measles antibody titer ≥207.5 mIU/mL.
Samples from Protocols 009 and 011 were assayed in the legacy format Rubella ELISA, which reported antibody titers in Rubella ELISA units. To convert titers from ELISA units to IU/mL, titers for these 2 protocols were divided by 1.28.Measles ≥120 mIU/mL† 915 98.1% (97.0%, 98.9%) 2956.8 (2786.3, 3137.7) 915 99.5% (98.7%, 99.8%) 5958.0 (5518.9, 6432.1) ≥255 mIU/mL 943 97.8% (96.6%, 98.6%) 2966.0 (2793.4, 3149.2) 943 99.4% (98.6%, 99.8%) 5919.3 (5486.2, 6386.6) Mumps ≥OD Cutoff (ELISA antibody units) 920 98.7% (97.7%, 99.3%) 106.7 (99.1, 114.8) 920 99.9% (99.4%, 100%) 253.1 (237.9, 269.2) Rubella ≥10 IU/mL 937 97.7% (96.5%, 98.5%) 91.1 (85.9, 96.6) 937 98.3% (97.2%, 99.0%) 158.8 (149.1, 169.2) Varicella <1.25 to ≥5 gpELISA units 864 86.6% (84.1%, 88.8%) 11.6 (10.9, 12.3) 864 99.4% (98.7%, 99.8%) 477.5 (437.8, 520.7) ≥OD Cutoff (gpELISA units) 695 87.2% (84.5%, 89.6%) 11.6 (10.9, 12.4) 695 99.4% (98.5%, 99.8%) 478.7 (434.8, 527.1) Immunogenicity in Children 4 to 6 Years of Age Who Received a First Dose of ProQuad After Primary Vaccination With M-M-R II and VARIVAX
In a clinical trial, 799 healthy 4- to 6-year-old children who had received M-M-R II and VARIVAX at least 1 month prior to study entry were randomized to receive ProQuad and placebo (N=399), M-M-R II and placebo concomitantly at separate injection sites (N=205), or M-M-R II and VARIVAX concomitantly at separate injection sites (N=195). Children were eligible if they were previously administered primary doses of M-M-R II and VARIVAX, either concomitantly or non-concomitantly, at 12 months of age or older. Children were excluded if they were recently exposed to measles, mumps, rubella, and/or varicella, had an immune impairment, or had a history of allergy to components of the vaccine(s). No concomitant vaccines were permitted during study participation. [See Adverse Reactions (6.1) for ethnicity and gender information.]
A summary of antibody responses to measles, mumps, rubella, and varicella at 6 weeks postvaccination in subjects who had previously received M-M-R II and VARIVAX is shown in Table 12. Results from this study showed that a first dose of ProQuad after primary vaccination with M-M-R II and VARIVAX elicited a positive antibody response to all four antigens in greater than 98% of subjects. Postvaccination GMTs for recipients of ProQuad were similar to those following a second dose of M-M-R II and VARIVAX administered concomitantly at separate injection sites (the lower bound of the 95% CI around the fold difference in measles, mumps, rubella, and varicella GMTs excluded 0.5). Additionally, GMTs for measles, mumps, and rubella were similar to those following a second dose of M-M-R II given concomitantly with placebo (the lower bound of the 95% CI around the fold difference for the comparison of measles, mumps, and rubella GMTs excluded 0.5).
Table 12: Summary of Antibody Responses to Measles, Mumps, Rubella, and Varicella at 6 Weeks Postvaccination in Subjects 4 to 6 Years of Age Who Had Previously Received M-M-R II and VARIVAX (Per-Protocol Population) Group Number GMT
(95% CI)Seropositivity Rate
(95% CI)% ≥4-Fold Rise in Titer
(95% CI)Geometric Mean Fold Rise
(95% CI)(Description) n Measles* gpELISA = Glycoprotein enzyme-linked immunosorbent assay; ELISA = Enzyme-linked immunosorbent assay; CI = Confidence interval; GMT = Geometric mean titer; N/A = Not applicable; N = Number of subjects vaccinated; n = number of subjects in the per-protocol analysis. - * Measles GMTs are reported in mIU/mL; seropositivity corresponds to ≥120 mIU/mL.
- † Mumps GMTs are reported in mumps Ab units/mL; seropositivity corresponds to ≥10 Ab units/mL.
- ‡ Rubella titers obtained by the legacy format were converted to their corresponding titers in the modified format. Rubella serostatus was determined after the conversion to IU/mL: seropositivity corresponds to ≥10 IU/mL.
- § Varicella GMTs are reported in gpELISA units/mL; seropositivity rate is reported by % of subjects with postvaccination antibody titers ≥5 gpELISA units/mL. Percentages are calculated as the number of subjects who met the criterion divided by the number of subjects contributing to the per-protocol analysis.
Group 1 (N=399) 367 1985.9 100% 4.9% 1.21 (ProQuad + placebo) (1817.6, 2169.9) (99.0%, 100%) (2.9%, 7.6%) (1.13, 1.30) Group 2 (N=205) 185 2046.9 100% 4.3% 1.28 (M-M-R II + placebo) (1815.2, 2308.2) (98.0%, 100%) (1.9%, 8.3%) (1.17, 1.40) Group 3 (N=195) 171 2084.3 99.4% 4.7% 1.31 (M-M-R II + VARIVAX) (1852.3, 2345.5) (96.8%, 100%) (2.0%, 9.0%) (1.17, 1.46) Mumps† Group 1 (N=399) 367 206.0 99.5% 27.2% 2.43 (ProQuad + placebo) (188.2, 225.4) (98.0%, 99.9%) (22.8%, 32.1%) (2.19, 2.69) Group 2 (N=205) 185 308.5 100% 41.1% 3.69 (M-M-R II + placebo) (269.6, 352.9) (98.0%, 100%) (33.9%, 48.5%) (3.14, 4.32) Group 3 (N=195) 171 295.9 100% 41.5% 3.36 (M-M-R II + VARIVAX) (262.5, 333.5) (97.9%, 100%) (34.0%, 49.3%) (2.84, 3.97) Rubella‡ Group 1 (N=399) 367 217.3 100% 32.7% 3.00 (ProQuad + placebo) (200.1, 236.0) (99.0%, 100%) (27.9%, 37.8%) (2.72, 3.31) Group 2 (N=205) 185 174.0 100% 31.9% 2.81 (M-M-R II + placebo) (157.3, 192.6) (98.0%, 100%) (25.2%, 39.1%) (2.41, 3.27) Group 3 (N=195) 171 154.1 99.4% 26.9% 2.47 (M-M-R II + VARIVAX) (138.9, 170.9) (96.8%, 100%) (20.4%, 34.2%) (2.17, 2.81) Varicella§ Group 1 (N=399) 367 322.2 98.9% 80.7% 12.43 (ProQuad + placebo) (278.9, 372.2) (97.2%, 99.7%) (76.2%, 84.6%) (10.63, 14.53) Group 2 (N=205)
(M-M-R II + placebo)185 N/A N/A N/A N/A Group 3 (N=195) 171 209.3 99.4% 71.9% 8.50 (M-M-R II + VARIVAX) (171.2, 255.9) (96.8%, 100%) (64.6%, 78.5%) (6.69, 10.81) Immunogenicity Following Concomitant Use with Other Vaccines
ProQuad with Pneumococcal 7-valent Conjugate Vaccine and/or VAQTA
In a clinical trial, 1027 healthy children 12 to 15 months of age were randomized to receive ProQuad and pneumococcal 7-valent conjugate vaccine concomitantly (N=510) at separate injection sites or ProQuad and pneumococcal 7-valent conjugate vaccine non-concomitantly (N=517) at separate clinic visits. [See Adverse Reactions (6.1) for ethnicity and gender information.] The statistical analysis of non-inferiority in antibody response rates to measles, mumps, rubella, and varicella at 6 weeks postvaccination for subjects are shown in Table 13. In the per-protocol population, seroconversion rates were not inferior in children given ProQuad and pneumococcal 7-valent conjugate vaccine concomitantly when compared to seroconversion rates seen in children given these vaccines non-concomitantly for measles, mumps, and rubella. In children with baseline varicella antibody titers <1.25 gpELISA units/mL, the varicella seroprotection rates were not inferior when rates after concomitant and non-concomitant vaccination were compared 6 weeks postvaccination. Statistical analysis of non-inferiority in GMTs to S. pneumoniae serotypes at 6 weeks postvaccination are shown in Table 14. Geometric mean antibody titers (GMTs) for S. pneumoniae types 4, 6B, 9V, 14, 18C, 19F, and 23F were not inferior when antibody titers in the concomitant and non-concomitant groups were compared 6 weeks postvaccination.
Table 13: Statistical Analysis of Non-Inferiority in Antibody Response Rates to Measles, Mumps, Rubella, and Varicella at 6 Weeks Postvaccination for Subjects Initially Seronegative to Measles, Mumps, or Rubella, or With Varicella Antibody Titer <1.25 gpELISA units at Baseline in the ProQuad + PCV7* Treatment Group and the ProQuad Followed by PCV7 Control Group (Per-Protocol Analysis) ProQuad + PCV7
(N=510)ProQuad followed by PCV7
(N=259)Difference Assay
Parametern Estimated Response† n Estimated Response† (percentage points)†,‡ (95% CI) N = Number of subjects vaccinated in each treatment group.
n = Number of subjects with measles antibody titer <255 mIU/mL, mumps antibody titer <10 ELISA Ab units/mL, rubella antibody titer <10 IU/mL, or varicella antibody titer <1.25 gpELISA units/mL at baseline and with postvaccination serology contributing to the per-protocol analysis.
Ab = antibody; ELISA = Enzyme-linked immunosorbent assay; gpELISA = Glycoprotein enzyme-linked immunosorbent assay; CI = Confidence interval.- * PCV7 = Pneumococcal 7-valent conjugate vaccine.
Seronegative defined as baseline measles antibody titer <255 mIU/mL for measles, baseline mumps antibody titer <10 ELISA Ab units/mL for mumps, and baseline rubella antibody titer <10 IU/mL for rubella.- † Estimated responses and their differences were based on statistical analysis models adjusting for study center.
- ‡ ProQuad + PCV7 - ProQuad followed by PCV7.
The conclusion of non-inferiority is based on the lower bound of the 2-sided 95% CI on the risk difference being greater than -10 percentage points (i.e., excluding a decrease equal to or more than the prespecified criterion of 10.0 percentage points). This indicates that the difference is statistically significantly less than the prespecified clinically relevant decrease of 10.0 percentage points at the 1-sided alpha = 0.025 level.Measles
% ≥255 mIU/mL406 97.3% 204 99.5% -2.2 (-4.6, 0.2) Mumps
% ≥10 Ab units/mL403 96.6% 208 98.6% -1.9 (-4.5, 1.0) Rubella
% ≥10 IU/mL377 98.7% 195 97.9% 0.9 (-1.3, 4.1) Varicella
% ≥5 gpELISA units/mL379 92.5% 192 87.9% 4.5 (-0.4, 10.4) Table 14: Statistical Analysis of Non-Inferiority in GMTs to S. pneumoniae Serotypes at 6 Weeks Postvaccination in the ProQuad + PCV7* Treatment Group and the PCV7 Followed by ProQuad Control Group (Per-Protocol Analysis) Group 1
ProQuad + PCV7 (N=510)Group 2
PCV7 followed by ProQuad (N=258)Serotype Parameter n Estimated Response† n Estimated Response† Fold-Difference*,‡ (95% CI) N = Number of subjects vaccinated in each treatment group; n = Number of subjects contributing to the per-protocol analysis for the given serotype; GMT = geometric mean titer; CI = Confidence interval. - * PCV7 = Pneumococcal 7-valent conjugate vaccine.
- † Estimated responses and their fold-difference were based on statistical analysis models adjusting for study center and prevaccination titer.
- ‡ ProQuad + PCV7 / PCV7 followed by ProQuad.
The conclusion of non-inferiority is based on the lower bound of the 2-sided 95% CI on the fold-difference being greater than 0.5, (i.e., excluding a decrease of 2-fold or more). This indicates that the fold-difference is statistically significantly less than the pre-specified clinically relevant 2-fold difference at the 1-sided alpha = 0.025 level.4 GMT 410 1.5 193 1.3 1.2 (1.0, 1.4) 6B GMT 410 8.9 192 8.4 1.1 (0.9, 1.2) 9V GMT 409 2.9 193 2.5 1.2 (1.0, 1.3) 14 GMT 408 6.5 193 5.7 1.1 (1.0, 1.3) 18C GMT 408 2.3 193 2.0 1.2 (1.0, 1.3) 19F GMT 408 3.5 192 3.1 1.1 (1.0, 1.3) 23F GMT 413 4.1 197 3.7 1.1 (1.0, 1.3) In a clinical trial, 653 healthy children 12 to 15 months of age were randomized to receive VAQTA, ProQuad, and pneumococcal 7-valent conjugate vaccine concomitantly (N=330) or ProQuad and pneumococcal 7-valent conjugate vaccine concomitantly followed by VAQTA 6 weeks later (N=323). [See Adverse Reactions (6.1) for ethnicity and gender information.] Statistical analysis of non-inferiority of the response rate for varicella antibody at 6 weeks postvaccination among subjects who received VAQTA concomitantly or non-concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine is shown in Table 15. For the varicella component of ProQuad, in subjects with baseline antibody titers <1.25 gpELISA units/mL, the proportion with a titer ≥5 gpELISA units/mL 6 weeks after their first dose of ProQuad was non-inferior when ProQuad was administered with VAQTA and pneumococcal 7-valent conjugate vaccine as compared to the proportion with a titer ≥5 gpELISA units/mL when ProQuad was administered with pneumococcal 7-valent conjugate vaccine alone. Statistical analysis of non-inferiority of the seropositivity rate for hepatitis A antibody at 4 weeks postdose 2 of VAQTA among subjects who received VAQTA concomitantly or non-concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine is shown in Table 16. The seropositivity rate to hepatitis A 4 weeks after a second dose of VAQTA given concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine (defined as the percent of subjects with a titer ≥10 mIU/mL) was non-inferior to the seropositivity rate observed when VAQTA was administered separately from ProQuad and pneumococcal 7-valent conjugate vaccine. Statistical analysis of non-inferiority in GMT to S. pneumoniae serotypes at 6 weeks postvaccination among subjects who received VAQTA concomitantly or non-concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine is shown in Table 17. Additionally, the GMTs for S. pneumoniae types 4, 6B, 9V, 14, 18C, 19F, and 23F 6 weeks after vaccination with pneumococcal 7-valent conjugate vaccine administered concomitantly with ProQuad and VAQTA were non-inferior as compared to GMTs observed in the group given pneumococcal 7-valent conjugate vaccine with ProQuad alone. An earlier clinical study involving 617 healthy children provided data that indicated that the seroresponse rates 6 weeks post vaccination for measles, mumps, and rubella in those given M-M-R II and VAQTA concomitantly (N=309) were non-inferior as compared to historical controls.
Table 15: Statistical Analysis of Non-Inferiority of the Response Rate for Varicella Antibody at 6 Weeks Postvaccination Among Subjects Who Received VAQTA Concomitantly or Non-Concomitantly With ProQuad and PCV7* (Per-Protocol Analysis Set) Group 1: Concomitant VAQTA with ProQuad + PCV7 (N=330) Group 2: Non-concomitant VAQTA separate from ProQuad + PCV7 (N=323) Difference† (percentage points): Group 1 – Group 2 (95% CI) Parameter n Estimated Response† n Estimated Response† N = Number of subjects enrolled/randomized; n = Number of subjects contributing to the per-protocol analysis for varicella; CI = Confidence interval. - * PCV7 = Pneumococcal 7-valent conjugate vaccine.
- † Estimated responses and their differences were based on a statistical analysis model adjusting for combined study center.
- ‡ 6 weeks following Dose 1.
- § Initial Serostatus <1.25 gpELISA units/ mL.
The conclusion of similarity (non-inferiority) was based on the lower bound of the 2-sided 95% CI on the risk difference excluding a decrease of 10 percentage points or more (lower bound >-10.0). This indicated that the risk difference was statistically significantly greater than the pre-specified clinically relevant difference of -10 percentage points at the 1-sided alpha = 0.025 level.% ≥5 gpELISA units/mL‡ 225§ 93.2% 232§ 98.3% -5.1 (-9.3, -1.4) Table 16: Statistical Analysis of Non-Inferiority of the Seropositivity Rate (SPR) for Hepatitis A Antibody at 4 Weeks Postdose 2 of VAQTA Among Subjects Who Received VAQTA Concomitantly or Non-Concomitantly With ProQuad and PCV7* (Per-Protocol Analysis Set) Group 1: Concomitant VAQTA with ProQuad + PCV7
(N=330)Group 2: Non-concomitant VAQTA separate from ProQuad + PCV7 (N=323) Difference† (percentage points): Group 1 - Group 2 (95% CI) Parameter n Estimated Response† n Estimated Response† CI = Confidence interval; N = Number of subjects enrolled/randomized; n = Number of subjects contributing to the per-protocol analysis for hepatitis A. - * PCV7 = Pneumococcal 7-valent conjugate vaccine.
- † Estimated responses and their differences were based on a statistical analysis model adjusting for combined study center.
- ‡ 4 weeks following receipt of 2 doses of VAQTA.
- § Regardless of initial serostatus.
The conclusion of non-inferiority was based on the lower bound of the 2-sided 95% CI on the risk difference being greater than -10 percentage points (i.e., excluding a decrease of 10 percentage points or more) (lower bound >-10.0). This indicated that the risk difference was statistically significantly greater than the pre-specified clinically relevant difference of -10 percentage points at the 1-sided alpha = 0.025 level.% ≥10 mIU/mL‡ 182§ 100.0% 159§ 99.3% 0.7 (-1.4, 3.8) Table 17: Statistical Analysis of Non-Inferiority in Geometric Mean Titers (GMT) to S. pneumoniae Serotypes at 6 Weeks Postvaccination Among Subjects Who Received VAQTA Concomitantly or Non-Concomitantly With ProQuad and PCV7* (Per-Protocol Analysis Set) Group 1: Concomitant VAQTA with ProQuad + PCV7 (N=330) Group 2: Non-concomitant VAQTA separate from ProQuad + PCV7 (N=323) Serotype n Estimated Response† n Estimated Response† Fold-Difference†
(95% CI)CI = Confidence interval; GMT = Geometric mean titer; N = Number of subjects enrolled/randomized; n = Number of subjects contributing to the per-protocol analysis for S. pneumoniae serotypes. - * PCV7 = Pneumococcal 7-valent conjugate vaccine.
- † Estimated responses and their fold-difference were based on statistical analysis models adjusting for combined study center and prevaccination titer.
The conclusion of non-inferiority was based on the lower bound of the 2-sided 95% CI on the fold-difference being greater than 0.5 (i.e., excluding a decrease of 2-fold or more). This indicates that the fold-difference was statistically significantly less than the prespecified clinically relevant 2-fold difference at the 1-sided alpha = 0.025 level.4 246 1.9 247 1.7 1.1 (0.9, 1.3) 6B 246 9.9 246 9.9 1.0 (0.8, 1.2) 9V 247 3.7 247 4.2 0.9 (0.8, 1.0) 14 248 7.8 247 7.6 1.0 (0.9, 1.2) 18C 247 2.9 247 2.7 1.1 (0.9, 1.3) 19F 248 4.0 248 3.8 1.1 (0.9, 1.2) 23F 247 5.1 247 4.4 1.1 (1.0, 1.3) ProQuad Administered with Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine
In a clinical trial, 1913 healthy children 12 to 15 months of age were randomized to receive ProQuad plus diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (DTaP) and Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccine concomitantly at separate injection sites (N=949), ProQuad at the initial visit followed by DTaP and Haemophilus b conjugate and hepatitis B (recombinant) vaccine given concomitantly 6 weeks later (N=485), or M-M-R II and VARIVAX given concomitantly at separate injection sites (N=479) at the first visit. [See Adverse Reactions (6.1) for ethnicity and gender information.] Seroconversion rates and antibody titers for measles, mumps, rubella, varicella, anti-PRP, and hepatitis B were comparable between the 2 groups given ProQuad at approximately 6 weeks postvaccination indicating that ProQuad and Haemophilus b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccine may be administered concomitantly at separate injection sites (see Table 18 below). Response rates for measles, mumps, rubella, varicella, Haemophilus influenzae type b, and hepatitis B were not inferior in children given ProQuad plus Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccines concomitantly when compared to ProQuad at the initial visit and Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccines given concomitantly 6 weeks later. There are insufficient data to support concomitant vaccination with diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (data not shown).
Table 18: Summary of the Comparison of the Immunogenicity Endpoints for Measles, Mumps, Rubella, Varicella, Haemophilus influenzae type b, and Hepatitis B Responses Following Vaccination with ProQuad, Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate), and Hepatitis B (Recombinant) Vaccine and DTaP Administered Concomitantly Versus Non-Concomitant Vaccination with ProQuad Followed by These Vaccines Concomitant Group Non-Concomitant Group N=949 N=485 Vaccine Antigen Parameter Response Response Risk Difference
(95% CI)Criterion for Non-inferiority HiB-PRP = Haemophilus influenzae type b, polyribosyl phosphate; HepB = hepatitis B; LB = lower bound, limit for non-inferiority comparison. Measles % ≥120 mIU/mL 97.8% 98.7% -0.9
(-2.3, 0.6)LB >-5.0 Mumps % ≥10 ELISA Ab units/mL 95.4% 95.1% 0.3
(-1.7, 2.6)LB >-5.0 Rubella % ≥10 IU/mL 98.6% 99.3% -0.7
(-1.8, 0.5)LB >-5.0 Varicella % ≥5 gpELISA units/mL 89.6% 90.8% -1.2
(-4.1, 2.0)LB >-10.0 HiB-PRP % ≥1.0 mcg/mL 94.6% 96.5% -1.9
(-4.1, 0.8)LB >-10.0 HepB % ≥10 mIU/mL 95.9% 98.8% -2.8
(-4.8, -0.8)LB >10.0 -
15 REFERENCES
- Levy O, et al. Disseminated varicella infection due to the vaccine strain of varicella-zoster virus, in a patient with a novel deficiency in natural killer T cells. J Infect Dis. 188(7):948-53, 2003.
- Committee on Infectious Diseases, American Academy of Pediatrics. In: Pickering LK, Baker CJ, Overturf GD, et al., eds. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics. 419-29, 2003.
- Peltola H, et al. The elimination of indigenous measles, mumps, and rubella from Finland by a 12-year, two-dose vaccination program. N Engl J Med. 331(21):1397-1402, 1994.
- Bennetto L, Scolding N. Inflammatory/post-infectious encephalomyelitis. J Neurol Neurosurg Psychiatry 2004;75(Suppl 1):i22-8.
- Fenichel GM. Neurological complications of immunization. AnnNeurol 1982;12(2):119-28.
- Guess HA, et al. Population-based studies of varicella complications. Pediatrics. 78(4 Pt 2):723-727, 1986.
- Recommendations of the Immunization Practices Advisory Committee (ACIP), Mumps Prevention. MMWR. 38(22):388-392, 397-400, 1989.
- Rubella vaccination during pregnancy--United States, 1971-1986. MMWR Morb Mortal Wkly Rep. 36(28):457-61, 1987.
- Rynn L, Cragan J, Correa A. Update on overall prevalence of major birth defects Atlanta, 1978-2005. CDC MMWR. 57(01):1-5, January 11, 2008.
- American College of Obstetricians and Gynecologists Frequently Asked Questions: Miscarriage and Molar Pregnancy, 2011.
- Bohlke K, Galil K, Jackson LA, et al. Postpartum varicella vaccination: Is the vaccine virus excreted in breast milk? Obstetrics and Gynecology. 102(5):970-977, 2003.
- Dolbear GL, Moffat J, Falkner C and Wojtowycz M. A Pilot Study: Is attenuated varicella virus present in breast milk after postpartum immunization? Obstetrics and Gynecology. 101(4 Suppl.):47S-47S, 2003.
- Weibel RE, et al. Clinical and laboratory studies of combined live measles, mumps, and rubella vaccines using the RA 27/3 rubella virus. Proc Soc Exp Biol Med. 165(2):323-326, 1980.
- Hilleman MR, Stokes J, Jr., Buynak EB, Weibel R, Halenda R, Goldner H. Studies of live attenuated measles virus vaccine in man: II. appraisal of efficacy. Am J Public Health. 52(2):44-56, 1962.
- Krugman S, Giles JP, Jacobs AM. Studies on an attenuated measles-virus vaccine: VI. clinical, antigenic and prophylactic effects of vaccine in institutionalized children. N Engl J Med. 263(4):174-7, 1960.
- Hilleman MR, Weibel RE, Buynak EB, Stokes J, Jr., Whitman JE, Jr. Live, attenuated mumps-virus vaccine. 4. Protective efficacy as measured in a field evaluation. N Engl J Med. 276(5):252-8, 1967.
- Sugg WC, Finger JA, Levine RH, Pagano JS. Field evaluation of live virus mumps vaccine. J Pediatr. 72(4):461-6, 1968.
- The Benevento and Compobasso Pediatricians Network for the Control of Vaccine-Preventable Diseases, D'Argenio P, Citarella A, Selvaggi MTM. Field evaluation of the clinical effectiveness of vaccines against pertussis, measles, rubella and mumps. Vaccine. 16(8):818-22, 1998.
- Furukawa T, Miyata T, Kondo K, Kuno K, Isomura S, Takekoshi T. Rubella vaccination during an epidemic. JAMA. 213(6):987-90, 1970.
- Vazquez M, et al. The effectiveness of the varicella vaccine in clinical practice. N Engl J Med. 344(13):955-960, 2001.
- Kuter B, et al. Ten year follow-up of healthy children who received one or two injections of varicella vaccine. Pediatr Infect Dis J. 23(2):132-137, 2004.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
No. 4171 — ProQuad is supplied as follows:
(1) a package of 10 single-dose vials of lyophilized vaccine, NDC: 0006-4171-00 (package A)
(2) a separate package of 10 vials of sterile water diluent (package B).
Storage
To maintain potency, ProQuad must be stored frozen between -58°F and +5°F (-50°C to -15°C). Use of dry ice may subject ProQuad to temperatures colder than -58°F (-50°C).
Before reconstitution, store the lyophilized vaccine in a freezer at a temperature between −58°F and +5°F (−50°C and −15°C) for up to 18 months. Any freezer (e.g., chest, frost-free) that reliably maintains an average temperature between −58°F and +5°F (−50°C and −15°C) and has a separate sealed freezer door is acceptable for storing ProQuad. Routine defrost cycling of a frost-free freezer is acceptable.
ProQuad may be stored at refrigerator temperature (36° to 46°F, 2° to 8°C) for up to 72 hours prior to reconstitution. Discard any ProQuad vaccine stored at 36° to 46°F which is not used within 72 hours of removal from 5°F (-15°C) storage.
Protect the vaccine from light at all times since such exposure may inactivate the vaccine viruses.
IF NOT USED IMMEDIATELY, THE RECONSTITUTED VACCINE MAY BE STORED AT ROOM TEMPERATURE, PROTECTED FROM LIGHT, FOR UP TO 30 MINUTES.
DISCARD RECONSTITUTED VACCINE IF IT IS NOT USED WITHIN 30 MINUTES.
DO NOT FREEZE RECONSTITUTED VACCINE.
Diluent should be stored separately at room temperature (68° to 77°F, 20° to 25°C), or in a refrigerator (36° to 46°F, 2° to 8°C).
For information regarding the product or questions regarding storage conditions, call 1-800-MERCK-90.
-
17 PATIENT COUNSELING INFORMATION
Instructions
Provide the required vaccine information to the patient, parent, or guardian.
Inform the patient, parent, or guardian of the benefits and risks associated with vaccination.
Inform the patient, parent, or guardian that the vaccine recipient should avoid use of salicylates for 6 weeks after vaccination with ProQuad [see Warnings and Precautions (5.10) and Drug Interactions (7.2)].
Instruct postpubertal females to avoid pregnancy for 3 months following vaccination [see Indications and Usage (1), Contraindications (4.4) and Use in Specific Populations (8.1)].
Inform patients, parents, or guardians that vaccination with ProQuad may not offer 100% protection from measles, mumps, rubella, and varicella infection.
Instruct patients, parents, or guardians to report any adverse reactions to their health care provider. The U.S. Department of Health and Human Services has established a Vaccine Adverse Event Reporting System (VAERS) to accept all reports of suspected adverse events after the administration of any vaccine, including but not limited to the reporting of events required by the National Childhood Vaccine Injury Act of 1986. For information or a copy of the vaccine reporting form, call the VAERS toll-free number at 1-800-822-7967, or report online at www.vaers.hhs.gov.
-
SPL UNCLASSIFIED SECTION
Dist. by: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USAFor patent information: www.merck.com/product/patent/home.html
Copyright © 2005-2020 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All rights reserved.uspi-v221-i-fro-rha-2003r010
-
PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Carton
NDC: 0006-4171-00
10 Single-dose 0.5-mL VialsA
Measles, Mumps, Rubella and Varicella
Virus Vaccine Live
ProQuad®STORE FROZEN
Measles vaccine: More attenuated Enders' Edmonston strain. Chick cell tissue culture origin.
Mumps vaccine: Jeryl Lynn™ strain. Chick cell tissue culture origin.
Rubella vaccine: Wistar RA 27/3 strain. Human diploid cell (WI-38) culture origin.
Varicella vaccine: Oka/Merck strain. Human diploid cell (MRC-5) culture origin.Contains no preservative. Contains trace quantities of neomycin.
Rx only
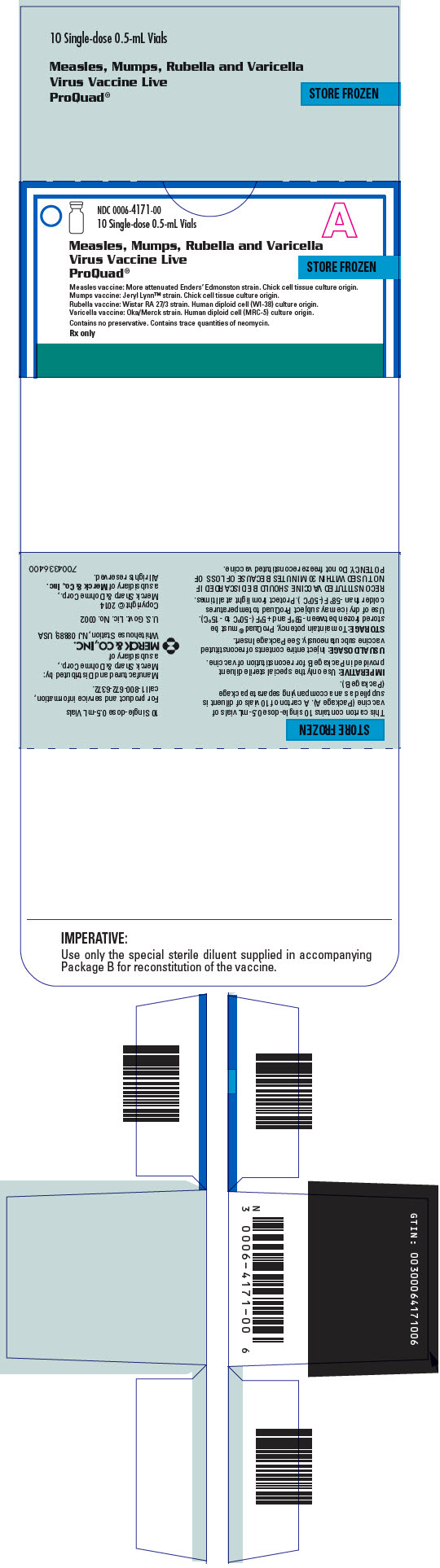
-
INGREDIENTS AND APPEARANCE
PROQUAD
measles, mumps, rubella and varicella virus vaccine live injection, powder, lyophilized, for suspensionProduct Information Product Type VACCINE Item Code (Source) NDC: 0006-4171 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MEASLES VIRUS STRAIN ENDERS' ATTENUATED EDMONSTON LIVE ANTIGEN (UNII: MFZ8I7277D) (MEASLES VIRUS STRAIN ENDERS' ATTENUATED EDMONSTON LIVE ANTIGEN - UNII:MFZ8I7277D) MEASLES VIRUS STRAIN ENDERS' ATTENUATED EDMONSTON LIVE ANTIGEN 1000 [TCID_50] in 0.5 mL MUMPS VIRUS STRAIN B LEVEL JERYL LYNN LIVE ANTIGEN (UNII: 47QB6MX9KU) (MUMPS VIRUS STRAIN B LEVEL JERYL LYNN LIVE ANTIGEN - UNII:47QB6MX9KU) MUMPS VIRUS STRAIN B LEVEL JERYL LYNN LIVE ANTIGEN 20000 [TCID_50] in 0.5 mL RUBELLA VIRUS STRAIN WISTAR RA 27/3 LIVE ANTIGEN (UNII: 52202H034Z) (RUBELLA VIRUS STRAIN WISTAR RA 27/3 LIVE ANTIGEN - UNII:52202H034Z) RUBELLA VIRUS STRAIN WISTAR RA 27/3 LIVE ANTIGEN 1000 [TCID_50] in 0.5 mL VARICELLA-ZOSTER VIRUS STRAIN OKA/MERCK LIVE ANTIGEN (UNII: GPV39ZGD8C) (VARICELLA-ZOSTER VIRUS STRAIN OKA/MERCK LIVE ANTIGEN - UNII:GPV39ZGD8C) VARICELLA-ZOSTER VIRUS STRAIN OKA/MERCK LIVE ANTIGEN 9772 [PFU] in 0.5 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 0.31 mg in 0.5 mL ALBUMIN BOVINE (UNII: 27432CM55Q) 0.5 ug in 0.5 mL GELATIN, UNSPECIFIED (UNII: 2G86QN327L) 11 mg in 0.5 mL MONOSODIUM GLUTAMATE (UNII: W81N5U6R6U) 0.4 mg in 0.5 mL NEOMYCIN (UNII: I16QD7X297) 16 ug in 0.5 mL POTASSIUM CHLORIDE (UNII: 660YQ98I10) 60 ug in 0.5 mL DIBASIC POTASSIUM PHOSPHATE (UNII: CI71S98N1Z) 36 ug in 0.5 mL POTASSIUM PHOSPHATE, MONOBASIC (UNII: 4J9FJ0HL51) 72 ug in 0.5 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.17 mg in 0.5 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 2.4 mg in 0.5 mL SODIUM PHOSPHATE, DIBASIC, UNSPECIFIED FORM (UNII: GR686LBA74) 0.34 mg in 0.5 mL SORBITOL (UNII: 506T60A25R) 1.8 mg in 0.5 mL SUCROSE (UNII: C151H8M554) 21 mg in 0.5 mL Product Characteristics Color YELLOW, PINK (clear pale yellow to light pink) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0006-4171-00 10 in 1 CARTON 1 NDC: 0006-4171-01 0.5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125108 07/01/2015 Labeler - Merck Sharp & Dohme Corp. (001317601)
Trademark Results [ProQuad]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 PROQUAD 75608198 2455941 Live/Registered |
MERCK SHARP & DOHME CORP. 1998-12-18 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.