Bicalutamide by Apotex Corp. / Intas Pharmaceuticals Limited BICALUTAMIDE tablet
Bicalutamide by
Drug Labeling and Warnings
Bicalutamide by is a Prescription medication manufactured, distributed, or labeled by Apotex Corp., Intas Pharmaceuticals Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use bicalutamide safely and effectively. See full prescribing information for bicalutamide.
Bicalutamide Tablets USP for Oral use
Initial U.S. Approval : 1995INDICATIONS AND USAGE
- Bicalutamide tablets 50 mg is an androgen receptor inhibitor indicated for use in combination therapy with a luteinizing hormone-releasing hormone (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of the prostate.
- Bicalutamide tablets 150 mg daily is not approved for use alone or with other treatments. (1)
DOSAGE AND ADMINISTRATION
The recommended dose for bicalutamide therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). (2)
DOSAGE FORMS AND STRENGTHS
50 mg tablets (3)
WARNINGS AND PRECAUTIONS
- Severe hepatic injury and fatal hepatic failure have been observed. Monitor serum transaminase levels prior to starting treatment with bicalutamide, at regular intervals for the first four months of treatment and periodically thereafter, and for symptoms or signs suggestive of hepatic dysfunction. Use bicalutamide with caution in patients with hepatic impairment. (5.1)
- Gynecomastia and breast pain have been reported during treatment with bicalutamide 150 mg when used as a single agent. (5.2)
- Bicalutamide is used in combination with an LHRH agonist. LHRH agonists have been shown to cause a reduction in glucose tolerance in males. Consideration should be given to monitoring blood glucose in patients receiving bicalutamide in combination with LHRH agonists. (5.3)
- Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate for clinical progression if PSA increases. (5.4)
ADVERSE REACTIONS
Adverse reactions that occurred in more than 10% of patients receiving bicalutamide plus an LHRH-A were: hot flashes, pain (including general, back, pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral edema, dyspnea, diarrhea, hematuria, nocturia and anemia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact at 1-866-941-7875 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
Pediatric patients: Efficacy has not been demonstrated for the treatment of familial male-limited precocious puberty (testotoxicosis). (8.4)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2012
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1. INDICATIONS AND USAGE
2. DOSAGE AND ADMINISTRATION
2.1. Dosage Adjustment in Renal Impairment
2.2. Dosage Adjustment in Hepatic Impairment
3. DOSAGE FORMS & STRENGTHS
4. CONTRAINDICATIONS
4.1. Hypersensitivity
4.2. Women
4.3. Pregnancy
5. WARNINGS AND PRECAUTIONS
5.1. Hepatitis
5.2. Gynecomastia and Breast Pain
5.3. Glucose Tolerance
5.4. Laboratory Tests
6. ADVERSE REACTIONS
6.1. Clinical Trials Experience
6.2. Postmarketing Experience
7. DRUG INTERACTIONS
8. USE IN SPECIFIC POPULATIONS
8.1. Pregnancy
8.3. Nursing Mothers
8.4. Pediatric Use
8.5. Geriatric Use
8.6. Hepatic Impairment
8.7. Renal Impairment
8.8. Women
10. OVERDOSAGE
11. DESCRIPTION
12. CLINICAL PHARMACOLOGY
12.1. Mechanism of Action
12.3. Pharmacokinetics
13. NONCLINICAL TOXICOLOGY
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
14. CLINICAL STUDIES
14.1. Bicalutamide Tablets 50 mg Daily in Combination with an LHRH-A
14.2. Safety Data from Clinical Studies using Bicalutamide Tablets 150 mg
16. HOW SUPPLIED/STORAGE AND HANDLING
16.1. Storage and Handling
17. PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1. INDICATIONS AND USAGE
Bicalutamide tablets 50 mg daily is indicated for use in combination therapy with a luteinizing hormone-releasing hormone (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of the prostate.
Bicalutamide tablets 150 mg daily is not approved for use alone or with other treatments [see Clinical Studies (14.2)].
-
2. DOSAGE AND ADMINISTRATION
The recommended dose for bicalutamide tablets therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening), with or without food. It is recommended that bicalutamide tablets be taken at the same time each day. Treatment with bicalutamide tablets should be started at the same time as treatment with an LHRH analog.
2.1. Dosage Adjustment in Renal Impairment
No dosage adjustment is necessary for patients with renal impairment [see Use in Specific Populations (8.7)].
2.2. Dosage Adjustment in Hepatic Impairment
No dosage adjustment is necessary for patients with mild to moderate hepatic impairment. In patients with severe liver impairment (n=4), although there was a 76% increase in the half-life (5.9 and 10.4 days for normal and impaired patients, respectively) of the active enantiomer of bicalutamide no dosage adjustment is necessary [see Use in Specific Populations (8.6)].
- 3. DOSAGE FORMS & STRENGTHS
-
4. CONTRAINDICATIONS
4.1. Hypersensitivity
Bicalutamide is contraindicated in any patient who has shown a hypersensitivity reaction to the drug or any of the tablet’s components. Hypersensitivity reactions including angioneurotic edema and urticaria have been reported [see Adverse Reactions (6.2)].
4.3. Pregnancy
Bicalutamide may cause fetal harm when administered to a pregnant woman. Bicalutamide is contraindicated in women, including those who are or may become pregnant. There are no studies in pregnant women using bicalutamide. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be appraised of the potential hazard to the fetus [see Use in Specific Populations (8.1)].
-
5. WARNINGS AND PRECAUTIONS
5.1. Hepatitis
Cases of death or hospitalization due to severe liver injury (hepatic failure) have been reported post-marketing in association with the use of bicalutamide. Hepatotoxicity in these reports generally occurred within the first three to four months of treatment. Hepatitis or marked increases in liver enzymes leading to drug discontinuation occurred in approximately 1% of bicalutamide patients in controlled clinical trials.
Serum transaminase levels should be measured prior to starting treatment with bicalutamide, at regular intervals for the first four months of treatment, and periodically thereafter. If clinical symptoms or signs suggestive of liver dysfunction occur (e.g., nausea, vomiting, abdominal pain, fatigue, anorexia, “flu-like” symptoms, dark urine, jaundice, or right upper quadrant tenderness), the serum transaminases, in particular the serum ALT, should be measured immediately. If at any time a patient has jaundice, or their ALT rises above two times the upper limit of normal, bicalutamide should be immediately discontinued with close follow-up of liver function.
5.2. Gynecomastia and Breast Pain
In clinical trials with bicalutamide 150 mg as a single agent for prostate cancer, gynecomastia and breast pain have been reported in up to 38% and 39% of patients, respectively.
5.3. Glucose Tolerance
A reduction in glucose tolerance has been observed in males receiving LHRH agonists. This may manifest as diabetes or loss of glycemic control in those with pre-existing diabetes. Consideration should therefore be given to monitoring blood glucose in patients receiving bicalutamide in combination with LHRH agonists.
5.4. Laboratory Tests
Regular assessments of serum Prostate Specific Antigen (PSA) may be helpful in monitoring the patient’s response.
If PSA levels rise during bicalutamide therapy, the patient should be evaluated for clinical progression. For patients who have objective progression of disease together with an elevated PSA, a treatment-free period of antiandrogen, while continuing the LHRH analog, may be considered.
-
6. ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1. Clinical Trials Experience
In patients with advanced prostate cancer treated with bicalutamide in combination with an LHRH analog, the most frequent adverse reaction was hot flashes (53%).
In the multicenter, double-blind, controlled clinical trial comparing bicalutamide 50 mg once daily with flutamide 250 mg three times a day, each in combination with an LHRH analog, the following adverse reactions with an incidence of 5% or greater, regardless of causality, have been reported.
Table 1. Incidence of Adverse Reactions (≥5% in Either Treatment Group) Regardless of Causality Treatment Group Number of Patients (%) Body System
Adverse ReactionBicalutamide Plus
LHRH Analog
(n=401)Flutamide Plus
LHRH Analog
(n=407)Body as a Whole Pain (General) 142 (35) 127 (31) Back Pain 102 (25) 105 (26) Asthenia 89 (22) 87 (21) Pelvic Pain 85 (21) 70 (17) Infection 71 (18) 57 (14) Abdominal Pain 46 (11) 46 (11) Chest Pain 34 (8) 34 (8) Headache 29 (7) 27 (7) Flu Syndrome 28 (7) 30 (7) Cardiovascular Hot Flashes 211 (53) 217 (53) Hypertension 34 (8) 29 (7) Digestive Constipation 87 (22) 69 (17) Nausea 62 (15) 58 (14) Diarrhea 49 (12) 107 (26) Increased Liver Enzyme Test 30 (7) 46 (11) Dyspepsia 30 (7) 23 (6) Flatulence 26 (6) 22 (5) Anorexia 25 (6) 29 (7) Vomiting 24 (6) 32 (8) Hemic and Lymphatic Anemia 45 (11) 53 (13) Metabolic and Nutritional Peripheral Edema 53 (13) 42 (10) Weight Loss 30 (7) 39 (10) Hyperglycemia 26 (6) 27 (7) Alkaline Phosphatase Increased 22 (5) 24 (6) Weight Gain 22 (5) 18 (4) Muscoloskeletal Bone Pain 37 (9) 43 (11) Myasthenia 27 (7) 19 (5) Arthritis 21 (5) 29 (7) Pathological Fracture 17 (4) 32 (8) Nervous System Dizziness 41 (10) 35 (9) Paresthesia 31 (8) 40 (10) Insomnia 27 (7) 39 (10) Anxiety 20 (5) 9 (2) Depression 16 (4) 33 (8) Respiratory System Dyspnea 51 (13) 32 (8) Cough Increased 33 (8) 24 (6) Pharyngitis 32 (8) 23 (6) Bronchitis 24 (6) 22 (3) Pneumonia 18 (4) 19 (5) Rhinitis 15 (4) 22 (5) Skin and Appendages Rash 35 (9) 30 (7) Sweating 25 (6) 20 (5) Urogenital Nocturia 49 (12) 55 (14) Hematuria 48 (12) 26 (6) Urinary Tract Infection 35 (9) 36 (9) Gynecomastia 36 (9) 30 (7) Impotence 27 (7) 35 (9) Breast Pain 23 (6) 15 (4) Urinary Frequency 23 (6) 29 (7) Urinary Retention 20 (5) 14 (3) Urinary Impaired 19 (5) 15 (4) Urinary Incontinence 15 (4) 32 (8) Other adverse reactions (greater than or equal to 2%, but less than 5%) reported in the bicalutamide-LHRH analog treatment group are listed below by body system and are in order of decreasing frequency within each body system regardless of causality.
Cardiovascular:
Angina Pectoris; Congestive Heart Failure; Myocardial Infarct; Heart Arrest; Coronary Artery Disorder; Syncope
Digestive:
Melena; Rectal Hemorrhage; Dry Mouth; Dysphagia; Gastrointestinal Disorder; Periodontal Abscess; Gastrointestinal Carcinoma
6.2. Postmarketing Experience
The following adverse reactions have been identified during postapproval use of bicalutamide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Uncommon cases of hypersensitivity reactions, including angioneurotic edema and urticaria have been seen [see Contraindications (4.1)]. Cases of interstitial lung disease (some fatal), including interstitial pneumonitis and pulmonary fibrosis, have been reported with bicalutamide. Interstitial lung disease has been reported most often at doses greater than 50 mg. A few cases of fatal hepatic failure have been reported.
Reduction in glucose tolerance, manifesting as diabetes or a loss of glycemic control in those with pre-existing diabetes, has been reported during treatment with LHRH agonists.
-
7. DRUG INTERACTIONS
Clinical studies have not shown any drug interactions between bicalutamide and LHRH analogs (goserelin or leuprolide). There is no evidence that bicalutamide induces hepatic enzymes.
In vitro studies have shown that R-bicalutamide is an inhibitor of CYP 3A4 with lesser inhibitory effects on CYP 2C9, 2C19 and 2D6 activity. Clinical studies have shown that with co-administration of bicalutamide, mean midazolam (a CYP 3A4 substrate) levels may be increased 1.5 fold (for Cmax) and 1.9 fold (for AUC). Hence, caution should be exercised when bicalutamide is co-administered with CYP 3A4 substrates.
In vitro protein-binding studies have shown that bicalutamide can displace coumarin anticoagulants from binding sites. Prothrombin times should be closely monitored in patients already receiving coumarin anticoagulants who are started on bicalutamide and adjustment of the anticoagulant dose may be necessary.
-
8. USE IN SPECIFIC POPULATIONS
8.1. Pregnancy
PREGNANCY CATEGORY X
[see Contraindications (4.3)]. Based on its mechanism of action, bicalutamide may cause fetal harm when administered to a pregnant woman. Bicalutamide is contraindicated in women, including those who are or may become pregnant. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
While there are no human data on the use of bicalutamide in pregnancy and bicalutamide is not for use in women, it is important to know that maternal use of an androgen receptor inhibitor could affect development of the fetus.
In animal reproduction studies, male offspring of rats receiving doses of 10 mg/kg/day (approximately 2/3 of clinical exposure at the recommended dose) and above, were observed to have reduced anogenital distance and hypospadias. These pharmacological effects have been observed with other antiandrogens. No other teratogenic effects were observed in rabbits receiving doses up to 200 mg/kg/day (approximately 1/3 of clinical exposure at the recommended dose) or rats receiving doses up to 250 mg/kg/day (approximately 2 times the clinical exposure at the recommended dose).
8.4. Pediatric Use
The safety and effectiveness of bicalutamide in pediatric patients have not been established.
Bicalutamide orodispersible tablet was studied in combination with anastrozole orodispersible tablet in an open-label, non-comparative, multi-center study that assessed the efficacy and safety of this combination regimen over 12 months in the treatment of gonadotropin-independent precocious puberty in boys with familial male-limited precocious puberty, also known as testotoxicosis. Patients were enrolled in the study if they had a baseline age ≥ 2 years and a diagnosis of testotoxicosis based on clinical features of progressive precocious puberty, symmetrical testicular enlargement, advanced bone age, pubertal levels of serum testosterone, prepubertal pattern of gonadotropin secretion following a GnRH stimulation test, and absence of other clinical and biochemical causes of testosterone excess. Thirteen out of the 14 patients enrolled completed 12 months of combination treatment (one patient was lost to follow-up). If central precocious puberty (CPP) developed an LHRH analog was to be added. Four patients were diagnosed with CPP during the 12-month study and received LHRH analog treatment and 2 additional patients were diagnosed at the end of the 12 months and received treatment subsequently. Mean ± SD characteristics at baseline were as follows: chronological age: 3.9±1.9 years; bone age 8.8±2.5; bone age/chronological age ratio: 2.06 ± 0.51; growth rate (cm/yr): 10.81 ± 4.22; growth rate standard deviation score (SDS): 0.41 ± 1.36.
The starting bicalutamide dose was 12.5 mg. Bicalutamide was titrated in each patient until steady-state R-bicalutamide (the active isomer of bicalutamide) trough plasma concentration reached 5 to 15 mcg/mL, which is the range of therapeutic concentrations achieved in adults with prostate cancer following the administration of the currently approved bicalutamide dose of 50 mg. The starting daily dose of anastrozole was 0.5 mg. Anastrozole was independently titrated in each patient until it reached at steady-state a serum estradiol concentration of <10 pmol/L (2.7 pg/mL). The following ascending doses were used for bicalutamide: 12.5 mg, 25 mg, 50 mg, and 100 mg. For anastrozole there were two ascending doses: 0.5 mg and 1 mg. At the end of the titration phase 1 patient was on 12.5 mg bicalutamide, 8 patients were on 50 mg bicalutamide, and 4 patients were on 100 mg bicalutamide; 10 patients were on 0.5 mg anastrozole and 3 patients were on 1 mg anastrozole. In the majority of patients, steady-state trough concentrations of R-bicalutamide appeared to be attained by Day 21 with once daily dosing. Steady-state trough plasma anastrozole concentrations appeared to be attained by Day 8.
The primary efficacy analysis of the study was to assess the change in growth rate after 12 months of treatment, relative to the growth rate during the ≥6 months prior to entering the study. Pre-study growth rates were obtained retrospectively. There was no statistical evidence that the growth rate was reduced during treatment. During bicalutamide /anastrozole treatment the mean growth rate (cm/yr) decreased by 1.6 cm/year, 95% CI (-4.7 to 1.5) p=0.28; the mean growth rate SDS decreased by 0.1 SD, 95% CI (–1.2 to 1.0) p=0.88. Table 2 shows descriptive data for growth rates for the overall population and for subgroups defined by history of previous treatment for testotoxicosis with ketoconazole, spironolactone, anastrozole or other aromatase inhibitors.
Table 2. Growth rates - * Change compared to pre-study growth rate
- † PT = Previous treatment for testotoxicosis with ketoconazole, spironolactone, anastrazole or other aromatase inhibitors
- ‡ Median calculated as midpoint of 3rd and 4th ranked observations
- § NPT = no previous treatment for testotoxicosis with ketoconazole, spironolactone, anastrozole or other aromatase inhibitors
Endpoint Analysis population Pre-study Mean Change from pre-study to 12 months % patients with growth reduction* Mean Median (Min, Max) Growth rate (cm/yr) All treated (n=13) 10.8 -1.6 -2.8 (-7.4, 8.4) 9/13 (69%) PT†
(n=6)10.3 -0.2 -2.6‡ (-7.2, 8.4) 4/6 (67%) NPT§
(n=7)11.2 -2.8 -2.8 (-7.4, 1.1) 5/7 (71%) Growth rate
(SD units)All treated
(n=13)0.4 -0.1 -0.4 (-2.7, 3.5) 9/13 (69%) PT†
(n=6)-0.1 +0.7 -0.2‡ (-1.6, 3.5) 4/6 (67%) NPT §
(n=7)0.8 -0.7 -0.4 (-2.7, 0.5) 5/7 (71%) Total testosterone concentrations increased by a mean of 5 mmol/L over the 12 months of treatment from a baseline mean of 10 mmol/L. Estradiol concentrations were at or below the level of quantification (9.81 pmol/L) for 11 of 12 patients after 12 months of treatment. Six of the 12 patients started treatment at an estradiol concentration below the level of quantification.
There were no deaths, serious adverse events, or discontinuations due to adverse events during the study. Of the 14 patients exposed to study treatment, 13 (92.9%) experienced at least one adverse event. The most frequently reported (>3 patients) adverse events were gynecomastia (7/14, 50%), central precocious puberty (6/14, 43%), vomiting (5/14, 36%), headache (3/14, 21%), pyrexia (3/14, 21%) and upper respiratory tract infection (3/14, 21%). Adverse reactions considered possibly related to bicalutamide by investigators included gynecomastia (6/14, 43%), central precocious puberty (2/14, 14%), breast tenderness (2/14, 14%), breast pain (1/14, 7%), asthenia (1/14, 7%), increased alanine aminotransferase [ALT] (1/14, 7%), increased aspartate aminotransferase [AST] (1/14, 7%), and musculoskeletal chest pain (1/14, 7%). Headache was the only adverse reaction considered possibly related to anastrazole by investigators. For the patient who developed elevated ALT and AST, the elevation was <3X ULN, and returned to normal without stopping treatment; there was no concomitant elevation in total bilirubin.
8.5. Geriatric Use
In two studies in patients given 50 or 150 mg daily, no significant relationship between age and steady-state levels of total bicalutamide or the active R-enantiomer has been shown.
8.6. Hepatic Impairment
Bicalutamide should be used with caution in patients with moderate-to-severe hepatic impairment. Bicalutamide is extensively metabolized by the liver. Limited data in subjects with severe hepatic impairment suggest that excretion of bicalutamide may be delayed and could lead to further accumulation. Periodic liver function tests should be considered for hepatic-impaired patients on long-term therapy [see Warnings and Precautions (5.1)].
No clinically significant difference in the pharmacokinetics of either enantiomer of bicalutamide was noted in patients with mild-to-moderate hepatic disease as compared to healthy controls. However, the half-life of the R-enantiomer was increased approximately 76% (5.9 and 10.4 days for normal and impaired patients, respectively) in patients with severe liver disease (n=4).
-
10. OVERDOSAGE
Long-term clinical trials have been conducted with dosages up to 200 mg of bicalutamide daily and these dosages have been well tolerated. A single dose of bicalutamide that results in symptoms of an overdose considered to be life threatening has not been established.
There is no specific antidote; treatment of an overdose should be symptomatic.
In the management of an overdose with bicalutamide, vomiting may be induced if the patient is alert. It should be remembered that, in this patient population, multiple drugs may have been taken. Dialysis is not likely to be helpful since bicalutamide is highly protein bound and is extensively metabolized. General supportive care, including frequent monitoring of vital signs and close observation of the patient, is indicated.
-
11. DESCRIPTION
Bicalutamide tablets contain 50 mg of bicalutamide, a non-steroidal androgen receptor inhibitor with no other known endocrine activity. The chemical name is propanamide, N [4 cyano-3-(trifluoromethyl)phenyl]-3-[(4-fluorophenyl)sulfonyl]-2-hydroxy-2-methyl-,(+-). The structural and empirical formulas are:
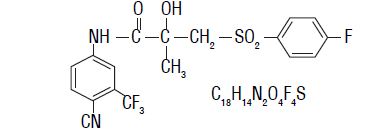
Bicalutamide has a molecular weight of 430.37. The pKa’ is approximately 12. Bicalutamide is a fine white to off-white powder which is practically insoluble in water at 37°C (5 mg per 1000 mL), slightly soluble in chloroform and absolute ethanol, sparingly soluble in methanol, and soluble in acetone and tetrahydrofuran.
Bicalutamide is a racemate with its antiandrogenic activity being almost exclusively exhibited by the R-enantiomer of bicalutamide; the S-enantiomer is essentially inactive.
The inactive ingredients of bicalutamide tablets are lactose monohydrate, magnesium stearate, hypromellose E5, polyethylene glycol 400, povidone K 30, sodium starch glycolate, and titanium dioxide.
Bicalutamide tablets 50 mg meets USP Dissolution Test 2.
-
12. CLINICAL PHARMACOLOGY
12.1. Mechanism of Action
Bicalutamide is a non-steroidal androgen receptor inhibitor. It competitively inhibits the action of androgens by binding to cytosol androgen receptors in the target tissue. Prostatic carcinoma is known to be androgen sensitive and responds to treatment that counteracts the effect of androgen and/or removes the source of androgen.
When bicalutamide is combined with luteinizing hormone releasing hormone (LHRH) analog therapy, the suppression of serum testosterone induced by the LHRH analog is not affected. However, in clinical trials with bicalutamide as a single agent for prostate cancer, rises in serum testosterone and estradiol have been noted.
In a subset of patients who have been treated with bicalutamide and an LHRH agonist, and who discontinue bicalutamide therapy due to progressive advanced prostate cancer, a reduction in Prostate Specific Antigen (PSA) and/or clinical improvement (antiandrogen withdrawal phenomenon) may be observed.
12.3. Pharmacokinetics
Absorption
Bicalutamide is well-absorbed following oral administration, although the absolute bioavailability is unknown. Co-administration of bicalutamide with food has no clinically significant effect on rate or extent of absorption.
Metabolism/Elimination
Bicalutamide undergoes stereospecific metabolism. The S (inactive) isomer is metabolized primarily by glucuronidation. The R (active) isomer also undergoes glucuronidation but is predominantly oxidized to an inactive metabolite followed by glucuronidation. Both the parent and metabolite glucuronides are eliminated in the urine and feces. The S-enantiomer is rapidly cleared relative to the R-enantiomer, with the R-enantiomer accounting for about 99% of total steady-state plasma levels.
Pharmacokinetics of the active enantiomer of bicalutamide in normal males and patients with prostate cancer are presented in Table 3.
Table 3 Parameter Mean Standard Deviation Normal Males (n=30) Apparent Oral Clearance (L/hr) 0.320 0.103 Single Dose Peak Concentration (μg/mL) 0.768 0.178 Single Dose Time to Peak Concentration (hours) 31.3 14.6 Half-life (days) 5.8 2.29 Patients with Prostate Cancer (n=40) Css (μg/mL) 8.939 3.504 -
13. NONCLINICAL TOXICOLOGY
13.1. Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year oral carcinogenicity studies were conducted in both male and female rats and mice at doses of 5, 15 or 75 mg/kg/day of bicalutamide. A variety of tumor target organ effects were identified and were attributed to the antiandrogenicity of bicalutamide, namely, testicular benign interstitial (Leydig) cell tumors in male rats at all dose levels (the steady-state plasma concentration with the 5 mg/kg/day dose is approximately 2/3 human therapeutic concentrations1) and uterine adenocarcinoma in female rats at 75 mg/kg/day (approximately 1 1/2 times the human therapeutic concentrations1). There is no evidence of Leydig cell hyperplasia in patients; uterine tumors are not relevant to the indicated patient population.
A small increase in the incidence of hepatocellular carcinoma in male mice given 75 mg/kg/day of bicalutamide (approximately 4 times human therapeutic concentrations1) and an increased incidence of benign thyroid follicular cell adenomas in rats given 5 mg/kg/day (approximately 2/3 human therapeutic concentrations1) and above were recorded. These neoplastic changes were progressions of non-neoplastic changes related to hepatic enzyme induction observed in animal toxicity studies. Enzyme induction has not been observed following bicalutamide administration in man. There were no tumorigenic effects suggestive of genotoxic carcinogenesis.
A comprehensive battery of both in vitro and in vivo genotoxicity tests (yeast gene conversion, Ames, E.coli, CHO/HGPRT, human lymphocyte cytogenetic, mouse micronucleus, and rat bone marrow cytogenetic tests) has demonstrated that bicalutamide does not have genotoxic activity.
Administration of bicalutamide may lead to inhibition of spermatogenesis. The long-term effects of bicalutamide on male fertility have not been studied.
In male rats dosed at 250 mg/kg/day (approximately 2 times human therapeutic concentrations1), the precoital interval and time to successful mating were increased in the first pairing but no effects on fertility following successful mating were seen. These effects were reversed by 7 weeks after the end of an 11-week period of dosing.
No effects on female rats dosed at 10, 50 and 250 mg/kg/day (approximately 2/3, 1 and 2 times human therapeutic concentrations, respectively1) or their female offspring were observed. Administration of bicalutamide to pregnant females resulted in feminization of the male offspring leading to hypospadias at all dose levels. Affected male offspring were also impotent.
- 1 Based on a maximum dose of 50 mg/day of bicalutamide for an average 70 kg patient.
-
14. CLINICAL STUDIES
14.1. Bicalutamide Tablets 50 mg Daily in Combination with an LHRH-A
In a multicenter, double-blind, controlled clinical trial, 813 patients with previously untreated advanced prostate cancer were randomized to receive bicalutamide 50 mg once daily (404 patients) or flutamide 250 mg (409 patients) three times a day, each in combination with LHRH analogs (either goserelin acetate implant or leuprolide acetate depot).
In an analysis conducted after a median follow-up of 160 weeks was reached, 213 (52.7%) patients treated with bicalutamide -LHRH analog therapy and 235 (57.5%) patients treated with flutamide-LHRH analog therapy had died. There was no significant difference in survival between treatment groups (see Figure 1). The hazard ratio for time to death (survival) was 0.87 (95% confidence interval 0.72 to 1.05).
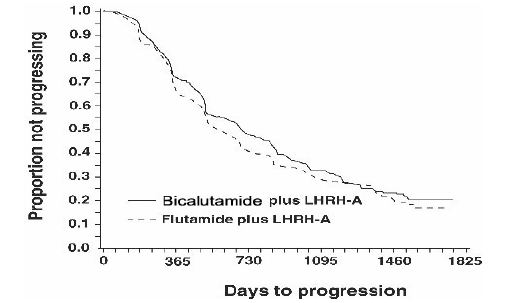
Figure 1 - The Kaplan-Meier probability of death for both antiandrogen treatment groups.
There was no significant difference in time to objective tumor progression between treatment groups (see Figure 2).
Objective tumor progression was defined as the appearance of any bone metastases or the worsening of any existing bone metastases on bone scan attributable to metastatic disease, or an increase by 25% or more of any existing measurable extraskeletal metastases. The hazard ratio for time to progression of bicalutamide plus LHRH analog to that of flutamide plus LHRH analog was 0.93 (95% confidence interval, 0.79 to 1.10).
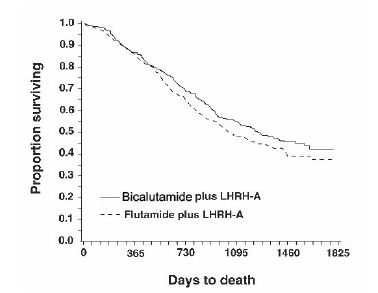
Figure 2 - Kaplan-Meier curve for time to progression for both antiandrogen treatment groups.
Quality of life was assessed with self-administered patient questionnaires on pain, social functioning, emotional well being, vitality, activity limitation, bed disability, overall health, physical capacity, general symptoms, and treatment related symptoms. Assessment of the Quality of Life questionnaires did not indicate consistent significant differences between the two treatment groups.
14.2. Safety Data from Clinical Studies using Bicalutamide Tablets 150 mg
Bicalutamide tablet 150 mg is not approved for use either alone or with other treatments.
Two identical multicenter, randomized, open-label trials comparing bicalutamide 150 mg daily monotherapy to castration were conducted in patients that had locally advanced (T3-4, NX, MO) or metastatic (M1) prostate cancer.
Monotherapy – M1 Group
Bicalutamide 150 mg daily is not approved for use in patients with M1 cancer of the prostate. Based on an interim analysis of the two trials for survival, the Data Safety Monitoring Board recommended that bicalutamide treatment be discontinued in the M1 patients because the risk of death was 25% (HR 1.25, 95% CI 0.87 to 1.81) and 31% (HR 1.31, 95% CI 0.97 to 1.77) higher in the bicalutamide treated group compared to that in the castrated group, respectively.
Locally Advanced (T3-4, NX, MO) Group
Bicalutamide 150 mg daily is not approved for use in patients with locally advanced (T3-4, NX, MO) cancer of the prostate. Following discontinuation of all M1 patients, the trials continued with the T3-4, NX, MO patients until study completion. In the larger trial (N=352), the risk of death was 25% (HR 1.25, 95% CI 0.92 to 1.71) higher in the bicalutamide group and in the smaller trial (N=140), the risk of death was 36% (HR 0.64, 95% CI, 0.39 to 1.03) lower in the bicalutamide group.
In addition to the above two studies, there are three other on-going clinical studies that provide additional safety information for bicalutamide 150 mg, a dose that is not approved for use. These are three multicenter, randomized, double-blind, parallel group trials comparing bicalutamide 150 mg daily monotherapy (adjuvant to previous therapy or under watchful waiting) with placebo, for death or time to disease progression, in a population of 8113 patients with localized or locally advanced prostate cancer.
Bicalutamide 150 mg daily is not approved for use as therapy for patients with localized prostate cancer who are candidates for watchful waiting. Data from a planned subgroup analysis of two of these trials in 1627 patients with localized prostate cancer who were under watchful waiting, revealed a trend toward decreased survival in the bicalutamide arm after a median follow-up of 7.4 years. There were 294 (37.7%) deaths in the bicalutamide treated patients versus 279 (32.9%) deaths in the placebo treated patients (localized watchful waiting group) for a hazard ratio of 1.16 (95% CI 0.99 to 1.37).
-
16. HOW SUPPLIED/STORAGE AND HANDLING
Bicalutamide tablets 50 mg are white to off-white, round, biconvex, film coated tablets, debossed ‘B 50’ on one side and plain on other side and supplied in bottles of 30 tablets (NDC: 60505-2642-3) and bottles of 100 tablets (NDC: 60505-2642-1).
-
17. PATIENT COUNSELING INFORMATION
Patients should be informed that therapy with bicalutamide and the LHRH analog should be started at the same time and that they should not interrupt or stop taking these medications without consulting their physician.
During treatment with bicalutamide, somnolence has been reported, and those patients who experience this symptom should observe caution when driving or operating machines.
Patients should be informed that diabetes, or loss of glycemic control in patients with pre-existing diabetes has been reported during treatment with LHRH agonists. Consideration should therefore be given to monitoring blood glucose in patients receiving bicalutamide in combination with LHRH agonists.
Manufactured For:
Apotex Corp.
Weston,
Florida 33326Manufactured By:
Intas Pharmaceuticals Limited,
Plot No. : 457, 458, Village – Matoda,
Bavla Road, Ta.- Sanand,
Dist.- Ahmedabad – 382 210. India.
10 5741 3 639799
Issued June 2012
-
PATIENT PACKAGE INSERT
Patient Information
Bicalutamide Tablets USP
Read the Patient Information that comes with bicalutamide tablets before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or your treatment.
What are bicalutamide tablets?
Bicalutamide is a prescription medicine called an androgen receptor inhibitor, used in combination with lutenizing hormone-releasing hormone (LHRH) medicines to treat stage D2 metatastic prostate cancer. It is not known if bicalutamide is safe and effective in children.
Who should not take bicalutamide tablets?
Do not take bicalutamide tablets if:
- you are a woman.
- you are allergic to any of the ingredients in bicalutamide tablets. See the end of this leaflet for a complete list of ingredients.
What should I tell my healthcare provider before taking bicalutamide tablets?
Before you take bicalutamide tablets, tell your healthcare provider about all your medical conditions including if you:
- are a woman (see who should not take bicalutamide tablets).
- are pregnant or think you may be pregnant.
- have liver problems.
- take a medicine to thin your blood. Ask your healthcare provider or pharmacist if you are not sure if your medicine is a blood thinner.
- have diabetes (poor blood sugar control has been reported in people taking bicalutamide in combination with LHRH medicines).
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Bicalutamide tablets and other medicines may affect each other causing side effects. Bicalutamide tablets may affect the way other medicines work, and other medicines may affect how bicalutamide tablets works.
Know the medicines you take. Keep a list of your medicines with you to show your healthcare providers when you get a new medicine.
How should I take bicalutamide tablets?
- Take bicalutamide tablets exactly as prescribed.
- Take bicalutamide tablets at the same time everyday.
- Your treatment with bicalutamide tablets should start at the same time as your treatment with the LHRH medicine.
- If you miss a dose do not take an extra dose, take the next dose at your regular time. Do not take 2 doses at the same time.
- Bicalutamide tablets can be taken with or without food.
- If you take too much bicalutamide tablets, call your healthcare provider or Poison Control Center or go to the nearest hospital emergency room right away.
- Do not stop taking bicalutamide tablets unless your healthcare provider tells you.
- Your healthcare provider may do blood tests while you take bicalutamide tablets.
- Your prostate cancer may get worse while taking bicalutamide in combination with LHRH medicines. Regular monitoring of your prostate cancer with your healthcare provider is important to determine if your disease is worse.
What should I avoid while taking bicalutamide tablets?
Driving and operating machinery. Do not drive, operate machinery, or do other dangerous activities until you know how bicalutamide tablets affect you.
What are the possible side effects of bicalutamide tablets?
Bicalutamide tablets can cause serious side effects.
Get medical help right away, if you have:
- Trouble breathing with or without a cough or fever. Some people who take bicalutamide tablets get an inflammation in the lungs called interstitial lung disease.
- An allergic reaction. Symptoms of an allergic reaction include: itching of the skin, hives (raised bumps), swelling of the face, lips, tongue, throat, or trouble swallowing.
- Yellowing of the skin and eyes (jaundice), dark urine, right upper stomach pain, nausea, vomiting, tiredness, loss of appetite, chills, fever, whole body pain. These may be symptoms of liver damage.
- Poor blood sugar control can happen in people who take bicalutamide in combination with LHRH medicines.
- Enlargement of breast (gynecomastia) and breast pain.
The most common side effects of bicalutamide tablets include:
- hot flashes, or short periods of feeling warm and sweating
- whole body pain in your back, pelvis, stomach
- feeling weak
- constipation
- infection
- nausea
- swelling in your ankles, legs or feet
- diarrhea
- blood in your urine
- waking from sleep to urinate at night
- a decrease in red blood cells (anemia)
- feeling dizzy
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of bicalutamide tablets. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
HOW SHOULD I STORE BICALUTAMIDE TABLETS?
Store bicalutamide tablets at 20 to 25°C (68 to 77°F) [See USP Controlled Room Temperature].
Keep bicalutamide tablets and all medicines out of the reach of children.
General information about the safe and effective use of bicalutamide tablets.
Medicines are sometimes prescribed for purposes other than those listed in a patient information leaflet. Do not use bicalutamide tablets for a condition for which it was not prescribed. Do not give bicalutamide tablets to other people, even if they have the same symptoms that you have. It may harm them.
This patient information leaflet summarizes the most important information about bicalutamide tablets. If you would like more information about bicalutamide tablets talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about bicalutamide tablets that is written for health professionals.
What are the ingredients in bicalutamide tablets?
Active ingredients include: bicalutamide.
Inactive ingredients include: lactose monohydrate, magnesium stearate, hypromellose E5, polyethylene glycol 400, povidone K 30, sodium starch glycolate and titanium dioxide.
-
PRINCIPAL DISPLAY PANEL
30 Tablets
NDC: 60505-2642-3
Bicalutamide
Tablets, USP50 mg
Pharmacist: Dispense with a patient
package insert.Rx Only
APOTEX CORP.
-
INGREDIENTS AND APPEARANCE
BICALUTAMIDE
bicalutamide tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 60505-2642 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength BICALUTAMIDE (UNII: A0Z3NAU9DP) (BICALUTAMIDE - UNII:A0Z3NAU9DP) BICALUTAMIDE 50 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) HYPROMELLOSE 2910 (5 MPA.S) (UNII: R75537T0T4) POLYETHYLENE GLYCOL 400 (UNII: B697894SGQ) POVIDONE K30 (UNII: U725QWY32X) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color WHITE (white to off-white,) Score no score Shape ROUND Size 7mm Flavor Imprint Code B;50 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 60505-2642-3 30 in 1 BOTTLE 2 NDC: 60505-2642-1 100 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078917 07/06/2009 Labeler - Apotex Corp. (845263701) Registrant - Apotex Corp. (845263701) Establishment Name Address ID/FEI Business Operations Intas Pharmaceuticals Limited 725927649 MANUFACTURE(60505-2642)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.