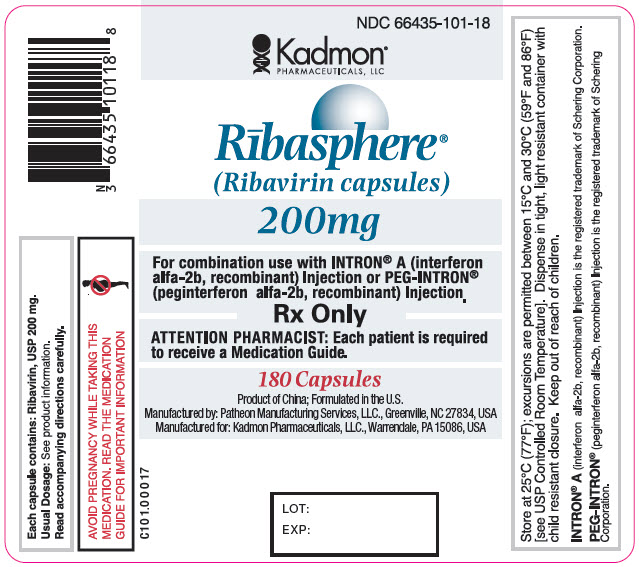
These highlights do not include all the information needed to use RIBASPHERE® (ribavirin capsules USP) safely and effectively. See full prescribing information for RIBASPHERE.RIBASPHERE (ribavirin capsules USP) 200 mg, for oral useInitial U.S. Approval: 1998
Ribasphere by
Drug Labeling and Warnings
Ribasphere by is a Prescription medication manufactured, distributed, or labeled by Kadmon Pharmaceuticals, LLC, Patheon Manufacturing Services LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
RIBASPHERE- ribavirin capsule
Kadmon Pharmaceuticals, LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use RIBASPHERE® (ribavirin capsules USP) safely and effectively. See full prescribing information for RIBASPHERE.
RIBASPHERE (ribavirin capsules USP) 200 mg, for oral use Initial U.S. Approval: 1998 WARNING: RISK OF SERIOUS DISORDERS AND RIBAVIRIN-ASSOCIATED EFFECTSSee full prescribing information for complete boxed warning
INDICATIONS AND USAGERIBASPHERE (ribavirin capsules USP) is a nucleoside analogue indicated in combination with interferon alfa-2b (pegylated and nonpegylated) for the treatment of Chronic Hepatitis C (CHC) in patients 3 years of age or older with compensated liver disease. (1.1)
DOSAGE AND ADMINISTRATIONDOSAGE FORMS AND STRENGTHSRIBASPHERE Capsules 200 mg (3) CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
Patients exhibiting the following conditions should be closely monitored and may require dose reduction or discontinuation of therapy:
ADVERSE REACTIONSHemolytic anemia. (6.1) Most common adverse reactions (approximately 40%) in adult patients receiving RIBASPHERE/peginterferon alfa-2b or interferon alfa-2b combination therapy are injection site reaction, fatigue/asthenia, headache, rigors, fevers, nausea, myalgia and anxiety/emotional lability/irritability. (6.1, 6.2) Most common adverse reactions (greater than 25%) in pediatric patients receiving RIBASPHERE/peginterferon alfa-2b therapy are: pyrexia, headache, neutropenia, fatigue, anorexia, injection site erythema, and vomiting. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact Kadmon Pharmaceuticals at 1-877-377-7862 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch DRUG INTERACTIONSNucleoside analogues: Closely monitor for toxicities. Discontinue nucleoside reverse transcriptase inhibitors or reduce dose or discontinue interferon, ribavirin or both with worsening toxicities. (7.2) USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 12/2015 |
FULL PRESCRIBING INFORMATION
WARNING: RISK OF SERIOUS DISORDERS AND RIBAVIRIN-ASSOCIATED EFFECTS
- RIBASPHERE® (ribavirin capsules USP) monotherapy is not effective for the treatment of chronic hepatitis C virus infection and should not be used alone for this indication [see Warnings and Precautions (5.10)].
- The primary toxicity of ribavirin is hemolytic anemia. The anemia associated with RIBASPHERE therapy may result in worsening of cardiac disease that has led to fatal and nonfatal myocardial infarctions. Patients with a history of significant or unstable cardiac disease should not be treated with RIBASPHERE [see Dosage and Administration (2.4), Warnings and Precautions (5.2), and Adverse Reactions (6.1)].
- Significant teratogenic and embryocidal effects have been demonstrated in all animal species exposed to ribavirin. In addition, ribavirin has a multiple-dose half-life of 12 days, and so it may persist in nonplasma compartments for as long as 6 months. Therefore, RIBASPHERE therapy is contraindicated in women who are pregnant and in the male partners of women who are pregnant. Extreme care must be taken to avoid pregnancy during therapy and for 6 months after completion of treatment in both female patients and in female partners of male patients who are taking RIBASPHERE therapy. At least two reliable forms of effective contraception must be utilized during treatment and during the 6-month post-treatment follow-up period [see Contraindications (4), Warnings and Precautions (5.1), Use in Specific Populations (8.1), Nonclinical Toxicology (13.1), and Patient Counseling Information (17.2)].
1 INDICATIONS AND USAGE
1.1 Chronic Hepatitis C (CHC)
RIBASPHERE® (ribavirin capsules USP) in combination with interferon alfa-2b (pegylated and nonpegylated) is indicated for the treatment of Chronic Hepatitis C (CHC) in patients 3 years of age and older with compensated liver disease [see Warnings and Precautions (5.9, 5.10), and Use in Specific Populations (8.4)].
The following points should be considered when initiating RIBASPHERE combination therapy with peginterferon alfa-2b or interferon alfa-2b:
- These indications are based on achieving undetectable HCV-RNA after treatment for 24 or 48 weeks and maintaining a Sustained Virologic Response (SVR) 24 weeks after the last dose.
- Combination therapy with RIBASPHERE/peginterferon alfa-2b is preferred over RIBASPHERE/interferon alfa-2b as this combination provides substantially better response rates [see Clinical Studies (14)].
- Patients with the following characteristics are less likely to benefit from re-treatment after failing a course of therapy: previous nonresponse, previous pegylated interferon treatment, significant bridging fibrosis or cirrhosis, and genotype 1 infection [see Clinical Studies (14)].
- No safety and efficacy data are available for treatment of longer than one year.
2 DOSAGE AND ADMINISTRATION
Under no circumstances should RIBASPHERE capsules be opened, crushed, or broken. RIBASPHERE should be taken with food [see Clinical Pharmacology (12.3)]. RIBASPHERE should not be used in patients with creatinine clearance less than 50 mL/min.
2.1 RIBASPHERE/Peginterferon alfa-2b Combination Therapy
Adult Patients
The recommended dose of peginterferon alfa-2b is 1.5 mcg/kg/week subcutaneously in combination with 800 to 1400 mg RIBASPHERE capsules orally based on patient body weight (see Table 1). The volume of peginterferon alfa-2b to be injected depends on the strength of peginterferon alfa-2b and patient’s body weight, refer to labeling for peginterferon alfa-2b for additional dosing information.
Duration of Treatment – Interferon Alpha-naïve Patients
The treatment duration for patients with genotype 1 is 48 weeks. Discontinuation of therapy should be considered in patients who do not achieve at least a 2 log10 drop or loss of HCV-RNA at 12 weeks, or if HCV-RNA remains detectable after 24 weeks of therapy. Patients with genotype 2 and 3 should be treated for 24 weeks.
Duration of Treatment – Re-treatment with Peginterferon alfa-2b/Ribavirin of Prior Treatment Failures
The treatment duration for patients who previously failed therapy is 48 weeks, regardless of HCV genotype. Re-treated patients who fail to achieve undetectable HCV-RNA at week 12 of therapy, or whose HCV-RNA remains detectable after 24 weeks of therapy, are highly unlikely to achieve SVR and discontinuation of therapy should be considered [see Clinical Studies (14.1)].
|
Body Weight kg (lbs) |
RIBASPHERE Daily Dose |
RIBASPHERE Number of Capsules |
|
<66 (<144) |
800 mg/day |
2 x 200-mg capsules A.M. 2 x 200-mg capsules P.M. |
|
66-80 (145-177) |
1000 mg/day |
2 x 200-mg capsules A.M. 3 x 200-mg capsules P.M. |
|
81-105 (178-231) |
1200 mg/day |
3 x 200-mg capsules A.M. 3 x 200-mg capsules P.M. |
|
>105 (231) |
1400 mg/day |
3 x 200-mg capsules A.M. 4 x 200-mg capsules P.M. |
Pediatric Patients
Dosing for pediatric patients is determined by body surface area for peginterferon alfa-2b and by body weight for RIBASPHERE. The recommended dose of peginterferon alfa-2b is 60 mcg/m2/week subcutaneously in combination with 15 mg/kg/day of RIBASPHERE orally in two divided doses (see Table 2) for pediatric patients ages 3-17 years. Patients who reach their 18th birthday while receiving peginterferon alfa-2b/RIBASPHERE should remain on the pediatric dosing regimen. The treatment duration for patients with genotype 1 is 48 weeks. Patients with genotype 2 and 3 should be treated for 24 weeks.
|
|
||
|
Body Weight kg (lbs) |
RIBASPHERE
|
RIBASPHERE Number of Capsules |
|
47–59 |
800 mg/day |
2 x 200-mg capsules A.M. |
|
60–73 |
1000 mg/day |
2 x 200-mg capsules A.M. |
|
>73 |
1200 mg/day |
3 x 200-mg capsules A.M. |
2.2 RIBASPHERE/Interferon alfa-2b Combination Therapy
Adults
Duration of Treatment – Interferon Alpha-naïve Patients
The recommended dose of interferon alfa-2b is 3 million IU three times weekly subcutaneously. The recommended dose of RIBASPHERE capsules depends on the patient’s body weight (refer to Table 3). The recommended duration of treatment for patients previously untreated with interferon is 24 to 48 weeks. The duration of treatment should be individualized to the patient depending on baseline disease characteristics, response to therapy, and tolerability of the regimen [see Indications and Usage (1.1), Adverse Reactions (6.1), and Clinical Studies (14)]. After 24 weeks of treatment, virologic response should be assessed. Treatment discontinuation should be considered in any patient who has not achieved an HCV-RNA below the limit of detection of the assay by 24 weeks. There are no safety and efficacy data on treatment for longer than 48 weeks in the previously untreated patient population.
Duration of Treatment – Re-treatment with Interferon alfa-2b/RIBASPHERE in Relapse Patients
In patients who relapse following nonpegylated interferon monotherapy, the recommended duration of treatment is 24 weeks.
|
Body Weight |
RIBASPHERE® (ribavirin capsules) |
|
≤75 kg |
2 × 200-mg capsules AM |
|
>75 kg |
3 × 200-mg capsules AM |
Pediatrics
The recommended dose of RIBASPHERE is 15 mg/kg per day orally (divided dose AM and PM). Refer to Table 2 for Pediatric Dosing of RIBASPHERE in combination with interferon alfa-2b. Interferon alfa-2b for Injection by body weight of 25 kg to 61 kg is 3 million IU/m2 three times weekly subcutaneously. Refer to adult dosing table for greater than 61 kg body weight.
The recommended duration of treatment is 48 weeks for pediatric patients with genotype 1. After 24 weeks of treatment, virologic response should be assessed. Treatment discontinuation should be considered in any patient who has not achieved an HCV-RNA below the limit of detection of the assay by this time. The recommended duration of treatment for pediatric patients with genotype 2/3 is 24 weeks.
2.3 Laboratory Tests
The following laboratory tests are recommended for all patients treated with RIBASPHERE, prior to beginning treatment and then periodically thereafter.
- Standard hematologic tests - including hemoglobin (pretreatment, Week 2 and Week 4 of therapy, and as clinically appropriate [see Warnings and Precautions (5.2, 5.7)]), complete and differential white blood cell counts, and platelet count.
- Blood chemistries - liver function tests and TSH.
- Pregnancy - including monthly monitoring for women of childbearing potential.
- ECG [see Warnings and Precautions (5.2)].
2.4 Dose Modifications
If severe adverse reactions or laboratory abnormalities develop during combination RIBASPHERE/interferon alfa-2b therapy or RIBASPHERE/peginterferon alfa-2b therapy, modify, or discontinue the dose until the adverse reaction abates or decreases in severity [see Warnings and Precautions (5)]. If intolerance persists after dose adjustment, combination therapy should be discontinued. Dose reduction of peginterferon alfa-2b in adult patients on RIBASPHERE/peginterferon alfa-2b combination therapy is accomplished in a two-step process from the original starting dose of 1.5 mcg/kg/week, to 1 mcg/kg/week, then to 0.5 mcg/kg/week, if needed.
Refer to labeling for peginterferon alfa-2b for additional information regarding dose reduction of peginterferon alfa-2b.
In the adult combination therapy Study 2, dose reductions occurred in 42% of subjects receiving peginterferon alfa-2b 1.5 mcg/kg and RIBASPHERE 800 mg daily, including 57% of those subjects weighing 60 kg or less. In Study 4, 16% of subjects had a dose reduction of peginterferon alfa-2b to 1 mcg/kg in combination with RIBASPHERE, with an additional 4% requiring the second dose reduction of peginterferon alfa-2b to 0.5 mcg/kg due to adverse events [see Adverse Reactions (6.1)].
Dose reduction in pediatric patients is accomplished by modifying the recommended peginterferon alfa-2b dose in a two-step process from the original starting dose of 60 mcg/m2/week, to 40 mcg/m2/week, then to 20 mcg/m2/week, if needed (see Table 4). In the pediatric combination therapy trial, dose reductions occurred in 25% of subjects receiving peginterferon alfa-2b 60 mcg/m2 weekly and RIBASPHERE 15 mg/kg daily. Dose reduction in pediatric patients is accomplished by modifying the recommended RIBASPHERE dose from the original starting dose of 15 mg/kg daily in a two-step process to 12 mg/kg/day, then to 8 mg/kg/day, if needed (see Table 4).
RIBASPHERE should not be used in patients with creatinine clearance less than 50 mL/min. Patients with impaired renal function and those over the age of 50 should be carefully monitored with respect to development of anemia [see Warnings and Precautions (5.2), Use in Specific Populations (8.5), and Clinical Pharmacology (12.3)].
RIBASPHERE should be administered with caution to patients with pre-existing cardiac disease. Patients should be assessed before commencement of therapy and should be appropriately monitored during therapy. If there is any deterioration of cardiovascular status, therapy should be stopped [see Warnings and Precautions (5.2)].
For patients with a history of stable cardiovascular disease, a permanent dose reduction is required if the hemoglobin decreases by greater than or equal to 2 g/dL during any 4-week period. In addition, for these cardiac history patients, if the hemoglobin remains less than 12 g/dL after 4 weeks on a reduced dose, the patient should discontinue combination therapy.
It is recommended that a patient whose hemoglobin level falls below 10 g/dL have his/her RIBASPHERE dose modified or discontinued per Table 4 [see Warnings and Precautions (5.2)].
| Laboratory Parameters | Reduce RIBASPHERE Daily Dose
(see note 1) if: | Reduce Peginterferon alfa‑2b or Interferon alfa‑2b Dose (see note 2) if: | Discontinue Therapy if: |
|---|---|---|---|
| Note 1: Adult patients: 1st dose reduction of ribavirin is by 200 mg/day (except in patients receiving the 1,400 mg, dose reduction should be by 400 mg/day). If needed, 2nd dose reduction of ribavirin is by an additional 200 mg/day. Patients whose dose of ribavirin is reduced to 600 mg daily receive one 200 mg capsule in the morning and two 200 mg capsules in the evening. Pediatric patients: 1st dose reduction of ribavirin is to 12 mg/kg/day, 2nd dose reduction of ribavirin is to 8 mg/kg/day. |
|||
| Note 2: Adult patients treated with RIBASPHERE and Peginterferon alfa-2b: 1st dose reduction of Peginterferon alfa-2b is to 1 mcg/kg/week. If needed, 2nd dose reduction of Peginterferon alfa-2b is to 0.5 mcg/kg/week. Pediatric patients treated with RIBASPHERE and Peginterferon alfa-2b: 1st dose reduction of Peginterferon alfa-2b is to 40 mcg/m2/week, 2nd dose reduction of Peginterferon alfa-2b is to 20 mcg/m2/week. For patients on Ribavirin/Interferon alfa-2b combination therapy: reduce Interferon alfa-2b dose by 50%. |
|||
|
|
|||
|
WBC |
N/A |
1.0 to <1.5 x 109/L |
<1.0 x 109/L |
|
Neutrophils |
N/A |
0.5 to <0.75 x 109/L |
<0.5 x 109/L |
|
Platelets |
N/A |
25 to <50 x 109/L (adults) |
<25 x 109/L (adults) |
|
N/A |
50 to <70 x 109/L (pediatrics) |
<50 x 109/L (pediatrics) |
|
|
Creatinine |
N/A |
N/A |
>2 mg/dL (pediatrics) |
|
Hemoglobin in patients without history of cardiac disease |
8.5 to <10 g/dL |
N/A |
<8.5 g/dL |
|
Reduce RIBASPHERE Dose by 200 mg/day and Peginterferon alfa-2b or Interferon alfa-2b Dose by Half if: | |||
|
Hemoglobin in patients with history of stable cardiac disease*† |
≥2 g/dL decrease in hemoglobin during any four week period during treatment |
<8.5 g/dL or <12 g/dL after four weeks of dose reduction |
|
Refer to labeling for interferon alfa-2b or peginterferon alfa-2b for additional information about how to reduce an interferon alfa-2b or peginterferon alfa-2b dose.
2.5 Discontinuation of Dosing
Adults
In HCV genotype 1, interferon-alfa-naïve patients receiving peginterferon alfa-2b in combination with ribavirin, discontinuation of therapy is recommended if there is not at least a 2 log10 drop or loss of HCV-RNA at 12 weeks of therapy, or if HCV-RNA levels remain detectable after 24 weeks of therapy. Regardless of genotype, previously treated patients who have detectable HCV-RNA at Week 12 or 24 are highly unlikely to achieve SVR and discontinuation of therapy should be considered.
Pediatrics (3-17 years of age)
It is recommended that patients receiving peginterferon alfa-2b/RIBASPHERE combination (excluding HCV Genotype 2 and 3) be discontinued from therapy at 12 weeks if their treatment Week 12 HCV-RNA dropped less than 2 log10 compared to a pretreatment or at 24 weeks if they have detectable HCV-RNA at treatment Week 24.
4 CONTRAINDICATIONS
RIBASPHERE combination therapy is contraindicated in:
- women who are pregnant. RIBASPHERE may cause fetal harm when administered to a pregnant woman. RIBASPHERE is contraindicated in women who are or may become pregnant. If RIBASPHERE is used during pregnancy, or if the patient becomes pregnant while taking RIBASPHERE, the patient should be apprised of the potential hazard to her fetus [see Warnings and Precautions (5.1), Use in Specific Populations (8.1), and Patient Counseling Information (17.2)]
- men whose female partners are pregnant
- patients with known hypersensitivity reactions such as Stevens-Johnson syndrome, toxic, epidermal necrolysis, and erythema multiforme to ribavirin or any component of the product
- patients with autoimmune hepatitis
- patients with hemoglobinopathies (e.g., thalassemia major, sickle-cell anemia)
- patients with creatinine clearance less than 50 mL/min. [see Use in Specific Populations (8.5) and Clinical Pharmacology (12.3)]
- Coadministration of RIBASPHERE and didanosine is contraindicated because exposure to the active metabolite of didanosine (dideoxyadenosine 5’-triphosphate) is increased. Fatal hepatic failure, as well as peripheral neuropathy, pancreatitis, and symptomatic hyperlactatemia/lactic acidosis have been reported in patients receiving didanosine in combination with ribavirin [see Drug Interactions (7.1)].
5 WARNINGS AND PRECAUTIONS
5.1 Pregnancy
RIBASPHERE (ribavirin capsules) may cause birth defects and death of the unborn child. RIBASPHERE therapy should not be started until a report of a negative pregnancy test has been obtained immediately prior to planned initiation of therapy. Patients should use at least two forms of contraception and have monthly pregnancy tests during treatment and during the 6-month period after treatment has been stopped. Extreme care must be taken to avoid pregnancy in female patients and in female partners of male patients. Ribavirin has demonstrated significant teratogenic and embryocidal effects in all animal species in which adequate studies have been conducted. These effects occurred at doses as low as one twentieth of the recommended human dose of ribavirin. RIBASPHERE therapy should not be started until a report of a negative pregnancy test has been obtained immediately prior to planned initiation of therapy [see Boxed Warning, Contraindications (4), Use in Specific Populations (8.1), and Patient Counseling Information (17.2)].
5.2 Anemia
The primary toxicity of ribavirin is hemolytic anemia, which was observed in approximately 10% of RIBASPHERE/interferon alfa-2b treated subjects in clinical trials. The anemia associated with RIBASPHERE capsules occurs within 1 to 2 weeks of initiation of therapy. Because the initial drop in hemoglobin may be significant, it is advised that hemoglobin or hematocrit be obtained before the start of treatment and at Week 2 and Week 4 of therapy, or more frequently if clinically indicated. Patients should then be followed as clinically appropriate [see Dosage and Administration (2.4, 2.5)].
Fatal and nonfatal myocardial infarctions have been reported in patients with anemia caused by ribavirin. Patients should be assessed for underlying cardiac disease before initiation of ribavirin therapy. Patients with pre-existing cardiac disease should have electrocardiograms administered before treatment, and should be appropriately monitored during therapy. If there is any deterioration of cardiovascular status, therapy should be suspended or discontinued [see Dosage and Administration (2.4, 2.5)]. Because cardiac disease may be worsened by drug-induced anemia, patients with a history of significant or unstable cardiac disease should not use RIBASPHERE.
5.3 Pancreatitis
RIBASPHERE and interferon alfa-2b or peginterferon alfa-2b therapy should be suspended in patients with signs and symptoms of pancreatitis and discontinued in patients with confirmed pancreatitis.
5.4 Pulmonary Disorders
Pulmonary symptoms, including dyspnea, pulmonary infiltrates, pneumonitis, pulmonary hypertension, and pneumonia, have been reported during therapy with ribavirin with alpha interferon combination therapy; occasional cases of fatal pneumonia have occurred. In addition, sarcoidosis or the exacerbation of sarcoidosis has been reported. If there is evidence of pulmonary infiltrates or pulmonary function impairment, the patient should be closely monitored, and if appropriate, combination therapy should be discontinued.
5.5 Ophthalmologic Disorders
Ribavirin is used in combination therapy with alpha interferons. Decrease or loss of vision, retinopathy including macular edema, retinal artery or vein, thrombosis, retinal hemorrhages and cotton wool spots, optic neuritis, papilledema, and serous retinal detachment are induced or aggravated by treatment with alpha interferons. All patients should receive an eye examination at baseline. Patients with pre-existing ophthalmologic disorders (e.g., diabetic or hypertensive retinopathy) should receive periodic ophthalmologic exams during combination therapy with alpha interferon treatment. Any patient who develops ocular symptoms should receive a prompt and complete eye examination. Combination therapy with alpha interferons should be discontinued in patients who develop new or worsening ophthalmologic disorders.
5.6 Laboratory Tests
Peginterferon alfa-2b in combination with ribavirin may cause severe decreases in neutrophil and platelet counts, and hematologic, endocrine (e.g., TSH), and hepatic abnormalities.
Patients on peginterferon alfa-2b/ RIBASPHERE combination therapy should have hematology and blood chemistry testing before the start of treatment and then periodically thereafter. In the adult clinical trial, complete blood counts (including hemoglobin, neutrophil, and platelet counts) and chemistries (including AST, ALT, bilirubin, and uric acid) were measured during the treatment period at Weeks 2, 4, 8, 12, and then at 6-week intervals, or more frequently if abnormalities developed. In pediatric subjects, the same laboratory parameters were evaluated with additional assessment of hemoglobin at treatment Week 6. TSH levels were measured every 12 weeks during the treatment period. HCV-RNA should be measured periodically during treatment [see Dosage and Administration (2)].
5.7 Dental and Periodontal Disorders
Dental and periodontal disorders have been reported in patients receiving ribavirin and interferon or peginterferon combination therapy. In addition, dry mouth could have a damaging effect on teeth and mucous membranes of the mouth during long-term treatment with the combination of ribavirin and pegylated or nonpegylated interferon alfa-2b. Patients should brush their teeth thoroughly twice daily and have regular dental examinations. If vomiting occurs, they should be advised to rinse out their mouth thoroughly afterwards.
5.8 Concomitant Administration of Azathioprine
Pancytopenia (marked decreases in red blood cells, neutrophils, and platelets) and bone marrow suppression have been reported in the literature to occur within 3 to 7 weeks after the concomitant administration of pegylated interferon/ribavirin and azathioprine. In this limited number of patients (n=8), myelotoxicity was reversible within 4 to 6 weeks upon withdrawal of both HCV antiviral therapy and concomitant azathioprine and did not recur upon reintroduction of either treatment alone. Peginterferon alfa-2b, RIBASPHERE and azathioprine should be discontinued for pancytopenia, and pegylated interferon/ribavirin should not be reintroduced with concomitant azathioprine [see Drug Interactions (7.4)].
5.9 Impact on Growth - Pediatric Use
Data on the effects of peginterferon alfa-2b and ribavirin on growth come from an open-label study in subjects 3 through 17 years of age, in which weight and height changes are compared to US normative population data. In general, the weight and height gain of pediatric subjects treated with peginterferon alfa-2b and ribavirin lags behind that predicted by normative population data for the entire length of treatment. Severely inhibited growth velocity (less than 3rd percentile) was observed in 70% of the subjects while on treatment. Following treatment, rebound growth and weight gain occurred in most subjects. Long-term follow-up data in pediatric subjects, however, indicates that peginterferon alfa-2b in combination therapy with ribavirin may induce a growth inhibition that results in reduced adult height in some patients [see Adverse Reactions (6.1)].
Similarly, an impact on growth was seen in subjects after treatment with ribavirin and interferon alfa-2b combination therapy for one year. In a long-term follow-up trial of a limited number of these subjects, combination therapy resulted in reduced final adult height in some subjects [see Adverse Reactions (6.2)].
5.10 Usage Safeguards
Based on results of clinical trials, ribavirin monotherapy is not effective for the treatment of chronic hepatitis C virus infection; therefore, RIBASPHERE capsules must not be used alone. The safety and efficacy of ribavirin capsules have only been established when used together with interferon alfa-2b or peginterferon alfa-2b (not other interferons) as combination therapy.
The safety and efficacy of ribavirin/interferon alfa-2b and peginterferon alfa-2b therapy for the treatment of HIV infection, adenovirus, RSV, parainfluenza, or influenza infections have not been established. RIBASPHERE capsules should not be used for these indications. Ribavirin for inhalation has separate labeling, which should be consulted if ribavirin inhalation therapy is being considered.
There are significant adverse reactions caused by ribavirin/interferon alfa-2b or peginterferon alfa-2b therapy, including severe depression and suicidal ideation, hemolytic anemia, suppression of bone marrow function, autoimmune and infectious disorders, pulmonary dysfunction, pancreatitis, and diabetes. Suicidal ideation or attempts occurred more frequently among pediatric patients, primarily adolescents, compared to adult patients (2.4% versus 1%) during treatment and off-therapy follow-up. Labeling for interferon alfa-2b and peginterferon alfa-2b should be reviewed in their entirety for additional safety information prior to initiation of combination treatment.
6 ADVERSE REACTIONS
Clinical trials with ribavirin in combination with peginterferon alfa-2b or interferon alfa-2b have been conducted in over 7800 subjects from 3 to 76 years of age.
The primary toxicity of ribavirin is hemolytic anemia. Reductions in hemoglobin levels occurred within the first 1 to 2 weeks of oral therapy. Cardiac and pulmonary reactions associated with anemia occurred in approximately 10% of patients [see Warnings and Precautions (5.2)].
Greater than 96% of all subjects in clinical trials experienced one or more adverse reactions. The most commonly reported adverse reactions in adult subjects receiving peginterferon alfa-2b or interferon alfa-2b in combination with ribavirin were injection site inflammation/reaction, fatigue/asthenia, headache, rigors, fevers, nausea, myalgia and anxiety/emotional lability/irritability. The most common adverse reactions in pediatric subjects, ages 3 and older, receiving ribavirin in combination with peginterferon alfa-2b or interferon alfa-2b were pyrexia, headache, neutropenia, fatigue, anorexia, injection site erythema, and vomiting.
The Adverse Reactions section references the following clinical trials:
-
Ribavirin/Peginterferon alfa-2b Combination therapy trials:
- Clinical Study 1 - evaluated peginterferon alfa-2b monotherapy (not further described in this label; see labeling for peginterferon alfa-2b for information about this trial).
- Study 2 - evaluated ribavirin capsules 800 mg/day flat dose in combination with 1.5 mcg/kg/week peginterferon alfa-2b or with interferon alfa-2b.
- Study 3 - evaluated peginterferon alfa-2b/weight-based ribavirin capsules in combination with peginterferon alfa-2b/flat dose ribavirin capsules regimen.
- Study 4- compared two peginterferon alfa-2b (1.5 mcg/kg/week and 1 mcg/kg/week) doses in combination with ribavirin capsules and a third treatment group receiving peginterferon alfa-2a (180 mcg/week)/ribavirin tablets (1000-1200 mg/day).
- Study 5 – evaluated peginterferon alfa-2b (1.5 mcg/kg/week) in combination with weight-based ribavirin capsules in prior treatment failure subjects.
- Peginterferon alfa-2b/ribavirin capsules Combination Therapy in Pediatric Patients
- Ribavirin capsules/interferon alfa-2b Combination Therapy trials for adults and pediatrics
Serious adverse reactions have occurred in approximately 12% of subjects in clinical trials with peginterferon alfa-2b with or without ribavirin [see BOXED WARNING, Warnings and Precautions (5)]. The most common serious events occurring in subjects treated with peginterferon alfa-2b and ribavirin were depression and suicidal ideation [see Warnings and Precautions (5.2)], each occurring at a frequency of less than 1%. Suicidal ideation or attempts occurred more frequently among pediatric patients, primarily adolescents, compared to adult patients (2.4% versus 1%) during treatment and off-therapy follow-up [see Warnings and Precautions (5.10)]. The most common fatal reaction occurring in subjects treated with peginterferon alfa-2b and ribavirin was cardiac arrest, suicide ideation, and suicide attempt [see Warnings and Precautions (5.10)], all occurring in less than 1% of subjects.
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
6.1 Clinical Trials Experience - Ribavirin/Peginterferon alfa-2b Combination Therapy
Adult Subjects
Adverse reactions that occurred in the clinical trial at greater than 5% incidence are provided by treatment group from the ribavirin/peginterferon alfa-2b Combination Therapy (Study 2) in Table 5.
|
|
|||||
|
Percentage of Subjects
|
Percentage of Subjects
|
||||
|
Adverse Reactions |
Peginterferon
|
Interferon
|
Adverse Reactions |
Peginterferon
|
Interferon
|
|
Application Site |
Musculoskeletal | ||||
|
Injection Site Inflammation |
25 |
18 |
Myalgia |
56 |
50 |
|
Injection Site Reaction |
58 |
36 |
Arthralgia |
34 |
28 |
|
Autonomic Nervous System |
Musculoskeletal Pain |
21 |
19 |
||
|
Dry Mouth |
12 |
8 |
Psychiatric | ||
|
Increased Sweating |
11 |
7 |
Insomnia |
40 |
41 |
|
Flushing |
4 |
3 |
Depression |
31 |
34 |
|
Body as a Whole |
Anxiety/Emotional Lability/ |
47 |
47 |
||
|
Fatigue/Asthenia |
66 |
63 |
Concentration Impaired |
17 |
21 |
|
Headache |
62 |
58 |
Agitation |
8 |
5 |
|
Rigors |
48 |
41 |
Nervousness |
6 |
6 |
|
Fever |
46 |
33 |
Reproductive, Female | ||
|
Weight Loss |
29 |
20 |
Menstrual Disorder |
7 |
6 |
|
Right Upper Quadrant Pain |
12 |
6 |
Resistance Mechanism | ||
|
Chest Pain |
8 |
7 |
Viral Infection |
12 |
12 |
|
Malaise |
4 |
6 |
Fungal Infection |
6 |
1 |
|
Central/Peripheral Nervous System |
Respiratory System | ||||
|
Dizziness |
21 |
17 |
Dyspnea |
26 |
24 |
|
Endocrine |
Coughing |
23 |
16 |
||
|
Hypothyroidism |
5 |
4 |
Pharyngitis |
12 |
13 |
|
Gastrointestinal |
Rhinitis |
8 |
6 |
||
|
Nausea |
43 |
33 |
Sinusitis |
6 |
5 |
|
Anorexia |
32 |
27 |
Skin and Appendages | ||
|
Diarrhea |
22 |
17 |
Alopecia |
36 |
32 |
|
Vomiting |
14 |
12 |
Pruritus |
29 |
28 |
|
Abdominal Pain |
13 |
13 |
Rash |
24 |
23 |
|
Dyspepsia |
9 |
8 |
Skin Dry |
24 |
23 |
|
Constipation |
5 |
5 |
Special Senses, Other | ||
|
Hematologic Disorders |
Taste Perversion |
9 |
4 |
||
|
Neutropenia |
26 |
14 |
Vision Disorders | ||
|
Anemia |
12 |
17 |
Vision Blurred |
5 |
6 |
|
Leukopenia |
6 |
5 |
Conjunctivitis |
4 |
5 |
|
Thrombocytopenia |
5 |
2 | |||
|
Liver and Biliary System | |||||
|
Hepatomegaly |
4 |
4 | |||
Table 6 summarizes the treatment-related adverse reactions in Study 4 that occurred at a greater than or equal to 10% incidence.
|
Study 4
|
|||
|
Adverse Reactions |
Peginterferon alfa-2b
|
Peginterferon alfa-2b
|
Peginterferon alfa-2a
|
|
Fatigue |
67 |
68 |
64 |
|
Headache |
50 |
47 |
41 |
|
Nausea |
40 |
35 |
34 |
|
Chills |
39 |
36 |
23 |
|
Insomnia |
38 |
37 |
41 |
|
Anemia |
35 |
30 |
34 |
|
Pyrexia |
35 |
32 |
21 |
|
Injection Site Reactions |
34 |
35 |
23 |
|
Anorexia |
29 |
25 |
21 |
|
Rash |
29 |
25 |
34 |
|
Myalgia |
27 |
26 |
22 |
|
Neutropenia |
26 |
19 |
31 |
|
Irritability |
25 |
25 |
25 |
|
Depression |
25 |
19 |
20 |
|
Alopecia |
23 |
20 |
17 |
|
Dyspnea |
21 |
20 |
22 |
|
Arthralgia |
21 |
22 |
22 |
|
Pruritus |
18 |
15 |
19 |
|
Influenza-like Illness |
16 |
15 |
15 |
|
Dizziness |
16 |
14 |
13 |
|
Diarrhea |
15 |
16 |
14 |
|
Cough |
15 |
16 |
17 |
|
Weight Decreased |
13 |
10 |
10 |
|
Vomiting |
12 |
10 |
9 |
|
Unspecified Pain |
12 |
13 |
9 |
|
Dry Skin |
11 |
11 |
12 |
|
Anxiety |
11 |
11 |
10 |
|
Abdominal Pain |
10 |
10 |
10 |
|
Leukopenia |
9 |
7 |
10 |
The incidence of serious adverse reactions was comparable in all trials. In Study 3, there was a similar incidence of serious adverse reactions reported for the weight-based ribavirin group (12%) and for the flat-dose ribavirin regimen. In Study 2, the incidence of serious adverse reactions was 17% in the peginterferon alfa-2b/ribavirin groups compared to 14% in the interferon alfa-2b/ribavirin group.
In many but not all cases, adverse reactions resolved after dose reduction or discontinuation of therapy. Some subjects experienced ongoing or new serious adverse reactions during the 6-month follow-up period. In Study 2, many subjects continued to experience adverse reactions several months after discontinuation of therapy. By the end of the 6-month follow-up period, the incidence of ongoing adverse reactions by body class in the peginterferon alfa-2b 1.5/ribavirin group was 33% (psychiatric), 20% (musculoskeletal), and 10% (for endocrine and for GI). In approximately 10 to 15% of subjects, weight loss, fatigue, and headache had not resolved.
There have been 31 subject deaths that occurred during treatment or during follow-up in these clinical trials. In Study 1, there was 1 suicide in a subject receiving peginterferon alfa-2b monotherapy and 2 deaths among subjects receiving interferon alfa-2b monotherapy (1 murder/suicide and 1 sudden death). In Study 2, there was 1 suicide in a subject receiving peginterferon alfa-2b/ribavirin combination therapy; and 1 subject death in the interferon alfa-2b/ribavirin group (motor vehicle accident). In Study 3, there were 14 deaths, 2 of which were probable suicides and 1 was an unexplained death in a person with a relevant medical history of depression. In Study 4, there were 12 deaths, 6 of which occurred in subjects who received peginterferon alfa-2b/ribavirin combination therapy, 5 in the peginterferon alfa-2b 1.5 mcg/ribavirin arm (N=1019) and 1 in the peginterferon alfa-2b 1 mcg/ribavirin arm (N=1016), and 6 of which occurred in subjects receiving peginterferon alfa-2a/ribavirin tablets (N=1035); there were 3 suicides that occurred during the off treatment follow-up period in subjects who received peginterferon alfa-2b (1.5 mcg/kg)/ribavirin combination therapy.
In Studies 1 and 2, 10 to 14% of subjects receiving peginterferon alfa-2b, alone or in combination with ribavirin, discontinued therapy compared with 6% treated with interferon alfa-2b alone and 13% treated with interferon alfa-2b in combination with ribavirin. Similarly in Study 3, 15% of subjects receiving peginterferon alfa-2b in combination with weight-based ribavirin and 14% of subjects receiving peginterferon alfa-2b and flat dose ribavirin discontinued therapy due to an adverse reaction. The most common reasons for discontinuation of therapy were related to known interferon effects of psychiatric, systemic (e.g., fatigue, headache), or gastrointestinal adverse reactions. In Study 4, 13% of subjects in the peginterferon alfa-2b 1.5 mcg/ribavirin arm, 10% in the peginterferon alfa-2b 1 mcg/ribavirin arm and 13% in the peginterferon alfa-2a 180 mcg/ribavirin tablets arm discontinued due to adverse events.
In Study 2, dose reductions due to adverse reactions occurred in 42% of subjects receiving peginterferon alfa-2b (1.5 mcg/kg)/ribavirin and in 34% of those receiving interferon alfa-2b/ribavirin. The majority of subjects (57%) weighing 60 kg or less receiving peginterferon alfa-2b (1.5 mcg/kg)/ribavirin required dose reduction. Reduction of interferon was dose-related (peginterferon alfa-2b 1.5 mcg/kg greater than peginterferon alfa-2b 0.5 mcg/kg or interferon alfa-2b), 40%, 27%, 28%, respectively. Dose reduction for ribavirin was similar across all three groups, 33 to 35%. The most common reasons for dose modifications were neutropenia (18%), or anemia (9%) (see Laboratory Values). Other common reasons included depression, fatigue, nausea, and thrombocytopenia. In Study 3, dose modifications due to adverse reactions occurred more frequently with weight-based dosing (WBD) compared to flat dosing (29% and 23%, respectively). In Study 4, 16% of subjects had a dose reduction of peginterferon alfa-2b to 1 mcg/kg in combination with ribavirin, with an additional 4% requiring the second dose reduction of peginterferon alfa-2b to 0.5 mcg/kg due to adverse events compared to 15% of subjects in the peginterferon alfa-2a/ribavirin tablets arm, who required a dose reduction to 135 mcg/week with peginterferon alfa-2a, with an additional 7% in the peginterferon alfa-2a/ribavirin tablets arm requiring second dose reduction to 90 mcg/week with peginterferon alfa-2a.
In the peginterferon alfa-2b/ribavirin combination trials the most common adverse reactions were psychiatric, which occurred among 77% of subjects in Study 2 and 68% to 69% of subjects in Study 3. These psychiatric adverse reactions included most commonly depression, irritability, and insomnia, each reported by approximately 30% to 40% of subjects in all treatment groups. Suicidal behavior (ideation, attempts, and suicides) occurred in 2% of all subjects during treatment or during follow-up after treatment cessation [see Warnings and Precautions (5)]. In Study 4, psychiatric adverse reactions occurred in 58% of subjects in the peginterferon alfa-2b 1.5 mcg/ribavirin arm, 55% of subjects in the peginterferon alfa-2b 1 mcg/ribavirin arm, and 57% of subjects in the peginterferon alfa-2a 180 mcg/ribavirin tablets arm.
Peginterferon alfa-2b induced fatigue or headache in approximately two-thirds of subjects, with fever or rigors in approximately half of the subjects. The severity of some of these systemic symptoms (e.g., fever and headache) tended to decrease as treatment continued. In Studies 1 and 2, application site inflammation and reaction (e.g., bruise, itchiness, and irritation) occurred at approximately twice the incidence with peginterferon alfa-2b therapies (in up to 75% of subjects) compared with interferon alfa-2b. However, injection site pain was infrequent (2 to 3%) in all groups. In Study 3, there was a 23% to 24% incidence overall for injection site reactions or inflammation.
Subjects receiving ribavirin/peginterferon alfa-2b as re-treatment after failing a previous interferon combination regimen reported adverse reactions similar to those previously associated with this regimen during clinical trials of treatment-naïve subjects.
Pediatric Subjects
In general, the adverse-reaction profile in the pediatric population was similar to that observed in adults. In the pediatric trial, the most prevalent adverse reactions in all subjects were pyrexia (80%), headache (62%), neutropenia (33%), fatigue (30%), anorexia (29%), injection-site erythema (29%) and vomiting (27%). The majority of adverse reactions reported in the trial were mild or moderate in severity. Severe adverse reactions were reported in 7% (8/107) of all subjects and included injection site pain (1%), pain in extremity (1%), headache (1%), neutropenia (1%), and pyrexia (4%). Important adverse reactions that occurred in this subject population were nervousness (7%; 7/107), aggression (3%; 3/107), anger (2%; 2/107), and depression (1%; 1/107). Five subjects received levothyroxine treatment, three with clinical hypothyroidism and two with asymptomatic TSH elevations. Weight and height gain of pediatric subjects treated with peginterferon alfa-2b plus ribavirin lagged behind that predicted by normative population data for the entire length of treatment. Severely inhibited growth velocity (less than 3rd percentile) was observed in 70% of the subjects while on treatment.
Dose modifications of peginterferon alfa-2b and/or ribavirin were required in 25% of subjects due to treatment-related adverse reactions, most commonly for anemia, neutropenia and weight loss. Two subjects (2%; 2/107) discontinued therapy as the result of an adverse reaction.
Adverse reactions that occurred with a greater than or equal to 10% incidence in the pediatric trial subjects are provided in Table 7.
|
System Organ Class
|
All Subjects
|
|
Blood and Lymphatic System Disorders | |
|
Neutropenia |
33% |
|
Anemia |
11% |
|
Leukopenia |
10% |
|
Gastrointestinal Disorders | |
|
Abdominal Pain |
21% |
|
Abdominal Pain Upper |
12% |
|
Vomiting |
27% |
|
Nausea |
18% |
|
General Disorders and Administration Site Conditions | |
|
Pyrexia |
80% |
|
Fatigue |
30% |
|
Injection-Site Erythema |
29% |
|
Chills |
21% |
|
Asthenia |
15% |
|
Irritability |
14% |
|
Investigations | |
|
Weight Loss |
19% |
|
Metabolism and Nutrition Disorders | |
|
Anorexia |
29% |
|
Decreased Appetite |
22% |
|
Musculoskeletal and Connective Tissue Disorders | |
|
Arthralgia |
17% |
|
Myalgia |
17% |
|
Nervous System Disorders | |
|
Headache |
62% |
|
Dizziness |
14% |
|
Skin and Subcutaneous Tissue Disorders | |
|
Alopecia |
17% |
Ninety-four of 107 subjects enrolled in a 5 year long-term follow-up trial. The long-term effects on growth were less in those subjects treated for 24 weeks than those treated for 48 weeks. Twenty-four percent of subjects (11/46) treated for 24 weeks and 40% of subjects (19/48) treated for 48 weeks had a >15 percentile height-for-age decrease from pre-treatment to the end of 5 year long-term follow-up compared to pre-treatment baseline percentiles. Eleven percent of subjects (5/46) treated for 24 weeks and 13% of subjects (6/48) treated for 48 weeks were observed to have a decrease from pre-treatment baseline of >30 height-for-age percentiles to the end of the 5 year long-term follow-up. While observed across all age groups, the highest risk for reduced height at the end of long-term follow-up appeared to correlate with initiation of combination therapy during the years of expected peak growth velocity. [See Warnings and Precautions (5.9).]
Laboratory Values
Adult and Pediatric Subjects
The adverse reaction profile in Study 3, which compared peginterferon alfa-2b/weight-based ribavirin combination to a peginterferon alfa-2b/flat dose ribavirin regimen, revealed an increased rate of anemia with weight-based dosing (29% vs. 19% for weight-based vs. flat dose regimens, respectively). However, the majority of cases of anemia were mild and responded to dose reductions.
Changes in selected laboratory values during treatment in combination with ribavirin treatment are described below. Decreases in hemoglobin, leukocytes, neutrophils, and platelets may require dose reduction or permanent discontinuation from therapy [see Dosage and Administration (2.4)]. Changes in selected laboratory values during therapy are described in Table 8. Most of the changes in laboratory values in the peginterferon alfa-2b/ribavirin trial with pediatrics were mild or moderate.
|
|
|||
|
Laboratory Parameters* |
Percentage of Subjects |
||
|
Adults (Study 2) |
Pediatrics |
||
|
Peginterferon alfa-2b/
|
Interferon alfa-2b/
|
Peginterferon alfa-2b/
|
|
|
Hemoglobin (g/dL) | |||
|
9.5 to <11.0 |
26 |
27 |
30 |
|
8.0 to <9.5 |
3 |
3 |
2 |
|
6.5 to 7.9 |
0.2 |
0.2 |
- |
|
Leukocytes (x109/L) | |||
|
2.0 to 2.9 |
46 |
41 |
39 |
|
1.5 to <2.0 |
24 |
8 |
3 |
|
1.0 to 1.4 |
5 |
1 |
- |
|
Neutrophils (x109/L) | |||
|
1.0 to 1.5 |
33 |
37 |
35 |
|
0.75 to <1.0 |
25 |
13 |
26 |
|
0.5 to <0.75 |
18 |
7 |
13 |
|
<0.5 |
4 |
2 |
3 |
|
Platelets (x109/L) | |||
|
70 to 100 |
15 |
5 |
1 |
|
50 to <70 |
3 |
0.8 |
- |
|
30 to 49 |
0.2 |
0.2 |
-- |
|
25 to <50 |
-- |
-- |
1 |
|
Total Bilirubin |
(mg/dL) |
(µmole/L) |
|
|
1.5 to 3.0 |
10 |
13 |
-- |
|
1.26 to 2.59 x ULN† |
-- |
-- |
7 |
|
3.1 to 6.0 |
0.6 |
0.2 |
-- |
|
2.6-5 x ULN† |
-- |
-- |
- |
|
6.1 to 12.0 |
0 |
0.2 |
-- |
|
ALT (U/L) | |||
|
2 x Baseline |
0.6 |
0.2 |
1 |
|
2.1 to 5 x Baseline |
3 |
1 |
5 |
|
5.1 to 10 x Baseline |
0 |
0 |
3 |
Hemoglobin. Hemoglobin levels decreased to less than 11 g/dL in about 30% of subjects in Study 2. In Study 3, 47% of subjects receiving WBD ribavirin and 33% on flat-dose ribavirin had decreases in hemoglobin levels less than 11 g/dL. Reductions in hemoglobin to less than 9 g/dL occurred more frequently in subjects receiving WBD compared to flat dosing (4% and 2%, respectively). In Study 2, dose modification was required in 9% and 13% of subjects in the peginterferon alfa-2b/ribavirin and interferon alfa-2b/ribavirin groups. In Study 4, subjects receiving peginterferon alfa-2b (1.5 mcg/kg)/ribavirin had decreases in hemoglobin levels to between 8.5 to less than 10 g/dL (28%) and to less than 8.5 g/dL (3%), whereas in patients receiving peginterferon alfa-2a 180 mcg/ribavirin tablets these decreases occurred in 26% and 4% of subjects respectively. Hemoglobin levels became stable by treatment Weeks 4-6 on average. The typical pattern observed was a decrease in hemoglobin levels by treatment Week 4 followed by stabilization and a plateau, which was maintained to the end of treatment. In the peginterferon alfa-2b monotherapy trial, hemoglobin decreases were generally mild and dose modifications were rarely necessary [see Dosage and Administration (2.4)].
Neutrophils. Decreases in neutrophil counts were observed in a majority of adult subjects treated with combination therapy with ribavirin in Study 2 (85%) and interferon alfa-2b/ribavirin (60%). Severe potentially life-threatening neutropenia (less than 0.5 x 109/L) occurred in 2% of subjects treated with interferon alfa-2b/ribavirin and in approximately 4% of subjects treated with peginterferon alfa-2b/ribavirin in Study 2. Eighteen percent of subjects receiving peginterferon alfa-2b/ribavirin in Study 2 required modification of interferon dosage. Few subjects (less than 1%) required permanent discontinuation of treatment. Neutrophil counts generally returned to pre-treatment levels 4 weeks after cessation of therapy [see Dosage and Administration (2.4)].
Platelets. Platelet counts decreased to less than 100,000/mm3 in approximately 20% of subjects treated with peginterferon alfa-2b alone or with ribavirin and in 6% of adult subjects treated with interferon alfa-2b/ribavirin. Severe decreases in platelet counts (less than 50,000/mm3) occur in less than 4% of adult subjects. Patients may require discontinuation or dose modification as a result of platelet decreases [see Dosage and Administration (2.4)]. In Study 2, 1% or 3% of subjects required dose modification of interferon alfa-2b or peginterferon alfa-2b, respectively. Platelet counts generally returned to pretreatment levels 4 weeks after the cessation of therapy.
Thyroid Function. Development of TSH abnormalities, with or without clinical manifestations, is associated with interferon therapies. In Study 2, clinically apparent thyroid disorders occurred among subjects treated with either interferon alfa-2b or peginterferon alfa-2b (with or without ribavirin) at a similar incidence (5% for hypothyroidism and 3% for hyperthyroidism). Subjects developed new onset TSH abnormalities while on treatment and during the follow-up period. At the end of the follow-up period 7% of subjects still had abnormal TSH values.
Bilirubin and uric acid. In Study 2, 10 to 14% of subjects developed hyperbilirubinemia and 33 to 38% developed hyperuricemia in association with hemolysis. Six subjects developed mild to moderate gout.
6.2 Clinical Trials Experience - Ribavirin/Interferon alfa-2b Combination Therapy
Adult Subjects
In clinical trials, 19% and 6% of previously untreated and relapse subjects, respectively, discontinued therapy due to adverse reactions in the combination arms compared to 13% and 3% in the interferon arms. Selected treatment-related adverse reactions that occurred in the US trials with greater than or equal to 5% incidence are provided by treatment group (see Table 9). In general, the selected treatment-related adverse reactions were reported with lower incidence in the international trials as compared to the US trials, with the exception of asthenia, influenza-like symptoms, nervousness, and pruritus.
Pediatric Subjects
In clinical trials of 118 pediatric subjects 3 to 16 years of age, 6% discontinued therapy due to adverse reactions. Dose modifications were required in 30% of subjects, most commonly for anemia and neutropenia. In general, the adverse-reaction profile in the pediatric population was similar to that observed in adults. Injection site disorders, fever, anorexia, vomiting, and emotional lability occurred more frequently in pediatric subjects compared to adult subjects. Conversely, pediatric subjects experienced less fatigue, dyspepsia, arthralgia, insomnia, irritability, impaired concentration, dyspnea, and pruritus compared to adult subjects. Selected treatment-related adverse reactions that occurred with greater than or equal to 5% incidence among all pediatric subjects who received the recommended dose of ribavirin/interferon alfa-2b combination therapy are provided in Table 9.
|
|
|||||||
|
Subjects Reporting Adverse Reactions* |
Percentage of Subjects |
||||||
|
US Previously Untreated Study |
US Relapse Study |
Pediatric Subjects |
|||||
|
24 weeks of treatment |
48 weeks of treatment |
24 weeks of treatment |
48 weeks of treatment |
||||
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
|
|
Application Site Disorders | |||||||
|
Injection Site Inflammation |
13 |
10 |
12 |
14 |
6 |
8 |
14 |
|
Injection Site Reaction |
7 |
9 |
8 |
9 |
5 |
3 |
19 |
|
Body as a Whole -
| |||||||
|
Headache |
63 |
63 |
66 |
67 |
66 |
68 |
69 |
|
Fatigue |
68 |
62 |
70 |
72 |
60 |
53 |
58 |
|
Rigors |
40 |
32 |
42 |
39 |
43 |
37 |
25 |
|
Fever |
37 |
35 |
41 |
40 |
32 |
36 |
61 |
|
Influenza-like Symptoms |
14 |
18 |
18 |
20 |
13 |
13 |
31 |
|
Asthenia |
9 |
4 |
9 |
9 |
10 |
4 |
5 |
|
Chest Pain |
5 |
4 |
9 |
8 |
6 |
7 |
5 |
|
Central & Peripheral
| |||||||
|
Dizziness |
17 |
15 |
23 |
19 |
26 |
21 |
20 |
|
Gastrointestinal
| |||||||
|
Nausea |
38 |
35 |
46 |
33 |
47 |
33 |
33 |
|
Anorexia |
27 |
16 |
25 |
19 |
21 |
14 |
51 |
|
Dyspepsia |
14 |
6 |
16 |
9 |
16 |
9 |
<1 |
|
Vomiting |
11 |
10 |
9 |
13 |
12 |
8 |
42 |
|
Musculoskeletal
| |||||||
|
Myalgia |
61 |
57 |
64 |
63 |
61 |
58 |
32 |
|
Arthralgia |
30 |
27 |
33 |
36 |
29 |
29 |
15 |
|
Musculoskeletal Pain |
20 |
26 |
28 |
32 |
22 |
28 |
21 |
|
Psychiatric Disorders | |||||||
|
Insomnia |
39 |
27 |
39 |
30 |
26 |
25 |
14 |
|
Irritability |
23 |
19 |
32 |
27 |
25 |
20 |
10 |
|
Depression |
32 |
25 |
36 |
37 |
23 |
14 |
13 |
|
Emotional Lability |
7 |
6 |
11 |
8 |
12 |
8 |
16 |
|
Concentration Impaired |
11 |
14 |
14 |
14 |
10 |
12 |
5 |
|
Nervousness |
4 |
2 |
4 |
4 |
5 |
4 |
3 |
|
Respiratory
| |||||||
|
Dyspnea |
19 |
9 |
18 |
10 |
17 |
12 |
5 |
|
Sinusitis |
9 |
7 |
10 |
14 |
12 |
7 |
<1 |
|
Skin and
| |||||||
|
Alopecia |
28 |
27 |
32 |
28 |
27 |
26 |
23 |
|
Rash |
20 |
9 |
28 |
8 |
21 |
5 |
17 |
|
Pruritus |
21 |
9 |
19 |
8 |
13 |
4 |
12 |
|
Special Senses,
| |||||||
|
Taste Perversion |
7 |
4 |
8 |
4 |
6 |
5 |
<1 |
During a 48-week course of therapy there was a decrease in the rate of linear growth (mean percentile assignment decrease of 7%) and a decrease in the rate of weight gain (mean percentile assignment decrease of 9%). A general reversal of these trends was noted during the 24-week post-treatment period. Long-term data in a limited number of patients, however, suggests that combination therapy may induce a growth inhibition that results in reduced final adult height in some patients [see Warnings and Precautions (5.9)].
Laboratory Values
Changes in selected hematologic values (hemoglobin, white blood cells, neutrophils, and platelets) during therapy are described below (see Table 10).
Hemoglobin. Hemoglobin decreases among subjects receiving ribavirin therapy began at Week 1, with stabilization by Week 4. In previously untreated subjects treated for 48 weeks, the mean maximum decrease from baseline was 3.1 g/dL in the US trial and 2.9 g/dL in the international trial. In relapse subjects, the mean maximum decrease from baseline was 2.8 g/dL in the US trial and 2.6 g/dL in the international trial. Hemoglobin values returned to pretreatment levels within 4 to 8 weeks of cessation of therapy in most subjects.
Bilirubin and Uric Acid. Increases in both bilirubin and uric acid, associated with hemolysis, were noted in clinical trials. Most were moderate biochemical changes and were reversed within 4 weeks after treatment discontinuation. This observation occurred most frequently in subjects with a previous diagnosis of Gilbert’s syndrome. This has not been associated with hepatic dysfunction or clinical morbidity.
|
Percentage of Subjects |
|||||||
|
US Previously Untreated Study |
US Relapse Study |
Pediatric Subjects |
|||||
|
24 weeks of treatment |
48 weeks of treatment |
24 weeks of treatment |
48 weeks of treatment |
||||
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
|
|
Hemoglobin (g/dL) | |||||||
|
9.5 to 10.9 |
24 |
1 |
32 |
1 |
21 |
3 |
24 |
|
8.0 to 9.4 |
5 |
0 |
4 |
0 |
4 |
0 |
3 |
|
6.5 to 7.9 |
0 |
0 |
0 |
0.4 |
0 |
0 |
0 |
|
< 6.5 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Leukocytes (x109/L) | |||||||
|
2.0 to 2.9 |
40 |
20 |
38 |
23 |
45 |
26 |
35 |
|
1.5 to 1.9 |
4 |
1 |
9 |
2 |
5 |
3 |
8 |
|
1.0 to 1.4 |
0.9 |
0 |
2 |
0 |
0 |
0 |
0 |
|
< 1.0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Neutrophils (x109/L) | |||||||
|
1.0 to 1.49 |
30 |
32 |
31 |
44 |
42 |
34 |
37 |
|
0.75 to 0.99 |
14 |
15 |
14 |
11 |
16 |
18 |
15 |
|
0.5 to 0.74 |
9 |
9 |
14 |
7 |
8 |
4 |
16 |
|
< 0.5 |
11 |
8 |
11 |
5 |
5 |
8 |
3 |
|
Platelets (x109/L) | |||||||
|
70 to 99 |
9 |
11 |
11 |
14 |
6 |
12 |
0.8 |
|
50 to 69 |
2 |
3 |
2 |
3 |
0 |
5 |
2 |
|
30 to 49 |
0 |
0.4 |
0 |
0.4 |
0 |
0 |
0 |
|
< 30 |
0.9 |
0 |
1 |
0.9 |
0 |
0 |
0 |
|
Total Bilirubin (mg/dL) | |||||||
|
1.5 to 3.0 |
27 |
13 |
32 |
13 |
21 |
7 |
2 |
|
3.1 to 6.0 |
0.9 |
0.4 |
2 |
0 |
3 |
0 |
0 |
|
6.1 to 12.0 |
0 |
0 |
0.4 |
0 |
0 |
0 |
0 |
|
> 12.0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
6.3 Postmarketing Experiences
The following adverse reactions have been identified and reported during post approval use of ribavirin in combination with interferon alfa-2b or peginterferon alfa-2b. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System disorders
- Pure red cell aplasia, aplastic anemia
Ear and Labyrinth disorders
- Hearing disorder, vertigo
Respiratory, Thoracic and Mediastinal disorders
- Pulmonary hypertension
Eye disorders
- Serous retinal detachment
Endocrine disorders
- Diabetes
7 DRUG INTERACTIONS
7.1 Didanosine
Exposure to didanosine or its active metabolite (dideoxyadenosine 5’-triphosphate) is increased when didanosine is coadministered with ribavirin, which could cause or worsen clinical toxicities; therefore, coadministration of RIBASPHERE capsules and didanosine is contraindicated. Reports of fatal hepatic failure, as well as peripheral neuropathy, pancreatitis, and symptomatic hyperlactatemia/lactic acidosis have been reported in clinical trials.
7.2 Nucleoside Analogues
Hepatic decompensation (some fatal) has occurred in cirrhotic HIV/HCV co-infected patients receiving combination antiretroviral therapy for HIV and interferon alpha and ribavirin. Adding treatment with alpha interferons alone or in combination with ribavirin may increase the risk in this patient population. Patients receiving interferon with ribavirin and nucleoside reverse transcriptase inhibitors (NRTIs) should be closely monitored for treatment- associated toxicities, especially hepatic decompensation and anemia. Discontinuation of NRTIs should be considered as medically appropriate (see labeling for individual NRTI product). Dose reduction or discontinuation of interferon, ribavirin, or both should also be considered if worsening clinical toxicities are observed, including hepatic decompensation (e.g., Child-Pugh greater than 6).
Ribavirin may antagonize the cell culture antiviral activity of stavudine and zidovudine against HIV. Ribavirin has been shown in cell culture to inhibit phosphorylation of lamivudine, stavudine, and zidovudine, which could lead to decreased antiretroviral activity. However, in a study with another pegylated interferon in combination with ribavirin, no pharmacokinetic (e.g., plasma concentrations or intracellular triphosphorylated active metabolite concentrations) or pharmacodynamic (e.g., loss of HIV/HCV virologic suppress) interaction was observed when ribavirin and lamivudine (n=18), stavudine (n=10), or zidovudine (n=6) were coadministered as part of a multidrug regimen in HIV/HCV co-infected subjects. Therefore, concomitant use of ribavirin with either of these drugs should be used with caution.
7.3 Drugs Metabolized by Cytochrome P-450
Results of in vitro studies using both human and rat liver microsome preparations indicated little or no cytochrome P-450 enzyme-mediated metabolism of ribavirin, with minimal potential for P-450 enzyme-based drug interactions.
No pharmacokinetic interactions were noted between interferon alfa-2b and ribavirin capsules in a multiple-dose pharmacokinetic study.
7.4 Azathioprine
The use of ribavirin for the treatment of chronic hepatitis C in patients receiving azathioprine has been reported to induce severe pancytopenia and may increase the risk of azathioprine-related myelotoxicity. Inosine monophosphate dehydrogenase (IMDH) is required for one of the metabolic pathways of azathioprine. Ribavirin is known to inhibit IMDH, thereby leading to accumulation of an azathioprine metabolite, 6-methylthioinosine monophosphate (6-MTITP), which is associated with myelotoxicity (neutropenia, thrombocytopenia, and anemia). Patients receiving azathioprine with ribavirin should have complete blood counts, including platelet counts, monitored weekly for the first month, twice monthly for the second and third months of treatment, then monthly or more frequently if dosage or other therapy changes are necessary [see Warnings and Precautions (5.8)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category X
[See Contraindications (4), Warnings and Precautions (5.1), and Nonclinical Toxicology (13.1)].
Treatment and Post-treatment:
Potential Risk to the Fetus:
Ribavirin is known to accumulate in intracellular components from where it is cleared very slowly. It is not known whether ribavirin contained in sperm will exert a potential teratogenic effect upon fertilization of the ova. In a study in rats, it was concluded that dominant lethality was not induced by ribavirin at doses up to 200 mg/kg for 5 days (estimated human equivalent doses of 7.14 to 28.6 mg/kg, based on body surface area adjustment for a 60 kg adult; up to 1.7 times the maximum recommended human dose of ribavirin). However, because of the potential human teratogenic effects of ribavirin, male patients should be advised to take every precaution to avoid risk of pregnancy for their female partners.
Women of childbearing potential should not receive RIBASPHERE unless they are using effective contraception (two reliable forms) during the therapy period. In addition, effective contraception should be utilized for 6 months post-therapy based on a multiple-dose half-life (t1/2) of ribavirin of 12 days.
Male patients and their female partners must practice effective contraception (two reliable forms) during treatment with RIBASPHERE and for the 6-month post-therapy period (e.g., 15 half-lives for ribavirin clearance from the body).
A Ribavirin Pregnancy Registry has been established to monitor maternal-fetal outcomes of pregnancies in female patients and female partners of male patients exposed to ribavirin during treatment and for 6 months following cessation of treatment. Physicians and patients are encouraged to report such cases by calling 1-800-593-2214.
8.3 Nursing Mothers
It is not known whether the RIBASPHERE product is excreted in human milk. Because of the potential for serious adverse reactions from the drug in nursing infants, a decision should be made whether to discontinue nursing or to delay or discontinue RIBASPHERE.
8.4 Pediatric Use
Safety and effectiveness of RIBASPHERE in combination with peginterferon alfa-2b has not been established in pediatric patients below the age of 3 years. For treatment with ribavirin/interferon alfa-2b, evidence of disease progression, such as hepatic inflammation and fibrosis, as well as prognostic factors for response, HCV genotype and viral load should be considered when deciding to treat a pediatric patient. The benefits of treatment should be weighed against the safety findings observed.
Long-term follow-up data in pediatric subjects indicates that ribavirin in combination with peginterferon alfa-2b or with interferon alfa-2b may induce a growth inhibition that results in reduced height in some patients [see Warnings and Precautions (5.9) and Adverse Reactions (6.1, 6.2)].
Suicidal ideation or attempts occurred more frequently among pediatric patients, primarily adolescents, compared to adult patients (2.4% vs. 1%) during treatment and off-therapy follow-up [see Warnings and Precautions (5.10)]. As in adult patients, pediatric patients experienced other psychiatric adverse reactions (e.g., depression, emotional lability, somnolence), anemia, and neutropenia [see Warnings and Precautions (5.2)].
8.5 Geriatric Use
Clinical trials of ribavirin/interferon alfa-2b or peginterferon alfa-2b therapy did not include sufficient numbers of subjects aged 65 and over to determine if they respond differently from younger subjects.
Ribavirin is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients often have decreased renal function, care should be taken in dose selection. Renal function should be monitored and dosage adjustments should be made accordingly. RIBASPHERE should not be used in patients with creatinine clearance less than 50 mL/min [see Contraindications (4)].
In general, RIBASPHERE capsules should be administered to elderly patients cautiously, starting at the lower end of the dosing range, reflecting the greater frequency of decreased hepatic and cardiac function, and of concomitant disease or other drug therapy. In clinical trials, elderly subjects had a higher frequency of anemia (67%) than younger patients (28%) [see Warnings and Precautions (5.2)].
8.6 Organ Transplant Recipients
The safety and efficacy of interferon alfa-2b and peginterferon alfa-2b alone or in combination with RIBASPHERE for the treatment of hepatitis C in liver or other organ transplant recipients have not been established. In a small (n=16) single-center, uncontrolled case experience, renal failure in renal allograft recipients receiving interferon alpha and ribavirin combination therapy was more frequent than expected from the center’s previous experience with renal allograft recipients not receiving combination therapy. The relationship of the renal failure to renal allograft rejection is not clear.
10 OVERDOSAGE
There is limited experience with overdosage. Acute ingestion of up to 20 g of ribavirin capsules, interferon alfa-2b ingestion of up to 120 million units, and subcutaneous doses of interferon alfa-2b up to 10 times the recommended doses have been reported. Primary effects that have been observed are increased incidence and severity of the adverse reactions related to the therapeutic use of interferon alfa-2b and ribavirin. However, hepatic enzyme abnormalities, renal failure, hemorrhage, and myocardial infarction have been reported with administration of single subcutaneous doses of interferon alfa-2b that exceed dosing recommendations.
There is no specific antidote for interferon alfa-2b or RIBASPHERE overdose, and hemodialysis and peritoneal dialysis are not effective for treatment of overdose of these agents.
11 DESCRIPTION
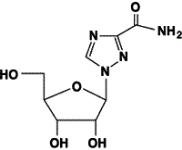
RIBASPHERE® (ribavirin capsules USP) is a synthetic nucleoside analogue (purine analogue). The chemical name of ribavirin is 1-ß-D-ribofuranosyl-1 H-1,2,4-triazole-3-carboxamide and has the following structural formula (see Figure 1):
Ribavirin is a white, crystalline powder. It is freely soluble in water and slightly soluble in anhydrous alcohol. The empirical formula is C 8H12N4O5 and the molecular weight is 244.21.
RIBASPHERE® (ribavirin capsules USP) consists of white pellets in a white, opaque, gelatin capsule. Each capsule contains 200 mg ribavirin and the inactive ingredients: Croscarmellose Sodium, NF, Lactose Monohydrate, NF, Microcrystalline Cellulose, NF, and Povidone, USP. The capsule shell consists of gelatin and titanium dioxide. The capsule is printed horizontally with "riba 200" on both the body and the cap of the capsule using edible, green pharmaceutical ink which is made of butyl alcohol, NF, Yellow Iron Oxide, NF, dehydrated alcohol, USP, FD&C Blue #2 Aluminum Lake, isopropyl alcohol, USP, propylene glycol, USP, Shellac, NF, strong ammonia solution, NF, and titanium dioxide.
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Single- and multiple-dose pharmacokinetic properties in adults are summarized in Table 11. Ribavirin was rapidly and extensively absorbed following oral administration. However, due to first-pass metabolism, the absolute bioavailability averaged 64% (44%). There was a linear relationship between dose and AUCtf (AUC from time zero to last measurable concentration) following single doses of 200 to 1200 mg ribavirin. The relationship between dose and Cmax was curvilinear, tending to asymptote above single doses of 400 to 600 mg.
Upon multiple oral dosing, based on AUC12 hr, a 6-fold accumulation of ribavirin was observed in plasma. Following oral dosing with 600 mg twice daily, steady-state was reached by approximately 4 weeks, with mean steady-state plasma concentrations of 2200 ng/mL (37%). Upon discontinuation of dosing, the mean half-life was 298 (30%) hours, which probably reflects slow elimination from nonplasma compartments.
Effect of Antacid on Absorption of Ribavirin
Coadministration of ribavirin capsules with an antacid containing magnesium, aluminum, and simethicone resulted in a 14% decrease in mean ribavirin AUCtf. The clinical relevance of results from this single-dose study is unknown.
|
|
||
|
Parameter |
Ribavirin Capsules |
|
|
Single Dose
|
Multiple Dose
|
|
|
Tmax (hr) |
1.7 (46)* |
3 (60) |
|
Cmax (ng/mL) |
782 (37) |
3680 (85) |
|
AUCtf (ng∙hr/mL) |
13,400 (48) |
228,000 (25) |
|
T1/2 (hr) |
43.6 (47) |
298 (30) |
|
Apparent Volume of Distribution (L) |
2825 (9)† | |
|
Apparent Clearance (L/hr) |
38.2 (40) | |
|
Absolute Bioavailability |
64% (44)‡ | |
Tissue Distribution: Ribavirin transport into nonplasma compartments has been most extensively studied in red blood cells, and has been identified to be primarily via an es-type equilibrative nucleoside transporter. This type of transporter is present on virtually all cell types and may account for the extensive volume of distribution. Ribavirin does not bind to plasma proteins.
Metabolism and Excretion: Ribavirin has two pathways of metabolism: (i) a reversible phosphorylation pathway in nucleated cells; and (ii) a degradative pathway involving deribosylation and amide hydrolysis to yield a triazole carboxylic acid metabolite. Ribavirin and its triazole carboxamide and triazole carboxylic acid metabolites are excreted renally. After oral administration of 600 mg of 14C-ribavirin, approximately 61% and 12% of the radioactivity was eliminated in the urine and feces, respectively, in 336 hours. Unchanged ribavirin accounted for 17% of the administered dose.
Special Populations:
Renal Dysfunction
The pharmacokinetics of ribavirin were assessed after administration of a single oral dose (400 mg) of ribavirin to non HCV-infected subjects with varying degrees of renal dysfunction. The mean AUCtf value was threefold greater in subjects with creatinine clearance values between 10 to 30 mL/min when compared to control subjects (creatinine clearance greater than 90 mL/min). In subjects with creatinine clearance values between 30 to 60 mL/min, AUCtf was twofold greater when compared to control subjects. The increased AUCtf appears to be due to reduction of renal and nonrenal clearance in these subjects. Phase 3 efficacy trials included subjects with creatinine clearance values greater than 50 mL/min. The multiple-dose pharmacokinetics of ribavirin cannot be accurately predicted in patients with renal dysfunction. Ribavirin is not effectively removed by hemodialysis. Patients with creatinine clearance less than 50 mL/min should not be treated with RIBASPHERE [see Contraindications (4)].
Hepatic Dysfunction
The effect of hepatic dysfunction was assessed after a single oral dose of ribavirin (600 mg). The mean AUCtf values were not significantly different in subjects with mild, moderate, or severe hepatic dysfunction (Child-Pugh Classification A, B, or C) when compared to control subjects. However, the mean Cmax values increased with severity of hepatic dysfunction and was twofold greater in subjects with severe hepatic dysfunction when compared to control subjects.
Elderly Patients
Pharmacokinetic evaluations in elderly subjects have not been performed.
Gender
There were no clinically significant pharmacokinetic differences noted in a single-dose trial of 18 male and 18 female subjects.
Pediatric Patients
Multiple-dose pharmacokinetic properties for ribavirin capsules and interferon alfa-2b in pediatric subjects with chronic hepatitis C between 5 and 16 years of age are summarized in Table 12. The pharmacokinetics of ribavirin and interferon alfa-2b (dose-normalized) are similar in adults and pediatric subjects.
| Note: numbers in parenthesis indicate % coefficient of variation. | |||||
|
|
|||||
|
Parameter |
Ribavirin 15 mg/kg/day as
|
Interferon alfa-2b
|
|||
|
Tmax (hr) |
1.9 (83) |
5.9 (36) |
|||
|
Cmax (ng/mL) |
3275 (25) |
51 (48) |
|||
|
AUC* |
29,774 (26) |
622 (48) |
|||
|
Apparent Clearance L/hr/kg |
0.27 (27) |
ND† |
|||
A clinical trial in pediatric subjects with chronic hepatitis C between 3 and 17 years of age was conducted in which pharmacokinetics for peginterferon alfa-2b and ribavirin capsules were evaluated. In pediatric subjects receiving body surface area-adjusted dosing of peginterferon alfa-2b at 60 mcg/m2/week, the log transformed ratio estimate of exposure during the dosing interval was predicted to be 58% [90% CI: 141%, 177%] higher than observed in adults receiving 1.5 mcg/kg/week. The pharmacokinetics of ribavirin (dose-normalized) in this trial were similar to those reported in a prior study of ribavirin in combination with interferon alfa-2b in pediatric subjects and in adults.
Effect of Food on Absorption of Ribavirin
Both AUCtf and Cmax increased by 70% when ribavirin capsules were administered with a high-fat meal (841 kcal, 53.8 g fat, 31.6 g protein, and 57.4 g carbohydrate) in a single-dose pharmacokinetic study [see Dosage and Administration (2)].
12.4 Microbiology
Mechanism of Action
The mechanism by which ribavirin contributes to its antiviral efficacy in the clinic is not fully understood. Ribavirin has direct antiviral activity in tissue culture against many RNA viruses. Ribavirin increases the mutation frequency in the genomes of several viruses and ribavirin triphosphate inhibits HCV polymerase in a biochemical reaction.
Antiviral Activity in Cell Culture
The antiviral activity of ribavirin in the HCV-replicon is not well understood and has not been defined because of the cellular toxicity of ribavirin. Direct antiviral activity has been observed in tissue culture of other RNA viruses. The anti-HCV activity of interferon was demonstrated in cell containing self-replicating HCV-RNS (HCV replicon cells) or HCV infection.
Resistance
HCV genotypes show wide variability in their response to pegylated recombinant human interferon/ribavirin therapy. Genetic changes associated with the variable response have not been identified.
Cross-resistance
There is no reported cross-resistance between pegylated/non-pegylated interferons and ribavirin.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Ribavirin did not cause an increase in any tumor type when administered for 6 months in the transgenic p53 deficient mouse model at doses up to 300 mg/kg (estimated human equivalent of 25 mg/kg based on body surface area adjustment for a 60 kg adult; approximately 1.9 times the maximum recommended human daily dose). Ribavirin was noncarcinogenic when administered for 2 years to rats at doses up to 40 mg/kg (estimated human equivalent of 5.71 mg/kg based on body surface area adjustment for a 60 kg adult).
Mutagenesis
Ribavirin demonstrated increased incidences of mutation and cell transformation in multiple genotoxicity assays. Ribavirin was active in the Balb/3T3 In Vitro Cell Transformation Assay. Mutagenic activity was observed in the mouse lymphoma assay, and at doses of 20 to 200 mg/kg (estimated human equivalent of 1.67 to 16.7 mg/kg, based on body surface area adjustment for a 60 kg adult; 0.1 to 1 times the maximum recommended human 24-hour dose of ribavirin) in a mouse micronucleus assay. A dominant lethal assay in rats was negative, indicating that if mutations occurred in rats they were not transmitted through male gametes.
Impairment of Fertility
Ribavirin demonstrated significant embryocidal and teratogenic effects at doses well below the recommended human dose in all animal species in which adequate studies have been conducted. Malformations of the skull, palate, eye, jaw, limbs, skeleton, and gastrointestinal tract were noted. The incidence and severity of teratogenic effects increased with escalation of the drug dose. Survival of fetuses and offspring was reduced. In conventional embryotoxicity/teratogenicity studies in rats and rabbits, observed no-effect dose levels were well below those for proposed clinical use (0.3 mg/kg/day for both the rat and rabbit; approximately 0.06 times the recommended human 24-hour dose of ribavirin). No maternal toxicity or effects on offspring were observed in a peri/postnatal toxicity study in rats dosed orally at up to 1 mg/kg/day (estimated human equivalent dose of 0.17 mg/kg based on body surface area adjustment for a 60 kg adult; approximately 0.01 times the maximum recommended human 24-hour dose of ribavirin) [see Contraindications (4), and Warnings and Precautions (5.1)].
Fertile women and partners of fertile women should not receive RIBASPHERE unless the patient and his/her partner are using effective contraception (two reliable forms). Based on a multiple-dose half-life (t1/2) of ribavirin of 12 days, effective contraception must be utilized for 6 months post-therapy (e.g., 15 half-lives of clearance for ribavirin).
RIBASPHERE should be used with caution in fertile men. In studies in mice to evaluate the time course and reversibility of ribavirin-induced testicular degeneration at doses of 15 to 150 mg/kg/day (estimated human equivalent of 1.25 to 12.5 mg/kg/day, based on body surface area adjustment for a 60kg adult; 0.1-0.8 times the maximum human 24-hour dose of ribavirin) administered for 3 or 6 months, abnormalities in sperm occurred. Upon cessation of treatment, essentially total recovery from ribavirin-induced testicular toxicity was apparent within 1 or 2 spermatogenesis cycles.
13.2 Animal Toxicology and/or Pharmacology
Long-term studies in the mouse and rat [18 to 24 months; doses of 20 to 75 and 10 to 40 mg/kg/day respectively, (estimated human equivalent doses of 1.67 to 6.25 and 1.43 to 5.71 mg/kg/day, respectively, based on body surface area adjustment for a 60 kg adult; approximately 0.1 to 0.4 times the maximum human 24-hour dose of ribavirin)] have demonstrated a relationship between chronic ribavirin exposure and increased incidences of vascular lesions (microscopic hemorrhages) in mice. In rats, retinal degeneration occurred in controls, but the incidence was increased in ribavirin-treated rats.
In a study in which rat pups were dosed postnatally with ribavirin at doses of 10, 25, and 50 mg/kg/day, drug-related deaths occurred at 50 mg/kg (at rat pup plasma concentrations below human plasma concentrations at the human therapeutic dose) between study Days 13 and 48. Rat pups dosed from postnatal Days 7 through 63 demonstrated a minor, dose-related decrease in overall growth at all doses, which was subsequently manifested as slight decreases in body weight, crown-rump length, and bone length. These effects showed evidence of reversibility, and no histopathological effects on bone were observed. No ribavirin effects were observed regarding neurobehavioral or reproductive development.
14 CLINICAL STUDIES
Clinical Study 1 evaluated peginterferon alfa-2b monotherapy. See peginterferon alfa-2b labeling for information about this trial.
14.1 Ribavirin/Peginterferon alfa-2b Combination Therapy
Adult Subjects
Study 2
A randomized trial compared treatment with two peginterferon alfa-2b/ribavirin regimens [peginterferon alfa-2b 1.5 mcg/kg subcutaneously once weekly/ribavirin 800 mg orally daily (in divided doses); peginterferon alfa-2b 1.5 mcg/kg subcutaneously once weekly for 4 weeks then 0.5 mcg/kg subcutaneously once weekly for 44 weeks/ribavirin 1000 or 1200 mg orally daily (in divided doses)] with interferon alfa-2b [3 MIU subcutaneously three times weekly/ribavirin 1000 or 1200 mg orally daily (in divided doses)] in 1530 adults with chronic hepatitis C. Interferon-naïve subjects were treated for 48 weeks and followed for 24 weeks post-treatment. Eligible subjects had compensated liver disease, detectable HCV-RNA, elevated ALT, and liver histopathology consistent with chronic hepatitis.
Response to treatment was defined as undetectable HCV-RNA at 24 weeks post-treatment (see Table 13). The response rate to the peginterferon alfa-2b 1.5 mcg/kg and ribavirin 800 mg dose was higher than the response rate to interferon alfa-2b/ribavirin (see Table 13).
The response rate to peginterferon alfa-2b 1.5→0.5 mcg/kg/ribavirin was essentially the same as the response to interferon alfa-2b/ribavirin (data not shown).
|
|
||
|
Peginterferon alfa-2b
|
Interferon alfa-2b
|
|
|
52% (264/511) |
46% (231/505) |
|
|
Genotype 1 |
41% (141/348) |
33% (112/343) |
|
Genotype 2-6 |
75% (123/163) |
73% (119/162) |
Subjects with viral genotype 1, regardless of viral load, had a lower response rate to peginterferon alfa-2b (1.5 mcg/kg)/ribavirin (800 mg) compared to subjects with other viral genotypes. Subjects with both poor prognostic factors (genotype 1 and high viral load) had a response rate of 30% (78/256) compared to a response rate of 29% (71/247) with interferon alfa-2b/ribavirin combination therapy.
Subjects with lower body weight tended to have higher adverse-reaction rates [see Adverse Reactions (6.1)] and higher response rates than subjects with higher body weights. Differences in response rates between treatment arms did not substantially vary with body weight.
Treatment response rates with peginterferon alfa-2b/ribavirin combination therapy were 49% in men and 56% in women. Response rates were lower in African American and Hispanic subjects and higher in Asians compared to Caucasians. Although African Americans had a higher proportion of poor prognostic factors compared to Caucasians, the number of non-Caucasians studied (11% of the total) was insufficient to allow meaningful conclusions about differences in response rates after adjusting for prognostic factors in this trial.
Liver biopsies were obtained before and after treatment in 68% of subjects. Compared to baseline, approximately two-thirds of subjects in all treatment groups were observed to have a modest reduction in inflammation.
Study 3
In a large United States community-based trial, 4913 subjects with chronic hepatitis C were randomized to receive peginterferon alfa-2b 1.5 mcg/kg subcutaneously once weekly in combination with a ribavirin dose of 800 to 1400 mg (weight-based dosing [WBD]) or 800 mg (flat) orally daily (in divided doses) for 24 or 48 weeks based on genotype. Response to treatment was defined as undetectable HCV-RNA (based on an assay with a lower limit of detection of 125 IU/mL) at 24 weeks post-treatment.
Treatment with peginterferon alfa-2b 1.5 mcg/kg and ribavirin 800 to 1400 mg resulted in a higher sustained virologic response compared to peginterferon alfa-2b in combination with a flat 800 mg daily dose of ribavirin. Subjects weighing greater than 105 kg obtained the greatest benefit with WBD, although a modest benefit was also observed in subjects weighing greater than 85 to 105 kg (see Table 14). The benefit of WBD in subjects weighing greater than 85 kg was observed with HCV genotypes 1-3. Insufficient data were available to reach conclusions regarding other genotypes. Use of WBD resulted in an increased incidence of anemia [see Adverse Reactions (6.1)].
|
|
||||
|
Treatment Group |
Subject Baseline Weight |
|||
|
<65 kg
|
65-85 kg
|
>85-105 kg
|
>105 kg
|
|
|
WBD* |
50% (173/348) |
45% (449/994) |
42% (351/835) |
47% (138/292) |
|
Flat |
51% (173/342) |
44% (443/1011) |
39% (318/819) |
33% (91/272) |
A total of 1552 subjects weighing greater than 65 kg in Study 3 had genotype 2 or 3 and were randomized to 24 or 48 weeks of therapy. No additional benefit was observed with the longer treatment duration.
Study 4
A large randomized trial compared the safety and efficacy of treatment for 48 weeks with two peginterferon alfa-2b/ribavirin regimens [peginterferon alfa-2b 1.5 mcg/kg and 1 mcg/kg subcutaneously once weekly both in combination with ribavirin 800 to 1400 mg PO daily (in two divided doses)] and peginterferon alfa-2a 180 mcg subcutaneously once weekly in combination with ribavirin tablets 1000 to 1200 mg PO daily (in two divided doses) in 3070 treatment-naïve adults with chronic hepatitis C genotype 1. In this trial, lack of early virologic response (undetectable HCV-RNA or greater than or equal to 2 log10 reduction from baseline) by treatment Week 12 was the criterion for discontinuation of treatment. SVR was defined as undetectable HCV-RNA (Roche COBAS TaqMan assay, a lower limit of quantitation of 27 IU/mL) at 24 weeks post-treatment (see Table 15).
|
% (number) of Subjects |
||
|
Peginterferon alfa-2b
|
Peginterferon alfa-2b
|
Peginterferon alfa-2a
|
|
40 (406/1019) |
38 (386/1016) |
41 (423/1035) |
Overall SVR rates were similar among the three treatment groups. Regardless of treatment group, SVR rates were lower in subjects with poor prognostic factors. Subjects with poor prognostic factors randomized to peginterferon alfa-2b (1.5 mcg/kg)/ribavirin capsules or peginterferon alfa-2a/ ribavirin tablets, however, achieved higher SVR rates compared to similar subjects randomized to peginterferon alfa-2b 1 mcg/kg/ribavirin capsules. For the peginterferon alfa-2b 1.5 mcg/kg and ribavirin capsules dose, SVR rates for subjects with and without the following prognostic factors were as follows: cirrhosis (10% vs. 42%), normal ALT levels (32% vs. 42%), baseline viral load greater than 600,000 IU/mL (35% vs. 61%), 40 years of age and older (38% vs. 50%), and African American race (23% vs. 44%). In subjects with undetectable HCV-RNA at treatment Week 12 who received peginterferon alfa-2b (1.5 mcg/kg)/ribavirin capsules, the SVR rate was 81% (328/407).
Study 5 - Ribavirin/Peginterferon alfa-2b Combination Therapy in Prior Treatment Failures
In a noncomparative trial, 2293 subjects with moderate to severe fibrosis who failed previous treatment with combination alpha interferon/ribavirin were re-treated with peginterferon alfa-2b, 1.5 mcg/kg subcutaneously, once weekly, in combination with weight adjusted ribavirin. Eligible subjects included prior nonresponders (subjects who were HCV-RNA positive at the end of a minimum 12 weeks of treatment) and prior relapsers (subjects who were HCV-RNA negative at the end of a minimum 12 weeks of treatment and subsequently relapsed after post-treatment follow-up). Subjects who were negative at Week 12 were treated for 48 weeks and followed for 24 weeks post-treatment. Response to treatment was defined as undetectable HCV-RNA at 24 weeks post-treatment (measured using a research-based test, limit of detection 125 IU/mL). The overall response rate was 22% (497/2293) (99% CI: 19.5, 23.9). Subjects with the following characteristics were less likely to benefit from re-treatment: previous nonresponse, previous pegylated interferon treatment, significant bridging fibrosis or cirrhosis, and genotype 1 infection.
The re-treatment sustained virologic response rates by baseline characteristics are summarized in Table 16.
|
HCV Genotype/
|
Overall SVR by Previous Response and Treatment |
|||
|
Nonresponder |
Relapser |
|||
|
interferon alfa/ ribavirin %
|
peginterferon (2a and 2b combined)/
|
interferon alfa/ ribavirin %
|
peginterferon (2a and 2b combined)/ ribavirin % (number of subjects) |
|
|
Overall |
18 (158/903) |
6 (30/476) |
43 (130/300) |
35 (113/344) |
|
HCV 1 |
13 (98/761) |
4 (19/431) |
32 (67/208) |
23 (56/243) |
|
F2 |
18 (36/202) |
6 (7/117) |
42 (33/79) |
32 (23/72) |
|
F3 |
16 (38/233) |
4 (4/112) |
28 (16/58) |
21 (14/67) |
|
F4 |
7 (24/325) |
4 (8/202) |
26 (18/70) |
18 (19/104) |
|
HCV 2/3 |
49 (53/109) |
36 (10/28) |
67 (54/81) |
57 (52/92) |
|
F2 |
68 (23/34) |
56 (5/9) |
76 (19/25) |
61 (11/18) |
|
F3 |
39 (11/28) |
38 (3/8) |
67 (18/27) |
62 (18/29) |
|
F4 |
40 (19/47) |
18 (2/11) |
59 (17/29) |
51 (23/45) |
|
HCV 4 |
17 (5/29) |
7 (1/15) |
88 (7/8) |
50 (4/8) |
Achievement of an undetectable HCV-RNA at treatment Week 12 was a strong predictor of SVR. In this trial, 1470 (64%) subjects did not achieve an undetectable HCV-RNA at treatment Week 12, and were offered enrollment into long-term treatment trials, due to an inadequate treatment response. Of the 823 (36%) subjects who were HCV-RNA undetectable at treatment Week 12, those infected with genotype 1 had an SVR of 48% (245/507), with a range of responses by fibrosis scores (F4-F2) of 39-55%. Subjects infected with genotype 2/3 who were HCV-RNA undetectable at treatment Week 12 had an overall SVR of 70% (196/281), with a range of responses by fibrosis scores (F4-F2) of 60-83%. For all genotypes, higher fibrosis scores were associated with a decreased likelihood of achieving SVR.
Pediatric Subjects
Previously untreated pediatric subjects 3 to 17 years of age with compensated chronic hepatitis C and detectable HCV-RNA were treated with ribavirin 15 mg/kg per day and peginterferon alfa-2b 60 mcg/m2 once weekly for 24 or 48 weeks based on HCV genotype and baseline viral load. All subjects were to be followed for 24 weeks post-treatment. A total of 107 subjects received treatment, of which 52% were female, 89% were Caucasian, and 67% were infected with HCV Genotype 1. Subjects infected with Genotypes 1, 4 or Genotype 3 with HCV-RNA greater than or equal to 600,000 IU/mL received 48 weeks of therapy while those infected with Genotype 2 or Genotype 3 with HCV-RNA less than 600,000 IU/mL received 24 weeks of therapy. The trial results are summarized in Table 17.
|
|
||
|
Genotype |
All Subjects
|
|
|
24 Weeks |
48 Weeks |
|
|
All |
26/27 (96.3) |
44/80 (55.0) |
|
1 |
- |
38/72 (52.8) |
|
2 |
14/15 (93.3) |
- |
|
3‡ |
12/12 (100) |
2/3 (66.7) |
|
4 |
- |
4/5 (80.0) |
14.2 Ribavirin/Interferon alfa-2b Combination Therapy
Adult Subjects
Previously Untreated Subjects
Adults with compensated chronic hepatitis C and detectable HCV-RNA (assessed by a central laboratory using a research-based RT-PCR assay) who were previously untreated with alpha interferon therapy were enrolled into two multicenter, double-blind trials (US and international) and randomized to receive ribavirin capsules 1200 mg/day (1000 mg/day for subjects weighing less than or equal to 75 kg) and interferon alfa-2b 3 MIU three times weekly or interferon alfa-2b and placebo for 24 or 48 weeks followed by 24 weeks of off-therapy follow-up. The international trial did not contain a 24-week interferon alfa-2b and placebo treatment arm. The US trial enrolled 912 subjects who, at baseline, were 67% male, 89% Caucasian with a mean Knodell HAI score (I+II+III) of 7.5, and 72% genotype 1. The international trial, conducted in Europe, Israel, Canada, and Australia, enrolled 799 subjects (65% male, 95% Caucasian, mean Knodell score 6.8, and 58% genotype 1).
Trial results are summarized in Table 18.
|
|
|||||||
|
US Trial |
International Trial |
||||||
|
24 weeks of treatment |
48 weeks of treatment |
24 weeks of treatment |
48 weeks of treatment |
||||
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
Interferon
|
|
|
Virologic Response | |||||||
|
Responder† |
65 (29) |
13 (6) |
85 (37) |
27 (12) |
86 (32) |
113 (42) |
46 (17) |
|
Nonresponder |
147 (64) |
194 (84) |
110 (48) |
168 (75) |
158 (60) |
120 (45) |
196 (74) |
|
Missing Data |
16 (7) |
24 (10) |
33 (14) |
30 (13) |
21 (8) |
35 (13) |
24 (9) |
|
Histologic Response | |||||||
|
Improvement‡ |
102 (45) |
77 (33) |
96 (42) |
65 (29) |
103 (39) |
102 (38) |
69 (26) |
|
No improvement |
77 (34) |
99 (43) |
61 (27) |
93 (41) |
85 (32) |
58 (22) |
111 (41) |
|
Missing Data |
49 (21) |
55 (24) |
71 (31) |
67 (30) |
77 (29) |
108 (40) |
86 (32) |
Of subjects who had not achieved HCV-RNA below the limit of detection of the research-based assay by Week 24 of ribavirin/interferon alfa-2b treatment, less than 5% responded to an additional 24 weeks of combination treatment.
Among subjects with HCV Genotype 1 treated with ribavirin/interferon alfa-2b therapy who achieved HCV-RNA below the detection limit of the research-based assay by 24 weeks, those randomized to 48 weeks of treatment had higher virologic responses compared to those in the 24-week treatment group. There was no observed increase in response rates for subjects with HCV non-genotype 1 randomized to ribavirin/interferon alfa-2b therapy for 48 weeks compared to 24 weeks.
Relapse Subjects
Subjects with compensated chronic hepatitis C and detectable HCV-RNA (assessed by a central laboratory using a research-based RT-PCR assay) who had relapsed following one or two courses of interferon therapy (defined as abnormal serum ALT levels) were enrolled into two multicenter, double-blind trials (US and international) and randomized to receive ribavirin 1200 mg/day (1000 mg/day for subjects weighing ≤ 75 kg) and interferon alfa-2b 3 MIU three times weekly or interferon alfa-2b and placebo for 24 weeks followed by 24 weeks of off-therapy follow-up. The US trial enrolled 153 subjects who, at baseline, were 67% male, 92% Caucasian with a mean Knodell HAI score (I+II+III) of 6.8, and 58% genotype 1. The international trial, conducted in Europe, Israel, Canada, and Australia, enrolled 192 subjects (64% male, 95% Caucasian, mean Knodell score 6.6, and 56% genotype 1). Trial results are summarized in Table 19.
|
|
||||
|
US Trial |
International Trial |
|||
|
Interferon alfa-2b/
|
Interferon alfa-2b/
|
Interferon alfa-2b/
|
Interferon alfa-2b/
|
|
|
Virologic Response | ||||
|
Responder† |
33 (43) |
3 (4) |
46 (48) |
5 (5) |
|
Nonresponder |
36 (47) |
66 (87) |
45 (47) |
91 (95) |
|
Missing Data |
8 (10) |
7 (9) |
5 (5) |
0 (0) |
|
Histologic Response | ||||
|
Improvement‡ |
38 (49) |
27 (36) |
49 (51) |
30 (31) |
|
No improvement |
23 (30) |
37 (49) |
29 (30) |
44 (46) |
|
Missing Data |
16 (21) |
12 (16) |
18 (19) |
22 (23) |
Virologic and histologic responses were similar among male and female subjects in both the previously untreated and relapse trials.
Pediatric Subjects
Pediatric subjects 3 to 16 years of age with compensated chronic hepatitis C and detectable HCV-RNA (assessed by a central laboratory using a research-based RT-PCR assay) were treated with ribavirin 15 mg/kg per day and interferon alfa-2b 3 MIU/m2 three times weekly for 48 weeks followed by 24 weeks of off-therapy follow-up. A total of 118 subjects received treatment, of which 57% were male, 80% Caucasian, and 78% genotype 1. Subjects less than 5 years of age received ribavirin oral solution and those 5 years of age or older received either ribavirin oral solution or capsules.
Trial results are summarized in Table 20.
|
|
|
|
Interferon alfa-2b 3 MIU/m2
|
|
|
Overall Response† (N=118) |
54 (46) |
|
Genotype 1 (N=92) |
33 (36) |
|
Genotype non-1 (N=26) |
21 (81) |
Subjects with viral genotype 1, regardless of viral load, had a lower response rate to interferon alfa-2b/ribavirin combination therapy compared to subjects with genotype non-1, 36% vs. 81%. Subjects with both poor prognostic factors (genotype 1 and high viral load) had a response rate of 26% (13/50).
16 HOW SUPPLIED/STORAGE AND HANDLING
RIBASPHERE (ribavirin capsules USP) is available as capsules for oral administration.
RIBASPHERE 200 mg capsules are white, opaque, gelatin capsules printed horizontally with "riba 200" on both the body and the cap of the capsule in edible green pharmaceutical ink. RIBASPHERE 200 mg capsules are packaged in HDPE bottles with child-resistant closures containing 84 capsules (NDC: 66435-101-84) and 180 capsules (NDC: 66435-101-18).
The bottle of RIBASPHERE capsules should be stored at 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-Approved Patient Labeling (Medication Guide).
Anemia
The most common adverse experience occurring with RIBASPHERE capsules is anemia, which may be severe [see Warnings and Precautions (5.2) and Adverse Reactions (6)]. Patients should be advised that laboratory evaluations are required prior to starting therapy and periodically thereafter [see Dosage and Administration (2.3)]. It is advised that patients be well hydrated, especially during the initial stages of treatment.
Pregnancy
Patients must be informed that RIBASPHERE capsules may cause birth defects and death of the unborn child. RIBASPHERE must not be used by women who are pregnant or by men whose female partners are pregnant. Extreme care must be taken to avoid pregnancy in female patients and in female partners of male patients taking RIBASPHERE. RIBASPHERE should not be initiated until a report of a negative pregnancy test has been obtained immediately prior to initiation of therapy. Patients must perform a pregnancy test monthly during therapy and for 6 months post therapy. Women of childbearing potential must be counseled about use of effective contraception (two reliable forms) prior to initiating therapy. Patients (male and female) must be advised of the teratogenic/embryocidal risks and must be instructed to practice effective contraception during RIBASPHERE and for 6 months post therapy. Patients (male and female) should be advised to notify the physician immediately in the event of a pregnancy [see Contraindications (4), Warnings and Precautions (5.1), and Use in Specific Populations (8.1)].
If pregnancy does occur during treatment or during 6 months post therapy, the patient must be advised of the teratogenic risk of RIBASPHERE therapy to the fetus. Patients, or partners of patients, should immediately report any pregnancy that occurs during treatment or within 6 months after treatment cessation to their physician. Prescribers should report such cases by calling 1-800-593-2214.
Risks versus Benefits
Patients receiving RIBASPHERE capsules should be informed of the benefits and risks associated with treatment, directed in its appropriate use, and referred to the patient MEDICATION GUIDE. Patients should be informed that the effect of treatment of hepatitis C infection on transmission is not known, and that appropriate precautions to prevent transmission of the hepatitis C virus should be taken.
Patients should be informed about what to do in the event they miss a dose of RIBASPHERE; the missed dose should be taken as soon as possible during the same day. Patients should not double the next dose. Patients should be advised to contact their healthcare provider if they have questions.
Manufactured by
PATHEON MANUFACTURING SERVICES, LLC.
Greenville, NC 27834, USA
Manufactured for
KADMON PHARMACEUTICALS, LLC
Warrendale, PA 15086, USA
Copyright © 2015, Kadmon Pharmaceuticals, LLC. All rights reserved.
U.S. Patent No. 6,720,000
C101.00018 v1.1
MEDICATION GUIDE
RIBASPHERE® (Rīb-a-sphere) (ribavirin capsules)
Rx Only
Read this Medication Guide before you start taking RIBASPHERE® (ribavirin capsules), and each time you get a refill. There may be new information. This information does not take the place of talking to your health care provider about your medical condition or your treatment.
What is the most important information I should know about RIBASPHERE (ribavirin capsules)?
- 1. Do Not take RIBASPHERE (ribavirin capsules) alone to treat chronic hepatitis C infection. RIBASPHERE (ribavirin capsules) should be used in combination with either interferon alfa-2b (INTRON® A1) or peginterferon alfa-2b (PegIntron® 2) to treat chronic hepatitis C infection.
- 2. RIBASPHERE (ribavirin capsules) may cause a significant drop in your red blood cell count and cause anemia in some cases. Anemia has been associated with worsening of Heart Problems, and in rare cases can cause a Heart Attack and Death. Tell your health care provider if you have ever had any heart problems. RIBASPHERE (ribavirin capsules) may not be right for you. Seek medical attention right away if you experience chest pain.
- 3.
RIBASPHERE (ribavirin capsules) may cause Birth Defects or the Death of your unborn baby. Do Not Take RIBASPHERE (ribavirin capsules) if you or your sexual partner is pregnant or plan to become pregnant. Do Not become Pregnant within 6 months after discontinuing RIBASPHERE (ribavirin capsules) therapy. You must use 2 forms of birth control when you take RIBASPHERE (ribavirin capsules) and for the 6 months after treatment.
- Females must have a pregnancy test before starting RIBASPHERE (ribavirin capsules), every month while taking RIBASPHERE (ribavirin capsules), and every month for the 6 months after the last dose of RIBASPHERE (ribavirin capsules).
- If you or your female sexual partner becomes pregnant while taking RIBASPHERE (ribavirin capsules) or within 6 months after you stop taking RIBASPHERE (ribavirin capsules), tell your health care provider right away. You or your health care provider should contact the Ribavirin pregnancy registry by calling 1-800-593-2214. The Ribavirin pregnancy registry collects information about what happens to mothers and their babies if the mother takes RIBASPHERE (ribavirin capsules) while she is pregnant.
What is RIBASPHERE (ribavirin capsules)?
RIBASPHERE is a medicine used with either interferon alfa-2b or peginterferon alfa-2b to treat chronic (lasting a long time) hepatitis C infection in people 3 years and older with liver disease.
It is not known if RIBASPHERE (ribavirin capsules) use for longer than 1 year is safe and will work.
It is not known if RIBASPHERE (ribavirin capsules) use in children younger than 3 years old is safe and will work.
Who should not take RIBASPHERE (ribavirin capsules)?
See “What is the most important information I should know about RIBASPHERE (ribavirin capsules)?”
Do not take RIBASPHERE (ribavirin capsules) if you have:
- or ever had serious allergic reactions to the ingredients in RIBASPHERE (ribavirin capsules). See the end of this Medication Guide for a complete list of ingredients.
- certain types of hepatitis (autoimmune hepatitis).
- certain blood disorders (hemoglobinopathies).
- severe kidney disease.
- taken or currently take didanosine (VIDEX® 3).
- Talk to your health care provider before taking RIBASPHERE (ribavirin capsules) if you have any of these conditions.
What should I tell my health care provider before taking RIBASPHERE (ribavirin capsules)?
Before you take RIBASPHERE (ribavirin capsules), tell your health care provider if you have or ever had:
- treatment for hepatitis C that did not work for you.
- breathing problems. RIBASPHERE (ribavirin capsules) may cause or worsen breathing problems you already have.
- vision problems. RIBASPHERE (ribavirin capsules) may cause eye problems or worsen eye problems you already have. You should have an eye exam before you start treatment with RIBASPHERE (ribavirin capsules).
- certain blood disorders such as anemia (low red blood cell count).
- high blood pressure, heart problems, or have had a heart attack. Your health care provider should check your blood and heart before you start treatment with RIBASPHERE (ribavirin capsules).
- thyroid problems.
- liver problems other than hepatitis C infection.
- human immunodeficiency virus (HIV) or any immunity problems.
- mental health problems, including depression or thoughts of suicide.
- kidney problems.
- an organ transplant.
- diabetes. RIBASPHERE (ribavirin capsules) may make your diabetes worse or harder to treat.
- any other medical condition.
- are breastfeeding. It is not known if RIBASPHERE (ribavirin capsules) passes into your breast milk. You and your health care provider should decide if you will take RIBASPHERE (ribavirin capsules) or breastfeed.
Tell your health care provider about all the medicines you take, including prescription medicines, vitamins, and herbal supplements. RIBASPHERE (ribavirin capsules) may affect the way other medicines work.
Especially tell your health care provider if you take didanosine (VIDEX® 3) or azathioprine (Imuran® 4 and Azasan® 5).
Know the medicines you take. Keep a list of them to show your health care provider or pharmacist when you get a new medicine.
How should I take RIBASPHERE (ribavirin capsules)?
- Take RIBASPHERE (ribavirin capsules) exactly as your health care provider tells you. Your health care provider will tell you how much RIBASPHERE (ribavirin capsules) to take and when to take it.
- Take RIBASPHERE (ribavirin capsules) with food.
- Take RIBASPHERE capsules whole. Do not open, break, or crush RIBASPHERE capsules before swallowing. If you cannot swallow RIBASPHERE capsules whole, tell your health care provider.
- If you miss a dose of RIBASPHERE (ribavirin capsules), take the missed dose as soon as possible during the same day. Do not double the next dose. If you have questions about what to do, call your health care provider.
- If you take too much RIBASPHERE (ribavirin capsules), call your health care provider or Poison Control Center at 1-800-222-1222, or go to the nearest hospital emergency room right away.
What are the possible side effects of RIBASPHERE (ribavirin capsules)?
RIBASPHERE (ribavirin capsules) may cause serious side effects, including:
See “What is the most important information I should know about RIBASPHERE (ribavirin capsules)?”
- Swelling and irritation of your pancreas (pancreatitis). You may have stomach pain, nausea, vomiting, or diarrhea.
- Serious breathing problems. Difficulty breathing may be a sign of a serious lung infection (pneumonia) that can lead to death.
- Serious eye problems that may lead to vision loss or blindness.
- Dental problems. Your mouth may be very dry, which can lead to problems with your teeth and gums.
- Severe depression.
- Suicidal thoughts and attempts. Adults and children who take RIBASPHERE (ribavirin capsules), especially teenagers, are more likely to have suicidal thoughts or attempt to hurt themselves while taking RIBASPHERE (ribavirin capsules). Call your health care provider right away or go to the nearest hospital emergency room if you have new or worse depression or thoughts about suicide or dying.
- Severe blood disorders. An increased risk when used in combination with pegylated alpha interferons and azathioprine.
- Growth problems in children. Weight loss and slowed growth are common in children during combination treatment with peginterferon alfa-2b (PegIntron® 2) or interferon alfa-2b (INTRON® A1). Most children will go through a growth spurt and gain weight after treatment stops. Some children may not reach the height that they were expected to have before treatment. Talk to your health care provider if you are concerned about your child’s growth during treatment with RIBASPHERE and peginterferon alfa-2b (PegIntron® 2) or with RIBASPHERE and interferon alfa-2b (INTRON® A1).
Tell your health care provider right away if you have any side effect that bothers you or that does not go away.
The most common side effects of RIBASPHERE (ribavirin capsules) include:
- flu-like symptoms - feeling tired, headache, shaking along with high temperature (fever), nausea, and muscle aches.
- mood changes, feeling irritable.
The most common side effects of RIBASPHERE (ribavirin capsules) in children include:
- a decrease in the blood cells that fight infection (neutropenia).
- a decrease in appetite.
- stomach pain and vomiting.
Tell your health care provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of RIBASPHERE (ribavirin capsules). For more information ask your health care provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store RIBASPHERE (ribavirin capsules)?
Store RIBASPHERE (ribavirin capsules) between 59°-86°F (15°-30°C).
Keep RIBASPHERE (ribavirin capsules) and all medicines out of the reach of children.
GENERAL INFORMATION ABOUT THE SAFE AND EFFECTIVE USE OF RIBASPHERE (RIBAVIRIN CAPSULES).
It is not known if treatment with RIBASPHERE (ribavirin capsules) will cure hepatitis C virus infections or prevent cirrhosis, liver failure, or liver cancer that can be caused by hepatitis C virus infections. It is not known if taking RIBASPHERE (ribavirin capsules) will prevent you from infecting another person with the hepatitis C virus.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use RIBASPHERE (ribavirin capsules) for a condition for which it was not prescribed. Do not give RIBASPHERE (ribavirin capsules) to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about RIBASPHERE (ribavirin capsules). If you would like more information, talk with your health care provider. You can ask your pharmacist or health care provider for information about RIBASPHERE (ribavirin capsules) that is written for health professionals.
What are the ingredients in RIBASPHERE (ribavirin capsules)?
Active ingredients: ribavirin
Inactive ingredients: croscarmellose sodium, lactose monohydrate, microcrystalline cellulose, and povidone. The capsule shell consists of gelatin and titanium dioxide. The capsule is printed with edible green pharmaceutical ink which is made of butyl alcohol, NF, Yellow Iron Oxide, dehydrated alcohol USP, FD&C Blue #2 Aluminum Lake, isopropyl alcohol USP, propylene glycol USP, Shellac, NF, strong ammonia solution, NF, and titanium dioxide.
This Medication Guide has been approved by the U.S. Food and Drug Administration
Manufactured by:
PATHEON MANUFACTURING SERVICES, LLC.
Greenville, NC 27834, USA
Manufactured for
KADMON PHARMACEUTICALS, LLC
Warrendale, PA 15086, USA
Copyright© 2015 Kadmon Pharmaceuticals, LLC.
All rights reserved.
U.S. Patent No. 6,720,000
C101.00014 v2.0
1. INTRON® A is a registered trademark of Schering Corporation
2. PegIntron® is a registered trademark of Schering Corporation
3. VIDEX® is a registered trademark of Bristol-Myers Squibb Company.
4. Imuran® is a registered trademark of Prometheus Laboratories, Inc.
5. Azasan® is a registered trademark of AAI Properties, Inc.
Principal Display Panel - Bottle Label
Bottle Label
NDC: 66435-101-18
Kadmon®
Pharmaceuticals, LLC
Ribasphere®
(Ribavirin capsules)
200 mg
For combination use with INTRON® A (interferon
alfa-2b, recombinant) Injection or PEG-INTRON®
(peginterferon alfa-2b, recombinant) Injection.
Rx Only
ATTENTION PHARMACIST: Each patient is required
to receive a Medication Guide.
180 Capsules
Product of China; Formulated in the U.S.
Manufactured by: Patheon Manufacturing Services, LLC., Greenville, NC 27834, USA
Manufactured for: Kadmon Pharmaceuticals, LLC., Warrendale, PA 15086, USA
C101.00017
LOT:
EXP:
Each capsule contains: Ribavirin, USP 200 mg.
Usual Dosage: See product information.
Read accompanying directions carefully.
AVOID PREGNANCY WHILE TAKING THIS
MEDICATION. READ THE MEDICATION
GUIDE FOR IMPORTANT INFORMATION
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F)
[see USP Controlled Room Temperature]. Dispense in tight, light resistant container with
child resistant closure. Keep out of reach of children.
INTRON® A (interferon alfa-2b, recombinant) Injection is the registered trademark of Schering Corporation.
PEG-INTERON® (peginterferon alfa-2b, recombinant) Injection is the registered trademark of Schering
Corporation.
| RIBASPHERE
ribavirin capsule |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
| Labeler - Kadmon Pharmaceuticals, LLC (843913216) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Patheon Manufacturing Services LLC | 079415560 | MANUFACTURE(66435-101) | |