pimecrolimus by REMEDYREPACK INC. PIMECROLIMUS cream
pimecrolimus by
Drug Labeling and Warnings
pimecrolimus by is a Prescription medication manufactured, distributed, or labeled by REMEDYREPACK INC.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use PIMECROLIMUS CREAM safely and effectively. See full prescribing information for PIMECROLIMUS CREAM.
PIMECROLIMUScream, 1% for topical use
Initial U.S. Approval: 2001WARNING: LONG-TERM SAFETY OF TOPICAL CALCINEURIN INHIBITORS HAS NOT BEEN ESTABLISHED
See full prescribing information for complete boxed warning.
Although a causal relationship has not been established, rare cases of malignancy (e.g., skin and lymphoma) have been reported in patients treated with topical calcineurin inhibitors, including pimecrolimus cream, 1%. (5.1)
Therefore:
-
Continuous long-term use of topical calcineurin inhibitors, including pimecrolimus cream, 1%, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis. (2, 5.1)
- Pimecrolimus cream, 1% is not indicated for use in children less than 2 years of age. (1, 5.1, 8.4)
INDICATIONS AND USAGE
Pimecrolimus cream, 1% is a calcineurin inhibitor immunosuppressant indicated as second-line therapy for the short-term and non-continuous chronic treatment of mild to moderate atopic dermatitis in non-immunocompromised adults and children 2 years of age and older, who have failed to respond adequately to other topical prescription treatments, or when those treatments are not advisable. ( 1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Cream, 1%. ( 3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Should not be used in immunocompromised adults and children, including patients on systemic immunosuppressive medications. (
5.1)
- Avoid treatment on malignant or pre-malignant skin conditions, as these can present as dermatitis. (
5.2)
- Should not be used in patients with Netherton’s Syndrome or skin diseases with a potential for increased systemic absorption. ( 5.2)
ADVERSE REACTIONS
The most commonly reported adverse reactions (greater than or equal to 1%) were application site burning, headache, nasopharyngitis, cough, influenza, pyrexia and viral infection. ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Teva Pharmaceuticals USA, Inc. at 1-888-838-2872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 9/2019
-
Continuous long-term use of topical calcineurin inhibitors, including pimecrolimus cream, 1%, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis. (2, 5.1)
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: LONG-TERM SAFETY OF TOPICAL CALCINEURIN INHIBITORS HAS NOT BEEN ESTABLISHED
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Immunosuppression
5.2 Application to Malignant or Pre-malignant Skin Conditions
5.3 Bacterial and Viral Skin Infections
5.4 Patients with Lymphadenopathy
5.5 Sun Exposure
5.6 Immunocompromised Patients
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: LONG-TERM SAFETY OF TOPICAL CALCINEURIN INHIBITORS HAS NOT BEEN ESTABLISHED
Although a causal relationship has not been established, rare cases of malignancy (e.g., skin and lymphoma) have been reported in patients treated with topical calcineurin inhibitors, including pimecrolimus cream, 1% [see Warnings and Precautions (5.1)].
Therefore:-
Continuous long-term use of topical calcineurin inhibitors, including pimecrolimus cream, 1%, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis [see Dosage and Administration (2), Warnings and Precautions (5.1)].
- Pimecrolimus cream, 1% is not indicated for use in children less than 2 years of age [see Warnings and Precautions (5.1), Use in Specific Populations (8.4)].
-
Continuous long-term use of topical calcineurin inhibitors, including pimecrolimus cream, 1%, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis [see Dosage and Administration (2), Warnings and Precautions (5.1)].
-
1 INDICATIONS AND USAGE
Pimecrolimus cream, 1% is indicated as second-line therapy for the short-term and non-continuous chronic treatment of mild to moderate atopic dermatitis in non-immunocompromised adults and children 2 years of age and older, who have failed to respond adequately to other topical prescription treatments, or when those treatments are not advisable.
Pimecrolimus cream, 1% is not indicated for use in children less than 2 years of age [see Warnings and Precautions (5.1), Use in Specific Populations (8.4)].
-
2 DOSAGE AND ADMINISTRATION
Apply a thin layer of pimecrolimus cream, 1% to the affected skin twice daily. The patient should stop using pimecrolimus cream, 1% when signs and symptoms (e.g., itch, rash and redness) resolve and should be instructed on what actions to take if symptoms recur.
If signs and symptoms persist beyond 6 weeks, patients should be re-examined by their health care provider to confirm the diagnosis of atopic dermatitis.
Continuous long-term use of pimecrolimus cream, 1% should be avoided, and application should be limited to areas of involvement with atopic dermatitis [see Warnings and Precautions (5.1)].
The safety of pimecrolimus cream, 1% under occlusion, which may promote systemic exposure, has not been evaluated. Avoid use of pimecrolimus cream, 1% with occlusive dressings.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Immunosuppression
Prolonged systemic use of calcineurin inhibitors for sustained immunosuppression in animal studies and transplant patients following systemic administration has been associated with an increased risk of infections, lymphomas, and skin malignancies. These risks are associated with the intensity and duration of immunosuppression.
Based on this information and the mechanism of action, there is a concern about a potential risk with the use of topical calcineurin inhibitors, including pimecrolimus cream, 1%. While a causal relationship has not been established, rare cases of skin malignancy and lymphoma have been reported in patients treated with topical calcineurin inhibitors, including pimecrolimus cream, 1%. Therefore:
- Continuous long-term use of topical calcineurin inhibitors, including pimecrolimus cream, 1%, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis
- Pimecrolimus cream, 1% is not indicated for use in children less than 2 years of age
- Pimecrolimus cream, 1% should not be used in immunocompromised adults and children, including patients on systemic immunosuppressive medications.
- If signs and symptoms of atopic dermatitis do not improve within 6 weeks, patients should be re-examined by their healthcare provider and their diagnosis be confirmed.
- The safety of pimecrolimus cream, 1% has not been established beyond one year of non-continuous use.
5.2 Application to Malignant or Pre-malignant Skin Conditions
The use of pimecrolimus cream, 1% should be avoided on malignant or pre-malignant skin conditions. Malignant or pre-malignant skin conditions, such as cutaneous T-cell lymphoma (CTCL), can present as dermatitis.
Pimecrolimus cream, 1% should not be used in patients with Netherton’s Syndrome or other skin diseases where there is the potential for increased systemic absorption of pimecrolimus. The safety of pimecrolimus cream, 1% has not been established in patients with generalized erythroderma.
The use of pimecrolimus cream, 1% may cause local symptoms such as skin burning (burning sensation, stinging, soreness) or pruritus. Localized symptoms are most common during the first few days of pimecrolimus cream, 1% application and typically improve as the lesions of atopic dermatitis resolve [see Adverse Reactions (6.1)].
5.3 Bacterial and Viral Skin Infections
Before commencing treatment with pimecrolimus cream, 1%, bacterial or viral infections at treatment sites should be resolved. Trials have not evaluated the safety and efficacy of pimecrolimus cream, 1% in the treatment of clinically infected atopic dermatitis.
While patients with atopic dermatitis are predisposed to superficial skin infections including eczema herpeticum (Kaposi’s varicelliform eruption), treatment with pimecrolimus cream, 1% may be independently associated with an increased risk of varicella zoster virus infection (chicken pox or shingles), herpes simplex virus infection, or eczema herpeticum.
In clinical trials, 15/1,544 (1%) cases of skin papilloma (warts) were observed in subjects using pimecrolimus cream, 1%. The youngest subject was age 2 and the oldest was age 12. In cases where there is worsening of skin papillomas or they do not respond to conventional therapy, discontinuation of pimecrolimus cream, 1% should be considered until complete resolution of the warts is achieved.
5.4 Patients with Lymphadenopathy
In clinical trials, 14/1,544 (0.9%) cases of lymphadenopathy were reported while using pimecrolimus cream, 1%. These cases of lymphadenopathy were usually related to infections and noted to resolve upon appropriate antibiotic therapy. Of these 14 cases, the majority had either a clear etiology or were known to resolve. Patients who receive pimecrolimus cream, 1% and who develop lymphadenopathy should have the etiology of their lymphadenopathy investigated. In the absence of a clear etiology for the lymphadenopathy, or in the presence of acute infectious mononucleosis, pimecrolimus cream, 1% should be discontinued. Patients who develop lymphadenopathy should be monitored to ensure that the lymphadenopathy resolves.
- Continuous long-term use of topical calcineurin inhibitors, including pimecrolimus cream, 1%, in any age group should be avoided, and application limited to areas of involvement with atopic dermatitis
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
No phototoxicity and no photoallergenicity were detected in clinical trials with 24 and 33 normal volunteers, respectively. In human dermal safety trials, pimecrolimus cream, 1% did not induce contact sensitization or cumulative irritation.
In a one-year safety trial in pediatric subjects age 2 to 17 years old involving sequential use of pimecrolimus cream, 1% and a topical corticosteroid, 43% of pimecrolimus cream, 1% treated subjects and 68% of vehicle-treated subjects used corticosteroids during the trial. Corticosteroids were used for more than 7 days by 34% of pimecrolimus cream, 1% treated subjects and 54% of vehicle-treated subjects. An increased incidence of impetigo, skin infection, superinfection (infected atopic dermatitis), rhinitis, and urticaria were found in the subjects that had used pimecrolimus cream, 1% and topical corticosteroid sequentially as compared to pimecrolimus cream, 1% alone.
In 3 randomized, double-blind vehicle-controlled pediatric trials and one active-controlled adult trial, 843 and 328 subjects respectively, were treated with pimecrolimus cream, 1%. In these clinical trials, 48 (4%) of the 1,171 pimecrolimus treated subjects and 13 (3%) of 408 vehicle-treated subjects discontinued therapy due to adverse events. Discontinuations for AEs were primarily due to application site reactions, and cutaneous infections. The most common application site reaction was application site burning, which occurred in 8% to 26% of subjects treated with pimecrolimus cream, 1%.
Table 1 depicts the incidence of adverse events pooled across the 2 identically designed 6-week trials with their open label extensions and the 1-year safety trial for pediatric subjects ages 2 to 17. Data from the adult active-controlled trial is also included in Table 1. Adverse events are listed regardless of relationship to trial drug.
Table 1. Treatment Emergent Adverse Events (≥1%) in Pimecrolimus Cream Treatment Groups
Pediatric Subjects*Pediatric Subjects* Pediatric Subjects* Adult Active Vehicle-Controlled Open-Label Vehicle-Controlled Comparator (6 weeks) (20 weeks) (1 year) (1 year) Pimecrolimus Cream
VehiclePimecrolimus Cream Pimecrolimus Cream
VehiclePimecrolimus Cream (N=267) (N=136) (N=335) (N=272) (N=75) (N=328) N (%) N (%) N (%) N (%) N (%) N (%) At least 1 AE 182 (68.2%) 97 (71.3%) 240 (72.0%) 230 (84.6%) 56 (74.7%) 256 (78.0%) Infections and Infestations Upper Respiratory Tract
Infection NOS38 (14.2%) 18 (13.2%) 65 (19.4%) 13 (4.8%) 6 (8.0%) 14 (4.3%) Nasopharyngitis 27 (10.1%) 10 (7.4%) 32 (19.6%) 72 (26.5%) 16 (21.3%) 25 (7.6%) Skin Infection NOS 8 (3.0%) 9 (5.1%) 18 (5.4%) 6 (2.2%) 3 (4.0%) 21 (6.4%) Influenza 8 (3.0%) 1 (0.7%) 22 (6.6%) 36 (13.2%) 3 (4.0%) 32 (9.8%) Ear Infection NOS 6 (2.2%) 2 (1.5%) 19 (5.7%) 9 (3.3%) 1 (1.3%) 2 (0.6%) Otitis Media 6 (2.2%) 1 (0.7%) 10 (3.0%) 8 (2.9%) 4 (5.3%) 2 (0.6%) Impetigo 5 (1.9%) 3 (2.2%) 12 (3.6%) 11 (4.0%) 4 (5.3%) 8 (2.4%) Bacterial Infection 4 (1.5%) 3 (2.2%) 4 (1.2%) 3 (1.1%) 0 6 (1.8%) Folliculitis 3 (1.1%) 1 (0.7%) 3 (0.9%) 6 (2.2%) 3 (4.0%) 20 (6.1%) Sinusitis 3 (1.1%) 1 (0.7%) 11 (3.3%) 6 (2.2%) 1 (1.3%) 2 (0.6%) Pneumonia NOS 3 (1.1%) 1 (0.7%) 5 (1.5%) 0 1 (1.3%) 1 (0.3%) Pharyngitis NOS 2 (0.7%) 2 (1.5%) 3 (0.9%) 22 (8.1%) 2 (2.7%) 3 (0.9%) Pharyngitis Streptococcal 2 (0.7%) 2 (1.5%) 10 (3.0%) 0 <1% 0 Molluscum Contagiosum 2 (0.7%) 0 4 (1.2%) 5 (1.8%) 0 0 Staphylococcal Infection 1 (0.4%) 5 (3.7%) 7 (2.1%) 0 <1% 3 (0.9%) Bronchitis NOS 1 (0.4%) 3 (2.2%) 4 (1.2%) 29 (10.7%) 6 (8.0%) 8 (2.4%) Herpes Simplex 1 (0.4%) 0 4 (1.2%) 9 (3.3%) 2 (2.7%) 13 (4.0%) Tonsillitis NOS 1 (0.4%) 0 3 (0.9%) 17 (6.3%) 0 2 (0.6%) Viral Infection NOS 2 (0.7%) 1 (0.7%) 1 (0.3%) 18 (6.6%) 1 (1.3%) 0 Gastroenteritis NOS 0 3 (2.2%) 2 (0.6%) 20 (7.4%) 2 (2.7%) 6 (1.8%) Chickenpox 2 (0.7%) 0 3 (0.9%) 8 (2.9%) 3 (4.0%) 1 (0.3%) Skin Papilloma 1 (0.4%) 0 2 (0.6%) 9 (3.3%) <1% 0 Tonsillitis Acute NOS 0 0 0 7 (2.6%) 0 0 Upper Respiratory Tract
Infection Viral NOS1 (0.4%) 0 3 (0.9%) 4 (1.5%) 0 1 (0.3%) Herpes Simplex Dermatitis 0 0 1 (0.3%) 4 (1.5%) 0 2 (0.6%) Bronchitis Acute NOS 0 0 0 4 (1.5%) 0 0 Eye Infection NOS 0 0 0 3 (1.1%) <1% 1 (0.3%) General Disorders and Administration Site Conditions Application Site Burning 28 (10.4%) 17 (12.5%) 5 (1.5%) 23 (8.5%) 5 (6.7%) 85 (25.9%) Pyrexia 20 (7.5%) 12 (8.8%) 41 (12.2%) 34 (12.5%) 4 (5.3%) 4 (1.2%) Application Site Reaction
NOS8 (3.0%) 7 (5.1%) 7 (2.1%) 9 (3.3%) 2 (2.7%) 48 (14.6%) Application Site Irritation 8 (3.0%) 8 (5.9%) 3 (0.9%) 1 (0.4%) 3 (4.0%) 21 (6.4%) Influenza Like Illness 1 (0.4%) 0 2 (0.6%) 5 (1.8%) 2 (2.7%) 6 (1.8%) Application Site Erythema 1 (0.4%) 0 0 6 (2.2%) 0 7 (2.1%) Application Site Pruritus 3 (1.1%) 2 (1.5%) 2 (0.6%) 5 (1.8%) 0 18 (5.5%) Respiratory, Thoracic and Mediastinal Disorders Cough 31 (11.6%) 11 (8.1%) 31 (9.3%) 43 (15.8%) 8 (10.7%) 8 (2.4%) Nasal Congestion 7 (2.6%) 2 (1.5%) 6 (1.8%) 4 (1.5%) 1 (1.3%) 2 (0.6%) Rhinorrhea 5 (1.9%) 1 (0.7%) 3 (0.9%) 1 (0.4%) 1 (1.3%) 0 Asthma Aggravated 4 (1.5%) 3 (2.2%) 13 (3.9%) 3 (1.1%) 1 (1.3%) 0 Sinus Congestion 3 (1.1%) 1 (0.7%) 2 (0.6%) <1% <1% 3 (0.9%) Rhinitis 1 (0.4%) 0 5 (1.5%) 12 (4.4%) 5 (6.7%) 7 (2.1%) Wheezing 1 (0.4%) 1 (0.7%) 4 (1.2%) 2 (0.7%) <1% 0 Asthma NOS 2 (0.7%) 1 (0.7%) 11 (3.3%) 10 (3.7%) 2 (2.7%) 8 (2.4%) Epistaxis 0 1 (0.7%) 0 9 (3.3%) 1 (1.3%) 1 (0.3%) Dyspnea NOS 0 0 0 5 (1.8%) 1 (1.3%) 2 (0.6%) Gastrointestinal Disorders Abdominal Pain Upper 11 (4.1%) 6 (4.4%) 10 (3.0%) 15 (5.5%) 5 (6.7%) 1 (0.3%) Sore Throat 9 (3.4%) 5 (3.7%) 15 (5.4%) 22 (8.1%) 4 (5.3%) 12 (3.7%) Vomiting NOS 8 (3.0%) 6 (4.4%) 14 (4.2%) 18 (6.6%) 6 (8.0%) 2 (0.6%) Diarrhea NOS 3 (1.1%) 1 (0.7%) 2 (0.6%) 21 (7.7%) 4 (5.3%) 7 (2.1%) Nausea 1 (0.4%) 3 (2.2%) 4 (1.2%) 11 (4.0%) 5 (6.7%) 6 (1.8%) Abdominal Pain NOS 1 (0.4%) 1 (0.7%) 5 (1.5%) 12 (4.4%) 3 (4.0%) 1 (0.3%) Toothache 1 (0.4%) 1 (0.7%) 2 (0.6%) 7 (2.6%) 1 (1.3%) 2 (0.6%) Constipation 1 (0.4%) 0 2 (0.6%) 10 (3.7%) <1% 0 Loose Stools 0 1 (0.7%) 4 (1.2%) <1% <1% 0 Reproductive System and Breast Disorders Dysmenorrhea 3 (1.1%) 0 5 (1.5%) 3 (1.1%) 1 (1.3%) 4 (1.2%) Eye Disorders Conjunctivitis NEC 2 (0.7%) 1 (0.7%) 7 (2.1%) 6 (2.2%) 3 (4.0%) 10 (3.0%) Skin & Subcutaneous Tissue Disorders Urticaria 3 (1.1%) 0 1 (0.3%) 1 (0.4%) <1% 3 (0.9%) Acne NOS 0 1 (0.7%) 1 (0.3%) 4 (1.5%) <1% 6 (1.8%) Immune System Disorders Hypersensitivity NOS 11 (4.1%) 6 (4.4%) 16 (4.8%) 14 (5.1%) 1 (1.3%) 11 (3.4%) Injury and Poisoning Accident NOS 3 (1.1%) 1 (0.7%) 1 (0.3%) <1% 1 (1.3%) 0 Laceration 2 (0.7%) 1 (0.7%) 5 (1.5%) <1% <1% 0 Musculoskeletal, Connective Tissue and Bone Disorders Back Pain 1 (0.4%) 2 (1.5%) 1 (0.3%) <1% 0 6 (1.8%) Arthralgias 0 0 1 (0.3%) 3 (1.1%) 1 (1.3%) 5 (1.5%) Ear and Labyrinth Disorders Earache 2 (0.7%) 1 (0.7%) 0 8 (2.9%) 2 (2.7%) 0 Nervous System Disorders Headache 37 (13.9%) 12 (8.8%) 38 (11.3%) 69 (25.4%) 12 (16.0%) 23 (7.0%) *Ages 2 to 17 years Two cases of septic arthritis have been reported in infants less than one year of age in clinical trials conducted with pimecrolimus cream, 1% (n = 2,443). Causality has not been established.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of pimecrolimus cream, 1%. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General: Anaphylactic reactions, ocular irritation after application of the cream to the eye lids or near the eyes, angioneurotic edema, facial edema, skin flushing associated with alcohol use, skin discoloration.
Hematology/Oncology: Lymphomas, basal cell carcinoma, malignant melanoma, squamous cell carcinoma.
-
7 DRUG INTERACTIONS
Potential interactions between pimecrolimus cream, 1% and other drugs, including immunizations, have not been systematically evaluated. Due to low blood levels of pimecrolimus detected in some patients after topical application, systemic drug interactions are not expected, but cannot be ruled out. The concomitant administration of known CYP3A family of inhibitors in patients with widespread and/or erythrodermic disease should be done with caution. Some examples of such drugs are erythromycin, itraconazole, ketoconazole, fluconazole, calcium channel blockers and cimetidine.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies with pimecrolimus cream, 1% in pregnant women. Therefore, pimecrolimus cream, 1% should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In dermal embryofetal developmental studies, no maternal or fetal toxicity was observed up to the highest practicable doses tested, 10 mg/kg/day (1% pimecrolimus cream) in rats (0.14X MRHD based on body surface area) and 10 mg/kg/day (1% pimecrolimus cream) in rabbits (0.65X MRHD based on AUC comparisons). The 1% pimecrolimus cream was administered topically for 6 hours/day during the period of organogenesis in rats and rabbits (gestational days 6 to 21 in rats and gestational days 6 to 20 in rabbits).
A second dermal embryofetal development study was conducted in rats using pimecrolimus cream applied dermally to pregnant rats (1 g cream/kg body weight of 0.2%, 0.6% and 1.0% pimecrolimus cream) from gestation day 6 to 17 at doses of 2, 6, and 10 mg/kg/day with daily exposure of approximately 22 hours. No maternal, reproductive, or embryo-fetal toxicity attributable to pimecrolimus was noted at 10 mg/kg/day (0.66X MRHD based on AUC comparisons), the highest dose evaluated in this study. No teratogenicity was noted in this study at any dose.
A combined oral fertility and embryofetal developmental study was conducted in rats and an oral embryofetal developmental study was conducted in rabbits. Pimecrolimus was administered during the period of organogenesis (2 weeks prior to mating until gestational day 16 in rats, gestational days 6 to 18 in rabbits) up to dose levels of 45 mg/kg/day in rats and 20 mg/kg/day in rabbits. In the absence of maternal toxicity, indicators of embryofetal toxicity (post-implantation loss and reduction in litter size) were noted at 45 mg/kg/day (38X MRHD based on AUC comparisons) in the oral fertility and embryofetal developmental study conducted in rats. No malformations in the fetuses were noted at 45 mg/kg/day (38X MRHD based on AUC comparisons) in this study. No maternal toxicity, embryotoxicity or teratogenicity were noted in the oral rabbit embryofetal developmental toxicity study at 20 mg/kg/day (3.9X MRHD based on AUC comparisons), which was the highest dose tested in this study.
A second oral embryofetal development study was conducted in rats. Pimecrolimus was administered during the period of organogenesis (gestational days 6 to 17) at doses of 2, 10 and 45 mg/kg/day. Maternal toxicity, embryolethality and fetotoxicity were noted at 45 mg/kg/day (271X MRHD based on AUC comparisons). A slight increase in skeletal variations that were indicative of delayed skeletal ossification was also noted at this dose. No maternal toxicity, embryolethality or fetotoxicity were noted at 10 mg/kg/day (16X MRHD based on AUC comparisons). No teratogenicity was noted in this study at any dose.
A second oral embryofetal development study was conducted in rabbits. Pimecrolimus was administered during the period of organogenesis (gestational days 7 to 20) at doses of 2, 6 and 20 mg/kg/day. Maternal toxicity, embryotoxicity and fetotoxicity were noted at 20 mg/kg/day (12X MRHD based on AUC comparisons). A slight increase in skeletal variations that were indicative of delayed skeletal ossification was also noted at this dose. No maternal toxicity, embryotoxicity or fetotoxicity were noted at 6 mg/kg/day (5X MRHD based on AUC comparisons). No teratogenicity was noted in this study at any dose.
An oral peri- and post-natal developmental study was conducted in rats. Pimecrolimus was administered from gestational day 6 through lactational day 21 up to a dose level of 40 mg/kg/day. Only 2 of 22 females delivered live pups at the highest dose of 40 mg/kg/day. Postnatal survival, development of the F1 generation, their subsequent maturation and fertility were not affected at 10 mg/kg/day (12X MRHD based on AUC comparisons), the highest dose evaluated in this study.
Pimecrolimus was transferred across the placenta in oral rat and rabbit embryofetal developmental studies.
8.3 Nursing Mothers
It is not known whether this drug is excreted in human milk. Because of the potential for serious adverse reactions in nursing infants from pimecrolimus, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Pimecrolimus cream, 1% is not indicated for use in children less than 2 years of age.
The long-term safety and effects of pimecrolimus cream, 1% on the developing immune system are unknown.
Three Phase 3 pediatric trials were conducted involving 1,114 subjects 2 to 17 years of age. Two trials were 6-week randomized vehicle-controlled trials with a 20-week open-label phase and one was a vehicle-controlled (up to 1 year) safety trial with the option for sequential topical corticosteroid use. Of these subjects 542 (49%) were 2 to 6 years of age. In the short-term trials, 11% of pimecrolimus subjects did not complete these trials and 1.5% of pimecrolimus subjects discontinued due to adverse events. In the one-year trial, 32% of pimecrolimus subjects did not complete this trial and 3% of pimecrolimus subjects discontinued due to adverse events. Most discontinuations were due to unsatisfactory therapeutic effect.
The most common local adverse event in the short-term trials of pimecrolimus cream, 1% in pediatric subjects ages 2 to 17 was application site burning (10% vs. 13% vehicle); the incidence in the long-term trial was 9% pimecrolimus vs. 7% vehicle [see Adverse Reactions (6.1)]. Adverse events that were more frequent (greater than 5%) in subjects treated with pimecrolimus cream, 1% compared to vehicle were headache (14% vs. 9%) in the short-term trial. Nasopharyngitis (26% vs. 21%), influenza (13% vs. 4%), pharyngitis (8% vs. 3%), viral infection (7% vs. 1%), pyrexia (13% vs. 5%), cough (16% vs. 11%), and headache (25% vs. 16%) were increased over vehicle in the 1-year safety trial [see Adverse Reactions (6.1)]. In 843 subjects ages 2 to 17 years treated with pimecrolimus cream, 1%, 9 (0.8%) developed eczema herpeticum (5 on pimecrolimus cream, 1% alone and 4 on pimecrolimus cream, 1% used in sequence with corticosteroids). In 211 subjects on vehicle alone, there were no cases of eczema herpeticum. The majority of adverse events were mild to moderate in severity.
Two Phase 3 trials were conducted involving 436 infants age 3 months-23 months. One 6-week randomized vehicle-controlled trial with a 20-week open-label phase and one safety trial, up to one year, were conducted. In the 6-week trial, 11% of pimecrolimus and 48% of vehicle subjects did not complete this trial; no subject in either group discontinued due to adverse events. Infants on pimecrolimus cream, 1% had an increased incidence of some adverse events compared to vehicle. In the 6-week vehicle-controlled trial these adverse events included pyrexia (32% vs. 13% vehicle), URI (24% vs. 14%), nasopharyngitis (15% vs. 8%), gastroenteritis (7% vs. 3%), otitis media (4% vs. 0%), and diarrhea (8% vs. 0%). In the open-label phase of the trial, for infants who switched to pimecrolimus cream, 1% from vehicle, the incidence of the above-cited adverse events approached or equaled the incidence of those subjects who remained on pimecrolimus cream, 1%. In the 6 month safety data, 16% of pimecrolimus and 35% of vehicle subjects discontinued early and 1.5% of pimecrolimus and 0% of vehicle subjects discontinued due to adverse events. Infants on pimecrolimus cream, 1% had a greater incidence of some adverse events as compared to vehicle. These included pyrexia (30% vs. 20%), URI (21% vs. 17%), cough (15% vs. 9%), hypersensitivity (8% vs. 2%), teething (27% vs. 22%), vomiting (9% vs. 4%), rhinitis (13% vs. 9%), viral rash (4% vs. 0%), rhinorrhea (4% vs. 0%), and wheezing (4% vs. 0%).
The systemic exposure to pimecrolimus from pimecrolimus cream, 1% was investigated in 28 pediatric subjects with atopic dermatitis (20% to 80% BSA involvement) between the ages of 8 months to 14 yrs. Following twice daily application for three weeks, blood concentrations of pimecrolimus were less than 2 ng/mL with 60% (96/161) of the blood samples having blood concentration below the limit of quantification (0.5 ng/mL). However, more children (23 children out of the total 28 children investigated) had at least one detectable blood level as compared to the adults (12 adults out of the total 52 adults investigated) over a 3-week treatment period. Due to the erratic nature of the blood levels observed, no correlation could be made between amount of cream, degree of BSA involvement, and blood concentrations. In general, the blood concentrations measured in adult atopic dermatitis subjects were comparable to those seen in the pediatric population.
In a second group of 30 pediatric subjects aged 3 to 23 months with 10% to 92% BSA involvement, following twice daily application for three weeks, blood concentrations of pimecrolimus were less than 2.6 ng/mL with 65% (75/116) of the blood samples having blood concentration below 0.5ng/mL, and 27% (31/116) below the limit of quantification (0.1 ng/mL) for these trials.
Overall, a higher proportion of detectable blood levels was seen in the pediatric subject population as compared to adult population. This increase in the absolute number of positive blood levels may be due to the larger surface area to body mass ratio seen in these younger subjects. In addition, a higher incidence of upper respiratory symptoms/infections was also seen relative to the older age group in the PK trials. At this time, a causal relationship between these findings and pimecrolimus use cannot be ruled out.
-
11 DESCRIPTION
Pimecrolimus cream, 1%, for topical use, contains the compound pimecrolimus, the immunosuppressant 33-epi-chloro-derivative of the macrolactam ascomycin.
Chemically, pimecrolimus is (1R,9S,12S,13R,14S,17R,18E,21S,23S,24R,25S,27R)-12-[(1E)-2-{(1R,3R,4S)-4-chloro-3-methoxycyclohexyl}-1-methylvinyl]-17-ethyl-1,14-dihydroxy-23,25-dimethoxy-13,19,21,27-tetramethyl-11,28-dioxa-4-aza-tricyclo[22.3.1.04,9]octacos-18-ene-2,3,10,16-tetraone. The compound has the molecular formula C 43H 68CINO 11 and the molecular weight of 810.47. The structural formula is:
![The Structural formula of pimecrolimus is (1R,9S,12S,13R,14S,17R,18E,21S,23S,24R,25S,27R)-12-[(1E)-2-{(1R,3R,4S)-4-chloro-3-methoxycyclohexyl}-1-methylvinyl]-17-ethyl-1,14-dihydroxy-23,25-dimethoxy-13](https://fda.report/DailyMed/802a1ab4-690f-47bd-b1f3-f20a7a04978b/pimecrolimus-cream-a209345-1.jpg)
Pimecrolimus is a white to off-white fine crystalline powder. It is soluble in methanol and ethanol and insoluble in water.
Each gram of pimecrolimus cream, 1% contains 10 mg of pimecrolimus in a whitish cream base of benzyl alcohol, cetyl alcohol, cetostearyl alcohol (type A), citric acid anhydrous, medium-chain triglycerides, mono- and di-glycerides, oleyl alcohol, propylene glycol, sodium hydroxide, stearyl alcohol, and water.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of pimecrolimus in atopic dermatitis is not known. While the following have been observed, the clinical significance of these observations in atopic dermatitis is not known. It has been demonstrated that pimecrolimus binds with high affinity to macrophilin-12 (FKBP-12) and inhibits the calcium-dependent phosphatase, calcineurin. As a consequence, it inhibits T cell activation by blocking the transcription of early cytokines. In particular, pimecrolimus inhibits at nanomolar concentrations Interleukin-2 and interferon gamma (Th1-type) and Interleukin-4 and Interleukin-10 (Th2-type) cytokine synthesis in human T-cells. In addition, pimecrolimus prevents the release of inflammatory cytokines and mediators from mast cells in vitro after stimulation by antigen/IgE.
12.3 Pharmacokinetics
Absorption
In adult subjects (n=52) being treated for atopic dermatitis [13% to 62% Body Surface Area (BSA) involvement] for periods up to a year, a maximum pimecrolimus concentration of 1.4 ng/mL was observed among those subjects with detectable blood levels. In the majority of samples in adult (91%; 1,244/1,362) subjects, blood concentrations of pimecrolimus were below 0.5 ng/mL. Data on blood levels of pimecrolimus measured in pediatric subjects are described in Use in Specific Populations (8.4).
Distribution
Laboratory in vitro plasma protein binding studies using equilibrium gel filtration have shown that 99.5% of pimecrolimus in plasma is bound to proteins over the pimecrolimus concentration range of 2 ng/mL to 100 ng/mL tested. The major fraction of pimecrolimus in plasma appears to be bound to various lipoproteins. As with other topical calcineurin inhibitors, it is not known whether pimecrolimus is absorbed into cutaneous lymphatic vessels or in regional lymph nodes.
Metabolism
Following the administration of a single oral radiolabeled dose of pimecrolimus numerous circulating Odemethylation metabolites were seen. Studies with human liver microsomes indicate that pimecrolimus is metabolized in vitro by the CYP3A sub-family of metabolizing enzymes. No evidence of skin mediated drug metabolism was identified in vivo using the minipig or in vitro using stripped human skin.
Elimination
Based on the results of the aforementioned radiolabeled study, following a single oral dose of pimecrolimus ~81% of the administered radioactivity was recovered, primarily in the feces (78.4%) as metabolites. Less than 1% of the radioactivity found in the feces was due to unchanged pimecrolimus.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year rat dermal carcinogenicity study using pimecrolimus cream, 1%, a statistically significant increase in the incidence of follicular cell adenoma of the thyroid was noted in low, mid and high dose male animals compared to vehicle and saline control male animals. Follicular cell adenoma of the thyroid was noted in the dermal rat carcinogenicity study at the lowest dose of 2 mg/kg/day [0.2% pimecrolimus cream; 1.5X the Maximum Recommended Human Dose (MRHD) based on AUC comparisons]. No increase in the incidence of follicular cell adenoma of the thyroid was noted in the oral carcinogenicity study in male rats up to 10 mg/kg/day (66X MRHD based on AUC comparisons). However, oral studies may not reflect continuous exposure or the same metabolic profile as by the dermal route. In a mouse dermal carcinogenicity study using pimecrolimus in an ethanolic solution, no increase in incidence of neoplasms was observed in the skin or other organs up to the highest dose of 4 mg/kg/day (0.32% pimecrolimus in ethanol) 27X MRHD based on AUC comparisons. However, lymphoproliferative changes (including lymphoma) were noted in a 13 week repeat dose dermal toxicity study conducted in mice using pimecrolimus in an ethanolic solution at a dose of 25 mg/kg/day (47X MRHD based on AUC comparisons). No lymphoproliferative changes were noted in this study at a dose of 10 mg/kg/day (17X MRHD based on AUC comparison). However, the latency time to lymphoma formation was shortened to 8 weeks after dermal administration of pimecrolimus dissolved in ethanol at a dose of 100 mg/kg/day (179-217X MRHD based on AUC comparisons).
In a mouse oral (gavage) carcinogenicity study, a statistically significant increase in the incidence of lymphoma was noted in high dose male and female animals compared to vehicle control male and female animals. Lymphomas were noted in the oral mouse carcinogenicity study at a dose of 45 mg/kg/day (258-340X MRHD based on AUC comparisons). No drug-related tumors were noted in the mouse oral carcinogenicity study at a dose of 15 mg/kg/day (60-133X MRHD based on AUC comparisons).
In an oral (gavage) rat carcinogenicity study, a statistically significant increase in the incidence of benign thymoma was noted in 10 mg/kg/day pimecrolimus treated male and female animals compared to vehicle control treated male and female animals. In addition, a significant increase in the incidence of benign thymoma was noted in another oral (gavage) rat carcinogenicity study in 5 mg/kg/day pimecrolimus treated male animals compared to vehicle control treated male animals. No drug-related tumors were noted in the rat oral carcinogenicity study at a dose of 1 mg/kg/day male animals (1.1X MRHD based on AUC comparisons) and at a dose of 5 mg/kg/day for female animals (21X MRHD based on AUC comparisons).
In a 52-week dermal photo-carcinogenicity study, the median time to onset of skin tumor formation was decreased in hairless mice following chronic topical dosing with concurrent exposure to UV radiation (40 weeks of treatment followed by 12 weeks of observation) with the pimecrolimus cream, 1% vehicle alone. No additional effect on tumor development beyond the vehicle effect was noted with the addition of the active ingredient, pimecrolimus, to the vehicle cream.
A 39-week oral monkey toxicology study was conducted with pimecrolimus doses of 15 mg/kg/day,
45 mg/kg/day and 120 mg/kg/day. A dose dependent increase in expression of immunosuppressive-related lymphoproliferative disorder (IRLD) associated with lymphocryptovirus (a monkey strain of virus related to human Epstein Barr virus) was observed. IRLD in monkeys mirrors what has been noted in human transplant patients after chronic systemic immunosuppressive therapy, post transplantation lymphoproliferative disease (PTLD), after treatment with chronic systemic immunosuppressive therapy. Both IRLD and PTLD can progress to lymphoma, which is dependent on the dose and duration of systemic immunosuppressive therapy. A dose dependent increase in opportunistic infections (a signal of systemic immunosuppression) was also noted in this monkey study. A no observed adverse effect level (NOAEL) for IRLD and opportunistic infections was not established in this study. IRLD occurred at the lowest dose of 15 mg/kg/day for 39 weeks [31X the Maximum Recommended Human Dose (MRHD) of pimecrolimus cream, 1% based on AUC comparisons] in this study. A partial recovery from IRLD was noted upon cessation of dosing in this study.A battery of in vitro genotoxicity tests, including Ames assay, mouse lymphoma L5178Y assay, and chromosome aberration test in V79 Chinese hamster cells and an in vivo mouse micronucleus test revealed no evidence for a mutagenic or clastogenic potential for the drug.
An oral fertility and embryofetal developmental study in rats revealed estrus cycle disturbances, post-implantation loss and reduction in litter size at the 45 mg/kg/day dose (38X MRHD based on AUC comparisons). No effect on fertility in female rats was noted at 10 mg/kg/day (12X MRHD based on AUC comparisons). No effect on fertility in male rats was noted at 45 mg/kg/day (23X MRHD based on AUC comparisons), which was the highest dose tested in this study.
A second oral fertility and embryofetal developmental study in rats revealed reduced testicular and epididymal weights, reduced testicular sperm counts and motile sperm for males and estrus cycle disturbances, decreased corpora lutea, decreased implantations and viable fetuses for females at 45 mg/kg/day dose (123X MRHD for males and 192X MRHD for females based on AUC comparisons). No effect on fertility in female rats was noted at 10 mg/kg/day (5X MRHD based on AUC comparisons). No effect on fertility in male rats was noted at 2 mg/kg/day (0.7X MRHD based on AUC comparisons).
-
14 CLINICAL STUDIES
Three randomized, double-blind, vehicle-controlled, multi-center, Phase 3 trials were conducted in 589 pediatric subjects ages 3 months-17 years old to evaluate pimecrolimus cream, 1% for the treatment of mild to moderate atopic dermatitis. Two of the three trials support the use of pimecrolimus cream, 1% in subjects 2 years and older with mild to moderate atopic dermatitis [see Warnings and Precautions (5.1)]. Three other trials in 1,619 pediatric and adult subjects provided additional data regarding the safety of pimecrolimus cream, 1% in the treatment of atopic dermatitis. Two of these other trials were vehicle-controlled with optional sequential use of a medium potency topical corticosteroid in pediatric subjects and one trial was an active comparator trial in adult subjects with atopic dermatitis [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
Two identical 6-week, randomized, vehicle-controlled, multi-center, Phase 3 trials were conducted to evaluate pimecrolimus cream, 1% for the treatment of mild to moderate atopic dermatitis. A total of 403 pediatric subjects 2 to 17 years old were included in the trials. The male/female ratio was approximately 50% and 29% of the subjects were African American. At trial entry, 59% of subjects had moderate disease and the mean body surface area (BSA) affected was 26%. About 75% of subjects had atopic dermatitis affecting the face and/or neck region. In these trials, subjects applied either pimecrolimus cream, 1% or vehicle cream twice daily to 5% to 96% of their BSA for up to 6 weeks. At endpoint, based on the physician’s global evaluation of clinical response, 35% of subjects treated with pimecrolimus cream, 1% were clear or almost clear of signs of atopic dermatitis compared to only 18% of vehicle-treated subjects. More pimecrolimus subjects (57%) had mild or no pruritus at 6 weeks compared to vehicle subjects (34%). The improvement in pruritus occurred in conjunction with the improvement of the subjects’ atopic dermatitis.
In these two 6-week trials of pimecrolimus, the combined efficacy results at endpoint are presented in Table 2 as follows:
Table 2. Combined Efficacy Results at Endpoint for Two 6-week Trials of Pimecrolimus Cream % Subjects
Pimecrolimus (N= 267) Vehicle (N= 136) Global Assessment Clear 28 (10%) 5 (4%) Clear or Almost Clear 93 (35%) 25 (18%) Clear to Mild Disease 180 (67%) 55 (40%) In the two pediatric trials that independently support the use of pimecrolimus cream, 1% in mild to moderate atopic dermatitis, a significant treatment effect was seen by day 15. Of the key signs of atopic dermatitis, erythema, infiltration/papulation, lichenification, and excoriations were reduced at day 8 when compared to vehicle.
Figure 1 depicts the time course of improvement in the percent body surface area affected as a result of treatment with pimecrolimus cream, 1% in 2 to 17 year olds.
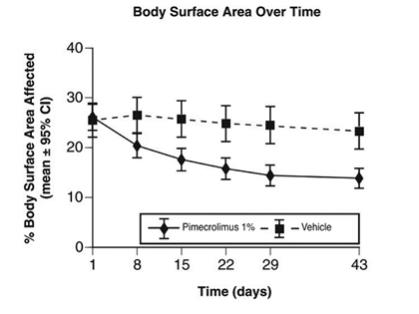
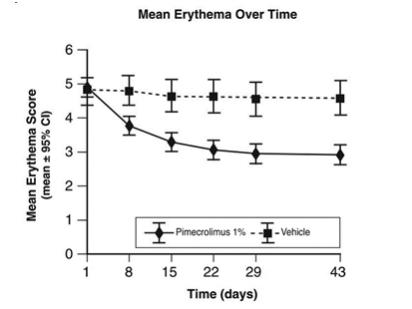
Figure 2 shows the time course of improvement in erythema as a result of treatment with pimecrolimus cream, 1% in 2 to 17 year olds.
-
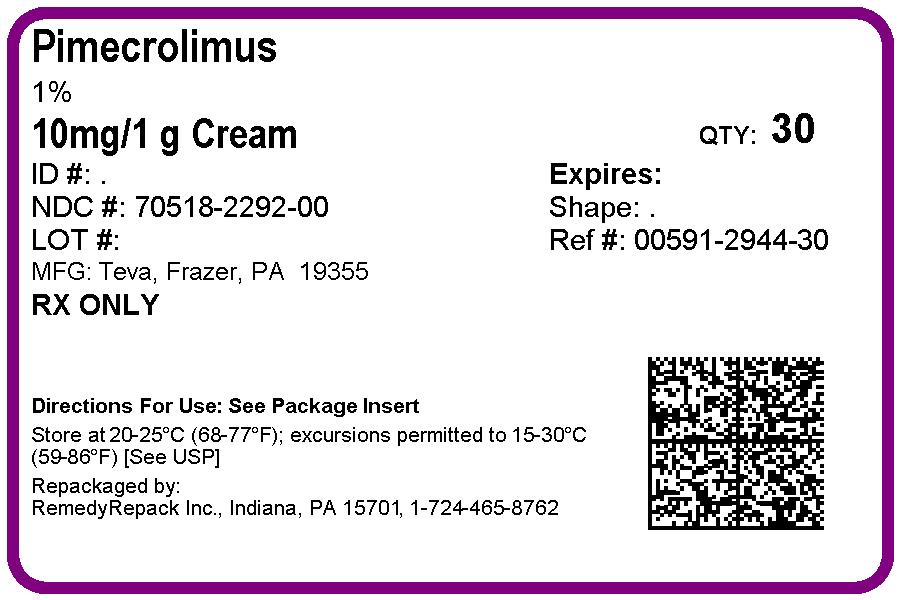
16 HOW SUPPLIED/STORAGE AND HANDLING
Pimecrolimus cream, 1% is a whitish cream available in tubes of 30 grams, 60 grams, and 100 grams.
30 gram tube………………………………………………………………NDC: 0591-2944-30
60 gram tube………………………………………………………………NDC: 0591-2944-60
100 gram tube……………………………………………………………..NDC: 0591-2944-87
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Do not freeze.
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling ( Medication Guide)
Patients using pimecrolimus cream, 1% should receive the following information and instructions:
-
Pimecrolimus cream, 1% may cause serious side effects. It is not known if pimecrolimus cream, 1% is safe to use for a long period of time. A very small number of people who have used pimecrolimus cream, 1% have had cancer (for example, skin or lymphoma). However, a link with pimecrolimus cream, 1% use has not been shown. Because of this concern:
- A patient should not use pimecrolimus cream, 1% continuously for a long time.
- Pimecrolimus cream, 1% should be used only on areas of skin that have eczema.
- Pimecrolimus cream, 1% is not for use on a child under 2 years old.
- A patient should not use sun lamps, tanning beds, or get treatment with ultraviolet light therapy during treatment with pimecrolimus cream, 1%.
- A patient should limit sun exposure during treatment with pimecrolimus cream, 1% even when the medicine is not on the skin. If a patient needs to be outdoors after applying pimecrolimus cream, 1%, the patient should wear loose fitting clothing that protects the treated area from the sun. The physician should advise the patient about other types of protection from the sun.
- A patient should not cover the skin being treated with bandages, dressings or wraps. A patient can wear normal clothing.
- Pimecrolimus cream, 1% is for use on the skin only. Do not get pimecrolimus cream, 1% in your eyes, nose, mouth, vagina, or rectum (mucous membranes). If you get pimecrolimus cream, 1% in any of these areas, burning or irritation can happen. Wipe off any pimecrolimus cream, 1% from the affected area and then rinse the area well with cold water. Pimecrolimus cream, 1% is for external use only.
- A patient should use pimecrolimus cream, 1% for short periods, and if needed, treatment may be repeated with breaks in between.
- Wash hands before using pimecrolimus cream, 1%. When applying pimecrolimus cream, 1% after a bath or shower, the skin should be dry.
- Apply a thin layer of pimecrolimus cream, 1% only to the affected skin areas, twice a day, as directed by the physician.
- Use the smallest amount of pimecrolimus cream, 1% needed to control the signs and symptoms of eczema.
- A patient should not bathe, shower or swim right after applying pimecrolimus cream, 1%. This could wash off the cream.
- A patient can use moisturizers with pimecrolimus cream, 1%. They should be sure to check with the physician first about the products that are right for them. Because the skin of patients with eczema can be very dry, it is important they keep up good skin care practices. If a patient uses moisturizers, he or she should apply them after pimecrolimus cream, 1%.
Teva Pharmaceuticals USA, Inc.
North Wales, PA 19454Iss. 5/2018
-
Pimecrolimus cream, 1% may cause serious side effects. It is not known if pimecrolimus cream, 1% is safe to use for a long period of time. A very small number of people who have used pimecrolimus cream, 1% have had cancer (for example, skin or lymphoma). However, a link with pimecrolimus cream, 1% use has not been shown. Because of this concern:
-
MEDICATION GUIDE
MEDICATION GUIDE
Pimecrolimus (pimʺ e kroeʹ li mus) Cream, 1%Important: Pimecrolimus cream, 1% is for use on the skin only (topical). Do not get pimecrolimus cream, 1% in your eyes, nose, mouth, vagina, or rectum.
What is the most important information I should know about pimecrolimus cream, 1%?
It is not known if pimecrolimus cream, 1% is safe to use for a long period of time. A very small number of people who have used pimecrolimus cream, 1% have developed cancer (for example, skin cancer or lymphoma). But a link that pimecrolimus cream, 1% use caused these cancers has not been shown. Because of this concern:
- Do not use pimecrolimus cream, 1% continuously for a long time.
- Use pimecrolimus cream, 1% only on areas of your skin that have eczema.
- Do not use pimecrolimus cream, 1% on a child under 2 years of age.
What is pimecrolimus cream, 1%?
Pimecrolimus cream, 1% is a prescription medicine used on the skin (topical) to treat mild to moderate eczema (atopic dermatitis). Pimecrolimus cream, 1% is for adults and children age 2 years and older who do not have a weakened immune system. Pimecrolimus cream, 1% is used on the skin for short periods, and if needed, treatment may be repeated with breaks in between. Pimecrolimus cream, 1% is for use after other prescription medicines have not worked for you or if your doctor recommends that other prescription medicines should not be used.
It is not known if pimecrolimus cream, 1% is safe and effective in people who have a weakened immune system.
Pimecrolimus cream, 1% is not for use in children under 2 years of age.
Who should not use pimecrolimus cream, 1%?
Do not use pimecrolimus cream, 1% if you are allergic to pimecrolimus or any of the ingredients in pimecrolimus cream, 1%. See the end of this Medication Guide for a complete list of ingredients in pimecrolimus cream, 1%.
What should I tell my doctor before using pimecrolimus cream, 1%?
Before using pimecrolimus cream, 1%, tell your doctor about all of your medical conditions, including if you:
- have a skin disease called Netherton’s syndrome (a rare inherited condition)
- have any infection on your skin including chicken pox or herpes
- have been told you have a weakened immune system
- are pregnant or plan to become pregnant. It is not known if pimecrolimus cream, 1% will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if pimecrolimus, 1% passes into your breast milk. You and your doctor should decide if you will use pimecrolimus cream, 1% or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Tell your doctor about all the skin medicines and products you use.
Know the medicines you take. Keep a list of them with you to show your doctor and pharmacist each time you get a new medicine.
How should I use pimecrolimus cream, 1%?
- Use pimecrolimus cream, 1% exactly as your doctor tells you to use it.
- Stop pimecrolimus cream, 1% when the signs and symptoms of eczema, such as itching, rash, and redness go away, or as directed by your doctor.
- Wash your hands before using pimecrolimus cream, 1%. If you apply pimecrolimus cream, 1% after a bath or shower, make sure your skin is dry.
- Apply a thin layer of pimecrolimus cream, 1% only to the affected skin areas, two times each day, as directed by your doctor.
- Use the smallest amount of pimecrolimus cream, 1% to help control the signs and symptoms of eczema.
- If you apply pimecrolimus cream, 1% to another person, or if you have eczema and are not treating your hands, it is important for you to wash your hands with soap and water after applying pimecrolimus cream, 1%. This should remove any cream left on your hands.
- Do not bathe, shower or swim right after applying pimecrolimus cream, 1%. This could wash off the cream.
- You can use moisturizers with pimecrolimus cream, 1%. Ask your doctor first about the products that are right for you. People with eczema can have very dry skin, so it is important to keep up good skin care practices. If you use moisturizers, apply them after pimecrolimus cream, 1%.
- Call your doctor if your symptoms get worse with pimecrolimus cream, 1% or your symptoms do not improve after 6 weeks of treatment.
What should I avoid while using pimecrolimus cream, 1%?
- You should not use sun lamps, tanning beds, or get treatment with ultraviolet light therapy during treatment with pimecrolimus cream, 1%.
- Limit your time in the sun during treatment with pimecrolimus cream, 1% even when the medicine is not on your skin. If you need to be outdoors after applying pimecrolimus cream, 1%, wear loose fitting clothing that protects the treated area from the sun. Ask your doctor what other types of protection from the sun you should use. It is not known how pimecrolimus cream, 1% may affect your skin with exposure to ultraviolet light.
- Do not cover the skin being treated with bandages, dressings or wraps. You can wear normal clothing.
- Pimecrolimus cream, 1% is for use on the skin only. Do not get pimecrolimus cream, 1% in your eyes, nose, mouth, vagina, or rectum (mucous membranes). If you get pimecrolimus cream, 1% in any of these areas, burning or irritation can happen. Wipe off any pimecrolimus cream, 1% from the affected area and then rinse the area well with cold water.
- Do not swallow pimecrolimus cream, 1%. If you do, call your doctor.
- Avoid using pimecrolimus cream, 1% on skin areas that have cancers or pre-cancers.
What are the possible side effects of pimecrolimus cream, 1%?
Pimecrolimus cream, 1% may cause serious side effects.
- See “What is the most important information I should know about pimecrolimus cream, 1%?”
- The most common side effect at the skin application site is burning or a feeling of warmth. These side effects are usually mild or moderate, happen during the first few days of treatment, and usually clear up in a few days.
Other common side effects include:
- headache
- common cold or stuffy nose, sore throat
- cough
- flu (influenza)
- fever
- viral infection. Some people may get viral skin infections (like cold sores, chicken pox, shingles, or warts) or swollen lymph nodes (glands).
Tell your doctor if you get a skin infection or if you have any side effect (for example, swollen glands) that bothers you or that does not go away.
These are not all the possible side effects with pimecrolimus cream, 1%. Ask your doctor or pharmacist for more information.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store pimecrolimus cream, 1%?
- Store pimecrolimus cream, 1% at room temperature between 68° to 77°F (20° to 25°C).
- Do not freeze pimecrolimus cream, 1%.
Keep pimecrolimus cream, 1% and all medicines out of the reach of children.
General information about the safe and effective use of pimecrolimus cream, 1%
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use pimecrolimus cream, 1% for conditions other than which it was prescribed. Do not give pimecrolimus cream, 1% to other people even if they have the same symptoms you have. It may harm them.
You can ask your doctor or pharmacist for information about pimecrolimus cream, 1% that is written for health professionals.
For more information call Teva Pharmaceuticals USA, Inc. at 1-888-838-2872.
What are the ingredients in pimecrolimus cream, 1%?
Active ingredient: pimecrolimus
Inactive ingredients: benzyl alcohol, cetyl alcohol, cetostearyl alcohol (type A), citric acid anhydrous, medium-chain triglycerides, mono- and di-glycerides, oleyl alcohol, propylene glycol, sodium hydroxide, stearyl alcohol, and water.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Teva Pharmaceuticals USA, Inc.
North Wales, PA 19454Iss. 5/2018
- Do not use pimecrolimus cream, 1% continuously for a long time.
-
PRINCIPAL DISPLAY PANEL
DRUG: pimecrolimus
GENERIC: pimecrolimus
DOSAGE: CREAM
ADMINSTRATION: TOPICAL
NDC: 70518-2292-0
COLOR: white
PACKAGING: 30 g in 1 TUBE
ACTIVE INGREDIENT(S):
- PIMECROLIMUS 10mg in 1g
INACTIVE INGREDIENT(S):
- BENZYL ALCOHOL
- PROPYLENE GLYCOL
- OLEYL ALCOHOL
- SODIUM HYDROXIDE
- STEARYL ALCOHOL
- CETOSTEARYL ALCOHOL
- CETYL ALCOHOL
- MEDIUM-CHAIN TRIGLYCERIDES
- ANHYDROUS CITRIC ACID
- WATER
-
INGREDIENTS AND APPEARANCE
PIMECROLIMUS
pimecrolimus creamProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70518-2292(NDC:0591-2944) Route of Administration TOPICAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PIMECROLIMUS (UNII: 7KYV510875) (PIMECROLIMUS - UNII:7KYV510875) PIMECROLIMUS 10 mg in 1 g Inactive Ingredients Ingredient Name Strength BENZYL ALCOHOL (UNII: LKG8494WBH) CETYL ALCOHOL (UNII: 936JST6JCN) CETOSTEARYL ALCOHOL (UNII: 2DMT128M1S) ANHYDROUS CITRIC ACID (UNII: XF417D3PSL) MEDIUM-CHAIN TRIGLYCERIDES (UNII: C9H2L21V7U) OLEYL ALCOHOL (UNII: 172F2WN8DV) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM HYDROXIDE (UNII: 55X04QC32I) STEARYL ALCOHOL (UNII: 2KR89I4H1Y) WATER (UNII: 059QF0KO0R) Product Characteristics Color white Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70518-2292-0 30 g in 1 TUBE; Type 0: Not a Combination Product 09/03/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA209345 09/03/2019 Labeler - REMEDYREPACK INC. (829572556)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.