FINASTERIDE tablet, film coated
FINASTERIDE by
Drug Labeling and Warnings
FINASTERIDE by is a Prescription medication manufactured, distributed, or labeled by H.J. Harkins Company, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- INDICATIONS & USAGE
-
DOSAGE & ADMINISTRATION
- Finasteride tablets may be administered with or without meals.
- The recommended dose of finasteride tablets is one tablet (1 mg) taken once daily.
- In general, daily use for three months or more is necessary before benefit is observed. Continued use is recommended to sustain benefit, which should be re-evaluated periodically. Withdrawal of treatment leads to reversal of effect within 12 months.
- DOSAGE FORMS & STRENGTHS
-
CONTRAINDICATIONS
Finasteride is contraindicated in the following:
- Pregnancy. Finasteride use is contraindicated in women when they are or may potentially be pregnant. Because of the ability of Type II 5α-reductase inhibitors to inhibit the conversion of testosterone to 5α-dihydrotestosterone (DHT), finasteride may cause abnormalities of the external genitalia of a male fetus of a pregnant woman who receives finasteride. If this drug is used during pregnancy, or if pregnancy occurs while taking this drug, the pregnant woman should be apprised of the potential hazard to the male fetus. [See WARNINGS AND PRECAUTIONS (5.1), USE IN SPECIFIC POPULATIONS (8.1), HOW SUPPLIED/STORAGE AND HANDLING (16) and PATIENT COUNSELING INFORMATION (17.1).] In female rats, low doses of finasteride administered during pregnancy have produced abnormalities of the external genitalia in male offspring.
- Hypersensitivity to any component of this medication.
-
WARNINGS AND PRECAUTIONS
5.1 Exposure of Women — Risk to Male Fetus
Finasteride is not indicated for use in women. Women should not handle crushed or broken finasteride tablets when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to a male fetus. Finasteride tablets are coated and will prevent contact with the active ingredient during normal handling, provided that the tablets have not been broken or crushed. [See INDICATIONS AND USAGE (1), CONTRAINDICATIONS (4), USE IN SPECIFIC POPULATIONS (8.1), HOW SUPPLIED/STORAGE AND HANDLING (16) and PATIENT COUNSELING INFORMATION (17.1).]
5.2 Effects on Prostate Specific Antigen (PSA)
In clinical studies with finasteride, 1 mg in men 18 to 41 years of age, the mean value of serum prostate specific antigen (PSA) decreased from 0.7 ng/mL at baseline to 0.5 ng/mL at Month 12. Further, in clinical studies with finasteride, 5 mg when used in older men who have benign prostatic hyperplasia (BPH), PSA levels are decreased by approximately 50%. Other studies with finasteride, 5 mg showed it may also cause decreases in serum PSA in the presence of prostate cancer. These findings should be taken into account for proper interpretation of serum PSA when evaluating men treated with finasteride. Any confirmed increase from the lowest PSA value while on finasteride 1 mg may signal the presence of prostate cancer and should be evaluated, even if PSA levels are still within the normal range for men not taking a 5α-reductase inhibitor. Non-compliance to therapy with finasteride 1 mg may also affect PSA test results.
5.3 Increased Risk of High-Grade Prostate Cancer with 5α-Reductase Inhibitors
Men aged 55 and over with a normal digital rectal examination and PSA ≤3.0 ng/mL at baseline taking finasteride 5 mg/day (5 times the dose of finasteride 1 mg) in the 7-year Prostate Cancer Prevention Trial (PCPT) had an increased risk of Gleason score 8 to 10 prostate cancer (finasteride 1.8% vs placebo 1.1%). [See ADVERSE REACTIONS (6.1). ] Similar results were observed in a 4-year placebo-controlled clinical trial with another 5α-reductase inhibitor (dutasteride, AVODART) (1% dutasteride vs 0.5% placebo). 5α-reductase inhibitors may increase the risk of development of high-grade prostate cancer. Whether the effect of 5α-reductase inhibitors to reduce prostate volume, or study-related factors, impacted the results of these studies has not been established.
5.4 Pediatric Patients
Finasteride is not indicated for use in pediatric patients [see USE IN SPECIFIC POPULATIONS (8.4)] .
-
DRUG INTERACTIONS
7.1 Cytochrome P450-Linked Drug Metabolizing Enzyme System
No drug interactions of clinical importance have been identified. Finasteride does not appear to affect the cytochrome P450-linked drug-metabolizing enzyme system. Compounds that have been tested in man include antipyrine, digoxin, propranolol, theophylline, and warfarin and no clinically meaningful interactions were found.
7.2 Other Concomitant Therapy
Although specific interaction studies were not performed, finasteride doses of 1 mg or more were concomitantly used in clinical studies with acetaminophen, acetylsalicylic acid, α-blockers, analgesics, angiotensin-converting enzyme (ACE) inhibitors, anticonvulsants, benzodiazepines, beta blockers, calcium-channel blockers, cardiac nitrates, diuretics, H 2 antagonists, HMG-CoA reductase inhibitors, prostaglandin synthetase inhibitors (also referred to as NSAIDs), and quinolone anti-infectives without evidence of clinically significant adverse interactions.
-
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category X [see CONTRAINDICATIONS (4)].
Finasteride is contraindicated for use in women who are or may become pregnant. Finasteride is a Type II 5α-reductase inhibitor that prevents conversion of testosterone to 5α-dihydrotestosterone (DHT), a hormone necessary for normal development of male genitalia. In animal studies, finasteride caused abnormal development of external genitalia in male fetuses. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the male fetus.
Abnormal male genital development is an expected consequence when conversion of testosterone to 5α-dihydrotestosterone (DHT) is inhibited by 5α-reductase inhibitors. These outcomes are similar to those reported in male infants with genetic 5α-reductase deficiency. Women could be exposed to finasteride through contact with crushed or broken finasteride tablets or semen from a male partner taking finasteride. With regard to finasteride exposure through the skin, finasteride tablets are coated and will prevent skin contact with finasteride during normal handling if the tablets have not been crushed or broken. Women who are pregnant or may become pregnant should not handle crushed or broken finasteride tablets because of possible exposure of a male fetus. If a pregnant woman comes in contact with crushed or broken finasteride tablets, the contact area should be washed immediately with soap and water. With regard to potential finasteride exposure through semen, a study has been conducted in men receiving finasteride 1 mg/day that measured finasteride concentrations in semen[see CLINICAL PHARMACOLOGY (12.3)].
In an embryo-fetal development study, pregnant rats received finasteride during the period of major organogenesis (gestation days 6 to 17). At maternal doses of oral finasteride approximately 1 to 684 times the recommended human dose (RHD) of 1 mg/day (based on AUC at animal doses of 0.1 to 100 mg/kg/day) there was a dose-dependent increase in hypospadias that occurred in 3.6 to 100% of male offspring. Exposure multiples were estimated using data from nonpregnant rats. Days 16 to 17 of gestation is a critical period in male fetal rats for differentiation of the external genitalia. At oral maternal doses approximately 0.2 times the RHD (based on AUC at animal dose of 0.03 mg/kg/day), male offspring had decreased prostatic and seminal vesicular weights, delayed preputial separation and transient nipple development. Decreased anogenital distance occurred in male offspring of pregnant rats that received approximately 0.02 times the RHD (based on AUC at animal dose of 0.003 mg/kg/day). No abnormalities were observed in female offspring exposed to any dose of finasteride in utero.
No developmental abnormalities were observed in the offspring of untreated females mated with finasteride-treated male rats that received approximately 488 times the RHD (based on AUC at animal dose of 80 mg/kg/day). Slightly decreased fertility was observed in male offspring after administration of about 20 times the RHD (based on AUC at animal dose of 3 mg/kg/day) to female rats during late gestation and lactation. No effects on fertility were seen in female offspring under these conditions.
No evidence of male external genital malformations or other abnormalities were observed in rabbit fetuses exposed to finasteride during the period of major organogenesis (gestation days 6 to 18) at maternal doses up to 100 mg/kg/day (finasteride exposure levels were not measured in rabbits). However, this study may not have included the critical period for finasteride effects on development of male external genitalia in the rabbit.
The fetal effects of maternal finasteride exposure during the period of embryonic and fetal development were evaluated in the rhesus monkey (gestation days 20 to 100), in a species and development period more predictive of specific effects in humans than the studies in rats and rabbits. Intravenous administration of finasteride to pregnant monkeys at doses as high as 800 ng/day (estimated maximal blood concentration of 1.86 ng/mL or about 930 times the highest estimated exposure of pregnant women to finasteride from semen of men taking 1 mg/day) resulted in no abnormalities in male fetuses. In confirmation of the relevance of the rhesus model for human fetal development, oral administration of a dose of finasteride (2 mg/kg/day or approximately 120,000 times the highest estimated blood levels of finasteride from semen of men taking 1 mg/day) to pregnant monkeys resulted in external genital abnormalities in male fetuses. No other abnormalities were observed in male fetuses and no finasteride-related abnormalities were observed in female fetuses at any dose.
8.3 Nursing Mothers
Finasteride is not indicated for use in women.
It is not known whether finasteride is excreted in human milk.
8.4 Pediatric Use
Finasteride is not indicated for use in pediatric patients.
Safety and effectiveness in pediatric patients have not been established.
8.5 Geriatric Use
Clinical efficacy studies with finasteride did not include subjects aged 65 and over. Based on the pharmacokinetics of finasteride 5 mg, no dosage adjustment is necessary in the elderly for finasteride[see CLINICAL PHARMACOLOGY (12.3)] . However the efficacy of finasteride in the elderly has not been established.
8.6 Hepatic Impairment
Caution should be exercised in the administration of finasteride in those patients with liver function abnormalities, as finasteride is metabolized extensively in the liver [see CLINICAL PHARMACOLOGY (12.3)].
8.7 Renal Impairment
No dosage adjustment is necessary in patients with renal impairment [see CLINICAL PHARMACOLOGY (12.3)] .
-
OVERDOSAGE
In clinical studies, single doses of finasteride up to 400 mg and multiple doses of finasteride up to 80 mg/day for three months did not result in adverse reactions. Until further experience is obtained, no specific treatment for an overdose with finasteride can be recommended.
Significant lethality was observed in male and female mice at single oral doses of 1500 mg/m 2 (500 mg/kg) and in female and male rats at single oral doses of 2360 mg/m 2 (400 mg/kg) and 5900 mg/m 2(1000 mg/kg), respectively.
-
DESCRIPTION
Finasteride tablets, USP contain finasteride as the active ingredient. Finasteride, a synthetic 4-azasteroid compound, is a specific inhibitor of steroid Type II 5α-reductase, an intracellular enzyme that converts the androgen testosterone into 5α-dihydrotestosterone (DHT).
The chemical name of finasteride is N-tert-Butyl-3-oxo-4-aza-5α-androst-1-ene-17β-carboxamide. The empirical formula of finasteride is C 23H 36N 2O 2 and its molecular weight is 372.55. Its structural formula is:
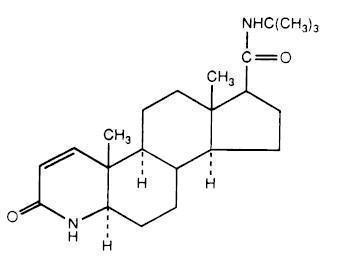
Finasteride is a white crystalline powder with a melting point near 250°C. It is freely soluble in chloroform and in lower alcohol solvents but is practically insoluble in water.
Finasteride tablets, USP are film-coated tablets for oral administration. Each tablet contains 1 mg of finasteride and the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, pregelatinized starch (maize), sodium starch glycolate, lauroyl macrogolglycerides, magnesium stearate, hypromellose, titanium dioxide, polyethylene glycol, iron oxide red, and iron oxide yellow.
-
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of a tumorigenic effect was observed in a 24-month study in Sprague-Dawley rats receiving doses of finasteride up to 160 mg/kg/day in males and 320 mg/kg/day in females. These doses produced respective systemic exposure in rats of 888 and 2192 times those observed in man receiving the recommended human dose of 1 mg/day. All exposure calculations were based on calculated AUC (0-24 hr) for animals and mean AUC (0-24 hr) for man (0.05 µg∙hr/mL).
In a 19-month carcinogenicity study in CD-1 mice, a statistically significant (p≤0.05) increase in the incidence of testicular Leydig cell adenomas was observed at 1824 times the human exposure (250 mg/kg/day). In mice at 184 times the human exposure, estimated (25 mg/kg/day) and in rats at 312 times the human exposure (≥40 mg/kg/day) an increase in the incidence of Leydig cell hyperplasia was observed. A positive correlation between the proliferative changes in the Leydig cells and an increase in serum LH levels (2- to 3-fold above control) has been demonstrated in both rodent species treated with high doses of finasteride. No drug-related Leydig cell changes were seen in either rats or dogs treated with finasteride for 1 year at 240 and 2800 times (20 mg/kg/day and 45 mg/kg/day, respectively), or in mice treated for 19 months at 18.4 times the human exposure, estimated (2.5 mg/kg/day).
No evidence of mutagenicity was observed in an in vitro bacterial mutagenesis assay, a mammalian cell mutagenesis assay, or in an in vitro alkaline elution assay. In an in vitro chromosome aberration assay, using Chinese hamster ovary cells, there was a slight increase in chromosome aberrations. In an in vivochromosome aberration assay in mice, no treatment-related increase in chromosome aberration was observed with finasteride at the maximum tolerated dose of 250 mg/kg/day (1824 times the human exposure) as determined in the carcinogenicity studies.
In sexually mature male rabbits treated with finasteride at 4344 times the human exposure (80 mg/kg/day) for up to 12 weeks, no effect on fertility, sperm count, or ejaculate volume was seen. In sexually mature male rats treated with 488 times the human exposure (80 mg/kg/day), there were no significant effects on fertility after 6 or 12 weeks of treatment; however, when treatment was continued for up to 24 or 30 weeks, there was an apparent decrease in fertility, fecundity, and an associated significant decrease in the weights of the seminal vesicles and prostate. All these effects were reversible within 6 weeks of discontinuation of treatment. No drug-related effect on testes or on mating performance has been seen in rats or rabbits. This decrease in fertility in finasteride-treated rats is secondary to its effect on accessory sex organs (prostate and seminal vesicles) resulting in failure to form a seminal plug. The seminal plug is essential for normal fertility in rats but is not relevant in man.
-
CLINICAL STUDIES
14.1 Studies in Men
The efficacy of finasteride was demonstrated in men (88% Caucasian) with mild to moderate androgenetic alopecia (male pattern hair loss) between 18 and 41 years of age. In order to prevent seborrheic dermatitis which might confound the assessment of hair growth in these studies, all men, whether treated with finasteride or placebo, were instructed to use a specified, medicated, tar-based shampoo (Neutrogena T/Gel ® Shampoo) during the first 2 years of the studies.
There were three double-blind, randomized, placebo-controlled studies of 12-month duration. The two primary endpoints were hair count and patient self-assessment; the two secondary endpoints were investigator assessment and ratings of photographs. In addition, information was collected regarding sexual function (based on a self-administered questionnaire) and non-scalp body hair growth. The three studies were conducted in 1879 men with mild to moderate, but not complete, hair loss. Two of the studies enrolled men with predominantly mild to moderate vertex hair loss (n=1553). The third enrolled men having mild to moderate hair loss in the anterior mid-scalp area with or without vertex balding (n=326).
Studies in Men with Vertex Baldness
Of the men who completed the first 12 months of the two vertex baldness trials, 1215 elected to continue in double-blind, placebo-controlled, 12-month extension studies. There were 547 men receiving finasteride for both the initial study and first extension periods (up to 2 years of treatment) and 60 men receiving placebo for the same periods. The extension studies were continued for 3 additional years, with 323 men on finasteride and 23 on placebo entering the fifth year of the study.
In order to evaluate the effect of discontinuation of therapy, there were 65 men who received finasteride for the initial 12 months followed by placebo in the first 12-month extension period. Some of these men continued in additional extension studies and were switched back to treatment with finasteride, with 32 men entering the fifth year of the study. Lastly, there were 543 men who received placebo for the initial 12 months followed by finasteride in the first 12-month extension period. Some of these men continued in additional extension studies receiving finasteride, with 290 men entering the fifth year of the study (see FIGURE 1 below).
Hair counts were assessed by photographic enlargements of a representative area of active hair loss. In these two studies in men with vertex baldness, significant increases in hair count were demonstrated at 6 and 12 months in men treated with finasteride, while significant hair loss from baseline was demonstrated in those treated with placebo. At 12 months there was a 107-hair difference from placebo (p<0.001, finasteride [n=679] vs placebo [n=672]) within a 1-inch diameter circle (5.1 cm 2). Hair count was maintained in those men taking finasteride for up to 2 years, resulting in a 138-hair difference between treatment groups (p<0.001, finasteride [n=433] vs placebo [n=47]) within the same area. In men treated with finasteride, the maximum improvement in hair count compared to baseline was achieved during the first 2 years. Although the initial improvement was followed by a slow decline, hair count was maintained above baseline throughout the 5 years of the studies. Furthermore, because the decline in the placebo group was more rapid, the difference between treatment groups also continued to increase throughout the studies, resulting in a 277-hair difference (p<0.001, finasteride [n=219] vs placebo [n=15]) at 5 years (see FIGURE 1 below).
Patients who switched from placebo to finasteride (n=425) had a decrease in hair count at the end of the initial 12-month placebo period, followed by an increase in hair count after 1 year of treatment with finasteride. This increase in hair count was less (56 hairs above original baseline) than the increase (91 hairs above original baseline) observed after 1 year of treatment in men initially randomized to finasteride. Although the increase in hair count, relative to when therapy was initiated, was comparable between these two groups, a higher absolute hair count was achieved in patients who were started on treatment with finasteride in the initial study. This advantage was maintained through the remaining 3 years of the studies. A change of treatment from finasteride to placebo (n=48) at the end of the initial 12 months resulted in reversal of the increase in hair count 12 months later, at 24 months (see FIGURE 1 below).
At 12 months, 58% of men in the placebo group had further hair loss (defined as any decrease in hair count from baseline), compared with 14% of men treated with finasteride. In men treated for up to 2 years, 72% of men in the placebo group demonstrated hair loss, compared with 17% of men treated with finasteride. At 5 years, 100% of men in the placebo group demonstrated hair loss, compared with 35% of men treated with finasteride.
Figure 1:

Patient self-assessment was obtained at each clinic visit from a self-administered questionnaire, which included questions on their perception of hair growth, hair loss, and appearance. This self-assessment demonstrated an increase in amount of hair, a decrease in hair loss, and improvement in appearance in men treated with finasteride. Overall improvement compared with placebo was seen as early as 3 months (p<0.05), with improvement maintained over 5 years.
Investigator assessment was based on a 7-point scale evaluating increases or decreases in scalp hair at each patient visit. This assessment showed significantly greater increases in hair growth in men treated with finasteride compared with placebo as early as 3 months (p<0.001). At 12 months, the investigators rated 65% of men treated with finasteride as having increased hair growth compared with 37% in the placebo group. At 2 years, the investigators rated 80% of men treated with finasteride as having increased hair growth compared with 47% of men treated with placebo. At 5 years, the investigators rated 77% of men treated with finasteride as having increased hair growth, compared with 15% of men treated with placebo.
An independent panel rated standardized photographs of the head in a blinded fashion based on increases or decreases in scalp hair using the same 7-point scale as the investigator assessment. At 12 months, 48% of men treated with finasteride had an increase as compared with 7% of men treated with placebo. At 2 years, an increase in hair growth was demonstrated in 66% of men treated with finasteride, compared with 7% of men treated with placebo. At 5 years, 48% of men treated with finasteride demonstrated an increase in hair growth, 42% were rated as having no change (no further visible progression of hair loss from baseline) and 10% were rated as having lost hair when compared to baseline. In comparison, 6% of men treated with placebo demonstrated an increase in hair growth, 19% were rated as having no change and 75% were rated as having lost hair when compared to baseline.
A 48-week, placebo-controlled study designed to assess by phototrichogram the effect of finasteride on total and actively growing (anagen) scalp hairs in vertex baldness enrolled 212 men with androgenetic alopecia. At baseline and 48 weeks, total and anagen hair counts were obtained in a 1-cm 2 target area of the scalp. Men treated with finasteride showed increases from baseline in total and anagen hair counts of 7 hairs and 18 hairs, respectively, whereas men treated with placebo had decreases of 10 hairs and 9 hairs, respectively. These changes in hair counts resulted in a between-group difference of 17 hairs in total hair count (p<0.001) and 27 hairs in anagen hair count (p<0.001), and an improvement in the proportion of anagen hairs from 62% at baseline to 68% for men treated with finasteride.
Other Results in Vertex Baldness Studies
A sexual function questionnaire was self-administered by patients participating in the two vertex baldness trials to detect more subtle changes in sexual function. At Month 12, statistically significant differences in favor of placebo were found in 3 of 4 domains (sexual interest, erections, and perception of sexual problems). However, no significant difference was seen in the question on overall satisfaction with sex life.
In one of the two vertex baldness studies, patients were questioned on non-scalp body hair growth. Finasteride did not appear to affect non-scalp body hair.
Study in Men with Hair Loss in the Anterior Mid-Scalp Area
A study of 12-month duration, designed to assess the efficacy of finasteride in men with hair loss in the anterior mid-scalp area, also demonstrated significant increases in hair count compared with placebo. Increases in hair count were accompanied by improvements in patient self-assessment, investigator assessment, and ratings based on standardized photographs. Hair counts were obtained in the anterior mid-scalp area, and did not include the area of bitemporal recession or the anterior hairline.
Summary of Clinical Studies in Men
Clinical studies were conducted in men aged 18 to 41 with mild to moderate degrees of androgenetic alopecia. All men treated with finasteride or placebo received a tar-based shampoo (Neutrogena T/Gel® Shampoo) during the first 2 years of the studies. Clinical improvement was seen as early as 3 months in the patients treated with finasteride and led to a net increase in scalp hair count and hair regrowth. In clinical studies for up to 5 years, treatment with finasteride slowed the further progression of hair loss observed in the placebo group. In general, the difference between treatment groups continued to increase throughout the 5 years of the studies.
Ethnic Analysis of Clinical Data from Men
In a combined analysis of the two studies on vertex baldness, mean hair count changes from baseline were 91 vs -19 hairs (finasteride vs placebo) among Caucasians (n=1185), 49 vs -27 hairs among Blacks (n=84), 53 vs -38 hairs among Asians (n=17), 67 vs 5 hairs among Hispanics (n=45) and 67 vs -15 hairs among other ethnic groups (n=20). Patient self-assessment showed improvement across racial groups with finasteride treatment, except for satisfaction of the frontal hairline and vertex in Black men, who were satisfied overall.
14.2 Study in Women
In a study involving 137 postmenopausal women with androgenetic alopecia who were treated with finasteride (n=67) or placebo (n=70) for 12 months, effectiveness could not be demonstrated. There was no improvement in hair counts, patient self-assessment, investigator assessment, or ratings of standardized photographs in the women treated with finasteride when compared with the placebo group [see INDICATIONS AND USAGE (1)].
- 88436-1 - Section Title Not Found In Database
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FINASTERIDE
finasteride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 76519-1204 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FINASTERIDE (UNII: 57GNO57U7G) (FINASTERIDE - UNII:57GNO57U7G) FINASTERIDE 1 mg Product Characteristics Color brown (Reddish) Score no score Shape ROUND Size 7mm Flavor Imprint Code F1 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 76519-1204-3 30 in 1 VIAL, PLASTIC; Type 0: Not a Combination Product 04/26/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA091643 04/26/2018 Labeler - H.J. Harkins Company, Inc. (147681894) Establishment Name Address ID/FEI Business Operations H.J. Harkins Company, Inc. 147681894 manufacture(76519-1204) , relabel(76519-1204) , repack(76519-1204)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
