NEOSTIGMINE METHYLSULFATE injection
neostigmine methylsulfate by
Drug Labeling and Warnings
neostigmine methylsulfate by is a Prescription medication manufactured, distributed, or labeled by Civica Inc., Biological E. Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use NEOSTIGMINE METHYLSULFATE INJECTION safely and effectively. See full prescribing information for NEOSTIGMINE METHYLSULFATE INJECTION.
NEOSTIGMINE METHYLSULFATE Injection, for intravenous use
Initial U.S. Approval: 1939INDICATIONS AND USAGE
Neostigmine methylsulfate injection, a cholinesterase inhibitor, is indicated for the reversal of the effects of non-depolarizing neuromuscular blocking agents (NMBAs) after surgery (1).
DOSAGE AND ADMINISTRATION
Should be administered by trained healthcare providers (2.1)
Peripheral nerve stimulator and monitoring for twitch responses should be used to determine when neostigmine methylsulfate injection should be initiated and if additional doses are needed (2.2)
– For reversal of NMBAs with shorter half-lives, when first twitch response is substantially greater than 10% of baseline, or when a second twitch is present: 0.03 mg/kg by intravenous route (2.2)
– For reversal of NMBAs with longer half-lives or when first twitch response is close to 10% of baseline: 0.07 mg/kg by intravenous route (2.2)
Maximum total dosage is 0.07 mg/kg or up to a total of 5 mg (whichever is less) (2.2)
An anticholinergic agent, e.g., atropine sulfate or glycopyrrolate, should be administered prior to or concomitantly with neostigmine methylsulfate injection (2.4)
DOSAGE FORMS AND STRENGTHS
Injection: 0.5 mg/mL and 1 mg/mL in 10 mL multiple-dose vials (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
Bradycardia: Atropine or glycopyrrolate should be administered prior to neostigmine methylsulfate injection to lessen risk of bradycardia. (5.1)
Serious Reactions with Coexisting Conditions: Use with caution in patients with, coronary artery disease, cardiac arrhythmias, recent acute coronary syndrome or myasthenia gravis. (5.2)
Neuromuscular Dysfunction: Can occur if large doses of neostigmine methylsulfate injection are administered when neuromuscular blockade is minimal; reduce dose if recovery from neuromuscular blockade is nearly complete. (5.4)
ADVERSE REACTIONS
Most common adverse reactions during treatment: bradycardia, nausea and vomiting. (6)
To report SUSPECTED ADVERSE REACTIONS, contact BE Pharmaceuticals Inc. at 1-877-648-9517 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
Pregnancy: No human data and limited animal data exist. Use only if clearly needed. (8)
Revised: 11/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS & USAGE
2 DOSAGE & ADMINISTRATION
2.1. Important Dosage Information
2.2. Dosage in Adults
2.3. Dosage in Pediatric Patients, including Neonates
2.4. Anticholinergic (Atropine or Glycopyrrolate) Administration
3 DOSAGE FORMS & STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1. Bradycardia
5.2. Serious Adverse Reactions in Patients with Certain Coexisting Conditions
5.3. Hypersensitivity
5.4. Neuromuscular Dysfunction
5.5. Cholinergic Crisis
6 ADVERSE REACTIONS
6.1. Clinical Trials Experience
6.2. Post Marketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor & Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6. Renal Impairment
8.7. Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis & Mutagenesis & Impairment Of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS & USAGE
-
2 DOSAGE & ADMINISTRATION
2.1. Important Dosage Information
Neostigmine methylsulfate injection should be administered by trained healthcare providers familiar with the use, actions, characteristics, and complications of neuromuscular blocking agents (NMBA) and neuromuscular block reversal agents. Doses of neostigmine methylsulfate injection should be individualized, and a peripheral nerve stimulator should be used to determine the time of initiation of neostigmine methylsulfate injection and should be used to determine the need for additional doses.
Neostigmine methylsulfate injection is for intravenous use only and should be injected slowly over a period of at least 1 minute. The neostigmine methylsulfate injection dosage is weight-based [see Dosage and Administration (2.2)].
Prior to neostigmine methylsulfate injection administration and until complete recovery of normal ventilation, the patient should be well ventilated and a patent airway maintained. Satisfactory recovery should be judged by adequacy of skeletal muscle tone and respiratory measurements in addition to the response to peripheral nerve stimulation.
An anticholinergic agent, e.g., atropine sulfate or glycopyrrolate, should be administered prior to or concomitantly with neostigmine methylsulfate injection [see Dosage and Administration (2.4)]
2.2. Dosage in Adults
a. Peripheral nerve stimulation devices capable of delivering a train-of-four (TOF) stimulus are essential to effectively using neostigmine methylsulfate injection.
b. There must be a twitch response to the first stimulus in the TOF of at least 10% of its baseline level, i.e., the response prior to NMBA administration, prior to the administration of neostigmine methylsulfate injection.
c. Prior to administration, visually inspect neostigmine methylsulfate injection for particulate matter and discoloration.
d. Neostigmine methylsulfate injection should be injected slowly by intravenous route over a period of at least 1 minute.
e. A 0.03 mg/kg to 0.07 mg/kg dose of neostigmine methylsulfate injection will generally achieve a TOF twitch ratio of 90% (TOF0.9) within 10 to 20 minutes of administration. Dose selection should be based on the extent of spontaneous recovery that has occurred at the time of administration, the half-life of the NMBA being reversed, and whether there is a need to rapidly reverse the NMBA.
The 0.03 mg/kg dose is recommended for:
i. Reversal of NMBAs with shorter half-lives, e.g., rocuronium, or
ii. When the first twitch response to the TOF stimulus is substantially greater than 10% of baseline or when a second twitch is present.
The 0.07 mg/kg dose is recommended for
iii. NMBAs with longer half-lives, e.g., vecuronium and pancuronium, or
iv. When the first twitch response is relatively weak, i.e., not substantially greater than 10% of baseline or
v. There is need for more rapid recovery.
f. TOF monitoring should continue to be used to evaluate the extent of recovery of neuromuscular function and the possible need for an additional dose of neostigmine methylsulfate injection.
g. TOF monitoring alone should not be relied upon to determine the adequacy of reversal of neuromuscular blockade as related to a patient’s ability to adequately ventilate and maintain a patent airway following tracheal extubation.
h. Patients should continue to be monitored for adequacy of reversal from NMBAs for a period of time that would assure full recovery based on the patient’s medical condition and the pharmacokinetics of neostigmine and the NMBA used.
i. The recommended maximum total dose is 0.07 mg/kg or up to a total of 5 mg, whichever is less.
2.3. Dosage in Pediatric Patients, including Neonates
Adult guidelines should be followed when neostigmine methylsulfate injection is administered to pediatric patients. Pediatric patients require neostigmine methylsulfate injection doses similar to those for adult patients.
2.4. Anticholinergic (Atropine or Glycopyrrolate) Administration
An anticholinergic agent, e.g., atropine sulfate or glycopyrrolate, should be administered prior to or concomitantly with neostigmine methylsulfate injection. The anticholinergic agent should be administered intravenously using a separate syringe. In the presence of bradycardia, it is recommended that the anticholinergic agent be administered prior to neostigmine methylsulfate injection.
- 3 DOSAGE FORMS & STRENGTHS
-
4 CONTRAINDICATIONS
Neostigmine methylsulfate injection is contraindicated in patients with:
known hypersensitivity to neostigmine methylsulfate (known hypersensitivity reactions have included urticaria, angioedema, erythema multiforme, generalized rash, facial swelling, peripheral edema, pyrexia, flushing, hypotension, bronchospasm,
bradycardia and anaphylaxis).
with peritonitis or mechanical obstruction of the intestinal or urinary tract.
-
5 WARNINGS AND PRECAUTIONS
5.1. Bradycardia
Neostigmine has been associated with bradycardia. Atropine sulfate or glycopyrrolate should be administered prior to neostigmine methylsulfate injection to lessen the risk of bradycardia [see Dosage and Administration (2.4)].
5.2. Serious Adverse Reactions in Patients with Certain Coexisting Conditions
Neostigmine methylsulfate injection should be used with caution in patients with coronary artery disease, cardiac arrhythmias, recent acute coronary syndrome or myasthenia gravis. Because of the known pharmacology of neostigmine methylsulfate as an acetylcholinesterase inhibitor, cardiovascular effects such as bradycardia, hypotension or dysrhythmia would be anticipated. In patients with certain cardiovascular conditions such as coronary artery disease, cardiac arrhythmias or recent acute coronary syndrome, the risk of blood pressure and heart rate complications may be increased. Risk of these complications may also be increased in patients with myasthenia gravis. Standard antagonism with anticholinergics (e.g., atropine) is generally successful to mitigate the risk of cardiovascular complications.
5.3. Hypersensitivity
Because of the possibility of hypersensitivity, atropine and medications to treat anaphylaxis should be readily available.
5.4. Neuromuscular Dysfunction
Large doses of neostigmine methylsulfate injection administered when neuromuscular blockade is minimal can produce neuromuscular dysfunction. The dose of neostigmine methylsulfate injection should be reduced if recovery from neuromuscular blockade is nearly complete.
5.5. Cholinergic Crisis
It is important to differentiate between myasthenic crisis and cholinergic crisis caused by overdosage of neostigmine methylsulfate injection. Both conditions result in extreme muscle weakness but require radically different treatment. [see Overdosage (10)]
-
6 ADVERSE REACTIONS
6.1. Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse reactions to neostigmine methylsulfate are most often attributable to exaggerated pharmacological effects, in particular, at muscarinic receptor sites. The use of an anticholinergic agent, e.g., atropine sulfate or glycopyrrolate, may prevent or mitigate these reactions.
Quantitative adverse event data are available from trials of neostigmine methylsulfate in which 200 adult patients were exposed to the product. The following table lists the adverse reactions that occurred with an overall frequency of 1% or greater.
System Organ Class
Adverse Reaction
Cardiovascular Disorders
bradycardia, hypotension, tachycardia/heart rate increase
Gastrointestinal Disorders
dry mouth, nausea, post-procedural nausea, vomiting
General Disorders and Administration Site Conditions
incision site complication, pharyngolaryngeal pain, procedural complication, procedural pain
Nervous System Disorders
dizziness, headache, postoperative shivering, prolonged neuromuscular blockade
Psychiatric Disorders
insomnia
Respiratory, Thoracic and Mediastinal Disorders
dyspnea, oxygen desaturation <90%
Skin and Subcutaneous Tissue Disorders
pruritus
6.2. Post Marketing Experience
The following adverse reactions have been identified during parenteral use of neostigmine methylsulfate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
System Organ Class
Adverse Reaction
Allergic Disorders
allergic reactions, anaphylaxis
Nervous System Disorders
convulsions, drowsiness, dysarthria, fasciculation, loss of consciousness, miosis, visual changes
Cardiovascular Disorders
cardiac arrest, cardiac arrhythmias (A-V block, nodal rhythm), hypotension, nonspecific EKG changes, syncope
Respiratory, Thoracic and Mediastinal Disorders
bronchospasm; increased oral, pharyngeal and bronchial secretions; respiratory arrest; respiratory depression
Skin and Sub-cutaneous Tissue Disorders
rash, urticaria
Gastrointestinal Disorders
bowel cramps, diarrhea, flatulence, increased peristalsis
Renal and Urinary Disorders
urinary frequency
Musculoskeletal and Connective Tissue Disorders
arthralgia, muscle cramps, spasms, weakness
Miscellaneous
diaphoresis, flushing
-
7 DRUG INTERACTIONS
The pharmacokinetic interaction between neostigmine methylsulfate and other drugs has not been studied. Neostigmine methylsulfate is metabolized by microsomal enzymes in the liver. Use with caution when using neostigmine methylsulfate injection with other drugs which may alter the activity of metabolizing enzymes or transporters.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no adequate or well-controlled studies of neostigmine methylsulfate injection in pregnant women. It is not known whether neostigmine methylsulfate injection can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. The incidence of malformations in human pregnancies has not been established for neostigmine as the data are limited. All pregnancies, regardless of drug exposure, have a background risk of 2 to 4% for major birth defects, and 15 to 20% for pregnancy loss.
No adverse effects were noted in rats or rabbits treated with human equivalent doses of neostigmine methylsulfate doses up to 8.1 and 13 mcg/kg/day, respectively, during organogenesis (0.1 to 0.2-times the maximum recommended human dose of 5 mg/60 kg person/day based on body surface area comparisons).
Anticholinesterase drugs, including neostigmine may cause uterine irritability and induce premature labor when administered to pregnant women near term.
Neostigmine methylsulfate injection should be given to a pregnant woman only if clearly needed.
Data
Animal Data
In embryofetal development studies, rats and rabbits were administered neostigmine methylsulfate at human equivalent doses (HED, on a mg/m2 basis) of 1.6, 4 and 8.1 mcg/kg/day 3.2, 8.1, and 13 mcg/kg/day, respectively, during the period of organogenesis (Gestation Days 6 through 17 for rats and Gestation Days 6 through 18 for rabbits). There was no evidence for a teratogenic effect in rats and rabbits up to HED 8.1 and 13 mcg/kg/day, which are approximately 0.097-times and 0.16-times the MRHD of 5 mg/60 kg, respectively in the presence of minimal maternal toxicity (tremors, ataxia, and prostration). The studies resulted in exposures in the animals well below predicted exposures in humans.
In a pre- and postnatal development study in rats, neostigmine methylsulfate was administered to pregnant female rats at human equivalent doses (HED) of 1.6, 4 and 8.1 mcg/kg/day from Day 6 of gestation through Day 20 of lactation, with weaning on Day 21. There were no adverse effects on physical development, behavior, learning ability, or fertility in the offspring occurred at HED doses up 8.1 mcg/kg/day which is 0.097-times the MRHD of 5 mg/60 kg on a mg/m2 basis in the presence of minimal maternal toxicity (tremors, ataxia, and prostration). The studies resulted in exposures in the animals well below predicted exposures in humans.
8.2 Labor & Delivery
The effect of neostigmine methylsulfate injection on the mother and fetus with regard to labor, delivery, the need for forceps delivery or other intervention or resuscitation of the newborn, is not known.
Cholinesterase inhibitor drugs may induce premature labor when given intravenously to pregnant women near term.
8.3 Nursing Mothers
It is not known whether neostigmine methylsulfate is excreted in human milk. Caution should be exercised when neostigmine methylsulfate injection is administered to a nursing woman.
8.4 Pediatric Use
Neostigmine methylsulfate injection is approved for the reversal of the effects of non-depolarizing neuromuscular blocking agents after surgery in pediatric patients of all ages.
Recovery of neuromuscular activity occurs more rapidly with smaller doses of cholinesterase inhibitors in infants and children than in adults. However, infants and small children may be at greater risk of complications from incomplete reversal of neuromuscular blockade due to decreased respiratory reserve. The risks associated with incomplete reversal outweigh any risk from giving higher doses of neostigmine methylsulfate injection (up to 0.07 mg/kg or up to a total of 5 mg, whichever is less).
The dose of neostigmine methylsulfate injection required to reverse neuromuscular blockade in children varies between 0.03 mg to 0.07 mg/kg, the same dose range shown to be effective in adults, and should be selected using the same criteria as used for adult patients. [see Clinical Pharmacology (12.3)]
Since the blood pressure in pediatric patients, particularly infants and neonates, is sensitive to changes in heart rate, the effects of an anticholinergic agent (e.g., atropine) should be observed prior to administration of neostigmine to lessen the probability of bradycardia and hypotension.
8.5 Geriatric Use
Because elderly patients are more likely to have decreased renal function, neostigmine methylsulfate injection should be used with caution and monitored for a longer period in elderly patients. The duration of action of neostigmine methylsulfate is prolonged in the elderly; however, elderly patients also experience slower spontaneous recovery from neuromuscular blocking agents. Therefore, dosage adjustments are not generally needed in geriatric patients; however, they should be monitored for longer periods than younger adults to assure additional doses of neostigmine methylsulfate injection are not required. The duration of monitoring should be predicated on the anticipated duration of action for the NMBA used on the patient. [see Dosage and Administration (2.3)].
8.6. Renal Impairment
Elimination half-life of neostigmine methylsulfate was prolonged in anephric patients compared to normal subjects.
Although no adjustments to neostigmine methylsulfate injection dosing appear to be warranted in patients with impaired renal function, they should be closely monitored to assure the effects of the neuromuscular blocking agent, particularly one cleared by the kidneys, do not persist beyond those of neostigmine methylsulfate injection. In this regard, the interval for re-dosing the neuromuscular blocking agent during the surgical procedure may be useful in determining whether, and to what extent, post-operative monitoring needs to be extended.
8.7. Hepatic Impairment
The pharmacokinetics of neostigmine methylsulfate in patients with hepatic impairment have not been studied. Neostigmine methylsulfate is metabolized by microsomal enzymes in the liver. No adjustments to the dosing of neostigmine methylsulfate injection appear to be warranted in patients with hepatic insufficiency. However, patients should be carefully monitored if hepatically cleared neuromuscular blocking agents were used during their surgical procedure as their duration of action may be prolonged by hepatic insufficiency whereas neostigmine methylsulfate injection, which undergoes renal elimination, will not likely be affected. This could result in the effects of the neuromuscular blocking agent outlasting those of neostigmine methylsulfate injection. This same situation may arise if the neuromuscular blocking agent has active metabolites. In this regard, the interval for re-dosing the neuromuscular blocking agent during the surgical procedure may be useful in determining whether, and to what extent, post-operative monitoring needs to be extended.
-
10 OVERDOSAGE
Muscarinic symptoms (nausea, vomiting, diarrhea, sweating, increased bronchial and salivary secretions, and bradycardia) may appear with overdosage of neostigmine methylsulfate injection (cholinergic crisis), but may be managed by the use of additional atropine or glycopyrrolate. The possibility of iatrogenic overdose can be lessened by carefully monitoring the muscle twitch response to peripheral nerve stimulation. Should overdosage occur, ventilation should be supported by artificial means until the adequacy of spontaneous respiration is assured, and cardiac function should be monitored.
Overdosage of neostigmine methylsulfate injection can cause cholinergic crisis, which is characterized by increasing muscle weakness, and through involvement of the muscles of respiration, may result in death. Myasthenic crisis, due to an increase in the severity of the disease, is also accompanied by extreme muscle weakness and may be difficult to distinguish from cholinergic crisis on a symptomatic basis. However, such differentiation is extremely important because increases in the dose of neostigmine methylsulfate injection or other drugs in this class, in the presence of cholinergic crisis or of a refractory or “insensitive” state, could have grave consequences. The two types of crises may be differentiated by the use of edrophonium chloride as well as by clinical judgment.
Treatment of the two conditions differs radically. Whereas the presence of myasthenic crisis requires more intensive anticholinesterase therapy, cholinergic crisis calls for the prompt withdrawal of all drugs of this type. The immediate use of atropine in cholinergic crisis is also recommended. Atropine may also be used to lessen gastrointestinal side effects or other muscarinic reactions; but such use, by masking signs of overdosage, can lead to inadvertent induction of cholinergic crisis.
-
11 DESCRIPTION
Neostigmine methylsulfate, a cholinesterase inhibitor, is (m-hydroxyphenyl) trimethylammonium methylsulfate dimethylcarbamate. The structural formula is:
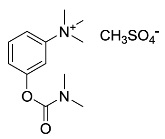
Neostigmine methylsulfate USP is a white powder and is very soluble in water and freely soluble in ethanol (96%). Neostigmine methylsulfate USP is a sterile, nonpyrogenic solution intended for intravenous use.
Each mL of the 0.5 mg/mL strength contains neostigmine methylsulfate USP 0.5 mg, phenol 4.5 mg (used as preservative) and sodium acetate trihydrate 0.2 mg, in water for injection. The pH is adjusted, when necessary, with acetic acid/sodium hydroxide to a value of 5.5.
Each mL of the 1 mg/mL strength contains neostigmine methylsulfate USP 1 mg, phenol 4.5 mg (used as preservative), and sodium acetate trihydrate 0.2 mg, in water for injection. The pH is adjusted, when necessary, with acetic acid/sodium hydroxide to achieve a value of 5.5.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Neostigmine methylsulfate is a competitive cholinesterase inhibitor. By reducing the breakdown of acetylcholine, neostigmine methylsulfate induces an increase in acetylcholine in the synaptic cleft which competes for the same binding site as non-depolarizing neuromuscular blocking agents, and reverses the neuromuscular blockade.
12.2 Pharmacodynamics
Neostigmine methylsulfate-induced increases in acetylcholine levels results in the potentiation of both muscarinic and nicotinic cholinergic activity. The resulting elevation of acetylcholine competes with non-depolarizing neuromuscular blocking agents to reverse neuromuscular blockade. Neostigmine methylsulfate does not readily cross the blood-brain barrier and, therefore, does not significantly affect cholinergic function in the central nervous system.
12.3 Pharmacokinetics
Distribution: Following intravenous injection, the observed neostigmine methylsulfate volume of distribution is reported between 0.12 and 1.4 L/kg. Protein binding of neostigmine methylsulfate to human serum albumin ranges from 15 to 25%.
Metabolism: Neostigmine methylsulfate is metabolized by microsomal enzymes in the liver.
Elimination: Following intravenous injection, the reported elimination half-life of neostigmine methylsulfate is between 24 and 113 minutes. Total body clearance of neostigmine methylsulfate is reported between 1.14 and 16.7 mL/min/kg.
Renal impairment: Elimination half-life of neostigmine methylsulfate was prolonged in anephric patients compared to normal subjects; elimination half-life for normal, transplant and anephric patients were 79.8 ± 48.6, 104.7 ± 64 and 181 ± 54 min (mean ± SD), respectively.
Hepatic impairment: The pharmacokinetics of neostigmine methylsulfate in patients with hepatic impairment has not been studied.
Pediatrics: Elimination half-life of neostigmine methylsulfate in infants (2 to 10 months), children (1 to 6 years) and adults (29 to 48 years) were 39 ± 5 min, 48 ± 16 min, and 67 ± 8 min (mean ± SD), respectively. Observed neostigmine methylsulfate clearance for infants, children and adults were 14 ± 3, 11 ± 3 and 10 ± 2 mL/min/kg (mean ± SD), respectively.
Drug Interaction Studies: The pharmacokinetic interaction between neostigmine methylsulfate and other drugs has not been studied.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis & Mutagenesis & Impairment Of Fertility
Carcinogenesis: Long-term animal studies have not been performed to evaluate the carcinogenic potential of neostigmine.
Genotoxicity: Neostigmine methylsulfate was not mutagenic or clastogenic when evaluated in an in vitro bacterial reverse mutation assay (Ames test), an in vitro Chinese hamster ovary cell chromosomal aberration assay, or an in vivo mouse bone marrow micronucleus assay.
Impairment of Fertility: In a fertility and early embryonic development study in rats, male rats were treated for 28 days prior to mating and female rats were treated for 14 days prior to mating with intravenous neostigmine methylsulfate (human equivalent doses of 1.6, 4, and 8.1 mcg/kg/day, based on body surface area). No adverse effects were reported at any dose (up to 0.1-times the MRHD of 5 mg/60 kg person based on a body surface area comparison).
-
14 CLINICAL STUDIES
The evidence for the efficacy of neostigmine methylsulfate for the reversal of the effects of non-depolarizing neuromuscular blocking agents after surgery is derived from the published literature. Randomized, spontaneous-recovery or placebo-controlled studies using similar efficacy endpoints evaluated a total of 404 adult and 80 pediatric patients undergoing various surgical procedures. Patients had reductions in their recovery time from neuromuscular blockade with neostigmine methylsulfate treatment compared to spontaneous recovery.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Neostigmine methylsulfate injection, USP is a clear, colourless solution free from visible particles in a glass vial. It is available as follows:
NDC No.
Strength
Vial Size
72572-460-24
0.5 mg/mL
10 mL multiple-dose vials (supplied in packages of 24)
72572-461-24
1 mg/mL
10 mL multiple-dose vials (supplied in packages of 24)
The vial stopper is not made with natural rubber latex.
Neostigmine Methylsulfate Injection, USP should be stored at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) (see USP Controlled Room Temperature). Protect from light. Store in carton until time of use.
Distributed by:
Civica, Inc.
Lehi, Utah 84043
Manufactured by:

Biological E. Limited
Plot No.4, Survey no. 542/P, Biotech Park Phase-II,
Kolthur Village, Shameerpet Mandal,
Medchal, Telangana 500078, India.
Revised: September 2019
20001702
-
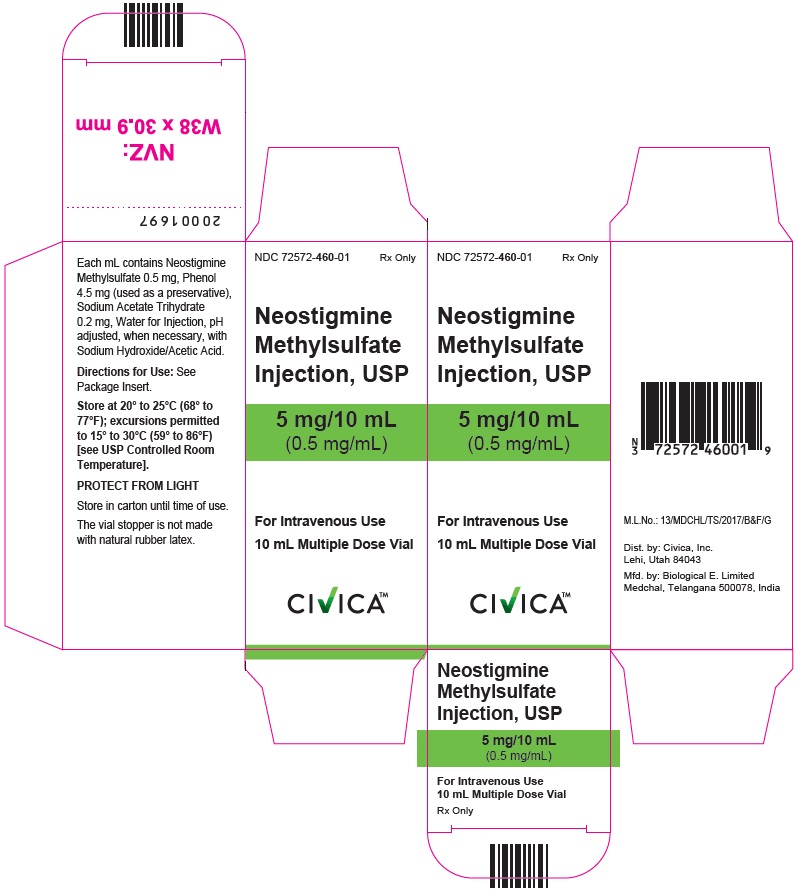
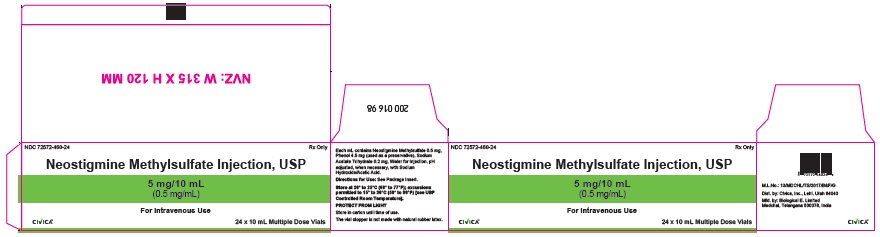
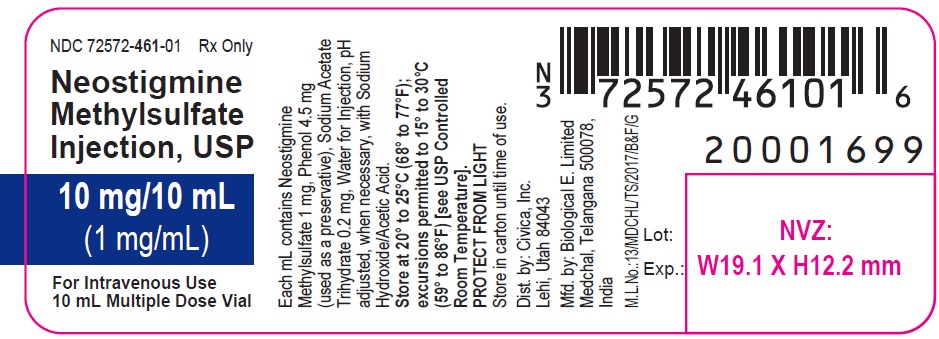
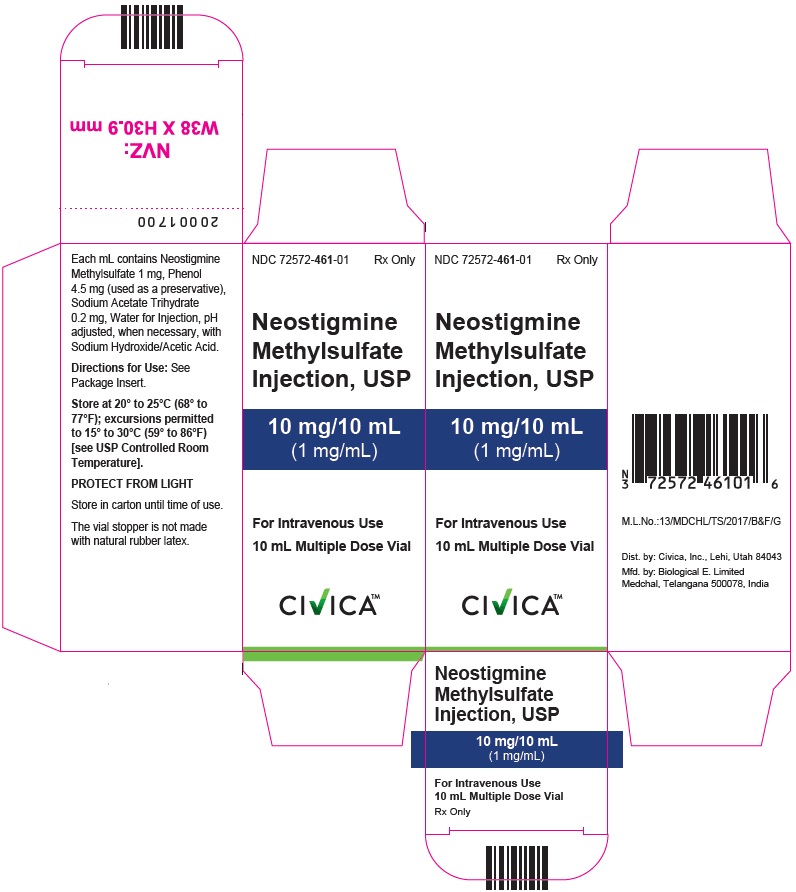
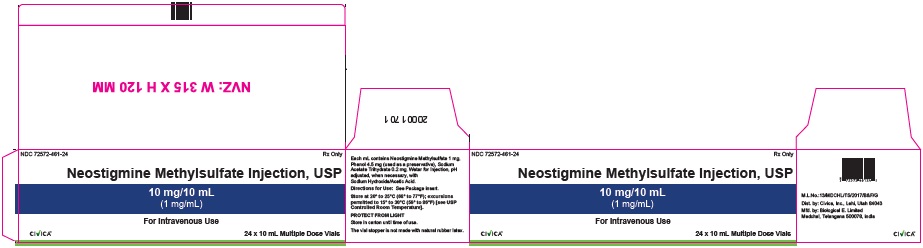
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Neostigmine Methylsulfate Injection USP, 5 mg/10 mL (0.5 mg/mL) - Vial Label
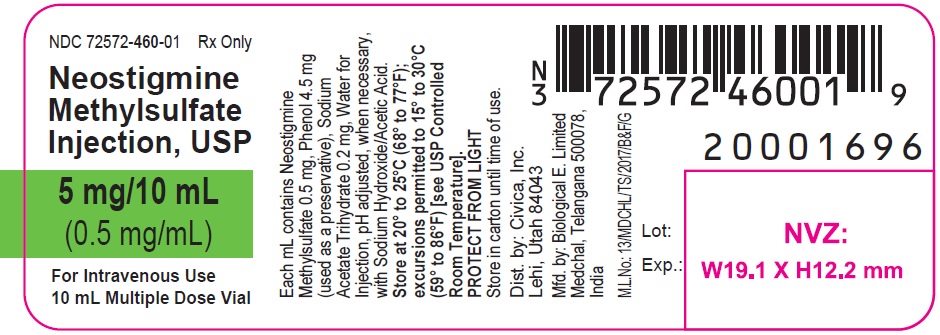
Neostigmine Methylsulfate Injection USP, 5 mg/10 mL (0.5 mg/mL) - Carton Label
Neostigmine Methylsulfate Injection USP, 5 mg/10 mL (0.5 mg/mL) - 24s Outer Carton Label
Neostigmine Methylsulfate Injection USP, 10 mg/10 mL (1 mg/mL) - Vial Label
Neostigmine Methylsulfate Injection USP, 10 mg/10 mL (1 mg/mL) - Carton Label
Neostigmine Methylsulfate Injection USP, 10 mg/10 mL (1 mg/mL) - 24s Outer Carton Label
-
INGREDIENTS AND APPEARANCE
NEOSTIGMINE METHYLSULFATE
neostigmine methylsulfate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 72572-460 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NEOSTIGMINE METHYLSULFATE (UNII: 98IMH7M386) (NEOSTIGMINE - UNII:3982TWQ96G) NEOSTIGMINE METHYLSULFATE 0.5 mg in 1 mL Inactive Ingredients Ingredient Name Strength PHENOL (UNII: 339NCG44TV) 4.5 mg in 1 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.2 mg in 1 mL ACETIC ACID (UNII: Q40Q9N063P) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 72572-460-24 24 in 1 CARTON 05/13/2019 1 NDC: 72572-460-01 1 in 1 CARTON 1 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212512 05/13/2019 NEOSTIGMINE METHYLSULFATE
neostigmine methylsulfate injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 72572-461 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength NEOSTIGMINE METHYLSULFATE (UNII: 98IMH7M386) (NEOSTIGMINE - UNII:3982TWQ96G) NEOSTIGMINE METHYLSULFATE 1 mg in 1 mL Inactive Ingredients Ingredient Name Strength PHENOL (UNII: 339NCG44TV) 4.5 mg in 1 mL SODIUM ACETATE (UNII: 4550K0SC9B) 0.2 mg in 1 mL ACETIC ACID (UNII: Q40Q9N063P) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 72572-461-24 24 in 1 CARTON 05/13/2019 1 NDC: 72572-461-01 1 in 1 CARTON 1 10 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212512 05/13/2019 Labeler - Civica Inc. (081373942) Establishment Name Address ID/FEI Business Operations Biological E. Limited 871410645 ANALYSIS(72572-460, 72572-461) , MANUFACTURE(72572-460, 72572-461)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.