CPDA-1- anticoagulant citrate phosphate dextrose adenine solution
CPDA-1 by
Drug Labeling and Warnings
CPDA-1 by is a Prescription medication manufactured, distributed, or labeled by Fenwal, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
BLOOD-PACK™ Unit with an Integral SEPACELL™ RS-2000/RZ-2000 Whole Blood Leukocyte Reduction Filter for Collection and Filtration of Whole Blood Using Either CPD/ADSOL™ Red Cell Preservation Solution or Anticoagulant Citrate Phosphate Dextrose Adenine Solution, USP CPDA-1
Rx only
Contains FENWAL EXPRESS™ System. Also Contains Sample Diversion System for the collection of whole blood samples for laboratory testing and the DONORCARE™ Needle Guard.
Integral filter unit intended for leukocyte reduction of Whole Blood up to 8 hours after blood collection when Whole Blood is stored at ambient temperatures or up to 72 hours after blood collection when Whole Blood is refrigerated. The leukocyte reduced blood products may then be stored for the maximum allowable dating period.
Instructions for Use
Collection Procedure:
Use aseptic technique.
Notes:
- If Sample Diversion System is not used, donor samples may be collected using an alternate method following standard procedures.
- Nominal tubing dimensions of product are 0.118" inner diameter x 0.025" wall thickness.
Precautions:
- Upon removal of BLOOD-PACK unit from the clear plastic overwrap, visually inspect the unit.
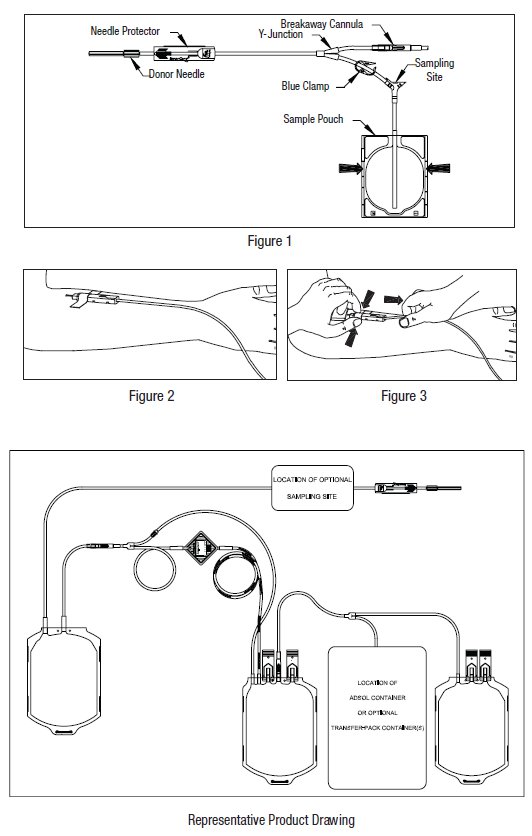
- Do not use the product if the breakaway cannula is broken and/or anticoagulant is present in the sample pouch or in the tubing from the breakaway cannula to the sample pouch and donor needle (see Figure 1). Note that condensation in the empty tubing of the BLOOD-PACK unit is expected as a result of the sterilization process.
- Do not use unless the solutions are clear.
- 1. Identify BLOOD-PACK unit using appropriate donor identification system.
- 2. Donor scale
- Adjust donor scale to desired collection weight.
- Position primary container on the donor scale as far as possible below donor arm.
- 3. Clamp donor tubing between the needle and Y-junction with hemostat. (This step can be performed prior to step 1 or 2.)
- 4. Visually inspect the tubing from the breakaway cannula to the sample pouch and donor needle, as well as the sample pouch to reconfirm that there is no anticoagulant present.
Note: Ensure that the sample pouch remains below the donor’s arm.- 5. Following blood center procedures, apply pressure to donor’s arm and disinfect site of venipuncture.
- 6. Remove needle cover per instructions below:
- Holding the hub and cover near the tamper-evident seal, twist cover 1/4 turn to break seal.
- Remove needle cover, being careful not to drag the cover across the needle point.
- 7. Following blood center procedures, perform venipuncture, appropriately secure donor needle and/or tubing and release hemostat.
- 8. When good blood flow is established, slide the DONORCARE needle guard over the needle hub into the engaged position. Leave the front third of the needle hub exposed for access. Stabilize the front of the needle guard to arm with tape. (see Figure 2)
Note: In difficult collection conditions (e.g., slow blood flow), leave the needle guard disengaged behind the hub during collection. Engage the needle guard at the end of blood collection. Appropriately secure needle and/or tubing.- 9. Allow the sample pouch to fill with blood according to center procedure. Monitor blood flow into sample pouch.
Notes:
- The sample pouch contains an average fill volume of approximately 53 mL with a maximum fill volume of approximately 60 mL when filled to capacity.
- If less blood sample volume is required, the flow to the sample pouch may be stopped prior to completely filling the pouch. For example, in order to target a fill volume of approximately 40 mL, fill to the level indicated by the arrows in Figure 1. Ensure the pouch is hanging vertically.
- The tube leading from the Y-junction to the sample pouch contains an additional volume of approximately 2 mL.
Precautions:
- Do not elevate or squeeze the sample pouch as this could cause blood to backflow from the sample pouch into the collection system.
- Once the sample pouch is filled to desired volume, complete steps 10 - 18 within approximately 4 minutes to avoid possible clot formation in the tubing and/or sample pouch.
- 10. Close the blue clamp on tubing between the Y-junction and the sample pouch.
- 11. Break the breakaway cannula below the Y-junction in the donor tubing to the primary container allowing blood collection to proceed. To completely break the breakaway cannula, grasp with both hands. Snap it at a 90° angle in one direction, and then bend it at a 90° angle in the opposite direction. Ensure the breakaway cannula is completely broken and that the blood flows freely to the primary container.
Precaution: Failure to break the breakaway cannula completely may result in restricted blood flow.
- 12. Following blood center procedures, mix blood and anticoagulant in the primary container immediately and at several intervals during collection, and immediately after collection.
- 13. Following blood center procedures, hermetically seal the tubing between the sampling site and the Y-junction to maintain sterility of the blood collection system prior to removing blood samples.
Warning:
- Do not proceed with the remaining steps until the tubing leading to the sample pouch is hermetically sealed between the sampling site and the Y-junction. To maintain the whole blood collection container as a closed system, the tubing between the sample pouch and Y-junction must be hermetically sealed prior to inserting the access device into the sampling site. Failure to do so may lead to contamination of the whole blood collection.
- 14. Insert the access device by pushing firmly into the sampling site until the membrane seal is penetrated.
Note: If the access device is assembled such that the outer barrel is screwed onto the Luer, make sure to rotate clockwise upon insertion to avoid barrel detaching from Luer.
- 15. Open the cap on the access device (if applicable). Hold access device so that the sample pouch hangs down.
- 16. Directly align the vacuum sample tube with the internal needle in the access device. Insert vacuum sample tube into device until the stopper is punctured.
- 17. Allow vacuum sample tube to fill with blood then remove from the access device.
- 18. Repeat steps 16 and 17 until the desired number of vacuum sample tubes have been filled.
Notes:
- If the access device needs to be replaced, use a hemostat to clamp the tubing between the sampling site and the sample pouch. Then, grasp base of sampling site with one hand and pull the access device out with the other hand. Firmly insert the new access device as before. Remove hemostat and continue sampling.
- If the access device is assembled such that the outer barrel is screwed onto the Luer, make sure to rotate clockwise upon removal to avoid barrel detaching from Luer.
- The access device can only be replaced one time.
Precaution: When replacing access device, be careful to avoid contact with any blood droplets on the Luer or sampling site. Discard used access device appropriately.
- 19. Collect the appropriate volume based on BLOOD-PACK unit used.
Note: The volume of anticoagulant is sufficient for the blood collection indicated on BLOOD-PACK unit ± 10%.Precaution: Once the desired blood volume is collected, complete steps 20-24 within approximately 4 minutes to avoid possible clot formation in the tubing.
- 20. Release pressure on the donor’s arm. If appropriate, apply hemostat to donor tubing between the needle and the Y-junction.
- 21. Hermetically seal donor tubing between the in-line cannula and the primary container.
- 22. Withdrawal of Needle (see Figure 3)
Precaution: The needle guard must be held stationary while the needle is withdrawn into it.
- a) Place folded sterile gauze over puncture site and hold in place with finger tip without exerting pressure.
- b) Hold sides of needle guard near the front, between the index finger and thumb. Pull the tubing smoothly until the needle is locked into the needle guard.
- c) Confirm the needle lock by:
- Listen for the 2nd “click” as the needle is drawn into the needle guard.
- Ensure the tubing cannot be pulled through the needle guard.
- 23. Remove and discard the Sample Diversion System and needle guard into an appropriate biohazardous waste container following established procedures. If the donor tubing is also to be discarded, hermetically seal donor tubing directly above the primary container and remove.
Note: Step 24 may be performed prior to step 23 if desired.
- 24. If the donor tubing is not sealed directly above the primary container, then strip the blood from the remaining donor tubing into the primary container. Mix and allow tubing to refill; repeat once.
Filtration Procedure:
Precaution: Whole blood collected from certain donors may have extended filtration times and the potential for ineffective filtration and leukoreduction.
Note: The time of Whole Blood filtration may vary depending on processing option selected.
- a) Within 8 hours of collection if Whole Blood is held at ambient temperature.
- b) Within 72 hours of collection if Whole Blood is refrigerated following collection.
- 25. Mix unfiltered Whole Blood thoroughly. Invert the primary container and hang the filter set such that the filter remains vertical. To achieve maximum flow rate, allow set to hang to full length.
Note: The filtered Whole Blood container must remain below the level of the filter during filtration. For proper air expression to occur, ensure the filtered Whole Blood container is vertical.
- 26. Inspect all tubing to insure it hangs freely without kinks. Install and close clamp on bypass line.
- 27. Break the in-line cannula above the filter to start filtration. To completely break the in-line cannula, grasp with both hands. Snap it at a 90° angle in one direction, and then bend it at a 90° angle in the opposite direction. Allow filtration to continue until flow stops.
Note: Manual or mechanical pressure should not be used to increase the flow rate through the filter.
Note: Tubing below the filter should not be stripped at any time during the filtration process.
Note: If the filtration of Whole Blood is initiated at ambient temperature and not completed within 8 hours after blood collection, then filtration should be completed between 1 and 6°C.
Note: If recovery of residual blood in the primary container is desired, install and close a clamp on the segment line prior to removing the clamp on the bypass line. The segment line clamp can then be removed after step 28.
- 28. Open the clamp on the bypass line and allow air to transfer from the filtered Whole Blood container to the primary container.
Note: If desired, gently squeeze the filtered Whole Blood container to transfer remaining air through the bypass line.
- 29. Allow filtration to continue until the inlet side of the filter is filled with air.
- 30. Hermetically seal and separate the bypass line above the filtered Whole Blood container. Also hermetically seal and separate the segment line tubing directly above the top donor segment number. Use care to avoid fluid splatter. Discard filter and primary container appropriately.
Note: If a QC sample is desired, thoroughly mix the filtered Whole Blood and strip the donor segment tubing or bypass line tubing as desired. Use the tubing farthest away from the filtered Whole Blood container as the QC sample.
- 31. Make donor segments. Leave segments attached to the filtered Whole Blood container.
Component Preparation Procedure:
Note: Platelet concentrates are not intended to be made with this product.
- 32. Centrifuge filtered Whole Blood and secondary containers to prepare CPD/CPDA-1 Red Blood Cells using the appropriate spin condition.
Note: It is recommended that the filtered Whole Blood container and secondary container(s) be loaded into the centrifuge cups with a snug fit and that contact with rigid components is avoided.
- 33. Place filtered Whole Blood container in plasma extractor, and express plasma into empty TRANSFER-PACK™ container by releasing pressure plate and opening closure in tubing of filtered Whole Blood container.
- 34. When the desired amount of plasma has been removed, clamp the tubing between Y and plasma container. Hermetically seal and separate transfer tubing being careful to avoid fluid splatter.
Note: If applicable, ADSOL Red Cell Preservation Solution should be added to the Red Blood Cells immediately after the removal of plasma. Preparation of AS-1 Red Blood Cells may vary depending on processing option selected:
- a) Within 8 hours of blood collection if whole blood is held at ambient temperature.
- b) Within 3 days of blood collection if whole blood is refrigerated.
- 35. If applicable, suspend ADSOL Red Cell Preservation Solution container; open closure in tubing and drain contents onto CPD Red Blood Cells. Clamp tubing.
- 36. Hermetically seal and separate transfer tubing near the container of filtered Red Blood Cells. Be careful to avoid fluid splatter. For double BLOOD-PACK unit ADSOL products, discard ADSOL Solution Container. For all other ADSOL products, the empty solution container may now be used as a TRANSFER-PACK container for further component preparation.
- 37. For further processing of plasma product with multiple BLOOD-PACK units, use standard component processing and storage techniques.
Note: Fresh Frozen Plasma should be separated from the red blood cells and placed in the freezer at -18°C or colder within 8 hours after blood collection.
- 38. If set contains ADSOL Red Cell Preservative Solution, mix the ADSOL Red Cell Preservation Solution and Red Blood Cells thoroughly, producing AS-1 Red Blood Cells, Leukocytes Reduced.
- 39. Store suspended AS-1 Red Blood Cells, Leukocytes Reduced, or suspended CPDA-1 Whole Blood/Red Blood Cells, Leukocytes Reduced (as applicable), between 1 and 6°C.
- 40. Infuse AS-1 Red Blood Cells, Leukocytes Reduced, within 42 days of collection and CPDA-1 Whole Blood/Red Blood Cells, Leukocytes Reduced, within 35 days of collection.
Warning: Failure to achieve closed system processing conditions negates the extended storage claim and the red blood cell product must be transfused within 24 hours.
Store at Controlled Room Temperature.
USP Definition of “Controlled Room Temperature”
United States Pharmacopeia, General Notices.
United States Pharmacopeial Convention, Inc.
12601 Twinbrook Parkway, Rockville, MD.FENWAL, FENWAL EXPRESS, BLOOD-PACK, TRANSFER-PACK and ADSOL are trademarks of Fenwal, Inc.
SEPACELL is a trademark of Asahi Kasei Medical Co., Ltd.
DONORCARE is a trademark of ITL Corporation. Fenwal, Inc.
Fenwal, Inc.
Lake Zurich, IL 60047 USAMade in USA
07-19-06-120 REV: A
07/2011 -
PACKAGE/LABEL DISPLAY PANEL
Code 4R3327E
12 Units
Fenwal™
Anticoagulant Citrate Phosphate Dextrose Adenine Solution, USP (CPDA-1) BLOOD-PACK™ Unit; Integral SEPACELL™ RS-2000 Whole Blood Leukocyte Reduction Filter
Double For the Collection of 500 mL Blood
FENWAL EXPRESS™ System, Sample Diversion System, DONORCARE™ Needle Guard, 16 ga. Ultra Thin Wall Needle
Rx only
Each unit consists of a PL 146 Plastic primary container with 70 mL of CPDA-1 solution containing 2.23 g Dextrose (monohydrate) USP, 1.84 g Sodium Citrate (dihydrate) USP, 209 mg Citric Acid (anhydrous) USP, 155 mg Monobasic Sodium Phosphate (monohydrate) USP and 19.3 mg Adenine USP, pH may have been adjusted with sodium hydroxide; an integral RS-2000 filter with one empty 450 mL PL 146 Plastic container for red cell storage and one empty 400 mL PL 146 Plastic TRANSFER-PACK™ container.
Sterile, non-pyrogenic fluid path
See direction insert.Store at Controlled Room Temperature (refer to direction insert).
- Open pouch by tearing across at notch.
- Direct handling of product surfaces prior to extended storage in the foil pouch, may result in mold growth.
- Unused units in open foil pouch may be kept up to 60 days by folding and securing open end of foil pouch to prevent possible loss of moisture, provided:
- I) Units are not removed from foil pouch, or
- II) Unused units removed from foil pouch are returned to the foil pouch within 12 hours. Units may be removed from the pouch and returned only once.
- Units removed from the foil pouch (that are not returned to the pouch within 12 hours) must be used within 4 days (96 hours). Units out of the foil pouch for longer than 96 hours must be discarded.
FENWAL, FENWAL EXPRESS, BLOOD-PACK, ADSOL and TRANSFER-PACK are trademarks of Fenwal, Inc.
SEPACELL is a trademark of Asahi Kasei Medical Co., Ltd.
DONORCARE is a trademark of ITL Corporation.
 Fenwal, Inc.
Fenwal, Inc.
Lake Zurich, IL 60047 USAMade in USA
07-28-05-680 REV: A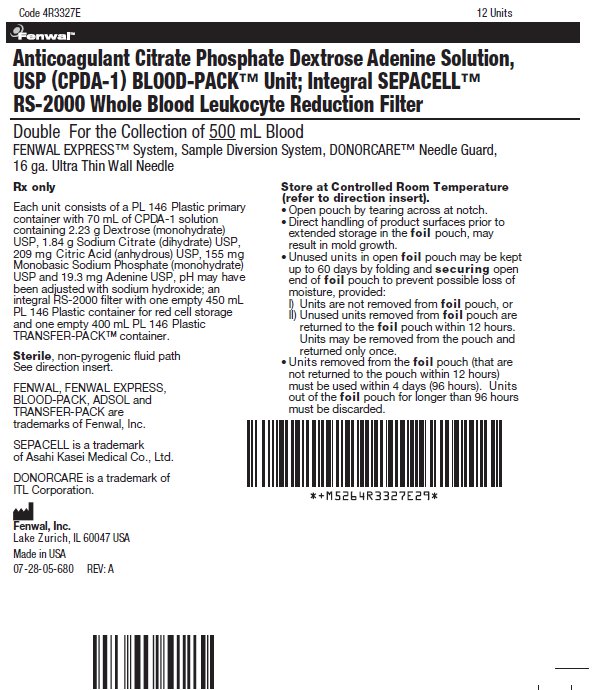
-
INGREDIENTS AND APPEARANCE
CPDA-1
anticoagulant citrate phosphate dextrose adenine solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0942-6308 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Dextrose Monohydrate (UNII: LX22YL083G) (ANHYDROUS DEXTROSE - UNII:5SL0G7R0OK) Dextrose Monohydrate 2.23 g in 70 mL Trisodium Citrate Dihydrate (UNII: B22547B95K) (Anhydrous Citric Acid - UNII:XF417D3PSL) Anhydrous Citric Acid 1.84 g in 70 mL Anhydrous Citric Acid (UNII: XF417D3PSL) (Anhydrous Citric Acid - UNII:XF417D3PSL) Anhydrous Citric Acid 209 mg in 70 mL Sodium Phosphate, Monobasic, Monohydrate (UNII: 593YOG76RN) (PHOSPHATE ION - UNII:NK08V8K8HR) Sodium Phosphate, Monobasic, Monohydrate 155 mg in 70 mL Adenine (UNII: JAC85A2161) (Adenine - UNII:JAC85A2161) Adenine 19.3 mg in 70 mL Inactive Ingredients Ingredient Name Strength Sodium Hydroxide (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0942-6308-02 70 mL in 1 BAG; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA BN770420 03/01/2007 Labeler - Fenwal, Inc. (794519020)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.