LABETALOL HYDROCHLORIDE tablet, film coated
Labetalol Hydrochloride by
Drug Labeling and Warnings
Labetalol Hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Innogenix, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LABETALOL HYDROCHLORIDE TABLETS safely and effectively. See full prescribing information for LABETALOL HYDROCHLORIDE TABLETS.
LABETALOL HYDROCHLORIDE tablets, for oral use.
Initial U.S. Approval: 1984INDICATIONS AND USAGE
Labetalol Hydrochloride Tablets are a beta adrenergic blocker indicated for the treatment of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. ( 1)
DOSAGE AND ADMINISTRATION
- The recommended initial dosage is 100 mg twice daily, alone or added to a diuretic regimen. Titrate in increments of 100 mg twice daily every 2 or 3 days. Maintenance dosage is between 200 and 400 mg twice daily. ( 2.1)
- Severe Hypertension: May require from 1,200 to 2,400mg per day, with or without thiazide diuretics. Titrate in increments not to exceed 200 mg twice daily. ( 2.2)
- Elderly patients: Initiate at 100 mg twice daily. Titrate in increments of 100 mg twice daily as required for blood pressure control. Many elderly patients will require between 100 and 200 mg twice daily. ( 2.3)
DOSAGE FORMS AND STRENGTHS
Tablets: 100 mg, 200 mg, and 300 mg tablets ( 3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Monitor patients for symptomatic postural hypotension and syncope after initial dosing or dose increments. ( 5.1)
- Monitor heart rate and rhythm for bradycardia, including sinus pause, heart block, severe bradycardia, and cardiac arrest in patients receiving Labetalol Hydrochloride Tablets. ( 5.2)
- Beta-blockade can depress myocardial contractility and precipitating more severe failure. Avoid use in patients with overt heart failure. ( 5.3).
- Monitor heart rate and rhythm for bradycardia, including sinus pause, heart block, severe bradycardia, and cardiac arrest in patients receiving Labetalol Hydrochloride Tablets. ( 5.2)
- Beta-blockade can depress myocardial contractility and precipitating more severe failure. Avoid use in patients with overt heart failure. ( 5.3)
- Acute exacerbation of coronary artery disease upon cessation of therapy. Do not abruptly discontinue. ( 5.4)
- Avoid use in patients with bronchospastic disease. ( 5.5)
- Beta‑adrenergic blockade may prevent the appearance of premonitory signs and symptoms (e.g., tachycardia) of acute hypoglycemia. ( 5.6)
- Exacerbation of pheochromocytoma: Paradoxical increases in blood pressure may occur. ( 5.7)
- Hepatic necrosis and death have been reported. If the patient develops signs or symptoms of liver injury, institute appropriate treatment and investigate the probable cause. ( 5.8)
- Do not routinely withdraw chronic beta blocker therapy prior to surgery. ( 5.10)
ADVERSE REACTIONS
Most commonly observed adverse reactions: fatigue, nausea, dizziness ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Innogenix, LLC at 1-844-466-6469 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Revised: 12/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypotension
5.2 Bradycardia
5.3 Cardiac Failure
5.4 Ischemic Heart Disease
5.5 Reactive Airway Disease and Nonallergic Bronchospasm
5.6 Hypoglycemia
5.7 Use in Patients with Pheochromocytoma
5.8 Hepatic Injury
5.9 Use in Patients at Risk of Severe Acute Hypersensitivity Reactions
5.10 Major Surgery
5.11 Intraoperative Floppy Iris Syndrome (IFIS)
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
7 DRUG INTERACTIONS
7.1 Negative Chronotopes
7.2 Bronchodilators
7.3 Anesthesia
7.4 Nitroglycerin
7.5 Drug/Laboratory Test Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics and Metabolism
13 NONCLINICAL TOXICOLOGY
16 HOW SUPPLIED/STORAGE AND HANDLING
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
Labetalol Hydrochloride is indicated in the management of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes including beta adrenergic blockers.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than one drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality also have been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Labetalol Hydrochloride Tablets may be used alone or in combination with other antihypertensive agents, especially thiazide and loop diuretics.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
Labetalol Hydrochloride dosage must be individualized.
The recommended initial dosage of labetalol hydrochloride is 100 mg twice daily. Adjust dosage in increments of 100 mg twice daily at 2- to 3-day intervals based on response. The recommended maintenance dosage of labetalol hydrochloride is between 200 and 400 mg twice daily.
-
3 DOSAGE FORMS AND STRENGTHS
Labetalol Hydrochloride Tablets are available in the following strengths:
- 100 mg - Round, beige, film-coated tablets, plain on one side, scored and debossed with “I/126” on the other side.
- 200 mg - Round, white, film-coated tablets, plain on one side, scored and debossed with “I/127” on the other side.
- 300 mg - Round, blue, film-coated tablets, plain on one side and debossed with “I/130” on the other side.
-
4 CONTRAINDICATIONS
Labetalol Hydrochloride Tablets are contraindicated in patients with:
- bronchial asthma or obstructive airway disease
- decompensated heart failure
- greater than first degree heart block
- cardiogenic shock
- severe bradycardia
- Hypersensitivity reactions, including anaphylaxis, to labetalol
- non-dihydropyridine calcium-channel antagonists
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypotension
Monitor patients for symptomatic postural hypotension and syncope after initial dosing or dose increments with Labetalol Hydrochloride Tablets. Elderly patients are generally more likely than younger patients to experience orthostatic symptoms [see Dosage and Administration (2.1), Use in Specific Populations (8.5), Clinical Pharmacology (12.2)].
5.2 Bradycardia
Bradycardia, including sinus pause, heart block, severe bradycardia, and cardiac arrest have occurred with the use of beta blockers. Monitor heart rate and rhythm in patients receiving Labetalol Hydrochloride Tablets.
5.3 Cardiac Failure
Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure. Beta‑blockade carries a potential hazard of further depressing myocardial contractility and precipitating more severe failure. Avoid Labetalol Hydrochloride Tablets in patients with overt congestive heart failure. If patients develop signs or symptoms of heart failure during administration, discontinue Labetalol Hydrochloride Tablets and treat appropriately.
5.4 Ischemic Heart Disease
Abrupt cessation of therapy with beta blocking agents in patients with coronary artery disease can cause exacerbations of angina pectoris and, in some cases, myocardial infarction has been reported. Therefore, even in the absence of overt angina pectoris, after the discontinuation of Labetalol Hydrochloride Tablets observe patients for development or worsening of angina. If patient experiences angina or angina markedly worsens or if acute coronary insufficiency develops, promptly reinstitute Labetalol Hydrochloride Tablets and manage as unstable angina.
5.5 Reactive Airway Disease and Nonallergic Bronchospasm
Avoid use in patients with reactive airways disease. If Labetalol Hydrochloride Tablets are used, use the smallest effective dose, to minimize inhibition of endogenous or exogenous beta agonists.
5.6 Hypoglycemia
Beta-blockers may prevent early warning signs of hypoglycemia, such as tachycardia, and increase the risk for severe or prolonged hypoglycemia at any time during treatment, especially in patients with diabetes mellitus or children and patients who are fasting (i.e., surgery, not eating regularly, or are vomiting). If severe hypoglycemia occurs, patients should be instructed to seek emergency treatment.
5.7 Use in Patients with Pheochromocytoma
Labetalol hydrochloride has been shown to be effective in lowering blood pressure and relieving symptoms in patients with pheochromocytoma; higher than usual doses may be required. However, paradoxical hypertensive responses have been reported in a few patients with this tumor; therefore, blood pressure when administering labetalol hydrochloride to patients with pheochromocytoma.
5.8 Hepatic Injury
Severe hepatocellular injury occurs rarely with labetalol therapy. The hepatic injury is usually reversible, but hepatic necrosis and death have been reported. If the patient develops signs or symptoms of liver injury, institute appropriate treatment and investigate the probable cause. Do not restart labetalol in patients without another explanation for the observed liver injury.
5.9 Use in Patients at Risk of Severe Acute Hypersensitivity Reactions
Patients at risk of anaphylactic reactions may be more reactive to allergen exposure (accidental, diagnostic, or therapeutic). Patients using beta-blockers may be unresponsive to the usual doses of epinephrine used to treat anaphylactic or anaphylactoid reactions. Avoid Labetalol Hydrochloride Tablets in patients at high risk of anaphylactic reactions.
5.10 Major Surgery
Do not routinely withdraw chronic beta blocker therapy prior to surgery. The effect of labetalol’s alpha adrenergic activity has not been evaluated in this setting.
A synergism between labetalol hydrochloride and halothane anesthesia has been shown [ see Drug Interactions (7.3)].
5.11 Intraoperative Floppy Iris Syndrome (IFIS)
IFIS has been observed during cataract surgery in some patients treated with alpha-1 blockers (labetalol is an alpha/beta blocker). This variant of small pupil syndrome is characterized by the combination of a flaccid iris that billows in response to intraoperative irrigation currents, progressive intraoperative miosis despite preoperative dilation with standard mydriatic drugs, and potential prolapse of the iris toward the phacoemulsification incisions. Inform the patient’s ophthalmologist to be prepared for possible modifications to the surgical technique, such as the utilization of iris hooks, iris dilator rings, or viscoelastic substances.
-
6 ADVERSE REACTIONS
- Hypotension [see Warnings and Precautions (5.1)
- Bradycardia [see Warnings and Precautions (5.2)]
- Cardiac failure [see Warnings and Precautions (5.3)]
- Ischemic heart disease [see Warnings and Precautions (5.4)]
- Nonallergic bronchospasm [see Warnings and Precautions (5.5))]
- Use in patients with pheochromocytoma [see Warnings and Precautions (5.7)]
- Hepatic injury [see Warnings and Precautions (5.8)]
- Risk of severe acute hypersensitivity reaction [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Adverse Reactions Resulting in Discontinuation of Treatment
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In controlled clinical trials of 3 to 4 months' duration, discontinuation of Labetalol Hydrochloride Tablets due to one or more adverse effects was required in 7% of all patients.
The incidence rates of adverse reactions listed in Table 1 were derived from multicenter, controlled clinical trials comparing labetalol hydrochloride and placebo over treatment periods of 3 and 4 months.
Table 1: Adverse Reactions Occurring in at Least 2% of Patients and More Frequent on Labetalol
Labetalol HCl
(n=227)Placebo
(n=98)Body as a whole
Fatigue
5%
0%
Headache
2%
1%
Gastrointestinal
Nausea
6%
1%
Dyspepsia
3%
1%
Central and Peripheral Nervous Systems
Dizziness
11%
3%
Autonomic Nervous System
Nasal stuffiness
3%
0%
Respiratory
Dyspnea
2%
0%
Special Senses
Vertigo
2%
1%
The adverse effects were reported spontaneously and are representative of the incidence of adverse effects that may be observed in a properly selected hypertensive patient population, i.e., a group excluding patients with bronchospastic disease, overt congestive heart failure, or other contraindications to beta‑blocker therapy.
Clinical trials also included studies utilizing daily doses up to 2,400 mg in more severely hypertensive patients. Certain of the side effects increased with increasing dose, as shown in Table 2 that depicts the entire US therapeutic trials data base for adverse reactions that are clearly or possibly dose related.
-
7 DRUG INTERACTIONS
7.1 Negative Chronotopes
Digitalis glycosides, diltiazem, verapamil, and beta-blockers slow atrioventricular conduction and decrease heart rate. Concomitant use with negative chronotropes can increase the risk of bradycardia or hypotension [see Warnings and Precautions (5.2)]. Coadministration of labetalol HCl with non-dihydropyridine calcium-channel antagonists (e.g., verapamil) is contraindicated [see Contraindications (4)].
7.2 Bronchodilators
Labetalol HCl antagonizes the bronchodilatory effect of beta-receptor agonist drugs; therefore, labetalol HCl is contraindicated in patients with bronchial asthma [see Contraindications (4)].
7.3 Anesthesia
Synergism has been shown between halothane anesthesia and intravenously administered labetalol. During controlled hypotensive anesthesia using labetalol in association with halothane, high concentrations (3% or above) of halothane should not be used because the degree of hypotension will be increased and because of the possibility of a large reduction in cardiac output and an increase in central venous pressure.
7.4 Nitroglycerin
Coadministration of labetalol HCl and nitroglycerine will have an additive effect in lowering blood pressure. Additionally, labetalol HCl blunts the reflex tachycardia produced by nitroglycerin. If labetalol HCl is used in patients with angina pectoris on nitroglycerin, monitor patients’ blood pressure and adjust labetalol dose as needed. In these patients, avoid initiating Labetalol Hydrochloride Tablets.
7.5 Drug/Laboratory Test Interactions
The presence of labetalol metabolites in the urine may result in falsely elevated levels of urinary catecholamines, metanephrine, normetanephrine, and vanillylmandelic acid (VMA) when measured by fluorimetric or photometric methods. In screening patients suspected of having a pheochromocytoma and being treated with labetalol, a specific method, such as a high-performance liquid chromatographic assay with solid phase extraction should be employed in determining levels of catecholamines.
Labetalol has also been reported to produce a false positive test for amphetamine when screening urine for the presence of drugs using the commercially available assay methods. When patients being treated with labetalol have a positive urine test for amphetamine using these techniques, confirm using more specific methods, such as a gas chromatographic mass spectrometer technique.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
The extensive experience with use of labetalol in pregnant women, based on published interventional and observational studies, has not identified a drug-associated risk for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data). Untreated hypertension during pregnancy can lead to serious adverse outcomes for the mother and the fetus (see Clinical Considerations). In animal reproductive studies, oral administration of labetalol to pregnant rats and rabbits during organogenesis at doses up to approximately six and four times the maximum recommended human dose (MRHD), respectively, resulted in no fetal malformations; however, increased fetal resorptions were seen in both species at doses approximating the MRHD (see Data).
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Consideration
Disease-Associated Maternal and/or Embryo/Fetal Risk
Hypertension in pregnancy increase the maternal risk for pre-eclampsia, gestational diabetes, premature delivery, and delivery complications (e.g., need for cesarean section, and post-partum hemorrhage). Hypertension increases the fetal risk for intrauterine growth restriction and intrauterine death. Pregnant women with hypertension should be carefully monitored and managed accordingly.
Fetal/Neonatal Adverse Reactions
Labetalol crosses the placenta. Newonates born to mothers who are receiving labetalol during pregnancy, may be at risk for hypotension, bradycardia, hypoglycemia, and respiratory depression. Neonates should be monitored for symptoms of hypotension, bradycardia, hypoglycemia and respiratly depression and mange accordingly.
Data
Human Data
Data from published interventional and observational studies did not demonstrate an association between major congenital malformations and the use of labetalol in pregnancy, however, most studies reported the maternal use of intravenous labetalol occurring after 20 weeks gestation. The published literature has reported inconsistent findings of intrauterine growth retardation, preterm birth and perinatal mortality with maternal use of labetalol during pregnancy; however, these studies have methodological limitations hindering interpretation. These studies cannot definitively establish the absence of risk during pregnancy.
Animal Data
Teratogenic studies were performed with labetalol in rats and rabbits at oral doses up to approximately six and four times the maximum recommended human dose (MRHD), respectively. No
reproducible evidence of fetal malformations was observed. Increased fetal resorptions were seen in both species at doses approximating the MRHD.
A teratology study performed with labetalol in rabbits at intravenous doses up to 1.7 times the MRHD revealed no evidence of drug-related harm to the fetus.
Oral administration of labetalol to rats during late gestation through weaning at doses of two to four times the MRHD caused a decrease in neonatal survival.
8.2 Lactation
Risk Summary
Available published data report the presence of labetalol in human milk at low levels. There are no data on the effects on the breastfed infant and on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for labetalol and any potential adverse effects on the breastfed infant from labetalol or from the underlying maternal condition.
8.5 Geriatric Use
Pharmacokinetic studies indicate that the elimination of labetalol is reduced in elderly patients. Although elderly patients may initiate therapy at the currently recommended dosage of 100 mg twice daily, elderly patients will generally require lower maintenance dosages than nonelderly patients.
-
10 OVERDOSAGE
Overdosage with labetalol hydrochloride causes excessive hypotension that is posture sensitive and, sometimes, excessive bradycardia. Patients should be placed supine and their legs raised if necessary to improve the blood supply to the brain. Treat symptoms of overdose with standard supportive care. If overdosage with labetalol hydrochloride follows oral ingestion, gastric lavage or pharmacologically induced emesis (using syrup of ipecac) may be useful for removal of the drug shortly after ingestion. Treat symptoms of overdose with standard supportive care.
Neither hemodialysis nor peritoneal dialysis removes a significant amount of labetalol hydrochloride from the general circulation (<1%).
The oral LD50 value of labetalol hydrochloride in the mouse is approximately 600 mg/kg and in the rat is >2 g/kg. The IV LD50in these species is 50 mg/kg to 60 mg/kg.
-
11 DESCRIPTION
Labetalol hydrochloride tablets, USP are an adrenergic receptor blocking agent that has both selective alpha 1-adrenergic and nonselective beta-adrenergic receptor blocking actions in a single substance.
Labetalol hydrochloride, USP is a racemate, chemically designated as 2-hydroxy-5-[1-hydroxy-2-[(1-methyl-3-phenylpropyl)amino]ethyl] benzamide monohydrochloride, and it has the following structure:
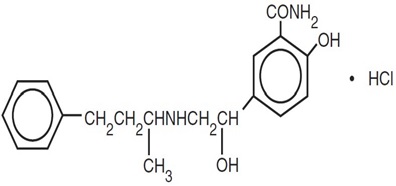
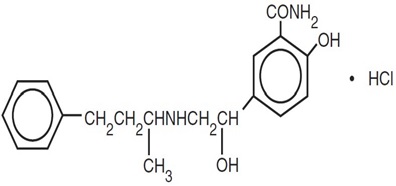
Labetalol hydrochloride, USP has the molecular formula C 19H 24N 2O 3HCl and a molecular weight of 364.87. It has two asymmetric centers and therefore exists as a molecular complex of two diastereoisomeric pairs. Dilevalol, the R,R’ stereoisomer, makes up 25% of racemic labetalol.
Labetalol hydrochloride, USP is a white or off-white crystalline powder, soluble in water.
Labetalol hydrochloride tablets, USP, for oral administration, contain 100 mg, 200 mg or 300 mg labetalol hydrochloride, USP.
In addition, each 100 mg tablet contains the following inactive ingredients: anhydrous lactose, carnauba wax, hypromellose, magnesium stearate, polyethylene glycol, polysorbate 80, pregelatinized starch (corn), red iron oxide, titanium dioxide and yellow iron oxide.
In addition, each 200 mg tablet contains the following inactive ingredients: anhydrous lactose, carnauba wax, hypromellose, magnesium stearate, polydextrose, polyethylene glycol, pregelatinized starch (corn), titanium dioxide and triacetin.
In addition, each 300 mg tablet contains the following inactive ingredients: anhydrous lactose, carnauba wax, FD&C Blue #2, hypromellose, magnesium stearate, polyethylene glycol, polysorbate 80, pregelatinized starch (corn), titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Labetalol hydrochloride combines both selective, competitive, alpha1‑adrenergic blocking and nonselective, competitive, beta‑adrenergic blocking activity. The ratios of alpha- to beta‑blockade have been estimated to be approximately 1:3 and 1:7 following oral and intravenous (IV) administration, respectively.
12.2 Pharmacodynamics
The capacity of labetalol hydrochloride to block alpha receptors in man has been demonstrated by attenuation of the pressor effect of phenylephrine and by a significant reduction of the pressor response caused by immersing the hand in ice cold water ("cold pressor test"). Labetalol hydrochloride's beta1 receptor blockade in man was demonstrated by a small decrease in the resting heart rate, attenuation of tachycardia produced by isoproterenol or exercise, and by attenuation of the reflex tachycardia to the hypotension produced by amyl nitrite. Beta2 receptor blockade was demonstrated by inhibition of the isoproterenol induced fall in diastolic blood pressure. Both the alpha- and beta blocking actions of orally administered labetalol hydrochloride contribute to a decrease in blood pressure in hypertensive patients. Labetalol hydrochloride consistently, in dose related fashion, blunted increases in exercise induced blood pressure and heart rate, and in their double product. The pulmonary circulation during exercise was not affected by labetalol hydrochloride dosing.
The effects on A‑V nodal refractoriness were inconsistent. Single oral doses of labetalol hydrochloride administered to patients with coronary artery disease had no significant effect on sinus rate, intraventricular conduction, or QRS duration. The atrioventricular (A‑V) conduction time was modestly prolonged in two of seven patients. In another study, IV labetalol hydrochloride slightly prolonged A‑V nodal conduction time and atrial effective refractory period with only small changes in heart rate.
Labetalol hydrochloride produces dose‑related falls in blood pressure without reflex tachycardia and without significant reduction in heart rate, presumably through a mixture of its alpha- and beta‑blocking effects. Hemodynamic effects are variable, with small, nonsignificant changes in cardiac output seen in some studies but not others, and small decreases in total peripheral resistance. Elevated plasma renins are reduced.Due to the alpha1‑receptor blocking activity of labetalol hydrochloride, blood pressure is lowered more in the standing than in the supine position, and symptoms of postural hypotension (2%), including rare instances of syncope, can occur. Following oral administration, when postural hypotension has occurred, it has been transient and is uncommon when the recommended starting dose and titration increments are closely followed [see Dosage and Administration (2.1)]. Symptomatic postural hypotension is most likely to occur 2 to 4 hours after a dose, especially following the use of large initial doses or upon large changes in dose.
The peak effects of single oral doses of labetalol hydrochloride occur within 2 to 4 hours. The duration of effect depends upon dose, lasting at least 8 hours following single oral doses of 100 mg and more than 12 hours following single oral doses of 300 mg. The maximum, steady‑state blood pressure response upon oral, twice‑a‑day dosing occurs within 24 to 72 hours.
The antihypertensive effect of labetalol has a linear correlation with the logarithm of labetalol plasma concentration, and there is also a linear correlation between the reduction in exercise induced tachycardia occurring at 2 hours after oral administration of labetalol hydrochloride and the logarithm of the plasma concentration.
About 70% of the maximum beta‑blocking effect is present for 5 hours after the administration of a single oral dose of 400 mg with suggestion that about 40% remains at 8 hours.
12.3 Pharmacokinetics and Metabolism
Absorption
Labetalol hydrochloride is absorbed with peak plasma levels occurring 1 to 2 hours after oral administration.
The relative bioavailability of Labetalol Hydrochloride Tablets compared to an oral solution is 100%.
The absolute bioavailability (fraction of drug reaching systemic circulation) of labetalol when compared to an IV infusion is 25%; this is due to extensive "first-pass" metabolism. There is a linear relationship between oral doses of 100 mg to 3,000 mg and peak plasma levels.
Effect of Food
The absolute bioavailability of labetalol is increased when administered with food.
Distribution
Labetalol has been shown to cross the placental barrier in humans. Labetalol is approximately 50% protein bound.
Elimination
The plasma half-life of labetalol following oral administration is about 6 to 8 hours. Steady-state plasma levels of labetalol are reached by about the third day of dosing.
Metabolism
Metabolism of labetalol is mainly through conjugation to glucuronide metabolites.
Excretion
Approximately 55% to 60% of a dose appears in the urine as conjugates or unchanged labetalol within the first 24 hours of dosing. These metabolites are present in plasma and are excreted in the urine and, via the bile, into the feces. Neither hemodialysis nor peritoneal dialysis removes a significant amount of labetalol hydrochloride from the general circulation (<1%).
Specific Populations
Patients with Renal or Hepatic Impairment
In patients with decreased hepatic or renal function, the elimination half‑life of labetalol is not altered; however, the relative bioavailability in hepatically impaired patients is increased due to decreased "first‑pass" metabolism.
Drug Interaction Studies
Tricyclic Antidepressants
In one survey, 2.3% of patients taking labetalol hydrochloride in combination with tricyclic antidepressants experienced tremor, as compared to 0.7% reported to occur with labetalol hydrochloride alone. The contribution of each of the treatments to this adverse reaction is unknown, but the possibility of a drug interaction cannot be excluded.
Cimetidine
Cimetidine has been shown to increase the bioavailability of labetalol hydrochloride. Since this could be explained either by enhanced absorption or by an alteration of hepatic metabolism of labetalol hydrochloride, special care should be used in establishing the dose required for blood pressure control in such patients.
-
13 NONCLINICAL TOXICOLOGY
Carcinogenesis
Long‑term oral dosing studies with labetalol hydrochloride for 18 months in mice and for 2 years in rats showed no evidence of carcinogenesis. Studies with labetalol hydrochloride using dominant lethal assays in rats and mice and exposing microorganisms according to modified Ames tests showed no evidence of mutagenesis.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
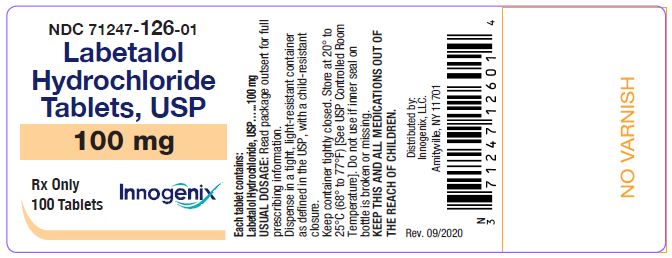
Labetalol Hydrochloride Tablets, USP 100 mg: Round, beige, film-coated tablets, plain on one side, scored and debossed with “I/126” on the other side.
NDC: 71247-126-01 bottles of 100
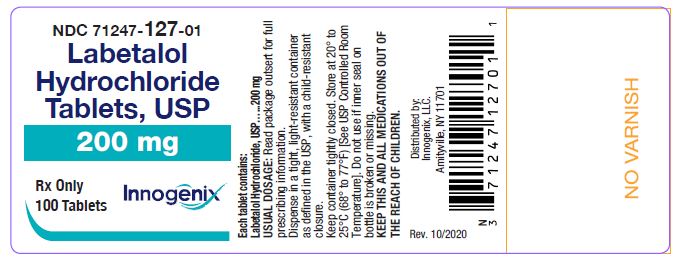
NDC: 71247-126-05 bottles of 500Labetalol Hydrochloride Tablets, USP 200 mg: Round, white, film-coated tablets, plain on one side, scored and debossed with “I/127” on the other side.
NDC: 71247-127-01 bottles of 100
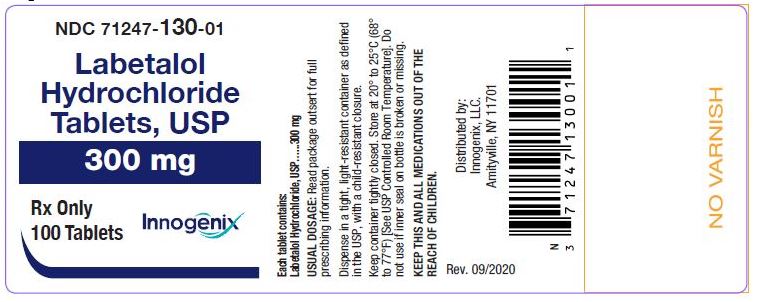
NDC: 71247-127-05 bottles of 500Labetalol Hydrochloride Tablets, USP 300 mg: Round, blue, film-coated tablets, plain on one side and debossed with “I/130” on the other side:
NDC: 71247-130-01 bottles of 100
NDC: 71247-130-05 bottles of 500Storage
Store Labetalol Hydrochloride Tablets at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].Dispense in a tight, light-resistant container as defined in the USP with a child-resistant closure as required.
To report SUSPECTED ADVERSE REACTIONS, contact Innogenix, LLC. at 1-844-466-6469 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Distributed by:
Innogenix, LLC.
Amityville, NY 11701Rev. 09/2025
-
17 PATIENT COUNSELING INFORMATION
- Advise patients to not interrupt or discontinue using Labetalol Hydrochloride Tablets without advice from their healthcare provider
- Advise patients to contact their healthcare provider about any signs or symptoms of impending cardiac failure or hepatic dysfunction [see Warnings and Precautions (5.3,5.8)]
- Inform patients or caregivers that there is a risk of hypoglycemia when Labetalol Hydrochloride Tablets is given to patients who are fasting or who are vomiting. Monitor for symptoms of hypoglycemia [ see Warnings and Precautions (5.6)].
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
LABETALOL HYDROCHLORIDE
labetalol hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71247-126 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LABETALOL HYDROCHLORIDE (UNII: 1GEV3BAW9J) (LABETALOL - UNII:R5H8897N95) LABETALOL HYDROCHLORIDE 100 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CARNAUBA WAX (UNII: R12CBM0EIZ) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) STARCH, CORN (UNII: O8232NY3SJ) FERRIC OXIDE RED (UNII: 1K09F3G675) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color brown (beige) Score 2 pieces Shape ROUND Size 8mm Flavor Imprint Code I;126 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71247-126-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/08/2021 2 NDC: 71247-126-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 02/08/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075215 02/08/2021 LABETALOL HYDROCHLORIDE
labetalol hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71247-127 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LABETALOL HYDROCHLORIDE (UNII: 1GEV3BAW9J) (LABETALOL - UNII:R5H8897N95) LABETALOL HYDROCHLORIDE 200 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CARNAUBA WAX (UNII: R12CBM0EIZ) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) STARCH, CORN (UNII: O8232NY3SJ) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) POLYDEXTROSE (UNII: VH2XOU12IE) TRIACETIN (UNII: XHX3C3X673) Product Characteristics Color white Score 2 pieces Shape ROUND Size 10mm Flavor Imprint Code I;127 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71247-127-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/08/2021 2 NDC: 71247-127-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 02/08/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075215 02/08/2021 LABETALOL HYDROCHLORIDE
labetalol hydrochloride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71247-130 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LABETALOL HYDROCHLORIDE (UNII: 1GEV3BAW9J) (LABETALOL - UNII:R5H8897N95) LABETALOL HYDROCHLORIDE 300 mg Inactive Ingredients Ingredient Name Strength ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) CARNAUBA WAX (UNII: R12CBM0EIZ) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) HYPROMELLOSES (UNII: 3NXW29V3WO) MAGNESIUM STEARATE (UNII: 70097M6I30) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYSORBATE 80 (UNII: 6OZP39ZG8H) STARCH, CORN (UNII: O8232NY3SJ) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color blue Score no score Shape ROUND Size 11mm Flavor Imprint Code I;130 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71247-130-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 02/08/2021 2 NDC: 71247-130-05 500 in 1 BOTTLE; Type 0: Not a Combination Product 02/08/2021 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA075215 02/08/2021 Labeler - Innogenix, Inc. (080501434)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.