DROXIA- hydroxyurea capsule
DROXIA by
Drug Labeling and Warnings
DROXIA by is a Prescription medication manufactured, distributed, or labeled by E.R. Squibb & Sons, L.L.C.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DROXIA safely and effectively. See full prescribing information for DROXIA.
DROXIA (hydroxyurea) capsules, for oral use
Initial U.S. Approval: 1967WARNING: MYELOSUPPRESSION AND MALIGNANCIES
See full prescribing information for complete boxed warning.
Myelosuppression: DROXIA may cause severe myelosuppression. Do not give if bone marrow function is markedly depressed. Monitor blood counts at baseline and throughout treatment. Interrupt treatment and reduce dose as necessary. (5.1)
Malignancies: Hydroxyurea is carcinogenic. Advise sun protection and monitor patients for malignancies. (5.2)RECENT MAJOR CHANGES
Warnings and Precautions, Pulmonary Toxicity (5.8) 7/2019
INDICATIONS AND USAGE
DROXIA is an antimetabolite indicated to reduce the frequency of painful crises and to reduce the need for blood transfusions in patients with sickle cell anemia with recurrent moderate to severe painful crises. (1)
DOSAGE AND ADMINISTRATION
- Initial dose: 15 mg/kg once daily. Monitor the patient’s blood count every two weeks. (2.1)
- The dose may be increased by 5 mg/kg/day every 12 weeks until a maximum tolerated dose or 35 mg/kg/day is reached if blood counts are in an acceptable range. (2.1)
- The dose is not increased if blood counts are between the acceptable range and toxic. Discontinue DROXIA until hematologic recovery if blood counts are considered toxic. Treatment may then be resumed after reducing the dose by 2.5 mg/kg/day from the dose associated with hematological toxicity. (2.1)
- Renal impairment: Reduce the dose of DROXIA by 50% in patients with creatinine clearance less than 60 mL/min. (2.2, 8.6, 12.3)
DOSAGE FORMS AND STRENGTHS
- Capsules: 200 mg, 300 mg, and 400 mg (3)
CONTRAINDICATIONS
- In patients who have demonstrated a previous hypersensitivity to hydroxyurea or any other component of its formulation. (4)
WARNINGS AND PRECAUTIONS
- Embryo-Fetal toxicity: Can cause fetal harm. Advise of potential risk to a fetus and use of effective contraception. (5.3, 8.1, 8.3)
- Vasculitic toxicities: Institute treatment and discontinue DROXIA if this occurs. (5.4)
- Live Vaccinations: Avoid live vaccine use in a patient taking DROXIA. (5.5)
- Risks with concomitant use of antiretroviral drugs: Pancreatitis, hepatotoxicity, and neuropathy have occurred. Monitor for signs and symptoms in patients with HIV infection using antiretroviral drugs; discontinue DROXIA and implement treatment. (5.6)
ADVERSE REACTIONS
Most common adverse reactions (≥30%) are hematological, gastrointestinal symptoms, and anorexia. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: MYELOSUPPRESSION AND MALIGNANCIES
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
2.2 Dose Modifications for Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
5.2 Malignancies
5.3 Embryo-Fetal Toxicity
5.4 Vasculitic Toxicities
5.5 Live Vaccinations
5.6 Risks with Concomitant Use of Antiretroviral Drugs
5.7 Macrocytosis
5.8 Pulmonary Toxicity
5.9 Laboratory Test Interference
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Increased Toxicity with Concomitant Use of Antiretroviral Drugs
7.2 Laboratory Test Interference
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
16.3 Handling and Disposal
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: MYELOSUPPRESSION AND MALIGNANCIES
Myelosuppression: DROXIA may cause severe myelosuppression. Monitor blood counts at baseline and throughout treatment. Interrupt treatment and reduce dose as necessary [see Warnings and Precautions (5.1)].
Malignancies: Hydroxyurea is carcinogenic. Advise sun protection and monitor patients for malignancies [see Warnings and Precautions (5.2)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
Table 1: Dosing Recommendation Based on Blood Count Dosing Regimen
Dose
Dose Modification Criteria
Monitoring Parameters
Initial Recommended
Dosing15 mg/kg/day as a single dose once daily based on the patient’s actual or ideal weight, whichever is less.
Monitor the patient’s blood count every 2 weeks [see Warnings and Precautions (5.1)]. Dosing Based on
Blood CountsIn an acceptable
rangeIncrease dose
5 mg/kg/day every 12 weeksMaximal dose:
35 mg/kg/day**Maximal dose is the highest dose that does not produce toxic blood counts over 24 consecutive weeks.
Increase dosing only if blood counts are in an acceptable range.
Do not increase if myelosuppression occurs.
Blood Counts Acceptable Range
neutrophils ≥2500 cells/mm3
platelets ≥95,000/mm3
hemoglobin >5.3 g/dL
reticulocytes ≥95,000/mm3 if
the hemoglobin
concentration <9 g/dLBetween acceptable
and toxic rangeDo not increase dose.
If blood counts are considered toxic, discontinue DROXIA until hematologic recovery.
Blood Counts Toxic Range
neutrophils <2000 cells/mm3
platelets <80,000/mm3
hemoglobin <4.5 g/dL
reticulocytes <80,000/mm3 if
the hemoglobin
concentration <9 g/dLDosing After
Hematologic
RecoveryReduce dose by
2.5 mg/kg/day.Reduce the dose from the dose associated with hematologic toxicity.
May titrate up or down every 12 weeks in 2.5 mg/kg/day increments.
The patient should be at a stable dose with no hematologic toxicity for 24 weeks.
Discontinue the treatment permanently if a patient develops hematologic toxicity twice.
Swallow DROXIA capsules whole. Do NOT open, break, or chew capsules because DROXIA is a cytotoxic drug. Patients must be able to follow directions regarding drug administration and their monitoring and care.
Fetal hemoglobin (HbF) levels may be used to evaluate the efficacy of DROXIA in clinical use. Obtain HbF levels every three to four months. Monitor for an increase in HbF of at least two-fold over the baseline value.
DROXIA causes macrocytosis, which may mask the incidental development of folic acid deficiency. Prophylactic administration of folic acid is recommended.
DROXIA is a cytotoxic drug. Follow applicable special handling and disposal procedures [see References (15)].
2.2 Dose Modifications for Renal Impairment
Reduce the dose of DROXIA by 50% in patients with creatinine clearance of less than 60 mL/min or with end-stage renal disease (ESRD) [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. Creatinine clearance values were obtained using 24-hour urine collections.
* On dialysis days, administer DROXIA to patients with ESRD following hemodialysis. Creatinine Clearance
(mL/min)
Recommended DROXIA Initial Dose
(mg/kg once daily)
≥60
15
<60 or ESRD*
7.5
Monitor the hematologic parameters closely in these patients.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Myelosuppression
Hydroxyurea causes severe myelosuppression. Treatment with hydroxyurea should not be initiated if bone marrow function is markedly depressed. Bone marrow suppression may occur, and leukopenia is generally its first and most common manifestation. Thrombocytopenia and anemia occur less often, and are seldom seen without a preceding leukopenia.
Some patients, treated at the recommended initial dose of 15 mg/kg/day, have experienced severe or life-threatening myelosuppression.
Evaluate hematologic status prior to and during treatment with DROXIA. Provide supportive care and modify dose or discontinue DROXIA as needed. Recovery from myelosuppression is usually rapid when therapy is interrupted.
5.2 Malignancies
Hydroxyurea is a human carcinogen. In patients receiving long-term hydroxyurea for myeloproliferative disorders, secondary leukemia has been reported. Skin cancer has also been reported in patients receiving long-term hydroxyurea. Advise protection from sun exposure and monitor for the development of secondary malignancies.
5.3 Embryo-Fetal Toxicity
Based on the mechanism of action and findings in animals, DROXIA can cause fetal harm when administered to a pregnant woman. Hydroxyurea was embryotoxic and teratogenic in rats and rabbits at doses 0.8 times and 0.3 times, respectively, the maximum recommended human daily dose on a mg/m2 basis. Advise pregnant women of the potential risk to a fetus [see Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during and after treatment with DROXIA for at least 6 months after therapy. Advise males of reproductive potential to use effective contraception during and after treatment with DROXIA for at least 1 year after therapy [see Use in Specific Populations (8.1, 8.3)].5.4 Vasculitic Toxicities
Cutaneous vasculitic toxicities, including vasculitic ulcerations and gangrene, have occurred in patients with myeloproliferative disorders during therapy with hydroxyurea. These vasculitic toxicities were reported most often in patients with a history of, or currently receiving, interferon therapy. If cutaneous vasculitic ulcers occur, institute treatment and discontinue DROXIA.
5.5 Live Vaccinations
Avoid use of live vaccine in patients taking DROXIA. Concomitant use of DROXIA with a live virus vaccine may potentiate the replication of the virus and/or may increase the adverse reaction of the vaccine because normal defense mechanisms may be suppressed by DROXIA. Vaccination with live vaccines in a patient receiving DROXIA may result in severe infection. Patient’s antibody response to vaccines may be decreased. Consider consultation with a specialist.
5.6 Risks with Concomitant Use of Antiretroviral Drugs
Pancreatitis, hepatotoxicity, and peripheral neuropathy have occurred when hydroxyurea was administered concomitantly with antiretroviral drugs, including didanosine and stavudine [see Drug Interactions (7.1)].
5.7 Macrocytosis
DROXIA may cause macrocytosis, which is self-limiting, and is often seen early in the course of treatment. The morphologic change resembles pernicious anemia, but is not related to vitamin B12 or folic acid deficiency. This may mask the diagnosis of pernicious anemia. Prophylactic administration of folic acid is recommended.
5.8 Pulmonary Toxicity
Interstitial lung disease including pulmonary fibrosis, lung infiltration, pneumonitis, and alveolitis/allergic alveolitis (including fatal cases) have been reported in patients treated for myeloproliferative neoplasm. Safety and effectiveness have not been established for the use of DROXIA in the treatment of myeloproliferative neoplasms and the use is not approved by the FDA. Monitor patients developing pyrexia, cough, dyspnea, or other respiratory symptoms frequently, investigate and treat promptly. Discontinue DROXIA and manage with corticosteroids. [see Adverse Reactions (6.1)].
5.9 Laboratory Test Interference
Interference with Uric Acid, Urea, or Lactic Acid Assays is possible, rendering falsely elevated results of these in patients treated with hydroxyurea [see Drug Interactions (7.2)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described in detail in other labeling sections:
- Myelosuppression [see Warnings and Precautions (5.1)]
- Malignancies [see Warnings and Precautions (5.2)]
- Vasculitic toxicities [see Warnings and Precautions (5.4)]
- Risks with concomitant use of antiretroviral drugs [see Warnings and Precautions (5.6)]
- Macrocytosis [see Warnings and Precautions (5.7)]
- Pulmonary Toxicity [see Warnings and Precautions (5.8)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1 Clinical Trial Experience
In 299 patients treated for sickle cell anemia in the Multicenter Study of Hydroxyurea in Sickle Cell Anemia, the most common adverse reactions were hematologic, with neutropenia, and low reticulocyte and platelet levels necessitating temporary cessation in almost all patients. Hematologic recovery usually occurred in two weeks.
Other adverse reactions include hair loss, macrocytosis, bleeding, and melanonychia.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of hydroxyurea in the treatment of neoplastic diseases. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency.
- Reproductive System and Breast disorders: azoospermia, and oligospermia
- Gastrointestinal disorders: stomatitis, nausea, vomiting, diarrhea, and constipation
- Metabolism and Nutrition disorders: anorexia
- Skin and subcutaneous tissue disorders: maculopapular rash, skin ulceration, cutaneous lupus erythematosus, dermatomyositis-like skin changes, peripheral and facial erythema, hyperpigmentation, nail hyperpigmentation, atrophy of skin and nails, scaling, violet papules, and alopecia
- Renal and urinary disorders: dysuria, elevations in serum uric acid, blood urea nitrogen (BUN), and creatinine levels
- Nervous system disorders: headache, dizziness, drowsiness, disorientation, hallucinations, and convulsions
- General disorders: fever, chills, malaise, edema, and asthenia
- Hepatobiliary disorders: elevation of hepatic enzymes, cholestasis, and hepatitis
- Respiratory disorders: diffuse pulmonary infiltrates, dyspnea, and pulmonary fibrosis, interstitial lung disease, pneumonitis, alveolitis, allergic alveolitis and cough
- Immune disorders: systemic lupus erythematosus
- Hypersensitivity: Drug-induced fever (pyrexia) (>39°C, >102°F) requiring hospitalization has been reported concurrently with gastrointestinal, pulmonary, musculoskeletal, hepatobiliary, dermatological or cardiovascular manifestations. Onset typically occurred within 6 weeks of initiation and resolved upon discontinuation of hydroxyurea. Upon re-administration fever re-occurred typically within 24 hours.
-
7 DRUG INTERACTIONS
7.1 Increased Toxicity with Concomitant Use of Antiretroviral Drugs
Pancreatitis
In patients with HIV infection during therapy with hydroxyurea and didanosine, with or without stavudine, fatal and nonfatal pancreatitis have occurred. Hydroxyurea is not indicated for the treatment of HIV infection; however, if patients with HIV infection are treated with hydroxyurea, and in particular, in combination with didanosine and/or stavudine, close monitoring for signs and symptoms of pancreatitis is recommended. Permanently discontinue therapy with hydroxyurea in patients who develop signs and symptoms of pancreatitis.
Hepatotoxicity
Hepatotoxicity and hepatic failure resulting in death have been reported during postmarketing surveillance in patients with HIV infection treated with hydroxyurea and other antiretroviral drugs. Fatal hepatic events were reported most often in patients treated with the combination of hydroxyurea, didanosine, and stavudine. Avoid this combination.
7.2 Laboratory Test Interference
Interference with Uric Acid, Urea, or Lactic Acid Assays
Studies have shown that there is an analytical interference of hydroxyurea with the enzymes (urease, uricase, and lactate dehydrogenase) used in the determination of urea, uric acid, and lactic acid, rendering falsely elevated results of these in patients treated with hydroxyurea.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
DROXIA can cause fetal harm based on findings from animal studies and the drug’s mechanism of action [see Clinical Pharmacology (12.1)]. There are no data with DROXIA use in pregnant women to inform a drug-associated risk. In animal reproduction studies, administration of hydroxyurea to pregnant rats and rabbits during organogenesis produced embryotoxic and teratogenic effects at doses 0.8 times and 0.3 times, respectively, the maximum recommended human daily dose on a mg/m2 basis (see Data). Advise women of the potential risk to a fetus and to avoid becoming pregnant while being treated with DROXIA.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%–4% and 15%–20%, respectively.
Data
Animal Data
Hydroxyurea has been demonstrated to be a potent teratogen in a wide variety of animal models, including mice, hamsters, cats, miniature swine, dogs, and monkeys at doses within 1-fold of the human dose given on a mg/m2 basis. Hydroxyurea is embryotoxic and causes fetal malformations (partially ossified cranial bones, absence of eye sockets, hydrocephaly, bipartite sternebrae, missing lumbar vertebrae) at 180 mg/kg/day (about 0.8 times the maximum recommended human daily dose on a mg/m2 basis) in rats and at 30 mg/kg/day (about 0.3 times the maximum recommended human daily dose on a mg/m2 basis) in rabbits. Embryotoxicity was characterized by decreased fetal viability, reduced live litter sizes, and developmental delays. Hydroxyurea crosses the placenta. Single doses of ≥375 mg/kg (about 1.7 times the maximum recommended human daily dose on a mg/m2 basis) to rats caused growth retardation and impaired learning ability.
8.3 Females and Males of Reproductive Potential
Pregnancy Testing
Verify the pregnancy status of females of reproductive potential prior to initiating DROXIA therapy.
Contraception
Females
DROXIA can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during and after treatment with DROXIA for at least 6 months after therapy. Advise females to immediately report pregnancy.
Males
DROXIA may damage spermatozoa and testicular tissue, resulting in possible genetic abnormalities. Males with female sexual partners of reproductive potential should use effective contraception during and after treatment with DROXIA for at least 1 year after therapy [see Nonclinical Toxicology (13.1)].
Infertility
Males
Based on findings in animals and humans, male fertility may be compromised by treatment with DROXIA. Azoospermia or oligospermia, sometimes reversible, has been observed in men. Inform male patients about the possibility of sperm conservation before the start of therapy [see Adverse Reactions (6) and Nonclinical Toxicology (13.1)].
8.5 Geriatric Use
Clinical studies of DROXIA did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Elderly patients may be more sensitive to the effects of hydroxyurea and may require a lower dose regimen. Hydroxyurea is excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Dosage and Administration (2.2)].
8.6 Renal Impairment
The exposure to hydroxyurea is higher in patients with creatinine clearance of less than 60 mL/min. Reduce dosage and closely monitor the hematologic parameters when DROXIA is to be administered to these patients [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Acute mucocutaneous toxicity has been reported in patients receiving hydroxyurea at dosages several times the therapeutic dose. Soreness, violet erythema, edema on palms and soles followed by scaling of hands and feet, severe generalized hyperpigmentation of the skin, and stomatitis have been observed.
-
11 DESCRIPTION
DROXIA® (hydroxyurea capsules, USP) is available for oral use as capsules containing 200 mg, 300 mg, and 400 mg hydroxyurea. Inactive ingredients include citric acid, gelatin, lactose, magnesium stearate, sodium phosphate, titanium dioxide, and capsule colorants: FD&C Blue No. 1 and FD&C Green No. 3 (200 mg capsules); D&C Red No. 28, D&C Red No. 33, and FD&C Blue No. 1 (300 mg capsules); D&C Red No. 28, D&C Red No. 33, and D&C Yellow No. 10 (400 mg capsules).
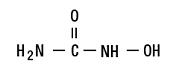
Hydroxyurea is a white to off-white crystalline powder. It is hygroscopic and freely soluble in water, but practically insoluble in alcohol. The empirical formula is CH4N2O2 and it has a molecular weight of 76.05. Its structural formula is:
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism by which hydroxyurea produces its cytotoxic and cytoreductive effects is not known. However, various studies support the hypothesis that hydroxyurea causes an immediate inhibition of DNA synthesis by acting as a ribonucleotide reductase inhibitor, without interfering with the synthesis of ribonucleic acid or of protein.
The mechanisms by which DROXIA produces its beneficial effects in patients with sickle cell anemia (SCA) are uncertain. Known pharmacologic effects of DROXIA that may contribute to its beneficial effects include increasing hemoglobin F levels in red blood cells (RBCs), decreasing neutrophils, increasing the water content of RBCs, increasing deformability of sickled cells, and altering the adhesion of RBCs to endothelium.
12.3 Pharmacokinetics
Absorption
Following oral administration of DROXIA, hydroxyurea reaches peak plasma concentrations in 1 to 4 hours. Mean peak plasma concentrations and AUCs increase more than proportionally with increase of dose.
There are no data on the effect of food on the absorption of hydroxyurea.
Distribution
Hydroxyurea distributes throughout the body with a volume of distribution approximating total body water.
Hydroxyurea concentrates in leukocytes and erythrocytes.
Metabolism
Up to 60% of an oral dose undergoes conversion through saturable hepatic metabolism and a minor pathway of degradation by urease found in intestinal bacteria.
Excretion
In patients with sickle cell anemia, the mean cumulative urinary recovery of hydroxyurea was about 40% of the administered dose.
Specific Populations
Renal Impairment
The effect of renal impairment on the pharmacokinetics of hydroxyurea was assessed in adult patients with sickle cell disease and renal impairment. Patients with normal renal function (creatinine clearance [CrCl] >80 mL/min), mild (CrCl 50-80 mL/min), moderate (CrCl =30-<50 mL/min), or severe (<30 mL/min) renal impairment received a single oral dose of 15 mg/kg hydroxyurea. Creatinine clearance values were obtained using 24-hour urine collections. Patients with ESRD received two doses of 15 mg/kg separated by 7 days; the first was given following a 4-hour hemodialysis session, the second prior to hemodialysis. The exposure to hydroxyurea (mean AUC) in patients with CrCl <60 mL/min and those with ESRD was 64% higher than in patients with normal renal function (CrCl >60 mL/min). Reduce the dose of DROXIA when it is administered to patients with creatinine clearance of <60 mL/min or with ESRD following hemodialysis [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Conventional long-term studies to evaluate the carcinogenic potential of DROXIA have not been performed. However, intraperitoneal administration of 125 to 250 mg/kg hydroxyurea (about 0.6-1.2 times the maximum recommended human oral daily dose on a mg/m2 basis) thrice weekly for 6 months to female rats increased the incidence of mammary tumors in rats surviving to 18 months compared to control. Hydroxyurea is mutagenic in vitro to bacteria, fungi, protozoa, and mammalian cells. Hydroxyurea is clastogenic in vitro (hamster cells, human lymphoblasts) and in vivo (SCE assay in rodents, mouse micronucleus assay). Hydroxyurea causes the transformation of rodent embryo cells to a tumorigenic phenotype.
Hydroxyurea administered to male rats at 60 mg/kg/day (about 0.3 times the maximum recommended human daily dose on a mg/m2 basis) produced testicular atrophy, decreased spermatogenesis, and significantly reduced their ability to impregnate females.
-
14 CLINICAL STUDIES
The efficacy of hydroxyurea in sickle cell anemia was assessed in a large clinical study (Multicenter Study of Hydroxyurea in Sickle Cell Anemia) (see Table 2).
The study was a randomized, double-blind, placebo-controlled trial that evaluated 299 adult patients (≥18 years) with moderate to severe disease (≥3 painful crises yearly). The trial was stopped by the Data Safety Monitoring Committee, after accrual was completed but before the scheduled 24 months of follow-up was completed in all patients, based on observations of fewer painful crises among patients receiving hydroxyurea.
Compared to placebo treatment, treatment with hydroxyurea resulted in a significant decrease in the yearly rate of painful crises, the yearly rate of painful crises requiring hospitalization, the incidence of chest syndrome, the number of patients transfused, and units of blood transfused. Hydroxyurea treatment significantly increased the median time to both first and second painful crises.
Although patients with 3 or more painful crises during the preceding 12 months were eligible for the study, most of the benefit in crisis reduction was seen in the patients with 6 or more painful crises during the preceding 12 months.
Table 2: Results from the Multicenter Study of Hydroxyurea in Sickle Cell Anemia Event Hydroxyurea
(N=152)Placebo
(N=147)Percent Change Versus Placebo P-value * A painful crisis was defined in the study as acute sickling-related pain that resulted in a visit to a medical facility, that lasted more than 4 hours, and that required treatment with a parenteral narcotic or NSAID. Chest syndrome, priapism, and hepatic sequestration were also included in this definition. Median yearly rate of painful crises*
2.5
4.6
−46
=0.001
Median yearly rate of painful crises requiring hospitalization
1.0
2.5
−60
=0.0027
Median time to first painful crisis (months)
2.76
1.35
+104
=0.014
Median time to second painful crisis (months)
6.58
4.13
+59
=0.0024
Incidence of chest syndrome (# episodes)
56
101
−45
=0.003
Number of patients transfused
55
79
−30
=0.002
Number of units of blood transfused
423
670
−37
=0.003
In patients with SCA treated with hydroxyurea, fetal hemoglobin (HbF) increases 4 to 12 weeks after initiation of treatment. In general, average HbF levels correlate with dose and plasma level with possible plateauing at higher dosages.
A clear relation between reduction in crisis frequency and increased HbF or F-cell levels has not been demonstrated. The dose-related cytoreductive effects of hydroxyurea, particularly on neutrophils, was the factor most strongly correlated with reduced crisis frequency.
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
DROXIA® (hydroxyurea capsules, USP) is supplied in HDPE bottles with a plastic safety screw cap. Each bottle contains 60 capsules. DROXIA is supplied in the following strengths:
200 mg opaque blue-green capsules, marked in black ink with “DROXIA” and “6335” (NDC: 0003-6335-17).
300 mg opaque purple capsules, marked in black ink with “DROXIA” and “6336” (NDC: 0003-6336-17).
400 mg opaque reddish-orange capsules, marked in black ink with “DROXIA” and “6337” (NDC: 0003-6337-17).
16.2 Storage
Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F) [see USP Controlled Room Temperature]. Keep tightly closed.
16.3 Handling and Disposal
DROXIA is a cytotoxic drug. Follow applicable special handling and disposal procedures [see References (15)].
To decrease the risk of contact, advise caregivers to wear disposable gloves when handling DROXIA or bottles containing DROXIA. Wash hands with soap and water before and after contact with the bottle or capsules when handling DROXIA. Do not open DROXIA capsules. Avoid exposure to crushed or opened capsules. If contact with crushed or opened capsules occurs on the skin, wash affected area immediately and thoroughly with soap and water. If contact with crushed or opened capsules occurs on the eye(s), the affected area should be flushed thoroughly with water or isotonic eyewash designated for that purpose for at least 15 minutes. If the powder from the capsule is spilled, immediately wipe it up with a damp disposable towel and discard in a closed container, such as a plastic bag; as should the empty capsules. The spill areas should then be cleaned three times using a detergent solution followed by clean water. Keep the medication away from children and pets. Contact your doctor for instructions on how to dispose of outdated capsules.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
- There is a risk of myelosuppression. Monitoring blood counts every two weeks throughout the duration of therapy should be emphasized to patients taking DROXIA [see Warnings and Precautions (5.1)]. Advise patients to report signs and symptoms of infection or bleeding immediately.
- Advise patients that there is a risk of cutaneous vasculitic toxicities and secondary malignancies including leukemia and skin cancers.
- Advise use of sun protection [see Warnings and Precautions (5.2, 5.4)].
- Advise patients to inform their healthcare provider if they have received or are planning to receive vaccinations while taking DROXIA as this may result in a severe infection [see Warnings and Precautions (5.5)].
- Advise females of reproductive potential of the potential risk to a fetus and to inform their healthcare provider of a known or suspected pregnancy. Advise females and males of reproductive potential to use contraception during and after treatment with DROXIA [see Warnings and Precautions (5.3) and Use in Specific Populations (8.1, 8.3)].
- Advise females to discontinue breastfeeding during treatment with DROXIA [see Use in Specific Populations (8.2)].
- Patients with HIV infection should contact their physician for signs and symptoms of pancreatitis, hepatic events, and peripheral neuropathy [see Warnings and Precautions (5.6)].
- Advise patients of the symptoms of potential pulmonary toxicity and instruct them to seek prompt medical attention in the event of pyrexia, cough, dyspnea, or other respiratory symptoms [see Warnings and Precautions (5.8)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
Medication Guide
DROXIA® (drock-SEE-yuh)
(hydroxyurea)
capsulesWhat is the most important information I should know about DROXIA?
DROXIA can cause serious side effects including:- Low blood counts are common with DROXIA, including low red blood cells, white blood cells, and platelets, and can be severe and life-threatening. If your white blood cell count becomes very low, you are at increased risk for infection. Your healthcare provider will check your blood cell counts before and during treatment with DROXIA. Your healthcare provider may change your dose or tell you to stop taking DROXIA if you have low blood cell counts. Tell your healthcare provider right away if you get any of the following symptoms:
- Fever
- feeling very tired
- chills
- shortness of breath
- body aches
- bleeding or unexplained bruising
- Cancer. Some people have developed cancer, such as leukemia and skin cancer, after taking DROXIA for a long time. Your healthcare provider will check you for cancer. You should protect your skin from the sun using sunblock, hats, and sun-protective clothing.
- DROXIA can harm your unborn baby.
For females taking DROXIA who can become pregnant:
- You should talk with your healthcare provider about the risks of DROXIA to your unborn baby.
- You should use effective birth control during treatment with DROXIA and for at least 6 months after treatment.
- Your healthcare provider will perform a pregnancy test before you start treatment with DROXIA.
- You should avoid becoming pregnant during treatment with DROXIA. Tell your healthcare provider right away if you become pregnant or think you may be pregnant.
For males taking DROXIA:
- DROXIA can affect your sperm. If you have a female sexual partner who can become pregnant, you should use a condom during treatment with DROXIA and for at least 1 year after treatment.
DROXIA may cause fertility problems in males. Talk to your healthcare provider if this is a concern for you.
See "What are the possible side effects of DROXIA?" for more information about side effects.
What is DROXIA?
DROXIA is a prescription medicine that is used to reduce the frequency of painful crises and reduce the need for blood transfusions in people with sickle cell anemia with recurrent moderate to severe painful crises.
It is not known if DROXIA is safe and effective in children.Do not take DROXIA if you are allergic to hydroxyurea or any of the ingredients in DROXIA. See the end of this leaflet for a list of the ingredients in DROXIA.
Before taking DROXIA, tell your healthcare provider about all of your medical conditions, including if you:
- have kidney problems or are receiving hemodialysis.
- have human immunodeficiency virus (HIV). Taking DROXIA with certain HIV medicines can cause serious reactions and may lead to death. Tell your healthcare provider if you take an HIV medicine.
- have increased level of uric acid in your blood (hyperuricemia).
- have a history of receiving interferon therapy or are currently receiving interferon therapy.
- have leg wounds or ulcers
- plan to receive any vaccinations. You should not receive "live vaccines" during treatment with DROXIA.
- are pregnant or plan to become pregnant. See "What is the most important information I should know about DROXIA?"
- are breastfeeding or plan to breastfeed. DROXIA can pass into your breast milk. Do not breastfeed during treatment with DROXIA.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I take DROXIA?
- Take DROXIA exactly as your healthcare provider tells you. DROXIA is taken 1 time a day.
- If you take too much DROXIA, call your healthcare provider or go to the nearest hospital emergency room right away.
- DROXIA capsules must be handled with care. To decrease the risk of exposure, you or your caregivers should do the following when handling DROXIA:
- Wear disposable gloves when handling DROXIA capsules or bottles containing DROXIA.
- Wash your hands with soap and water before and after handling DROXIA capsules or bottles containing DROXIA.
- Do NOT open, break, or chew the capsules.
- Avoid contact with crushed or opened capsules. If contact from crushed or opened capsules happens on the skin, wash the skin area right away and thoroughly with soap and water. If contact from crushed or opened capsules happens in the eyes, flush the eyes thoroughly with water or isotonic eyewash used for that purpose for at least 15 minutes.
- If the powder from the capsule is spilled, wipe it up right away with a damp disposable towel. Throw the damp disposable towel and the empty capsules away in a closed container, such as a plastic bag. The spill areas should then be cleaned three times using a detergent solution followed by clean water.
What are the possible side effects of DROXIA?
DROXIA may cause serious side effects, including:- See "What is the most important information I should know about DROXIA?"
- Skin ulcers and death of tissue (gangrene) have happened in people who take DROXIA. This has happened most often in people who receive interferon therapy or have a history of interferon therapy. Your healthcare provider will stop treatment with DROXIA if you develop any skin ulcers.
- Enlarged red blood cells (macrocytosis). Macrocytosis is common in people who take DROXIA and can make it difficult to detect a decrease of folic acid. Your healthcare provider may prescribe a folic acid supplement for you.
- Respiratory (breathing) problems. Some people have developed life-threatening respiratory conditions called interstitial lung disease. Your healthcare provider may tell you to stop taking DROXIA if you develop respiratory problems. Tell your healthcare provider right away if you get any of the following symptoms:
- fever
- shortness of breath
- cough
The most common side effects of DROXIA include:
- reduced blood counts
- bleeding
- mouth ulcers
- nausea
- diarrhea or constipation
- loss of appetite
These are not all the possible side effects of DROXIA.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.How should I store DROXIA?
- Store DROXIA at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep the DROXIA bottle tightly closed.
- Call your healthcare provider for instructions on how to throw away (dispose of) DROXIA that is out of date.
Keep DROXIA and all medicines out of the reach of children. Keep DROXIA away from pets.
General information about the safe and effective use of DROXIA
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use DROXIA for a condition for which it was not prescribed. Do not give DROXIA to other people, even if they have the same symptoms you have. It may harm them. You can ask your healthcare provider or pharmacist for information about DROXIA that is written for health professionals.What are the ingredients of DROXIA?
Active ingredient: hydroxyurea
Inactive ingredients: citric acid, gelatin, lactose, magnesium stearate, sodium phosphate, titanium dioxide, and capsule colorants: FD&C Blue No. 1 and FD&C Green No. 3 (200 mg capsules); D&C Red No. 28, D&C Red No. 33, and FD&C Blue No. 1 (300 mg capsules); D&C Red No. 28, D&C Red No. 33, and D&C Yellow No. 10 (400 mg capsules).
Manufactured for: Bristol-Myers Squibb Company, Princeton, New Jersey 08543 USA
For more information, go to www.BMS.com or call 1-800-721-5072.This Patient Information has been approved by the U.S. Food and Drug Administration.
1375188A2 Revised: July 2019
-
DROXIA 200 mg capsules Representative Packaging
See How Supplied section for a complete list of available packages of DROXIA.
60 CAPSULES
NDC: 0003-6335-17
DROXIA®
(hydroxyurea capsules, USP)
200 mg per capsule
Rx only
Bristol-Myers Squibb
-
DROXIA 300 mg capsules Representative Packaging
60 CAPSULES
NDC: 0003-6336-17
DROXIA®
(hydroxyurea capsules, USP)
300 mg per capsule
Rx only
Bristol-Myers Squibb
-
DROXIA 400 mg capsules Representative Packaging
60 CAPSULES
NDC: 0003-6337-17
DROXIA®
(hydroxyurea capsules, USP)
400 mg per capsule
Rx only
Bristol-Myers Squibb
-
INGREDIENTS AND APPEARANCE
DROXIA
hydroxyurea capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0003-6336 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength hydroxyurea (UNII: X6Q56QN5QC) (hydroxyurea - UNII:X6Q56QN5QC) hydroxyurea 300 mg Inactive Ingredients Ingredient Name Strength citric acid monohydrate (UNII: 2968PHW8QP) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) magnesium stearate (UNII: 70097M6I30) sodium phosphate (UNII: SE337SVY37) titanium dioxide (UNII: 15FIX9V2JP) D&C Red No. 28 (UNII: 767IP0Y5NH) D&C Red No. 33 (UNII: 9DBA0SBB0L) FD&C Blue No. 1 (UNII: H3R47K3TBD) Product Characteristics Color PURPLE Score no score Shape CAPSULE Size 19mm Flavor Imprint Code DROXIA;6336;DROXIA;6336 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0003-6336-17 60 in 1 BOTTLE; Type 0: Not a Combination Product 07/16/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016295 06/01/2009 DROXIA
hydroxyurea capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0003-6335 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength hydroxyurea (UNII: X6Q56QN5QC) (hydroxyurea - UNII:X6Q56QN5QC) hydroxyurea 200 mg Inactive Ingredients Ingredient Name Strength citric acid monohydrate (UNII: 2968PHW8QP) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) magnesium stearate (UNII: 70097M6I30) sodium phosphate (UNII: SE337SVY37) titanium dioxide (UNII: 15FIX9V2JP) FD&C Blue No. 1 (UNII: H3R47K3TBD) FD&C Green No. 3 (UNII: 3P3ONR6O1S) Product Characteristics Color TURQUOISE (blue-green) Score no score Shape CAPSULE Size 16mm Flavor Imprint Code DROXIA;6335;DROXIA;6335 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0003-6335-17 60 in 1 BOTTLE; Type 0: Not a Combination Product 07/16/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016295 06/01/2009 DROXIA
hydroxyurea capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0003-6337 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength hydroxyurea (UNII: X6Q56QN5QC) (hydroxyurea - UNII:X6Q56QN5QC) hydroxyurea 400 mg Inactive Ingredients Ingredient Name Strength citric acid monohydrate (UNII: 2968PHW8QP) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) LACTOSE, UNSPECIFIED FORM (UNII: J2B2A4N98G) magnesium stearate (UNII: 70097M6I30) sodium phosphate (UNII: SE337SVY37) titanium dioxide (UNII: 15FIX9V2JP) D&C Red No. 28 (UNII: 767IP0Y5NH) D&C Red No. 33 (UNII: 9DBA0SBB0L) D&C Yellow No. 10 (UNII: 35SW5USQ3G) Product Characteristics Color ORANGE Score no score Shape CAPSULE Size 22mm Flavor Imprint Code DROXIA;6337;DROXIA;6337 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0003-6337-17 60 in 1 BOTTLE; Type 0: Not a Combination Product 07/16/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA016295 06/01/2009 Labeler - E.R. Squibb & Sons, L.L.C. (011550092)
Trademark Results [DROXIA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 DROXIA 75318230 2222043 Live/Registered |
BRISTOL-MYERS SQUIBB COMPANY 1997-07-02 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.