CONRAY 43- iothalamate meglumine injection
Conray 43 by
Drug Labeling and Warnings
Conray 43 by is a Prescription medication manufactured, distributed, or labeled by Liebel-Flarsheim Company LLC, LIEBEL-FLARSHEIM COMPANY LLC, Justesa Imagen, S.A.U.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- BOXED WARNING (What is this?)
-
DESCRIPTION
Conray 43 is a sterile aqueous solution intended for use as a diagnostic radiopaque medium. Conray 43 contains 43% w/v iothalamate meglumine which is 1-deoxy-1-(methylamino)-D-glucitol 5-acetamido-2,4,6-triiodo-N-methylisophthalamate (salt), and has the following structural formula:
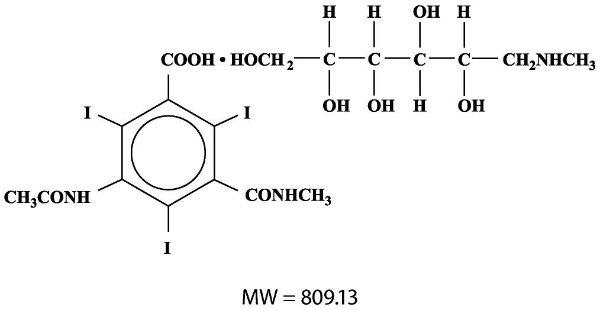
Each milliliter contains 430 mg of iothalamate meglumine, 0.110 mg edetate calcium disodium as a stabilizer and 0.115 mg of monobasic sodium phosphate as a buffer. The solution provides 20.2% (202 mg/mL) organically bound iodine. Conray 43 has an osmolarity of approximately 800 mOsmol per liter, an osmolality of approximately 1000 mOsmol per kilogram and is, therefore, hypertonic under conditions of use. The viscosity (cps) is approximately 3 at 25°C and 2 at 37°C. The pH is 6.6 to 7.6.
Conray 43 is a clear solution containing no undissolved solids. Crystallization does not occur at normal room temperatures. It is supplied in containers from which the air has been displaced by nitrogen.
-
CLINICAL PHARMACOLOGY
Intravascular Procedures
Following intravascular injection, Conray 43 is rapidly transported through the circulatory system to the kidneys and is excreted unchanged in the urine by glomerular filtration. The pharmacokinetics of intravascularly administered radiopaque contrast media are usually best described by a two compartment model with a rapid alpha phase for drug distribution and a slower beta phase for drug elimination. In patients with normal renal function, the alpha and beta half-lives of Conray 43 were approximately 10 and 90 minutes, respectively.
Arteriography and venography may be performed following injection into an appropriate vessel and will permit visualization until significant hemodilution occurs.
Following infusion of Conray 43, the upper and lower urinary tract is opacified. Renal accumulation is sufficiently rapid that maximum radiographic density in the calyces and pelves occurs by the time the infusion is complete. In patients with impaired renal function, diagnostic opacification frequently is achieved only after prolonged periods.
Injectable iodinated contrast agents are excreted either through the kidneys or through the liver. These two excretory pathways are not mutually exclusive, but the main route of excretion seems to be related to the affinity of the contrast medium for serum albumin. Iothalamate salts are poorly bound to serum albumin, and are excreted mainly through the kidneys.
The liver and small intestine provide the major alternate route of excretion. In patients with severe renal impairment, the excretion of this contrast medium through the gallbladder and into the small intestine sharply increases.
Iothalamate salts cross the placental barrier in humans and are excreted unchanged in human milk.
CT Scanning of the Head
When used for contrast enhancement in computed tomographic brain scanning, the degree of enhancement is directly related to the amount of iodine administered. Rapid injection of the entire dose yields peak blood iodine concentrations immediately following the injection, which fall rapidly over the next five to ten minutes. This can be accounted for by the dilution in the vascular and extracellular fluid compartments which causes an initial sharp fall in plasma concentration. Equilibration with the extracellular compartments is reached by about ten minutes; thereafter the fall becomes exponential. Maximum contrast enhancement frequently occurs after peak blood iodine levels are reached. The delay in maximum contrast enhancement can range from five to forty minutes, depending on the peak iodine levels achieved and the cell type of the lesion. This lag suggests that the contrast enhancement of the image is at least in part dependent on the accumulation of iodine within the lesion and outside the blood pool.
In brain scanning, the contrast medium (Conray 43) does not accumulate in normal brain tissue due to the presence of the “blood brain barrier.” The increase in x-ray absorption in the normal brain is due to the presence of the contrast agent within the blood pool. A break in the blood brain barrier, such as occurs in malignant tumors of the brain, allows accumulation of contrast medium within the interstitial tumor tissue; adjacent normal brain tissue does not contain the contrast medium.
The image enhancement of non-tumoral lesions, such as arteriovenous malformations and aneurysms, is dependent on the iodine content of the circulating blood pool.
CT Scanning of the Body
Conray 43 may also be used for enhancement of computed tomographic scans performed for detection and evaluation of lesions in the liver, pancreas, kidneys, abdominal aorta, mediastinum, abdominal cavity and retroperitoneal space.
In non-neural tissues (during computed tomography of the body), Conray 43 diffuses rapidly from the vascular to the extra-vascular space. Increase in x-ray absorption is related to blood flow, concentration of the contrast medium and extraction of the contrast medium by interstitial tissue since no barrier exists; contrast enhancement is thus due to the relative differences in extra-vascular diffusion between normal and abnormal tissue, a situation quite different than that in the brain.
The pharmacokinetics of Conray 43 in normal and abnormal tissues has been shown to be variable.
Enhancement of CT with Conray 43 may be of benefit in establishing diagnoses of certain lesions in some sites with greater assurance than is possible with unenhanced CT and in supplying additional features of the lesions. In other cases, the contrast medium may allow visualization of lesions not seen with CT alone or may help to define suspicious lesions seen with unenhanced CT.
Contrast enhancement appears to be greatest within the 30 to 90 seconds after bolus administration of the contrast agent, and after intra-arterial rather than intravenous administration. Therefore, the use of a continuous scanning technique (a series of two to three second scans beginning at the injection – dynamic CT scanning) may improve enhancement and diagnostic assessment of tumors and other lesions such as an abscess, occasionally revealing more extensive disease.
A cyst or similar non-vascularized lesion may be distinguished from vascularized solid lesions by comparing enhanced and unenhanced scans; the non-vascularized lesions show no change in CT number, the vascularized lesions would show an increase. The latter might be benign, malignant or normal, but it is unlikely that it would be a cyst, hematoma, or other non-vascularized lesion.
Because unenhanced scanning may provide adequate information in the individual patient, the decision to employ contrast enhancement, which is associated with additional risk and increased radiation exposure, should be based upon a careful evaluation of clinical, other radiological, and unenhanced CT findings.
Retrograde Urographic Procedures
The most important characteristic of contrast media is the iodine content. The relatively high atomic weight of iodine contributes sufficient radiodensity for radiographic contrast.
Following instillation by sterile catheter, Conray 43 provides for visualization of the lower urinary tract. Clinical literature reports indicate that routinely less than 1 percent of a retrograde urographic radiopaque is absorbed systemically; however, as much as 12 percent absorption was observed with pyelorenal back flow and may produce iodine mediated thyrotropic effects described under PRECAUTIONS.
-
INDICATIONS AND USAGE
Intravascular Indications
Conray 43 is indicated for use in lower extremity venography, intravenous infusion urography, contrast enhancement of computed tomographic brain images and arterial digital subtraction angiography.
Conray 43 may also be used for enhancement of computed tomographic scans performed for detection and evaluation of lesions in the liver, pancreas, kidneys, abdominal aorta, mediastinum, abdominal cavity and retroperitoneal space. Continuous or multiple scans separated by intervals of 1 to 3 seconds during the first 30 to 90 seconds post-injection of the contrast medium (dynamic CT scanning) may provide enhancement of diagnostic significance, and may be of benefit in establishing diagnoses of certain lesions in these sites with greater assurance than is possible with CT alone and in supplying additional features of the lesions. In other cases, the contrast agent may allow visualization of lesions not seen with CT alone, or may help to define suspicious lesions seen with unenhanced CT (see CLINICAL PHARMACOLOGY). Subsets of patients in whom delayed body CT scans might be helpful have not been identified. Inconsistent results have been reported and abnormal and normal tissues may be isodense during the same time frame used for delayed CT scanning. The risks of such indiscriminate use of contrast media are well known and such use is not recommended. At present, consistent results have been documented using dynamic CT techniques only.
-
CONTRAINDICATIONS
Conray 43 should not be used for myelography.
Refer to PRECAUTIONS, General, concerning hypersensitivity.
Contraindications to the procedure of retrograde pyelography include obstruction to endoscopy or catheterization of the ureters, severe systemic disease which contraindicates instrumentation and acute infection of the upper urinary tract.
-
WARNINGS
SEVERE ADVERSE EVENTS – INADVERTENT INTRATHECAL ADMINISTRATION:
Serious adverse reactions have been reported due to the inadvertent intrathecal administration of iodinated contrast media that are not indicated for intrathecal use. These serious adverse reactions include: death, convulsions, cerebral hemorrhage, coma, paralysis, arachnoiditis, acute renal failure, cardiac arrest, seizures, rhabdomyolysis, hyperthermia, and brain edema. Special attention must be given to ensure that this drug product is not administered intrathecally.
Ionic iodinated contrast media inhibit blood coagulation, in vitro, more than nonionic contrast media. Nonetheless, it is prudent to avoid prolonged contact of blood with syringes containing ionic contrast media.
Serious, rarely fatal, thromboembolic events causing myocardial infarction and stroke have been reported during angiographic procedures with both ionic and nonionic contrast media. Therefore, meticulous intravascular administration technique is necessary, particularly during angiographic procedures, to minimize thromboembolic events. Numerous factors, including length of procedure, catheter and syringe material, underlying disease state and concomitant medications may contribute to the development of thromboembolic events. For these reasons, meticulous angiographic techniques are recommended including close attention to guidewire and catheter manipulation, use of manifold systems and/or three-way stopcocks, frequent catheter flushing with heparinized saline solutions and minimizing the length of the procedure. The use of plastic syringes in place of glass syringes has been reported to decrease but not eliminate the likelihood of in vitro clotting.
Serious or fatal reactions have been associated with the administration of iodine containing radiopaque media. It is of utmost importance to be completely prepared to treat any contrast medium reaction.
Serious neurologic sequelae, including permanent paralysis, have been reported following cerebral arteriography, selective spinal arteriography and arteriography of vessels supplying the spinal cord. The intravascular injection of a contrast medium should never be made following the administration of vasopressors since they strongly potentiate neurologic effects.
In patients with subarachnoid hemorrhage, a rare association between contrast administration and clinical deterioration, including convulsions and death, has been reported. Therefore, administration of intravascular iodinated ionic contrast media in these patients should be undertaken with caution.
A definite risk exists in the use of intravascular contrast agents in patients who are known to have multiple myeloma. In such instances anuria has developed resulting in progressive uremia, renal failure and eventually death. Although neither the contrast agent nor dehydration has separately proved to be the cause of anuria in myeloma, it has been speculated that the combination of both may be causative factors. The risk in myelomatous patients is not a contraindication to the procedure; however, partial dehydration in the preparation of these patients for the examination is not recommended since this may predispose to precipitation of myeloma protein in the renal tubules. No form of therapy, including dialysis, has been successful in reversing the effect. Myeloma, which occurs most commonly in persons over 40, should be considered before instituting intravascular administration of contrast agents.
Administration of radiopaque materials to patients known or suspected to have pheochromocytoma should be performed with extreme caution. If, in the opinion of the physician, the possible benefits of such procedures outweigh the considered risks, the procedures may be performed; however, the amount of radiopaque medium injected should be kept to an absolute minimum. The blood pressure should be assessed throughout the procedure, and measures for treatment of a hypertensive crisis should be available.
Contrast media have been shown to promote the phenomenon of sickling in individuals who are homozygous for sickle cell disease when the material is injected intravenously or intra-arterially.
Convulsions have occurred in patients with primary or metastatic cerebral lesions following the administration of iodine-containing radiopaque media for the contrast enhancement of CT brain images.
In patients with advanced renal disease, iodinated contrast media should be used with caution, and only when the need for the examination dictates, since excretion of the medium may be impaired. Patients with combined renal and hepatic disease, those with severe hypertension or congestive heart failure, and recent renal transplant recipients may present an additional risk.
Renal failure has been reported in patients with liver dysfunction who were given an oral cholecystographic agent followed by an intravascular iodinated radiopaque agent and also in patients with occult renal disease, notably diabetics and hypertensives. In these classes of patients there should be no fluid restriction and every attempt made to maintain normal hydration, prior to contrast medium administration, since dehydration is the single most important factor influencing further renal impairment.
Acute renal failure has been reported in diabetic patients with diabetic nephropathy and in susceptible non-diabetic patients (often elderly with pre-existing renal disease) following the administration of iodinated contrast agents. Therefore, careful consideration of the potential risks should be given before performing this radiographic procedure in these patients.
Caution should be exercised in performing contrast medium studies in patients with endotoxemia and/or those with elevated body temperatures.
Reports of thyroid storm occurring following the intravascular use of iodinated radiopaque agents in patients with hyperthyroidism or with an autonomously functioning thyroid nodule, suggest that this additional risk be evaluated in such patients before use of this drug. Iodine containing contrast agents may alter the results of thyroid function tests which depend on iodine estimation, e.g. PBI and radioactive iodine uptake studies. Such tests, if indicated, should be performed prior to the administration of this preparation.
Severe Cutaneous Adverse Reactions: Severe cutaneous adverse reactions (SCAR) may develop from 1 hour to several weeks after intravascular contrast agent administration. These reactions include Stevens-Johnson syndrome and toxic epidermal necrolysis (SJS/TEN), acute generalized exanthematous pustulosis (AGEP) and drug reaction with eosinophilia and systemic symptoms (DRESS). Reaction severity may increase and time to onset may decrease with repeat administration of contrast agent; prophylactic medications may not prevent or mitigate severe cutaneous adverse reactions. Avoid administering Conray 43 to patients with a history of a severe cutaneous adverse reaction to Conray 43.
-
PRECAUTIONS
General
Diagnostic procedures which involve the use of iodinated intravascular contrast agents should be carried out under the direction of personnel skilled and experienced in the particular procedure to be performed. All procedures utilizing contrast media carry a definite risk of producing adverse reactions. While most reactions may be minor, life threatening and fatal reactions may occur without warning. The risk-benefit factor should always be carefully evaluated before such a procedure is undertaken. At all times a fully equipped emergency cart, or equivalent supplies and equipment, and personnel competent in recognizing and treating adverse reactions of all severity, or situations which may arise as a result of the procedure, should be immediately available. If a serious reaction should occur, immediately discontinue administration. Since severe delayed reactions have been known to occur, emergency facilities and competent personnel should be available for at least 30 to 60 minutes after administration (see ADVERSE REACTIONS).
Preparatory dehydration is dangerous and may contribute to acute renal failure in infants, young children, the elderly, patients with pre-existing renal insufficiency, patients with advanced vascular disease and diabetic patients.
Severe reactions to contrast media often resemble allergic responses. This has prompted the use of several provocative pretesting methods, none of which can be relied on to predict severe reactions. No conclusive relationship between severe reactions and antigen-antibody reactions or other manifestations of allergy has been established. The possibility of an idiosyncratic reaction in patients who have previously received a contrast medium without ill effect should always be considered. Prior to the injection of any contrast medium, the patient should be questioned to obtain a medical history with emphasis on allergy and hypersensitivity. A positive history of bronchial asthma, hay fever or allergy, including food, a family history of allergy, a known sensitivity to iodine per se, patients with a known clinical hypersensitivity to a contrast agent may imply a greater than usual risk. Such a history, by suggesting histamine sensitivity and consequently proneness to reactions, may be more accurate than pre-testing in predicting the potential for reaction, although not necessarily the severity or type of reaction in the individual case. A positive history of this type does not arbitrarily contraindicate the use of a contrast agent, when a diagnostic procedure is thought essential, but does call for caution (see ADVERSE REACTIONS).
Prophylactic therapy including corticosteroids and antihistamines should be considered for patients who present with a strong allergic history, a previous reaction to a contrast medium, or a positive pre-test since in these patients the incidence of reaction is two to three times that of the general population. Adequate doses of corticosteroids should be started early enough prior to contrast medium injection to be effective and should continue through the time of injection and for 24 hours after injection. Antihistamines should be administered within 30 minutes of the contrast medium injection. Recent reports indicate that such pre-treatment does not prevent life-threatening reactions, but may reduce both their incidence and severity. A separate syringe should be used for these injections.
Intravascular Precautions
Angiography should be avoided whenever possible in patients with homocystinuria because of the risk of inducing thrombosis and embolism.
Urographic Precautions
Since these procedures require instrumentation, special precautions should be observed in those patients known to have an acute urinary tract infection.
Filling of the bladder should be done at a steady rate, exercising caution to avoid excessive pressure. Sterile procedures should be employed in administration.
Information for Patients
Patients receiving iodinated contrast agents should be instructed to:
- Inform your physician if you are, or might be, pregnant.
- Inform your physician if you are diabetic or if you have multiple myeloma, pheochromocytoma, homozygous sickle cell disease or known thyroid disease (see WARNINGS).
- Inform your physician if you are allergic to any drugs, food or if you had any reactions to previous injections of dyes used for x-ray procedures (see PRECAUTIONS, General).
- Inform your physician about any other medications you are currently taking including nonprescription drugs.
- Consult with your physician if, at some future date, any thyroid tests are planned. The iodine in this agent may interfere with later thyroid tests.
- Advise patients to inform their physician if they develop a rash after receiving Conray 43.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term animal studies have been performed to evaluate carcinogenic potential. However, animal studies suggest that this drug is not mutagenic and does not affect fertility in males or females.
Nursing Mothers
Iothalamate salts are excreted unchanged in human milk. Because of the potential for adverse effects in nursing infants, bottle feedings should be substituted for breast feedings for 24 hours following the administration of this drug.
(Precautions for specific procedures receive comment under that procedure.)
-
ADVERSE REACTIONS
Intravascular Procedures
Adverse reactions to injectable contrast media fall into two categories: chemotoxic reactions and idiosyncratic reactions.
Chemotoxic reactions result from the physio-chemical properties of the contrast media, the dose and speed of injection. All hemodynamic disturbances and injuries to organs or vessels perfused by the contrast medium are included in this category.
Idiosyncratic reactions include all other reactions. They occur more frequently in patients 20 to 40 years old. Idiosyncratic reactions may or may not be dependent on the amount of dose injected, the speed of injection, the mode of injection and the radiographic procedure. Idiosyncratic reactions are subdivided into minor, intermediate and severe. The minor reactions are self-limited and of short duration; the severe reactions are life-threatening and treatment is urgent and mandatory.
Fatalities have been reported following the administration of iodine-containing contrast agents. Based upon clinical literature, the incidence of death is reported to range from one in 10,000 (0.01 percent) to less than one in 100,000 (0.001 percent).
The following adverse reactions have been observed in conjunction with the use of iodine-containing contrast agents.
The most frequent adverse reactions are nausea, vomiting, facial flush and a feeling of body warmth. These are usually of brief duration. Other reactions include the following:
Hypersensitivity reactions: Dermal manifestations of urticaria with or without pruritus, erythema and maculopapular rash. Dry mouth. Sweating. Conjunctival symptoms. Facial, peripheral and angioneurotic edema. Symptoms related to the respiratory system include sneezing, nasal stuffiness, coughing, choking, dyspnea, chest tightness and wheezing, which may be initial manifestations of more severe and infrequent reactions including asthmatic attack, laryngospasm and bronchospasm with or without edema, pulmonary edema, apnea and cyanosis. Rarely, these allergic-type reactions can progress into anaphylaxis with loss of consciousness and coma and severe cardiovascular disturbances.
Cardiovascular reactions: Generalized vasodilation, flushing and venospasm. Occasionally, thrombosis or rarely, thrombophlebitis. Red blood cell clumping and agglutination, crenation and interference in clot formation. Extremely rare cases of disseminated intravascular coagulation resulting in death have been reported. Severe cardiovascular responses include rare cases of hypotensive shock, coronary insufficiency, cardiac arrhythmia, fibrillation and arrest. These severe reactions are usually reversible with prompt and appropriate management; however, fatalities have occurred.
Endocrine reactions: Thyroid function tests indicative of hypothyroidism or transient thyroid suppression have been uncommonly reported following iodinated contrast media administration to adult and pediatric patients, including infants. Some patients were treated for hypothyroidism.
Skin and Subcutaneous Tissue Disorders: Reactions range from mild (e.g. rash, erythema, pruritus, urticaria and skin discoloration) to severe: [Stevens-Johnson syndrome and toxic epidermal necrolysis (SJS/TEN), acute generalized exanthematous pustulosis (AGEP) and drug reaction with eosinophilia and systemic symptoms (DRESS)].
Technique reactions: Extravasation with burning pain, hematomas, ecchymosis and tissue necrosis, paresthesia or numbness, vascular constriction due to injection rate, thrombosis and thrombophlebitis.
Neurological reactions: Spasm, convulsions, aphasia, syncope, paresis, paralysis resulting from spinal cord injury and pathology associated with syndrome of transverse myelitis, visual field losses which are usually transient but may be permanent, coma and death.
Other reactions: Headache, trembling, shaking, chills without fever and lightheadedness. Temporary renal shutdown or other nephropathy.
(Adverse reactions to specific procedures receive comment under that procedure.)
Retrograde Urographic Procedures
Irritation of the bladder or ureter, common to some degree to all contrast media administered for retrograde urographic procedures, may occasionally occur.
As with all contrast media, intravasation may lead to hypersensitivity reactions such as a sense of warmth, flushing, sneezing, sweating, chills, fever, urticaria, laryngeal edema, bronchospasm, hypertension, hypotension, cardiac arrhythmias and cardiac arrest.
Oliguria or anuria may occur following retrograde pyelography, especially in patients with severe pre-existing renal disease.
Adverse reactions associated with procedural technique include injury to the urethra, bladder, ureter, and introduction of infection.
In the event of serious or anaphylactoid reactions, it should be kept in mind that the reactions known to occur with intravenous administration of radiopaque contrast materials are possible.
-
OVERDOSAGE
Overdosage may occur. The adverse effects of overdosage are life-threatening and affect mainly the pulmonary and cardiovascular system. The symptoms may include cyanosis, bradycardia, acidosis, pulmonary hemorrhage, convulsions, coma and cardiac arrest. Treatment of an overdose is directed toward the support of all vital functions and prompt institution of symptomatic therapy.
Iothalamate salts are dialyzable.
The intravenous LD50 value of various concentrations of Iothalamate Meglumine (in grams of iodine/kilogram body weight) varied from 5.7 to 8.9 g/kg in mice and 9.8 to 11.2 g/kg in rats. The LD50 values decrease as the rate of injection increases.
-
DOSAGE AND ADMINISTRATION
Intravascular Administration
It is advisable that Conray 43 be at or close to body temperature when injected.
The patient should be instructed to omit the meal that precedes the examination. Appropriate premedication, which may include a barbiturate, tranquilizer or analgesic drug, may be administered prior to the examination.
A preliminary film is recommended to check the position of the patient and the x-ray exposure factors.
If during administration a minor reaction occurs the injection should be slowed or stopped until the reaction has subsided. If a major reaction occurs the injection should be discontinued immediately.
Under no circumstances should either corticosteroids or antihistamines be mixed in the same syringe with the contrast medium because of a potential for chemical incompatibility.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
-
LOWER EXTREMITY VENOGRAPHY
Precautions
All patients should be well hydrated prior to the procedure. In addition to the general precautions previously described, special care is required when venography is performed in patients with suspected thrombosis, phlebitis, severe ischemic disease, local infection or a totally obstructed venous system. Extreme caution during injection of the contrast agent is necessary to avoid extravasation and fluoroscopy is recommended. This is especially important in patients with severe arterial or venous disease.
Adverse Reactions
In addition to the general adverse reactions previously described, thrombophlebitis, syncope and very rare cases of gangrene have been reported following venography.
Usual Dosage
The usual dose for adults is 30 to 125 mL per lower extremity. The dose for children is reduced in proportion to body weight. Following the procedure, the venous system should be flushed with either 5% dextrose in water (D5W) or normal saline (Sodium Chloride Injection USP) or the contrast medium should be removed by leg massage and/or leg elevation.
-
INTRAVENOUS INFUSION UROGRAPHY
Intravenous infusion urography enhances the potential for more diagnostic information in those patients in whom the usual excretory urographic technique either has not provided or is not expected to provide satisfactory visualization. The entire urinary tract, including nephrogram and cystogram, may be visualized in the unobstructed patient with normal renal function.
Patient Preparation
Appropriate preparation of the patient is important for optimal visualization. A low residue diet is recommended for the day preceding the examination and a laxative is given the evening before the examination, unless contraindicated.
Dehydration is not indicated for the performance of infusion urography. Patients should be maintained in an optimal state of hydration prior to the procedure.
Usual Dosage
The usual dosage in adults and children is 3 mL/kg (1.5 mL/lb) by intravenous administration, not to exceed a total dose of 200 mL.
The solution is infused through an appropriate I.V. needle at a rate of approximately 40 to 50 mL per minute. Any appropriate intravenous administration set may be used observing the usual precautions for maintaining sterility and safety in administration. Films are usually taken at 5 minute intervals following the initiation of the infusion for a total of 20 minutes.
In patients with impaired renal function, diagnostic opacification frequently is achieved only after prolonged periods. In these individuals, periodic films obtained up to 24 hours after infusion might yield useful information.
-
CONTRAST ENHANCEMENT OF COMPUTED TOMOGRAPHIC (CT) HEAD IMAGING
Tumors
Conray 43 may be useful to enhance the demonstration of the presence and extent of certain malignancies such as: gliomas including malignant gliomas, glioblastomas, astrocytomas, oligodendrogliomas and gangliomas; ependymomas; medulloblastomas; meningiomas; neuromas; pinealomas; pituitary adenomas; craniopharyngiomas; germinomas; and metastatic lesions.
The usefulness of contrast enhancement for the investigation of the retrobulbar space and in cases of low grade or infiltrative glioma has not been demonstrated.
In cases where lesions have calcified, there is less likelihood of enhancement. Following therapy, tumors may show decreased or no enhancement.
Non-Neoplastic Conditions
The use of Conray 43 may be beneficial in the image enhancement of non-neoplastic lesions. Cerebral infarctions of recent onset may be better visualized with the contrast enhancement, while some infarctions are obscured if contrast media are used. The use of iodinated contrast media results in contrast enhancement in about 60% of cerebral infarctions studied from one to four weeks from the onset of symptoms.
Sites of active infection may also be enhanced following contrast medium administration.
Arteriovenous malformations and aneurysms will show contrast enhancement. In the case of these vascular lesions, the enhancement is probably dependent on the iodine content of the circulating blood pool.
The opacification of the inferior vermis following contrast medium administration has resulted in false positive diagnoses in a number of normal studies.
Patient Preparation
No special patient preparation is required for contrast enhancement of CT head scanning. However, it is advisable to ensure that patients are well hydrated prior to examination.
Usual Dosage
The usual dose in adults and children is 3 mL/kg (1.5 mL/lb) by intravenous administration, not to exceed a total dose of 200 mL. In most cases, scanning may be performed immediately after completion of administration; however, when fast scanning equipment (less than 1 minute) is used, consideration should be given to waiting approximately 5 minutes to allow for maximum contrast enhancement.
-
CONTRAST ENHANCEMENT IN BODY COMPUTED TOMOGRAPHY
Patient Preparation
No special patient preparation is required. However, it is advisable to ensure that patients are well hydrated. In patients undergoing abdominal or pelvic examination, opacification of the bowel may be valuable in scan interpretation.
Precautions
In addition to the general precautions previously described, patient cooperation is essential since patient motion, including respiration, can markedly affect image quality. The use of an intravascular contrast medium can obscure tumors in patients undergoing CT evaluation of the liver resulting in a false negative diagnosis. Dynamic CT scanning is the procedure of choice for malignant tumor enhancement (see CLINICAL PHARMACOLOGY).
Usual Dosage
The usual adult dose is 200 to 250 mL administered by bolus injection, by rapid infusion or by a combination of both.
In adults, when the combination bolus and infusion technique is used, a 50 to 100 mL bolus injection followed by a rapid infusion of 100 to 150 mL may be used. In children, the dose is reduced in proportion to the body weight.
-
ARTERIAL DIGITAL SUBTRACTION ANGIOGRAPHY
Arterial digital subtraction angiography provides images similar in quality to conventional film-screen systems. The advantages of arterial DSA when compared to standard film angiography include the use of less contrast medium; the use of a lower concentration of contrast medium as provided by Conray 43; a decreased need for selective arterial catheterization and a shortened examination time. The limitations of arterial DSA include: reduced spatial resolution and limited field size.
Patient Preparation
No special patient preparation is required for arterial DSA. However, it is advisable to ensure that patients are well hydrated prior to examination.
Precautions
In addition to the general precautions described, the risks associated with arterial DSA are those usually attendant with catheter procedures. Following the procedure, gentle pressure hemostasis is required, followed by observation and immobilization of the limb for several hours to prevent hemorrhage from the site of arterial puncture.
Usual Dosage
It is advisable to inject at rates approximately equal to the flow rate of the vessel being injected. The following volumes per injection, have been used, and may be repeated as necessary:
Carotid or Vertebral Arteries 3-10 mL
Aortic Arch 15-30 mL
Subclavian and Brachial Arteries 5-15 mL
Major branches of the Aorta 5-30 mL
Abdominal Aorta 10-30 mLA total dose of 200 mL (representing 40.4 grams of iodine) should not be exceeded. Consideration should be given to the patient's clinical condition and whether large volumes of fluids may be detrimental to patient care.
Retrograde Urographic Administration
Patient Preparation
Unless contraindicated, an appropriate laxative is given the night before the examination.
Radiographic Technique
The radiographic procedure normally employed for cystography, cystourethrography and retrograde pyelography should be employed. A preliminary radiograph is recommended before the contrast agent is administered.
Administration
Sterile catherization is essential. Conray 43 may be introduced by gravity flow using an appropriate venoclysis set or by syringe. Excessive pressure should be avoided with any method of administration.
Usual Dosage
Retrograde Pyelography – Ordinarily about 25 mL of Conray 43 are required for bilateral and 15 mL for unilateral pyelograms. About 5 to 6 mL are usually administered for each exposure. Children usually require a volume reduced in proportion to their body size.
Cystography and Cystourethrography – Either Conray 43 supplied at 43% w/v concentration of iothalamate meglumine or Cysto-Conray II supplied at a 17.2% w/v concentration of iothalamate meglumine may be used for these procedures. (SEE CYSTO-CONRAY II PACKAGE INSERT FOR SPECIFIC INFORMATION ABOUT THE USE OF THIS PRODUCT.) The desired concentration will vary depending upon the patient's size and age and also with the technique and equipment used. Sufficient volume of contrast medium is administered to adequately fill the urinary bladder. The volume of solution required will vary depending upon the individual patient. Adults usually require a volume in the range of 200 to 400 mL. Children require a volume in proportion to their body size. The usual dose ranges from 30 to 300 mL.
-
HOW SUPPLIED
Conray® 43 Glass Vials/Bottles NDC Number 25x50 mL vials 0019-3183-05 12x250 mL bottles 0019-3183-50 Storage
Store below 30°C (86°F). Exposing this product to very cold temperatures may result in crystallization of the salt. If this occurs the container should be brought to room temperature. Shake vigorously to assure complete dissolution of any crystals. The speed of dissolution may be increased by heating with circulating warm air. Before use, examine the product to assure that all solids are redissolved and that the container and closure have not been damaged. This preparation is sensitive to light and must be protected from strong daylight or direct exposure to the sun.
As with all contrast media, the containers should be inspected prior to use to ensure that breakage or other damage has not occurred during shipping and handling. All containers should be inspected for closure integrity. Damaged containers should not be used.
- SPL UNCLASSIFIED SECTION
-
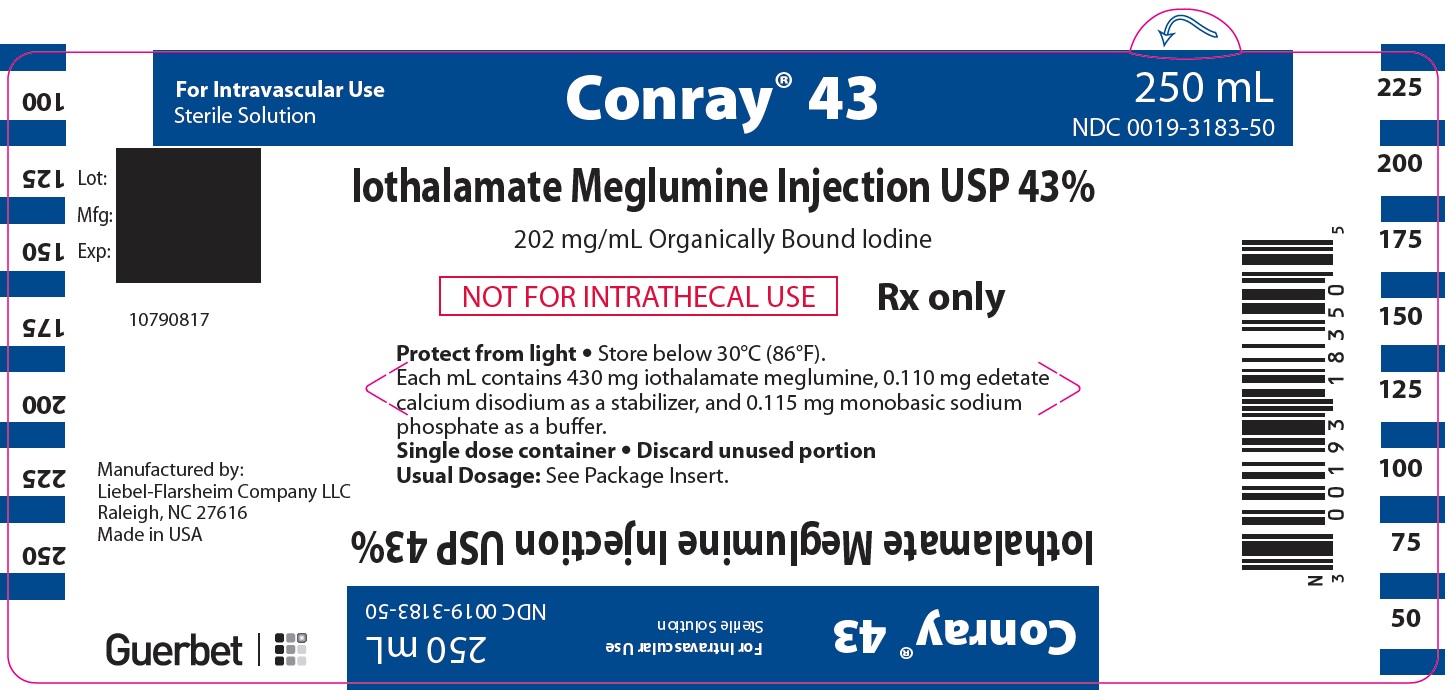
Package Label Principal Display Panel - 250mL Bottle
For Intravascular Use
Sterile SolutionConray® 43
250 mL
NDC: 0019-3183-50
Iothalamate Meglumine Injection USP 43%202 mg/mL Organically Bound Iodine
NOT FOR INTRATHECAL USE
Rx OnlyProtect from light Store below 30°C (86°F).
Each mL contains 430 mg iothalamate meglumine, 0.110 mg edetate calcium disodium as a stabilizer, and 0.115 mg monobasic sodium phosphate as a buffer.
Single dose container Discard unused portion
Usual Dosage: See Package Insert.10790817
Manufactured by:
Liebel-Flarsheim Company LLC
Raleigh, NC 27616
Made in USAGuerbet
-
INGREDIENTS AND APPEARANCE
CONRAY 43
iothalamate meglumine injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0019-3183 Route of Administration INTRAVASCULAR Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength IOTHALAMATE MEGLUMINE (UNII: XUW72GOP7W) (IOTHALAMIC ACID - UNII:16CHD79MIX) IOTHALAMATE MEGLUMINE 430 mg in 1 mL Inactive Ingredients Ingredient Name Strength EDETATE CALCIUM DISODIUM (UNII: 25IH6R4SGF) SODIUM PHOSPHATE, MONOBASIC, UNSPECIFIED FORM (UNII: 3980JIH2SW) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0019-3183-09 12 in 1 BOX 10/11/2010 1 250 mL in 1 BOTTLE, GLASS; Type 0: Not a Combination Product 2 NDC: 0019-3183-50 12 in 1 BOX 10/11/2010 06/28/2019 2 250 mL in 1 BOTTLE, GLASS; Type 0: Not a Combination Product 3 NDC: 0019-3183-15 50 in 1 BOX 10/11/2010 3 50 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product 4 NDC: 0019-3183-05 25 in 1 BOX 10/11/2010 06/28/2019 4 50 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA013295 10/11/2010 Labeler - Liebel-Flarsheim Company LLC (057880002) Establishment Name Address ID/FEI Business Operations LIEBEL-FLARSHEIM COMPANY LLC 109024984 ANALYSIS(0019-3183) , MANUFACTURE(0019-3183) Establishment Name Address ID/FEI Business Operations Justesa Imagen, S.A.U. 477020325 API MANUFACTURE(0019-3183)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.