PITAVASTATIN tablet, film coated
Pitavastatin by
Drug Labeling and Warnings
Pitavastatin by is a Prescription medication manufactured, distributed, or labeled by Amneal Pharmaceuticals LLC, Amneal Pharmaceuticals Private Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PITAVASTATIN TABLETS safely and effectively. See full prescribing information for PITAVASTATIN TABLETS.
PITAVASTATIN tablets, for oral use
Initial U.S. Approval: 2009INDICATIONS AND USAGE
Pitavastatin tablets are a HMG-CoA reductase inhibitor (statin) indicated as an adjunct to diet to reduce low-density lipoprotein cholesterol (LDL-C) in: (1)
- Adults with primary hyperlipidemia.
- Adults and pediatric patients aged 8 years and older with heterozygous familial hypercholesterolemia (HeFH).
DOSAGE AND ADMINISTRATION
- Take orally once daily with or without food at the same time each day. (2.1)
- For patients requiring a high-intensity statin or are unable to achieve their LDL-C goal receiving pitavastatin tablets 4 mg daily, prescribe alternative LDL-C-lowering treatment. (2.1)
- Assess LDL-C when clinically appropriate, as early as 4 weeks after initiation of pitavastatin tablets, and adjust the dosage if necessary. (2.1)
- Recommended dosage is 2 mg to 4 mg once daily. Maximum recommended dosage is 4 mg once daily. (2.2)
- Recommended starting dosage for patients with moderate and severe renal impairment and end-stage renal disease on hemodialysis is 1 mg once daily. Maximum recommended dosage is 2 mg once daily. (2.3)
- See full prescribing information for pitavastatin tablets dosage modifications due to drug interactions. (2.4)
DOSAGE FORMS AND STRENGTHS
Tablets: 1 mg, 2 mg, and 4 mg. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Myopathy and Rhabdomyolysis: Risk factors include age 65 or greater, uncontrolled hypothyroidism, renal impairment, concomitant use with certain other drugs, and higher pitavastatin dosage. Discontinue pitavastatin if markedly elevated CK levels occur or myopathy is diagnosed or suspected. Temporarily discontinue pitavastatin in patients experiencing an acute or serious condition at high risk of developing renal failure secondary to rhabdomyolysis. Inform patients of the risk of myopathy and rhabdomyolysis when starting or increasing the pitavastatin dosage. Instruct patients to promptly report unexplained muscle pain, tenderness or weakness particularly if accompanied by malaise or fever. (5.1, 7, 8.5, 8.6)
- Immune-Mediated Necrotizing Myopathy (IMNM): Rare reports of IMNM, an autoimmune myopathy, have been reported. Discontinue pitavastatin if IMNM is suspected. (5.2)
- Hepatic Dysfunction: Increases in serum transaminases have occurred, some persistent. Rare reports of fatal and non-fatal hepatic failure have occurred. Consider testing liver enzymes before initiating therapy and as clinically indicated thereafter. If serious hepatic injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs, promptly discontinue pitavastatin. (5.3)
ADVERSE REACTIONS
The most frequent adverse reactions (rate ≥ 2%) were myalgia, constipation, diarrhea, back pain, and pain in extremity. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Amneal Pharmaceuticals. at 1-877-835-5472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 7/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
2.2 Recommended Dosage for Adults and Pediatric Patients Aged 8 Years and Older
2.3 Recommended Dosage in Patients with Renal Impairment
2.4 Dosage Modifications Due to Drug Interactions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
5.2 Immune-Mediated Necrotizing Myopathy
5.3 Hepatic Dysfunction
5.4 Increases in HbA1c and Fasting Serum Glucose Levels
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Post-marketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
- Take pitavastatin tablets orally once daily with or without food at the same time each day.
- For patients that require a high-intensity statin or are unable to achieve their LDL-C goal receiving pitavastatin tablets 4 mg daily, prescribe alternative LDL-C-lowering treatment.
- Assess LDL-C when clinically appropriate, as early as 4 weeks after initiating pitavastatin tablets, and adjust the dosage if necessary.
2.2 Recommended Dosage for Adults and Pediatric Patients Aged 8 Years and Older
- The recommended dosage range of pitavastatin tablets is 2 mg to 4 mg daily.
- The maximum recommended dosage is pitavastatin tablets 4 mg once daily.
2.3 Recommended Dosage in Patients with Renal Impairment
- The recommended starting dosage for patients with moderate and severe renal impairment (estimated glomerular filtration rate 30 to 59 mL/minute/1.73 m2 and 15 to 29 mL/minute/1.73 m2, respectively) and patients with end-stage renal disease receiving hemodialysis is pitavastatin tablets 1 mg once daily. The maximum recommended dose for these patients is pitavastatin tablets 2 mg once daily [see Use in Specific Populations (8.5)].
- There are no dosage adjustment recommendations for patients with mild renal impairment.
2.4 Dosage Modifications Due to Drug Interactions
- In patients taking erythromycin, do not exceed pitavastatin tablets 1 mg once daily [see Drug Interactions (7)].
- In patients taking rifampin, do not exceed pitavastatin tablets 2 mg once daily [see Drug Interactions (7)].
-
3 DOSAGE FORMS AND STRENGTHS
Tablets:
- 1 mg: White to off-white colored, round shaped, beveled edges, film-coated tablet, debossed with “AN” on one side and “029” on the other side.
- 2 mg: White to off-white colored, round shaped, beveled edges, film-coated tablet, debossed with “AN” on one side and “030” on the other side.
- 4 mg: White to off-white colored, round shaped, film-coated tablet, debossed with “AN” on one side and “031” on the other side.
-
4 CONTRAINDICATIONS
Pitavastatin tablets are contraindicated in the following conditions:
- Concomitant use of cyclosporine [see Drug Interactions (7)].
- Acute liver failure or decompensated cirrhosis [see Warnings and Precautions (5.3)].
- Hypersensitivity to pitavastatin or any excipents in pitavastatin tablets. Hypersensitivity reactions including angioedema, rash, pruritus, and urticaria have been reported with pitavastatin tablets [see Adverse Reactions (6)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Myopathy and Rhabdomyolysis
Pitavastatin may cause myopathy (muscle pain, tenderness, or weakness associated with elevated creatine kinase [CK]) and rhabdomyolysis. Acute kidney injury secondary to myoglobinuria and rare fatalities have occurred as a result of rhabdomyolysis in patients treated with statins, including pitavastatin.
Risk Factors for Myopathy
Risk factors for myopathy include age 65 years or greater, uncontrolled hypothyroidism, renal impairment, concomitant use of certain drugs (including other lipid-lowering therapies), and higher pitavastatin dosage [see Dosage and Administration (2.2), Drug Interactions (7), and Use in Specific Populations (8.5, 8.6)]. Dosages of pitavastatin greater than 4 mg once daily were associated with an increased risk for severe myopathy in premarketing clinical studies. The maximum recommended dose of pitavastatin is 4 mg once daily.
Steps to Prevent or Reduce the Risk of Myopathy and Rhabdomyolysis
Pitavastatin is contraindicated in patients taking cyclosporine and not recommended in patients taking gemfibrozil [see Contraindications (4) and Drug Interactions (7)]. There are pitavastatin dosage restrictions for patients taking erythromycin or rifampin [see Dosage and Administration (2.4)]. The following drugs when used concomitantly with pitavastatin may also increase the risk of myopathy and rhabdomyolysis: lipid-modifying dosages of niacin (> 1 grams/day), fibrates, and colchicine [see Drug Interactions (7)].
Discontinue pitavastatin if markedly elevated CK levels occur or if myopathy is either diagnosed or suspected. Muscle symptoms and CK elevations may resolve if pitavastatin is discontinued. Temporarily discontinue pitavastatin in patients experiencing an acute or serious condition at high risk of developing renal failure secondary to rhabdomyolysis (e.g., sepsis; shock; severe hypovolemia; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; or uncontrolled epilepsy).
Inform patients of the risk of myopathy and rhabdomyolysis when starting or increasing the pitavastatin dosage. Instruct patients to promptly report any unexplained muscle pain, tenderness or weakness, particularly if accompanied by malaise or fever.
5.2 Immune-Mediated Necrotizing Myopathy
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use, including reports of recurrence when the same or a different statin was administered. IMNM is characterized by proximal muscle weakness and elevated serum creatine kinase that persist despite discontinuation of statin treatment; positive anti-HMG CoA reductase antibody; muscle biopsy showing necrotizing myopathy; and improvement with immunosuppressive agents. Additional neuromuscular and serologic testing may be necessary. Treatment with immunosuppressive agents may be required. Discontinue pitavastatin if IMNM is suspected.
5.3 Hepatic Dysfunction
Increases in serum transaminases have been reported with pitavastatin [see Adverse Reactions (6)]. In most cases, these changes appeared soon after initiation, were transient, were not accompanied by symptoms, and resolved or improved on continued therapy or after a brief interruption in therapy. There have been rare post-marketing reports of fatal and non-fatal hepatic failure in patients taking statins, including pitavastatin.
Patients who consume substantial quantities of alcohol and/or have a history of liver disease may be at increased risk for hepatic injury.
Consider liver enzyme testing before the initiation of pitavastatin and when clinically indicated thereafter. Pitavastatin is contraindicated in patients with acute liver failure or decompensated cirrhosis [see Contraindications (4)]. If serious hepatic injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs, promptly discontinue pitavastatin.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in other sections of the labeling:
- Myopathy and Rhabdomyolysis [see Warnings and Precautions (5.1)]
- Immune-Mediated Necrotizing Myopathy [see Warning and Precautions (5.2)]
- Hepatic Dysfunction [see Warning and Precautions (5.3)]
- Increases in HbA1c and Fasting Serum Glucose Levels [see Warning and Precautions (5.4)].
6.1 Clinical Studies Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of one drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Adverse Reactions in Adults with Primary Hyperlipidemia
In 10 controlled clinical studies and 4 subsequent open-label extension studies, 3,291 adult patients with primary hyperlipidemia were administered pitavastatin 1 mg to 4 mg daily. The mean continuous exposure of pitavastatin (1 mg to 4 mg) was 36.7 weeks (median 51.1 weeks). The mean age of the patients was 60.9 years (range; 18 years to 89 years) and 52% were females. Approximately 93% of the patients were White, 7% were Asian/Indian, 0.2% were African American and 0.3% were Hispanic and other.
In controlled clinical studies and their open-label extensions, 3.9% (1 mg), 3.3% (2 mg), and 3.7% (4 mg) of pitavastatin-treated patients were discontinued due to adverse reactions. The most common adverse reactions that led to treatment discontinuation were: elevated creatine phosphokinase (0.6% on 4 mg) and myalgia (0.5% on 4 mg).
Adverse reactions reported in ≥ 2% of patients in controlled clinical studies and at a rate greater than or equal to placebo are shown in Table 1. These studies had treatment duration of up to 12 weeks.
Table 1: Adverse Reactions (≥ 2% and ≥ placebo) in Adults with Primary Hyperlipidemia in Studies up to 12 Weeks
Adverse Reactions
Placebo
(n=208)
%
Pitavastatin 1 mg
(n=309)
%
Pitavastatin 2 mg
(n=951)
%
Pitavastatin 4 mg
(n=1540)
%
Myalgia
1.4
1.9
2.8
3.1
Constipation
1.9
3.6
1.5
2.2
Diarrhea
1.9
2.6
1.5
1.9
Back pain
2.9
3.9
1.8
1.4
Pain in extremity
1.9
2.3
0.6
0.9
Other adverse reactions reported from clinical studies were arthralgia, headache, influenza, and nasopharyngitis.
Hypersensitivity reactions including rash, pruritus, and urticaria have been reported with pitavastatin.
The following laboratory abnormalities have been reported: elevated creatine phosphokinase, transaminases, alkaline phosphatase, bilirubin, and glucose.
Adverse Reactions in Adult HIV-Infected Patients with Dyslipidemia
In a double-blind, randomized, controlled, 52-week trial, 252 HIV-infected patients with dyslipidemia were treated with either pitavastatin 4 mg once daily (n=126) or another statin (n=126). All patients were taking antiretroviral therapy (excluding darunavir) and had HIV-1 RNA less than 200 copies/mL and CD4 count greater than 200 cell/μL for at least 3 months prior to randomization. The safety profile of pitavastatin was generally consistent with that observed in the clinical trials described above. One patient (0.8%) treated with pitavastatin had a peak creatine phosphokinase value exceeding 10 times the upper limit of normal (ULN), which resolved spontaneously. Four patients (3%) treated with pitavastatin had at least one ALT value exceeding 3 times but less than 5 times the ULN, none of which led to drug discontinuation. Virologic failure was reported for four patients (3%) treated with pitavastatin, defined as a confirmed measurement of HIV-1 RNA exceeding 200 copies/mL that was also more than a 2-fold increase from baseline.
Adverse Reactions in Pediatric Patients Aged 8 Years and Older with HeFH
In a 12-week, double-blind, placebo-controlled trial of pitavastatin 1 mg, 2 mg, and 4 mg once daily in 82 pediatric patients 8 years to 16 years of age with HeFH and a 52-week open-label trial in 85 pediatric patients with HeFH, the safety profile was similar to that observed in the adult population.
6.2 Post-marketing Experience
The following adverse reactions have been identified during post-approval use of pitavastatin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Gastrointestinal disorders: abdominal discomfort, abdominal pain, dyspepsia, nausea
General disorders: asthenia, fatigue, malaise, dizziness Hepatobiliary disorders: hepatitis, jaundice, fatal and non-fatal hepatic failure Immune system disorders: angioedema, immune-mediated necrotizing myopathy associated with statin use
Metabolism and nutrition disorders: increases in HbA1c, fasting serum glucose levels
Musculoskeletal and connective tissue disorders: muscle spasms, myopathy, rhabdomyolysis
Nervous system disorders: hypoesthesia, peripheral neuropathy. There have been rare reports of new onset or exacerbation of myasthenia gravis, including ocular myasthenia, and reports of recurrence when the same or a different statin was administered. Rare reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with statin use. Cognitive impairment was generally nonserious, and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks).
Psychiatric disorders: insomnia, depression
Reproductive system and breast disorders: erectile dysfunction
Respiratory, thoracic and mediastinal disorders: interstitial lung disease
Skin and subcutaneous tissue disorders: lichen planus
-
7 DRUG INTERACTIONS
Table 2 includes a list of drugs that increase the risk of myopathy and rhabdomyolysis when administered concomitantly with pitavastatin and instructions for preventing or managing drug interactions [see Warnings and Precautions (5.1), Clinical Pharmacology (12.3)].
Table 2: Drug Interactions that Increase the Risk of Myopathy and Rhabdomyolysis with Pitavastatin
Cyclosporine
Clinical Impact:
Cyclosporine significantly increases pitavastatin exposure and increases the risk of myopathy and rhabdomyolysis.
Intervention:
Concomitant use of cyclosporine with pitavastatin is contraindicated [see Contraindications (4)].
Gemfibrozil
Clinical Impact:
Gemfibrozil may cause myopathy when given alone. The risk of myopathy and rhabdomyolysis is increased with concomitant use of gemfibrozil with statins, including pitavastatin.
Intervention:
Avoid concomitant use of gemfibrozil with pitavastatin.
Erythromycin
Clinical Impact:
Erythromycin significantly increases pitavastatin exposure and increases the risk of myopathy and rhabdomyolysis.
Intervention:
In patients taking erythromycin, do not exceed pitavastatin 1 mg once daily [see Dosage and Administration (2.4)].
Rifampin
Clinical Impact:
Rifampin significantly increases peak pitavastatin exposure and increases the risk of myopathy and rhabdomyolysis.
Intervention:
In patients taking rifampin, do not exceed pitavastatin 2 mg once daily [see Dosage and Administration (2.4)].
Fibrates
Clinical Impact:
Fibrates may cause myopathy when given alone. The risk of myopathy and rhabdomyolysis is increased with concomitant use of fibrates with statins, including pitavastatin.
Intervention:
Consider if the benefit of using fibrates concomitantly with pitavastatin outweighs the increased risk of myopathy and rhabdomyolysis.
Niacin
Clinical Impact:
The risk of myopathy and rhabdomyolysis may be increased with concomitant use of lipid-modifying doses (≥ 1 g/day) of niacin with pitavastatin.
Intervention:
Consider if the benefit of using lipid-modifying doses (≥ 1 g/day) of niacin concomitantly with pitavastatin outweighs the increased risk of myopathy and rhabdomyolysis.
Colchicine
Clinical Impact:
Cases of myopathy and rhabdomyolysis have been reported with concomitant use of colchicine with statins, including pitavastatin.
Intervention:
Consider the risk/benefit of concomitant use of colchicine with pitavastatin.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Discontinue pitavastatin when pregnancy is recognized. Alternatively, consider the ongoing therapeutic needs of the individual patient.
Pitavastatin decreases synthesis of cholesterol and possibly other biologically active substances derived from cholesterol; therefore, pitavastatin may cause fetal harm when administered to pregnant patients based on the mechanism of action [see Clinical Pharmacology (12.1)]. In addition, treatment of hyperlipidemia is not generally necessary during pregnancy. Atherosclerosis is a chronic process and the discontinuation of lipid-lowering drugs during pregnancy should have little impact on the outcome of long-term therapy of primary hyperlipidemia for most patients.
Available data from case series and prospective and retrospective observational cohort studies over decades of use with statins in pregnant women have not identified a drug-associated risk of major congenital malformations. Published data from prospective and retrospective observational cohort studies with statin use in pregnant women are insufficient to determine if there is a drug associated risk of miscarriage (see Data).
In animal reproduction studies, no embryo-fetal toxicity or congenital malformations were observed in pregnant rats and rabbits orally administered pitavastatin during the period of organogenesis at doses which were 22 and 4 times, respectively, the human exposure at the maximum recommended human dosage (MRHD) of 4 mg, based on AUC [see Data].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data
A Medicaid cohort linkage study of 1,152 statin-exposed pregnant women compared to 8,86,996 controls did not find a significant teratogenic effect from maternal use of statins in the first trimester of pregnancy, after adjusting for potential confounders – including maternal age, diabetes mellitus, hypertension, obesity, and alcohol and tobacco use – using propensity score-based methods. The relative risk of congenital malformations between the group with statin use and the group with no statin use in the first trimester was 1.07 (95% confidence interval 0.85 to 1.37) after controlling for confounders, particularly pre-existing diabetes mellitus. There were also no statistically significant increases in any of the organ-specific malformations assessed after accounting for confounders. In the majority of pregnancies, statin treatment was initiated prior to pregnancy and was discontinued at some point in the first trimester when pregnancy was identified. Study limitations include reliance on physician coding to define the presence of a malformation, lack of control for certain confounders such as body mass index, use of prescription dispensing as verification for the use of a statin, and lack of information on non-live births.
Animal Data
Embryo-fetal developmental studies were conducted in pregnant rats administered 3, 10, 30 mg/kg/day pitavastatin by oral gavage during organogenesis (gestation days 7 to 17). No adverse effects were observed at 3 mg/kg/day, systemic exposures 22 times human systemic exposure at 4 mg/day based on AUC.
Embryo-fetal developmental studies were conducted in pregnant rabbits administered 0.1, 0.3, 1 mg/kg/day pitavastatin by oral gavage during the period of fetal organogenesis (gestation days 6 to 18). Maternal toxicity consisting of reduced body weight and abortion was observed at all doses tested (4 times human systemic exposure at 4 mg/day based on AUC).
In perinatal/postnatal studies in pregnant rats given oral gavage doses of pitavastatin at 0.1, 0.3, 1, 3, 10, 30 mg/kg/day from organogenesis through weaning (gestation day 17 to lactation day 21), maternal toxicity consisting of mortality at ≥ 0.3 mg/kg/day and impaired lactation at all doses contributed to the decreased survival of neonates in all dose groups (0.1 mg/kg/day represents approximately 1 time human systemic exposure at 4 mg/day dose based on AUC).
Reproductive toxicity studies have shown that pitavastatin crosses the placenta in rats and is found in fetal tissues at ≤ 36% of maternal plasma concentrations following a single dose of 1 mg/kg/day during gestation (at the end of organogenesis).
8.2 Lactation
Risk Summary
There is no available information about the presence of pitavastatin in human or animal milk, the effects of the drug on the breastfed infant, or the effects of the drug on milk production. However, it has been shown that another drug in this class passes into human milk. Statins, including pitavastatin, decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol and may cause harm to the breastfed infant.
Because of the potential for serious adverse reactions in a breastfed infant, based upon the mechanism of action, advise patients that breastfeeding is not recommended during treatment with pitavastatin. [see Use in Specific Populations (8.1), Clinical Pharmacology (12.1)]
8.4 Pediatric Use
The safety and effectiveness of pitavastatin as an adjunctive therapy to diet to reduce elevated LDL-C in pediatric patients aged 8 years and older with HeFH have been established. Use of pitavastatin for this indication is supported by a 12-week, double-blind, placebo-controlled trial in 82 pediatric patients 8 to 16 years of age with HeFH [see Clinical Studies (14)] and a 52-week open-label trial in 85 pediatric patients with HeFH.
The safety and effectiveness of pitavastatin have not been established in pediatric patients younger than 8 years of age with HeFH or in pediatric patients with other types of hyperlipidemia (other than HeFH).
8.5 Geriatric Use
In controlled clinical studies, 1,209 (43%) patients were 65 years and older. No overall differences in safety or effectiveness were observed between these patients and younger patients.
Advanced age (≥ 65 years) is a risk factor for pitavastatin-associated myopathy and rhabdomyolysis. Dose selection for a geriatric patient should be cautious, recognizing the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy and the higher risk of myopathy. Monitor geriatric patients receiving pitavastatin for the increased risk of myopathy [see Warnings and Precautions (5.1)].
8.6 Renal Impairment
Renal impairment is a risk factor for myopathy and rhabdomyolysis. Monitor all patients with renal impairment for development of myopathy. Due to the risk of myopathy, a dosage modification of pitavastatin is recommended for patients with moderate and severe renal impairment (estimated glomerular filtration rate 30 to 59 mL/min/1.73 m2 and 15 to 29 mL/min/1.73 m2, respectively), as well as end-stage renal disease receiving hemodialysis. [see Dosage and Administration (2.3), Warnings and Precautions (5.1), Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Pitavastatin is contraindicated in patients with active liver failure or decompensated cirrhosis [see Contraindications (4), Warnings and Precautions (5.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Pitavastatin tablets for oral use is an HMG-CoA reductase inhibitor.
The chemical name for pitavastatin is (+)monocalcium bis{(3R,5S,6E)-7-[2-cyclopropyl-4-(4-fluorophenyl)quinolin-3-yl]-3,5-dihydroxyhept-6-enoate} pentahydrate. The structural formula is:
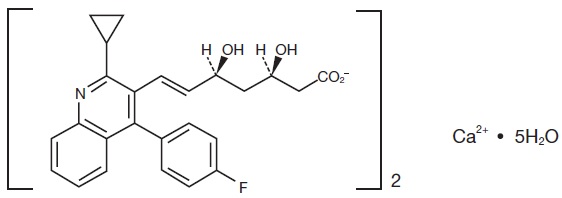
The molecular formula for pitavastatin is C50H46CaF2N2O8 ∙5H2O and the molecular weight is 971.06 g/mol. Pitavastatin is odorless and occurs as white to off-white powder. It is freely soluble in tetrahydrofuran, soluble in ethylene glycol, sparingly soluble in dimethyl sulphoxide and in 50 % aqueous acetonitrile, slightly soluble in methanol, very slightly soluble in water and in ethanol (96%), and insoluble in diethyl ether. Pitavastatin is hygroscopic and slightly unstable in light.
Each film-coated tablet of pitavastatin contains 1 mg, 2 mg, or 4 mg of pitavastatin, which is equivalent to 1.045 mg, 2.09 mg, or 4.18 mg, respectively, of pitavastatin calcium and the following inactive ingredients: hypromellose, lactose monohydrate, low-substituted hydroxypropyl cellulose, magnesium aluminometasilicate, and magnesium stearate. The film-coating contains the following inactive ingredients: colloidal silicon dioxide, hypromellose, titanium dioxide, and triethyl citrate.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Pitavastatin is an inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, the enzyme that catalyzes the conversion of HMG-CoA to mevalonate, a rate-limiting step in the biosynthetic pathway for cholesterol. As a result, the expression of LDL-receptors followed by the uptake of LDL from blood to liver is accelerated and then the plasma TC decreases. Sustained inhibition of cholesterol synthesis in the liver also decreases levels of very low density lipoproteins.
12.2 Pharmacodynamics
Cardiac Electrophysiology
In a randomized, double-blind, placebo-controlled, 4-way parallel, active-comparator study with moxifloxacin in 174 healthy participants, pitavastatin was not associated with clinically meaningful prolongation of the QTc interval or heart rate at daily doses up to 16 mg (4 times the recommended maximum dose of 4 mg daily).
12.3 Pharmacokinetics
Absorption
Pitavastatin peak plasma concentrations are achieved about 1 hour after oral administration. Both Cmax and AUC0-inf increased in an approximately dose-proportional manner for single pitavastatin doses from 1 mg to 24 mg once daily. The absolute bioavailability of pitavastatin oral solution is 51%. The Cmax and AUC of pitavastatin did not differ following evening or morning drug administration. In healthy volunteers receiving 4 mg pitavastatin, the percent change from baseline for LDL-C following evening dosing was slightly greater than that following morning dosing. Pitavastatin was absorbed in the small intestine but very little in the colon.
Effect of Food
Administration of pitavastatin with a high fat meal (50% fat content) decreases pitavastatin Cmax by 43% but does not significantly reduce pitavastatin AUC.
Distribution
Pitavastatin is more than 99% protein bound in human plasma, mainly to albumin and alpha 1-acid glycoprotein, and the mean volume of distribution is approximately 148 L.
Elimination
Metabolism
The principal route of pitavastatin metabolism is glucuronidation via liver uridine 5'-diphosphate glucuronosyltransferase (UGT) with subsequent formation of pitavastatin lactone. There is only minimal metabolism by the cytochrome P450 system. Pitavastatin is marginally metabolized by CYP2C9 and to a lesser extent by CYP2C8. The major metabolite in human plasma is the lactone, which is formed via an ester-type pitavastatin glucuronide conjugate by UGTs (UGT1A3 and UGT2B7).
Excretion
A mean of 15% of radioactivity of orally administered, single 32 mg 14C-labeled pitavastatin dose was excreted in urine, whereas a mean of 79% of the dose was excreted in feces within 7 days. The mean plasma elimination half-life is approximately 12 hours.
Specific Populations
Geriatric Patients
In a pharmacokinetic study which compared healthy young and geriatric (≥ 65 years) volunteers, pitavastatin Cmax and AUC were 10% and 30% higher, respectively, in the geriatric patients [see Use in Specific Populations (8.4)]
Pediatric Patients
A 12-week study in pediatric patients 8 to 16 years of age treated with pitavastatin 1 mg, 2 mg and 4 mg administered once daily, showed a dose-dependent increase in pitavastatin plasma concentrations at trough (for 2 mg and 4 mg doses) and 1 hour post dose. A dose-dependent increase in pitavastatin lactone plasma concentrations was observed at trough and 1 hour post dose.
Male and Female Patients
In a pharmacokinetic study, which compared healthy male and female volunteers, pitavastatin Cmax and AUC were 60% and 54% higher, respectively in females.
Racial or Ethnic Groups
In pharmacokinetic studies pitavastatin Cmax and AUC were 21% and 5% lower, respectively in Black or African American healthy volunteers compared with those of White healthy volunteers. In pharmacokinetic comparison between White volunteers and Japanese volunteers, there were no significant differences in Cmax and AUC.
Patients with Renal Impairment
In patients with moderate renal impairment (estimated glomerular filtration rate of 30 to 59 mL/min/1.73 m2) and end stage renal disease receiving hemodialysis, pitavastatin AUC0-inf is 102% and 86% higher than those of healthy volunteers, respectively, while pitavastatin Cmax is 60% and 40% higher than those of healthy volunteers, respectively. Patients received hemodialysis immediately before pitavastatin dosing and did not undergo hemodialysis during the pharmacokinetic study. Hemodialysis patients have 33% and 36% increases in the mean unbound fraction of pitavastatin as compared to healthy volunteers and patients with moderate renal impairment, respectively [see Use in Specific Populations (8.5)].
In another pharmacokinetic study, patients with severe renal impairment (estimated glomerular filtration rate 15 to 29 mL/min/1.73 m2) not receiving hemodialysis were administered a single dose of pitavastatin 4 mg. The AUC0-inf and the Cmax were 36% and 18% higher, respectively, compared with those of healthy volunteers. For both patients with severe renal impairment and healthy volunteers, the mean percentage of protein-unbound pitavastatin was approximately 0.6% [see Use in Specific Populations (8.5)].
The effect of mild renal impairment on pitavastatin exposure has not been studied.
Patients with Hepatic Impairment
The disposition of pitavastatin was compared in healthy volunteers and patients with various degrees of hepatic impairment. Pitavastatin Cmax and AUCinf in patients with moderate hepatic impairment (Child-Pugh B disease) was 2.7-fold and 3.8-fold higher, respectively as compared to healthy volunteers. In patients with mild hepatic impairment (Child-Pugh A disease), pitavastatin Cmax and AUCinf were 30% and 60% higher as compared to healthy volunteers. Mean pitavastatin half-life for moderate hepatic impairment, mild hepatic impairment, and healthy volunteers were 15, 10, and 8 hours, respectively [see Contraindications (4), Warnings and Precautions (5.3)].
Drug Interaction Studies
Warfarin
The steady-state pharmacodynamics (international normalized ratio [INR] and prothrombin time [PT]) and pharmacokinetics of warfarin in healthy volunteers were unaffected by the co-administration of pitavastatin 4 mg daily.
Table 3 presents the effect of co-administered drugs on pitavastatin systemic exposure:
Table 3: Effect of Co-administered Drugs on Pitavastatin Systemic Exposure
Co-administered drug Dosage regimen Change in
AUC*Change in
Cmax*Cyclosporine
Pitavastatin 2 mg QD for 6 days + cyclosporine 2 mg/kg on Day 6
↑ 4.6 fold†
↑ 6.6 fold†
Erythromycin
Pitavastatin 4 mg single dose on Day 4 + erythromycin 500 mg 4 times daily for
6 days
↑ 2.8 fold†
↑ 3.6 fold†
Rifampin
Pitavastatin 4 mg QD + rifampin 600 mg QD for 5 days
↑ 29%
↑ 2.0 fold†
Atazanavir
Pitavastatin 4 mg QD + atazanavir 300 mg daily for 5 days
↑ 31%
↑ 60%
Darunavir/Ritonavir
Pitavastatin 4 mg QD on Days 1 to 5 and 12 to 16 + darunavir/ritonavir 800 mg/100 mg QD on Days 6 to 16
↓ 26%
↓ 4%
Lopinavir/Ritonavir
Pitavastatin 4 mg QD on Days 1 to 5 and 20 to 24 + lopinavir/ritonavir 400 mg/100 mg BID on Days 9 to 24
↓ 20%
↓4 %
Gemfibrozil
Pitavastatin 4 mg QD + gemfibrozil 600 mg BID for 7 days
↑ 45%
↑ 31%
Fenofibrate
Pitavastatin 4 mg QD + fenofibrate 160 mg QD for 7 days
↑18%
↑ 11%
Ezetimibe
Pitavastatin 2 mg QD + ezetimibe 10 mg for 7 days
↓ 2%
↓0.2%
Enalapril
Pitavastatin 4 mg QD + enalapril 20 mg daily for 5 days
↑ 6%
↓ 7%
Digoxin
Pitavastatin 4 mg QD + digoxin 0.25 mg for 7 days
↑ 4%
↓ 9%
Diltiazem LA
Pitavastatin 4 mg QD on Days 1 to 5 and 11 to 15 and diltiazem LA 240 mg on Days 6 to 15
↑10%
↑15%
Grapefruit Juice
Pitavastatin 2 mg single dose on Day 3 + grapefruit juice for 4 days
↑ 15%
↓ 12%
Itraconazole
Pitavastatin 4 mg single dose on Day 4 + itraconazole 200 mg daily for 5 days
↓ 23%
↓ 22%
*Data presented as x-fold change represent the ratio between co-administration and pitavastatin alone (i.e., 1-fold = no change). Data presented as % change represent % difference relative to pitavastatin alone (i.e., 0% = no change).
†Considered clinically significant [see Dosage and Administration (2.4), Drug Interactions (7)]
BID = twice daily; QD = once daily; LA = Long Acting
Table 4 presents the effect of pitavastatin co-administration on systemic exposure of other drugs:
Table 4: Effect of Pitavastatin Co-administration on Systemic Exposure to Other Drugs
Co-administered drug Dosage regimen Change in
AUC*Change in
Cmax*Atazanavir
Pitavastatin 4 mg QD + atazanavir 300 mg daily for 5 days
↑ 6%
↑ 13%
Darunavir
Pitavastatin 4 mg QD on Days 1 to 5 and 12 to 16 + darunavir/ritonavir 800mg/100 mg QD on Days 6 to 16
↑ 3%
↑ 6%
Lopinavir
Pitavastatin 4 mg QD on Days 1 to 5 and 20 to 24 + lopinavir/ritonavir 400 mg/100 mg BID on Days 9 to 24
↓ 9%
↓ 7%
Ritonavir
Pitavastatin 4 mg QD on Days 1 to 5 and 20 to 24 + lopinavir/ritonavir 400 mg/100 mg BID on Days 9 to 24
↓ 11%
↓ 11%
Ritonavir
Pitavastatin 4mg QD on Days 1 to 5 and 12 to 16 + darunavir/ritonavir 800 mg/100 mg QD on Days 6 to 16
↑ 8%
↑ 2%
Enalapril
Pitavastatin 4 mg QD + enalapril 20 mg daily for 5 days
Enalapril
↑ 12%
↑ 12%
Enalaprilat
↓ 1%
↓ 1%
Warfarin
Individualized maintenance dose of warfarin (2 mg to 7 mg) for 8 days + pitavastatin 4 mg QD for 9 days
R-warfarin
↑ 7%
↑ 3%
S-warfarin
↑ 6%
↑ 3%
Ezetimibe
Pitavastatin 2 mg QD + ezetimibe 10 mg for 7 days
↑ 9%
↑ 2%
Digoxin
Pitavastatin 4 mg QD + digoxin 0.25 mg for 7 days
↓ 3%
↓ 4%
Diltiazem LA
Pitavastatin 4 mg QD on Days 1 to 5 and 11 to 15 and diltiazem LA 240 mg on Days 6 to 15
↓ 2%
↓ 7%
Rifampin
Pitavastatin 4 mg QD + rifampin 600 mg QD for 5 days
↓ 15%
↓ 18%
*Data presented as % change represent % difference relative to the investigated drug alone (i.e., 0% = no change).
BID = twice daily; QD = once daily; LA = Long Acting
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 92-week carcinogenicity study in mice given pitavastatin, at the maximum tolerated dose of 75 mg/kg/day with systemic maximum exposures (AUC) 26 times the clinical maximum exposure at 4 mg daily, there was an absence of drug-related tumors.
In a 92-week carcinogenicity study in rats given pitavastatin at 1, 5, 25 mg/kg/day by oral gavage there was a significant increase in the incidence of thyroid follicular cell tumors at 25 mg/kg/day, which represents 295 times human systemic exposures based on AUC at the 4 mg daily maximum human dose.
In a 26-week transgenic mouse (Tg rasH2) carcinogenicity study where animals were given pitavastatin at 30, 75, and 150 mg/kg/day by oral gavage, no clinically significant tumors were observed.
Pitavastatin was not mutagenic in the Ames test with Salmonella typhimurium and Escherichia coli with and without metabolic activation, the micronucleus test following a single administration in mice and multiple administrations in rats, the unscheduled DNA synthesis test in rats, and a Comet assay in mice. In the chromosomal aberration test, clastogenicity was observed at the highest doses tested, which also elicited high levels of cytotoxicity.
Pitavastatin had no adverse effects on male and female rat fertility at oral doses of 10 and 30 mg/kg/day, respectively, at systemic exposures 56- and 354-times clinical exposure at 4 mg daily based on AUC.
Pitavastatin treatment in rabbits resulted in mortality in males and females given 1 mg/kg/day (30-times clinical systemic exposure at 4 mg daily based on AUC) and higher during a fertility study. Although the cause of death was not determined, rabbits had gross signs of renal toxicity (kidneys whitened) indicative of possible ischemia. Lower doses (15-times human systemic exposure) did not show significant toxicity in adult males and females. However, decreased implantations, increased resorptions, and decreased viability of fetuses were observed.
-
14 CLINICAL STUDIES
Primary Hyperlipidemia in Adults
Study with Atorvastatin (Study 301)
Pitavastatin was compared with atorvastatin calcium tablets (referred to as atorvastatin) in a randomized, multicenter, double-blind, double-dummy, active-controlled, non-inferiority study of 817 adult patients with primary hyperlipidemia or mixed dyslipidemia. Patients entered a 6- to 8-week wash-out/dietary lead-in period and then were randomized to a 12-week treatment with either pitavastatin or atorvastatin (Table 5). Non-inferiority of pitavastatin to a given dose of atorvastatin was considered to be demonstrated if the lower bound of the 95% CI for the mean treatment difference was greater than -6% for the mean percent change in LDL-C.
Lipid results are shown in Table 5. For the percent change from baseline to endpoint in LDL-C, pitavastatin was non-inferior to atorvastatin for the two pairwise comparisons: pitavastatin 2 mg vs. atorvastatin 10 mg and pitavastatin 4 mg vs. atorvastatin 20 mg. Mean treatment differences (95% CI) were 0% (-3%, 3%) and 1% (-2%, 4%), respectively.
Table 5: Lipid Response by Dose of Pitavastatin and Atorvastatin in Adult Patients with Primary Hyperlipidemia or Mixed Dyslipidemia in Study 301 (Mean % Change from Baseline at Week 12)
Treatment
N
LDL-C
Apo-B
TC
TG
HDL-C
non-HDL-C
Pitavastatin 2 mg daily
315
-38
-30
-28
-14
4
-35
Pitavastatin 4 mg daily
298
-45
-35
-32
-19
5
-41
Atorvastatin
10 mg daily
102
-38
-29
-28
-18
3
-35
Atorvastatin
20 mg daily
102
-44
-36
-33
-22
2
-41
Study with Simvastatin (Study 302)
Pitavastatin was compared with simvastatin tablets (referred to as simvastatin) in a randomized, multicenter, double-blind, double-dummy, active-controlled, non-inferiority study of 843 adult patients with primary hyperlipidemia or mixed dyslipidemia. Patients entered a 6- to 8-week wash-out/dietary lead-in period and then were randomized to a 12 week treatment with either pitavastatin or simvastatin (Table 6). Non-inferiority of pitavastatin to a given dose of simvastatin was considered to be demonstrated if the lower bound of the 95% CI for the mean treatment difference was greater than -6% for the mean percent change in LDL-C.
Lipid results are shown in Table 6. For the percent change from baseline to endpoint in LDL-C, pitavastatin was non-inferior to simvastatin for the two pairwise comparisons: pitavastatin 2 mg vs. simvastatin 20 mg and pitavastatin 4 mg vs. simvastatin 40 mg. Mean treatment differences (95% CI) were 4% (1%, 7%) and 1% (-2%, 4%), respectively.
Table 6: Lipid Response by Dose of Pitavastatin and Simvastatin in Adult Patients with Primary Hyperlipidemia or Mixed Dyslipidemia in Study 302 (Mean % Change from Baseline at Week 12)
Treatment
N
LDL-C
Apo-B
TC
TG
HDL-C
non-HDL-C
Pitavastatin 2 mg daily
307
-39
-30
-28
-16
6
-36
Pitavastatin 4 mg daily
319
-44
-35
-32
-17
6
-41
Simvastatin
20 mg daily
107
-35
-27
-25
-16
6
-32
Simvastatin
40 mg daily
110
-43
-34
-31
-16
7
-39
Study with Pravastatin in Geriatric Patients (Study 306)
Pitavastatin was compared with pravastatin sodium tablets (referred to as pravastatin) in a randomized, multicenter, double-blind, double-dummy, parallel group, active-controlled non-inferiority study of 942 geriatric patients (≥ 65 years) with primary hyperlipidemia or mixed dyslipidemia. Patients entered a 6- to 8-week wash-out/dietary lead-in period, and then were randomized to a once daily dose of pitavastatin or pravastatin for 12 weeks (Table 7). Non-inferiority of pitavastatin to a given dose of pravastatin was assumed if the lower bound of the 95% CI for the treatment difference was greater than -6% for the mean percent change in LDL-C.
Lipid results are shown in Table 7. Pitavastatin significantly reduced LDL-C compared to pravastatin as demonstrated by the following pairwise dose comparisons: Pitavastatin 1 mg vs. pravastatin 10 mg, pitavastatin 2 mg vs. pravastatin 20 mg and pitavastatin 4 mg vs. pravastatin 40 mg. Mean treatment differences (95% CI) were 9% (6%, 12%), 10% (7%, 13%) and 10% (7%, 13% ), respectively.
Table 7: Lipid Response by Dose of Pitavastatin and Pravastatin in Geriatric Patients with Primary Hyperlipidemia or Mixed Dyslipidemia in Study 306 (Mean % Change from Baseline at Week 12)
Treatment
N
LDL-C
Apo-B
TC
TG
HDL-C
non-HDL-C
Pitavastatin 1 mg daily
207
-31
-25
-22
-13
1
-29
Pitavastatin 2 mg daily
224
-39
-31
-27
-15
2
-36
Pitavastatin 4 mg daily
210
-44
-37
-31
-22
4
-41
Pravastatin 10 mg daily
103
-22
-17
-15
-5
0
-20
Pravastatin 20 mg daily
96
-29
-22
-21
-11
-1
-27
Pravastatin 40 mg daily
102
-34
-28
-24
-15
1
-32
Study with Simvastatin in Patients with ≥ 2 Risk Factors for Coronary Heart Disease (Study 304)
Pitavastatin was compared with simvastatin tablets (referred to as simvastatin) in a randomized, multicenter, double-blind, double-dummy, active-controlled, non-inferiority study of 351 adult patients with primary hyperlipidemia or mixed dyslipidemia with ≥ 2 risk factors for coronary heart disease. After a 6- to 8-week wash-out/dietary lead-in period, patients were randomized to a 12-week treatment with either pitavastatin or simvastatin (Table 8). Non-inferiority of pitavastatin to simvastatin was considered to be demonstrated if the lower bound of the 95% CI for the mean treatment difference was greater than -6% for the mean percent change in LDL-C.
Lipid results are shown in Table 8. Pitavastatin 4 mg was non-inferior to simvastatin 40 mg for percent change from baseline to endpoint in LDL-C. The mean treatment difference (95% CI) was 0% (-2%, 3%).
Table 8: Lipid Response by Dose of Pitavastatin and Simvastatin in Adult Patients with Primary Hyperlipidemia or Mixed Dyslipidemia with ≥ 2 Risk Factors for Coronary Heart Disease in Study 304 (Mean % Change from Baseline at Week 12)
Treatment
N
LDL-C
Apo-B
TC
TG
HDL-C
non-HDL-C
Pitavastatin 4 mg daily
233
-44
-34
-31
-20
7
-40
Simvastatin 40 mg daily
118
-44
-34
-31
-15
5
-39
Study with Atorvastatin in Patients with Type 2 Diabetes Mellitus (Study 305)
Pitavastatin was compared with atorvastatin calcium tablets (referred to as atorvastatin) in a randomized, multicenter, double-blind, double-dummy, parallel group, active-controlled, non-inferiority study of 410 adult patients with type 2 diabetes mellitus and mixed dyslipidemia. Patients entered a 6- to 8-week washout/dietary lead-in period and were randomized to a once daily dose of pitavastatin or atorvastatin for 12 weeks. Non-inferiority of pitavastatin was considered to be demonstrated if the lower bound of the 95% CI for the mean treatment difference was greater than -6% for the mean percent change in LDL-C.
Lipid results are shown in Table 9. The treatment difference (95% CI) for LDL-C percent change from baseline was -2% (-6.2%, 1.5%). The two treatment groups were not statistically different on LDL-C. However, the lower limit of the CI was -6.2%, slightly exceeding the -6% non-inferiority limit. The study failed to demonstrate that pitavastatin was not significantly different than atorvastatin in lowering LDL-C in patients with type 2 diabetes mellitus and mixed dyslipidemia.
Table 9: Lipid Response by Dose of Pitavastatin and Atorvastatin in Adult Patients with Type 2 Diabetes Mellitus and Mixed Dyslipidemia in Study 305 (Mean % Change from Baseline at Week 12)
Treatment
N
LDL-C
Apo-B
TC
TG
HDL-C
non-HDL-C
Pitavastatin 4 mg daily
274
-41
-32
-28
-20
7
-36
Atorvastatin 20 mg daily
136
-43
-34
-32
-27
8
-40
The treatment differences in efficacy in LDL-C change from baseline between pitavastatin and active controls (i.e., atorvastatin, simvastatin, or pravastatin) in the in the active-controlled studies described above are summarized in Figure 1.
Figure 1: Treatment Difference in Adjusted Mean Percent Change in LDL-C between Pitavastatin and the Comparator (Atorvastatin, Simvastatin, or Pravastatin)
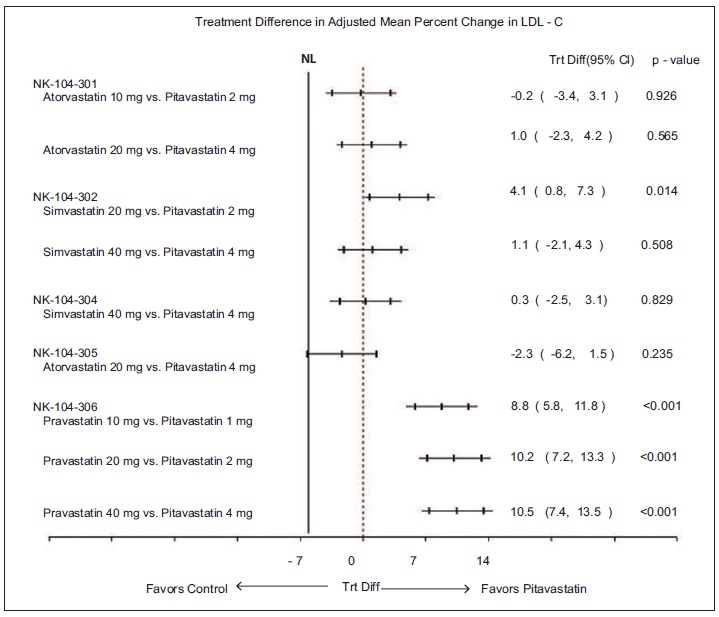
NL=non-inferiority limit.
HeFH in Pediatric Patients
In a double-blind, placebo-controlled, 12-week trial, 82 pediatric patients (36 boys and 46 girls), 8 to 16 years of age with genetically confirmed HeFH, fasting low-density lipoprotein cholesterol (LDL-C) ≥ 190 mg/dL or LDL-C ≥ 160 mg/dL with an additional cardiovascular risk factor (male gender, a family history of premature CV disease, presence of low HDL (< 45 mg/dL) or high TG (> 150 mg/dL), presence of high lipoprotein (a) (> 75 nmol/L), presence of type 2 diabetes mellitus or presence of hypertension) were randomized to pitavastatin 1 mg, 2 mg, and 4 mg. Mean LDL-C at baseline was 235 mg/dL (range 160.5 mg/dL to 441 mg/dL). Approximately 39% of patients were Tanner Stage 1 at baseline.
Pitavastatin significantly reduced plasma LDL-C, non-HDL-C, TC, and Apo-B compared to placebo. The reductions in LDL-C, Apo-B, TC, and non-HDL-C were dose dependent. There was no statistically significant improvement in HDL-C or TG at any pitavastatin dose. See the lipid results in Table 10.
Table 10: Lipid Response in Pediatric Patients with HeFH (Mean % Change from Baseline at Week 12)
Treatment
N
LDL-C
Apo-B
TC
TG*#
HDL-C*
non-HDL-C
Placebo
19
-1
-3
-1
-3
-1
-1
Pitavastatin 1 mg daily
20
-21
-20
-16
-14
7
-21
Pitavastatin 2 mg daily
24
-30
-25
-25
-15
-3
-29
Pitavastatin 4 mg daily
19
-38
-28
-30
5
-2
-36
*Difference from placebo not statistically significant
#Median Percent Change from Baseline at Week 12
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Pitavastatin tablets, 1 mg are supplied as white to off-white colored, round shaped, beveled edges, film-coated tablets, debossed with “AN” on one side and “029” on the other side.
They are available as follows:
Bottles of 30: NDC: 65162-029-03
Bottles of 90: NDC: 65162-029-09
Bottles of 500: NDC: 65162-029-50
Pitavastatin tablets, 2 mg are supplied as white to off-white colored, round shaped, beveled edges, film-coated tablets, debossed with “AN” on one side and “030” on the other side.
They are available as follows:
Bottles of 30: NDC: 65162-030-03
Bottles of 90: NDC: 65162-030-09
Bottles of 500: NDC: 65162-030-50
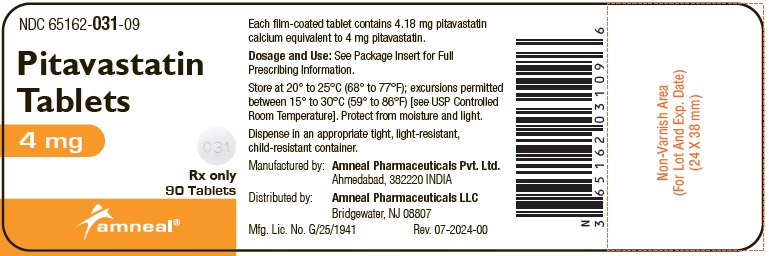
Pitavastatin tablets, 4 mg are supplied as white to off-white colored, round shaped, film-coated tablets, debossed with “AN” on one side and “031” on the other side.
They are available as follows:
Bottles of 30: NDC: 65162-031-03
Bottles of 90: NDC: 65162-031-09
Bottles of 500: NDC: 65162-031-50
Store at 20° to 25°C (68° to 77°F); excursions permitted between 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Protect from light.
-
17 PATIENT COUNSELING INFORMATION
Myopathy and Rhabdomyolysis
Advise patients that pitavastatin may cause myopathy and rhabdomyolysis. Inform patients that the risk is increased when taking certain types of medication and they should discuss all medication, both prescription and over the counter, with their healthcare provider. Instruct patients to promptly report any unexplained muscle pain, tenderness or weakness particularly if accompanied by malaise or fever [see Warnings and Precautions (5.1)].
Hepatic Dysfunction
Inform patients that pitavastatin may cause liver enzyme elevations and possibly liver failure. Advise patients to promptly report fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice [see Warnings and Precautions (5.3)].
Increases in HbA1c and Fasting Serum Glucose Levels
Inform patients that increases in HbA1c and fasting serum glucose levels may occur with pitavastatin. Encourage patients to optimize lifestyle measures, including regular exercise, maintaining a healthy body weight, and making healthy food choices [see Warnings and Precautions (5.4)].
Pregnancy
Advise pregnant patients and patients who become pregnant of the potential risk to a fetus. Advise patients to inform their healthcare provider of a known or suspected pregnancy to discuss if pitavastatin should be discontinued [see Use in Specific Populations (8.1)].
Lactation
Advise patients that breastfeeding is not recommended during treatment with pitavastatin [see Use in Specific Populations (8.2)].
Manufactured by:
Amneal Pharmaceuticals Pvt. Ltd.
Ahmedabad, 382220 INDIA
Distributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807
Rev. 07-2024-00
-
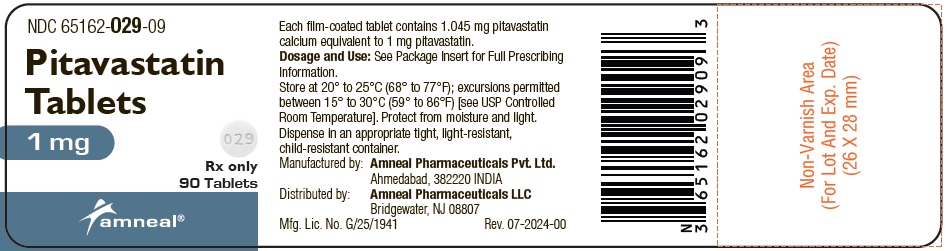
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC: 65162-029-09
Pitavastatin Tablets
1 mg
Rx only
90 Tablets
Amneal Pharmaceuticals LLC
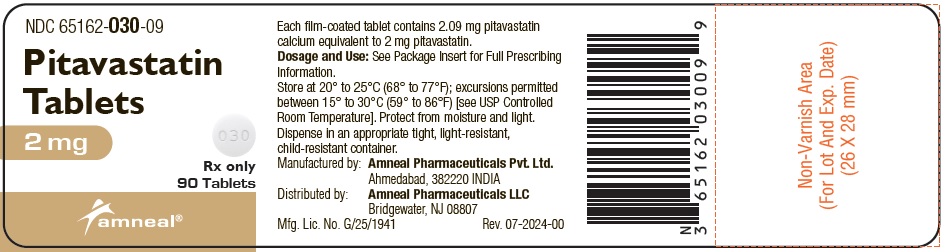
NDC: 65162-030-09
Pitavastatin Tablets
2 mg
Rx only
90 Tablets
Amneal Pharmaceuticals LLC
NDC: 65162-031-09
Pitavastatin Tablets
4 mg
Rx only
90 Tablets
Amneal Pharmaceuticals LLC
-
INGREDIENTS AND APPEARANCE
PITAVASTATIN
pitavastatin tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65162-029 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PITAVASTATIN CALCIUM (UNII: IYD54XEG3W) (PITAVASTATIN - UNII:M5681Q5F9P) PITAVASTATIN 1 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM ALUMINOMETASILICATE TYPE I-B (UNII: 8XK1039013) MAGNESIUM STEARATE (UNII: 70097M6I30) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) Product Characteristics Color white (white to off-white) Score no score Shape ROUND Size 6mm Flavor Imprint Code AN;029 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65162-029-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 2 NDC: 65162-029-09 90 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 3 NDC: 65162-029-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205961 08/21/2024 PITAVASTATIN
pitavastatin tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65162-030 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PITAVASTATIN CALCIUM (UNII: IYD54XEG3W) (PITAVASTATIN - UNII:M5681Q5F9P) PITAVASTATIN 2 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM ALUMINOMETASILICATE TYPE I-B (UNII: 8XK1039013) MAGNESIUM STEARATE (UNII: 70097M6I30) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) Product Characteristics Color white (white to off-white) Score no score Shape ROUND Size 8mm Flavor Imprint Code AN;030 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65162-030-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 2 NDC: 65162-030-09 90 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 3 NDC: 65162-030-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205961 08/21/2024 PITAVASTATIN
pitavastatin tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65162-031 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PITAVASTATIN CALCIUM (UNII: IYD54XEG3W) (PITAVASTATIN - UNII:M5681Q5F9P) PITAVASTATIN 4 mg Inactive Ingredients Ingredient Name Strength SILICON DIOXIDE (UNII: ETJ7Z6XBU4) HYDROXYPROPYL CELLULOSE (1600000 WAMW) (UNII: RFW2ET671P) HYPROMELLOSES (UNII: 3NXW29V3WO) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MAGNESIUM ALUMINOMETASILICATE TYPE I-B (UNII: 8XK1039013) MAGNESIUM STEARATE (UNII: 70097M6I30) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIETHYL CITRATE (UNII: 8Z96QXD6UM) Product Characteristics Color white (white to off-white) Score no score Shape ROUND Size 10mm Flavor Imprint Code AN;031 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65162-031-03 30 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 2 NDC: 65162-031-09 90 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 3 NDC: 65162-031-50 500 in 1 BOTTLE; Type 0: Not a Combination Product 08/21/2024 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA205961 08/21/2024 Labeler - Amneal Pharmaceuticals LLC (123797875) Establishment Name Address ID/FEI Business Operations Amneal Pharmaceuticals Private Limited 915076126 analysis(65162-029, 65162-030, 65162-031) , label(65162-029, 65162-030, 65162-031) , manufacture(65162-029, 65162-030, 65162-031) , pack(65162-029, 65162-030, 65162-031)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.