CLINDAMYCIN AND BENZOYL PEROXIDE gel
clindamycin and benzoyl peroxide by
Drug Labeling and Warnings
clindamycin and benzoyl peroxide by is a Prescription medication manufactured, distributed, or labeled by Glenmark Pharmaceuticals Inc., USA, Glenmark Pharmaceuticals Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Clindamycin and Benzoyl Peroxide Gel, 1%/5% contains clindamycin phosphate, (7(S)-chloro-7-deoxylincomycin-2-phosphate). Clindamycin phosphate is a water soluble ester of the semi-synthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent antibiotic lincomycin.
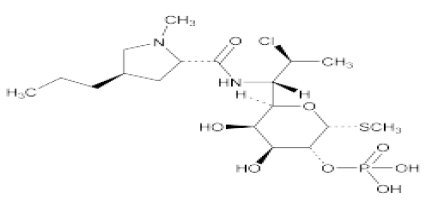
Chemically, clindamycin phosphate is (C18H34ClN2O8PS). The structural formula for clindamycin is represented below:
Clindamycin phosphate has a molecular weight of 504.96 and its chemical name is Methyl 7-chloro-6,7,8-trideoxy-6-(1-methyl-trans-4-propyl-L-2-pyrrolidinecarboxamido) -1-thio-L-threo-α-D- galacto-octopyranoside 2-(dihydrogen phosphate).
Clindamycin and Benzoyl Peroxide Gel, 1%/5% also contains benzoyl peroxide, for topical use.
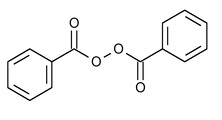
Chemically, benzoyl peroxide is (C14H10O4). It has the following structural formula:
Benzoyl peroxide has a molecular weight of 242.23.
Each gram of Clindamycin and Benzoyl Peroxide Gel, 1%/5% contains, as dispensed, 10 mg (1%) clindamycin as phosphate and 50 mg (5%) benzoyl peroxide in a base of carbomer homopolymer type C, docusate sodium, edetate disodium, sodium hydroxide, and purified water.
-
CLINICAL PHARMACOLOGY
An in vitro percutaneous penetration study comparing Clindamycin and Benzoyl Peroxide Gel and topical 1% clindamycin gel alone, demonstrated there was no statistical difference in penetration between the two drugs. Mean systemic bioavailability of topical clindamycin in Clindamycin and Benzoyl Peroxide Gel is suggested to be less than 1%.
Benzoyl peroxide has been shown to be absorbed by the skin where it is converted to benzoic acid. Less than 2% of the dose enters systemic circulation as benzoic acid. It is suggested that the lipophilic nature of benzoyl peroxide acts to concentrate the compound into the lipid-rich sebaceous follicle.
Pharmacokinetics:
The pharmacokinetics (plasma and urine) of clindamycin from Clindamycin and Benzoyl Peroxide Gel was studied in male and female patients (n=13) with acne vulgaris. Clindamycin and Benzoyl Peroxide Gel (~2g) was applied topically to the face and back twice daily for four and a half (4.5) days. Quantifiable (>LOQ=1 ng/mL) clindamycin plasma concentrations were obtained in six of thirteen subjects (46.2%) on Day 1 and twelve of thirteen subjects (92.3%) on Day 5. Peak plasma concentrations (Cmax) of clindamycin ranged from 1.47 ng/mL to 2.77 ng/mL on Day 1 and 1.43 ng/mL to 7.18 ng/mL on Day 5. The AUC (0 to 12h) ranged from 2.74 ng.h/mL to 12.86 ng.h/mL on Day 1 and 11.4 ng.h/mL to 69.7 ng.h/mL on Day 5.
The amount of clindamycin excreted in the urine during the 12 hour dosing interval increased from a mean (SD) of 5745 (3130) ng on Day 1 to 12069 (7660) ng on Day 5. The mean % (SD) of the administered dose that was excreted in the urine ranged from 0.03% (0.02) to 0.08% (0.04).
A comparison of the single (Day 1) and multiple (Day 5) dose plasma and urinary concentrations of clindamycin indicates that there is accumulation of clindamycin following multiple dosing of Clindamycin and Benzoyl Peroxide Gel. The degree of accumulation calculated from the plasma and urinary excretion data was ~2-fold.
Microbiology:
The clindamycin and benzoyl peroxide components individually have been shown to have in vitro activity against Propionibacterium acnes an organism which has been associated with acne vulgaris; however, the clinical significance of this activity against P. acnes was not examined in clinical trials with this product.
-
CLINICAL STUDIES
In two adequate and well controlled clinical studies of 758 patients, 214 used clindamycin and benzoyl peroxide gel, 210 used benzoyl peroxide, 168 used clindamycin, and 166 used vehicle. Clindamycin and benzoyl peroxide gel applied twice daily for 10 weeks was significantly more effective than vehicle in the treatment of moderate to moderately severe facial acne vulgaris. Patients were evaluated and acne lesions counted at each clinical visit; weeks 2, 4, 6, 8 and 10. The primary efficacy measures were the lesion counts and the investigator’s global assessment evaluated at week 10. Patients were instructed to wash the face with a mild soap, using only the hands. Fifteen minutes after the face was thoroughly dry, application was made to the entire face. Non-medicated make-up could be applied at one hour after the clindamycin and benzoyl peroxide gel application. If a moisturizer was required, the patients were provided a moisturizer to be used as needed. Patients were instructed to avoid sun exposure. Percent reductions in lesion counts after treatment for 10 weeks in these two studies are shown below:
Study 1 Clindamycin and Benzoyl Peroxide
n = 120Benzoyl Peroxide
n = 120Clindamycin
n = 120Vehicle
n = 120Mean percent reduction in inflammatory lesion counts
46%
32%
16%
+3%
Mean percent reduction in non-inflammatory lesion counts
22%
22%
9%
+1%
Mean percent reduction in total lesion counts
36%
28%
15%
0.2%
Study 2 Clindamycin and Benzoyl Peroxide
n = 95Benzoyl Peroxide
n = 95Clindamycin
n = 49Vehicle
n = 48Mean percent reduction in inflammatory lesion counts
63%
53%
45%
42%
Mean percent reduction in non-inflammatory lesion counts
54%
50%
39%
36%
Mean percent reduction in total lesion counts
58%
52%
42%
39%
The clindamycin and benzoyl peroxide gel group showed greater overall improvement than the benzoyl peroxide, clindamycin and vehicle groups as rated by the investigator.
- INDICATIONS AND USAGE
- CONTRAINDICATIONS
-
WARNINGS
ORALLY AND PARENTERALLY ADMINISTERED CLINDAMYCIN HAS BEEN ASSOCIATED WITH SEVERE COLITIS WHICH MAY RESULT IN PATIENT DEATH. USE OF THE TOPICAL FORMULATION OF CLINDAMYCIN RESULTS IN ABSORPTION OF THE ANTIBIOTIC FROM THE SKIN SURFACE. DIARRHEA, BLOODY DIARRHEA, AND COLITIS (INCLUDING PSEUDOMEMBRANOUS COLITIS) HAVE BEEN REPORTED WITH THE USE OF TOPICAL AND SYSTEMIC CLINDAMYCIN. STUDIES INDICATE A TOXIN(S) PRODUCED BY CLOSTRIDIA IS ONE PRIMARY CAUSE OF ANTIBIOTIC-ASSOCIATED COLITIS. THE COLITIS IS USUALLY CHARACTERIZED BY SEVERE PERSISTENT DIARRHEA AND SEVERE ABDOMINAL CRAMPS AND MAY BE ASSOCIATED WITH THE PASSAGE OF BLOOD AND MUCUS. ENDOSCOPIC EXAMINATION MAY REVEAL PSEUDOMEMBRANOUS COLITIS. STOOL CULTURE FOR Clostridium Difficile AND STOOL ASSAY FOR C. difficile TOXIN MAY BE HELPFUL DIAGNOSTICALLY. WHEN SIGNIFICANT DIARRHEA OCCURS, THE DRUG SHOULD BE DISCONTINUED. LARGE BOWEL ENDOSCOPY SHOULD BE CONSIDERED TO ESTABLISH A DEFINITIVE DIAGNOSIS IN CASES OF SEVERE DIARRHEA. ANTIPERISTALTIC AGENTS SUCH AS OPIATES AND DIPHENOXYLATE WITH ATROPINE MAY PROLONG AND/OR WORSEN THE CONDITION. DIARRHEA, COLITIS, AND PSEUDOMEMBRANOUS COLITIS HAVE BEEN OBSERVED TO BEGIN UP TO SEVERAL WEEKS FOLLOWING CESSATION OF ORAL AND PARENTERAL THERAPY WITH CLINDAMYCIN.
Mild cases of pseudomembranous colitis usually respond to drug discontinuation alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation and treatment with an antibacterial drug clinically effective against C. difficile colitis.
-
PRECAUTIONS
General:
For dermatological use only; not for ophthalmic use. Concomitant topical acne therapy should be used with caution because a possible cumulative irritancy effect may occur, especially with the use of peeling, desquamating, or abrasive agents.
The use of antibiotic agents may be associated with the overgrowth of non-susceptible organisms including fungi. If this occurs, discontinue use of this medication and take appropriate measures.
Avoid contact with eyes and mucous membranes.
Clindamycin and erythromycin containing products should not be used in combination. In vitro studies have shown antagonism between these two antimicrobials. The clinical significance of this in vitro antagonism is not known.
Information for Patients:
Patients using Clindamycin and Benzoyl Peroxide Gel should receive the following information and instructions:
1. Clindamycin and Benzoyl Peroxide Gel is to be used as directed by the physician. It is for external use only. Avoid contact with eyes, and inside the nose, mouth, and all mucous membranes, as this product may be irritating.
2. This medication should not be used for any disorder other than that for which it was prescribed.
3. Patients should not use any other topical acne preparation unless otherwise directed by physician.
4. Patients should minimize or avoid exposure to natural or artificial sunlight (tanning beds or UVA/B treatment) while using clindamycin and benzoyl peroxide gel. To minimize exposure to sunlight, a wide-brimmed hat or other protective clothing should be worn, and a sunscreen with SPF 15 rating or higher should be used.
5. Patients who develop allergic symptoms such as severe swelling or shortness of breath should discontinue Clindamycin and Benzoyl Peroxide Gel and contact their physician immediately. In addition, patients should report any signs of local adverse reactions to their physician.
6. Clindamycin and Benzoyl Peroxide Gel may bleach hair or colored fabric.
7. Clindamycin and Benzoyl Peroxide Gel can be stored at room temperature up to 25°C (77°F) for 3 months. Do not freeze. Discard any unused product after 3 months.
8. Before applying Clindamycin and Benzoyl Peroxide Gel to affected areas wash the skin gently, then rinse with warm water and pat dry.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Benzoyl peroxide has been shown to be a tumor promoter and progression agent in a number of animal studies. The clinical significance of this is unknown.
Benzoyl peroxide in acetone at doses of 5 and 10 mg administered twice per week induced skin tumors in transgenic Tg.AC mice in a study using 20 weeks of topical treatment.
In a 52 week dermal photocarcinogenicity study in hairless mice, the median time to onset of skin tumor formation was decreased and the number of tumors per mouse increased following chronic concurrent topical administration of clindamycin and benzoyl peroxide gel with exposure to ultraviolet radiation (40 weeks of treatment followed by 12 weeks of observation).
In a 2-year dermal carcinogenicity study in rats, treatment with clindamycin and benzoyl peroxide gel at doses of 100, 500 and 2000 mg/kg/day caused a dose-dependent increase in the incidence of keratoacanthoma at the treated skin site of male rats. The incidence of keratoacanthoma at the treated site of males treated with 2000 mg/kg/day (8 times the highest recommended adult human dose of 2.5 g clindamycin and benzoyl peroxide gel based on mg/m2) was statistically significantly higher than that in the sham- and vehicle-controls.
Genotoxicity studies were not conducted with clindamycin and benzoyl peroxide gel. Clindamycin phosphate was not genotoxic in Salmonella typhimurium or in a rat micronucleus test. Clindamycin phosphate sulfoxide, an oxidative degradation product of clindamycin phosphate and benzoyl peroxide, was not clastogenic in a mouse micronucleus test. Benzoyl peroxide has been found to cause DNA strand breaks in a variety of mammalian cell types, to be mutagenic in S. typhimurium tests by some but not all investigators, and to cause sister chromatid exchanges in Chinese hamster ovary cells. Studies have not been performed with Clindamycin and Benzoyl Peroxide Gel or benzoyl peroxide to evaluate the effect on fertility. Fertility studies in rats treated orally with up to 300 mg/kg/day of clindamycin (approximately 120 times the amount of clindamycin in the highest recommended adult human dose of 2.5 g clindamycin and benzoyl peroxide gel, based on mg/m2) revealed no effects on fertility or mating ability.
Pregnancy:
Teratogenic Effects: Pregnancy Category C:
Animal reproductive/developmental toxicity studies have not been conducted with clindamycin and benzoyl peroxide gel or benzoyl peroxide. Developmental toxicity studies performed in rats and mice using oral doses of clindamycin up to 600 mg/kg/day (240 and 120 times amount of clindamycin in the highest recommended adult human dose based on mg/m2, respectively) or subcutaneous doses of clindamycin up to 250 mg/kg/day (100 and 50 times the amount of clindamycin in the highest recommended adult human dose based on mg/m2, respectively) revealed no evidence of teratogenicity.
There are no well-controlled trials in pregnant women treated with Clindamycin and Benzoyl Peroxide Gel. It also is not known whether Clindamycin and Benzoyl Peroxide Gel can cause fetal harm when administered to a pregnant woman.
Nursing Women:
It is not known whether Clindamycin and Benzoyl Peroxide Gel is excreted in human milk after topical application. However, orally and parenterally administered clindamycin has been reported to appear in breast milk. Because of the potential for serious adverse reactions in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
-
ADVERSE REACTIONS
During clinical trials, the most frequently reported adverse event in the clindamycin and benzoyl peroxide gel treatment group was dry skin (12%). The Table below lists local adverse events reported by at least 1% of patients in the clindamycin and benzoyl peroxide gel and vehicle groups.
Local Adverse Events – all causalities in >/= 1% of patients
Clindamycin and Benzoyl Peroxide
n=420
Vehicle
n=168
Application site reaction
13 (3%)
1 (<1%)
Dry skin
50 (12%)
10 (6%)
Pruritus
8 (2%)
1 (<1%)
Peeling
9 (2%)
-
Erythema
6 (1%)
1 (<1%)
Sunburn
5 (1%)
-
The actual incidence of dry skin might have been greater were it not for the use of a moisturizer in these studies.Anaphylaxis, as well as allergic reactions leading to hospitalization, have been reported during post-marketing use of clindamycin/benzoyl peroxide products. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- DOSAGE AND ADMINISTRATION
-
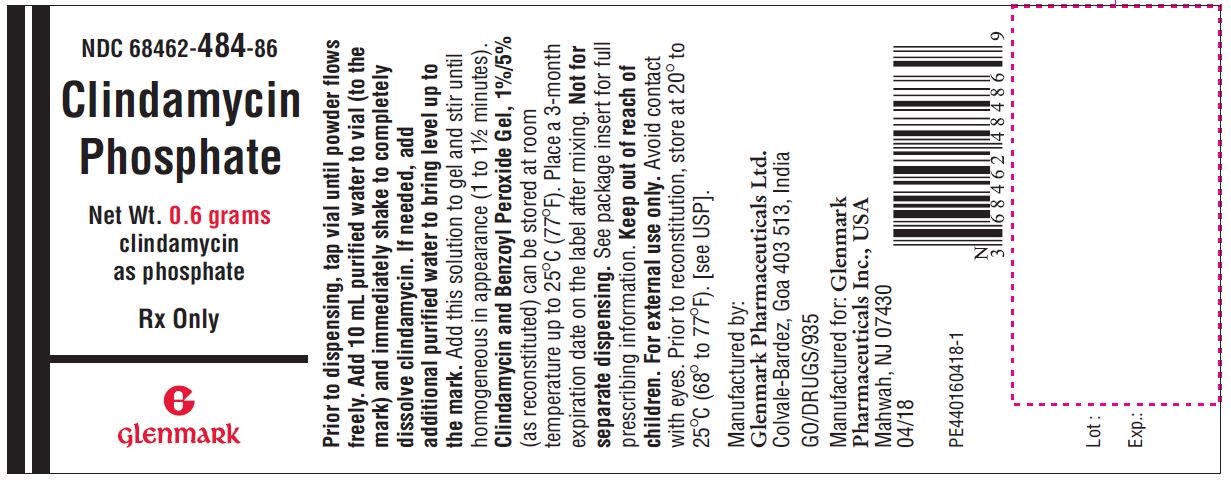
HOW SUPPLIED AND COMPOUNDING INSTRUCTIONS
Size
(Net Weight)NDC #
Benzoyl Peroxide Gel
Active Clindamycin powder (In plastic vial)
Purified Water To Be Added to each vial
25 grams
68462-486-19
19.7g
0.3g
5 mL
35 grams
68462-486-24
27.6g
0.4g
7 mL
50 grams
68462-486-27
39.4g
0.6g
10 mL
Prior to dispensing, tap the vial until powder flows freely. Add indicated amount of purified water to the vial (to the mark) and immediately shake to completely dissolve clindamycin. If needed, add additional purified water to bring level up to the mark. Add the solution in the vial to the gel and stir until homogenous in appearance (1 to 1½ minutes).
Clindamycin and Benzoyl Peroxide Gel (as reconstituted) can be stored at room temperature up to 25°C (77°F) for 3 months. Place a 3 month expiration date on the label immediately following mixing.
-
STORAGE AND HANDLING
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Do not freeze. Keep tightly closed. Keep out of the reach of children.
Rx Only
Manufactured by:
Glenmark Pharmaceuticals Ltd.
Colvale-Bardez, Goa 403513, IndiaManufactured for:
Glenmark Pharmaceuticals Inc., USA
Mahwah, NJ 07430Questions? 1(888) 721-7115
www.glenmarkpharma.com/usaMarch 2019
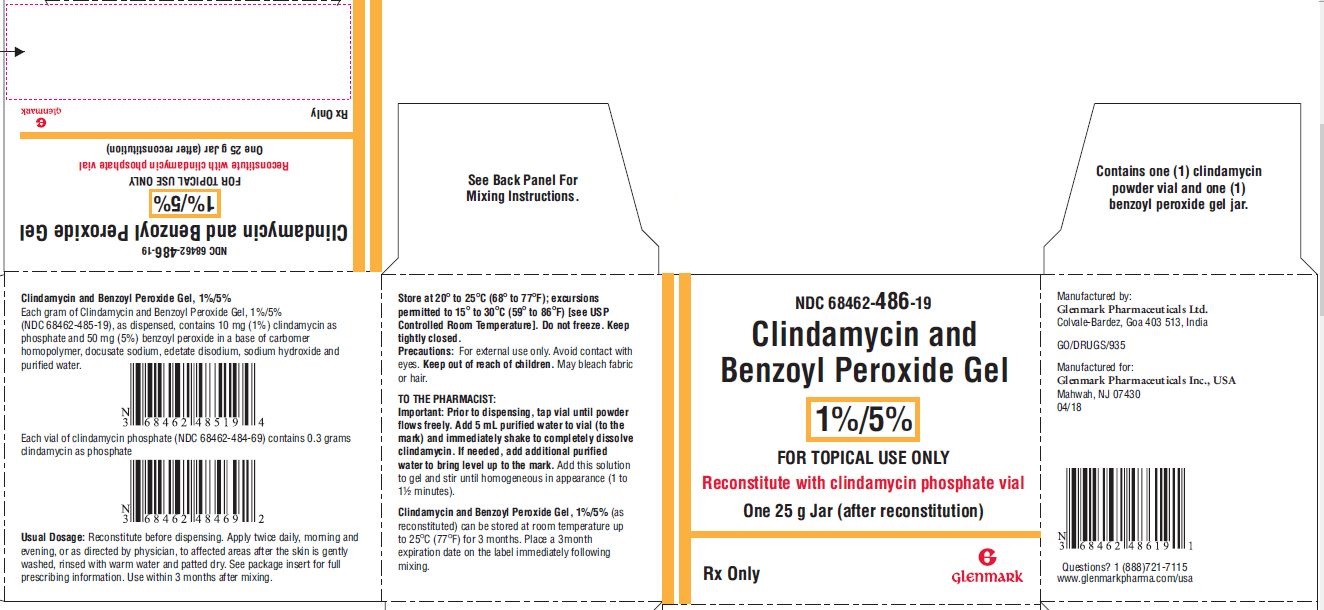
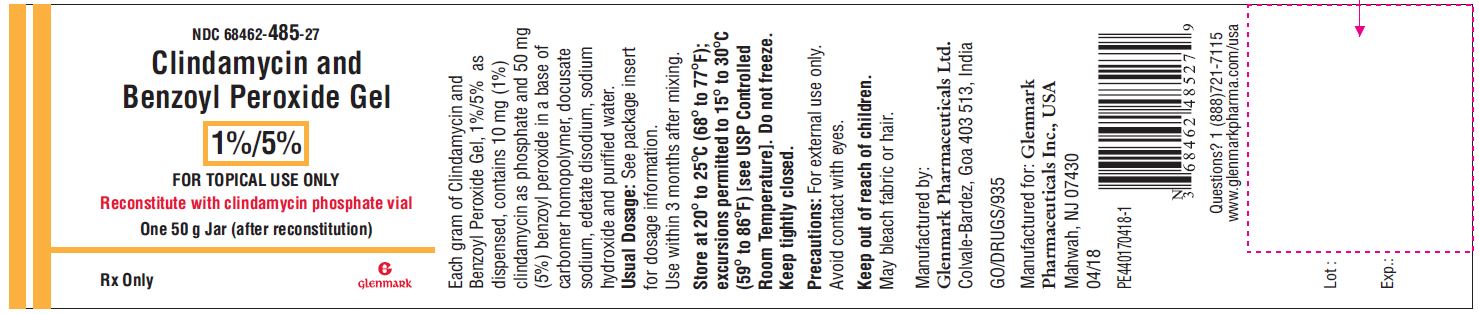
- Package/Label Display Panel – 25 gram Kit Carton
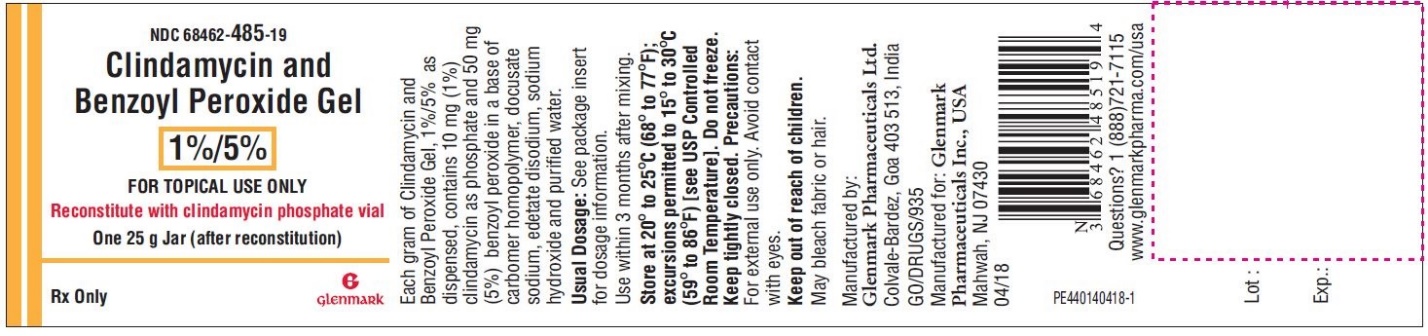
- Package/Label Display Panel – 25 gram Jar
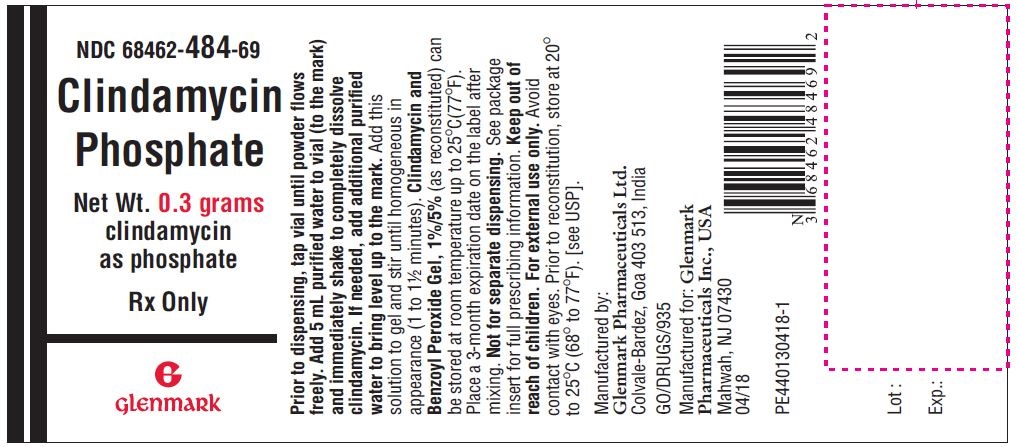
- Package/Label Display Panel – 25 gram Kit Vial
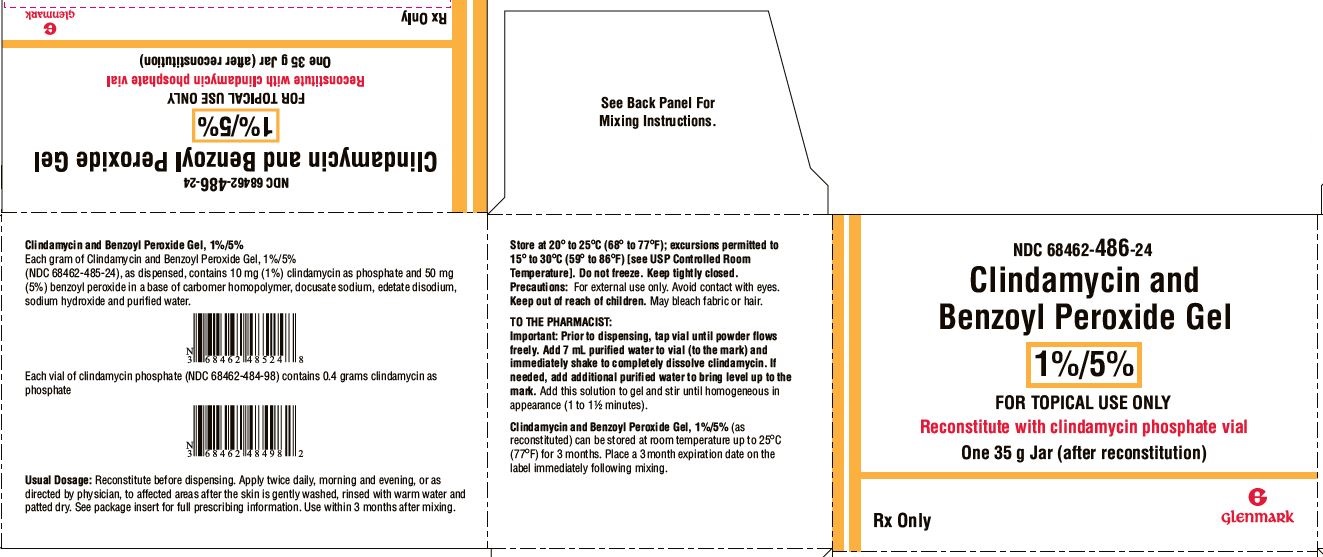
- Package/Label Display Panel - 35 gram Kit Carton
- Package/Label Display Panel-35 gram Jar
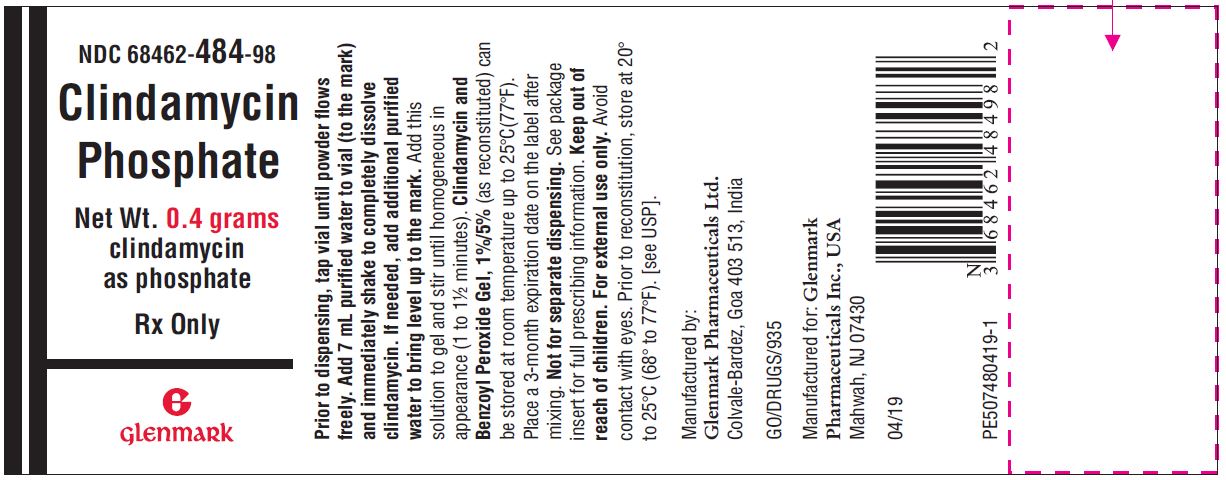
- Package/Label Display Panel-35 gram Kit Vial
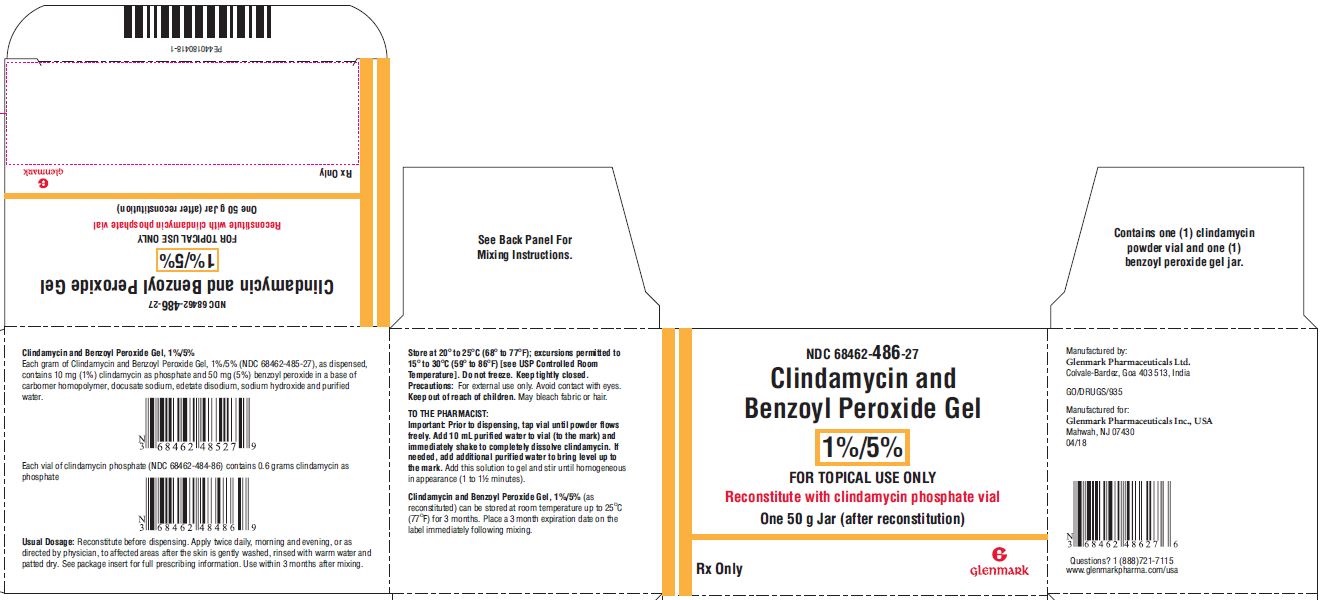
- Package/Label Display Panel – 50 gram Kit Carton
- Package/Label Display Panel-50 gram Jar
- Package/Label Display Panel – 50 gram Kit Vial
-
INGREDIENTS AND APPEARANCE
CLINDAMYCIN AND BENZOYL PEROXIDE
clindamycin and benzoyl peroxide gelProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68462-486 Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLINDAMYCIN PHOSPHATE (UNII: EH6D7113I8) (CLINDAMYCIN - UNII:3U02EL437C) CLINDAMYCIN PHOSPHATE 10 mg in 1 g BENZOYL PEROXIDE (UNII: W9WZN9A0GM) (BENZOYL PEROXIDE - UNII:W9WZN9A0GM) BENZOYL PEROXIDE 50 mg in 1 g Inactive Ingredients Ingredient Name Strength DOCUSATE SODIUM (UNII: F05Q2T2JA0) EDETATE DISODIUM (UNII: 7FLD91C86K) CARBOMER HOMOPOLYMER TYPE C (ALLYL PENTAERYTHRITOL CROSSLINKED) (UNII: 4Q93RCW27E) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68462-486-19 1 in 1 CARTON 03/14/2019 1 25 g in 1 JAR; Type 0: Not a Combination Product 2 NDC: 68462-486-24 1 in 1 CARTON 05/07/2019 2 35 g in 1 JAR; Type 0: Not a Combination Product 3 NDC: 68462-486-27 1 in 1 CARTON 03/14/2019 3 50 g in 1 JAR; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209252 03/14/2019 Labeler - Glenmark Pharmaceuticals Inc., USA (130597813) Establishment Name Address ID/FEI Business Operations Glenmark Pharmaceuticals Limited 677318665 MANUFACTURE(68462-486) , ANALYSIS(68462-486)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.