PRAVASTATIN SODIUM tablet
Pravastatin Sodium by
Drug Labeling and Warnings
Pravastatin Sodium by is a Prescription medication manufactured, distributed, or labeled by International Laboratories, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PRAVASTATIN SODIUM TABLETS safely and effectively. See full prescribing information for PRAVASTATIN SODIUM TABLETS.
PRAVASTATIN SODIUM tablets, for oral use
Initial U.S. Approval: 1991RECENT MAJOR CHANGES
INDICATIONS AND USAGE
Pravastatin sodium tablets are an HMG-CoA reductase inhibitor (statin) indicated as an adjunctive therapy to diet to:
-
Reduce the risk of MI, revascularization, and cardiovascular mortality in hypercholesterolemic patients without clinically evident CHD. (1.1)
-
Reduce the risk of total mortality by reducing coronary death, MI, revascularization, stroke/TIA, and the progression of coronary atherosclerosis in patients with clinically evident CHD. (1.1)
-
Reduce elevated Total-C, LDL-C, ApoB, and TG levels and to increase HDL-C in patients with primary hypercholesterolemia and mixed dyslipidemia. (1.2)
-
Reduce elevated serum TG levels in patients with hypertriglyceridemia. (1.2)
-
Treat patients with primary dysbetalipoproteinemia who are not responding to diet. (1.2)
-
Treat children and adolescent patients ages 8 years and older with heterozygous familial hypercholesterolemia after failing an adequate trial of diet therapy. (1.2)
Limitations of use:
-
Pravastatin sodium tablets have not been studied in Fredrickson Types I and V dyslipidemias. (1.3)
DOSAGE AND ADMINISTRATION
- Adults: the recommended starting dose is 40 mg once daily. Use 80 mg dose only for patients not reaching LDL-C goal with 40 mg. (2.2)
- Significant renal impairment: the recommended starting dose is pravastatin10 mg once daily. (2.3)
- Children (ages 8 to 13 years, inclusive): the recommended starting dose is 20 mg once daily. (2.4)
- Adolescents (ages 14 to 18 years): the recommended starting dose is 40 mg once daily. (2.4)
DOSAGE FORMS AND STRENGTHS
-
Tablets: 10 mg, 20 mg, 40 mg, and 80 mg. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Skeletal muscle effects (e.g., myopathy and rhabdomyolysis): predisposing factors include advanced age (> 65), uncontrolled hypothyroidism, and renal impairment. Patients should be advised to promptly report to their physician any unexplained and/or persistent muscle pain, tenderness, or weakness. Pravastatin therapy should be discontinued if myopathy is diagnosed or suspected. (5.1, 8.5)
- Liver enzyme abnormalities: persistent elevations in hepatic transaminases can occur. Check liver enzyme tests before initiating therapy and as clinically indicated thereafter. (5.2)
ADVERSE REACTIONS
In short-term clinical trials, the most commonly reported adverse reactions (≥ 2% and > placebo) regardless of causality were: musculoskeletal pain, nausea/vomiting, upper respiratory infection, diarrhea, and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-866-832-8537; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Concomitant lipid-lowering therapies: use with fibrates or lipid-modifying doses (≥ 1 g/day) of niacin increases the risk of adverse skeletal muscle effects. Caution should be used when prescribing with pravastatin sodium. (7)
- Cyclosporine: combination increases exposure. Limit pravastatin to 20 mg once daily. (2.6, 7.1)
- Clarithromycin: combination increases exposure. Limit pravastatin to 40 mg once daily. (2.7, 7.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2017
-
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Prevention of Cardiovascular Disease
1.2 Hyperlipidemia
1.3 Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Information
2.2 Adult Patients
2.3 Patients with Renal Impairment
2.4 Pediatric Patients
2.5 Concomitant Lipid-Altering Therapy
2.6 Dosage in Patients Taking Cyclosporine
2.7 Dosage in Patients Taking Clarithromycin
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Liver
4.3 Pregnancy
4.4 Lactation
5 WARNINGS AND PRECAUTIONS
5.1 Skeletal Muscle
5.2 Liver
5.3 Endocrine Function
6 ADVERSE REACTIONS
6.1 Adverse Clinical Events
6.2 Postmarketing Experience
6.3 Laboratory Test Abnormalities
6.4 Pediatric Patients
7 DRUG INTERACTIONS
7.1 Cyclosporine
7.2 Clarithromycin and Other Macrolide Antibiotics
7.3 Colchicine
7.4 Gemfibrozil
7.5 Other Fibrates
7.6 Niacin
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Homozygous Familial Hypercholesterolemia
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Prevention of Coronary Heart Disease
14.2 Secondary Prevention of Cardiovascular Events
14.3 Primary Hypercholesterolemia (Fredrickson Types IIa and IIb)
14.4 Hypertriglyceridemia (Fredrickson Type IV)
14.5 Dysbetalipoproteinemia (Fredrickson Type III)
14.6 Pediatric Clinical Study
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in individuals at significantly increased risk for atherosclerotic vascular disease due to hypercholesterolemia. Drug therapy is indicated as an adjunct to diet when the response to a diet restricted in saturated fat and cholesterol and other nonpharmacologic measures alone has been inadequate.
1.1 Prevention of Cardiovascular Disease
In hypercholesterolemic patients without clinically evident coronary heart disease (CHD), pravastatin sodium tablets are indicated to:
- reduce the risk of myocardial infarction (MI).
- reduce the risk of undergoing myocardial revascularization procedures.
- reduce the risk of cardiovascular mortality with no increase in death from non-cardiovascular causes.
In patients with clinically evident CHD, pravastatin sodium tablets are indicated to:
- reduce the risk of total mortality by reducing coronary death.
- reduce the risk of MI.
- reduce the risk of undergoing myocardial revascularization procedures.
- reduce the risk of stroke and stroke/transient ischemic attack (TIA).
- slow the progression of coronary atherosclerosis.
1.2 Hyperlipidemia
Pravastatin sodium tablets are indicated:
as an adjunct to diet to reduce elevated total cholesterol (Total-C), low-density lipoprotein cholesterol (LDL-C), apolipoprotein B (ApoB), and triglyceride (TG) levels and to increase high-density lipoprotein cholesterol (HDL-C) in patients with primary hypercholesterolemia and mixed dyslipidemia ( Fredrickson Types IIa and IIb). 1
as an adjunct to diet for the treatment of patients with elevated serum TG levels ( Fredrickson Type IV).
for the treatment of patients with primary dysbetalipoproteinemia ( Fredrickson Type III) who do not respond adequately to diet.
as an adjunct to diet and lifestyle modification for treatment of heterozygous familial hypercholesterolemia (HeFH) in children and adolescent patients ages 8 years and older if after an adequate trial of diet the following findings are present:
a. LDL-C remains ≥ 190 mg/dL or
b. LDL-C remains ≥ 160 mg/dL and
there is a positive family history of premature cardiovascular disease (CVD) or
two or more other CVD risk factors are present in the patient. -
2 DOSAGE AND ADMINISTRATION
2.1 General Dosing Information
The patient should be placed on a standard cholesterol-lowering diet before receiving pravastatin sodium tablets and should continue on this diet during treatment with pravastatin sodium tablets [see NCEP Treatment Guidelines for details on dietary therapy].
2.2 Adult Patients
The recommended starting dose is 40 mg once daily. If a daily dose of 40 mg does not achieve desired cholesterol levels, 80 mg once daily is recommended. Pravastatin sodium tablets can be administered orally as a single dose at any time of the day, with or without food. Since the maximal effect of a given dose is seen within 4 weeks, periodic lipid determinations should be performed at this time and dosage adjusted according to the patient’s response to therapy and established treatment guidelines.
2.3 Patients with Renal Impairment
In patients with severe renal impairment, a starting dose of 10 mg pravastatin daily is recommended.
2.4 Pediatric Patients
Children (Ages 8 to 13 Years, Inclusive)
The recommended dose is 20 mg once daily in children 8 to 13 years of age. Doses greater than 20 mg have not been studied in this patient population.
Adolescents (Ages 14 to 18 Years)
The recommended starting dose is 40 mg once daily in adolescents 14 to 18 years of age. Doses greater than 40 mg have not been studied in this patient population.
Children and adolescents treated with pravastatin should be reevaluated in adulthood and appropriate changes made to their cholesterol-lowering regimen to achieve adult goals for LDL-C [see Indications and Usage (1.2)].
2.5 Concomitant Lipid-Altering Therapy
Pravastatin sodium tablets may be used with bile acid resins. When administering a bile-acid-binding resin (e.g., cholestyramine, colestipol) and pravastatin, pravastatin sodium tablets should be given either 1 hour or more before or at least 4 hours following the resin [see Clinical Pharmacology (12.3)].
2.6 Dosage in Patients Taking Cyclosporine
In patients taking immunosuppressive drugs such as cyclosporine concomitantly with pravastatin, therapy should begin with 10 mg of pravastatin sodium once-a-day at bedtime and titration to higher doses should be done with caution. Most patients treated with this combination received a maximum pravastatin sodium dose of 20 mg/day. In patients taking cyclosporine, therapy should be limited to 20 mg of pravastatin sodium once daily [see Warnings and Precautions (5.1) and Drug Interactions (7.1)].
2.7 Dosage in Patients Taking Clarithromycin
In patients taking clarithromycin, therapy should be limited to 40 mg of pravastatin sodium once daily [see Drug Interactions (7.2)].
-
3 DOSAGE FORMS AND STRENGTHS
Pravastatin sodium tablets USP are supplied as:
10 mg tablets: Pink, unscored, round tablet, debossed “TEVA” on one side and “771” on the other side.
20 mg tablets: Light-yellow, unscored, round tablet, debossed “TEVA” on one side and “7201” on the other side.
40 mg tablets: Light-green, unscored, round tablet, debossed “TEVA” on one side and “7202” on the other side.
80 mg tablets : Off-white to mottled grey, unscored, oval-shaped tablet, debossed “TEVA” on one side and “7270” on the other side.
-
4 CONTRAINDICATIONS
4.2 Liver
Active liver disease or unexplained, persistent elevations of serum transaminases [see Warnings and Precautions (5.2)].
4.3 Pregnancy
Atherosclerosis is a chronic process and discontinuation of lipid-lowering drugs during pregnancy should have little impact on the outcome of long-term therapy of primary hypercholesterolemia. Cholesterol and other products of cholesterol biosynthesis are essential components for fetal development (including synthesis of steroids and cell membranes). Since statins decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol, they are contraindicated during pregnancy and in nursing mothers. PRAVASTATIN SHOULD BE ADMINISTERED TO WOMEN OF CHILDBEARING AGE ONLY WHEN SUCH PATIENTS ARE HIGHLY UNLIKELY TO CONCEIVE AND HAVE BEEN INFORMED OF THE POTENTIAL HAZARDS. If the patient becomes pregnant while taking this class of drug, therapy should be discontinued immediately and the patient apprised of the potential hazard to the fetus [see Use in Specific Populations (8.1), (8.3)].
4.4 Lactation
Pravastatin is present in human milk. Because statins have the potential for serious adverse reactions in nursing infants, women who require pravastatin sodium tablet treatment should not breastfeed their infants [see Use in Specific Populations (8.2)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Skeletal Muscle
Rare cases of rhabdomyolysis with acute renal failure secondary to myoglobinuria have been reported with pravastatin and other drugs in this class. A history of renal impairment may be a risk factor for the development of rhabdomyolysis. Such patients merit closer monitoring for skeletal muscle effects.
Uncomplicated myalgia has also been reported in pravastatin-treated patients [see Adverse Reactions (6)]. Myopathy, defined as muscle aching or muscle weakness in conjunction with increases in creatine phosphokinase (CPK) values to greater than 10 times the ULN, was rare (< 0.1%) in pravastatin clinical trials. Myopathy should be considered in any patient with diffuse myalgias, muscle tenderness or weakness, and/or marked elevation of CPK. Predisposing factors include advanced age (> 65), uncontrolled hypothyroidism, and renal impairment.
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use. IMNM is characterized by: proximal muscle weakness and elevated serum CPK, which persist despite discontinuation of statin treatment; muscle biopsy showing necrotizing myopathy without significant inflammation and improvement with immunosuppressive agents.
All patients should be advised to promptly report to their physician unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing pravastatin sodium.
Pravastatin therapy should be discontinued if markedly elevated CPK levels occur or myopathy is diagnosed or suspected. Pravastatin therapy should also be temporarily withheld in any patient experiencing an acute or serious condition predisposing to the development of renal failure secondary to rhabdomyolysis, e.g., sepsis; hypotension; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; or uncontrolled epilepsy.
The risk of myopathy during treatment with statins is increased with concurrent therapy with either erythromycin, cyclosporine, niacin, or fibrates. However, neither myopathy nor significant increases in CPK levels have been observed in 3 reports involving a total of 100 post-transplant patients (24 renal and 76 cardiac) treated for up to 2 years concurrently with pravastatin 10 to 40 mg and cyclosporine. Some of these patients also received other concomitant immunosuppressive therapies. Further, in clinical trials involving small numbers of patients who were treated concurrently with pravastatin and niacin, there were no reports of myopathy. Also, myopathy was not reported in a trial of combination pravastatin (40 mg/day) and gemfibrozil (1200 mg/day), although 4 of 75 patients on the combination showed marked CPK elevations versus 1 of 73 patients receiving placebo. There was a trend toward more frequent CPK elevations and patient withdrawals due to musculoskeletal symptoms in the group receiving combined treatment as compared with the groups receiving placebo, gemfibrozil, or pravastatin monotherapy. The use of fibrates alone may occasionally be associated with myopathy. The benefit of further alterations in lipid levels by the combined use of pravastatin sodium with fibrates should be carefully weighed against the potential risks of this combination.
Cases of myopathy, including rhabdomyolysis, have been reported with pravastatin coadministered with colchicine, and caution should be exercised when prescribing pravastatin with colchicine [see Drug Interactions (7.3)].
5.2 Liver
Statins, like some other lipid-lowering therapies, have been associated with biochemical abnormalities of liver function. In 3 long-term (4.8 to 5.9 years), placebo-controlled clinical trials (WOS, LIPID, CARE), 19,592 subjects (19,768 randomized) were exposed to pravastatin or placebo [see Clinical Studies (14)]. In an analysis of serum transaminase values (ALT, AST), incidences of marked abnormalities were compared between the pravastatin and placebo treatment groups; a marked abnormality was defined as a post-treatment test value greater than 3 times the ULN for subjects with pretreatment values less than or equal to the ULN, or 4 times the pretreatment value for subjects with pretreatment values greater than the ULN but less than 1.5 times the ULN. Marked abnormalities of ALT or AST occurred with similar low frequency (≤ 1.2%) in both treatment groups. Overall, clinical trial experience showed that liver function test abnormalities observed during pravastatin therapy were usually asymptomatic, not associated with cholestasis, and did not appear to be related to treatment duration. In a 320 patient placebo-controlled clinical trial, subjects with chronic (> 6 months) stable liver disease, due primarily to hepatitis C or non-alcoholic fatty liver disease, were treated with 80 mg pravastatin or placebo for up to 9 months. The primary safety endpoint was the proportion of subjects with at least one ALT ≥ 2 times the ULN for those with normal ALT (≤ ULN) at baseline or a doubling of the baseline ALT for those with elevated ALT (> ULN) at baseline. By Week 36, 12 out of 160 (7.5%) subjects treated with pravastatin met the prespecified safety ALT endpoint compared to 20 out of 160 (12.5%) subjects receiving placebo. Conclusions regarding liver safety are limited since the study was not large enough to establish similarity between groups (with 95% confidence) in the rates of ALT elevation.
It is recommended that liver function tests be performed prior to the initiation of therapy and when clinically indicated.
Active liver disease or unexplained persistent transaminase elevations are contraindications to the use of pravastatin [see Contraindications (4.2)]. Caution should be exercised when pravastatin is administered to patients who have a recent (< 6 months) history of liver disease, have signs that may suggest liver disease (e.g., unexplained aminotransferase elevations, jaundice), or are heavy users of alcohol.
There have been rare postmarketing reports of fatal and non-fatal hepatic failure in patients taking statins, including pravastatin. If serious liver injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment with pravastatin sodium, promptly interrupt therapy. If an alternate etiology is not found do not restart pravastatin sodium.
5.3 Endocrine Function
Statins interfere with cholesterol synthesis and lower circulating cholesterol levels and, as such, might theoretically blunt adrenal or gonadal steroid hormone production. Results of clinical trials with pravastatin in males and post-menopausal females were inconsistent with regard to possible effects of the drug on basal steroid hormone levels. In a study of 21 males, the mean testosterone response to human chorionic gonadotropin was significantly reduced (p < 0.004) after 16 weeks of treatment with 40 mg of pravastatin. However, the percentage of patients showing a ≥ 50% rise in plasma testosterone after human chorionic gonadotropin stimulation did not change significantly after therapy in these patients. The effects of statins on spermatogenesis and fertility have not been studied in adequate numbers of patients. The effects, if any, of pravastatin on the pituitary-gonadal axis in pre-menopausal females are unknown. Patients treated with pravastatin who display clinical evidence of endocrine dysfunction should be evaluated appropriately. Caution should also be exercised if a statin or other agent used to lower cholesterol levels is administered to patients also receiving other drugs (e.g., ketoconazole, spironolactone, cimetidine) that may diminish the levels or activity of steroid hormones.
In a placebo-controlled study of 214 pediatric patients with HeFH, of which 106 were treated with pravastatin (20 mg in the children aged 8 to 13 years and 40 mg in the adolescents aged 14 to 18 years) for 2 years, there were no detectable differences seen in any of the endocrine parameters (ACTH, cortisol, DHEAS, FSH, LH, TSH, estradiol [girls] or testosterone [boys]) relative to placebo. There were no detectable differences seen in height and weight changes, testicular volume changes, or Tanner score relative to placebo.
-
6 ADVERSE REACTIONS
Pravastatin is generally well tolerated; adverse reactions have usually been mild and transient. In 4-month-long placebo-controlled trials, 1.7% of pravastatin-treated patients and 1.2% of placebo-treated patients were discontinued from treatment because of adverse experiences attributed to study drug therapy; this difference was not statistically significant.
6.1 Adverse Clinical Events
Short-Term Controlled Trials
In the pravastatin sodium placebo-controlled clinical trials database of 1313 patients (age range 20 to 76 years, 32.4% women, 93.5% Caucasians, 5% Blacks, 0.9% Hispanics, 0.4% Asians, 0.2% Others) with a median treatment duration of 14 weeks, 3.3% of patients on pravastatin sodium and 1.2% patients on placebo discontinued due to adverse events regardless of causality. The most common adverse reactions that led to treatment discontinuation and occurred at an incidence greater than placebo were: liver function test increased, nausea, anxiety/depression, and dizziness.
All adverse clinical events (regardless of causality) reported in ≥ 2% of pravastatin-treated patients in placebo-controlled trials of up to 8 months duration are identified in Table 1:
Table 1: Adverse Events in ≥ 2% of Patients Treated With Pravastatin 5 to 40 mg and at an Incidence Greater Than Placebo in Short-Term Placebo-Controlled Trials (% of Patients)
5 mg
10 mg
20 mg
40 mg
Any Dose
Placebo
Body System/Event N = 100 N = 153 N = 478 N = 171 N = 902 N = 411 Cardiovascular
Angina Pectoris
5.0
4.6
4.8
3.5
4.5
3.4
Dermatologic Rash
3.0
2.6
6.7
1.2
4.5
1.4
Gastrointestinal Nausea/Vomiting
4.0
5.9
10.5
2.3
7.4
7.1
Diarrhea
8.0
8.5
6.5
4.7
6.7
5.6
Flatulence
2.0
3.3
4.6
0.0
3.2
4.4
Dyspepsia/Heartburn
0.0
3.3
3.6
0.6
2.5
2.7
Abdominal Distension
2.0
3.3
2.1
0.6
2.0
2.4
General Fatigue
4.0
1.3
5.2
0.0
3.4
3.9
Chest Pain
4.0
1.3
3.3
1.2
2.7
1.9
Influenza
4.0
2.6
1.9
0.6
2.0
0.7
Musculoskeletal Musculoskeletal Pain
13.0
3.9
13.2
5.3
10.1
10.2
Myalgia
1.0
2.6
2.9
1.2
2.3
1.2
Nervous System Headache
5.0
6.5
7.5
3.5
6.3
4.6
Dizziness
4.0
1.3
5.2
0.6
3.5
3.4
Respiratory Pharyngitis
2.0
4.6
1.5
1.2
2.0
2.7
Upper Respiratory
Infection6.0
9.8
5.2
4.1
5.9
5.8
Rhinitis
7.0
5.2
3.8
1.2
3.9
4.9
Cough
4.0
1.3
3.1
1.2
2.5
1.7
Investigation ALT Increased
2.0
2.0
4.0
1.2
2.9
1.2
g-GT Increased
3.0
2.6
2.1
0.6
2.0
1.2
CPK Increased
5.0
1.3
5.2
2.9
4.1
3.6
The safety and tolerability of pravastatin sodium at a dose of 80 mg in 2 controlled trials with a mean exposure of 8.6 months was similar to that of pravastatin sodium at lower doses except that 4 out of 464 patients taking 80 mg of pravastatin had a single elevation of CK > 10 times ULN compared to 0 out of 115 patients taking 40 mg of pravastatin.
Long-Term Controlled Morbidity and Mortality Trials
In the pravastatin sodium placebo-controlled clinical trials database of 21,483 patients (age range 24 to 75 years, 10.3% women, 52.3% Caucasians, 0.8% Blacks, 0.5% Hispanics, 0.1% Asians, 0.1% Others, 46.1% Not Recorded) with a median treatment duration of 261 weeks, 8.1% of patients on pravastatin sodium and 9.3% patients on placebo discontinued due to adverse events regardless of causality.
Adverse event data were pooled from 7 double-blind, placebo-controlled trials (West of Scotland Coronary Prevention Study [WOS]; Cholesterol and Recurrent Events study [CARE]; Long-term Intervention with Pravastatin in Ischemic Disease study [LIPID]; Pravastatin Limitation of Atherosclerosis in the Coronary Arteries study [PLAC I]; Pravastatin, Lipids and Atherosclerosis in the Carotids study [PLAC II]; Regression Growth Evaluation Statin Study [REGRESS]; and Kuopio Atherosclerosis Prevention Study [KAPS]) involving a total of 10,764 patients treated with pravastatin 40 mg and 10,719 patients treated with placebo. The safety and tolerability profile in the pravastatin group was comparable to that of the placebo group. Patients were exposed to pravastatin for a mean of 4.0 to 5.1 years in WOS, CARE, and LIPID and 1.9 to 2.9 years in PLAC I, PLAC II, KAPS, and REGRESS. In these long-term trials, the most common reasons for discontinuation were mild, non-specific gastrointestinal complaints. Collectively, these 7 trials represent 47,613 patient-years of exposure to pravastatin. All clinical adverse events (regardless of causality) occurring in ≥ 2% of patients treated with pravastatin in these studies are identified in Table 2.
Table 2: Adverse Events in ≥ 2% of Patients Treated With Pravastatin 40 mg and at an Incidence
Greater Than Placebo in Long-Term Placebo-Controlled Trials
Body System/EventPravastatin
(N = 10,764)
% of patientsPlacebo
(N = 10,719)
% of patientsDermatologic
Rash (including dermatitis)7.2
7.1
General
Edema
3.0
2.7
Fatigue
8.4
7.8
Chest Pain
10.0
9.8
Fever
2.1
1.9
Weight Gain
3.8
3.3
Weight Loss
3.3
2.8
Musculoskeletal Musculoskeletal Pain
24.9
24.4
Muscle Cramp
5.1
4.6
Musculoskeletal Traumatism
10.2
9.6
Nervous System Dizziness
7.3
6.6
Sleep Disturbance
3.0
2.4
Anxiety/Nervousness
4.8
4.7
Paresthesia 3.2
3.0
Renal/Genitourinary Urinary Tract Infection
2.7
2.6
Respiratory Upper Respiratory Tract Infection
21.2
20.2
Cough
8.2
7.4
Influenza
9.2
9.0
Pulmonary Infection
3.8
3.5
Sinus Abnormality
7.0
6.7
Tracheobronchitis 3.4
3.1
Special Senses Vision Disturbance (includes blurred vision, diplopia)
3.4
3.3
Infections Viral Infection
3.2
2.9
In addition to the events listed above in the long-term trials table, events of probable, possible, or uncertain relationship to study drug that occurred in < 2.0% of pravastatin-treated patients in the long-term trials included the following:
Dermatologic: scalp hair abnormality (including alopecia), urticaria.
Endocrine/Metabolic: sexual dysfunction, libido change.
General: flushing.
Immunologic: allergy, edema head/neck.
Musculoskeletal: muscle weakness.
Nervous System: vertigo, insomnia, memory impairment, neuropathy (including peripheral neuropathy).
Special Senses: taste disturbance.
6.2 Postmarketing Experience
In addition to the events reported above, as with other drugs in this class, the following events have been reported during postmarketing experience with pravastatin sodium, regardless of causality assessment:
Musculoskeletal: myopathy, rhabdomyolysis, tendon disorder, polymyositis.
There have been rare reports of immune-mediated necrotizing myopathy associated with statin use [see Warnings and Precautions (5.1)].
Nervous System: dysfunction of certain cranial nerves (including alteration of taste, impairment of extraocular movement, facial paresis), peripheral nerve palsy.
There have been rare postmarketing reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with statin use. These cognitive issues have been reported for all statins. The reports are generally nonserious, and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks).
Hypersensitivity: anaphylaxis, angioedema, lupus erythematosus-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, purpura, hemolytic anemia, positive ANA, ESR increase, arthritis, arthralgia, asthenia, photosensitivity, chills, malaise, toxic epidermal necrolysis, erythema multiforme (including Stevens-Johnson syndrome).
Gastrointestinal: abdominal pain, constipation, pancreatitis, hepatitis (including chronic active hepatitis), cholestatic jaundice, fatty change in liver, cirrhosis, fulminant hepatic necrosis, hepatoma, fatal and non-fatal hepatic failure.
Dermatologic: a variety of skin changes (e.g., nodules, discoloration, dryness of mucous membranes, changes to hair/nails).
Renal: urinary abnormality (including dysuria, frequency, nocturia).
Respiratory: dyspnea, interstitial lung disease.
Psychiatric: nightmare.
Reproductive: gynecomastia.
Laboratory Abnormalities: liver function test abnormalities, thyroid function abnormalities.
6.3 Laboratory Test Abnormalities
Increases in ALT, AST values and CPK have been observed [see Warnings and Precautions (5.1, 5.2)].
Transient, asymptomatic eosinophilia has been reported. Eosinophil counts usually returned to normal despite continued therapy. Anemia, thrombocytopenia, and leukopenia have been reported with statins.
6.4 Pediatric Patients
In a 2 year, double-blind, placebo-controlled study involving 100 boys and 114 girls with HeFH (n = 214; age range 8 to 18.5 years, 53% female, 95% Caucasians, < 1% Blacks, 3% Asians, 1% Other), the safety and tolerability profile of pravastatin was generally similar to that of placebo [see Warnings and Precautions (5.3), Use in Specific Populations (8.4), and Clinical Pharmacology (12.3)].
-
7 DRUG INTERACTIONS
For the concurrent therapy of either cyclosporine, fibrates, niacin (nicotinic acid), or erythromycin, the risk of myopathy increases [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
7.1 Cyclosporine
The risk of myopathy/rhabdomyolysis is increased with concomitant administration of cyclosporine. Limit pravastatin to 20 mg once daily for concomitant use with cyclosporine [see Dosage and Administration (2.6), Warnings and Precautions (5.1), and Clinical Pharmacology (12.3)].
7.2 Clarithromycin and Other Macrolide Antibiotics
The risk of myopathy/rhabdomyolysis is increased with concomitant administration of clarithromycin. Limit pravastatin to 40 mg once daily for concomitant use with clarithromycin [see Dosage and Administration (2.7), Warnings and Precautions (5.1), and Clinical Pharmacology (12.3)].
Other macrolides (e.g., erythromycin and azithromycin) have the potential to increase statin exposures while used in combination. Pravastatin should be used cautiously with macrolide antibiotics due to a potential increased risk of myopathies.
7.3 Colchicine
The risk of myopathy/rhabdomyolysis is increased with concomitant administration of colchicine [see Warnings and Precautions (5.1)].
7.4 Gemfibrozil
Due to an increased risk of myopathy/rhabdomyolysis when HMG-CoA reductase inhibitors are coadministered with gemfibrozil, concomitant administration of pravastatin sodium with gemfibrozil should be avoided [see Warnings and Precautions (5.1)].
7.5 Other Fibrates
Because it is known that the risk of myopathy during treatment with HMG-CoA reductase inhibitors is increased with concurrent administration of other fibrates, pravastatin sodium should be administered with caution when used concomitantly with other fibrates [see Warnings and Precautions (5.1)].
7.6 Niacin
The risk of skeletal muscle effects may be enhanced when pravastatin is used in combination with niacin; a reduction in pravastatin sodium dosage should be considered in this setting [see Warnings and Precautions (5.1)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Pravastatin sodium is contraindicated for use in pregnant woman because of the potential for fetal harm. As safety in pregnant women has not been established and there is no apparent benefit to therapy with pravastatin sodium during pregnancy, pravastatin sodium should be immediately discontinued as soon as pregnancy is recognized [see Contraindications (4.3)]. Limited published data on the use of pravastatin sodium in pregnant women are insufficient to determine a drug-associated risk of major congenital malformations or miscarriage. In animal reproduction studies, no evidence of fetal malformations was seen in rabbits or rats exposed to 10 times to 120 times, respectively, the maximum recommended human dose (MRHD) of 80 mg/day. Fetal skeletal abnormalities, offspring mortality, and developmental delays occurred when pregnant rats were administered 10 times to 12 times the MRHD during organogenesis to parturition [see Data]. Advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Human Data
Limited published data on pravastatin have not shown an increased risk of major congenital malformations or miscarriage.
Rare reports of congenital anomalies have been received following intrauterine exposure to other statins. In a review2 of approximately 100 prospectively followed pregnancies in women exposed to simvastatin or lovastatin, the incidences of congenital anomalies, spontaneous abortions, and fetal deaths/stillbirths did not exceed what would be expected in the general population. The number of cases is adequate to exclude a ≥ 3 to 4-fold increase in congenital anomalies over the background incidence. In 89% of the prospectively followed pregnancies, drug treatment was initiated prior to pregnancy and was discontinued at some point in the first trimester when pregnancy was identified.
Animal Data
Embryofetal and neonatal mortality was observed in rats given pravastatin during the period of organogenesis or during organogenesis continuing through weaning. In pregnant rats given oral gavage doses of 4, 20, 100, 500, and 1000 mg/kg/day from gestation days 7 through 17 (organogenesis) increased mortality of offspring and increased cervical rib skeletal anomalies were observed at ≥ 100 mg/kg/day systemic exposure, 10 times the human exposure at 80 mg/day MRHD based on body surface area (mg/m2).
In other studies, no teratogenic effects were observed when pravastatin was dosed orally during organogenesis in rabbits (gestation days 6 through 18) up to 50 mg/kg/day or in rats (gestation days 7 through 17) up to 1000 mg/kg/day. Exposures were 10 times (rabbit) or 120 times (rat) the human exposure at 80 mg/day MRHD based on body surface area (mg/m2).
In pregnant rats given oral gavage doses of 10, 100, and 1000 mg/kg/day from gestation day 17 through lactation day 21 (weaning), increased mortality of offspring and developmental delays were observed at ≥ 100 mg/kg/day systemic exposure, corresponding to 12 times the human exposure at 80 mg/day MRHD, based on body surface area (mg/m2).
In pregnant rats, pravastatin crosses the placenta and is found in fetal tissue at 30% of the maternal plasma levels following administration of a single dose of 20 mg/day orally on gestation day 18, which corresponds to exposure 2 times the MRHD of 80 mg daily based on body surface area (mg/m ). In lactating rats, up to 7 times higher levels of pravastatin are present in the breast milk than in the maternal plasma, which corresponds to exposure 2 times the MRHD of 80 mg/day based on body surface area (mg/m2).
8.2 Lactation
Risk Summary
Pravastatin use is contraindicated during breastfeeding [see Contraindications (4.4)]. Based on one lactation study in published literature, pravastatin is present in human milk. There is no available information on the effects of the drug on the breastfed infant or the effects of the drug on milk production. Because of the potential for serious adverse reactions in a breastfed infant, advise patients that breastfeeding is not recommended during treatment with pravastatin sodium.
8.3 Females and Males of Reproductive Potential
Contraception
Females
Pravastatin sodium may cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with pravastatin sodium.
8.4 Pediatric Use
The safety and effectiveness of pravastatin sodium in children and adolescents from 8 to 18 years of age have been evaluated in a placebo-controlled study of 2 years duration. Patients treated with pravastatin had an adverse experience profile generally similar to that of patients treated with placebo with influenza and headache commonly reported in both treatment groups [see Adverse Reactions (6.4)]. Doses greater than 40 mg have not been studied in this population. Children and adolescent females of childbearing potential should be counseled on appropriate contraceptive methods while on pravastatin therapy [see Contraindications (4.3) and Use in Specific Populations (8.1)]. For dosing information [see Dosage and Administration (2.4)].
Double-blind, placebo-controlled pravastatin studies in children less than 8 years of age have not been conducted.
8.5 Geriatric Use
Two secondary prevention trials with pravastatin (CARE and LIPID) included a total of 6593 subjects treated with pravastatin 40 mg for periods ranging up to 6 years. Across these 2 studies, 36.1% of pravastatin subjects were aged 65 and older and 0.8% were aged 75 and older. The beneficial effect of pravastatin in elderly subjects in reducing cardiovascular events and in modifying lipid profiles was similar to that seen in younger subjects. The adverse event profile in the elderly was similar to that in the overall population. Other reported clinical experience has not identified differences in responses to pravastatin between elderly and younger patients.
Mean pravastatin AUCs are slightly (25% to 50%) higher in elderly subjects than in healthy young subjects, but mean maximum plasma concentration (Cmax), time to maximum plasma concentration (Tmax), and half-life (t½) values are similar in both age groups and substantial accumulation of pravastatin would not be expected in the elderly [see Clinical Pharmacology (12.3)].
Since advanced age (≥ 65 years) is a predisposing factor for myopathy, pravastatin sodium should be prescribed with caution in the elderly [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Pravastatin sodium, USP is one of a class of lipid-lowering compounds, the statins, which reduce cholesterol biosynthesis. These agents are competitive inhibitors of HMG-CoA reductase, the enzyme catalyzing the early rate-limiting step in cholesterol biosynthesis, conversion of HMG-CoA to mevalonate.
Pravastatin sodium, USP is designated chemically as 1-naphthaleneheptanoic acid, 1,2,6,7,8,8a-hexahydro-β,δ,6-trihydroxy-2-methyl-8-(2-methyl-1-oxobutoxy)-, monosodium salt, [1S-[1α (βS*,δS*),2α,6α,8β(R*),8aα]]-. It has the following structural formula:
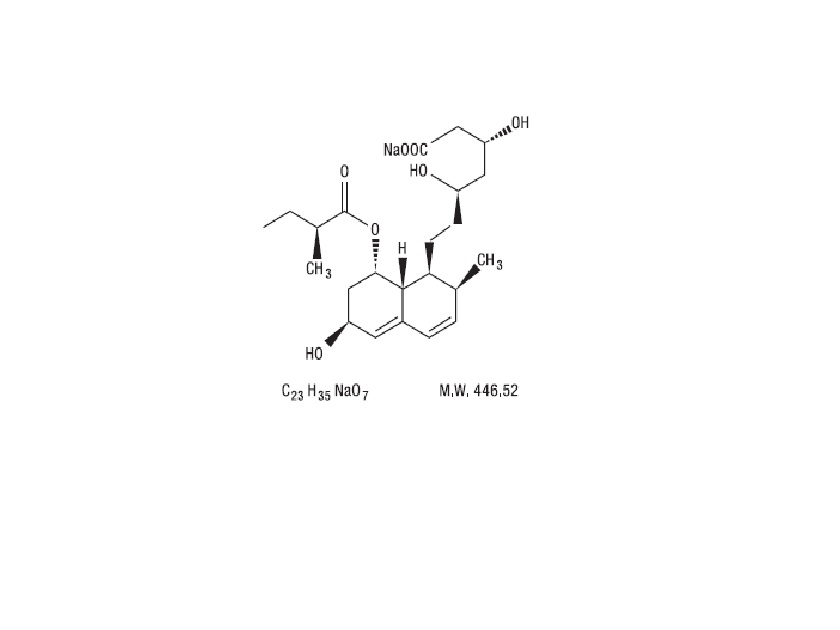
Pravastatin
Pravastatin sodium, USP is an odorless, white to off-white, fine or crystalline powder. It is a relatively polar hydrophilic compound with a partition coefficient (octanol/water) of 0.59 at a pH of 7.0. It is soluble in methanol and water (> 300 mg/mL), slightly soluble in isopropanol, and practically insoluble in acetone, acetonitrile, chloroform, and ether.
Pravastatin sodium tablets USP are available for oral administration as 10 mg, 20 mg, 40 mg, and 80 mg tablets. Inactive ingredients include: calcium phosphate dibasic, crospovidone, lactose anhydrous, microcrystalline cellulose, and povidone. Additionally, the 10 mg, 20 mg, and 40 mg tablet contains croscarmellose sodium and sodium stearyl fumarate. Additionally, the 10 mg tablet contains ferric oxide red; the 20 mg tablet contains ferric oxide yellow; the 40 mg tablet contains FD&C Blue No. 1 Aluminum Lake and Yellow D&C No. 10; and the 80 mg tablet contains magnesium stearate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pravastatin is a reversible inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, the enzyme that catalyzes the conversion of HMG-CoA to mevalonate, an early and rate limiting step in the biosynthetic pathway for cholesterol. In addition, pravastatin reduces VLDL and TG and increases HDL-C.
12.3 Pharmacokinetics
General
Absorption: Pravastatin sodium is administered orally in the active form. In studies in man, peak plasma pravastatin concentrations occurred 1 to 1.5 hours upon oral administration. Based on urinary recovery of total radiolabeled drug, the average oral absorption of pravastatin is 34% and absolute bioavailability is 17%. While the presence of food in the gastrointestinal tract reduces systemic bioavailability, the lipid-lowering effects of the drug are similar whether taken with or 1 hour prior to meals.
Pravastatin plasma concentrations, including area under the concentration-time curve (AUC), Cmax, and steady-state minimum (Cmin), are directly proportional to administered dose. Systemic bioavailability of pravastatin administered following a bedtime dose was decreased 60% compared to that following an AM dose. Despite this decrease in systemic bioavailability, the efficacy of pravastatin administered once daily in the evening, although not statistically significant, was marginally more effective than that after a morning dose.
The coefficient of variation (CV), based on between-subject variability, was 50% to 60% for AUC. The geometric means of pravastatin Cmax and AUC following a 20 mg dose in the fasted state were 26.5 ng/mL and 59.8 ng*hr/mL, respectively.
Steady-state AUCs, Cmax, and Cmin plasma concentrations showed no evidence of pravastatin accumulation following once or twice daily administration of pravastatin sodium tablets.
Distribution: Approximately 50% of the circulating drug is bound to plasma proteins.
Metabolism: The major biotransformation pathways for pravastatin are: (a) isomerization to 6-epi pravastatin and the 3α-hydroxyisomer of pravastatin (SQ 31,906) and (b) enzymatic ring hydroxylation to SQ 31,945. The 3α-hydroxyisomeric metabolite (SQ 31,906) has 1/10 to 1/40 the HMG-CoA reductase inhibitory activity of the parent compound. Pravastatin undergoes extensive first-pass extraction in the liver (extraction ratio 0.66).
Excretion: Approximately 20% of a radiolabeled oral dose is excreted in urine and 70% in the feces. After intravenous administration of radiolabeled pravastatin to normal volunteers, approximately 47% of total body clearance was via renal excretion and 53% by non-renal routes (i.e., biliary excretion and biotransformation).
Following single dose oral administration of 14C-pravastatin, the radioactive elimination t½ for pravastatin is 1.8 hours in humans.
Specific Populations
Renal Impairment: A single 20 mg oral dose of pravastatin was administered to 24 patients with varying degrees of renal impairment (as determined by creatinine clearance). No effect was observed on the pharmacokinetics of pravastatin or its 3α-hydroxy isomeric metabolite (SQ 31,906). Compared to healthy subjects with normal renal function, patients with severe renal impairment had 69% and 37% higher mean AUC and Cmax values, respectively, and a 0.61 hour shorter t½ for the inactive enzymatic ring hydroxylation metabolite (SQ 31,945).
Hepatic Impairment: In a study comparing the kinetics of pravastatin in patients with biopsy confirmed cirrhosis (N = 7) and normal subjects (N = 7), the mean AUC varied 18 fold in cirrhotic patients and 5 fold in healthy subjects. Similarly, the peak pravastatin values varied 47 fold for cirrhotic patients compared to 6 fold for healthy subjects [see Warnings and Precautions (5.2)].
Geriatric: In a single oral dose study using pravastatin 20 mg, the mean AUC for pravastatin was approximately 27% greater and the mean cumulative urinary excretion (CUE) approximately 19% lower in elderly men (65 to 75 years old) compared with younger men (19 to 31 years old). In a similar study conducted in women, the mean AUC for pravastatin was approximately 46% higher and the mean CUE approximately 18% lower in elderly women (65 to 78 years old) compared with younger women (18 to 38 years old). In both studies, Cmax, Tmax, and t½ values were similar in older and younger subjects [see Use in Specific Populations (8.5)].
Pediatric: After 2 weeks of once-daily 20 mg oral pravastatin administration, the geometric means of AUC were 80.7 (CV 44%) and 44.8 (CV 89%) ng*hr/mL for children (8 to 11 years, N = 14) and adolescents (12 to 16 years, N = 10), respectively. The corresponding values for Cmax were 42.4 (CV 54%) and 18.6 ng/mL (CV 100%) for children and adolescents, respectively. No conclusion can be made based on these findings due to the small number of samples and large variability [see Use in Specific Populations (8.4)].
Drug-Drug Interactions
Table 3: Effect of Coadministered Drugs on the Pharmacokinetics of Pravastatin
Coadministered Drug and Dosing
RegimenPravastatin Dose (mg)
Change in AUC
Change in Cmax
Cyclosporine 5 mg/kg single dose
40 mg single
dose↑282%
↑327%
Clarithromycin 500 mg BID for 9 days
40 mg OD for 8
days↑110%
↑128%
Boceprevir 800 mg TID for 6 days
40 mg single
dose↑63%
↑49%
Darunavir 600 mg BID/Ritonavir 100 mg
BID for 7 days40 mg single
dose↑81%
↑63%
Colestipol 10 g single dose
20 mg single dose
↓47%
↓53%
Cholestyramine 4 g single dose 20 mg single dose Administered simultaneously
↓40% ↓39%
Administered 1 hour prior to
cholestyramine↑12%
↑30%
Administered 4 hours after
cholestyramine↓12%
↓6.8%
Cholestyramine 24 g OD for 4 weeks 20 mg BID for 8
weeks↓51%
↑4.9%
5 mg BID for 8
weeks↓38%
↑23%
10 mg BID for 8
weeks↓18%
↓33%
Fluconazole
200 mg IV for 6 days
20 mg PO + 10
mg IV↓34%
↓33% 200 mg PO for 6 days
20 mg PO + 10
mg IV↓16%
↓16% Kaletra 400 mg/100 mg BID for 14 days
20 mg OD for 4 days
↑33%
↑26%
Verapamil IR 120 mg for 1 day and
Verapamil ER 480 mg for 3 days40 mg single
dose↑31%
↑42%
Cimetidine 300 mg QID for 3 days
20 mg single
dose↑30%
↑9.8%
Antacids 15 mL QID for 3 days
20 mg single
dose↓28%
↓24%
Digoxin 0.2 mg OD for 9 days
20 mg OD for 9 days
↑23%
↑26%
Probucol 500 mg single dose
20 mg single
dose↑14%
↑24%
Warfarin 5 mg OD for 6 days
20 mg BID for
6 days↓13%
↑6.7%
Itraconazole 200 mg OD for 30 days
40 mg OD for
30 days↑11% (compared to
Day 1)↑17% (compared to
Day 1)Gemfibrozil 600 mg single dose
20 mg single
dose↓7.0%
↓20%
Aspirin 324 mg single dose
20 mg single
dose↑4.7%
↑8.9%
Niacin 1 g single dose
20 mg single
dose↓3.6%
↓8.2%
Diltiazem
20 mg single
dose↑2.7%
↑30%
Grapefruit juice
40 mg single
dose↓1.8%
↑3.7%
BID = twice daily; OD = once daily; QID = four times daily
Table 4: Effect of Pravastatin on the Pharmacokinetics of Coadministered Drugs
Pravastatin Dosing
RegimenName and Dose
Change in AUC
Change in
Cmax20 mg BID for 6 days Warfarin 5 mg OD for 6 days
Change in mean prothrombin time↑17%
↑0.4 sec
↑15%
20 mg OD for 9 days
Digoxin 0.2 mg OD for 9 days
↑4.6%
↑5.3%
20 mg BID for 4 weeks
Antipyrine 1.2 g single dose
↑3.0%
Not Reported
10 mg BID for 4 weeks
↑1.6%
5 mg BID for 4 weeks
↑Less than1%
20 mg OD for 4 days
Kaletra 400 mg/100 mg BID for 14
daysNo change
No change
BID = twice daily; OD = once daily
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2 year study in rats fed pravastatin at doses of 10, 30, or 100 mg/kg body weight, there was an increased incidence of hepatocellular carcinomas in males at the highest dose (p < 0.01). These effects in rats were observed at approximately 12 times the human dose (HD) of 80 mg based on body surface area (mg/m2) and at approximately 4 times the HD, based on AUC.
In a 2 year study in mice fed pravastatin at doses of 250 and 500 mg/kg/day, there was an increased incidence of hepatocellular carcinomas in males and females at both 250 and 500 mg/kg/day (p < 0.0001). At these doses, lung adenomas in females were increased (p = 0.013). These effects in mice were observed at approximately 15 times (250 mg/kg/day) and 23 times (500 mg/kg/day) the HD of 80 mg, based on AUC. In another 2 year study in mice with doses up to 100 mg/kg/day (producing drug exposures approximately 2 times the HD of 80 mg, based on AUC), there were no drug-induced tumors.
No evidence of mutagenicity was observed in vitro, with or without rat-liver metabolic activation, in the following studies: microbial mutagen tests, using mutant strains of Salmonella typhimurium or Escherichia coli; a forward mutation assay in L5178Y TK +/− mouse lymphoma cells; a chromosomal aberration test in hamster cells; and a gene conversion assay using Saccharomyces cerevisiae. In addition, there was no evidence of mutagenicity in either a dominant lethal test in mice or a micronucleus test in mice.
In a fertility study in adult rats with daily doses up to 500 mg/kg, pravastatin did not produce any adverse effects on fertility or general reproductive performance.
13.2 Animal Toxicology and/or Pharmacology
CNS Toxicity
CNS vascular lesions, characterized by perivascular hemorrhage and edema and mononuclear cell infiltration of perivascular spaces, were seen in dogs treated with pravastatin at a dose of 25 mg/kg/day. These effects in dogs were observed at approximately 59 times the HD of 80 mg/day, based on AUC. Similar CNS vascular lesions have been observed with several other drugs in this class.
A chemically similar drug in this class produced optic nerve degeneration (Wallerian degeneration of retinogeniculate fibers) in clinically normal dogs in a dose-dependent fashion starting at 60 mg/kg/day, a dose that produced mean plasma drug levels about 30 times higher than the mean drug level in humans taking the highest recommended dose (as measured by total enzyme inhibitory activity). This same drug also produced vestibulocochlear Wallerian-like degeneration and retinal ganglion cell chromatolysis in dogs treated for 14 weeks at 180 mg/kg/day, a dose which resulted in a mean plasma drug level similar to that seen with the 60 mg/kg/day dose.
When administered to juvenile rats (postnatal days [PND] 4 through 80 at 5 to 45 mg/kg/day), no drug related changes were observed at 5 mg/kg/day. At 15 and 45 mg/kg/day, altered body-weight gain was observed during the dosing and 52 day recovery periods as well as slight thinning of the corpus callosum at the end of the recovery period. This finding was not evident in rats examined at the completion of the dosing period and was not associated with any inflammatory or degenerative changes in the brain. The biological relevance of the corpus callosum finding is uncertain due to the absence of any other microscopic changes in the brain or peripheral nervous tissue and because it occurred at the end of the recovery period. Neurobehavioral changes (enhanced acoustic startle responses and increased errors in water-maze learning) combined with evidence of generalized toxicity were noted at 45 mg/kg/day during the later part of the recovery period. Serum pravastatin levels at 15 mg/kg/day are approximately ≥ 1 times (AUC) the maximum pediatric dose of 40 mg. No thinning of the corpus callosum was observed in rats dosed with pravastatin (≥ 250 mg/kg/day) beginning PND 35 for 3 months suggesting increased sensitivity in younger rats. PND 35 in a rat is approximately equivalent to an 8 to 12-year-old human child. Juvenile male rats given 90 times (AUC) the 40 mg dose had decreased fertility (20%) with sperm abnormalities compared to controls.
-
14 CLINICAL STUDIES
14.1 Prevention of Coronary Heart Disease
In the Pravastatin Primary Prevention Study (WOS),3 the effect of pravastatin sodium on fatal and nonfatal CHD was assessed in 6595 men 45 to 64 years of age, without a previous MI, and with LDL-C levels between 156 to 254 mg/dL (4 to 6.7 mmol/L). In this randomized, double-blind, placebo-controlled study, patients were treated with standard care, including dietary advice, and either pravastatin sodium 40 mg daily (N = 3302) or placebo (N = 3293) and followed for a median duration of 4.8 years. Median (25th, 75th percentile) percent changes from baseline after 6 months of pravastatin treatment in Total-C, LDL-C, TG, and HDL-C were −20.3 (−26.9, −11.7), −27.7 (−36.0, −16.9), −9.1 (−27.6, 12.5), and 6.7 (−2.1, 15.6), respectively.
Pravastatin sodium significantly reduced the rate of first coronary events (either CHD death or nonfatal MI) by 31% (248 events in the placebo group [CHD death = 44, nonfatal MI = 204] versus 174 events in the pravastatin sodium group [CHD death = 31, nonfatal MI = 143], p = 0.0001 [see figure below]). The risk reduction with pravastatin sodium was similar and significant throughout the entire range of baseline LDL cholesterol levels. This reduction was also similar and significant across the age range studied with a 40% risk reduction for patients younger than 55 years and a 27% risk reduction for patients 55 years and older. The Pravastatin Primary Prevention Study included only men, and therefore it is not clear to what extent these data can be extrapolated to a similar population of female patients.
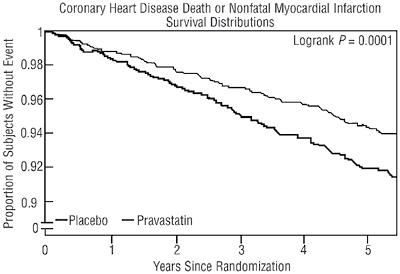
Figure 1
Pravastatin sodium also significantly decreased the risk for undergoing myocardial revascularization procedures (coronary artery bypass graft [CABG] surgery or percutaneous transluminal coronary angioplasty [PTCA]) by 37% (80 vs 51 patients, p = 0.009) and coronary angiography by 31% (128 vs 90, p = 0.007). Cardiovascular deaths were decreased by 32% (73 vs 50, p = 0.03) and there was no increase in death from non-cardiovascular causes.
14.2 Secondary Prevention of Cardiovascular Events
In the LIPID4 study, the effect of pravastatin 40 mg daily, was assessed in 9014 patients (7498 men; 1516 women; 3514 elderly patients [age ≥ 65 years]; 782 diabetic patients) who had experienced either an MI (5754 patients) or had been hospitalized for unstable angina pectoris (3260 patients) in the preceding 3 to 36 months. Patients in this multicenter, double-blind, placebo-controlled study participated for an average of 5.6 years (median of 5.9 years) and at randomization had Total-C between 114 and 563 mg/dL (mean 219 mg/dL), LDL-C between 46 and 274 mg/dL (mean 150 mg/dL), TG between 35 and 2710 mg/dL (mean 160 mg/dL), and HDL-C between 1 and 103 mg/dL (mean 37 mg/dL). At baseline, 82% of patients were receiving aspirin and 76% were receiving antihypertensive medication. Treatment with pravastatin significantly reduced the risk for total mortality by reducing coronary death (see Table 5). The risk reduction due to treatment with pravastatin on CHD mortality was consistent regardless of age. Pravastatin significantly reduced the risk for total mortality (by reducing CHD death) and CHD events (CHD mortality or nonfatal MI) in patients who qualified with a history of either MI or hospitalization for unstable angina pectoris.
Table 5: LIPID - Primary and Secondary Endpoints Number (%) of Subjects Event Pravastatin 40
mg
(N = 4512)Placebo
(N =4502)Risk Reduction p-value Primary Endpoint CHD mortality
287 (6.4) 373 (8.3) 24% 0.0004 Secondary Endpoints Total mortality
498 (11.0) 633 (14.1) 23% <0.0001 CHD mortality or nonfatal
MI557 (12.3) 715 (15.9) 24% <0.0001 Myocardial
revascularization
procedures (CABG or
PTCA)584 (12.9) 706 (15.7) 20% <0.0001 Stroke All-cause
169 (3.7) 204 (4.5) 19% 0.0477 Non-hemorrhagic
154 (3.4) 196 (4.4) 23% 0.0154 Cardiovascular mortality
331(7.3) 433 (9.6) 25% <0.0001 In the CARE5 study, the effect of pravastatin, 40 mg daily, on CHD death and nonfatal MI was assessed in 4159 patients (3583 men and 576 women) who had experienced a MI in the preceding 3 to 20 months and who had normal (below the 75th percentile of the general population) plasma total cholesterol levels. Patients in this double-blind, placebo-controlled study participated for an average of 4.9 years and had a mean baseline Total-C of 209 mg/dL. LDL-C levels in this patient population ranged from 101 to 180 mg/dL (mean 139 mg/dL). At baseline, 84% of patients were receiving aspirin and 82% were taking antihypertensive medications. Median (25th , 75th percentile) percent changes from baseline after 6 months of pravastatin treatment in Total-C, LDL-C, TG, and HDL-C were −22.0 (−28.4, −14.9), −32.4 (−39.9, −23.7), −11.0 (−26.5, 8.6), and 5.1 (−2.9, 12.7), respectively. Treatment with pravastatin significantly reduced the rate of first recurrent coronary events (either CHD death or nonfatal MI), the risk of undergoing revascularization procedures (PTCA, CABG), and the risk for stroke or TIA (see Table 6).
Table 6: CARE - Primary and Secondary Endpoints Number (%) of Subjects
Event Pravastatin 40
mg
(N = 2081)Placebo
(N = 2078)Risk Reduction p-value Primary Endpoint
CHD mortality or nonfatal
MI*212 (10.2) 274 (13.2) 24% 0.003 Secondary Endpoints Myocardial
revascularization
procedures (CABG or
PTCA)294 (14.1) 391 (18.8) 27% <0.001 Stroke or TIA
93 (4.5) 124 (6.0) 26% 0.029 * The risk reduction due to treatment with pravastatin was consistent in both sexes.
In the PLAC I6 study, the effect of pravastatin therapy on coronary atherosclerosis was assessed by coronary angiography in patients with coronary disease and moderate hypercholesterolemia (baseline LDL-C range: 130 to 190 mg/dL). In this double-blind, multicenter, controlled clinical trial, angiograms were evaluated at baseline and at 3 years in 264 patients. Although the difference between pravastatin and placebo for the primary endpoint (per-patient change in mean coronary artery diameter) and 1 of 2 secondary endpoints (change in percent lumen diameter stenosis) did not reach statistical significance, for the secondary endpoint of change in minimum lumen diameter, statistically significant slowing of disease was seen in the pravastatin treatment group (p = 0.02).
In the REGRESS7 study, the effect of pravastatin on coronary atherosclerosis was assessed by coronary angiography in 885 patients with angina pectoris, angiographically documented coronary artery disease, and hypercholesterolemia (baseline total cholesterol range: 160 to 310 mg/dL). In this double-blind, multicenter, controlled clinical trial, angiograms were evaluated at baseline and at 2 years in 653 patients (323 treated with pravastatin). Progression of coronary atherosclerosis was significantly slowed in the pravastatin group as assessed by changes in mean segment diameter (p = 0.037) and minimum obstruction diameter (p = 0.001).
Analysis of pooled events from PLAC I, PLAC II,8 REGRESS, and KAPS9 studies (combined N = 1891) showed that treatment with pravastatin was associated with a statistically significant reduction in the composite event rate of fatal and nonfatal MI (46 events or 6.4% for placebo versus 21 events or 2.4% for pravastatin, p = 0.001). The predominant effect of pravastatin was to reduce the rate of nonfatal MI.
14.3 Primary Hypercholesterolemia (Fredrickson Types IIa and IIb)
Pravastatin sodium is highly effective in reducing Total-C, LDL-C, and TG in patients with heterozygous familial, presumed familial combined, and non-familial (non-FH) forms of primary hypercholesterolemia, and mixed dyslipidemia. A therapeutic response is seen within 1 week, and the maximum response usually is achieved within 4 weeks. This response is maintained during extended periods of therapy. In addition, pravastatin sodium is effective in reducing the risk of acute coronary events in hypercholesterolemic patients with and without previous MI.
A single daily dose is as effective as the same total daily dose given twice a day. In multicenter, double-blind, placebo-controlled studies of patients with primary hypercholesterolemia, treatment with pravastatin in daily doses ranging from 10 to 40 mg consistently and significantly decreased Total-C, LDL-C, TG, and Total-C/HDL-C and LDL-C/HDL-C ratios (see Table 7).
In a pooled analysis of 2 multicenter, double-blind, placebo-controlled studies of patients with primary hypercholesterolemia, treatment with pravastatin at a daily dose of 80 mg (N = 277) significantly decreased Total-C, LDL-C, and TG. The 25th and 75th percentile changes from baseline in LDL-C for pravastatin 80 mg were −43% and −30%. The efficacy results of the individual studies were consistent with the pooled data (see Table 7).
Treatment with pravastatin sodium modestly decreased VLDL-C and pravastatin sodium across all doses produced variable increases in HDL-C (see Table 7).
Table 7: Primary Hypercholesterolemia Studies: Dose Response of Pravastatin Sodium Once Daily Administration
Dose Total-C LDL-C HDL-C TG Mean Percent Changes From Baseline After 8 Weeks * Placebo (N = 36) −3% −4% +1% −4% 10 mg (N = 18) −16% −22% +7% −15% 20 mg (N = 19) −24% −32% +2% −11% 40 mg (N = 18) −25% −34% +12% −24% Mean Percent Changes From Baseline After 6 Weeks † Placebo (N = 162) 0% −1% −1% +1% 80 mg (N = 277) −27% −37% +3% −19% * A multicenter, double-blind, placebo-controlled study.
† Pooled analysis of 2 multicenter, double-blind, placebo-controlled studies.In another clinical trial, patients treated with pravastatin in combination with cholestyramine (70% of patients were taking cholestyramine 20 or 24 g per day) had reductions equal to or greater than 50% in LDL-C. Furthermore, pravastatin attenuated cholestyramine-induced increases in TG levels (which are themselves of uncertain clinical significance).
14.4 Hypertriglyceridemia (Fredrickson Type IV)
The response to pravastatin in patients with Type IV hyperlipidemia (baseline TG > 200 mg/dL and LDL-C < 160 mg/dL) was evaluated in a subset of 429 patients from the CARE study. For pravastatin-treated subjects, the median (min, max) baseline TG level was 246.0 (200.5, 349.5) mg/dL (see Table 8).
Table 8: Patients With Fredrickson Type IV Hyperlipidemia Median (25th, 75th Percentile) % Change From Baseline
Pravastatin 40 mg (N = 429)
Placebo (N = 430)
TG
−21.1 (−34.8, 1.3)
−6.3 (−23.1, 18.3)
Total-C
−22.1 (−27.1, −14.8)
0.2 (−6.9, 6.8)
LDL-C
−31.7 (−39.6, −21.5)
0.7 (−9.0, 10.0)
HDL-C
7.4 (−1.2, 17.7)
2.8 (−5.7, 11.7)
Non-HDL-C
−27.2 (−34.0, −18.5)
−0.8 (−8.2, 7.0)
14.5 Dysbetalipoproteinemia (Fredrickson Type III)
The response to pravastatin in two double-blind crossover studies of 46 patients with genotype E2/E2 and Fredrickson Type III dysbetalipoproteinemia is shown in Table 9.
Table 9: Patients With Fredrickson Type III Dysbetalipoproteinemia Median (min, max) % Change From Baseline
Median (min, max) at Baseline
(mg/dL)Median % Change (min, max) Pravastatin 40 mg (N=
20)Study 1
Total-C
386.5 (245.0, 672.0)
−32.7 (−58.5, 4.6)
TG
443.0 (275.0, 1299.0)
−23.7 (−68.5, 44.7)
VLDL-C *
206.5 (110.0, 379.0)
−43.8 (−73.1, −14.3)
LDL-C *
117.5 (80.0, 170.0)
−40.8 (−63.7, 4.6)
HDL-C
30.0 (18.0, 88.0)
6.4 (−45.0, 105.6)
Non-HDL-C
344.5 (215.0, 646.0)
−36.7 (−66.3, 5.8)
Median (min, max) at Baseline
(mg/dL)Median % Change (min, max) Pravastatin 40 mg (N =
26)Study 2
Total-C
340.3 (230.1, 448.6)
−31.4 (−54.5, −13.0)
TG
343.2 (212.6, 845.9)
−11.9 (−56.5, 44.8)
VLDL-C
145.0 (71.5, 309.4)
−35.7 (−74.7, 19.1)
LDL-C
128.6 (63.8, 177.9)
−30.3 (−52.2, 13.5)
HDL-C
38.7 (27.1, 58.0)
5.0 (−17.7, 66.7)
Non-HDL-C
295.8 (195.3, 421.5)
−35.5 (−81.0, −13.5)
* N = 14
14.6 Pediatric Clinical Study
A double-blind, placebo-controlled study in 214 patients (100 boys and 114 girls) with heterozygous familial hypercholesterolemia (HeFH), aged 8 to 18 years was conducted for 2 years. The children (aged 8 to 13 years) were randomized to placebo (N = 63) or 20 mg of pravastatin daily (N = 65) and the adolescents (aged 14 to 18 years) were randomized to placebo (N = 45) or 40 mg of pravastatin daily (N = 41). Inclusion in the study required an LDL-C level > 95th percentile for age and sex and one parent with either a clinical or molecular diagnosis of familial hypercholesterolemia. The mean baseline LDL-C value was 239 mg/dL and 237 mg/dL in the pravastatin (range: 151 to 405 mg/dL) and placebo (range: 154 to 375 mg/dL) groups, respectively.
Pravastatin significantly decreased plasma levels of LDL-C, Total-C, and ApoB in both children and adolescents (see Table 10). The effect of pravastatin treatment in the 2 age groups was similar.
Table 10: Lipid-Lowering Effects of Pravastatin in Pediatric Patients With Heterozygous Familial Hypercholesterolemia: Least-Squares Mean % Change From Baseline at Month 24 (Last Observation Carried Forward: Intent-to-Treat)*
Pravastatin 20
mg (Aged 8 to
13 years)
N = 65Pravastatin 40
mg (Aged 14 to
18 years)
N = 41Combined
Pravastatin
(Aged 8 to 18
years)
N = 106Combined
Placebo (Aged
8 to 18 years)
N = 10895% CI of the
Difference Between
Combined
Pravastatin and
PlaceboLDL-C
−26.04†
−21.07†
−24.07†
−1.52
(−26.74, −18.86)
TC
−20.75†
−13.08†
−17.72†
−0.65
(−20.40, −13.83)
HDL-C
1.04
13.71
5.97
3.13
(−1.71, 7.43)
TG
−9.58
−0.30
−5.88
−3.27
(−13.95, 10.01)
Apo B (N)
−23.16†
(61)−18.08†
(39)−21.11†
(100)−0.97
(106)(−24.29, −16.18)
* The above least-squares mean values were calculated based on log-transformed lipid values.
† Significant at p ≤ 0.0001 when compared with placebo.The mean achieved LDL-C was 186 mg/dL (range: 67 to 363 mg/dL) in the pravastatin group compared to 236 mg/dL (range: 105 to 438 mg/dL) in the placebo group.
The safety and efficacy of pravastatin doses above 40 mg daily have not been studied in children. The long-term efficacy of pravastatin therapy in childhood to reduce morbidity and mortality in adulthood has not been established.
-
15 REFERENCES
1. Fredrickson DS, Levy RI, Lees RS. Fat transport in lipoproteins - An integrated approach to mechanisms and disorders. N Engl J Med. 1967;276: 34-44, 94-103, 148-156, 215-225, 273-281.
2. Manson JM, Freyssinges C, Ducrocq MB, Stephenson WP. Postmarketing surveillance of lovastatin and simvastatin exposure during pregnancy. Reprod Toxicol. 1996;10(6):439-446.
3. Shepherd J, Cobbe SM, Ford I, et al, for the West of Scotland Coronary Prevention Study Group (WOS). Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med. 1995;333:1301-1307.
4. The Long-term Intervention with Pravastatin in Ischemic Disease Group (LIPID). Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349-1357.
5. Sacks FM, Pfeffer MA, Moye LA, et al, for the Cholesterol and Recurrent Events Trial Investigators (CARE). The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001-1009.
6. Pitt B, Mancini GBJ, Ellis SG, et al, for the PLAC I Investigators. Pravastatin limitation of atherosclerosis in the coronary arteries (PLAC I): Reduction in atherosclerosis progression and clinical events. J Am Coll Cardiol. 1995;26:1133-1139.
7. Jukema JW, Bruschke AVG, van Boven AJ, et al, for the Regression Growth Evaluation Statin Study Group (REGRESS). Effects of lipid lowering by pravastatin on progression and regression of coronary artery disease in symptomatic man with normal to moderately elevated serum cholesterol levels. Circ. 1995;91:2528-2540.
8. Crouse JR, Byington RP, Bond MG, et al. Pravastatin, lipids, and atherosclerosis in the carotid arteries: Design features of a clinical trial with carotid atherosclerosis outcome (PLAC II). Control Clin Trials. 1992;13:495-506.
9. Salonen R, Nyyssonen K, Porkkala E, et al. Kuopio Atherosclerosis Prevention Study (KAPS). A population-based primary preventive trial of the effect of LDL lowering on atherosclerotic progression in carotid and femoral arteries. Circ. 1995;92:1758-1764. -
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Pravastatin sodium tablets USP are supplied as:
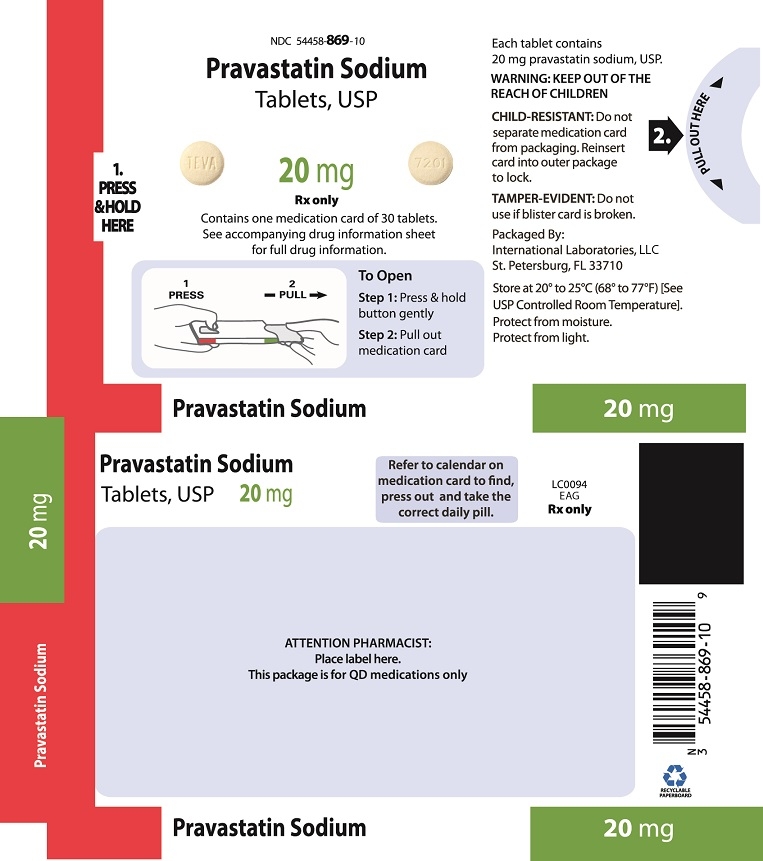
20 mg tablets: Light-yellow, unscored, round tablet, debossed “TEVA” on one side and “7201” on the other side in adherence packages of 30 (NDC: 54458-869-10).
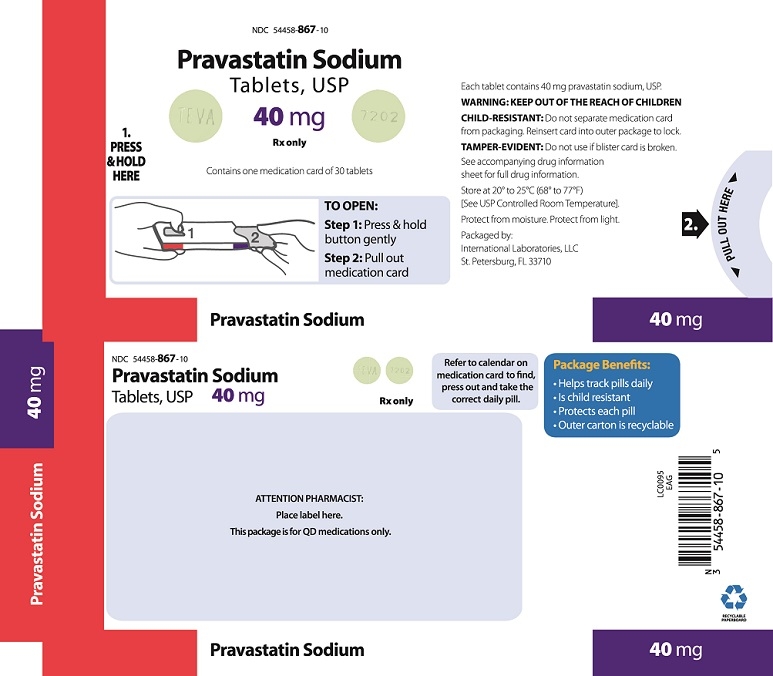
40 mg tablets: Light-green, unscored, round tablet, debossed “TEVA” on one side and “7202” on the other side in adherence packages of 30 (NDC: 54458-867-10).
-
17 PATIENT COUNSELING INFORMATION
Muscle Pain
Patients should be advised to report promptly unexplained muscle pain, tenderness or weakness, particularly if accompanied by malaise or fever or if these muscle signs or symptoms persist after discontinuing pravastatin sodium [see Warnings and Precautions (5.1)].
Liver Enzymes
It is recommended that liver enzyme tests be performed before the initiation of pravastatin sodium, and thereafter when clinically indicated. All patients treated with pravastatin sodium should be advised to promptly report any symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine, or jaundice [see Warnings and Precautions (5.2)].
Embryofetal Toxicity
Advise females of reproductive potential of the risk to a fetus, to use effective contraception during treatment, and to inform their healthcare provider of a known or suspected pregnancy [see Contraindications (4.3), Use in Specific Populations (8.1, 8.3)].
Lactation
Advise women not to breastfeed during treatment with pravastatin sodium [see Contraindications (4.4), Use in Specific Populations (8.2)].
Manufactured By:
Teva Czech Industries, s.r.o.
Opava-Komarov, Czech Republic
or
Teva Pharmaceutical Ind. Ltd.
Jerusalem, 9777402, Israel
Packaged by:
International Laboratories, LLC
St. Petersburg, FL 33710
Rev. 04/17 LI0073
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PRAVASTATIN SODIUM
pravastatin sodium tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 54458-869 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PRAVASTATIN SODIUM (UNII: 3M8608UQ61) (PRAVASTATIN - UNII:KXO2KT9N0G) PRAVASTATIN SODIUM 20 mg Inactive Ingredients Ingredient Name Strength FERRIC OXIDE YELLOW (UNII: EX438O2MRT) CALCIUM PHOSPHATE, DIBASIC, ANHYDROUS (UNII: L11K75P92J) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) CROSPOVIDONE (15 MPA.S AT 5%) (UNII: 68401960MK) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE K30 (UNII: U725QWY32X) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color YELLOW (light-yellow) Score no score Shape ROUND Size 8mm Flavor Imprint Code TEVA;7201 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54458-869-10 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 05/01/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076056 05/01/2015 PRAVASTATIN SODIUM
pravastatin sodium tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 54458-867 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PRAVASTATIN SODIUM (UNII: 3M8608UQ61) (PRAVASTATIN - UNII:KXO2KT9N0G) PRAVASTATIN SODIUM 40 mg Inactive Ingredients Ingredient Name Strength FD&C BLUE NO. 1 (UNII: H3R47K3TBD) D&C YELLOW NO. 10 (UNII: 35SW5USQ3G) CALCIUM PHOSPHATE, DIBASIC, ANHYDROUS (UNII: L11K75P92J) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) CROSPOVIDONE (15 MPA.S AT 5%) (UNII: 68401960MK) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE K30 (UNII: U725QWY32X) SODIUM STEARYL FUMARATE (UNII: 7CV7WJK4UI) Product Characteristics Color GREEN (light-green) Score no score Shape ROUND Size 10mm Flavor Imprint Code TEVA;7202 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 54458-867-10 30 in 1 BLISTER PACK; Type 0: Not a Combination Product 05/01/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076056 05/01/2015 Labeler - International Laboratories, LLC (023569924)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.