RELPAX- eletriptan hydrobromide tablet, film coated
Relpax by
Drug Labeling and Warnings
Relpax by is a Prescription medication manufactured, distributed, or labeled by ROERIG. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use RELPAX safely and effectively. See full prescribing information for RELPAX.
RELPAX® (eletriptan hydrobromide) tablets, for oral use
Initial U.S. Approval: 2002INDICATIONS AND USAGE
RELPAX is a serotonin (5-HT1B/1D) receptor agonist (triptan) indicated for the acute treatment of migraine with or without aura in adults (1)
Limitations of Use:
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Tablets: 20 mg and 40 mg (3)
CONTRAINDICATIONS
- History of coronary artery disease (CAD) or coronary artery vasospasm (4)
- Wolff-Parkinson-White syndrome or other cardiac accessory conduction pathway disorders (4)
- History of stroke, transient ischemic attack, or history or current evidence of hemiplegic or basilar migraine (4)
- Peripheral vascular disease (4)
- Ischemic bowel disease (4)
- Uncontrolled hypertension (4)
- Within 24 hours of treatment with another 5-HT1 agonist, or an ergotamine-containing medication (4)
- Hypersensitivity to RELPAX (angioedema and anaphylaxis seen) (4)
- Within at least 72 hours of treatment with the following potent CYP3A4 inhibitors: ketoconazole, itraconazole, nefazodone, troleandomycin, clarithromycin, ritonavir, or nelfinavir (4)
WARNINGS AND PRECAUTIONS
- Myocardial ischemia/infarction or Prinzmetal's angina: Perform cardiac evaluation in patients with multiple cardiovascular risk factors (5.1)
- Arrhythmias: Discontinue RELPAX if occurs (5.2)
- Chest/throat/neck/jaw pain, tightness, pressure, or heaviness: Generally not myocardial ischemia; evaluate high risk patients for CAD (5.3)
- Cerebral hemorrhage, subarachnoid hemorrhage, or stroke: Discontinue RELPAX if occurs (5.4)
- Gastrointestinal ischemia or infarction events, or peripheral vasospastic reactions: Discontinue RELPAX if occurs (5.5)
- Medication overuse headache: Detoxification may be necessary (5.6)
- Serotonin syndrome: Discontinue RELPAX if occurs (5.7, 7.3)
ADVERSE REACTIONS
Most common adverse reactions (≥ 5% and > placebo) were asthenia, nausea, dizziness, and somnolence. These reactions appear to be dose-related. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 3/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Myocardial Ischemia, Myocardial Infarction, and Prinzmetal's Angina
5.2 Arrhythmias
5.3 Chest, Throat, Neck and/or Jaw Pain/Tightness/Pressure
5.4 Cerebrovascular Events
5.5 Other Vasospasm Reactions
5.6 Medication Overuse Headache
5.7 Serotonin Syndrome
5.8 Increase in Blood Pressure
5.9 Anaphylactic/Anaphylactoid Reactions
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Ergot-Containing Drugs Including Other 5-HT1B/1D Agonists
7.2 CYP3A4 Inhibitors
7.3 Selective Serotonin Reuptake Inhibitors/Serotonin and Norepinephrine Reuptake Inhibitors and Serotonin Syndrome
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
RELPAX is indicated for the acute treatment of migraine with or without aura in adults.
Limitations of Use:
- Use only if a clear diagnosis of migraine has been established. If a patient has no response to the first migraine attack treated with RELPAX, reconsider the diagnosis of migraine before RELPAX is administered to treat any subsequent attacks.
- RELPAX is not intended for the prevention of migraine attacks.
- Safety and effectiveness of RELPAX have not been established for cluster headache.
-
2 DOSAGE AND ADMINISTRATION
The maximum recommended single dose is 40 mg.
In controlled clinical trials, single doses of 20 mg and 40 mg were effective for the acute treatment of migraine in adults. A greater proportion of patients had a response following a 40 mg dose than following a 20 mg dose [see Clinical Studies (14)].
If the migraine has not resolved by 2 hours after taking RELPAX, or returns after transient improvement, a second dose may be administered at least 2 hours after the first dose. The maximum daily dose should not exceed 80 mg.
The safety of treating an average of more than 3 migraine attacks in a 30-day period has not been established.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
RELPAX is contraindicated in patients with:
- Ischemic coronary artery disease (CAD) (angina pectoris, history of myocardial infarction, or documented silent ischemia) or coronary artery vasospasm, including Prinzmetal's angina [see Warnings and Precautions (5.1)].
- Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders [see Warnings and Precautions (5.2)].
- History of stroke, transient ischemic attack (TIA), or history or current evidence of hemiplegic or basilar migraine because these patients are at a higher risk of stroke [see Warnings and Precautions (5.4)].
- Peripheral vascular disease [see Warnings and Precautions (5.5)].
- Ischemic bowel disease [see Warnings and Precautions (5.5)].
- Uncontrolled hypertension [see Warnings and Precautions (5.8)].
- Recent use (i.e., within 24 hours) of another 5-hydroxytryptamine1 (5-HT1) agonist, ergotamine-containing medication, or ergot-type medication such as dihydroergotamine (DHE) or methysergide [see Drug Interactions (7.1)].
- Hypersensitivity to RELPAX (angioedema and anaphylaxis seen) [see Warnings and Precautions (5.9)].
- Recent use (i.e., within at least 72 hours) of the following potent CYP3A4 inhibitors: ketoconazole, itraconazole, nefazodone, troleandomycin, clarithromycin, ritonavir, or nelfinavir [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
-
5 WARNINGS AND PRECAUTIONS
RELPAX should only be used where a clear diagnosis of migraine has been established.
5.1 Myocardial Ischemia, Myocardial Infarction, and Prinzmetal's Angina
RELPAX is contraindicated in patients with ischemic or vasospastic CAD. There have been rare reports of serious cardiac adverse reactions, including acute myocardial infarction, occurring within a few hours following administration of RELPAX. Some of these reactions occurred in patients without known CAD. RELPAX may cause coronary artery vasospasm (Prinzmetal's angina), even in patients without a history of CAD.
Perform a cardiovascular evaluation in triptan-naïve patients who have multiple cardiovascular risk factors (e.g., increased age, diabetes, hypertension, smoking, obesity, strong family history of CAD) prior to receiving RELPAX. Do not use RELPAX if there is evidence of CAD or coronary artery vasospasm [see Contraindications (4)]. For patients with multiple cardiovascular risk factors who have a negative cardiovascular evaluation, consider administering the first RELPAX dose in a medically-supervised setting and performing an electrocardiogram (ECG) immediately following administration of RELPAX. For such patients, consider periodic cardiovascular evaluation in intermittent long-term users of RELPAX.
5.2 Arrhythmias
Life-threatening disturbances of cardiac rhythm including ventricular tachycardia and ventricular fibrillation leading to death have been reported within a few hours following the administration of 5-HT1 agonists. Discontinue RELPAX if these disturbances occur. RELPAX is contraindicated in patients with Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders [see Contraindications (4)].
5.3 Chest, Throat, Neck and/or Jaw Pain/Tightness/Pressure
Sensations of tightness, pain, and pressure in the chest, throat, neck, and jaw commonly occur after treatment with RELPAX and are usually non-cardiac in origin. However, perform a cardiac evaluation if these patients are at high cardiac risk. RELPAX is contraindicated in patients with CAD or Prinzmetal's variant angina [see Contraindications (4)].
5.4 Cerebrovascular Events
Cerebral hemorrhage, subarachnoid hemorrhage, and stroke have occurred in patients treated with 5-HT1 agonists, and some have resulted in fatalities. In a number of cases, it appears possible that the cerebrovascular events were primary, the 5-HT1 agonist having been administered in the incorrect belief that the symptoms experienced were a consequence of migraine, when they were not.
Before treating headaches in patients not previously diagnosed as migraineurs, and in migraineurs who present with symptoms atypical of migraine, other potentially serious neurological conditions need to be excluded. RELPAX is contraindicated in patients with a history of stroke or TIA [see Contraindications (4)].
5.5 Other Vasospasm Reactions
RELPAX may cause non-coronary vasospastic reactions, such as peripheral vascular ischemia, gastrointestinal vascular ischemia and infarction (presenting with abdominal pain and bloody diarrhea), and Raynaud's syndrome. In patients who experience symptoms or signs suggestive of a vasospastic reaction following the use of any 5-HT1 agonist, rule out a vasospastic reaction before receiving additional RELPAX doses [see Contraindications (4)].
5.6 Medication Overuse Headache
Overuse of acute migraine drugs (e.g. ergotamine, triptans, opioids, or combination of these drugs for 10 or more days per month) may lead to exacerbation of headache (medication overuse headache). Medication overuse headache may present as migraine-like daily headaches or as a marked increase in frequency of migraine attacks. Detoxification of patients, including withdrawal of the overused acute migraine drugs and treatment of withdrawal symptoms (which often includes a transient worsening of headache) may be necessary.
5.7 Serotonin Syndrome
Serotonin syndrome may occur with RELPAX, particularly during co-administration with selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and monoamine oxidase (MAO) inhibitors [see Drug Interactions (7.3)]. Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination), and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). The onset of symptoms usually occurs within minutes to hours of receiving a new or a greater dose of a serotonergic medication. Discontinue RELPAX if serotonin syndrome is suspected.
5.8 Increase in Blood Pressure
Significant elevation in blood pressure, including hypertensive crisis with acute impairment of organ systems, has been reported on rare occasions in patients treated with 5-HT1 agonists, including patients without a history of hypertension. Monitor blood pressure in patients treated with RELPAX. RELPAX is contraindicated in patients with uncontrolled hypertension [see Contraindications (4)].
5.9 Anaphylactic/Anaphylactoid Reactions
There have been reports of anaphylaxis, anaphylactoid, and hypersensitivity reactions including angioedema in patients receiving RELPAX. Such reactions can be life threatening or fatal. In general, anaphylactic reactions to drugs are more likely to occur in individuals with a history of sensitivity to multiple allergens. RELPAX is contraindicated in patients with a history of hypersensitivity reaction to RELPAX [see Contraindications (4)].
-
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in other sections of the prescribing information:
- Myocardial ischemia and myocardial infarction, and Prinzmetal's angina [see Warnings and Precautions (5.2)]
- Arrhythmias [see Warnings and Precautions (5.3)]
- Chest, throat, neck, and/or jaw pain/tightness/pressure [see Warnings and Precautions (5.4)]
- Cerebrovascular events [see Warnings and Precautions (5.4)]
- Other vasospasm reactions [see Warnings and Precautions (5.5)]
- Medication overuse headache [see Warnings and Precautions (5.6)]
- Serotonin syndrome [see Warnings and Precautions (5.7)]
- Increase in blood pressure [see Warnings and Precautions (5.8)]
- Hypersensitivity reactions [see Contraindications (4) and Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Among 4,597 patients who treated the first migraine headache with RELPAX in short-term placebo-controlled trials, the most common adverse reactions reported with treatment with RELPAX were asthenia, nausea, dizziness, and somnolence. These reactions appear to be dose-related.
In long-term open-label studies where patients were allowed to treat multiple migraine attacks for up to 1 year, 128 (8.3%) out of 1,544 patients discontinued treatment due to adverse reactions.
Table 1 lists adverse reactions that occurred in the subset of 5,125 migraineurs who received eletriptan doses of 20 mg, 40 mg and 80 mg or placebo in worldwide placebo-controlled clinical trials.
Only adverse reactions that were more frequent in a RELPAX treatment group compared to the placebo group with an incidence greater than or equal to 2% are included in Table 1.
Table 1: Adverse Reactions Incidence in Placebo-Controlled Migraine Clinical Trials: Reactions Reported by ≥ 2% Patients Treated with RELPAX and More Than Placebo Adverse Reaction Type Placebo
(n=988)RELPAX
20 mg
(n=431)RELPAX
40 mg
(n=1774)RELPAX
80 mg
(n=1932)ATYPICAL SENSATIONS Paresthesia 2% 3% 3% 4% Flushing/feeling of warmth 2% 2% 2% 2% PAIN AND PRESSURE SENSATIONS Chest – tightness/pain/pressure 1% 1% 2% 4% Abdominal –
pain/discomfort/stomach pain/ cramps/pressure1% 1% 2% 2% DIGESTIVE Dry mouth 2% 2% 3% 4% Dyspepsia 1% 1% 2% 2% Dysphagia – throat tightness/difficulty swallowing 0.2% 1% 2% 2% Nausea 5% 4% 5% 8% NEUROLOGICAL Dizziness 3% 3% 6% 7% Somnolence 4% 3% 6% 7% Headache 3% 4% 3% 4% OTHER Asthenia 3% 4% 5% 10% The frequency of adverse reactions in clinical trials did not increase when up to 2 doses of RELPAX were taken within 24 hours. The incidence of adverse reactions in controlled clinical trials was not affected by gender, age, or race of the patients. Adverse reaction frequencies were also unchanged by concomitant use of drugs commonly taken for migraine prophylaxis (e.g., SSRIs, beta blockers, calcium channel blockers, tricyclic antidepressants), estrogen replacement therapy or oral contraceptives.
6.2 Postmarketing Experience
The following adverse reaction(s) have been identified during post approval use of RELPAX. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Neurological: seizure
Digestive: vomiting
-
7 DRUG INTERACTIONS
7.1 Ergot-Containing Drugs Including Other 5-HT1B/1D Agonists
Ergot-containing drugs have been reported to cause prolonged vasospastic reactions. Because these effects may be additive, use of ergotamine-containing or ergot-type medications (like dihydroergotamine [DHE] or methysergide) and RELPAX within 24 hours of each other is contraindicated. Concomitant use of other 5-HT1 agonists within 24 hours of RELPAX treatment is contraindicated [see Contraindications (4)].
7.2 CYP3A4 Inhibitors
Potent CYP3A4 inhibitors significantly increase the exposure of RELPAX. RELPAX should not be used within at least 72 hours of treatment with potent CYP3A4 inhibitors [see Contraindications (4) and Clinical Pharmacology (12.3)].
7.3 Selective Serotonin Reuptake Inhibitors/Serotonin and Norepinephrine Reuptake Inhibitors and Serotonin Syndrome
Cases of serotonin syndrome have been reported during co-administration of triptans and SSRIs, SNRIs, TCAs and MAO inhibitors [see Warnings and Precautions (5.7)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available human data on the use of RELPAX in pregnant women are not sufficient to draw conclusions about drug-associated risk for major birth defects and miscarriage. In animal studies, oral administration of eletriptan during pregnancy or throughout pregnancy and lactation was associated with developmental toxicity (decreased fetal and pup weights, increased incidences of fetal structural abnormalities, decreased pup viability) at clinically-relevant doses [see Data].
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The reported rate of major birth defects among deliveries to women with migraine ranged from 2.2% to 2.9% and the reported rate of miscarriage was 17%, which were similar to rates reported in women without migraine.
Data
Human Data
A study using linked data from the Medical Birth Registry of Norway to the Norwegian Prescription Database compared pregnancy outcomes in women who redeemed prescriptions for triptans during pregnancy, as well as a migraine disease comparison group who redeemed prescriptions for triptans before pregnancy only. Of the 189 women who redeemed prescriptions for eletriptan during the first trimester, 4 (2.1%) had infants with major congenital malformations, while for the 174 women who redeemed prescriptions for eletriptan before, but not during, pregnancy, 11 (6.3%) had infants with major congenital malformations. Methodological limitations of this study, including small size of the eletriptan population and infrequent events, do not allow for thorough characterization of risk.
Animal Data
When pregnant rats were administered eletriptan (0, 10, 30, or 100 mg/kg/day) during the period of organogenesis, fetal weights were decreased and the incidences of vertebral and sternebral variations were increased at 100 mg/kg/day (approximately 12 times the maximum recommended human dose [MRHD] of 80 mg/day on a mg/m2 basis). The 30 and 100 mg/kg/day doses were also maternally toxic, as evidenced by decreased maternal body weight gain during gestation. The no-effect dose for adverse effects on embryofetal development in rats was 30 mg/kg/day, which is approximately 4 times the MRHD on a mg/m2 basis.
When eletriptan (0, 5, 10, or 50 mg/kg/day) was orally administered to pregnant rabbits throughout organogenesis, fetal weights were decreased at 50 mg/kg/day. The incidences of fused sternebrae and vena cava deviations were increased at all doses. Maternal toxicity was not evident at any dose. A no-effect dose for adverse effects on embryofetal development in rabbits was not established; the lowest dose tested (5 mg/kg/day) is similar to the MRHD on a mg/m2 basis.
Oral administration of eletriptan (0, 5, 15, or 50 mg/kg/day) to female rats throughout pregnancy and lactation resulted in a decrease in offspring viability and body weight at the highest dose tested. The no-effect dose for adverse effects on pre- and postnatal development in rats (15 mg/kg/day) is approximately 2 times the MRHD on a mg/m2 basis.
8.2 Lactation
Risk Summary
Eletriptan is excreted in human milk. There are no data on the effects of eletriptan on the breastfed infant or the effects of eletriptan on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for RELPAX and any potential adverse effects on the breastfed child from RELPAX or from the underlying maternal condition. Infant exposure can be minimized by avoiding breastfeeding for 24 hours after treatment.
8.4 Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
The efficacy of RELPAX Tablets (40 mg) in patients 11–17 was not established in a randomized, placebo-controlled trial of 274 adolescent migraineurs [see Clinical Studies (14)]. Adverse reactions observed were similar in nature to those reported in clinical trials in adults. Postmarketing experience with other triptans includes a limited number of reports that describe pediatric patients who have experienced clinically serious adverse reactions that are similar in nature to those reported rarely in adults. Long-term safety of eletriptan was studied in 76 adolescent patients who received treatment for up to one year. A similar profile of adverse reactions to that of adults was observed. The long-term safety of eletriptan in pediatric patients has not been established.
8.5 Geriatric Use
Blood pressure was increased to a greater extent in elderly subjects than in young subjects. The pharmacokinetic disposition of eletriptan in the elderly is similar to that seen in younger adults [see Clinical Pharmacology (12.3)]. In clinical trials, there were no apparent differences in efficacy or the incidence of adverse reactions between patients under 65 years of age and those 65 and above.
8.6 Hepatic Impairment
The effect of severe hepatic impairment on RELPAX metabolism has not been evaluated. RELPAX is not recommended for use in patients with severe hepatic impairment [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
The elimination half-life of eletriptan is about 4 hours [see Clinical Pharmacology (12.3)], therefore monitoring of patients after overdose with eletriptan should continue for at least 20 hours or longer while symptoms or signs persist.
There is no specific antidote to eletriptan.
It is unknown what effect hemodialysis or peritoneal dialysis has on the serum concentration of eletriptan.
-
11 DESCRIPTION
RELPAX (eletriptan hydrobromide) tablets contain eletriptan hydrobromide, which is a selective 5-hydroxytryptamine 1B/1D (5-HT1B/1D) receptor agonist. Eletriptan hydrobromide is chemically designated as (R)-3-[(1-Methyl-2-pyrrolidinyl)methyl]-5-[2-(phenylsulfonyl)ethyl]-1H-indole monohydrobromide, and it has the following chemical structure:
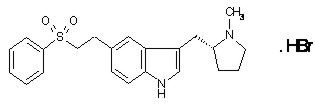
The empirical formula is C22H26N2O2S . HBr, representing a molecular weight of 463.43. Eletriptan hydrobromide is a white to light pale colored powder that is readily soluble in water.
Each RELPAX Tablet for oral administration contains 24.2 or 48.5 mg of eletriptan hydrobromide equivalent to 20 mg or 40 mg of eletriptan, respectively. Each tablet also contains the inactive ingredients microcrystalline cellulose NF, lactose monohydrate NF, croscarmellose sodium NF, magnesium stearate NF, titanium dioxide USP, hypromellose, triacetin USP and FD&C Yellow No. 6 aluminum lake.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Eletriptan binds with high affinity to 5-HT1B, 5-HT1D and 5-HT1F receptors, has modest affinity for 5-HT1A, 5-HT1E, 5-HT2B and 5-HT7 receptors.
Migraines are likely due to local cranial vasodilatation and/or to the release of sensory neuropeptides (vasoactive intestinal peptide, substance P and calcitonin gene-related peptide) through nerve endings in the trigeminal system. The therapeutic activity of RELPAX for the treatment of migraine headache is thought to be due to the agonist effects at the 5-HT1B/1D receptors on intracranial blood vessels (including the arterio-venous anastomoses) and sensory nerves of the trigeminal system which result in cranial vessel constriction and inhibition of pro-inflammatory neuropeptide release.
12.3 Pharmacokinetics
Absorption: Eletriptan is well absorbed after oral administration with peak plasma levels occurring approximately 1.5 hours after dosing to healthy subjects. In patients with moderate to severe migraine the median Tmax is 2.0 hours. The mean absolute bioavailability of eletriptan is approximately 50%. The oral pharmacokinetics are slightly more than dose-proportional over the clinical dose range. The AUC and Cmax of eletriptan are increased by approximately 20 to 30% following oral administration with a high fat meal. RELPAX can be taken with or without food.
Distribution: The volume of distribution of eletriptan following IV administration is 138L. Plasma protein binding is moderate and approximately 85%.
Metabolism: The N-demethylated metabolite of eletriptan is the only known active metabolite. This metabolite causes vasoconstriction similar to eletriptan in animal models. Though the half-life of the metabolite is estimated to be about 13 hours, the plasma concentration of the N-demethylated metabolite is 10–20% of parent drug and is unlikely to contribute significantly to the overall effect of the parent compound.
In vitro studies indicate that eletriptan is primarily metabolized by cytochrome P-450 enzyme CYP3A4 [see Contraindications (4) and Drug Interactions (7.2)].
Elimination: The terminal elimination half-life of eletriptan is approximately 4 hours. Mean renal clearance (CLR) following oral administration is approximately 3.9 L/h. Non-renal clearance accounts for about 90% of the total clearance.
Specific Populations
Age: The pharmacokinetics of eletriptan are generally unaffected by age. Blood pressure was increased to a greater extent in elderly subjects than in young subjects [see Use in Specific Populations (8.5)]. The pharmacokinetic disposition of eletriptan in the elderly is similar to that seen in younger adults.
There is a statistically significant increased half-life (from about 4.4 hours to 5.7 hours) between elderly (65 to 93 years of age) and younger adult subjects (18 to 45 years of age) [see Use in Specific Populations (8.5)].
Race: A comparison of pharmacokinetic studies run in western countries with those run in Japan has indicated an approximate 35% reduction in the exposure of eletriptan in Japanese male volunteers compared to western males. Population pharmacokinetic analysis of two clinical studies indicates no evidence of pharmacokinetic differences between Caucasians and non-Caucasian patients.
Menstrual Cycle: In a study of 16 healthy females, the pharmacokinetics of eletriptan remained consistent throughout the phases of the menstrual cycle.
Renal Impairment: There was no significant change in clearance observed in subjects with mild, moderate or severe renal impairment, though blood pressure elevations were observed in this population [see Warnings and Precautions (5.8)].
Hepatic Impairment: Subjects with mild or moderate hepatic impairment demonstrated an increase in both AUC (34%) and half-life. The Cmax was increased by 18%. No dose adjustment is necessary in subjects with mild or moderate hepatic impairment. The effects of severe hepatic impairment on eletriptan metabolism have not been evaluated [see Use in Specific Populations (8.6)].
Drug Interaction Studies
CYP3A4 inhibitors: In vitro studies have shown that eletriptan is metabolized by the CYP3A4 enzyme. A clinical study demonstrated about a 3-fold increase in Cmax and about a 6-fold increase in the AUC of eletriptan when combined with ketoconazole. The half-life increased from 5 hours to 8 hours and the Tmax increased from 2.8 hours to 5.4 hours. Another clinical study demonstrated about a 2-fold increase in Cmax and about a 4-fold increase in AUC when erythromycin was co-administered with eletriptan. It has also been shown that co-administration of verapamil and eletriptan yields about a 2-fold increase in Cmax and about a 3-fold increase in AUC of eletriptan, and that co-administration of fluconazole and eletriptan yields about a 1.4-fold increase in Cmax and about a 2-fold increase in AUC of eletriptan.
RELPAX is contraindicated within at least 72 hours of treatment with the following potent CYP3A4 inhibitors: ketoconazole, itraconazole, nefazodone, troleandomycin, clarithromycin, ritonavir and nelfinavir. RELPAX should not be used within 72 hours with drugs that have demonstrated potent CYP3A4 inhibition [see Contraindications (4)].
Propranolol: The Cmax and AUC of eletriptan were increased by 10 and 33%, respectively, in the presence of propranolol. No interactive increases in blood pressure were observed. No dosage adjustment appears to be needed for patients taking propranolol.
The effect of eletriptan on other drugs: The effect of eletriptan on enzymes other than cytochrome P450 has not been investigated. In vitro human liver microsome studies suggest that eletriptan has little potential to inhibit CYP1A2, 2C9, 2E1 and 3A4 at concentrations up to 100 µM. While eletriptan has an effect on CYP2D6 at high concentration, this effect should not interfere with metabolism of other drugs when eletriptan is used at recommended doses. There is no in vitro or in vivo evidence that clinical doses of eletriptan will induce drug metabolizing enzymes. Therefore, eletriptan is unlikely to cause clinically important drug interactions mediated by these enzymes.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Eletriptan was administered to rats and mice in the diet for 104 weeks. In rats, the incidence of testicular interstitial cell adenomas was increased at the high dose of 75 mg/kg/day, but not at 15 mg/kg/day, a dose associated with plasma exposures (AUC) approximately 2 times that in humans at the MRHD of 80 mg/day. In mice, the incidence of hepatocellular adenomas was increased at the high dose of 400 mg/kg/day, but not a dose of 90 mg/kg/day, associated with plasma AUC approximately 7 times that in humans at the MRHD.
Mutagenesis
Eletriptan was negative in in vitro (bacteria reverse mutation (Ames), mammalian cell gene mutation (CHO/ HGPRT), chromosomal aberration assay in human lymphocytes) and in vivo (mouse micronucleus) assays.
Impairment of Fertility
In a fertility and early embryonic development study, eletriptan (50, 100, or 200 mg/kg/day) was orally administered to male and female rats prior to and throughout mating and continuing in females to implantation. Plasma exposures (AUC) were 4, 8 and 16 times in males and 7, 14 and 28 times in females, respectively, that in humans at the MRHD. Prolongation of the estrous cycle and decreases in the number of corpora lutea, implants, and viable fetuses per dam were observed at 200 mg/kg/day. Male fertility parameters were not affected.
-
14 CLINICAL STUDIES
The efficacy of RELPAX in the acute treatment of migraines was evaluated in eight randomized, double-blind placebo-controlled studies. All eight studies used 40 mg. Seven studies evaluated an 80 mg dose and two studies included a 20 mg dose.
In all eight studies, randomized patients treated their headaches as outpatients. Seven studies enrolled adults and one study enrolled adolescents (age 11 to 17). Patients treated in the seven adult studies were predominantly female (85%) and Caucasian (94%) with a mean age of 40 years (range 18 to 78). In all studies, patients were instructed to treat a moderate to severe headache. Headache response, defined as a reduction in headache severity from moderate or severe pain to mild or no pain, was assessed up to 2 hours after dosing. Associated symptoms such as nausea, vomiting, photophobia and phonophobia were also assessed.
Maintenance of response was assessed for up to 24 hours post dose. In the adult studies, a second dose of RELPAX or other medication was allowed 2 to 24 hours after the initial treatment for both persistent and recurrent headaches. The incidence and time to use of these additional treatments were also recorded.
In the seven adult studies, the percentage of patients achieving headache response 2 hours after treatment was significantly greater among patients receiving RELPAX at all doses compared to those who received placebo. The two-hour response rates from these controlled clinical studies are summarized in Table 2.
Table 2: Percentage of Patients with Headache Response (Mild or No Headache) 2 Hours Following Treatment Placebo RELPAX
20 mgRELPAX
40 mgRELPAX
80 mgNA - Not Applicable - * p value < 0.05 vs placebo
Study 1 23.8%
(n=126)54.3%*
(n=129)65.0%*
(n=117)77.1%*
(n=118)Study 2 19.0%
(n=232)NA 61.6%*
(n=430)64.6%*
(n=446)Study 3 21.7%
(n=276)47.3%*
(n=273)61.9%*
(n=281)58.6%*
(n=290)Study 4 39.5%
(n=86)NA 62.3%*
(n=175)70.0%*
(n=170)Study 5 20.6%
(n=102)NA 53.9%*
(n=206)67.9%*
(n=209)Study 6 31.3%
(n=80)NA 63.9%*
(n=169)66.9%*
(n=160)Study 7 29.5%
(n=122)NA 57.5%*
(n=492)NA Comparisons of the performance of different drugs based upon results obtained in different clinical trials are never reliable. Because studies are generally conducted at different times, with different samples of patients, by different investigators, employing different criteria and/or different interpretations of the same criteria, under different conditions (dose, dosing regimen, etc.), quantitative estimates of treatment response and the timing of response may be expected to vary considerably from study to study.
The estimated probability of achieving an initial headache response within 2 hours following treatment is depicted in Figure 1.
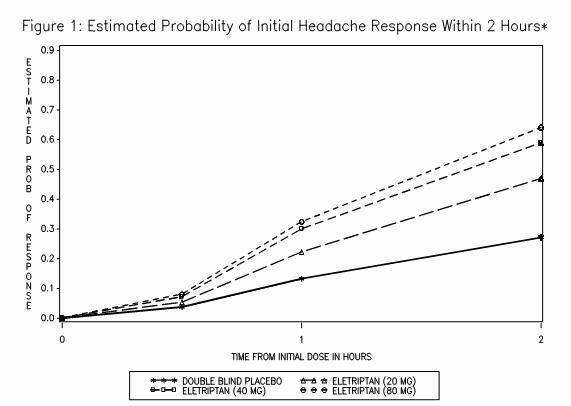
*Figure 1 shows the Kaplan-Meier plot of probability over time of obtaining headache response (no or mild pain) following treatment with eletriptan. The plot is based on 7 placebo-controlled, outpatient trials in adults providing evidence of efficacy (Studies 1 through 7). Patients not achieving headache response or taking additional treatment prior to 2 hours were censored at 2 hours.
For patients with migraine-associated photophobia, phonophobia, and nausea at baseline, there was a decreased incidence of these symptoms following administration of RELPAX as compared to placebo.
Two to 24 hours following the initial dose of study treatment, patients were allowed to use additional treatment for pain relief in the form of a second dose of study treatment or other medication. The estimated probability of taking a second dose or other medications for migraine over the 24 hours following the initial dose of study treatment is summarized in Figure 2.
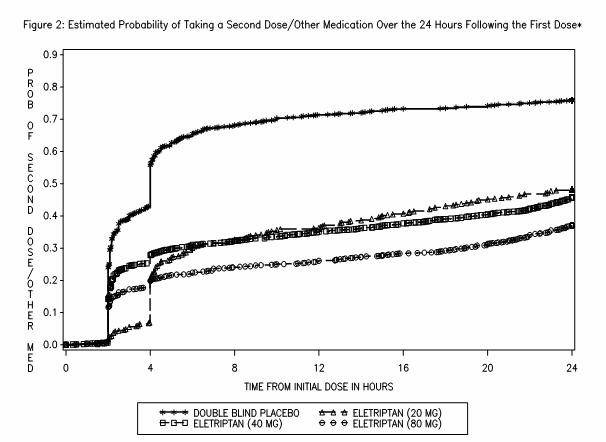
*This Kaplan-Meier plot is based on data obtained in 7 placebo-controlled trials in adults (Studies 1 through 7). Patients were instructed to take a second dose of study medication as follows: a) in the event of no response at 2 hours (studies 2 and 4–7) or at 4 hours (study 3); b) in the event of headache recurrence within 24 hours (studies 2–7). Patients not using additional treatments were censored at 24 hours. The plot includes both patients who had headache response at 2 hours and those who had no response to the initial dose. It should be noted that the protocols did not allow re-medication within 2 hours post dose.
The efficacy of RELPAX was unaffected by the duration of attack, gender or age of the patient, relationship to menses, or concomitant use of estrogen replacement therapy/oral contraceptives or frequently used migraine prophylactic drugs.
In a single study in adolescents (n=274), there were no statistically significant differences between treatment groups. The headache response rate at 2 hours was 57% for both RELPAX 40 mg Tablets and placebo.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
RELPAX Tablets containing 20 mg or 40 mg eletriptan (base) as the hydrobromide salt. RELPAX Tablets are orange, round, convex shaped, film-coated tablets with appropriate debossing.
They are supplied in the following strengths and package configurations:
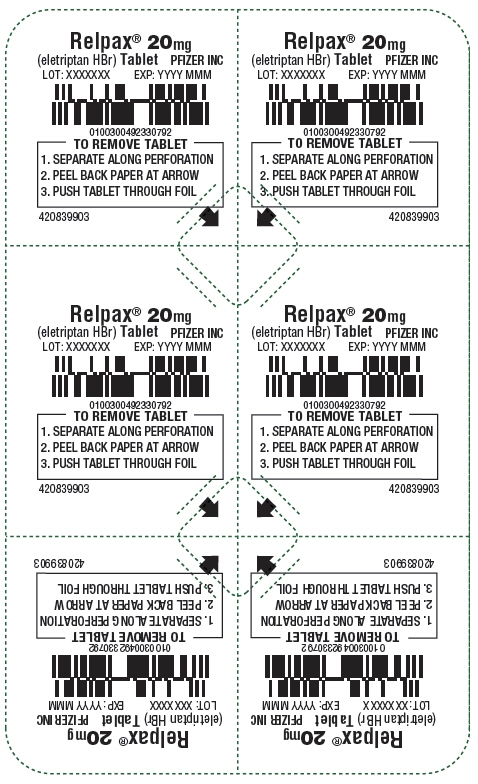
RELPAX Tablets Package Configuration Tablet Strength (mg) NDC Code Debossing Carton of 12 tablets.
Two blisters of 6 tablets in each carton.40 mg 0049-2340-05 REP40 and Pfizer Blister of 6 tablets 20 mg 0049-2330-45 REP20 and Pfizer Blister of 6 tablets 40 mg 0049-2340-45 REP40 and Pfizer -
17 PATIENT COUNSELING INFORMATION
See FDA Approved Patient Labeling (Patient Information)
Myocardial Ischemia and/or Infarction, Prinzmetal's Angina, Other Vasospastic Reactions, and Cerebrovascular Events
Inform patients that RELPAX may cause serious cardiovascular adverse reactions such as myocardial infarction or stroke, which may result in hospitalization and even death. Although serious cardiovascular reactions can occur without warning symptoms, instruct patients to be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and instruct them to ask for medical advice when observing any indicative sign or symptoms. Instruct patients to seek medical advice if they have symptoms of other vasospastic reactions [see Warnings and Precautions (5.1, 5.2, 5.4, 5.5, and 5.8)].
Anaphylactic/Anaphylactoid Reactions
Inform patients that anaphylactic/anaphylactoid reactions have occurred in patients receiving RELPAX. Such reactions can be life threatening or fatal. In general, anaphylactic reactions to drugs are more likely to occur in individuals with a history of sensitivity to multiple allergens [see Contraindications (4)].
Medication Overuse Headache
Inform patients that use of drugs to treat acute migraines for 10 or more days per month may lead to an exacerbation of headache, and encourage patients to record headache frequency and drug use (e.g., by keeping a headache diary) [see Warnings and Precautions (5.6)].
Serotonin Syndrome
Inform patients about the risk of serotonin syndrome with the use of RELPAX or other triptans, particularly during combined use with selective serotonin reuptake inhibitors (SSRIs) or serotonin and norepinephrine reuptake inhibitors (SNRIs) [see Warnings and Precautions (5.7) and Drug Interactions (7.3)].
Pregnancy
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during therapy [see Use in Specific Populations (8.1)].
Lactation
Inform patients to notify their healthcare provider if they are breastfeeding or plan to breastfeed [see Use in Specific Populations (8.2)].
- SPL UNCLASSIFIED SECTION
-
Patient Information
RELPAX® (REL - packs)
(eletriptan hydrobromide)
Tablets
Please read this information before you start taking RELPAX and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment.
What is the most important information I should know about RELPAX?
RELPAX can cause serious side effects, including:
Heart attack and other heart problems. Heart problems may lead to death.
Stop taking RELPAX and get emergency medical help right away if you have any of the following symptoms of a heart attack:
- discomfort in the center of your chest that lasts for more than a few minutes, or that goes away and comes back
- chest pain or chest discomfort that feels like an uncomfortable heavy pressure, squeezing, fullness, or pain
- pain or discomfort in your arms, back, neck, jaw, or stomach
- shortness of breath with or without chest discomfort
- breaking out in a cold sweat
- nausea or vomiting
- feeling lightheaded
RELPAX is not for people with risk factors for heart disease unless a heart exam is done and shows no problem. You have a higher risk for heart disease if you:
- have high blood pressure
- have high cholesterol levels
- smoke
- are overweight
- have diabetes
- have a family history of heart disease
- are a female who has gone through menopause
- are a male over age 40
Serotonin syndrome. Serotonin syndrome is a serious and life-threatening problem that can happen in people taking RELPAX, especially if RELPAX is taken with anti-depressant medicines called selective serotonin reuptake inhibitors (SSRIs) or serotonin and norepinephrine reuptake inhibitors (SNRIs).
Ask your doctor or pharmacist for a list of these medicines if you are not sure.
Call your doctor right away if you have any of the following symptoms of serotonin syndrome:
- mental changes such as seeing things that are not there (hallucinations), agitation, or coma
- fast heartbeat
- changes in blood pressure
- high body temperature
- tight muscles
- trouble walking
- nausea, vomiting, or diarrhea
What is RELPAX?
RELPAX is a prescription medicine used to treat acute migraine headaches with or without aura in adults.
RELPAX is for people who have been diagnosed with migraine headaches.
RELPAX is not used to prevent or decrease the number of migraine headaches you have.
It is not known if RELPAX is safe and effective to treat cluster headaches.
It is not known if RELPAX is safe and effective in children.
Who should not take RELPAX?
Do not take RELPAX if you:
- have heart problems or a history of heart problems
- have or have had a stroke or problems with your blood circulation
- have hemiplegic or basilar migraines. If you are not sure if you have these types of migraines, ask your doctor
- have narrowing of the blood vessels in your legs, arms, stomach, or kidney (peripheral vascular disease)
- have ischemic bowel disease
- have uncontrolled high blood pressure
- have taken any of the following medicines in the last 24 hours:
- other "triptans" or triptan combination products such as:
- almotriptan (Axert®)
- frovatriptan (Frova®)
- naratriptan (Amerge®)
- rizatriptan (Maxalt®)
- sumatriptan (Imitrex®)
- sumatriptan and naproxen sodium, (Treximet®)
- zolmitriptan (Zomig®)
- ergotamines such as:
- Bellergal-S®
- Cafergot®
- Ergomar®
- Wigraine®
- dihydroergotamines such as:
- D.H.E. 45® or Migranal® or methysergide (Sansert®)
- other "triptans" or triptan combination products such as:
- have taken the following medicines within the last 72 hours:
- ketoconazole (Nizoral®)
- itraconazole (Sporanox®)
- nefazodone (Serzone®)
- troleandomycin (TAO®)
- clarithromycin (Biaxin®)
- ritonavir (Norvir®)
- nelfinavir (Viracept®)
- are allergic to eletriptan or any of the ingredients in RELPAX. See the end of this leaflet for a complete list of ingredients in RELPAX.
What should I tell my doctor before taking RELPAX?
Before you take RELPAX, tell your doctor if you:
- have heart problems or family history of heart problems or stroke
- have high blood pressure
- have high cholesterol
- have diabetes
- smoke
- are overweight
- are a female who has gone through menopause
- have kidney problems
- have liver problems
- are pregnant or plan to become pregnant. It is not known if RELPAX will harm your unborn baby.
- are breastfeeding or plan to breastfeed. RELPAX passes into your breast milk and may harm your baby. Talk to your doctor about the best way to feed your baby if you take RELPAX.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Your doctor will decide if you can take RELPAX with your other medicines. RELPAX and other medicines may affect each other causing side effects.
Especially tell your doctor if you take anti-depressant medicines called:
- selective serotonin reuptake inhibitors (SSRIs)
- serotonin and norepinephrine reuptake inhibitors (SNRIs)
Ask your doctor or pharmacist for a list of these medicines if you are not sure.
Know the medicines you take. Keep a list of them to show your doctor or pharmacist when you get a new medicine.
How should I take RELPAX?
- Take RELPAX exactly as your doctor tells you to take it.
- Your doctor will tell you how much RELPAX to take and when to take it.
- Your doctor may change your dose if needed. Do not change your dose without first talking to your doctor.
- Take 1 RELPAX tablet as soon as you feel a migraine coming on.
- If you do not get any relief after your first RELPAX tablet, do not take a second tablet without first talking with your doctor.
- If your headache comes back or you only get some relief from your headache, you can take a second tablet 2 hours after the first tablet.
- Do not take more than a total of 80 mg of RELPAX tablets in a 24-hour period.
- If you take too much RELPAX, call your doctor or go to the nearest hospital emergency room right away.
- You should write down when you have headaches and when you take RELPAX so you can talk to your doctor about how well RELPAX is working for you.
What should I avoid while taking RELPAX?
RELPAX can cause dizziness, weakness, or drowsiness. If you have these symptoms, do not drive a car, use machinery, or do anything where you need to be alert.
What are the possible side effects of RELPAX?
RELPAX may cause serious side effects. See "What is the most important information I should know about RELPAX?"
These serious side effects include:
- changes in color or sensation in your fingers and toes (Raynaud's syndrome)
-
stomach and intestinal problems (gastrointestinal and colonic ischemic events). Symptoms of gastrointestinal and colonic ischemic events include:
- sudden or severe stomach pain
- stomach pain after meals
- weight loss
- nausea or vomiting
- constipation or diarrhea
- bloody diarrhea
- fever
-
problems with blood circulation to your legs and feet (peripheral vascular ischemia). Symptoms of peripheral vascular ischemia include:
- cramping and pain in your legs or hips
- feeling of heaviness or tightness in your leg muscles
- burning or aching pain in your feet or toes while resting
- numbness, tingling, or weakness in your legs
- cold feeling or color changes in 1 or both legs or feet
- medication overuse headaches. Some people who take too many RELPAX may have worse headaches (medication overuse headache). If your headaches get worse, your doctor may decide to stop your treatment with RELPAX.
The most common side effects of RELPAX include:
- dizziness
- nausea
- weakness
- tiredness
- drowsiness
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of RELPAX. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store RELPAX?
Store RELPAX at room temperature between 68°F to 77°F (20°C to 25°C).
General information about the safe and effective use of RELPAX
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use RELPAX for a condition for which it was not prescribed. Do not give RELPAX to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information summarizes the most important information about RELPAX. If you would like more information about RELPAX, talk with your doctor. You can ask your doctor or pharmacist for information on RELPAX that is written for health professionals.
For more information, call 1-866-4RELPAX (1-866-473-5729) or go to www.RELPAX.com.
What are the ingredients in RELPAX?
Active ingredient: eletriptan hydrobromide
Inactive ingredients: microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate, titanium dioxide, hypromellose, triacetin, and FD&C Yellow No. 6 aluminum lake.
All brands are trademarks of their owners.
This product's label may have been updated. For current full prescribing information, please visit www.pfizer.com.
This Patient Information has been approved by the U.S. Food and Drug Administration.
LAB-0077-13.0
Revised March 2020
- PRINCIPAL DISPLAY PANEL - 20 mg Tablet Blister Pack
- PRINCIPAL DISPLAY PANEL - 20 mg Tablet Blister Pack Carton
- PRINCIPAL DISPLAY PANEL - 40 mg Tablet Blister Pack
- PRINCIPAL DISPLAY PANEL - 40 mg Tablet Blister Pack Carton
-
INGREDIENTS AND APPEARANCE
RELPAX
eletriptan hydrobromide tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0049-2330 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ELETRIPTAN HYDROBROMIDE (UNII: M41W832TA3) (ELETRIPTAN - UNII:22QOO9B8KI) ELETRIPTAN 20 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) TRIACETIN (UNII: XHX3C3X673) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) ALUMINUM OXIDE (UNII: LMI26O6933) Product Characteristics Color ORANGE Score no score Shape ROUND Size 6mm Flavor Imprint Code REP20;Pfizer Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0049-2330-45 6 in 1 CARTON 12/26/2002 1 NDC: 0049-2330-79 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021016 12/26/2002 RELPAX
eletriptan hydrobromide tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0049-2340 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ELETRIPTAN HYDROBROMIDE (UNII: M41W832TA3) (ELETRIPTAN - UNII:22QOO9B8KI) ELETRIPTAN 40 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) MAGNESIUM STEARATE (UNII: 70097M6I30) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) HYPROMELLOSE, UNSPECIFIED (UNII: 3NXW29V3WO) TRIACETIN (UNII: XHX3C3X673) FD&C YELLOW NO. 6 (UNII: H77VEI93A8) ALUMINUM OXIDE (UNII: LMI26O6933) Product Characteristics Color ORANGE Score no score Shape ROUND Size 8mm Flavor Imprint Code REP40;Pfizer Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0049-2340-45 6 in 1 CARTON 12/26/2002 1 NDC: 0049-2340-79 1 in 1 BLISTER PACK; Type 0: Not a Combination Product 2 NDC: 0049-2340-05 12 in 1 CARTON 12/26/2002 2 NDC: 0049-2340-79 1 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021016 12/26/2002 Labeler - Roerig (829076996) Establishment Name Address ID/FEI Business Operations NEOLPHARMA, INC. 078709787 MANUFACTURE(0049-2330, 0049-2340) , PACK(0049-2330, 0049-2340) Establishment Name Address ID/FEI Business Operations Pfizer Ireland Pharmaceuticals 985104227 ANALYSIS(0049-2330, 0049-2340) , API MANUFACTURE(0049-2340) Establishment Name Address ID/FEI Business Operations Pfizer Pharmaceuticals LLC 829084552 ANALYSIS(0049-2330, 0049-2340) , MANUFACTURE(0049-2330, 0049-2340)
Trademark Results [Relpax]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 RELPAX 75655002 2747535 Dead/Cancelled |
Pfizer Inc. 1999-03-05 |
 RELPAX 75249087 2487796 Live/Registered |
Pfizer Inc. 1997-02-27 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.