Phytonadione by Cipla USA., Inc. / ScieGen Pharmaceuticals, Inc PHYTONADIONE tablet
Phytonadione by
Drug Labeling and Warnings
Phytonadione by is a Prescription medication manufactured, distributed, or labeled by Cipla USA., Inc., ScieGen Pharmaceuticals, Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PHYTONADIONE TABLETS safely and effectively. See full prescribing information for PHYTONADIONE TABLETS.
PHYTONADIONE tablets, for oral use
Initial U.S. Approval: 1955INDICATIONS AND USAGE
Phytonadione is a vitamin K replacement indicated for the treatment of adults with the following coagulation disorders which are due to faulty formation of factors II, VII, IX and X when caused by vitamin K deficiency or interference with vitamin K activity:
- Anticoagulant-induced prothrombin deficiency caused by coumarin or indanedione derivatives; (1)
- Hypoprothrombinemia secondary to antibacterial therapy; (1)
- Hypoprothrombinemia secondary to factors limiting absorption or synthesis of vitamin K, e.g., obstructive jaundice, biliary fistula, sprue, ulcerative colitis, celiac disease, intestinal resection, cystic fibrosis of the pancreas, and regional enteritis; (1)
- Other drug-induced hypoprothrombinemia where it is definitively shown that the result is due to interference with vitamin K metabolism, e.g., salicylates. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Tablets: 5 mg (3)
CONTRAINDICATIONS
Hypersensitivity to any component of this medication. (4)
ADVERSE REACTIONS
Most common adverse reactions are transient “flushing sensations”, “peculiar” sensations of taste and instances of dizziness, rapid and weak pulse, profuse sweating, brief hypotension, dyspnea, and cyanosis. (6)
To report SUSPECTED ADVERSE REACTIONS, contact ScieGen Pharmaceuticals, Inc. at 1-855-724-3436 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Anticoagulants: May induce temporary resistance to prothrombin depressing anticoagulants. (7)
Revised: 11/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Considerations
2.2 Recommended Dosage
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Phytonadione is indicated for the treatment of adults with the following coagulation disorders which are due to faulty formation of factors II, VII, IX and X when caused by vitamin K deficiency or interference with vitamin K activity.
- anticoagulant-induced hypoprothrombinemia caused by coumarin or indanedione derivatives;
- hypoprothrombinemia secondary to antibacterial therapy;
- hypoprothrombinemia secondary to factors limiting absorpsion or synthesis of vitamin K, e.g., obstructive jaundice, biliary fistula, sprue, ulcerative colitis, celiac disease, intestinal resection, cystic fibrosis of the pancrease, and regional enteritis;
- Other drug-induced hypoprothrombinemia where it is definitely shown that the result is due to interference with vitamin K metabolism, e.g., salicylates.
-
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Considerations
Avoid the oral route when the clinical disorder would prevent proper absorption. Bile salts must be given with the tablets when the endogenous supply of bile to the gastrointestinal tract is deficient. The coagulant effects of phytonadione are not immediate; improvement of international normalized ratio (INR) may take 1 to 8 hours. Interim use of whole blood or component therapy may also be necessary if bleeding is severe.
Phytonadione will not counteract the anticoagulant action of heparin.
When phytonadione is used to correct excessive anticoagulant-induced hypoprothrombinemia, anticoagulant therapy still being indicated, the patient is again faced with the clotting hazards existing prior to starting the anticoagulant therapy. Phytonadione is not a clotting agent, but overzealous therapy with vitamin K1 may restore conditions which originally permitted thromboembolic phenomena. Dosage should be kept as low as possible, and prothrombin time should be checked regularly as clinical conditions indicate.
2.2 Recommended Dosage
Anticoagulant-Induced Prothrombin Deficiency in Adults
The recommended dose to correct excessively prolonged prothrombin times caused by oral anticoagulant therapy is, 2.5 mg to 10 mg or up to 25 mg initially. In some instances 50 mg may be required. Frequency and amount of subsequent doses should be determined by prothrombin time response or clinical condition. If, in 12 to 48 hours after oral administration, the prothrombin time has not been shortened satisfactorily, repeat the dose.
Repeated large doses of phytonadione are not warranted in liver disease if the response to initial use of the vitamin is unsatisfactory. Failure to respond to phytonadione may indicate a congenital coagulation defect or that the condition being treated is unresponsive to vitamin K.
Hypoprothrombinemia Due to Other Causes in Adults
If possible, discontinuation or reduction of the dosage of drugs interfering with coagulation mechanisms (such as salicylates, antibiotics) is suggested as an alternative to administering concurrent phytonadione. The severity of the coagulation disorder should determine whether the immediate administration of phytonadione is required in addition to discontinuation or reduction of interfering drugs.
The recommended dose is 2.5 mg to 25 mg or more (sometimes up to 50 mg). Evaluate INR after 6 to 8 hours, and repeat dose if INR remains prolonged. Modify subsequent dosage (amount and frequency) based upon the INR or clinical condition.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Phytonadione is contraindicated in patients with a history of a hypersensitivity reaction to phytonadione or inactive ingredients [see Description (11)].
-
6 ADVERSE REACTIONS
The following adverse reactions associated with the use of parenteral phytonadione were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Severe hypersensitivity reactions, including anaphylactoid reactions and deaths, have been reported following parenteral administration. The majority of these reported events occurred following intravenous administration.
Transient “flushing sensations” and “peculiar” sensations of taste have been observed with parenteral phytonadione, as well as instances of dizziness, rapid and weak pulse, profuse sweating, brief hypotension, dyspnea, and cyanosis.
Hyperbilirubinemia has been observed in the newborn following administration of parenteral phytonadione. This has occurred primarily with doses above those recommended.
-
7 DRUG INTERACTIONS
Anticoagulants
Phytonadione may induce temporary resistance to prothrombin-depressing anticoagulants, especially when larger doses of phytonadione are used. Should this occur, higher doses of anticoagulant therapy may be needed when resuming anticoagulant therapy, or a change in therapy to a different class of anticoagulant may be necessary (i.e., heparin sodium).
Phytonadione does not affect the anticoagulant action of heparin.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
RiskSummaryPublished studies with the use of phytonadione during pregnancy have not reported a clear association with phytonadione and adverse developmental outcomes [see Data]. There are maternal and fetal risks associated with vitamin K deficiency during pregnancy [see Clinical Considerations]. Animal reproduction studies have not been conducted with phytonadione.
The estimated background risk for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Pregnant women with vitamin K deficiency hypoprothrombinemia may be at increased risk for bleeding diatheses during pregnancy and hemorrhagic events at delivery. Subclinical vitamin K deficiency during pregnancy has been implicated in rare cases of fetal intracranial hemorrhage.
Data
Human Data
Phytonadione has been measured in cord blood of infants whose mothers were treated with phytonadione during pregnancy in concentrations lower than seen in maternal plasma. Administration of vitamin K1 to pregnant women shortly before delivery increased both maternal and cord blood concentrations. Published data do not report a clear association with phytonadione and adverse maternal or fetal outcomes when used during pregnancy. However, these studies cannot definitively establish the absence of any risk because of methodologic limitations including small sample size and lack of blinding.
Animal Data
In pregnant rats receiving vitamin K1 orally, fetal plasma and liver concentrations increased following administration, supporting placental transfer.
8.2 Lactation
RiskSummary
Phytonadione is present in breastmilk. There are no data on the effects of phytonadione on the breastfed child or on milk production. The developmental and health benefits of breastfeeding should be considered along with the clinical need for phytonadione and any potential adverse effects on the breastfed child from phytonadione or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established with phytonadione. Hemolysis, jaundice, and hyperbilirubinemia in newborns, particularly in premature infants, have been reported with vitamin K.
8.5 Geriatric Use
Clinical studies of phytonadione did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
11 DESCRIPTION
Phytonadione is a vitamin K replacement, which is a clear, yellow to amber, viscous, and nearly odorless liquid. It is insoluble in water, soluble in chloroform and slightly soluble in ethanol. It has a molecular weight of 450.7.
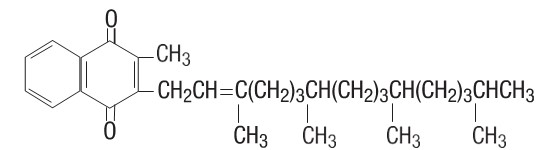
Phytonadione is 2-methyl-3-phytyl-1, 4-naphthoquinone. Its empirical formula is C31H46O2 and its structural formula is:
Phytonadione tablets, USP for oral administration contain 5 mg of phytonadione, USP and are pale yellow colored, round tablets, scored on one side. Inactive ingredients are acacia, anhydrous dibasic calcium phosphate, lactose monohydrate, magnesium stearate, pregelatinized starch, silicon dioxide and talc.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Phytonadione tablets possess the same type and degree of activity as does naturally-occurring vitamin K, which is necessary for the production via the liver of active prothrombin (factor II), proconvertin (factor VII), plasma thromboplastin component (factor IX), and Stuart factor (factor X). The prothrombin test is sensitive to the levels of three of these four factors – II, VII, and X. Vitamin K is an essential cofactor for a microsomal enzyme that catalyzes the posttranslational carboxylation of multiple, specific, peptide- bound glutamic acid residues in inactive hepatic precursors of factors II, VII, IX, and X. The resulting gamma-carboxyglutamic acid residues convert the precursors into active coagulation factors that are subsequently secreted by liver cells into the blood.
In normal animals and humans, phytonadione is virtually devoid of pharmacodynamic activity. However, in animals and humans deficient in vitamin K, the pharmacological action of vitamin K is related to its normal physiological function, that is, to promote the hepatic biosynthesis of vitamin K-dependent clotting factors.
12.3 Pharmacokinetics
AbsorptionOral phytonadione is adequately absorbed from the gastrointestinal tract only if bile salts are present.
Distribution
After absorption, phytonadione is initially concentrated in the liver, but the concentration declines rapidly. Very little vitamin K accumulates in tissues.
Elimination
Little is known about the metabolic fate of vitamin K. Almost no free unmetabolized vitamin K appears in bile or urine.
- 13 NONCLINICAL TOXICOLOGY
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Phytonadione tablets, USP 5 mg, are pale yellow colored, round, scored tablets, debossed with ‘SG 333’ on one side and score line on other side. They are supplied as follows:
Bottles of 30 tablets: NDC: 69097-999-02
Bottles of 100 tablets: NDC: 69097-999-07
Storage
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Always protect phytonadione from light. Store in tightly closed original container and carton until contents have been used.
-
17 PATIENT COUNSELING INFORMATION
Vitamin K1 is fairly rapidly degraded by light; therefore, advise patients to always protect phytonadione from light. Store phytonadione in closed original carton until contents have been used [see How Supplied/Storage and Handling (16)].
Manufactured for:
Cipla USA, Inc.
10 Independence Boulevard,
Suite 300, Warren, NJ 07059
Manufactured by:
ScieGen Pharmaceuticals, Inc.
Hauppauge, NY 11788 USA
Rev: 11/2023
21101736 -
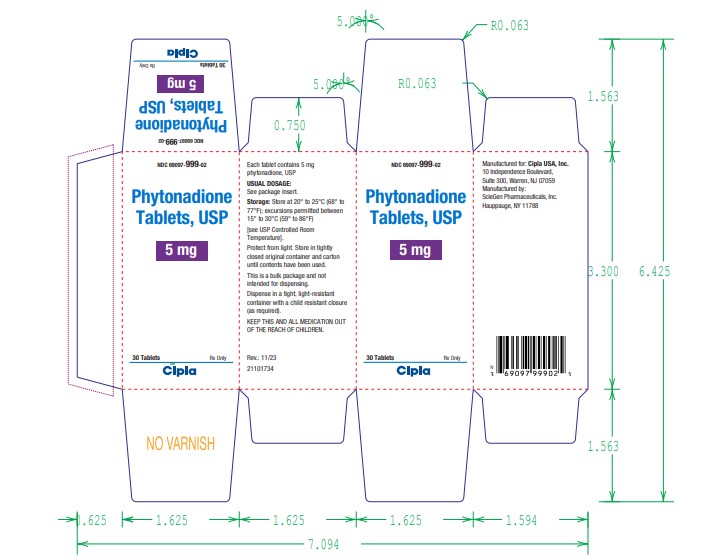
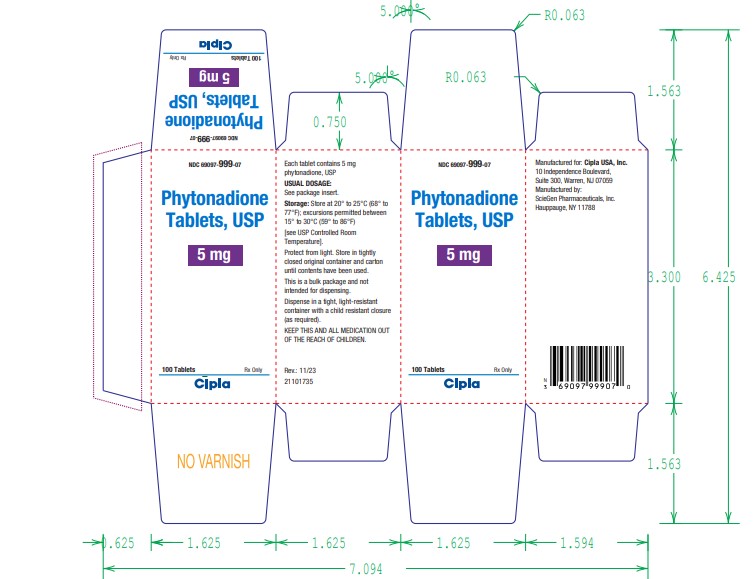
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 69097-999-02
Phytonadione Tablets USP,
5 mg
Each tablet contains
5 mg phytonadione, USP
30 Tablets Rx only
Cipla.
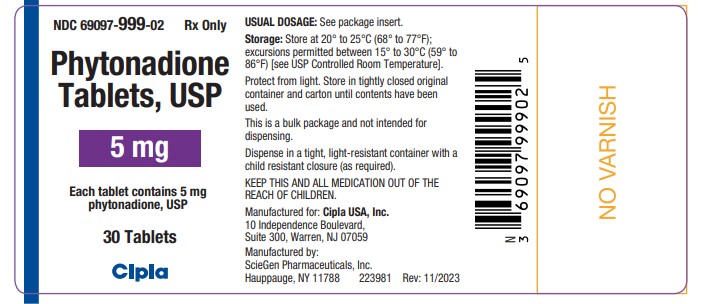
NDC 69097-999-02
Phytonadione Tablets USP,
5 mg
30 Tablets Rx only
Cipla.
NDC 69097-999-07
Phytonadione Tablets USP,
5 mg
Each tablet contains
5 mg phytonadione, USP
100 Tablets Rx only
Cipla.
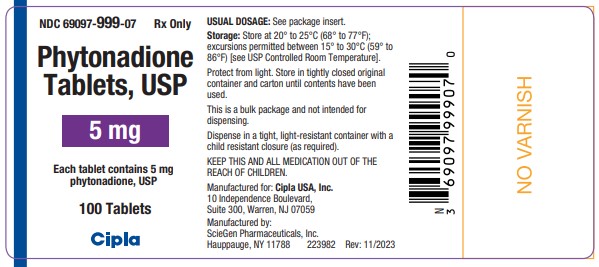
NDC 69097-999-07
Phytonadione Tablets USP,
5 mg
100 Tablets Rx only
Cipla.
-
INGREDIENTS AND APPEARANCE
PHYTONADIONE
phytonadione tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 69097-999 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHYTONADIONE (UNII: A034SE7857) (PHYTONADIONE - UNII:A034SE7857) PHYTONADIONE 5 mg Inactive Ingredients Ingredient Name Strength ACACIA (UNII: 5C5403N26O) ANHYDROUS DIBASIC CALCIUM PHOSPHATE (UNII: L11K75P92J) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM STEARATE (UNII: 70097M6I30) STARCH, CORN (UNII: O8232NY3SJ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) TALC (UNII: 7SEV7J4R1U) Product Characteristics Color yellow (pale yellow) Score 2 pieces Shape ROUND Size 6mm Flavor Imprint Code SG;333 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 69097-999-02 30 in 1 BOTTLE; Type 0: Not a Combination Product 12/01/2023 2 NDC: 69097-999-07 100 in 1 BOTTLE; Type 0: Not a Combination Product 12/01/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA213329 12/01/2023 Labeler - Cipla USA., Inc. (078719707) Registrant - ScieGen Pharmaceuticals, Inc (079391286) Establishment Name Address ID/FEI Business Operations ScieGen Pharmaceuticals, Inc 079391286 manufacture(69097-999) , analysis(69097-999) , pack(69097-999) , label(69097-999)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.