FETROJA- cefiderocol sulfate tosylate injection, powder, for solution
Fetroja by
Drug Labeling and Warnings
Fetroja by is a Prescription medication manufactured, distributed, or labeled by Shionogi Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use FETROJA® safely and effectively. See full prescribing information for FETROJA.
FETROJA (cefiderocol) for injection, for intravenous use
Initial U.S. Approval: 2019INDICATIONS AND USAGE
FETROJA is a cephalosporin antibacterial indicated in patients 18 years of age or older who have limited or no alternative treatment options, for the treatment of complicated urinary tract infections (cUTI), including pyelonephritis caused by susceptible Gram-negative microorganisms. (1.1)
Approval of this indication is based on limited clinical safety and efficacy data for FETROJA. (1.1, 14)
To reduce the development of drug-resistant bacteria and maintain the effectiveness of FETROJA and other antibacterial drugs, FETROJA should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. (1.2)
DOSAGE AND ADMINISTRATION
- Administer 2 grams of FETROJA for injection every 8 hours by intravenous (IV) infusion over 3 hours in patients with creatinine clearance (CLcr) 60 to 119 mL/min. (2.1)
- Dose adjustments are required for patients with CLcr less than 60 mL/min and for patients with CLcr 120 mL/min or greater. (2.2)
- See full prescribing information for instructions on preparation of FETROJA doses. (2.3)
- See full prescribing information for drug compatibilities. (2.4)
DOSAGE FORMS AND STRENGTHS
For injection: 1 gram of cefiderocol as a lyophilized powder for reconstitution in single-dose vials. (3)
CONTRAINDICATIONS
FETROJA is contraindicated in patients with a known history of severe hypersensitivity to cefiderocol and other beta-lactam antibacterial drugs or other components of FETROJA. (4)
WARNINGS AND PRECAUTIONS
- Increase in All-Cause Mortality in Patients With Carbapenem-Resistant Gram-Negative Bacterial Infections: An increase in all-cause mortality was observed in FETROJA-treated patients compared to those treated with best available therapy (BAT). Reserve FETROJA for use in patients who have limited or no alternative treatment options for the treatment of cUTI. Closely monitor the clinical response to therapy in patients with cUTI. (5.1)
- Hypersensitivity Reactions: Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving beta-lactam antibacterial drugs. Hypersensitivity was observed with FETROJA. Cross-hypersensitivity may occur in patients with a history of penicillin allergy. If an allergic reaction occurs, discontinue FETROJA. (5.2)
- Clostridioides difficile-Associated Diarrhea (CDAD): CDAD has been reported with nearly all systemic antibacterial agents, including FETROJA. Evaluate if diarrhea occurs. (5.3)
- Seizures and Other Central Nervous System (CNS) Adverse Reactions: CNS adverse reactions such as seizures have been reported with FETROJA. If focal tremors, myoclonus, or seizures occur, evaluate patients to determine whether FETROJA should be discontinued. (5.4)
ADVERSE REACTIONS
The most frequently occurring adverse reactions in greater than or equal to 2% of patients treated with FETROJA were diarrhea, infusion site reactions, constipation, rash, candidiasis, cough, elevations in liver tests, headache, hypokalemia, nausea, and vomiting. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Shionogi Inc. at 1-800-849-9707 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Use alternate testing methods to confirm positive results of dipstick tests (urine protein, ketones, or occult blood). (7.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Complicated Urinary Tract Infections (cUTI), Including Pyelonephritis
1.2 Usage
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Dosage Adjustments In Patients With Renal Impairment (CLcr Less Than 60 mL/min and CLcr 120 mL/min or Greater)
2.3 Preparation of FETROJA Solution for Administration
2.4 Drug Compatibility
2.5 Storage of Reconstituted Solutions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Increase in All-Cause Mortality in Patients With Carbapenem-Resistant Gram-Negative Bacterial Infections
5.2 Hypersensitivity Reactions
5.3 Clostridioides difficile-Associated Diarrhea (CDAD)
5.4 Seizures and Other Central Nervous System (CNS) Adverse Reactions
5.5 Development of Drug-Resistant Bacteria
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Drug/Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Complicated Urinary Tract Infections, Including Pyelonephritis
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Complicated Urinary Tract Infections (cUTI), Including Pyelonephritis
FETROJA® is indicated in patients 18 years of age or older who have limited or no alternative treatment options for the treatment of complicated urinary tract infections (cUTIs), including pyelonephritis caused by the following susceptible Gram-negative microorganisms: Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas aeruginosa, and Enterobacter cloacae complex.
Approval of this indication is based on limited clinical safety and efficacy data for FETROJA [see Clinical Studies (14.1)].
1.2 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of FETROJA and other antibacterial drugs, FETROJA should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dosage of FETROJA is 2 grams administered every 8 hours by intravenous (IV) infusion over 3 hours in adults with a creatinine clearance (CLcr) of 60 to 119 mL/min.
Dosage adjustment is recommended for patients with CLcr less than 60 mL/min or for patients with CLcr 120 mL/min or greater [see Dosage and Administration (2.2)].
The recommended duration of treatment with FETROJA is 7 to 14 days. The duration of therapy should be guided by the severity of infection and the patient's clinical status for up to 14 days.
2.2 Dosage Adjustments In Patients With Renal Impairment (CLcr Less Than 60 mL/min and CLcr 120 mL/min or Greater)
Dosage Adjustments in Patients with CLcr Less Than 60 mL/min
Dosage adjustment of FETROJA is recommended in patients with CLcr less than 60 mL/min (Table 1). For patients with fluctuating renal function, monitor CLcr and adjust dosage accordingly.
Table 1 Recommended Dosage of FETROJA for Patients with CLcr less than 60 mL/min Estimated Creatinine Clearance (CLcr)* Dose Frequency Infusion Time ESRD = end-stage renal disease; HD = hemodialysis. - * CLcr = creatinine clearance estimated by Cockcroft-Gault equation.
- † Cefiderocol is removed by hemodialysis (HD); thus, complete hemodialysis (HD) at the latest possible time before the start of cefiderocol dosing.
Patients with CLcr 30 to 59 mL/min 1.5 grams Every 8 hours 3 hours Patients with CLcr 15 to 29 mL/min 1 gram Every 8 hours 3 hours ESRD Patients (CLcr less than 15 mL/min) with or without intermittent HD† 0.75 gram Every 12 hours 3 hours 2.3 Preparation of FETROJA Solution for Administration
FETROJA is supplied as a sterile, lyophilized powder that must be reconstituted and subsequently diluted using aseptic technique prior to intravenous infusion.
Preparation of Doses
Reconstitute the powder for injection in the FETROJA vial with 10 mL of either 0.9% sodium chloride injection, USP or 5% dextrose injection, USP and gently shake to dissolve. Allow the vial(s) to stand until the foaming generated on the surface has disappeared (typically within 2 minutes). The final volume of the reconstituted solution will be approximately 11.2 mL. The reconstituted solution is for intravenous infusion only after dilution in an appropriate infusion solution.
To prepare the required doses, withdraw the appropriate volume of reconstituted solution from the vial according to Table 2 below. Add the withdrawn volume to an infusion bag containing 100 mL of 0.9% sodium chloride injection, USP or 5% dextrose injection, USP [see Dosage and Administration (2.4)].
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. FETROJA infusions are clear, colorless solutions. Discard any unused FETROJA solution in the vial (see Table 2).
Table 2 Preparation of FETROJA Doses FETROJA Dose Number of 1-gram FETROJA Vials to be Reconstituted Volume to Withdraw from Reconstituted Vial(s) Total Volume of FETROJA Reconstituted Solution for Further Dilution into at Least 100 mL 2 grams 2 vials 11.2 mL (entire contents) of each vial 22.4 mL 1.5 grams 2 vials 11.2 mL (entire contents) of first vial AND 5.6 mL from second vial 16.8 mL 1 gram 1 vial 11.2 mL (entire contents) 11.2 mL 0.75 gram 1 vial 8.4 mL 8.4 mL 2.4 Drug Compatibility
FETROJA solution for administration is compatible with:
- 0.9% sodium chloride injection, USP
- 5% dextrose injection, USP
The compatibility of FETROJA solution for administration with solutions containing other drugs or other diluents has not been established.
2.5 Storage of Reconstituted Solutions
Reconstituted FETROJA
Upon reconstitution with the appropriate diluent, the reconstituted FETROJA solution in the vial should be immediately transferred and diluted into the infusion bag. Reconstituted FETROJA can be stored for up to 1 hour at room temperature. Discard any unused reconstituted solution.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
FETROJA is contraindicated in patients with a known history of severe hypersensitivity to cefiderocol or other beta-lactam antibacterial drugs, or any other component of FETROJA [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Increase in All-Cause Mortality in Patients With Carbapenem-Resistant Gram-Negative Bacterial Infections
An increase in all-cause mortality was observed in patients treated with FETROJA as compared to best available therapy (BAT) in a multinational, randomized, open-label trial in critically-ill patients with carbapenem-resistant Gram-negative bacterial infections (NCT02714595). Patients with nosocomial pneumonia, bloodstream infections, sepsis, or cUTI were included in the trial. BAT regimens varied according to local practices and consisted of 1 to 3 antibacterial drugs with activity against Gram-negative bacteria. Most of the BAT regimens contained colistin.
The increase in all-cause mortality occurred in patients treated for nosocomial pneumonia, bloodstream infections, or sepsis. The 28-Day all-cause mortality was higher in patients treated with FETROJA than in patients treated with BAT [25/101 (24.8%) vs. 9/49 (18.4%), treatment difference 6.4%, 95% CI (-8.6, 19.2)]. All-cause mortality remained higher in patients treated with FETROJA than in patients treated with BAT through Day 49 [34/101 (33.7%) vs. 10/49 (20.4%), treatment difference 13.3%, 95% CI (-2.5, 26.9)]. Generally, deaths were in patients with infections caused by Gram-negative organisms, including non-fermenters such as Acinetobacter baumannii, Stenotrophomonas maltophilia, and Pseudomonas aeruginosa, and were the result of worsening or complications of infection, or underlying comorbidities. The cause of the increase in mortality has not been established. The safety and efficacy of FETROJA has not been established for the treatment of nosocomial pneumonia, bloodstream infections, or sepsis.
Reserve FETROJA for use in patients who have limited or no alternative treatment options for the treatment of cUTI [see Indications and Usage (1.1)]. Closely monitor the clinical response to therapy in patients with cUTI.
5.2 Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions and serious skin reactions have been reported in patients receiving beta-lactam antibacterial drugs. Hypersensitivity was observed in FETROJA clinical trials [see Adverse Reactions (6.1)]. These reactions are more likely to occur in individuals with a history of beta-lactam hypersensitivity and/or a history of sensitivity to multiple allergens. There have been reports of individuals with a history of penicillin hypersensitivity who have experienced severe reactions when treated with cephalosporins. Before therapy with FETROJA is instituted, inquire about previous hypersensitivity reactions to cephalosporins, penicillins, or other beta-lactam antibacterial drugs. Discontinue FETROJA if an allergic reaction occurs.
5.3 Clostridioides difficile-Associated Diarrhea (CDAD)
Clostridioides difficile-Associated diarrhea (CDAD) has been reported for nearly all systemic antibacterial agents, including FETROJA. CDAD may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of C. difficile.
C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary because CDAD has been reported to occur more than 2 months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, antibacterial drugs not directed against C. difficile may need to be discontinued. Manage fluid and electrolyte levels as appropriate, supplement protein intake, monitor antibacterial treatment of C. difficile, and institute surgical evaluation as clinically indicated.
5.4 Seizures and Other Central Nervous System (CNS) Adverse Reactions
Cephalosporins, including FETROJA, have been implicated in triggering seizures [see Adverse Reactions (6.1)]. Nonconvulsive status epilepticus (NCSE), encephalopathy, coma, asterixis, neuromuscular excitability, and myoclonia have been reported with cephalosporins particularly in patients with a history of epilepsy and/or when recommended dosages of cephalosporins were exceeded due to renal impairment. Adjust FETROJA dosing based on creatinine clearance [see Dosage and Administration (2.2)]. Anticonvulsant therapy should be continued in patients with known seizure disorders. If CNS adverse reactions including seizures occur, patients should undergo a neurological evaluation to determine whether FETROJA should be discontinued.
5.5 Development of Drug-Resistant Bacteria
Prescribing FETROJA in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and may increase the risk for development of drug-resistant bacteria [see Indications and Usage (1.2)].
-
6 ADVERSE REACTIONS
The following serious adverse reactions are described in greater detail in the Warnings and Precautions section:
- Increase in All-Cause Mortality in Patients With Carbapenem-Resistant Gram-Negative Bacterial Infections [see Warnings and Precautions (5.1)]
- Hypersensitivity Reactions [see Warnings and Precautions (5.2)]
- Clostridioides difficile-Associated Diarrhea (CDAD) [see Warnings and Precautions (5.3)]
- Seizures and Other Central Nervous System Adverse Reactions [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trial Experience in cUTI, including Pyelonephritis
FETROJA was evaluated in an active-controlled clinical trial in patients with cUTI, including pyelonephritis (Trial 1). In this trial, 300 patients received FETROJA 2 grams every 8 hours infused over 1 hour (or a renally-adjusted dose) and 148 patients were treated with imipenem/cilastatin 1 gram/1 gram every 8 hours infused over 1 hour (or a renally-adjusted dose). The median age of treated patients across treatment arms was 65 years (range 18 to 93 years), with approximately 53% of patients aged greater than or equal to 65. Approximately 96% of patients were white, most were from Europe, and 55% were female. Patients across treatment arms received treatment for a median duration of 9 days.
Serious Adverse Reactions and Adverse Reactions Leading to Discontinuation
In Trial 1, a total of 14/300 (4.7%) patients treated with FETROJA and 12/148 (8.1%) of patients treated with imipenem/cilastatin experienced serious adverse reactions. One death (0.3%) occurred in 300 patients treated with FETROJA as compared to none treated with imipenem/cilastatin. Discontinuation of treatment due to any adverse reaction occurred in 5/300 (1.7%) of patients treated with FETROJA and 3/148 (2.0%) of patients treated with imipenem/cilastatin. Specific adverse reactions leading to treatment discontinuation in patients who received FETROJA included diarrhea (0.3%), drug hypersensitivity (0.3%), and increased hepatic enzymes (0.3%).
Common Adverse Reactions
Table 3 lists the most common selected adverse reactions occurring in ≥ 2% of patients receiving FETROJA in the cUTI trial.
Table 3 Selected Adverse Reactions Occurring in ≥2% of Patients Receiving FETROJA in the cUTI Trial Adverse Reaction FETROJA*
(N = 300)Imipenem/Cilastatin†
(N = 148)cUTI = complicated urinary tract infections - * 2 grams IV over 1 hour every 8 hours (with dosing adjustment based on renal function)
- † 1 gram IV over 1 hour every 8 hours (with dosing adjustment based on renal function and body weight)
- ‡ Infusion site reactions include infusion site erythema, inflammation, pain, pruritis, injection site pain, and phlebitis.
- § Rash includes rash macular, rash maculopapular, erythema, skin irritation.
- ¶ Candidiasis includes oral or vulvovaginal candidiasis, candiduria.
- # Elevations in liver tests include alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl transferase, blood alkaline phosphatase, hepatic enzyme increased.
- Þ Hypokalemia includes blood potassium decreased.
Diarrhea 4% 6% Infusion site reactions‡ 4% 5% Constipation 3% 4% Rash§ 3% <1% Candidiasis¶ 2% 3% Cough 2% <1% Elevations in liver tests# 2% <1% Headache 2% 5% HypokalemiaÞ 2% 3% Nausea 2% 4% Vomiting 2% 1% Other Adverse Reactions of FETROJA in the cUTI Trial
The following selected adverse reactions were reported in FETROJA-treated patients at a rate of less than 2% in the cUTI trial:
Blood and lymphatic disorders: thrombocytosis
Cardiac disorders: congestive heart failure, bradycardia, atrial fibrillation
Gastrointestinal disorders: abdominal pain, dry mouth, stomatitis
General system disorders: pyrexia, peripheral edema
Hepatobiliary disorders: cholelithiasis, cholecystitis, gallbladder pain
Immune system disorders: drug hypersensitivity
Infections and infestations: Clostridioides difficile infection
Laboratory Investigations: prolonged prothrombin time (PT) and prothrombin time international normalized ratio (PT-INR), red blood cells urine positive, creatine phosphokinase increase
Metabolism and nutrition disorders: decreased appetite, hypocalcemia, fluid overload
Nervous system disorders: dysgeusia, seizure
Respiratory, thoracic, and mediastinal disorders: dyspnea, pleural effusion
Skin and subcutaneous tissue disorders: pruritis
Psychiatric disorders: insomnia, restlessness
- 7 DRUG INTERACTIONS
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on FETROJA use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes.
Available data from published prospective cohort studies, case series, and case reports over several decades with cephalosporin use in pregnant women have not established drug-associated risks of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data).
Developmental toxicity studies with cefiderocol administered during organogenesis to rats and mice showed no evidence of embryo-fetal toxicity, including drug-induced fetal malformations, at doses providing exposure levels 1.4 times (rats) or 2 times (mice) higher than the average observed in cUTI patients receiving the maximum recommended daily dose.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
While available studies cannot definitively establish the absence of risk, published data from prospective cohort studies, case series, and case reports over several decades have not identified an association with cephalosporin use during pregnancy, and major birth defects, miscarriage, or other adverse maternal or fetal outcomes. Available studies have methodologic limitations, including small sample size, retrospective data collection, and inconsistent comparator groups.
Animal Data
Developmental toxicity was not observed in rats at intravenous doses of up to 1000 mg/kg/day or mice at subcutaneous doses of up to 2000 mg/kg/day given during the period of organogenesis (gestation days 6-17 in rats and 6-15 in mice). No treatment-related malformations or reductions in fetal viability were observed. Mean plasma exposure (AUC) at these doses was approximately 1.4 times (rats) and 2 times (mice) the daily mean plasma exposure in cUTI patients that received 2 grams of cefiderocol infused intravenously every 8 hours.
In a pre- and postnatal development study, cefiderocol was administered intravenously at doses up to 1000 mg/kg/day to rats from day 6 of pregnancy until weaning. No adverse effects on parturition, maternal function, or pre- and postnatal development and viability of the pups were observed.
In pregnant rats, cefiderocol-derived radioactivity was shown to cross the placenta, but the amount detected in fetuses was a small percentage (<0.5%) of the dose.
8.2 Lactation
Risk Summary
It is not known whether cefiderocol is excreted into human milk; however, cefiderocol-derived radioactivity was detected in the milk of lactating rats that received the drug intravenously. When a drug is present in animal milk, it is likely that the drug will be present in human milk. No information is available on the effects of FETROJA on the breastfed infant or on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for FETROJA and any potential adverse effects on the breastfed child from FETROJA or from the underlying maternal condition.
8.4 Pediatric Use
Safety and efficacy of FETROJA in pediatric patients younger than 18 years of age have not been established.
8.5 Geriatric Use
Of the 300 subjects treated with FETROJA in the cUTI trial, 158 (52.7%) were 65 years of age and older, and 67 (22.3%) were 75 years of age and older. No overall differences in safety or efficacy were observed between these subjects and younger subjects.
FETROJA is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function. No dosage adjustment is required based on age. Dosage adjustment for elderly patients should be based on renal function [see Dosage and Administration (2.2), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
8.6 Renal Impairment
Patients with CLcr 60 to 89 mL/min
No dosage adjustment of FETROJA is recommended in patients with CLcr 60 to 89 mL/min.
Patients with CLcr Less Than 60 mL/min
Dose adjustment is required in patients with CLcr 15 to 59 mL/min, and in patients with end-stage renal disease or who are receiving hemodialysis (HD). In patients requiring HD, complete HD at the latest possible time before the start of cefiderocol dosing [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)]. Monitor renal function regularly and adjust the dosage of FETROJA accordingly as renal function may change during the course of therapy.
Patients with CLcr 120 mL/min or greater
CLcr 120 mL/min or greater may be seen in seriously ill patients, who are receiving intravenous fluid resuscitation. Dosage adjustment of FETROJA is required in patients with CLcr 120 mL/min or greater [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)]. Monitor renal function regularly and adjust the dosage of FETROJA accordingly as renal function may change during the course of therapy.
8.7 Hepatic Impairment
The effects of hepatic impairment on the pharmacokinetics of cefiderocol have not been evaluated. Hepatic impairment is not expected to alter the elimination of cefiderocol as hepatic metabolism/excretion represents a minor pathway of elimination for cefiderocol. Dosage adjustments are not necessary in patients with impaired hepatic function.
-
10 OVERDOSAGE
There is no information on clinical signs and symptoms associated with an overdose of FETROJA. Patients who receive doses greater than the recommended dose regimen and have unexpected adverse reactions possibly associated with FETROJA should be carefully observed and given supportive treatment, and discontinuation or interruption of treatment should be considered.
Approximately 60% of cefiderocol is removed by a 3- to 4-hour hemodialysis session [see Clinical Pharmacology (12.3)].
-
11 DESCRIPTION
FETROJA is a cephalosporin antibacterial drug product consisting of cefiderocol sulfate tosylate for intravenous infusion. Cefiderocol functions as a siderophore [see Microbiology (12.4)].
The chemical name of cefiderocol sulfate tosylate is Tris[(6R,7R)-7-[(2Z)-2-(2-amino-1,3-thiazol-4-yl)-2-{[(2-carboxypropan-2-yl)oxy]imino}acetamido]-3-({1-[2-(2-chloro-3,4-dihydroxybenzamido)ethyl]pyrrolidin-1-ium-1-yl}methyl)-8-oxo-5-thia-1-azabicyclo[4.2.0]oct-2-ene-2-carboxylate] tetrakis(4-methylbenzenesulfonate) monosulfate hydrate, and the molecular weight is 3043.50 (anhydrous). The molecular formula is 3C30H34ClN7O10S2∙4C7H8O3S∙H2SO4∙xH2O.
Figure 1 Chemical Structure of Cefiderocol Sulfate Tosylate 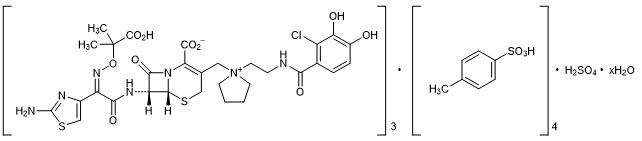
FETROJA for injection is a white to off-white, sterile, lyophilized powder formulated with 1 gram of cefiderocol (equivalent to 1.6 grams of cefiderocol sulfate tosylate), sucrose (900 mg), sodium chloride (216 mg), and sodium hydroxide to adjust pH. The sodium content is approximately 176 mg/vial. The pH of the reconstituted solution of 1 gram cefiderocol (1 vial) dissolved in 10 mL water is 5.2 to 5.8.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
The percent time of dosing interval that unbound plasma concentrations of cefiderocol exceed the minimum inhibitory concentration (MIC) against the infecting organism best correlates with antibacterial activity in neutropenic murine thigh and lung infection models with Enterobacteriaceae, P. aeruginosa, A. baumannii, and S. maltophilia. Compared to a 1-hour infusion, a 3-hour infusion increased the percent time of dosing interval that unbound plasma concentrations of cefiderocol exceed the MIC. The in vivo animal pneumonia studies showed that the antibacterial activity of cefiderocol was greater at the human equivalent dosing regimen of 3-hour infusion compared to that of 1-hour infusion.
12.3 Pharmacokinetics
In cUTI patients with CLcr 60 mL/min or greater, the mean cefiderocol Cmax was 138 mg/L and AUC was 394.7 mg∙hr/L (as 1184 mg∙hr/L of daily AUC) after multiple (every 8 hours) FETROJA 2-gram doses infused over 1 hour (1/3 of the recommended infusion duration).
In healthy volunteers, the mean cefiderocol Cmax and AUC was 89.7 mg/L and 386 mg∙hr/L, respectively, after a single FETROJA 2-gram dose was infused over 3 hours. Cefiderocol Cmax and AUC increased proportionally with dose.
Distribution
The geometric mean (±SD) cefiderocol volume of distribution was 18.0 (±3.36) L. Plasma protein binding, primarily to albumin, of cefiderocol is 40% to 60%.
Elimination
Cefiderocol terminal elimination half-life is 2 to 3 hours. The geometric mean (±SD) cefiderocol clearance is estimated to be 5.18 (±0.89) L/hr.
Specific Populations
No clinically significant differences in the pharmacokinetics of cefiderocol were observed based on age (18 to 93 years of age), sex, or race. The effect of hepatic impairment on the pharmacokinetics of cefiderocol was not evaluated.
Patients with Renal Impairment
Approximately 60% of cefiderocol was removed by a 3- to 4-hour hemodialysis session.
Cefiderocol AUC fold changes in subjects with renal impairment compared to subjects with CLcr 90 to 119 mL/min are summarized in Table 4.
Table 4 Effect of Renal Impairment on the AUC of Cefiderocol* CLcr (mL/min) Cefiderocol AUC
Geometric Mean Ratios (90% CI)†CI=confidence interval - * After a single FETROJA 1-gram dose (0.5 times the approved recommended dosage)
- † Compared to AUC in subjects with CLcr 90 to 119 mL/min (N=12)
60 to 89 (N=6) 1.37 (1.15, 1.62) 30 to 59 (N=7) 2.35 (2.00, 2.77) 15 to 29 (N=4) 3.21 (2.64, 3.91) <15 (N=6) 4.69 (3.95, 5.56) Patients with CLcr 120 mL/min or Greater
Increased cefiderocol clearance has been observed in patients with CLcr 120 mL/min or greater. A FETROJA 2-gram dose every 6 hours infused over 3 hours is predicted to provide cefiderocol exposures comparable to those in patients with CLcr 90 to 119 mL/min [see Dosage and Administration (2.2)].
Drug Interaction Studies
Clinical Studies
No clinically significant differences in the pharmacokinetics of furosemide (an organic anion transporter [OAT]1 and OAT3 substrate), metformin (an organic cation transporter [OCT]1, OCT2, and multi-drug and toxin extrusion [MATE]2-K substrate), and rosuvastatin (an organic anion transporting polypeptide [OATP]1B3 substrate) were observed when co-administered with cefiderocol.
12.4 Microbiology
Mechanism of Action
FETROJA is a cephalosporin antibacterial with activity against Gram-negative aerobic bacteria. Cefiderocol functions as a siderophore and binds to extracellular free ferric iron. In addition to passive diffusion via porin channels, cefiderocol is actively transported across the outer cell membrane of bacteria into the periplasmic space using a siderophore iron uptake mechanism. Cefiderocol exerts bactericidal action by inhibiting cell wall biosynthesis through binding to penicillin-binding proteins (PBPs).
Cefiderocol has no clinically relevant in vitro activity against most Gram-positive bacteria and anaerobic bacteria. Cefiderocol has shown in vitro activity against some isolates of S. maltophilia, and meropenem-resistant Enterobacteriaceae, P. aeruginosa, and A. baumannii. Cefiderocol is active against some P. aeruginosa and A. baumannii isolates resistant to meropenem, ciprofloxacin, and amikacin. Cefiderocol is active against some E. coli isolates containing mcr-1.
Cefiderocol demonstrated in vitro activity against certain Enterobacteriaceae genetically confirmed to contain the following: ESBLs (TEM, SHV, CTX-M, oxacillinase [OXA]), AmpC, AmpC-type ESBL (CMY), serine-carbapenemases (such as KPC, OXA-48), and metallo-carbapenemases (such as NDM and VIM). Cefiderocol demonstrated in vitro activity against certain P. aeruginosa genetically confirmed to contain VIM, GES, AmpC and certain A. baumannii containing OXA-23, OXA-24/40, OXA-51, OXA-58. Cefiderocol has demonstrated in vitro activity against some K. pneumoniae isolates with OmpK35/36 porin deletion and some isolates of P. aeruginosa with OprD porin deletion.
Resistance
Cross-resistance with other classes of antibacterial drugs has not been identified; therefore, isolates resistant to other antibacterial drugs may be susceptible to cefiderocol.
Cefiderocol does not cause induction of AmpC beta-lactamase in P. aeruginosa and E. cloacae. The frequency of resistance development in Gram-negative bacteria including carbapenemase producers exposed to cefiderocol at 10× minimum inhibitory concentration (MIC) ranged from 10-6 to 10-8.
In vitro, MIC increases that may result in resistance to cefiderocol in Gram-negative bacteria have been associated with the presence of beta-lactamases including AmpC beta-lactamase overproduction, modifications of penicillin binding proteins, and mutations of transcriptional regulators that impact siderophore or efflux pump expression.
In vitro, the addition of the beta-lactamase inhibitors (such as avibactam, clavulanic acid, and dipicolinic acid) results in the lowering of MICs of some isolates with relatively high MICs (range 2 to 256) to cefiderocol.
Interaction with Other Antimicrobials
In vitro studies showed no antagonism between cefiderocol and amikacin, ceftazidime/avibactam, ceftolozane/tazobactam, ciprofloxacin, clindamycin, colistin, daptomycin, linezolid, meropenem, metronidazole, tigecycline, or vancomycin against strains of Enterobacteriaceae, P. aeruginosa, and A. baumannii.
Activity against Bacteria in Animal Infection Models
In a neutropenic murine thigh infection model using a humanized dose (2 grams every 8 hours), cefiderocol demonstrated 1log10 reduction in bacterial burden against most Enterobacteriaceae A. baumannii, and P. aeruginosa including some carbapenemase-producing isolates with MICs of ≤ 4 mcg/mL.
In an immunocompetent rat pneumonia model, reduction in bacterial counts in the lungs of animals infected with K. pneumoniae with MICs ≤ 8 mcg/mL and P. aeruginosa with MICs ≤ 1 mcg/mL was observed using humanized cefiderocol dose.
In an immunocompetent murine urinary tract infection model, cefiderocol reduced bacterial counts in the kidneys of mice infected with Enterobacteriaceae, and P. aeruginosa isolates with MICs ≤ 1 mcg/mL. In an immunocompromised murine systemic infection model, cefiderocol increased survival in mice infected with E. cloacae, S. maltophilia, and Burkholderia cepacia isolates with MICs ≤ 0.5 mcg/mL compared to untreated mice. In an immunocompetent murine systemic infection model, cefiderocol increased survival in mice infected with S. marcescens and P. aeruginosa isolates with MICs ≤ 1 mcg/mL compared to untreated mice. The clinical significance of the above findings is not known.
Antimicrobial Activity
FETROJA has been shown to be active against the following bacteria, both in vitro and in clinical infections [see Indications and Usage (1.1)]:
Gram-negative
Escherichia coli
Enterobacter cloacae complex
Klebsiella pneumoniae
Proteus mirabilis
Pseudomonas aeruginosaCefiderocol demonstrated in vitro activity against the following bacteria, but the clinical significance is unknown. At least 90% of the following bacteria exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for cefiderocol. However, the efficacy of cefiderocol in treating clinical infections due to these bacteria has not been established in adequate and well-controlled clinical trials.
Gram-negative
Acinetobacter baumannii
Citrobacter freundii complex
Citrobacter koseri
Klebsiella aerogenes
Klebsiella oxytoca
Morganella morganii
Proteus vulgaris
Providencia rettgeri
Serratia marcescens
Stenotrophomonas maltophilia -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenesis
Cefiderocol was negative for genotoxicity in a reverse mutation test with S. typhimurium and E. coli and did not induce mutations in V79 Chinese hamster lung cells. Cefiderocol was positive in a chromosomal aberration test in cultured TK6 human lymphoblasts and increased mutation frequency in L5178Y mouse lymphoma cells. Cefiderocol was negative in an in vivo rat micronucleus test and a rat comet assay at the highest doses of 2000 and 1500 mg/kg/day, respectively.
Impairment of Fertility
Cefiderocol did not affect fertility in adult male or female rats when administered intravenously at doses up to 1000 mg/kg/day. The AUC at this dose is approximately 1.4 times the mean daily cefiderocol exposure in cUTI patients who received the maximum recommended clinical dose of 2 grams every 8 hours.
-
14 CLINICAL STUDIES
14.1 Complicated Urinary Tract Infections, Including Pyelonephritis
A total of 448 adults hospitalized with cUTI (including pyelonephritis) were randomized in a 2:1 ratio and received study medications in a multinational, double-blind trial (Trial 1) (NCT02321800) comparing FETROJA 2 grams intravenously (IV) every 8 hours (infused over 1 hour) to imipenem/cilastatin 1gram/1 gram IV every 8 hours (infused over 1 hour) for 7 to 14 days. No switch from IV to oral antibacterial therapy was permitted.
Efficacy was assessed as a composite of microbiological eradication and clinical cure in the microbiological intent-to-treat (Micro-ITT) population, which included all patients who received at least a single-dose of study medication and had at least one baseline Gram-negative uropathogen. Other efficacy endpoints included the microbiological eradication rate and the clinical response rate at the Test of Cure (TOC) visit in the Micro-ITT population.
The Micro-ITT population consisted of 371 patients of whom 25% had cUTI with pyelonephritis, 48% had cUTI without pyelonephritis, and 27% had acute uncomplicated pyelonephritis. Complicating conditions included obstructive uropathy, catheterization, and renal stones. The median age was 66 years, with 24% of patients over the age of 75 years, and 55% of the population was female. The median duration of therapy in both treatment groups was 9 days (range: 1-14 days). Of the 371 patients, 32% had CLcr >50-80 mL/min, 17% had CLcr 30-50 mL/min, and 3% had CLcr < 30 mL/min at baseline. Concomitant Gram-negative bacteremia was identified in 7% of patients. In the Micro-ITT population, the most common baseline pathogens were E. coli and K. pneumoniae.
Table 5 provides the results of a composite of microbiological eradication (all Gram-negative uropathogens found at baseline at ≥ 105 CFU/mL reduced to < 104 CFU/mL) and clinical response (resolution or improvement of cUTI symptoms and no new symptoms assessed by the investigator) at the TOC visit 7 +/- 2 days after the last dose of study drug. The response rates for the composite endpoint of microbiological eradication and clinical response at the TOC visit were higher in the FETROJA arm compared with imipenem/cilastatin as shown in Table 5. Clinical response rates at the TOC visit were similar between FETROJA and imipenem/cilastatin. Most patients with microbiological failure at the TOC visit in either treatment arm did not require further antibacterial drug treatment. Subgroup analyses examining composite outcomes by baseline pathogen are shown in Table 6 and demonstrated responses consistent with the overall population. Subgroup analyses examining outcomes by age, gender, and/or outcomes in patients with renal impairment, concomitant bacteremia, complicated UTI with or without pyelonephritis, or acute uncomplicated pyelonephritis demonstrated responses were consistent with the overall population.
Table 5 Composite, Microbiological, and Clinical Response Rates at the TOC Visit – Micro ITT Population Study Endpoint FETROJA
n/N (%)Imipenem/Cilastatin
n/N (%)Treatment Difference (95% CI)* CI = confidence interval; Micro-ITT = microbiological intent-to-treat; TOC = Test of Cure - * The treatment difference and 95% CI were based on the Cochran-Mantel-Haenszel method.
Composite response at TOC 183/252 (72.6%) 65/119 (54.6%) 18.6 (8.2, 28.9) Microbiologic response TOC 184/252 (73.0%) 67/119 (56.3%) 17.3 (6.9, 27.6) Clinical response TOC 226/252 (89.7%) 104/119 (87.4%) 2.4 (-4.7, 9.4) Table 6 Composite Endpoint of Microbiological Eradication and Clinical Response at the TOC Visits in the Micro-ITT by Baseline Pathogen* Subgroups Baseline Pathogen Subgroup FETROJA
n/N (%)Imipenem/Cilastatin
n/N (%)- * Patients may have been infected with more than one pathogen in the baseline urine culture.
Escherichia coli 113/152 (74.3) 45/79 (57.0) Klebsiella pneumoniae 36/48 (75.0) 12/25 (48.0) Proteus mirabilis 13/17 (76.5) 0/2 (0.0) Pseudomonas aeruginosa 8/18 (44.4) 3/5 (60.0) Enterobacter cloacae complex 8/13 (61.5) 3/3 (100.0) In the FETROJA treatment group, 61 (24.2%) bacterial isolates were ESBL producers compared with 32 (26.9%) in the imipenem/cilastatin group. The composite response rate of patients with these ESBL isolates at the TOC visit was consistent with the overall results.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
FETROJA 1 gram (cefiderocol) for injection is supplied as a white to off-white sterile lyophilized powder for reconstitution in single-dose, clear glass vials (NDC: 59630-266-01) sealed with a rubber stopper (not made with natural rubber latex) and an aluminum seal with flip-off cap. Each vial is supplied in cartons containing 10 single-dose vials.
NDC: 59630-266-10 FETROJA (cefiderocol) 1 gram/vial, 10 vials/carton 16.2 Storage and Handling
FETROJA vials should be stored refrigerated at 2°C to 8°C (36°F to 46°F). Protect from light. Store in the carton until time of use. Reconstituted and diluted solutions of FETROJA can be stored at room temperature [see Dosage and Administration (2.5)].
-
17 PATIENT COUNSELING INFORMATION
Serious Allergic Reactions
Advise patients and their families that allergic reactions, including serious allergic reactions, could occur with FETROJA and that serious reactions require immediate treatment. Ask patients about any previous hypersensitivity reactions to FETROJA, other beta-lactams (including cephalosporins), or other allergens [see Warnings and Precautions (5.2)].
Potentially Serious Diarrhea
Advise patients and their families that diarrhea is a common problem caused by antibacterial drugs, including FETROJA. Sometimes, frequent watery or bloody diarrhea may occur and may be a sign of a more serious intestinal infection. If severe watery or bloody diarrhea develops, tell patient to contact his or her healthcare provider [see Warnings and Precautions (5.3)].
Seizures
Counsel patients on the implication of cephalosporins in triggering seizures, particularly in patients with renal impairment when the dosage was not reduced and in patients with a history of epilepsy [see Warnings and Precautions (5.4)].
Antibacterial Resistance
Patients should be counseled that antibacterial drugs including FETROJA should only be used to treat bacterial infections. They do not treat viral infections (e.g., influenza, common cold). When FETROJA is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by FETROJA or other antibacterial drugs in the future [see Warnings and Precautions (5.5)].
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 1 gram Vial Carton
Rx ONLY
NDC: 59630-266-101 gram
Fetroja®
(cefiderocol) for injection
1 gram per vialFor Intravenous Infusion.
Must be reconstituted then diluted.
Contains 10 single-dose vials.SHIONOGI INC.

-
INGREDIENTS AND APPEARANCE
FETROJA
cefiderocol sulfate tosylate injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 59630-266 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Cefiderocol sulfate tosylate (UNII: TTP8LBP45D) (Cefiderocol - UNII:SZ34OMG6E8) Cefiderocol 1 g in 10 mL Inactive Ingredients Ingredient Name Strength Sucrose (UNII: C151H8M554) 900 mg in 10 mL Sodium chloride (UNII: 451W47IQ8X) 216 mg in 10 mL Sodium hydroxide (UNII: 55X04QC32I) Nitrogen (UNII: N762921K75) Product Characteristics Color WHITE (white to off-white) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 59630-266-10 10 in 1 CARTON 01/31/2020 1 NDC: 59630-266-01 10 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA209445 01/31/2020 Labeler - Shionogi Inc. (098241610)
Trademark Results [Fetroja]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 FETROJA 86890071 5288628 Live/Registered |
Shionogi & Co., Ltd. 2016-01-28 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.