OCTREOTIDE ACETATE injection, solution
Octreotide Acetate by
Drug Labeling and Warnings
Octreotide Acetate by is a Prescription medication manufactured, distributed, or labeled by Sagent Pharmaceuticals. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OCTREOTIDE ACETATE INJECTION safely and effectively. See full prescribing information for OCTREOTIDE ACETATE INJECTION.
OCTREOTIDE ACETATE injection, for subcutaneous or intravenous use
Initial U.S. Approval: 1988RECENT MAJOR CHANGES
Warnings and Precautions, Steatorrhea and Malabsorption of Dietary Fats (5.5) 07/2024 INDICATIONS AND USAGE
Octreotide Acetate Injection is a somatostatin analogue indicated:
- Acromegaly: To reduce blood levels of growth hormone (GH) and insulin growth factor-1 (IGF-1; somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. (1.1)
- Carcinoid Tumors: For the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease. (1.2)
- Vasoactive Intestinal Peptide Tumors (VIPomas): For the treatment of profuse watery diarrhea associated with VIP-secreting tumors. (1.3)
Limitations of Use
Improvement in clinical signs and symptoms, or reduction in tumor size or rate of growth, were not shown in clinical trials performed with Octreotide Acetate Injection; these trials were not optimally designed to detect such effects. (1.4)
DOSAGE AND ADMINISTRATION
- Octreotide acetate injection may be administered subcutaneously or intravenously. (2.1)
- Acromegaly: Recommended initial octreotide acetate injection dosage is 50 mcg three times daily during the initial 2 weeks of therapy. Maintenance dose 100 mcg to 500 mcg three times daily. (2.2)
- Carcinoid Tumors: Recommended dosage range of 100 mcg to 600 mcg daily in two to four divided doses during the initial 2 weeks of therapy. (2.3)
- VIPomas: Recommended dosage range of 200 mcg to 300 mcg daily in two to four divided doses during the initial 2 weeks of therapy. (2.4)
DOSAGE FORMS AND STRENGTHS
Injection:
- Single-dose vials: 50 mcg per mL, 100 mcg per mL and 500 mcg per mL
- Multi-dose vials: 1,000 mcg per 5 mL (200 mcg per mL) and 5,000 mcg per 5 mL (1,000 mcg per mL). (3)
CONTRAINDICATIONS
- Sensitivity to this drug or any of its components. (4)
WARNINGS AND PRECAUTIONS
- Cardiac Function Abnormalities: Increased risk for higher degree of atrioventricular blocks. Consider cardiac monitoring in patients receiving octreotide acetate intravenously. Bradycardia, arrhythmias, or conduction abnormalities may occur. Use with caution in at-risk patients. Dosage adjustment of cardiac medications may be necessary. (5.1)
- Cholelithiasis and Complications of Cholelithiasis: Monitor periodically. Discontinue if complications of cholelithiasis are suspected. (5.2)
- Glucose Metabolism: Hypoglycemia or hyperglycemia may occur. Glucose monitoring is recommended and anti-diabetic treatment may need adjustment. (5.3)
- Thyroid Function: Hypothyroidism may occur. Monitor thyroid levels periodically. (5.4)
- Steatorrhea and Malabsorption of Dietary Fats: New onset steatorrhea, stool discoloration, loose stools, abdominal bloating, and weight loss may occur. If new occurrence or worsening of these symptoms are reported, evaluate for potential pancreatic exocrine insufficiency. (5.5)
ADVERSE REACTIONS
Most common adverse reactions (incidence > 10%) in patients with acromegaly are gallbladder abnormalities, sinus bradycardia, diarrhea, loose stools, nausea, abdominal discomfort, hyperglycemia, and hypothyroidism. In other patients, most common adverse reactions (incidence > 10%) are gallbladder abnormalities. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sagent Pharmaceuticals at 1-866-625-1618 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- The following drugs require monitoring and possible dose adjustment when used with octreotide acetate: cyclosporine, insulin, oral hypoglycemic agents, beta-blockers, and bromocriptine. (7)
- Lutetium Lu 177 Dotatate Injection: Discontinue octreotide acetate at least 24 hours prior to each lutetium Lu 177 dotatate dose. (7.6)
USE IN SPECIFIC POPULATIONS
- Females and Males of Reproductive Potential: Advise premenopausal females of the potential for an unintended pregnancy. (8.3)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 9/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Acromegaly
1.2 Carcinoid Tumors
1.3 Vasoactive Intestinal Peptide Tumors
1.4 Important Limitations of Use
2 DOSAGE AND ADMINISTRATION
2.1 Dosage and Administration Overview
2.2 Recommended Dosage and Monitoring for Acromegaly
2.3 Recommended Dosage and Monitoring for Carcinoid Tumors
2.4 Recommended Dosage and Monitoring for Vasoactive Intestinal Peptide Tumors
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Function Abnormalities
5.2 Cholelithiasis and Complications of Cholelithiasis
5.3 Hyperglycemia and Hypoglycemia
5.4 Thyroid Function Abnormalities
5.5 Steatorrhea and Malabsorption of Dietary Fats
5.6 Changes in Vitamin B12 Levels
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Cyclosporine
7.2 Insulin and Oral Hypoglycemic Drugs
7.3 Bromocriptine
7.4 Other Concomitant Drug Therapy
7.5 Drug Metabolism Interactions
7.6 Lutetium Lu 177 Dotatate Injection
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment-Cirrhotic Patients
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Acromegaly
Octreotide Acetate Injection is indicated to reduce blood levels of growth hormone (GH) and insulin growth factor-1 (IGF-1; somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses.
1.2 Carcinoid Tumors
Octreotide Acetate Injection is indicated for treatment of severe diarrhea and flushing episodes associated with metastatic carcinoid tumors.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosage and Administration Overview
- Octreotide acetate injection may be administered subcutaneously or intravenously. Pain with subcutaneous administration may be reduced by using the smallest volume that will deliver the desired dose. Sites should be rotated in a systematic manner.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Do not use if particulates and/or discoloration are observed. Octreotide acetate injection is not compatible in Total Parenteral Nutrition solutions because of the formation of a glycosyl octreotide conjugate which may decrease the efficacy of the product.
- Octreotide acetate injection may be diluted in volumes of 50 mL to 200 mL and infused intravenously over 15 to 30 minutes or administered by intravenous (IV) push over 3 minutes. In emergency situations (e.g., carcinoid crisis), it may be given by rapid bolus.
- Assess total and/or free T4 levels at baseline and periodically during chronic octreotide acetate injection therapy.
2.2 Recommended Dosage and Monitoring for Acromegaly
The recommended initial dosage of octreotide acetate injection is 50 mcg three times daily to be administered subcutaneously. Increase octreotide acetate injection dose based upon GH or IGF-1 levels. The goal is to achieve GH levels less than 5 ng/mL or IGF-1 levels within normal range. Monitor GH or IGF-1 every two weeks after initiating octreotide acetate injection therapy or with dosage change, and to guide titration.
The most common dosage is 100 mcg three times daily, but some patients require up to 500 mcg three times daily for maximum effectiveness. Doses greater than 300 mcg/day seldom result in additional biochemical benefit, and if an increase in dose fails to provide additional benefit, the dose should be reduced.
Octreotide acetate injection should be withdrawn yearly for approximately 4 weeks from patients who have received irradiation to assess disease activity. If GH or IGF-1 levels increase and signs and symptoms recur, octreotide acetate injection therapy may be resumed.
2.3 Recommended Dosage and Monitoring for Carcinoid Tumors
The recommended daily dosage of octreotide acetate injection during the first 2 weeks of therapy ranges from 100 to 600 mcg/day in two to four divided doses given subcutaneously (mean daily dosage is 300 mcg). In the clinical studies, the median daily maintenance dosage was approximately 450 mcg, but clinical and biochemical benefits were obtained in some patients with as little as 50 mcg, while others required doses up to 1500 mcg/day. However, experience with doses above 750 mcg/day is limited. Measurement of urinary 5- hydroxyindole acetic acid, plasma serotonin, plasma Substance P may be useful in monitoring the progress of therapy.
2.4 Recommended Dosage and Monitoring for Vasoactive Intestinal Peptide Tumors
Daily dosages of 200 mcg to 300 mcg in two to four divided doses given subcutaneously are recommended during the initial 2 weeks of therapy (range, 150 mcg to 750 mcg) to control symptoms of the disease. On an individual basis, dosage may be adjusted to achieve a therapeutic response, but usually doses above 450 mcg/day are not required. Measurement of Plasma vasoactive intestinal peptide (VIP) may be useful in monitoring the progress of therapy.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Function Abnormalities
Complete Atrioventricular Block
Patients who receive octreotide acetate intravenously may be at increased risk for higher degree atrioventricular blocks. In post marketing reports, complete atrioventricular block was reported in patients receiving IV octreotide acetate during surgical procedures. In the majority of patients, octreotide acetate was given at higher than recommended doses and/or as a continuous IV infusion. The safety of continuous IV infusion has not been established in patients receiving octreotide acetate for the approved indications. Consider cardiac monitoring in patients receiving octreotide acetate intravenously.
Other Cardiac Conduction Abnormalities
Other cardiac conduction abnormalities have occurred during treatment with octreotide acetate. In acromegalic patients, bradycardia (< 50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias occurred in 9% of patients during octreotide acetate therapy [see Adverse Reactions (6)]. Other electrocardiogram (ECG) changes observed included QT prolongation, axis shifts, early repolarization, low voltage, R/S transition, and early R-wave progression. These ECG changes are not uncommon in acromegalic patients. Dose adjustments in drugs such as beta-blockers that have bradycardia effects may be necessary. In one acromegalic patient with severe congestive heart failure (CHF), initiation of octreotide acetate therapy resulted in worsening of CHF with improvement when drug was discontinued. Confirmation of a drug effect was obtained with a positive rechallenge.
5.2 Cholelithiasis and Complications of Cholelithiasis
Octreotide acetate may inhibit gallbladder contractility and decrease bile secretion, which may lead to gallbladder abnormalities or sludge. Acute cholecystitis, ascending cholangitis, biliary obstruction, cholestatic hepatitis, or pancreatitis have been reported with octreotide acetate therapy. In clinical trials (primarily patients with acromegaly or psoriasis), the incidence of biliary tract abnormalities was 63% (27% gallstones, 24% sludge without stones, 12% biliary duct dilatation). The incidence of stones or sludge in patients who received octreotide acetate for 12 months or longer was 52%. Less than 2% of patients treated with octreotide acetate for 1 month or less developed gallstones. One patient developed ascending cholangitis during octreotide acetate therapy and died. If complications of cholelithiasis are suspected, discontinue octreotide acetate and treat appropriately.
5.3 Hyperglycemia and Hypoglycemia
Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and GH, which may result in hypoglycemia or hyperglycemia. The hypoglycemia or hyperglycemia which occurs during octreotide acetate therapy is usually mild but may result in overt diabetes mellitus or necessitate dose changes in insulin or other anti-diabetic agents. Hypoglycemia and hyperglycemia occurred on octreotide acetate in 3% and 16% of acromegalic patients, respectively [see Adverse Reactions (6)]. Severe hyperglycemia, subsequent pneumonia, and death following initiation of octreotide acetate therapy was reported in one patient with no history of hyperglycemia.
Monitor glucose levels during octreotide acetate therapy. Adjust dosing of insulin or other anti-diabetic therapy accordingly.
5.4 Thyroid Function Abnormalities
Octreotide suppresses secretion of thyroid stimulating hormone (TSH), which may result in hypothyroidism. Baseline and periodic assessment of thyroid function (TSH, total, and/or free T4) is recommended during chronic therapy [see Adverse Reactions (6)].
5.5 Steatorrhea and Malabsorption of Dietary Fats
New onset steatorrhea, stool discoloration and loose stools have been reported in patients receiving somatostatin analogs, including octreotide acetate. Somatostatin analogs reversibly inhibit secretion of pancreatic enzymes and bile acids, which may result in malabsorption of dietary fats and subsequent symptoms of steatorrhea, loose stools, abdominal bloating, and weight loss. If new occurrence or worsening of these symptoms are reported in patients receiving octreotide acetate, evaluate patients for potential pancreatic exocrine insufficiency and manage accordingly.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Complete Atrioventricular Block [see Warnings and Precautions (5.1)]
- Cholelithiasis and Complications of Cholelithiasis [see Warnings and Precautions (5.2)]
- Hyperglycemia and Hypoglycemia [see Warnings and Precautions (5.3)]
- Thyroid Function Abnormalities [see Warnings and Precautions (5.4)]
- Steatorrhea and Malabsorption of Dietary Fats [see Warnings and Precautions (5.5)]
- Changes in Vitamin B12 Levels [see Warnings and Precautions (5.6)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic octreotide acetate therapy [see Warnings and Precautions (5.1)]. In clinical trials (primarily patients with acromegaly or psoriasis), the incidence of biliary tract abnormalities was 63% (27% gallstones, 24% sludge without stones, 12% biliary duct dilatation). The incidence of stones or sludge in patients who received octreotide acetate for 12 months or longer was 52%. Less than 2% of patients treated with octreotide acetate for 1 month or less developed gallstones.
Cardiac
In acromegalics, sinus bradycardia (< 50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during octreotide acetate therapy [see Warnings and Precautions (5.1)].
Gastrointestinal
Diarrhea, loose stools, nausea, and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies. 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with carcinoid tumors and VIPomas.
The frequency of these symptoms was not dose related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness, and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 8% and 4% required initiation of thyroid replacement therapy during octreotide acetate therapy [see Warnings and Precautions (5.4)]. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6%, and dizziness in 5%. Pancreatitis was also observed [see Warnings and Precautions (5.2)].
Other Adverse Events 1% to 4%
Other events, each observed in 1% to 4% of patients, included fatigue, weakness, pruritus, joint pain, backache, urinary tract infection, cold symptoms, flu symptoms, injection site hematoma, bruise, edema, flushing, blurred vision, pollakiuria, fat malabsorption, hair loss, visual disturbance, and depression.
Anaphylactoid reactions, including anaphylactic shock, have been reported in several patients receiving octreotide acetate.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of octreotide acetate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hepatobiliary: cholelithiasis, cholecystitis, cholangitis and pancreatitis, which have sometimes required cholecystectomy
Gastrointestinal: intestinal obstruction, pancreatic exocrine insufficiency
Hematologic: thrombocytopenia
-
7 DRUG INTERACTIONS
7.1 Cyclosporine
Octreotide has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
7.2 Insulin and Oral Hypoglycemic Drugs
Octreotide inhibits the secretion of insulin and glucagon. Therefore, blood glucose levels should be monitored when octreotide acetate treatment is initiated or when the dose is altered and anti-diabetic treatment should be adjusted accordingly.
7.3 Bromocriptine
Concomitant administration of octreotide and bromocriptine increases the availability of bromocriptine.
7.4 Other Concomitant Drug Therapy
Concomitant administration of bradycardia-inducing drugs (e.g., beta-blockers) may have an additive effect on the reduction of heart rate associated with octreotide. Dose adjustments of concomitant medication may be necessary.
Octreotide has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs.
7.5 Drug Metabolism Interactions
Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of GH. Since it cannot be excluded that octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The limited data with octreotide acetate in pregnant women are insufficient to inform a drug-associated risk for major birth defects and miscarriage. In animal reproduction studies, no adverse developmental-effects were observed with IV administration of octreotide to pregnant rats and rabbits during organogenesis at doses 7- and 13-times, respectively the maximum recommended human dose (MRHD) of 1.5 mg/day based on body surface area (BSA). Transient growth retardation, with no impact on postnatal development, was observed in rat offspring from a pre- and post-natal study of octreotide at IV doses below the MRHD based on BSA (see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
In postmarketing data, a limited number of exposed pregnancies have been reported in patients with acromegaly. Most women were exposed to octreotide during the first trimester of pregnancy at doses ranging from 100 to 300 mcg/day of octreotide acetate or 20 mg to 30 mg once a month of octreotide acetate for injectable suspension, however some women elected to continue octreotide therapy throughout pregnancy. In cases with a known outcome, no congenital malformations were reported.
Animal Data
In embryo-fetal development studies in rats and rabbits, pregnant animals received IV doses of octreotide up to 1 mg/kg/day during the period of organogenesis. A slight reduction in body weight gain was noted in pregnant rats at 0.1 and 1 mg/kg/day. There were no maternal effects in rabbits or embryo-fetal effects in either species up to the maximum dose tested. At 1 mg/kg/day in rats and rabbits, the dose multiple was approximately 7- and 13-times, respectively, at the highest recommended human dose of 1.5 mg/day based on BSA.
In a pre- and post-natal development rat study at IV doses of 0.02-1 mg/kg/day, a transient growth retardation of the offspring was observed at all doses which was possibly a consequence of GH inhibition by octreotide. The doses attributed to the delayed growth are below the human dose of 1.5 mg/day, based on BSA.
8.2 Lactation
Risk Summary
There is no information available on the presence of octreotide acetate in human milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production. Studies show that octreotide administered subcutaneously passes into the milk of lactating rats; however, due to species-specific differences in lactation physiology, animal data may not reliably predict drug levels in human milk (see Data). The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for octreotide acetate, and any potential adverse effects on the breastfed child from octreotide acetate or from the underlying maternal condition.
8.3 Females and Males of Reproductive Potential
Discuss the potential for unintended pregnancy with premenopausal women as the therapeutic benefits of a reduction in GH levels and normalization of insulin-like growth factor 1 (IGF-1) concentration in acromegalic females treated with octreotide may lead to improved fertility.
8.4 Pediatric Use
Safety and efficacy of octreotide acetate in the pediatric population have not been demonstrated.
No formal controlled clinical trials have been performed to evaluate the safety and effectiveness of octreotide acetate in pediatric patients under age 6 years. In postmarketing reports, serious adverse events, including hypoxia, necrotizing enterocolitis, and death, have been reported with octreotide acetate use in children, most notably in children under 2 years of age. The relationship of these events to octreotide has not been established as the majority of these pediatric patients had serious underlying co-morbid conditions.
The efficacy and safety of octreotide acetate using the octreotide acetate for injectable suspension formulation was examined in a single randomized, double-blind, placebo-controlled, 6 month pharmacokinetics study in 60 pediatric patients age 6 to 17 years with hypothalamic obesity resulting from cranial insult. The mean octreotide concentration after 6 doses of 40 mg octreotide acetate for injectable suspension administered by intramuscular (IM) injection every 4 weeks was approximately 3 ng/mL. Steady-state concentrations was achieved after 3 injections of a 40-mg dose. Mean body mass index (BMI) increased 0.1 kg/m2 in octreotide acetate for injectable suspension-treated subjects compared to 0.0 kg/m2 in saline control-treated subjects.
Efficacy was not demonstrated. Diarrhea occurred in 11 of 30 (37%) patients treated with octreotide acetate for injectable suspension. No unexpected adverse events were observed. However, with octreotide acetate for injectable suspension at 40 mg once a month, the incidence of new cholelithiasis in this pediatric population (33%) was higher than that seen in other adult indications such as acromegaly (22%) or malignant carcinoid syndrome (24%), where octreotide acetate for injectable suspension was 10 mg to 30 mg once a month.
8.5 Geriatric Use
Clinical studies of octreotide acetate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
In patients with severe renal failure requiring dialysis, the half-life of octreotide acetate may be increased, necessitating adjustment of the maintenance dosage [see Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment-Cirrhotic Patients
In patients with liver cirrhosis, the half-life of the drug may be increased, necessitating adjustment of the maintenance dosage [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
A limited number of accidental overdoses of octreotide acetate in adults have been reported. In adults, the doses ranged from 2,400 to 6,000 mcg/day administered by continuous infusion (100 to 250 mcg/hour) or subcutaneously (1,500 mcg 3 times a day). Adverse events in some patients included arrhythmia, complete atrioventricular block, hypotension, cardiac arrest, brain hypoxia, pancreatitis, hepatitis steatosis, hepatomegaly, lactic acidosis, flushing, diarrhea, lethargy, weakness, and weight loss.
If overdose occurs, symptomatic management is indicated. Up-to-date information about the treatment of overdose can often be obtained from the National Poison Control Center at 1-800-222-1222.
-
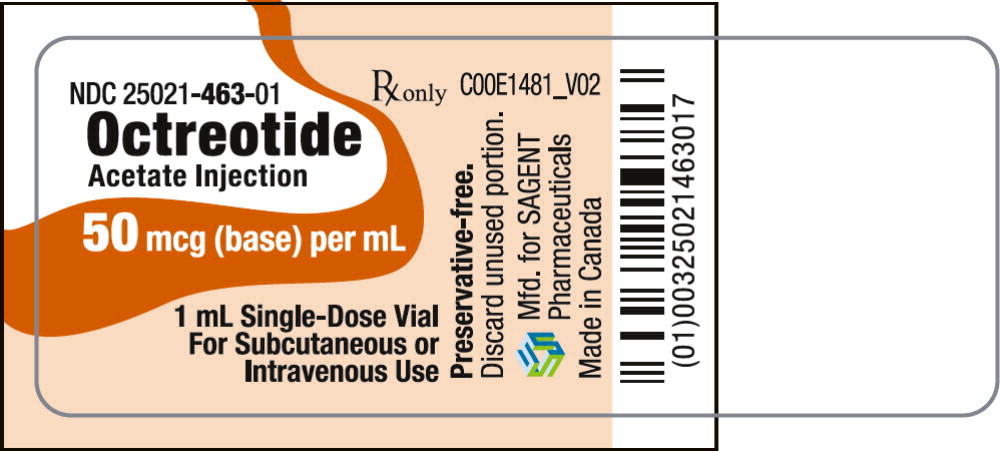
11 DESCRIPTION
Octreotide Acetate Injection, a cyclic octapeptide prepared as a clear sterile solution of octreotide, acetate salt, in a buffered acetate solution with a pH range 3.9 to 4.5 for administration by deep subcutaneous (intrafat) or intravenous (IV) injection. Octreotide acetate, known chemically as L-Cysteinamide, D-phenylalanyl-L-cysteinyl-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-[2-hydroxy-1-(hydroxymethyl) propyl]-,cyclic (2 → 7)-disulfide; [R-(R*, R*)] acetate salt, is a long-acting octapeptide with pharmacologic actions mimicking those of the natural hormone somatostatin.
Octreotide Acetate Injection is available as sterile 1 mL single-dose vials in 3 strengths, containing 50 mcg, 100 mcg, or 500 mcg octreotide acetate, USP. Each mL of the single-dose vial also contains sodium chloride, USP (7 mg), glacial acetic acid, USP (2 mg), sodium acetate trihydrate, USP (2 mg), and water for injection, USP (quantity sufficient to 1 mL).
Octreotide Acetate Injection is also available as sterile 5 mL multi-dose vials in 2 strengths, containing 200 mcg, or 1,000 mcg per mL of octreotide acetate, USP. Each mL of the multi-dose vial also contains sodium chloride, USP (7 mg), glacial acetic acid, USP (2 mg), sodium acetate trihydrate, USP (2 mg), phenol, USP (5 mg), and water for injection, USP (quantity sufficient to 1 mL).
The molecular weight of octreotide acetate is 1,019.3 g/mol (free peptide, C49H66N10O10S2) and its amino acid sequence is:
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Octreotide acetate exerts pharmacologic actions similar to the natural hormone, somatostatin. It is an even more potent inhibitor of GH, glucagon, and insulin than somatostatin. Like somatostatin, it also suppresses luteinizing hormone (LH) response to gonadotropin releasing hormone (GnRH), decreases splanchnic blood flow, and inhibits release of serotonin, gastrin, VIP, secretin, motilin, and pancreatic polypeptide.
By virtue of these pharmacological actions, octreotide has been used to treat the symptoms associated with metastatic carcinoid tumors (flushing and diarrhea), and VIP secreting adenomas (watery diarrhea).
12.2 Pharmacodynamics
Octreotide substantially reduces GH and/or IGF-1 (somatomedin C) levels in patients with acromegaly.
Single doses of octreotide have been shown to inhibit gallbladder contractility and to decrease bile secretion in normal volunteers. In controlled clinical trials, the incidence of gallstone or biliary sludge formation was markedly increased [see Warnings and Precautions (5.2)].
Octreotide suppresses secretion of TSH.
12.3 Pharmacokinetics
Absorption
After subcutaneous injection, octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, IV and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve (AUC) values were dose proportional after IV single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg 3 times a day (1,500 mcg/day). In patients with acromegaly, a mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing.
Distribution
In healthy volunteers, the distribution of octreotide from plasma was rapid (tα½ = 0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin. In patients with acromegaly, the volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L, and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%.
Elimination
The elimination of octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the disposition and elimination half-lives were similar to normal subjects.
Specific Populations
Renal Impairment
In patients with mild renal impairment (CLCR 40 to 60 mL/min), octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (CLCR 10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr. In patients with severe renal impairment not requiring dialysis (CLCR < 10 mL/min), octreotide t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
12.6 Immunogenicity
Evaluation of 20 patients treated for at least 6 months has failed to demonstrate titers of antibodies exceeding background levels. However, antibody titers to octreotide acetate were subsequently reported in 3 patients and resulted in prolonged duration of drug action in 2 patients.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies in laboratory animals have demonstrated no mutagenic potential of octreotide acetate.
No carcinogenic potential was demonstrated in mice treated subcutaneously for 85 to 99 weeks at doses up to 2,000 mcg/kg/day (8 x the human exposure based on BSA). In a 116-week subcutaneous study in rats, a 27% and 12% incidence of injection-site sarcomas or squamous cell carcinomas was observed in males and females, respectively, at the highest dose level of 1,250 mcg/kg/day (10 x the human exposure based on BSA) compared to an incidence of 8% to 10% in the vehicle-control groups. The increased incidence of injection-site tumors was most probably caused by irritation and the high sensitivity of the rat to repeated subcutaneous injections at the same site. Rotating injection sites would prevent chronic irritation in humans. There have been no reports of injection-site tumors in patients treated with octreotide acetate for up to 5 years. There was also a 15% incidence of uterine adenocarcinomas in the 1,250 mcg/kg/day females compared to 7% in the saline-control females and 0% in the vehicle-control females. The presence of endometritis coupled with the absence of corpora lutea, the reduction in mammary fibroadenomas, and the presence of uterine dilatation suggest that the uterine tumors were associated with estrogen dominance in the aged female rats which does not occur in humans.
Octreotide did not impair fertility in rats at doses up to 1,000 mcg/kg/day, which represents 7-times the human exposure based on BSA.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Octreotide Acetate Injection is available as follows:
NDC Octreotide Acetate Injection (Preservative-free) Package Factor 25021-463-01 50 mcg (base) per mL Single-Dose Vial 10 vials per carton 25021-464-01 100 mcg (base) per mL Single-Dose Vial 10 vials per carton 25021-465-01 500 mcg (base) per mL Single-Dose Vial 10 vials per carton NDC Octreotide Acetate Injection (Preservative) Package Factor 25021-466-05 1,000 mcg (base) per 5 mL Multi-Dose Vial 1 vial per carton 200 mcg (base) per mL 25021-467-05 5,000 mcg (base) per 5 mL Multi-Dose Vial 1 vial per carton 1,000 mcg (base) per mL Storage Conditions
Store refrigerated between 2° and 8°C (36° and 46°F). At room temperature (20° to 30°C or 70° to 86°F), Octreotide Acetate Injection is stable for 14 days if protected from light. The solution can be allowed to come to room temperature prior to administration. Do not warm artificially.
Single-Dose Vials—should be opened just prior to administration and the unused portion discarded.
Multi-Dose Vials—should be discarded within 14 days after initial use.
Protect from light. Retain in carton until time of use.
Dispose of unused product or waste properly. Octreotide Acetate Injection is stable in sterile isotonic saline solutions or sterile solutions of dextrose 5% in water for 24 hours.
Sterile, Nonpyrogenic.
The container closure is not made with natural rubber latex. -
17 PATIENT COUNSELING INFORMATION
Sterile Subcutaneous Injection Technique
Careful instruction in sterile subcutaneous injection technique should be given to the patients and to other persons who may administer octreotide acetate.
Cholelithiasis and Complications of Cholelithiasis
Advise patients to contact their healthcare provider if they experience signs or symptoms of gallstones (cholelithiasis) or complications of cholelithiasis (e.g., cholecystitis, cholangitis, and pancreatitis) [see Warnings and Precautions (5.2)].
Steatorrhea and Malabsorption of Dietary Fats
Advise patients to contact their healthcare provider if they experience new or worsening of steatorrhea, stool discoloration, loose stools, abdominal bloating, and weight loss [see Warnings and Precautions (5.5)].
Pregnancy
Inform female patients that treatment with octreotide acetate may result in unintended pregnancy [see Use in Specific Populations (8.3)].
SAGENT®
Mfd. for SAGENT Pharmaceuticals
Schaumburg, IL 60195 (USA)
Made in Canada
©2024 Sagent PharmaceuticalsRevised: September 2024
SAGENT Pharmaceuticals ®
-
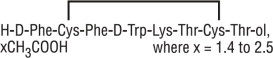
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NDC: 25021-466-05
Rx only
Octreotide Acetate Injection
1,000 mcg per 5 mL
(200 mcg per mL)
5 mL Multi-Dose Vial
For Subcutaneous or Intravenous Use
-
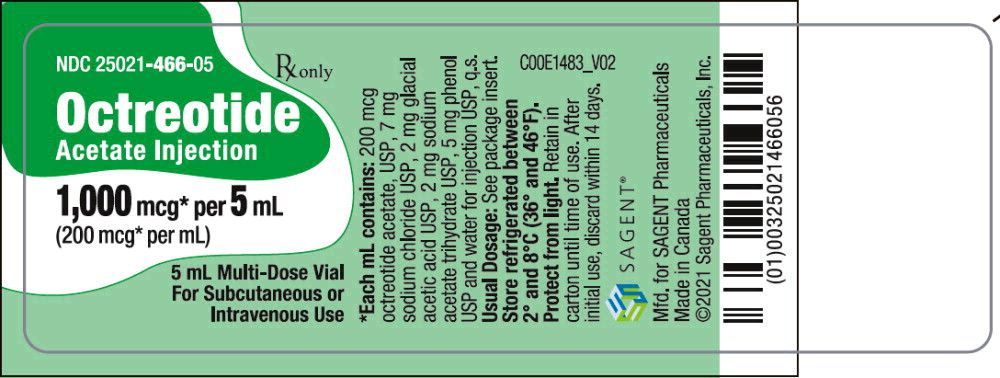
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NDC: 25021-467-05
Rx only
Octreotide Acetate Injection
5,000 mcg per 5 mL
(1,000 mcg per mL)
5 mL Multi-Dose Vial
For Subcutaneous or Intravenous Use
-
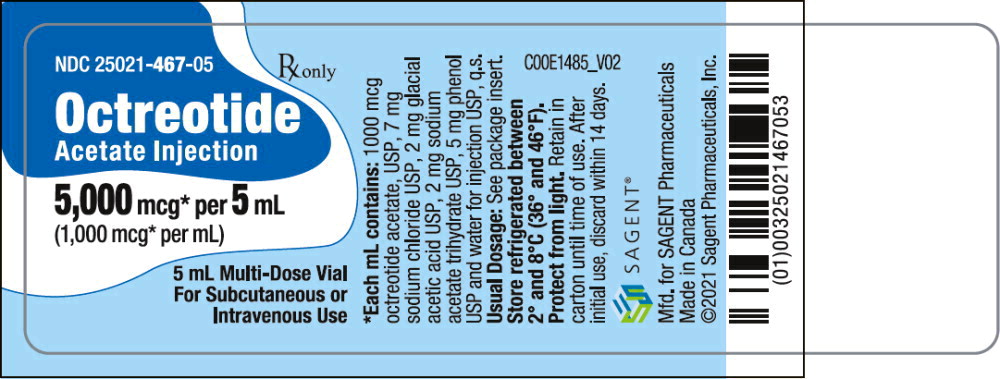
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NDC: 25021-463-01
Rx only
Octreotide Acetate Injection
50 mcg (base) per mL
1 mL Single-Dose Vial
For Subcutaneous or Intravenous Use
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NDC: 25021-464-01
Rx only
Octreotide Acetate Injection
100 mcg (base) per mL
1 mL Single-Dose Vial
For Subcutaneous or Intravenous Use
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – Vial Label
NDC: 25021-465-01
Rx only
Octreotide Acetate Injection
500 mcg (base) per mL
1 mL Single-Dose Vial
For Subcutaneous or Intravenous Use
-
INGREDIENTS AND APPEARANCE
OCTREOTIDE ACETATE
octreotide acetate injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-463 Route of Administration SUBCUTANEOUS, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength octreotide acetate (UNII: 75R0U2568I) (octreotide - UNII:RWM8CCW8GP) octreotide 50 ug in 1 mL Inactive Ingredients Ingredient Name Strength sodium chloride (UNII: 451W47IQ8X) sodium acetate (UNII: 4550K0SC9B) acetic acid (UNII: Q40Q9N063P) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-463-01 10 in 1 CARTON 06/15/2023 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090834 06/15/2023 OCTREOTIDE ACETATE
octreotide acetate injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-464 Route of Administration SUBCUTANEOUS, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength octreotide acetate (UNII: 75R0U2568I) (octreotide - UNII:RWM8CCW8GP) octreotide 100 ug in 1 mL Inactive Ingredients Ingredient Name Strength sodium chloride (UNII: 451W47IQ8X) sodium acetate (UNII: 4550K0SC9B) acetic acid (UNII: Q40Q9N063P) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-464-01 10 in 1 CARTON 06/15/2023 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090834 06/15/2023 OCTREOTIDE ACETATE
octreotide acetate injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-465 Route of Administration SUBCUTANEOUS, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength octreotide acetate (UNII: 75R0U2568I) (octreotide - UNII:RWM8CCW8GP) octreotide 500 ug in 1 mL Inactive Ingredients Ingredient Name Strength sodium chloride (UNII: 451W47IQ8X) sodium acetate (UNII: 4550K0SC9B) acetic acid (UNII: Q40Q9N063P) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-465-01 10 in 1 CARTON 06/15/2023 1 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090834 06/15/2023 OCTREOTIDE ACETATE
octreotide acetate injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-466 Route of Administration SUBCUTANEOUS, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength octreotide acetate (UNII: 75R0U2568I) (octreotide - UNII:RWM8CCW8GP) octreotide 200 ug in 1 mL Inactive Ingredients Ingredient Name Strength phenol (UNII: 339NCG44TV) sodium chloride (UNII: 451W47IQ8X) sodium acetate (UNII: 4550K0SC9B) acetic acid (UNII: Q40Q9N063P) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-466-05 1 in 1 CARTON 06/15/2023 1 5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA091041 06/15/2023 OCTREOTIDE ACETATE
octreotide acetate injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-467 Route of Administration SUBCUTANEOUS, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength octreotide acetate (UNII: 75R0U2568I) (octreotide - UNII:RWM8CCW8GP) octreotide 1000 ug in 1 mL Inactive Ingredients Ingredient Name Strength phenol (UNII: 339NCG44TV) sodium chloride (UNII: 451W47IQ8X) sodium acetate (UNII: 4550K0SC9B) acetic acid (UNII: Q40Q9N063P) water (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-467-05 1 in 1 CARTON 06/15/2023 1 5 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA091041 06/15/2023 Labeler - Sagent Pharmaceuticals (080579617)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.