IBRANCE- palbociclib capsule
Ibrance by
Drug Labeling and Warnings
Ibrance by is a Prescription medication manufactured, distributed, or labeled by U.S. Pharmaceuticals, Pfizer Pharmaceuticals LLC, Pharmacia & Upjohn Company LLC, Pfizer Ireland Pharmaceuticals, Pfizer Manufacturing Deutschland GmbH. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use IBRANCE safely and effectively. See full prescribing information for IBRANCE.
IBRANCE® (palbociclib) capsules, for oral use
Initial U.S. Approval: 2015RECENT MAJOR CHANGES
INDICATIONS AND USAGE
IBRANCE is a kinase inhibitor indicated for the treatment of hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced or metastatic breast cancer in combination with:
- letrozole as initial endocrine based therapy in postmenopausal women (1), or
- fulvestrant in women with disease progression following endocrine therapy.
The indication in combination with letrozole is approved under accelerated approval based on progression-free survival (PFS). Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial. (1)
DOSAGE AND ADMINISTRATION
IBRANCE capsules are taken orally with food in combination with letrozole or fulvestrant. (2)
DOSAGE FORMS AND STRENGTHS
Capsules: 125 mg, 100 mg, and 75 mg. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Neutropenia: Monitor complete blood count prior to start of IBRANCE therapy and at the beginning of each cycle, as well as on Day 14 of the first 2 cycles, and as clinically indicated. (2.2, 5.1)
- Pulmonary Embolism: Monitor patients for signs and symptoms of pulmonary embolism and treat as medically appropriate. (2.2, 5.2)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise patients of potential risk to a fetus and to use effective contraception. (5.3, 8.1, 8.3)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥10%) were neutropenia, leukopenia, infections, fatigue, nausea, anemia, stomatitis, headache, diarrhea, thrombocytopenia, constipation, alopecia, vomiting, rash, and decreased appetite. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer, Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- CYP3A Inhibitors: Avoid concurrent use of IBRANCE with strong CYP3A inhibitors. If the strong inhibitor cannot be avoided, reduce the IBRANCE dose. (2.2, 7.1)
- CYP3A Inducers: Avoid concurrent use of IBRANCE with strong CYP3A inducers. (7.2)
- CYP3A Substrates: The dose of sensitive CYP3A4 substrates with narrow therapeutic indices may need to be reduced when given concurrently with IBRANCE. (7.3)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 2/2016
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose and Schedule
2.2 Dose Modification
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Neutropenia
5.2 Pulmonary Embolism
5.3 Embryo-Fetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
7 DRUG INTERACTIONS
7.1 Agents That May Increase Palbociclib Plasma Concentrations
7.2 Agents That May Decrease Palbociclib Plasma Concentrations
7.3 Drugs That May Have Their Plasma Concentrations Altered by Palbociclib
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
IBRANCE is indicated for the treatment of HR-positive, HER2-negative advanced or metastatic breast cancer in combination with:
- letrozole as initial endocrine based therapy in postmenopausal women, or
- fulvestrant in women with disease progression following endocrine therapy.
The indication in combination with letrozole is approved under accelerated approval based on progression-free survival (PFS) [see Clinical Studies (14)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose and Schedule
The recommended dose of IBRANCE is a 125 mg capsule taken orally once daily for 21 consecutive days followed by 7 days off treatment to comprise a complete cycle of 28 days. IBRANCE should be taken with food [see Clinical Pharmacology (12.3)].
When coadministered with palbociclib, the recommended dose of letrozole is 2.5 mg taken once daily continuously throughout the 28-day cycle. Please refer to the full prescribing information of letrozole.
When coadministered with palbociclib, the recommended dose of fulvestrant is 500 mg administered on Days 1, 15, 29, and once monthly thereafter. Please refer to the full prescribing information of fulvestrant.
Patients should be encouraged to take their dose of IBRANCE at approximately the same time each day.
If the patient vomits or misses a dose, an additional dose should not be taken. The next prescribed dose should be taken at the usual time. IBRANCE capsules should be swallowed whole (do not chew, crush or open them prior to swallowing). Capsules should not be ingested if they are broken, cracked, or otherwise not intact.
Pre/perimenopausal women treated with the combination IBRANCE plus fulvestrant therapy should be treated with luteinizing hormone-releasing hormone (LHRH) agonists according to current clinical practice standards.
2.2 Dose Modification
The recommended dose modifications for adverse reactions are listed in Tables 1, 2 and 3.
Table 1. Recommended Dose Modification for Adverse Reactions Dose Level Dose - * If further dose reduction below 75 mg/day is required, discontinue.
Recommended starting dose 125 mg/day First dose reduction 100 mg/day Second dose reduction 75 mg/day* Table 2. Dose Modification and Management – Hematologic Toxicities* Grading according to CTCAE 4.0. CTCAE=Common Terminology Criteria for Adverse Events; LLN=lower limit of normal. - * Table applies to all hematologic adverse reactions except lymphopenia (unless associated with clinical events, e.g., opportunistic infections).
- † Absolute neutrophil count (ANC): Grade 1: ANC < LLN - 1500/mm3; Grade 2: ANC 1000 - <1500/mm3; Grade 3: ANC 500 - <1000/mm3; Grade 4: ANC <500/mm3
Monitor complete blood counts prior to the start of IBRANCE therapy and at the beginning of each cycle, as well as on Day 14 of the first 2 cycles, and as clinically indicated. CTCAE Grade Dose Modifications Grade 1 or 2 No dose adjustment is required. Grade 3 Day 1 of cycle:
Withhold IBRANCE, repeat complete blood count monitoring within 1 week. When recovered to Grade ≤2, start the next cycle at the same dose.
Day 14 of first 2 cycles:
Continue IBRANCE at current dose to complete cycle. Repeat complete blood count on Day 21.
Consider dose reduction in cases of prolonged (>1 week) recovery from Grade 3 neutropenia or recurrent Grade 3 neutropenia in subsequent cycles.Grade 3 neutropenia† with fever ≥38.5 °C and/or infection Withhold IBRANCE until recovery to Grade ≤2.
Resume at the next lower dose.Grade 4 Withhold IBRANCE until recovery to Grade ≤2.
Resume at the next lower dose.Table 3. Dose Modification and Management – Non-Hematologic Toxicities CTCAE Grade Dose Modifications Grading according to CTCAE 4.0.
CTCAE=Common Terminology Criteria for Adverse Events.Grade 1 or 2 No dose adjustment is required. Grade ≥3 non-hematologic toxicity (if persisting despite optimal medical treatment) Withhold until symptoms resolve to: - Grade ≤1;
- Grade ≤2 (if not considered a safety risk for the patient)
Refer to the full prescribing information for coadministered endocrine therapy dose adjustment guidelines in the event of toxicity and other relevant safety information or contraindications.
Dose Modifications for Use With Strong CYP3A Inhibitors
Avoid concomitant use of strong CYP3A inhibitors and consider an alternative concomitant medication with no or minimal CYP3A inhibition. If patients must be coadministered a strong CYP3A inhibitor, reduce the IBRANCE dose to 75 mg once daily. If the strong inhibitor is discontinued, increase the IBRANCE dose (after 3 to 5 half-lives of the inhibitor) to the dose used prior to the initiation of the strong CYP3A inhibitor [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
-
3 DOSAGE FORMS AND STRENGTHS
125 mg capsules: opaque hard gelatin capsules, size 0, with caramel cap and body, printed with white ink "Pfizer" on the cap, "PBC 125" on the body.
100 mg capsules: opaque hard gelatin capsules, size 1, with caramel cap and light orange body, printed with white ink "Pfizer" on the cap, "PBC 100" on the body.
75 mg capsules: opaque hard gelatin capsules, size 2, with light orange cap and body, printed with white ink "Pfizer" on the cap, "PBC 75" on the body.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Neutropenia
Neutropenia was the most frequently reported adverse reaction in both Study 1 (75%) and Study 2 (83%). A Grade ≥3 decrease in neutrophil counts was reported in 62% of patients receiving IBRANCE plus letrozole in Study 1 and 66% of patients receiving IBRANCE plus fulvestrant in Study 2. In Study 1 and 2, the median time to first episode of any grade neutropenia was 15 days and the median duration of Grade ≥3 neutropenia was 7 days [see Adverse Reactions (6.1)].
Monitor complete blood counts prior to starting IBRANCE therapy and at the beginning of each cycle, as well as on Day 14 of the first 2 cycles, and as clinically indicated. Dose interruption, dose reduction or delay in starting treatment cycles is recommended for patients who develop Grade 3 or 4 neutropenia [see Dosage and Administration (2.2)].
Febrile neutropenia has been reported in about 1% of patients exposed to IBRANCE. One death due to neutropenic sepsis was observed in Study 2. Physicians should inform patients to promptly report any episodes of fever [see Patient Counseling Information (17)].
5.2 Pulmonary Embolism
Pulmonary embolism has been reported at a higher rate in patients treated with IBRANCE plus letrozole in Study 1 (5%) and in patients treated with IBRANCE plus fulvestrant in Study 2 (1%) compared with no cases in patients treated either with letrozole alone or fulvestrant plus placebo. Monitor patients for signs and symptoms of pulmonary embolism and treat as medically appropriate.
5.3 Embryo-Fetal Toxicity
Based on findings from animal studies and its mechanism of action, IBRANCE can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of palbociclib to pregnant rats and rabbits during organogenesis resulted in embryo-fetal toxicity at maternal exposures that were ≥4 times the human clinical exposure based on area under the curve (AUC). Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with IBRANCE and for at least 3 weeks after the last dose [see Use in Specific Populations (8.1 and 8.3) and Clinical Pharmacology (12.1)].
-
6 ADVERSE REACTIONS
The following topics are described below and elsewhere in the labeling:
- Neutropenia [see Warnings and Precautions (5.1)]
- Pulmonary Embolism [see Warnings and Precautions (5.2)]
6.1 Clinical Studies Experience
Because clinical trials are conducted under varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice.
Study 1: IBRANCE plus Letrozole
Patients with ER-positive, HER2-negative advanced or metastatic breast cancer for initial endocrine based therapy
The safety of IBRANCE (125 mg/day) plus letrozole (2.5 mg/day) versus letrozole alone was evaluated in Study 1. The data described below reflect exposure to IBRANCE in 83 out of 160 patients with ER-positive, HER2-negative advanced breast cancer who received at least 1 dose of treatment in Study 1. The median duration of treatment for IBRANCE was 13.8 months while the median duration of treatment for letrozole on the letrozole-alone arm was 7.6 months.
Dose reductions due to an adverse reaction of any grade occurred in 36% of patients receiving IBRANCE plus letrozole. No dose reduction was allowed for letrozole in Study 1.
Permanent discontinuation associated with an adverse reaction occurred in 7 of 83 (8%) patients receiving IBRANCE plus letrozole and in 2 of 77 (3%) patients receiving letrozole alone. Adverse reactions leading to discontinuation for those patients receiving IBRANCE plus letrozole included neutropenia (6%), asthenia (1%), and fatigue (1%).
The most common adverse reactions (≥10%) of any grade reported in patients in the IBRANCE plus letrozole arm were neutropenia, leukopenia, fatigue, anemia, upper respiratory infection, nausea, stomatitis, alopecia, diarrhea, thrombocytopenia, decreased appetite, vomiting, asthenia, peripheral neuropathy, and epistaxis.
The most frequently reported serious adverse reactions in patients receiving IBRANCE plus letrozole were pulmonary embolism (3 of 83; 4%) and diarrhea (2 of 83; 2%).
An increased incidence of infections was observed in the IBRANCE plus letrozole arm (55%) compared to the letrozole alone arm (34%). Febrile neutropenia has been reported in the IBRANCE clinical program, although no cases were observed in Study 1. Grade ≥3 neutropenia was managed by dose reductions and/or dose delay or temporary discontinuation consistent with a permanent discontinuation rate of 6% due to neutropenia [see Dosage and Administration (2.2)].
Adverse reactions (≥10%) reported in patients who received IBRANCE plus letrozole or letrozole alone in Study 1 are listed in Table 4.
Table 4. Adverse Reactions* (≥10%) in Study 1 Adverse Reaction IBRANCE plus Letrozole
(N=83)Letrozole Alone
(N=77)All Grades
%Grade 3
%Grade 4
%All Grades
%Grade 3
%Grade 4
%Grading according to CTCAE 3.0. CTCAE=Common Terminology Criteria for Adverse Events; N=number of patients; N/A=not applicable; URI=Upper respiratory infection. - * URI includes: influenza, influenza like illness, laryngitis, nasopharyngitis, pharyngitis, rhinitis, sinusitis, upper respiratory tract infection.
- † Peripheral neuropathy includes: neuropathy peripheral, peripheral sensory neuropathy.
- ‡ Stomatitis includes: aphthous stomatitis, cheilitis, glossitis, glossodynia, mouth ulceration, mucosal inflammation, oral pain, oral discomfort, oropharyngeal pain, stomatitis.
- § Grade 1 events – 21%; Grade 2 events – 1%.
- ¶ Grade 1 events – 3%.
Infections and infestations URI* 31 1 0 18 0 0 Blood and lymphatic system disorders Neutropenia 75 48 6 5 1 0 Leukopenia 43 19 0 3 0 0 Anemia 35 5 1 7 1 0 Thrombocytopenia 17 2 0 1 0 0 Metabolism and nutrition disorders Decreased appetite 16 1 0 7 0 0 Nervous system disorders Peripheral neuropathy† 13 0 0 5 0 0 Respiratory, thoracic and mediastinal disorders Epistaxis 11 0 0 1 0 0 Gastrointestinal disorders Stomatitis‡ 25 0 0 7 1 0 Nausea 25 2 0 13 1 0 Diarrhea 21 4 0 10 0 0 Vomiting 15 0 0 4 1 0 Skin and subcutaneous tissue disorders Alopecia 22§ N/A N/A 3¶ N/A N/A General disorders and administration site conditions Fatigue 41 2 2 23 1 0 Asthenia 13 2 0 4 0 0 Table 5. Laboratory Abnormalities in Study 1 Laboratory Abnormality IBRANCE plus Letrozole
(N=83)Letrozole Alone
(N=77)All Grades
%Grade 3
%Grade 4
%All Grades
%Grade 3
%Grade 4
%N=number of patients; WBC=white blood cells WBC decreased 95 44 0 26 0 0 Neutrophils decreased 94 57 5 17 3 0 Lymphocytes decreased 81 17 1 35 3 0 Hemoglobin decreased 83 5 1 40 3 0 Platelets decreased 61 3 0 16 3 0 Study 2: IBRANCE plus Fulvestrant
Patients with HR-positive, HER2-negative advanced or metastatic breast cancer who have had disease progression on or after prior adjuvant or metastatic endocrine therapy
The safety of IBRANCE (125 mg/day) plus fulvestrant (500 mg) versus placebo plus fulvestrant was evaluated in Study 2. The data described below reflect exposure to IBRANCE in 345 out of 517 patients with HR-positive, HER2-negative advanced or metastatic breast cancer who received at least 1 dose of treatment in Study 2.
Dose reductions due to an adverse reaction of any grade occurred in 36% of patients receiving IBRANCE plus fulvestrant. No dose reduction was allowed for fulvestrant in Study 2.
Permanent discontinuation associated with an adverse reaction occurred in 19 of 345 (6%) patients receiving IBRANCE plus fulvestrant, and in 6 of 172 (3%) patients receiving placebo plus fulvestrant. Adverse reactions leading to discontinuation for those patients receiving IBRANCE plus fulvestrant included fatigue (0.6%), infections (0.6%), and thrombocytopenia (0.6%).
The most common adverse reactions (≥10%) of any grade reported in patients in the IBRANCE plus fulvestrant arm were neutropenia, leukopenia, infections, fatigue, nausea, anemia, stomatitis, headache, diarrhea, thrombocytopenia, constipation, vomiting, alopecia, rash, decreased appetite, and pyrexia.
The most frequently reported serious adverse reactions in patients receiving IBRANCE plus fulvestrant were infections (3%), pyrexia (1%), neutropenia (1%), and pulmonary embolism (1%).
Adverse reactions reported in patients who received IBRANCE plus fulvestrant or placebo plus fulvestrant in Study 2 are listed in Table 6.
Table 6. Adverse Reactions in Study 2 Adverse Reaction IBRANCE plus Fulvestrant
(N=345)Placebo plus Fulvestrant
(N=172)All Grades
%Grade 3
%Grade 4
%All Grades
%Grade 3
%Grade 4
%Grading according to CTCAE 4.0. CTCAE=Common Terminology Criteria for Adverse Events; N=number of patients; N/A=not applicable. - * Most common infections (>1%) include: nasopharyngitis, upper respiratory infection, urinary tract infection, influenza, bronchitis, rhinitis, conjunctivitis, pneumonia, sinusitis, cystitis, oral herpes, respiratory tract infection.
- † Stomatitis includes: aphthous stomatitis, cheilitis, glossitis, glossodynia, mouth ulceration, mucosal inflammation, oral pain, oropharyngeal discomfort, oropharyngeal pain, stomatitis.
- ‡ Grade 1 events – 17%; Grade 2 events – 1%.
- § Grade 1 events – 6%.
- ¶ Rash includes: rash, rash maculo-papular, rash pruritic, rash erythematous, rash papular, dermatitis, dermatitis acneiform, toxic skin eruption.
Infections and infestations Infections* 47 3 1 31 3 0 Blood and lymphatic system disorders Febrile neutropenia 1 1 0 1 0 1 Neutropenia 83 55 11 4 1 0 Leukopenia 53 30 1 5 1 1 Anemia 30 3 0 13 2 0 Thrombocytopenia 23 2 1 0 0 0 Eye disorders Vision blurred 6 0 0 2 0 0 Lacrimation increased 6 0 0 1 0 0 Dry eye 4 0 0 2 0 0 Metabolism and nutrition disorders Decreased appetite 16 1 0 8 1 0 Nervous system disorders Headache 26 1 0 20 0 0 Dysgeusia 7 0 0 3 0 0 Respiratory, thoracic and mediastinal disorders Epistaxis 7 0 0 2 0 0 Gastrointestinal disorders Nausea 34 0 0 28 1 0 Stomatitis† 28 1 0 13 0 0 Diarrhea 24 0 0 19 1 0 Constipation 20 0 0 16 0 0 Vomiting 19 1 0 15 1 0 Skin and subcutaneous tissue disorders Alopecia 18‡ N/A N/A 6§ N/A N/A Rash¶ 17 1 0 6 0 0 Dry skin 6 0 0 1 0 0 General disorders and administration site conditions Fatigue 41 2 0 29 1 0 Asthenia 8 0 0 5 1 0 Pyrexia 13 <1 0 5 0 0 Table 7. Laboratory Abnormalities in Study 2 Laboratory Abnormality IBRANCE plus Fulvestrant
(N=345)Placebo plus Fulvestrant
(N=172)All Grades
%Grade 3
%Grade 4
%All Grades
%Grade 3
%Grade 4
%N=number of patients; WBC=white blood cells. WBC decreased 99 45 1 26 0 1 Neutrophils decreased 96 56 11 14 0 1 Anemia 78 3 0 40 2 0 Platelets decreased 62 2 1 10 0 0 -
7 DRUG INTERACTIONS
Palbociclib is primarily metabolized by CYP3A and sulfotransferase (SULT) enzyme SULT2A1. In vivo, palbociclib is a time-dependent inhibitor of CYP3A.
7.1 Agents That May Increase Palbociclib Plasma Concentrations
Effect of CYP3A Inhibitors
Coadministration of a strong CYP3A inhibitor (itraconazole) increased the plasma exposure of palbociclib in healthy subjects by 87%. Avoid concomitant use of strong CYP3A inhibitors (e.g., clarithromycin, indinavir, itraconazole, ketoconazole, lopinavir/ritonavir, nefazodone, nelfinavir, posaconazole, ritonavir, saquinavir, telaprevir, telithromycin, and voriconazole). Avoid grapefruit or grapefruit juice during IBRANCE treatment. If coadministration of IBRANCE with a strong CYP3A inhibitor cannot be avoided, reduce the dose of IBRANCE [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
7.2 Agents That May Decrease Palbociclib Plasma Concentrations
Effect of CYP3A Inducers
Coadministration of a strong CYP3A inducer (rifampin) decreased the plasma exposure of palbociclib in healthy subjects by 85%. Avoid concomitant use of strong CYP3A inducers (e.g., phenytoin, rifampin, carbamazepine, enzalutamide, and St John's Wort) [see Clinical Pharmacology (12.3)].
7.3 Drugs That May Have Their Plasma Concentrations Altered by Palbociclib
Coadministration of midazolam with multiple doses of IBRANCE increased the midazolam plasma exposure by 61%, in healthy subjects, compared with administration of midazolam alone. The dose of the sensitive CYP3A substrate with a narrow therapeutic index (e.g., alfentanil, cyclosporine, dihydroergotamine, ergotamine, everolimus, fentanyl, pimozide, quinidine, sirolimus and tacrolimus) may need to be reduced as IBRANCE may increase their exposure [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and its mechanism of action, IBRANCE can cause fetal harm when administered to a pregnant woman [see Clinical Pharmacology (12.1)]. There are no available data in pregnant women to inform the drug-associated risk. In animal reproduction studies, administration of palbociclib to pregnant rats and rabbits during organogenesis resulted in embryofetal toxicity at maternal exposures that were ≥4 times the human clinical exposure based on AUC [see Data]. Advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
Data
Animal Data
In a fertility and early embryonic development study in female rats, palbociclib was administered orally for 15 days before mating through to Day 7 of pregnancy, which did not cause embryo toxicity at doses up to 300 mg/kg/day with maternal systemic exposures approximately 4 times the human exposure (AUC) at the recommended dose.
In embryo-fetal development studies in rats and rabbits, pregnant animals received oral doses up to 300 mg/kg/day and 20 mg/kg/day palbociclib, respectively, during the period of organogenesis. The maternally toxic dose of 300 mg/kg/day was fetotoxic in rats, resulting in reduced fetal body weights. At doses ≥100 mg/kg/day in rats, there was an increased incidence of a skeletal variation (increased incidence of a rib present at the seventh cervical vertebra). At the maternally toxic dose of 20 mg/kg/day in rabbits, there was an increased incidence of skeletal variations, including small phalanges in the forelimb. At 300 mg/kg/day in rats and 20 mg/kg/day in rabbits, the maternal systemic exposures were approximately 4 and 9 times the human exposure (AUC) at the recommended dose.
CDK4/6 double knockout mice have been reported to die in late stages of fetal development (gestation Day 14.5 until birth) due to severe anemia. However, knockout mouse data may not be predictive of effects in humans due to differences in degree of target inhibition.
8.2 Lactation
Risk Summary
There is no information regarding the presence of palbociclib in human milk, nor its effects on milk production or the breastfed infant. Because of the potential for serious adverse reactions in breastfed infants from IBRANCE, advise a lactating woman not to breastfeed during treatment with IBRANCE and for 3 weeks after the last dose.
8.3 Females and Males of Reproductive Potential
Contraception
Females
IBRANCE can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with IBRANCE and for at least 3 weeks after the last dose.
Males
Because of the potential for genotoxicity, advise male patients with female partners of reproductive potential to use effective contraception during treatment with IBRANCE and for 3 months after the last dose [see Nonclinical Toxicology (13.1)].
Infertility
Males
Based on animal studies, IBRANCE may impair fertility in males of reproductive potential [see Nonclinical Toxicology (13.1)].
8.5 Geriatric Use
Of 84 patients who received IBRANCE in Study 1, 37 patients (44%) were ≥65 years of age and 8 patients (10%) were ≥75 years of age. Of 347 patients who received IBRANCE in Study 2, 86 patients (25%) were ≥65 years of age. No overall differences in safety or effectiveness of IBRANCE were observed between these patients and younger patients.
8.6 Hepatic Impairment
Based on a population pharmacokinetic analysis that included 183 patients, where 40 patients had mild hepatic impairment (total bilirubin ≤ ULN and AST > ULN, or total bilirubin >1.0 to 1.5 × ULN and any AST), mild hepatic impairment had no effect on the exposure of palbociclib. The pharmacokinetics of palbociclib have not been studied in patients with moderate or severe hepatic impairment (total bilirubin >1.5 × ULN and any AST) [see Clinical Pharmacology (12.3)].
8.7 Renal Impairment
Based on a population pharmacokinetic analysis that included 183 patients, where 73 patients had mild renal impairment (60 mL/min ≤ CrCl <90 mL/min) and 29 patients had moderate renal impairment (30 mL/min ≤ CrCl <60 mL/min), mild and moderate renal impairment had no effect on the exposure of palbociclib. The pharmacokinetics of palbociclib have not been studied in patients with severe renal impairment [see Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
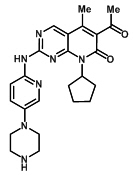
IBRANCE capsules for oral administration contain 125 mg, 100 mg, or 75 mg of palbociclib, a kinase inhibitor. The molecular formula for palbociclib is C24H29N7O2. The molecular weight is 447.54 daltons. The chemical name is 6-acetyl-8-cyclopentyl-5-methyl-2-{[5-(piperazin-1-yl)pyridin-2-yl]amino}pyrido[2,3-d]pyrimidin-7(8H)-one, and its structural formula is:
Palbociclib is a yellow to orange powder with pKa of 7.4 (the secondary piperazine nitrogen) and 3.9 (the pyridine nitrogen). At or below pH 4, palbociclib behaves as a high-solubility compound. Above pH 4, the solubility of the drug substance reduces significantly.
Inactive ingredients: Microcrystalline cellulose, lactose monohydrate, sodium starch glycolate, colloidal silicon dioxide, magnesium stearate, and hard gelatin capsule shells. The light orange, light orange/caramel and caramel opaque capsule shells contain gelatin, red iron oxide, yellow iron oxide, and titanium dioxide; and the printing ink contains shellac, titanium dioxide, ammonium hydroxide, propylene glycol and simethicone.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Palbociclib is an inhibitor of cyclin-dependent kinase (CDK) 4 and 6. Cyclin D1 and CDK4/6 are downstream of signaling pathways which lead to cellular proliferation. In vitro, palbociclib reduced cellular proliferation of estrogen receptor (ER)-positive breast cancer cell lines by blocking progression of the cell from G1 into S phase of the cell cycle. Treatment of breast cancer cell lines with the combination of palbociclib and antiestrogens leads to decreased retinoblastoma protein (Rb) phosphorylation resulting in reduced E2F expression and signaling, and increased growth arrest compared to treatment with each drug alone. In vitro treatment of ER-positive breast cancer cell lines with the combination of palbociclib and antiestrogens leads to increased cell senescence, which was sustained for up to 6 days following drug removal. In vivo studies using a patient-derived ER-positive breast cancer xenograft model demonstrated that the combination of palbociclib and letrozole increased the inhibition of Rb phosphorylation, downstream signaling and tumor growth compared to each drug alone.
12.2 Pharmacodynamics
Cardiac Electrophysiology
The effect of palbociclib on the QTc interval was evaluated in 184 patients with advanced cancer. No large change (i.e., >20 ms) in the QTc interval was detected at the mean observed maximal steady-state palbociclib concentration following a therapeutic schedule (e.g., 125 mg daily for 21 consecutive days followed by 7 days off to comprise a complete cycle of 28 days).
12.3 Pharmacokinetics
The pharmacokinetics (PK) of palbociclib were characterized in patients with solid tumors including advanced breast cancer and in healthy subjects.
Absorption
The mean Cmax of palbociclib is generally observed between 6 to 12 hours (time to reach maximum concentration, Tmax) following oral administration. The mean absolute bioavailability of IBRANCE after an oral 125 mg dose is 46%. In the dosing range of 25 mg to 225 mg, the AUC and Cmax increased proportionally with dose in general. Steady state was achieved within 8 days following repeated once daily dosing. With repeated once daily administration, palbociclib accumulated with a median accumulation ratio of 2.4 (range 1.5 to 4.2).
Food effect: Palbociclib absorption and exposure were very low in approximately 13% of the population under the fasted condition. Food intake increased the palbociclib exposure in this small subset of the population, but did not alter palbociclib exposure in the rest of the population to a clinically relevant extent. Therefore, food intake reduced the intersubject variability of palbociclib exposure, which supports administration of IBRANCE with food. Compared to IBRANCE given under overnight fasted conditions, the population average AUCinf and Cmax of palbociclib increased by 21% and 38%, respectively, when given with high-fat, high-calorie food (approximately 800 to 1000 calories with 150, 250, and 500 to 600 calories from protein, carbohydrate, and fat, respectively), by 12% and 27%, respectively, when given with low-fat, low-calorie food (approximately 400 to 500 calories with 120, 250, and 28 to 35 calories from protein, carbohydrate, and fat, respectively), and by 13% and 24%, respectively, when moderate-fat, standard calorie food (approximately 500 to 700 calories with 75 to 105, 250 to 350 and 175 to 245 calories from protein, carbohydrate, and fat, respectively) was given 1 hour before and 2 hours after IBRANCE dosing.
Distribution
Binding of palbociclib to human plasma proteins in vitro was approximately 85%, with no concentration dependence over the concentration range of 500 ng/mL to 5000 ng/mL. The geometric mean apparent volume of distribution (Vz/F) was 2583 L (26% CV).
Metabolism
In vitro and in vivo studies indicated that palbociclib undergoes hepatic metabolism in humans. Following oral administration of a single 125 mg dose of [14C]palbociclib to humans, the primary metabolic pathways for palbociclib involved oxidation and sulfonation, with acylation and glucuronidation contributing as minor pathways. Palbociclib was the major circulating drug-derived entity in plasma (23%). The major circulating metabolite was a glucuronide conjugate of palbociclib, although it only represented 1.5% of the administered dose in the excreta. Palbociclib was extensively metabolized with unchanged drug accounting for 2.3% and 6.9% of radioactivity in feces and urine, respectively. In feces, the sulfamic acid conjugate of palbociclib was the major drug-related component, accounting for 26% of the administered dose. In vitro studies with human hepatocytes, liver cytosolic and S9 fractions, and recombinant SULT enzymes indicated that CYP3A and SULT2A1 are mainly involved in the metabolism of palbociclib.
Elimination
The geometric mean apparent oral clearance (CL/F) of palbociclib was 63.1 L/hr (29% CV), and the mean (± standard deviation) plasma elimination half-life was 29 (±5) hours in patients with advanced breast cancer. In 6 healthy male subjects given a single oral dose of [14C]palbociclib, a median of 91.6% of the total administered radioactive dose was recovered in 15 days; feces (74.1% of dose) was the major route of excretion, with 17.5% of the dose recovered in urine. The majority of the material was excreted as metabolites.
Age, Gender, and Body Weight
Based on a population pharmacokinetic analysis in 183 patients with cancer (50 male and 133 female patients, age range from 22 to 89 years, and body weight range from 37.9 to 123 kg), gender had no effect on the exposure of palbociclib, and age and body weight had no clinically important effect on the exposure of palbociclib.
Pediatric Population
Pharmacokinetics of IBRANCE have not been evaluated in patients <18 years of age.
Drug Interactions
In vitro data indicate that CYP3A and SULT enzyme SULT2A1 are mainly involved in the metabolism of palbociclib. Palbociclib is a weak time-dependent inhibitor of CYP3A following daily 125 mg dosing to steady state in humans. In vitro, palbociclib is not an inhibitor of CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, and 2D6, and is not an inducer of CYP1A2, 2B6, 2C8, and 3A4 at clinically relevant concentrations.
CYP3A Inhibitors: Data from a drug interaction trial in healthy subjects (N=12) indicate that coadministration of multiple 200 mg daily doses of itraconazole with a single 125 mg IBRANCE dose increased palbociclib AUCinf and the Cmax by approximately 87% and 34%, respectively, relative to a single 125 mg IBRANCE dose given alone [see Drug Interactions (7.1)].
CYP3A Inducers: Data from a drug interaction trial in healthy subjects (N=15) indicate that coadministration of multiple 600 mg daily doses of rifampin, a strong CYP3A inducer, with a single 125 mg IBRANCE dose decreased palbociclib AUCinf and Cmax by 85% and 70%, respectively, relative to a single 125 mg IBRANCE dose given alone. Data from a drug interaction trial in healthy subjects (N=14) indicate that coadministration of multiple 400 mg daily doses of modafinil, a moderate CYP3A inducer, with a single 125 mg IBRANCE dose decreased palbociclib AUCinf and Cmax by 32% and 11%, respectively, relative to a single 125 mg IBRANCE dose given alone [see Drug Interactions (7.2)].
CYP3A Substrates: Palbociclib is a weak time-dependent inhibitor of CYP3A following daily 125 mg dosing to steady state in humans. In a drug interaction trial in healthy subjects (N=26), coadministration of midazolam with multiple doses of IBRANCE increased the midazolam AUCinf and the Cmax values by 61% and 37%, respectively, as compared with administration of midazolam alone [see Drug Interactions (7.3)].
Gastric pH Elevating Medications: In a drug interaction trial in healthy subjects, coadministration of a single 125 mg dose of IBRANCE with multiple doses of the proton pump inhibitor (PPI) rabeprazole under fed conditions decreased palbociclib Cmax by 41%, but had limited impact on AUCinf (13% decrease), when compared to a single dose of IBRANCE administered alone. Given the reduced effect on gastric pH of H2-receptor antagonists and local antacids compared to PPIs, the effect of these classes of acid-reducing agents on palbociclib exposure under fed conditions is expected to be minimal. Under fed conditions there is no clinically relevant effect of PPIs, H2-receptor antagonists, or local antacids on palbociclib exposure. In another healthy subject study, coadministration of a single dose of IBRANCE with multiple doses of the PPI rabeprazole under fasted conditions decreased palbociclib AUCinf and Cmax by 62% and 80%, respectively, when compared to a single dose of IBRANCE administered alone.
Letrozole: Data from a clinical trial in patients with breast cancer showed that there was no drug interaction between palbociclib and letrozole when the 2 drugs were coadministered.
Fulvestrant: Data from a clinical trial in patients with breast cancer showed that there was no clinically relevant drug interaction between palbociclib and fulvestrant when the 2 drugs were coadministered.
Goserelin: Data from a clinical trial in patients with breast cancer showed that there was no clinically relevant drug interaction between palbociclib and goserelin when the 2 drugs were coadministered.
Effect of Palbociclib on Transporters: In vitro evaluations indicated that palbociclib has a low potential to inhibit the activities of drug transporters P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), organic anion transporter (OAT)1, OAT3, organic cation transporter (OCT)2 and organic anion transporting polypeptide (OATP)1B1, OATP1B3 at clinically relevant concentrations.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with palbociclib.
Palbociclib was aneugenic in Chinese Hamster Ovary cells in vitro and in the bone marrow of male rats at doses ≥100 mg/kg/day for 3 weeks. Palbociclib was not mutagenic in an in vitro bacterial reverse mutation (Ames) assay and was not clastogenic in the in vitro human lymphocyte chromosome aberration assay.
In a fertility study in female rats, palbociclib did not affect mating or fertility at any dose up to 300 mg/kg/day (approximately 4 times human clinical exposure based on AUC) and no adverse effects were observed in the female reproductive tissues in repeat-dose toxicity studies up to 300 mg/kg/day in the rat and 3 mg/kg/day in the dog (approximately 6 times and similar to human exposure [AUC], at the recommended dose, respectively).
The adverse effects of palbociclib on male reproductive function and fertility were observed in the repeat-dose toxicology studies in rats and dogs and a male fertility study in rats. In repeat-dose toxicology studies, palbociclib-related findings in the testis, epididymis, prostate, and seminal vesicle at ≥30 mg/kg/day in rats and ≥0.2 mg/kg/day in dogs included decreased organ weight, atrophy or degeneration, hypospermia, intratubular cellular debris, lower sperm motility and density, and decreased secretion. Partial reversibility of male reproductive organ effects was observed in the rat and dog following a 4- and 12-week non-dosing period, respectively. These doses in rats and dogs resulted in approximately ≥10 and 0.1 times, respectively, the exposure [AUC] in humans at the recommended dose. In the fertility and early embryonic development study in male rats, palbociclib caused no effects on mating but resulted in a slight decrease in fertility at 100 mg/kg/day with projected exposure levels [AUC] of 20 times the exposure in humans at the recommended dose.
13.2 Animal Toxicology and/or Pharmacology
Altered glucose metabolism (glycosuria, hyperglycemia, decreased insulin) associated with changes in the pancreas (islet cell vacuolation), eye (cataracts, lens degeneration), teeth (degeneration/necrosis of ameloblasts in actively growing teeth), kidney (tubule vacuolation, chronic progressive nephropathy), and adipose tissue (atrophy) were identified in the 27-week repeat-dose toxicology study in rats and were most prevalent in males at doses ≥30 mg/kg/day (approximately 11 times the human exposure [AUC] at the recommended dose). Some of these findings (glycosuria/hyperglycemia, pancreatic islet cell vacuolation, and kidney tubule vacuolation) were present in the 15-week repeat-dose toxicology study in rats, but with lower incidence and severity. The rats used in these studies were approximately 7 weeks old at the beginning of the studies. Altered glucose metabolism or associated changes in pancreas, eye, teeth, kidney, and adipose tissue were not identified in dogs in repeat-dose toxicology studies up to 39 weeks duration.
-
14 CLINICAL STUDIES
Study 1: IBRANCE plus Letrozole
Patients with ER-positive, HER2-negative advanced or metastatic breast cancer for initial endocrine based therapy
Study 1 was a randomized, open-label, multicenter study of IBRANCE plus letrozole versus letrozole alone conducted in postmenopausal women with ER-positive, HER2-negative advanced breast cancer who had not received previous systemic treatment for their advanced disease. A total of 165 patients were randomized in Study 1. Randomization was stratified by disease site (visceral versus bone only versus other) and by disease-free interval (>12 months from the end of adjuvant treatment to disease recurrence versus ≤12 months from the end of adjuvant treatment to disease recurrence or de novo advanced disease). IBRANCE was given orally at a dose of 125 mg daily for 21 consecutive days followed by 7 days off treatment. Patients received study treatment until progressive disease, unmanageable toxicity, or consent withdrawal. The major efficacy outcome measure of the study was investigator-assessed PFS evaluated according to Response Evaluation Criteria in Solid Tumors Version 1.0 (RECIST).
Patients enrolled in this study had a median age of 63 years (range 38 to 89). The majority of patients were White (90%) and all patients had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0 or 1. Forty-three percent of patients had received chemotherapy and 33% had received antihormonal therapy in the neoadjuvant or adjuvant setting prior to their diagnosis of advanced breast cancer. Forty-nine percent of patients had no prior systemic therapy in the neoadjuvant or adjuvant setting. The majority of patients (98%) had metastatic disease. Nineteen percent of patients had bone only disease and 48% of patients had visceral disease.
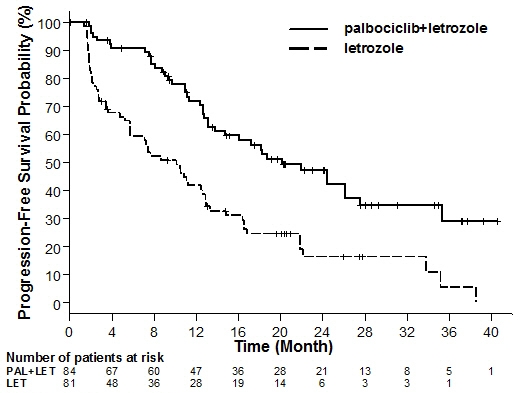
Major efficacy results from Study 1 are summarized in Table 8 and Figure 1. Consistent results were observed across patient subgroups of, disease-free interval, disease site and prior therapy. The treatment effect of the combination on PFS was also supported by a retrospective independent review of radiographs with an observed hazard ratio (HR) of 0.621 (95% CI: 0.378, 1.019). Overall response rate in patients with measurable disease as assessed by the investigator was higher in the IBRANCE plus letrozole compared to the letrozole-alone arm (55.4% versus 39.4%). At the time of the final analysis of PFS, overall survival (OS) data were not mature with 37% of events.
Table 8. Efficacy Results – Study 1 (Investigator Assessment, Intent-to-Treat Population) IBRANCE plus Letrozole
(N=84)Letrozole
(N=81)CI=confidence interval; N=number of patients. Progression-Free Survival (PFS)
Number of PFS Events (%)41 (48.8%) 59 (72.8%) Hazard ratio (95% CI) 0.488 (0.319, 0.748) Median PFS [months] (95% CI) 20.2 (13.8, 27.5) 10.2 (5.7, 12.6) Figure 1. Kaplan-Meier Curves of Progression-Free Survival – Study 1 (Investigator Assessment, Intent-to-Treat Population)
LET=letrozole; PAL=palbociclib. Study 2: IBRANCE plus Fulvestrant
Patients with HR-positive, HER2-negative advanced or metastatic breast cancer who have had disease progression on or after prior adjuvant or metastatic endocrine therapy
Study 2 was an international, randomized, double-blind, parallel group, multicenter study of IBRANCE plus fulvestrant versus placebo plus fulvestrant conducted in women with HR-positive, HER2-negative advanced breast cancer, regardless of their menopausal status, whose disease progressed on or after prior endocrine therapy. A total of 521 pre/postmenopausal women were randomized 2:1 to IBRANCE plus fulvestrant or placebo plus fulvestrant and stratified by documented sensitivity to prior hormonal therapy, menopausal status at study entry (pre/peri versus postmenopausal), and presence of visceral metastases. IBRANCE was given orally at a dose of 125 mg daily for 21 consecutive days followed by 7 days off treatment. Pre/perimenopausal women were enrolled in the study and received the LHRH agonist goserelin for at least 4 weeks prior to and for the duration of Study 2. Patients continued to receive assigned treatment until objective disease progression, symptomatic deterioration, unacceptable toxicity, death, or withdrawal of consent, whichever occurred first. The major efficacy outcome of the study was investigator-assessed PFS evaluated according to RECIST 1.1.
Patients enrolled in this study had a median age of 57 years (range 29 to 88). The majority of patients on study were White (74%), all patients had an ECOG PS of 0 or 1, and 80% were postmenopausal. All patients had received prior systemic therapy and 75% of patients had received a previous chemotherapy regimen. Twenty-five percent of patients had received no prior therapy in the metastatic disease setting, 60% had visceral metastases, and 23% had bone only disease.
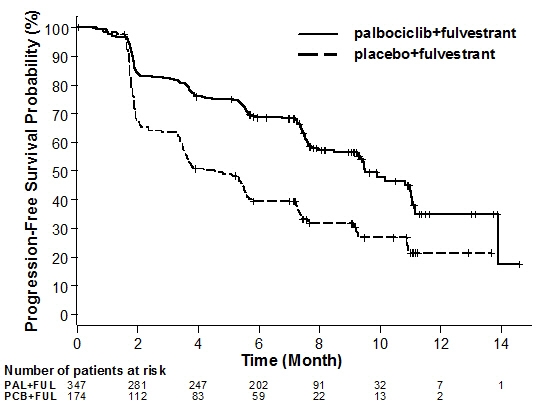
The results from the investigator-assessed PFS from Study 2 are summarized in Table 9 and Figure 2. Consistent results were observed across patient subgroups of disease site, sensitivity to prior hormonal therapy and menopausal status. Confirmed overall response rate in patients with measurable disease as assessed by the investigator was 24.6% in the IBRANCE plus fulvestrant and was 10.9% in the placebo plus fulvestrant arm. Duration of response was 9.3 months in the IBRANCE plus fulvestrant arm compared with 7.6 months in the placebo plus fulvestrant arm. At the time of final analysis of PFS, OS data were not mature with 29% of events.
Table 9. Efficacy Results – Study 2 (Investigator Assessment, Intent-to-Treat Population) IBRANCE plus Fulvestrant
(N=347)Placebo plus Fulvestrant
(N=174)CI=confidence interval; N=number of patients Progression-Free Survival
Number of PFS Events (%)145 (41.8%) 114 (65.5%) Hazard ratio (95% CI) and p-value 0.461 (0.360-0.591), p<0.0001 Median PFS [months] (95% CI) 9.5 (9.2-11.0) 4.6 (3.5-5.6) Figure 2. Kaplan-Meier Plot of Progression-Free Survival (Investigator Assessment, Intent-to-Treat Population) – Study 2
FUL=fulvestrant; PAL=palbociclib; PCB=placebo. -
16 HOW SUPPLIED/STORAGE AND HANDLING
IBRANCE is supplied in the following strengths and package configurations:
IBRANCE Capsules Package Configuration Capsule Strength (mg) NDC Capsule Description Bottles of 21 capsules 125 NDC: 0069-0189-21 opaque, hard gelatin capsules, size 0, with caramel cap and body, printed with white ink "Pfizer" on the cap, "PBC 125" on the body Bottles of 21 capsules 100 NDC: 0069-0188-21 opaque, hard gelatin capsules, size 1, with caramel cap and light orange body, printed with white ink "Pfizer" on the cap, "PBC 100" on the body Bottles of 21 capsules 75 NDC: 0069-0187-21 opaque, hard gelatin capsules, size 2, with light orange cap and body, printed with white ink "Pfizer" on the cap, "PBC 75" on the body -
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Myelosuppression/Infection
- Advise patients to immediately report any signs or symptoms of myelosuppression or infection, such as fever, chills, dizziness, shortness of breath, weakness or any increased tendency to bleed and/or to bruise [see Warnings and Precautions (5.1)].
Pulmonary Embolism
- Advise patients to immediately report any signs or symptoms of pulmonary embolism, such as shortness of breath, chest pain, tachypnea, and tachycardia [see Warnings and Precautions (5.2)].
Drug Interactions
- Grapefruit may interact with IBRANCE. Patients should not consume grapefruit products while on treatment with IBRANCE.
- Inform patients to avoid strong CYP3A inhibitors and strong CYP3A inducers.
- Advise patients to inform their health care providers of all concomitant medications, including prescription medicines, over-the-counter drugs, vitamins, and herbal products [see Drug Interactions (7)].
Dosing and Administration
- Advise patients to take IBRANCE with food.
- If the patient vomits or misses a dose, an additional dose should not be taken. The next prescribed dose should be taken at the usual time. IBRANCE capsules should be swallowed whole (do not chew, crush or open them prior to swallowing). No capsule should be ingested if it is broken, cracked, or otherwise not intact.
Pregnancy, Lactation, and Fertility
- Embryo-Fetal Toxicity
- Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception during treatment with IBRANCE therapy and for at least 3 weeks after the last dose. Advise females to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.3) and Use in Specific Populations (8.1 and 8.3)].
- Advise male patients with female partners of reproductive potential to use effective contraception during treatment with IBRANCE and for at least 3 months after the last dose [see Use in Specific Populations (8.3)].
- Lactation: Advise women not to breastfeed during treatment with IBRANCE and for 3 weeks after the last dose [see Use in Specific Populations (8.2)].
- SPL UNCLASSIFIED SECTION
-
PATIENT PACKAGE INSERT
This Patient Information has been approved by the U.S. Food and Drug Administration.
Revised: February 2016PATIENT INFORMATION
IBRANCE® (EYE-brans)
(palbociclib)
capsulesWhat is the most important information I should know about IBRANCE?
IBRANCE may cause serious side effects, including: Low white blood cell counts (neutropenia). Low white blood cell counts are very common when taking IBRANCE and may cause serious infections that can lead to death. Your healthcare provider should check your white blood cell counts before and during treatment. If you develop low white blood cell counts during treatment with IBRANCE, your healthcare provider may stop your treatment, decrease your dose, or may tell you to wait to begin your treatment cycle. Tell your healthcare provider right away if you have signs and symptoms of low white blood cell counts or infections such as fever and chills. Blood clots in the arteries of your lungs (pulmonary embolism or PE). IBRANCE may cause serious or life-threatening blood clots in the arteries of your lungs. Tell your healthcare provider right away if you have any of the following signs and symptoms of a PE: - shortness of breath
- sudden, sharp chest pain that may become worse with deep breathing
- rapid heart rate
- rapid breathing
See "What are the possible side effects of IBRANCE?" for more information about side effects. What is IBRANCE? IBRANCE is a prescription medicine used to treat hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative breast cancer that has spread to other parts of the body (metastatic) in combination with: - letrozole as the first hormonal based therapy in women who have gone through menopause, or
- fulvestrant in women with disease progression following hormonal therapy.
What should I tell my healthcare provider before taking IBRANCE? Before you take IBRANCE, tell your healthcare provider if you: - have fever, chills, or any other signs or symptoms of infection.
- have liver or kidney problems.
- have any other medical conditions.
- are pregnant, or plan to become pregnant. IBRANCE can harm your unborn baby.
- Females who are able to become pregnant and who take IBRANCE should use effective birth control during treatment and for at least 3 weeks after stopping IBRANCE.
- Males who are taking IBRANCE, with female partners who can become pregnant should use effective birth control during treatment with IBRANCE for 3 months after the final dose of IBRANCE.
- Talk to your healthcare provider about birth control methods that may be right for you during this time.
- If you become pregnant or think you are pregnant, tell your healthcare provider right away.
- are breastfeeding or plan to breastfeed. It is not known if IBRANCE passes into your breast milk. You and your healthcare provider should decide if you will take IBRANCE or breastfeed. You should not do both.
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. IBRANCE and other medicines may affect each other causing side effects. Know the medicines you take. Keep a list of them to show your healthcare provider or pharmacist when you get a new medicine. How should I take IBRANCE? - Take IBRANCE exactly as your healthcare provider tells you.
- Take IBRANCE with food.
- Swallow IBRANCE capsules whole. Do not chew, crush or open IBRANCE capsules before swallowing them.
- Do not take any IBRANCE capsules that are broken, cracked, or that look damaged.
- Avoid grapefruit and grapefruit products during treatment with IBRANCE. Grapefruit may increase the amount of IBRANCE in your blood.
- Do not change your dose or stop taking IBRANCE unless your healthcare provider tells you.
- If you miss a dose of IBRANCE or vomit after taking a dose of IBRANCE, do not take another dose on that day. Take your next dose at your regular time.
- If you take too much IBRANCE, call your healthcare provider right away or go to the nearest hospital emergency room.
IBRANCE may cause serious side effects. See "What is the most important information I should know about IBRANCE?" Common side effects of IBRANCE when used with either letrozole or fulvestrant include: - Low red blood cell counts and low platelet counts are common with IBRANCE. Call your healthcare provider right away if you develop any of these symptoms during treatment:
- dizziness
- shortness of breath
- weakness
- bleeding or bruising more easily
- nosebleeds
- infections (see "What is the most important information I should know about IBRANCE?")
- tiredness
- nausea
- sore mouth
- headache
- diarrhea
- constipation
- hair thinning or hair loss
- vomiting
- rash
- loss of appetite
IBRANCE may cause fertility problems in males. This may affect your ability to father a child. Talk to your healthcare provider if this is a concern for you. Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of IBRANCE. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store IBRANCE? - Store IBRANCE at 68 °F to 77 °F (20 °C to 25 °C).
Keep IBRANCE and all medicines out of the reach of children. General information about the safe and effective use of IBRANCE Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use IBRANCE for a condition for which it was not prescribed. Do not give IBRANCE to other people, even if they have the same symptoms you have. It may harm them. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for more information about IBRANCE that is written for health professionals. For more information, go to www.IBRANCE.com or call 1-800-438-1985. What are the ingredients in IBRANCE? Active ingredient: palbociclib Inactive ingredients: Microcrystalline cellulose, lactose monohydrate, sodium starch glycolate, colloidal silicon dioxide, magnesium stearate, and hard gelatin capsule shells. Light orange, light orange/caramel and caramel opaque capsule shells contain: gelatin, red iron oxide, yellow iron oxide, and titanium dioxide. Printing ink contains: shellac, titanium dioxide, ammonium hydroxide, propylene glycol and simethicone.

LAB-0724-2.0 -
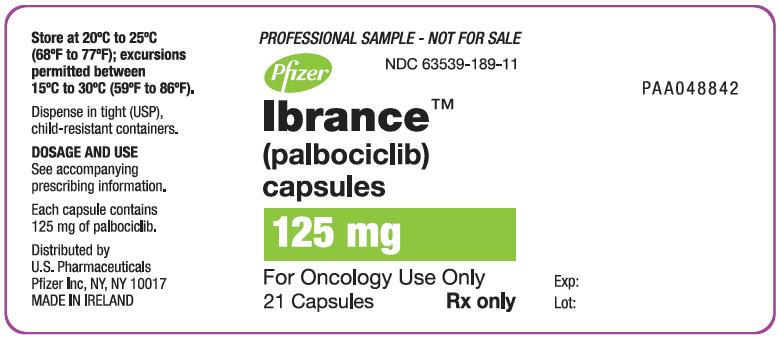
PRINCIPAL DISPLAY PANEL - 125 mg Capsule Bottle Label
PROFESSIONAL SAMPLE - NOT FOR SALE
NDC: 63539-189-11
Pfizer
Ibrance™
(palbociclib)
capsules125 mg
For Oncology Use Only
21 CapsulesRx only
-
PRINCIPAL DISPLAY PANEL - 100 mg Capsule Bottle Label
PROFESSIONAL SAMPLE - NOT FOR SALE
NDC: 63539-188-11
Pfizer
Ibrance®
(palbociclib)
capsules100 mg
21 Capsules
Rx only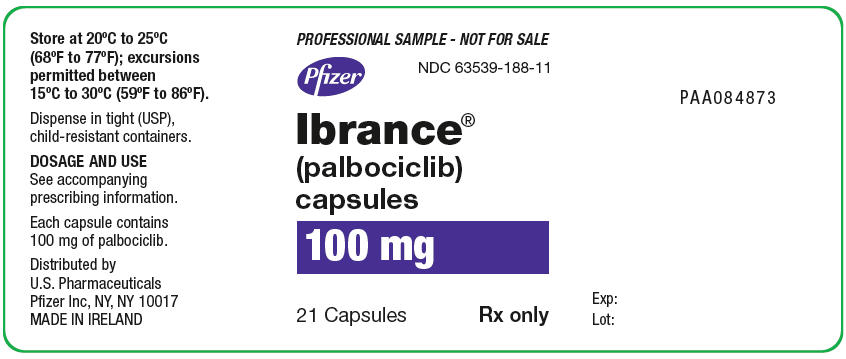
-
PRINCIPAL DISPLAY PANEL - 75 mg Capsule Bottle Label
PROFESSIONAL SAMPLE - NOT FOR SALE
NDC: 63539-187-11
Pfizer
Ibrance®
(palbociclib)
capsules75 mg
21 Capsules
Rx only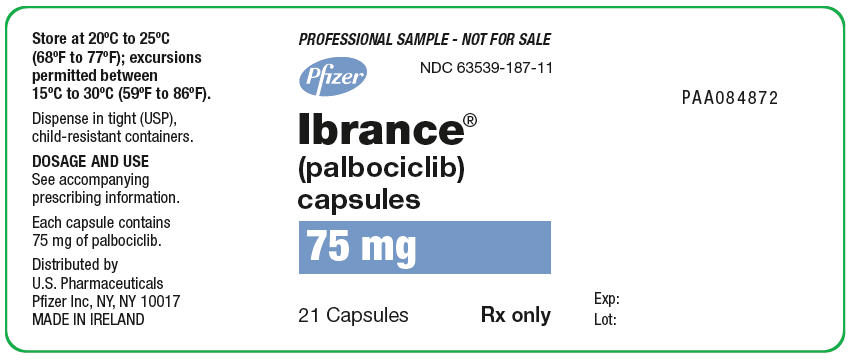
-
INGREDIENTS AND APPEARANCE
IBRANCE
palbociclib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63539-189 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PALBOCICLIB (UNII: G9ZF61LE7G) (PALBOCICLIB - UNII:G9ZF61LE7G) PALBOCICLIB 125 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SHELLAC (UNII: 46N107B71O) AMMONIA (UNII: 5138Q19F1X) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) DIMETHICONE (UNII: 92RU3N3Y1O) Product Characteristics Color BROWN (caramel) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code PBC;125;Pfizer Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63539-189-11 21 in 1 BOTTLE; Type 0: Not a Combination Product 02/03/2015 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA207103 02/03/2015 IBRANCE
palbociclib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63539-188 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PALBOCICLIB (UNII: G9ZF61LE7G) (PALBOCICLIB - UNII:G9ZF61LE7G) PALBOCICLIB 100 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SHELLAC (UNII: 46N107B71O) AMMONIA (UNII: 5138Q19F1X) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) DIMETHICONE (UNII: 92RU3N3Y1O) Product Characteristics Color ORANGE (light orange) , BROWN (caramel) Score no score Shape CAPSULE Size 20mm Flavor Imprint Code PBC;100;Pfizer Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63539-188-11 21 in 1 BOTTLE; Type 0: Not a Combination Product 05/08/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA207103 05/08/2017 IBRANCE
palbociclib capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 63539-187 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PALBOCICLIB (UNII: G9ZF61LE7G) (PALBOCICLIB - UNII:G9ZF61LE7G) PALBOCICLIB 75 mg Inactive Ingredients Ingredient Name Strength MICROCRYSTALLINE CELLULOSE (UNII: OP1R32D61U) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) GELATIN, UNSPECIFIED (UNII: 2G86QN327L) FERRIC OXIDE RED (UNII: 1K09F3G675) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) SHELLAC (UNII: 46N107B71O) AMMONIA (UNII: 5138Q19F1X) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) DIMETHICONE (UNII: 92RU3N3Y1O) Product Characteristics Color ORANGE (light orange) Score no score Shape CAPSULE Size 18mm Flavor Imprint Code PBC;75;Pfizer Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63539-187-11 21 in 1 BOTTLE; Type 0: Not a Combination Product 05/08/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA207103 05/08/2017 Labeler - U.S. Pharmaceuticals (829076905) Establishment Name Address ID/FEI Business Operations Pfizer Pharmaceuticals LLC 829084552 ANALYSIS(63539-187, 63539-188, 63539-189) , PACK(63539-187, 63539-188, 63539-189) Establishment Name Address ID/FEI Business Operations Pharmacia and Upjohn Company LLC 618054084 ANALYSIS(63539-187, 63539-188, 63539-189) , LABEL(63539-187, 63539-188, 63539-189) , PACK(63539-187, 63539-188, 63539-189) Establishment Name Address ID/FEI Business Operations Pfizer Ireland Pharmaceuticals 985104227 API MANUFACTURE(63539-187, 63539-188, 63539-189) Establishment Name Address ID/FEI Business Operations Pfizer Manufacturing Deutschland GmbH 341970073 ANALYSIS(63539-187, 63539-188, 63539-189) , LABEL(63539-187, 63539-188, 63539-189) , MANUFACTURE(63539-187, 63539-188, 63539-189) , PACK(63539-187, 63539-188, 63539-189)
Trademark Results [Ibrance]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 IBRANCE 86314613 4928206 Live/Registered |
Pfizer Inc. 2014-06-19 |
 IBRANCE 85444239 4518147 Live/Registered |
Pfizer Inc. 2011-10-11 |
 IBRANCE 77448185 not registered Dead/Abandoned |
Pfizer Inc. 2008-04-15 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.