FOSPHENYTOIN SODIUM injection
Fosphenytoin Sodium by
Drug Labeling and Warnings
Fosphenytoin Sodium by is a Prescription medication manufactured, distributed, or labeled by Amneal Pharmaceuticals of New York, LLC, Strides Arcolab Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
WARNING: CARDIOVASCULAR RISK ASSOCIATED WITH RAPID INFUSION RATES The rate of intravenous fosphenytoin administration should not exceed 150 mg phenytoin sodium equivalents (PE) per minute because of the risk of severe hypotension and cardiac arrhythmias. Careful cardiac monitoring is needed during and after administering intravenous fosphenytoin. Although the risk of cardiovascular toxicity increases with infusion rates above the recommended infusion rate, these events have also been reported at or below the recommended infusion rate. Reduction in rate of administration or discontinuation of dosing may be needed (see WARNINGS and DOSAGE AND ADMINISTRATION).
-
DESCRIPTION
Fosphenytoin sodium injection, USP is a prodrug intended for parenteral administration; its active metabolite is phenytoin. 1.5 mg fosphenytoin sodium, USP (hereafter referred to as fosphenytoin) equivalent to 1 mg phenytoin sodium and is referred to as 1 mg phenytoin equivalents (PE). The amount and concentration of fosphenytoin is always expressed in terms of mg PE.
Fosphenytoin injection is marketed in 2 mL vials containing a total of 100 mg PE and 10 mL vials containing a total of 500 mg PE. The concentration of each vial is 50 mg PE/mL. Fosphenytoin is supplied in vials as a ready-mixed solution in Water for Injection, USP, and Tromethamine, USP (TRIS), buffer adjusted to pH 8.6 to 9.0 with either Hydrochloric Acid, NF, or Sodium Hydroxide, NF. Fosphenytoin injection is a clear, colorless to pale yellow, sterile solution.
The chemical name of fosphenytoin is 5,5-diphenyl-3-[(phosphonooxy)methyl]-2,4-imidazolidinedione disodium salt.
The molecular structure of fosphenytoin is:
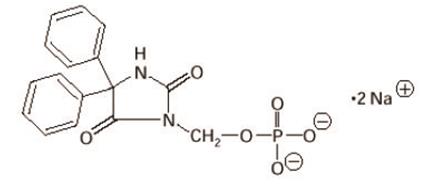
The molecular weight of fosphenytoin is 406.24.
IMPORTANT NOTE: Throughout all fosphenytoin injection product labeling, the amount and concentration of fosphenytoin are always expressed in terms of phenytoin sodium equivalents (PE). Fosphenytoin’s weight is expressed as phenytoin sodium equivalents to avoid the need to perform molecular weight-based adjustments when substituting fosphenytoin for phenytoin or vice versa.
Care should be taken to ensure that fosphenytoin is always prescribed and dispensed in phenytoin sodium equivalents (PE) (see DOSAGE AND ADMINISTRATION).
-
CLINICAL PHARMACOLOGY
Introduction
Following parenteral administration of fosphenytoin injection, fosphenytoin is converted to the anticonvulsant phenytoin. For every mmol of fosphenytoin administered, one mmol of phenytoin is produced. The pharmacological and toxicological effects of fosphenytoin include those of phenytoin. However, the hydrolysis of fosphenytoin to phenytoin yields two metabolites, phosphate and formaldehyde. Formaldehyde is subsequently converted to formate, which is in turn metabolized via a folate dependent mechanism. Although phosphate and formaldehyde (formate) have potentially important biological effects, these effects typically occur at concentrations considerably in excess of those obtained when fosphenytoin is administered under conditions of use recommended in this labeling.
Mechanism of Action
Fosphenytoin is a prodrug of phenytoin and accordingly, its anticonvulsant effects are attributable to phenytoin.
After IV administration to mice, fosphenytoin blocked the tonic phase of maximal electroshock seizures at doses equivalent to those effective for phenytoin. In addition to its ability to suppress maximal electroshock seizures in mice and rats, phenytoin exhibits anticonvulsant activity against kindled seizures in rats, audiogenic seizures in mice, and seizures produced by electrical stimulation of the brainstem in rats. The cellular mechanisms of phenytoin thought to be responsible for its anticonvulsant actions include modulation of voltage-dependent sodium channels of neurons, inhibition of calcium flux across neuronal membranes, modulation of voltage-dependent calcium channels of neurons, and enhancement of the sodium-potassium ATPase activity of neurons and glial cells. The modulation of sodium channels may be a primary anticonvulsant mechanism because this property is shared with several other anticonvulsants in addition to phenytoin.
Pharmacokinetics and Drug Metabolism
Fosphenytoin
Absorption/Bioavailability:
Intravenous: When fosphenytoin is administered by IV infusion, maximum plasma fosphenytoin concentrations are achieved at the end of the infusion. Fosphenytoin has a half-life of approximately 15 minutes.
Intramuscular: Fosphenytoin is completely bioavailable following IM administration of fosphenytoin. Peak concentrations occur at approximately 30 minutes postdose. Plasma fosphenytoin concentrations following IM administration are lower but more sustained than those following IV administration due to the time required for absorption of fosphenytoin from the injection site.
Distribution: Fosphenytoin is extensively bound (95% to 99%) to human plasma proteins, primarily albumin. Binding to plasma proteins is saturable with the result that the percent bound decreases as total fosphenytoin concentrations increase. Fosphenytoin displaces phenytoin from protein binding sites. The volume of distribution of fosphenytoin increases with fosphenytoin dose and rate, and ranges from 4.3 to 10.8 liters.
Metabolism and Elimination: The conversion half-life of fosphenytoin to phenytoin is approximately 15 minutes. The mechanism of fosphenytoin conversion has not been determined, but phosphatases probably play a major role. Fosphenytoin is not excreted in urine. Each mmol of fosphenytoin is metabolized to 1 mmol of phenytoin, phosphate, and formate (see CLINICAL PHARMACOLOGY, Introduction and PRECAUTIONS, Phosphate Load for Renally Impaired Patients).
Phenytoin (after fosphenytoin administration)
In general, IM administration of fosphenytoin generates systemic phenytoin concentrations that are similar enough to oral phenytoin sodium to allow essentially interchangeable use.
The pharmacokinetics of fosphenytoin following IV administration of fosphenytoin, however, are complex, and when used in an emergency setting (e.g., status epilepticus), differences in rate of availability of phenytoin could be critical. Studies have therefore empirically determined an infusion rate for fosphenytoin that gives a rate and extent of phenytoin systemic availability similar to that of a 50 mg/min phenytoin sodium infusion.
A dose of 15 to 20 mg PE/kg of fosphenytoin infused at 100 to 150 mg PE/min yields plasma free phenytoin concentrations over time that approximate those achieved when an equivalent dose of phenytoin sodium (e.g., parenteral phenytoin sodium) is administered at 50 mg/min (see DOSAGE AND ADMINISTRATION and WARNINGS).
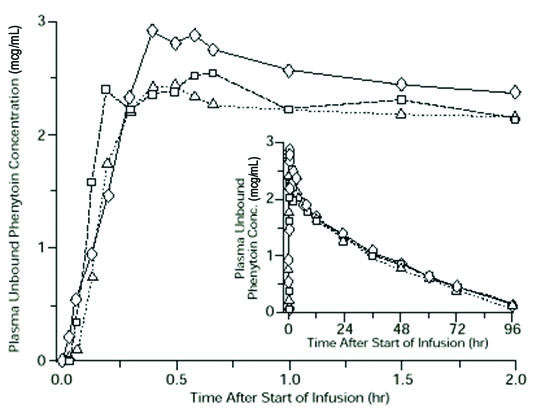
FIGURE 1. Mean plasma unbound phenytoin concentrations following IV administration of 1200 mg PE fosphenytoin infused at 100 mg PE/min (triangles) or 150 mg PE/min (squares) and 1200 mg phenytoin sodium infused at 50 mg/min (diamonds) to healthy subjects (N = 12). Inset shows time course for the entire 96-hour sampling period.
Following administration of single IV fosphenytoin doses of 400 to 1200 mg PE, mean maximum total phenytoin concentrations increase in proportion to dose, but do not change appreciably with changes in infusion rate. In contrast, mean maximum unbound phenytoin concentrations increase with both dose and rate.
Absorption/Bioavailability: Fosphenytoin is completely converted to phenytoin following IV administration, with a half-life of approximately 15 minutes. Fosphenytoin is also completely converted to phenytoin following IM administration and plasma total phenytoin concentrations peak in approximately 3 hours.
Distribution: Phenytoin is highly bound to plasma proteins, primarily albumin, although to a lesser extent than fosphenytoin. In the absence of fosphenytoin, approximately 12% of total plasma phenytoin is unbound over the clinically relevant concentration range. However, fosphenytoin displaces phenytoin from plasma protein binding sites. This increases the fraction of phenytoin unbound (up to 30% unbound) during the period required for conversion of fosphenytoin to phenytoin (approximately 0.5 to 1 hour post infusion).
Metabolism and Elimination: Phenytoin derived from administration of fosphenytoin is extensively metabolized in the liver and excreted in urine primarily as 5-(p-hydroxyphenyl)-5-phenylhydantoin and its glucuronide; little unchanged phenytoin (1% to 5% of the fosphenytoin dose) is recovered in urine. Phenytoin is metabolized by the cytochrome P450 enzymes CYP2C9 and CYP2C19. Phenytoin hepatic metabolism is saturable, and following administration of single IV fosphenytoin doses of 400 to 1200 mg PE, total and unbound phenytoin AUC values increase disproportionately with dose. Mean total phenytoin half-life values (12 to 28.9 hr) following fosphenytoin injection administration at these doses are similar to those after equal doses of parenteral phenytoin sodium and tend to be greater at higher plasma phenytoin concentrations.
Special Populations
Patients with Renal or Hepatic Disease: Due to an increased fraction of unbound phenytoin in patients with renal or hepatic disease, or in those with hypoalbuminemia, the interpretation of total phenytoin plasma concentrations should be made with caution (see DOSAGE AND ADMINISTRATION). Unbound phenytoin concentrations may be more useful in these patient populations. After IV administration of fosphenytoin to patients with renal and/or hepatic disease, or in those with hypoalbuminemia, fosphenytoin clearance to phenytoin may be increased without a similar increase in phenytoin clearance. This has the potential to increase the frequency and severity of adverse events (see PRECAUTIONS).
Age: The effect of age was evaluated in patients 5 to 98 years of age. Patient age had no significant impact on fosphenytoin pharmacokinetics. Phenytoin clearance tends to decrease with increasing age (20% less in patients over 70 years of age relative to that in patients 20 to 30 years of age). Phenytoin dosing requirements are highly variable and must be individualized (see DOSAGE AND ADMINISTRATION).
Gender and Race: Gender and race have no significant impact on fosphenytoin or phenytoin pharmacokinetics.
Pediatrics: The safety and efficacy of fosphenytoin in pediatric patients have not been established.
Clinical Studies
Infusion tolerance was evaluated in clinical studies. One double-blind study assessed infusion-site tolerance of equivalent loading doses (15 to 20 mg PE/kg) of fosphenytoin infused at 150 mg PE/min or phenytoin infused at 50 mg/min. The study demonstrated better local tolerance (pain and burning at the infusion site), fewer disruptions of the infusion, and a shorter infusion period for fosphenytoin-treated patients (Table 1).
TABLE 1. Infusion Tolerance of Equivalent Loading Doses of IV Fosphenytoin and IV Phenytoin IV Fosphenytoin
N=90IV Phenytoin
N=22Local Intolerance 9%a 90% Infusion Disrupted 21% 67% Average Infusion Time 13 min 44 min a Percent of patients Fosphenytoin-treated patients, however, experienced more systemic sensory disturbances (see PRECAUTIONS, Sensory Disturbances).
Infusion disruptions in fosphenytoin-treated patients were primarily due to systemic burning, pruritus, and/or paresthesia while those in phenytoin-treated patients were primarily due to pain and burning at the infusion site (see Table 1).
In a double-blind study investigating temporary substitution of fosphenytoin for oral phenytoin, IM fosphenytoin was as well-tolerated as IM placebo. IM fosphenytoin resulted in a slight increase in transient, mild to moderate local itching (23% of patients vs 11% of IM placebo-treated patients at any time during the study). This study also demonstrated that equimolar doses of IM fosphenytoin may be substituted for oral phenytoin sodium with no dosage adjustments needed when initiating IM or returning to oral therapy. In contrast, switching between IM and oral phenytoin requires dosage adjustments because of slow and erratic phenytoin absorption from muscle.
-
INDICATIONS AND USAGE
Fosphenytoin sodium injection, USP is indicated for the control of generalized tonic-clonic status epilepticus and prevention and treatment of seizures occurring during neurosurgery. Fosphenytoin can also be substituted, short-term, for oral phenytoin. Fosphenytoin should be used only when oral phenytoin administration is not possible. Fosphenytoin must not be given orally.
-
CONTRAINDICATIONS
Fosphenytoin sodium injection, USP is contraindicated in patients who have demonstrated hypersensitivity to fosphenytoin sodium injection, USP or its ingredients, or to phenytoin or other hydantoins.
Because of the effect of parenteral phenytoin on ventricular automaticity, fosphenytoin injection is contraindicated in patients with sinus bradycardia, sino-atrial block, second and third degree A-V block, and Adams-Stokes syndrome.
Coadministration of fosphenytoin is contraindicated with delavirdine due to potential for loss of virologic response and possible resistance to delavirdine or to the class of non-nucleoside reverse transcriptase inhibitors.
-
WARNINGS
DOSES OF FOSPHENYTOIN ARE ALWAYS EXPRESSED IN TERMS OF MILLIGRAMS OF PHENYTOIN SODIUM EQUIVALENTS (mg PE). 1 mg PE IS EQUIVALENT TO 1 mg PHENYTOIN SODIUM.
DO NOT, THEREFORE, MAKE ANY ADJUSTMENT IN THE RECOMMENDED DOSES WHEN SUBSTITUTING FOSPHENYTOIN FOR PHENYTOIN SODIUM OR VICE VERSA. FOR EXAMPLE, IF A PATIENT IS RECEIVING 1000 mg PE OF FOSPHENYTOIN, THAT IS EQUIVALENT TO 1000 mg OF PHENYTOIN SODIUM.
The following warnings are based on experience with fosphenytoin or phenytoin.
Dosing Errors
Do not confuse the amount of drug to be given in PE with the concentration of the drug in the vial.
Medication errors associated with fosphenytoin have resulted in patients receiving the wrong dose of fosphenytoin. Fosphenytoin is marketed in 2 mL vials containing a total of 100 mg PE and 10 mL vials containing a total of 500 mg PE. The concentration of each vial is 50 mg PE/mL. Errors have occurred when the concentration of the vial (50 mg PE/mL) was misinterpreted to mean that the total content of the vial was 50 mg PE. These errors have resulted in two- or ten-fold overdoses of fosphenytoin since each vial actually contains a total of 100 mg PE or 500 mg PE. In some cases, ten-fold overdoses were associated with fatal outcomes. To help minimize confusion, the prescribed dose of fosphenytoin should always be expressed in milligrams of phenytoin equivalents (mg PE) (see DOSAGE AND ADMINISTRATION). Additionally, when ordering and storing fosphenytoin, consider displaying the total drug content (i.e., 100 mg PE/2 mL or 500 mg PE/10 mL) instead of concentration in computer systems, pre-printed orders, and automated dispensing cabinet databases to help ensure that total drug content can be clearly identified. Care should be taken to ensure the appropriate volume of fosphenytoin is withdrawn from the vial when preparing the drug for administration. Attention to these details may prevent some fosphenytoin medication errors from occurring.
Status Epilepticus Dosing Regimen
Because of the increased risk of adverse cardiovascular reactions associated with rapid administration, do not administer fosphenytoin at a rate greater than 150 mg PE/min.
The dose of IV fosphenytoin (15 to 20 mg PE/kg) that is used to treat status epilepticus is administered at a maximum rate of 150 mg PE/min. The typical fosphenytoin infusion administered to a 50 kg patient would take between 5 and 7 minutes. Note that the delivery of an identical molar dose of phenytoin using parenteral phenytoin sodium or generic phenytoin sodium injection cannot be accomplished in less than 15 to 20 minutes because of the untoward cardiovascular effects that accompany the direct intravenous administration of phenytoin at rates greater than 50 mg/min.
If rapid phenytoin loading is a primary goal, IV administration of fosphenytoin is preferred because the time to achieve therapeutic plasma phenytoin concentrations is greater following IM than that following IV administration (see DOSAGE AND ADMINISTRATION).
Cardiovascular Risk Associated with Rapid Infusion
As non-emergency therapy, intravenous fosphenytoin should be administered more slowly. Because of the risks of cardiac and local toxicity associated with IV fosphenytoin, oral phenytoin should be used whenever possible.
Because adverse cardiovascular reactions have occurred during and after infusions, careful cardiac monitoring is needed during and after the administration of intravenous fosphenytoin. Reduction in rate of administration or discontinuation of dosing may be needed.
Adverse cardiovascular reactions include severe hypotension and cardiac arrhythmias. Cardiac arrhythmias have included bradycardia, heart block, QT interval prolongation, ventricular tachycardia, and ventricular fibrillation which have resulted in asystole, cardiac arrest, and death. Severe complications are most commonly encountered in critically ill patients, elderly patients, and patients with hypotension and severe myocardial insufficiency. However, cardiac events have also been reported in adults and children without underlying cardiac disease or comorbidities and at recommended doses and infusion rates.
Withdrawal Precipitated Seizure, Status Epilepticus
Antiepileptic drugs should not be abruptly discontinued because of the possibility of increased seizure frequency, including status epilepticus. When, in the judgment of the clinician, the need for dosage reduction, discontinuation, or substitution of alternative antiepileptic medication arises, this should be done gradually. However, in the event of an allergic or hypersensitivity reaction, rapid substitution of alternative therapy may be necessary. In this case, alternative therapy should be an antiepileptic drug not belonging to the hydantoin chemical class.
Serious Dermatologic Reactions
Serious and sometimes fatal dermatologic reactions, including toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS), have been reported with phenytoin treatment. The onset of symptoms is usually within 28 days, but can occur later. Fosphenytoin should be discontinued at the first sign of a rash, unless the rash is clearly not drug-related. If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered. If a rash occurs, the patient should be evaluated for signs and symptoms of Drug Reaction with Eosinophilia and Systemic Symptoms (see DRESS/Multiorgan Hypersensitivity below).
Studies in patients of Chinese ancestry have found a strong association between the risk of developing SJS/TEN and the presence of HLA-B*1502, an inherited allelic variant of the HLA B gene, in patients using carbamazepine. Limited evidence suggests that HLA-B*1502 may be a risk factor for the development of SJS/TEN in patients of Asian ancestry taking other antiepileptic drugs associated with SJS/TEN, including phenytoin. Consideration should be given to avoiding fosphenytoin as an alternative for carbamazepine patients positive for HLA-B*1502.
The use of HLA-B*1502 genotyping has important limitations and must never substitute for appropriate clinical vigilance and patient management. The role of other possible factors in the development of, and morbidity from, SJS/TEN, such as antiepileptic drug (AED) dose, compliance, concomitant medications, comorbidities, and the level of dermatologic monitoring have not been studied.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as Multiorgan hypersensitivity, has been reported in patients taking antiepileptic drugs, including phenytoin and fosphenytoin. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, and/or lymphadenopathy, in association with other organ system involvement, such as hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its expression, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. Fosphenytoin should be discontinued if an alternative etiology for the signs or symptoms cannot be established.
Hypersensitivity
Fosphenytoin and other hydantoins are contraindicated in patients who have experienced phenytoin hypersensitivity (see CONTRAINDICATIONS). Additionally, consider alternatives to structurally similar drugs such as carboxamides (e.g., carbamazepine), barbiturates, succinimides, and oxazolidinediones (e.g., trimethadione) in these same patients. Similarly, if there is a history of hypersensitivity reactions to these structurally similar drugs in the patient or immediate family members, consider alternatives to fosphenytoin.
Hepatic Injury
Cases of acute hepatotoxicity, including infrequent cases of acute hepatic failure, have been reported with phenytoin. These events may be part of the spectrum of DRESS or may occur in isolation. Other common manifestations include jaundice, hepatomegaly, elevated serum transaminase levels, leukocytosis, and eosinophilia. The clinical course of acute phenytoin hepatotoxicity ranges from prompt recovery to fatal outcomes. In these patients with acute hepatotoxicity, fosphenytoin should be immediately discontinued and not readministered.
Hematopoietic System
Hematopoietic complications, some fatal, have occasionally been reported in association with administration of phenytoin. These have included thrombocytopenia, leukopenia, granulocytopenia, agranulocytosis, and pancytopenia with or without bone marrow suppression.
There have been a number of reports that have suggested a relationship between phenytoin and the development of lymphadenopathy (local or generalized), including benign lymph node hyperplasia, pseudolymphoma, lymphoma, and Hodgkin’s disease. Although a cause and effect relationship has not been established, the occurrence of lymphadenopathy indicates the need to differentiate such a condition from other types of lymph node pathology. Lymph node involvement may occur with or without symptoms and signs resembling DRESS. In all cases of lymphadenopathy, follow-up observation for an extended period is indicated and every effort should be made to achieve seizure control using alternative antiepileptic drugs.
Alcohol Use
Acute alcohol intake may increase plasma phenytoin concentrations while chronic alcohol use may decrease plasma concentrations.
Usage in Pregnancy
Clinical
Risks to Mother
An increase in seizure frequency may occur during pregnancy because of altered phenytoin pharmacokinetics. Periodic measurement of plasma phenytoin concentrations may be valuable in the management of pregnant women as a guide to appropriate adjustment of dosage (see PRECAUTIONS, Laboratory Tests). However, postpartum restoration of the original dosage will probably be indicated.
Risks to the Fetus
If this drug is used during pregnancy, or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential harm to the fetus.
Prenatal exposure to phenytoin may increase the risks for congenital malformations and other adverse developmental outcomes. Increased frequencies of major malformations (such as orofacial clefts and cardiac defects), minor anomalies (dysmorphic facial features, nail and digit hypoplasia), growth abnormalities (including microcephaly), and mental deficiency have been reported among children born to epileptic women who took phenytoin alone or in combination with other antiepileptic drugs during pregnancy. There have also been several reported cases of malignancies, including neuroblastoma, in children whose mothers received phenytoin during pregnancy. The overall incidence of malformations for children of epileptic women treated with antiepileptic drugs (phenytoin and/or others) during pregnancy is about 10%, or two-to three-fold that in the general population. However, the relative contributions of antiepileptic drugs and other factors associated with epilepsy to this increased risk are uncertain and in most cases it has not been possible to attribute specific developmental abnormalities to particular antiepileptic drugs. Patients should consult with their physicians to weigh the risks and benefits of phenytoin during pregnancy.
Postpartum Period
A potentially life-threatening bleeding disorder related to decreased levels of vitamin K-dependent clotting factors may occur in newborns exposed to phenytoin in utero. This drug-induced condition can be prevented with vitamin K administration to the mother before delivery and to the neonate after birth.
Nonclinical
Administration of phenytoin to pregnant animals resulted in teratogenicity (increased incidences of fetal malformations) and other developmental toxicity (including embryofetal death, growth impairment, and behavioral abnormalities) in multiple animal species at clinically relevant doses.
-
PRECAUTIONS
General: (Fosphenytoin specific)
Sensory Disturbances
Severe burning, itching, and/or paresthesia were reported by 7 of 16 normal volunteers administered IV fosphenytoin at a dose of 1200 mg PE at the maximum rate of administration (150 mg PE/min). The severe sensory disturbance lasted from 3 to 50 minutes in 6 of these subjects and for 14 hours in the seventh subject. In some cases, milder sensory disturbances persisted for as long as 24 hours. The location of the discomfort varied among subjects with the groin mentioned most frequently as an area of discomfort. In a separate cohort of 16 normal volunteers (taken from 2 other studies) who were administered IV fosphenytoin at a dose of 1200 mg PE at the maximum rate of administration (150 mg PE/min), none experienced severe disturbances, but most experienced mild to moderate itching or tingling.
Patients administered fosphenytoin at doses of 20 mg PE/kg at 150 mg PE/min are expected to experience discomfort of some degree. The occurrence and intensity of the discomfort can be lessened by slowing or temporarily stopping the infusion.
The effect of continuing infusion unaltered in the presence of these sensations is unknown. No permanent sequelae have been reported thus far. The pharmacologic basis for these positive sensory phenomena is unknown, but other phosphate ester drugs, which deliver smaller phosphate loads, have been associated with burning, itching, and/or tingling predominantly in the groin area.
Local Toxicity (Purple Glove Syndrome)
Edema, discoloration, and pain distal to the site of injection (described as “purple glove syndrome”) have also been reported following peripheral intravenous fosphenytoin injection. This may or may not be associated with extravasation. The syndrome may not develop for several days after injection.
Phosphate Load
The phosphate load provided by fosphenytoin (0.0037 mmol phosphate/mg PE fosphenytoin) should be considered when treating patients who require phosphate restriction, such as those with severe renal impairment.
IV Loading in Renal and/or Hepatic Disease or in Those with Hypoalbuminemia
After IV administration to patients with renal and/or hepatic disease, or in those with hypoalbuminemia, fosphenytoin clearance to phenytoin may be increased without a similar increase in phenytoin clearance. This has the potential to increase the frequency and severity of adverse events (see CLINICAL PHARMACOLOGY, Special Populations and DOSAGE AND ADMINISTRATION, Dosing in Special Populations).
General: (phenytoin associated)
Fosphenytoin is not indicated for the treatment of absence seizures.
A small percentage of individuals who have been treated with phenytoin have been shown to metabolize the drug slowly. Slow metabolism may be due to limited enzyme availability and lack of induction; it appears to be genetically determined.
Phenytoin has been infrequently associated with the exacerbation of porphyria. Caution should be exercised when fosphenytoin is used in patients with this disease.
Hyperglycemia, resulting from phenytoin’s inhibitory effect on insulin release, has been reported. Phenytoin may also raise the serum glucose concentrations in diabetic patients.
Plasma concentrations of phenytoin sustained above the optimal range may produce confusional states referred to as “delirium,” “psychosis,” or “encephalopathy,” or rarely, irreversible cerebellar dysfunction. Accordingly, at the first sign of acute toxicity, determination of plasma phenytoin concentrations is recommended (see PRECAUTIONS, Laboratory Tests). Fosphenytoin dose reduction is indicated if phenytoin concentrations are excessive; if symptoms persist, administration of fosphenytoin should be discontinued.
The liver is the primary site of biotransformation of phenytoin; patients with impaired liver function, elderly patients, or those who are gravely ill may show early signs of toxicity.
Phenytoin and other hydantoins are not indicated for seizures due to hypoglycemic or other metabolic causes. Appropriate diagnostic procedures should be performed as indicated.
Phenytoin has the potential to lower serum folate levels.
Laboratory Tests
Phenytoin doses are usually selected to attain therapeutic plasma total phenytoin concentrations of 10 to 20 mcg/mL, (unbound phenytoin concentrations of 1 to 2 mcg/mL). Following fosphenytoin administration, it is recommended that phenytoin concentrations not be monitored until conversion to phenytoin is essentially complete. This occurs within approximately 2 hours after the end of IV infusion and 4 hours after IM injection.
Prior to complete conversion, commonly used immunoanalytical techniques, such as TDx®/TDxFLxTM (fluorescence polarization) and Emit® 2000 (enzyme multiplied), may significantly overestimate plasma phenytoin concentrations because of cross-reactivity with fosphenytoin. The error is dependent on plasma phenytoin and fosphenytoin concentration (influenced by fosphenytoin dose, route and rate of administration, and time of sampling relative to dosing), and analytical method. Chromatographic assay methods accurately quantitate phenytoin concentrations in biological fluids in the presence of fosphenytoin. Prior to complete conversion, blood samples for phenytoin monitoring should be collected in tubes containing EDTA as an anticoagulant to minimize ex vivo conversion of fosphenytoin to phenytoin. However, even with specific assay methods, phenytoin concentrations measured before conversion of fosphenytoin is complete will not reflect phenytoin concentrations ultimately achieved.
Drug Interactions
No drugs are known to interfere with the conversion of fosphenytoin to phenytoin. Conversion could be affected by alterations in the level of phosphatase activity, but given the abundance and wide distribution of phosphatases in the body it is unlikely that drugs would affect this activity enough to affect conversion of fosphenytoin to phenytoin. Drugs highly bound to albumin could increase the unbound fraction of fosphenytoin. Although, it is unknown whether this could result in clinically significant effects, caution is advised when administering fosphenytoin with other drugs that significantly bind to serum albumin.
The pharmacokinetics and protein binding of fosphenytoin, phenytoin, and diazepam were not altered when diazepam and fosphenytoin were concurrently administered in single submaximal doses.
The most significant drug interactions following administration of fosphenytoin are expected to occur with drugs that interact with phenytoin. Phenytoin is extensively bound to serum plasma proteins and is prone to competitive displacement. Phenytoin is metabolized by hepatic cytochrome P450 enzymes CYP2C9 and CYP2C19 and is particularly susceptible to inhibitory drug interactions because it is subject to saturable metabolism. Inhibition of metabolism may produce significant increases in circulating phenytoin concentrations and enhance the risk of drug toxicity. Phenytoin is a potent inducer of hepatic drug-metabolizing enzymes.
The most commonly occurring drug interactions are listed below:
Note: The list is not intended to be inclusive or comprehensive. Individual drug package inserts should be consulted.
Drugs that affect phenytoin concentrations:
- Drugs that may increase plasma phenytoin concentrations include: acute alcohol intake, amiodarone, anti-epileptic agents (ethosuximide, felbamate, oxcarbazepine, methsuximide, topiramate), azoles (fluconazole, ketoconazole, itraconazole, miconazole, voriconazole), capecitabine, chloramphenicol, chlordiazepoxide, disulfiram, estrogens, fluorouracil, fluoxetine, fluvastatin, fluvoxamine, H2-antagonists (e.g. cimetidine), halothane, isoniazid, methylphenidate, omeprazole, phenothiazines, salicylates, sertraline, succinimides, sulfonamides (e.g., sulfamethizole, sulfaphenazole, sulfadiazine, sulfamethoxazole-trimethoprim), tacrolimus, ticlopidine, tolbutamide, trazodone and warfarin.
- Drugs that may decrease plasma phenytoin concentrations include: anticancer drugs usually in combination (e.g., bleomycin, carboplatin, cisplatin, doxorubicin, methotrexate), carbamazepine, chronic alcohol abuse, diazepam, diazoxide, folic acid, fosamprenavir, nelfinavir, reserpine, rifampin, ritonavir, St. John’s Wort, theophylline and vigabatrin.
- Drugs that may either increase or decrease plasma phenytoin concentrations include: phenobarbital, valproic acid and sodium valproate. Similarly, the effects of phenytoin on phenobarbital, valproic acid and sodium plasma valproate concentrations are unpredictable.
- The addition or withdrawal of these agents in patients on phenytoin therapy may require an adjustment of the phenytoin dose to achieve optimal clinical outcome.
Drugs affected by phenytoin:
- Drugs that should not be coadministered with phenytoin: Delavirdine (see CONTRAINDICATIONS).
- Drugs whose efficacy is impaired by phenytoin include: azoles (fluconazole, ketoconazole, itraconazole, voriconazole, posaconazole), corticosteroids, doxycycline, estrogens, furosemide, irinotecan, oral contraceptives, paclitaxel, paroxetine, quinidine, rifampin, sertraline, teniposide, theophylline and vitamin D.
- Increased and decreased PT/INR responses have been reported when phenytoin is coadministered with warfarin.
- Phenytoin decreases plasma concentrations of active metabolites of albendazole, certain HIV antivirals (efavirenz, lopinavir/ritonavir, indinavir, nelfinavir, ritonavir, saquinavir), anti-epileptic agents (carbamazepine, felbamate, lamotrigine, topiramate, oxcarbazepine, quetiapine), atorvastatin, chlorpropamide, clozapine, cyclosporine, digoxin, fluvastatin, folic acid, methadone, mexiletine, nifedipine, nimodipine, nisoldipine, praziquantel, simvastatin and verapamil.
- Phenytoin when given with fosamprenavir alone may decrease the concentration of amprenavir, the active metabolite. Phenytoin when given with the combination of fosamprenavir and ritonavir may increase the concentration of amprenavir.
- Resistance to the neuromuscular blocking action of the nondepolarizing neuromuscular blocking agents pancuronium, vecuronium, rocuronium and cisatracurium has occurred in patients chronically administered phenytoin. Whether or not phenytoin has the same effect on other non-depolarizing agents is unknown. Patients should be monitored closely for more rapid recovery from neuromuscular blockade than expected, and infusion rate requirements may be higher.
- The addition or withdrawal of phenytoin during concomitant therapy with these agents may require adjustment of the dose of these agents to achieve optimal clinical outcome.
Monitoring of plasma phenytoin concentrations may be helpful when possible drug interactions are suspected (see Laboratory Tests).
Drug/Laboratory Test Interactions
Phenytoin may decrease serum concentrations of T4. It may also produce artifactually low results in dexamethasone or metyrapone tests. Phenytoin may also cause increased serum concentrations of glucose, alkaline phosphatase, and gamma glutamyl transpeptidase (GGT). Care should be taken when using immunoanalytical methods to measure plasma concentrations following fosphenytoin administration (see Laboratory Tests).
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: See WARNINGS (Hematopoietic System) section
The carcinogenic potential of fosphenytoin has not been assessed. In 2-year carcinogenicity studies, phenytoin (active metabolite of fosphenytoin) was administered in the diet at doses of 0, 10, 25, or 45 mg/kg/day (mice) and 0, 25, 50, or 100 mg/kg/day (rats). In mice, hepatocellular tumors were increased in males and females at the highest dose tested. No drug-related increase in tumors was observed in rats. The peak phenytoin levels at the highest doses tested were lower than those in humans at therapeutic concentrations.
In published 2-year carcinogenicity studies, phenytoin was administered in the diet at up to 600 ppm (approximately 90 mg/kg/day) to mice and up to 2400 ppm (approximately 120 mg/kg/day) to rats. The incidence of hepatocellular tumors was increased in mice. No drug-related increase in tumors was observed in rats.
Mutagenesis
An increase in structural chromosome aberrations were observed in cultured V79 Chinese hamster lung cells exposed to fosphenytoin in the presence of metabolic activation. No evidence of mutagenicity was observed in bacteria (Ames test) or Chinese hamster lung cells in vitro, and no evidence for clastogenic activity was observed in an in vivo mouse bone marrow micronucleus assay.
Fertility
Fosphenytoin was administered to male and female rats during mating and continuing in females throughout gestation and lactation at doses of 50 mg PE/kg or higher. No effects on fertility were observed in males. In females, altered estrous cycles, delayed mating, prolonged gestation length, and developmental toxicity were observed at all doses, which were associated with maternal toxicity. The lowest dose tested is approximately 40% of the maximum human loading dose on a mg/m2 basis.
Pregnancy - Category D:
(see WARNINGS)
Use in Nursing Mothers
It is not known whether fosphenytoin is excreted in human milk.
Following administration of phenytoin sodium, phenytoin appears to be excreted in low concentrations in human milk. Therefore, breast-feeding is not recommended for women receiving fosphenytoin.
Pediatric Use
Safety and effectiveness of fosphenytoin in pediatric patients has not been established.
Geriatric Use
No systematic studies in geriatric patients have been conducted. Phenytoin clearance tends to decrease with increasing age (see CLINICAL PHARMACOLOGY, Special Populations).
-
ADVERSE REACTIONS
The more important adverse clinical events caused by the IV use of fosphenytoin or phenytoin are cardiovascular collapse and/or central nervous system depression. Hypotension can occur when either drug is administered rapidly by the IV route. The rate of administration is very important; for fosphenytoin, it should not exceed 150 mg PE/min.
The adverse clinical events most commonly observed with the use of fosphenytoin in clinical trials were nystagmus, dizziness, pruritus, paresthesia, headache, somnolence, and ataxia. With two exceptions, these events are commonly associated with the administration of IV phenytoin. Paresthesia and pruritus, however, were seen much more often following fosphenytoin administration and occurred more often with IV fosphenytoin administration than with IM fosphenytoin administration. These events were dose and rate related; most alert patients (41 of 64; 64%) administered doses of ≥15 mg PE/kg at 150 mg PE/min experienced discomfort of some degree. These sensations, generally described as itching, burning, or tingling, were usually not at the infusion site. The location of the discomfort varied with the groin mentioned most frequently as a site of involvement. The paresthesia and pruritus were transient events that occurred within several minutes of the start of infusion and generally resolved within 10 minutes after completion of fosphenytoin infusion. Some patients experienced symptoms for hours. These events did not increase in severity with repeated administration. Concurrent adverse events or clinical laboratory change suggesting an allergic process were not seen (see PRECAUTIONS, Sensory Disturbances).
Approximately 2% of the 859 individuals who received fosphenytoin in premarketing clinical trials discontinued treatment because of an adverse event. The adverse events most commonly associated with withdrawal were pruritus (0.5%), hypotension (0.3%), and bradycardia (0.2%).
Dose and Rate Dependency of Adverse Events Following IV Fosphenytoin:
The incidence of adverse events tended to increase as both dose and infusion rate increased. In particular, at doses of ≥15 mg PE/kg and rates ≥150 mg PE/min, transient pruritus, tinnitus, nystagmus, somnolence, and ataxia occurred 2 to 3 times more often than at lower doses or rates.
Incidence in Controlled Clinical Trials
All adverse events were recorded during the trials by the clinical investigators using terminology of their own choosing. Similar types of events were grouped into standardized categories using modified COSTART dictionary terminology. These categories are used in the tables and listings below with the frequencies representing the proportion of individuals exposed to fosphenytoin or comparative therapy.
The prescriber should be aware that these figures cannot be used to predict the frequency of adverse events in the course of usual medical practice where patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with figures obtained from other clinical investigations involving different treatments, uses or investigators. An inspection of these frequencies, however, does provide the prescribing physician with one basis to estimate the relative contribution of drug and nondrug factors to the adverse event incidences in the population studied.
Incidence in Controlled Clinical Trials - IV Administration To Patients With Epilepsy or Neurosurgical Patients: Table 2 lists treatment-emergent adverse events that occurred in at least 2% of patients treated with IV fosphenytoin at the maximum dose and rate in a randomized, double-blind, controlled clinical trial where the rates for phenytoin and fosphenytoin administration would have resulted in equivalent systemic exposure to phenytoin.
TABLE 2. Treatment-Emergent Adverse Event Incidence Following IV Administration at the Maximum Dose and Rate to Patients with Epilepsy or Neurosurgical Patients (Events in at Least 2% of Fosphenytoin-Treated Patients) BODY SYSTEM
Adverse EventIV Fosphenytoin
N=90IV Phenytoin
N=22BODY AS A WHOLE Pelvic Pain 4.4 0 Asthenia 2.2 0 Back Pain 2.2 0 Headache 2.2 4.5 CARDIOVASCULAR Hypotension 7.7 9.1 Vasodilatation 5.6 4.5 Tachycardia 2.2 0 DIGESTIVE Nausea 8.9 13.6 Tongue Disorder 4.4 0 Dry Mouth 4.4 4.5 Vomiting 2.2 9.1 NERVOUS Nystagmus 44.4 59.1 Dizziness 31.1 27.3 Somnolence 20 27.3 Ataxia 11.1 18.2 Stupor 7.7 4.5 Incoordination 4.4 4.5 Paresthesia 4.4 0 Extrapyramidal Syndrome 4.4 0 Tremor 3.3 9.1 Agitation 3.3 0 Hypesthesia 2.2 9.1 Dysarthria 2.2 0 Vertigo 2.2 0 Brain Edema 2.2 4.5 SKIN AND APPENDAGES Pruritus 48.9 4.5 SPECIAL SENSES Tinnitus 8.9 9.1 Diplopia 3.3 0 Taste Perversion 3.3 0 Amblyopia 2.2 9.1 Deafness 2.2 0 Incidence in Controlled Trials - IM Administration To Patients With Epilepsy: Table 3 lists treatment-emergent adverse events that occurred in at least 2% of fosphenytoin-treated patients in a double-blind, randomized, controlled clinical trial of adult epilepsy patients receiving either IM fosphenytoin substituted for oral phenytoin sodium or continuing oral phenytoin sodium. Both treatments were administered for 5 days.
TABLE 3. Treatment-Emergent Adverse Event Incidence Following Substitution of IM Fosphenytoin for Oral Phenytoin Sodium in Patients With Epilepsy (Events in at Least 2% of Fosphenytoin-Treated Patients) BODY SYSTEM
Adverse EventIM Fosphenytoin
N=179Oral Phenytoin Sodium
N=61BODY AS A WHOLE Headache 8.9 4.9 Asthenia 3.9 3.3 Accidental Injury 3.4 6.6 DIGESTIVE Nausea 4.5 0 Vomiting 2.8 0 HEMATOLOGIC AND LYMPHATIC Ecchymosis 7.3 4.9 NERVOUS Nystagmus 15.1 8.2 Tremor 9.5 13.1 Ataxia 8.4 8.2 Incoordination 7.8 4.9 Somnolence 6.7 9.8 Dizziness 5 3.3 Paresthesia 3.9 3.3 Reflexes Decreased 2.8 4.9 SKIN AND APPENDAGES Pruritus 2.8 0 Adverse Events During All Clinical Trials
Fosphenytoin has been administered to 859 individuals during all clinical trials. All adverse events seen at least twice are listed in the following, except those already included in previous tables and listings. Events are further classified within body system categories and enumerated in order of decreasing frequency using the following definitions: frequent adverse events are defined as those occurring in greater than 1/100 individuals; infrequent adverse events are those occurring in 1/100 to 1/1000 individuals.
Body as a Whole: Frequent: fever, injection-site reaction, infection, chills, face edema, injection-site pain; Infrequent: sepsis, injection-site inflammation, injection-site edema, injection-site hemorrhage, flu syndrome, malaise, generalized edema, shock, photosensitivity reaction, cachexia, cryptococcosis.
Cardiovascular: Frequent: hypertension; Infrequent: cardiac arrest, migraine, syncope, cerebral hemorrhage, palpitation, sinus bradycardia, atrial flutter, bundle branch block, cardiomegaly, cerebral infarct, postural hypotension, pulmonary embolus, QT interval prolongation, thrombophlebitis, ventricular extrasystoles, congestive heart failure.
Digestive: Frequent: constipation; Infrequent: dyspepsia, diarrhea, anorexia, gastrointestinal hemorrhage, increased salivation, liver function tests abnormal, tenesmus, tongue edema, dysphagia, flatulence, gastritis, ileus.
Endocrine: Infrequent: diabetes insipidus.
Hematologic and Lymphatic: Infrequent: thrombocytopenia, anemia, leukocytosis, cyanosis,
hypochromic anemia, leukopenia, lymphadenopathy, petechia.
Metabolic and Nutritional: Frequent: hypokalemia; Infrequent: hyperglycemia, hypophosphatemia, alkalosis, acidosis, dehydration, hyperkalemia, ketosis.
Musculoskeletal: Frequent: myasthenia; Infrequent: myopathy, leg cramps, arthralgia, myalgia.
Nervous: Frequent: reflexes increased, speech disorder, dysarthria, intracranial hypertension, thinking abnormal, nervousness, hypesthesia; Infrequent: confusion, twitching, Babinski sign positive, circumoral paresthesia, hemiplegia, hypotonia, convulsion, extrapyramidal syndrome, insomnia, meningitis, depersonalization, CNS depression, depression, hypokinesia, hyperkinesia, brain edema, paralysis, psychosis, aphasia, emotional lability, coma, hyperesthesia, myoclonus, personality disorder, acute brain syndrome, encephalitis, subdural hematoma, encephalopathy, hostility, akathisia, amnesia, neurosis.
Respiratory: Frequent: pneumonia; Infrequent: pharyngitis, sinusitis, hyperventilation, rhinitis, apnea, aspiration pneumonia, asthma, dyspnea, atelectasis, cough increased, sputum increased, epistaxis, hypoxia, pneumothorax, hemoptysis, bronchitis.
Skin and Appendages: Frequent: rash; Infrequent: maculopapular rash, urticaria, sweating, skin discoloration, contact dermatitis, pustular rash, skin nodule.
Special Senses: Frequent: taste perversion; Infrequent: deafness, visual field defect, eye pain, conjunctivitis, photophobia, hyperacusis, mydriasis, parosmia, ear pain, taste loss.
Urogenital: Infrequent: urinary retention, oliguria, dysuria, vaginitis, albuminuria, genital edema, kidney failure, polyuria, urethral pain, urinary incontinence, vaginal moniliasis.
Post-Marketing Experience
The following adverse reactions have been identified during postapproval use of fosphenytoin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been post-marketing reports of anaphylactoid reaction and anaphylaxis.
Other Phenytoin-Associated Adverse Events:
Dyskinesia.
-
OVERDOSAGE
Nausea, vomiting, lethargy, tachycardia, bradycardia, asystole, cardiac arrest, hypotension, syncope, hypocalcemia, metabolic acidosis, and death have been reported in cases of overdosage with fosphenytoin.
The median lethal dose of fosphenytoin given intravenously in mice and rats was 156 mg PE/kg and approximately 250 mg PE/kg, or about 0.6 and 2 times, respectively, the maximum human loading dose on a mg/m2 basis. Signs of acute toxicity in animals included ataxia, labored breathing, ptosis, and hypoactivity.
Because fosphenytoin is a prodrug of phenytoin, the following information may be helpful. Initial symptoms of acute phenytoin toxicity are nystagmus, ataxia, and dysarthria. Other signs include tremor, hyperreflexia, lethargy, slurred speech, nausea, vomiting, coma, and hypotension. Depression of respiratory and circulatory systems leads to death. There are marked variations among individuals with respect to plasma phenytoin concentrations where toxicity occurs. Lateral gaze nystagmus usually appears at 20 mcg/mL, ataxia at 30 mcg/mL, and dysarthria and lethargy appear when the plasma concentration is over 40 mcg/mL. However, phenytoin concentrations as high as 50 mcg/mL have been reported without evidence of toxicity. As much as 25 times the therapeutic phenytoin dose has been taken, resulting in plasma phenytoin concentrations over 100 mcg/mL, with complete recovery.
Treatment is nonspecific since there is no known antidote to fosphenytoin or phenytoin overdosage. The adequacy of the respiratory and circulatory systems should be carefully observed, and appropriate supportive measures employed. Hemodialysis can be considered since phenytoin is not completely bound to plasma proteins. Total exchange transfusion has been used in the treatment of severe intoxication in children. In acute overdosage the possibility of other CNS depressants, including alcohol, should be borne in mind.
Formate and phosphate are metabolites of fosphenytoin and therefore may contribute to signs of toxicity following overdosage. Signs of formate toxicity are similar to those of methanol toxicity and are associated with severe anion-gap metabolic acidosis. Large amounts of phosphate, delivered rapidly, could potentially cause hypocalcemia with paresthesia, muscle spasms, and seizures. Ionized free calcium levels can be measured and, if low, used to guide treatment.
-
DOSAGE AND ADMINISTRATION
The dose, concentration, and infusion rate of intravenous fosphenytoin should always be expressed as phenytoin sodium equivalents (PE). There is no need to perform molecular weight-based adjustments when converting between fosphenytoin and phenytoin sodium doses. Fosphenytoin should always be prescribed and dispensed in phenytoin sodium equivalent units (PE). 1.5 mg of fosphenytoin sodium is equivalent to 1 mg phenytoin sodium, and is referred to as 1 mg PE. The amount and concentration of fosphenytoin is always expressed in terms of mg of phenytoin sodium equivalents (mg PE).
Do not confuse the concentration of fosphenytoin with the total amount of drug in the vial.
Caution must be used when administering fosphenytoin due to the risk of dosing errors (see WARNINGS). Medication errors associated with fosphenytoin have resulted in patients receiving the wrong dose of fosphenytoin. Fosphenytoin is marketed in 2 mL vials containing a total of 100 mg PE and 10 mL vials containing a total of 500 mg PE. Both vials contain a concentration of 50 mg PE/mL. Errors have occurred when the concentration of the vial (50 mg PE/mL) was misinterpreted to mean that the total content of the vial was 50 mg PE. These errors have resulted in two- or ten-fold overdoses of fosphenytoin since each of the vials actually contains a total of 100 mg PE or 500 mg PE. In some cases, ten-fold overdoses were associated with fatal outcomes. To help minimize confusion, the prescribed dose of fosphenytoin should always be expressed in milligrams of phenytoin equivalents (mg PE). Additionally, when ordering and storing fosphenytoin, consider displaying the total drug content (i.e., 100 mg PE/ 2 mL or 500 mg PE/ 10 mL) instead of concentration in computer systems, pre-printed orders, and automated dispensing cabinet databases to help ensure that total drug content can be clearly identified. Care should be taken to ensure the appropriate volume of fosphenytoin is withdrawn from the vial when preparing the dose for administration. Attention to these details may prevent some fosphenytoin medication errors from occurring.
Prior to intravenous infusion, dilute fosphenytoin injection in 5% dextrose or 0.9% saline solution for injection to a concentration ranging from 1.5 to 25 mg PE/mL. The maximum concentration of fosphenytoin in any solution should be 25 mg PE/mL. When fosphenytoin is given as an intravenous infusion, fosphenytoin needs to be diluted and should only be administered at a rate not exceeding 150 mg PE/min.
Parenteral drug products should be inspected visually for particulate matter or discoloration prior to administration, whenever solution and container permit.
Status Epilepticus
- The loading dose of fosphenytoin is 15 to 20 mg PE/kg administered at 100 to 150 mg PE/min.
- Because of the risk of hypotension, fosphenytoin should be administered no faster than 150 mg PE/min. Continuous monitoring of the electrocardiogram, blood pressure, and respiratory function is essential and the patient should be observed throughout the period where maximal serum phenytoin concentrations occur, approximately 10 to 20 minutes after the end of fosphenytoin infusions.
- Because the full antiepileptic effect of phenytoin, whether given as fosphenytoin or parenteral phenytoin, is not immediate, other measures, including concomitant administration of an intravenous benzodiazepine, will usually be necessary for the control of status epilepticus.
- The loading dose should be followed by maintenance doses of either fosphenytoin or phenytoin.
If administration of fosphenytoin does not terminate seizures, the use of other anticonvulsants and other appropriate measures should be considered.
Even though loading doses of fosphenytoin have been given by the intramuscular route for other indications when intravenous access is impossible, intramuscular fosphenytoin should ordinarily not be used in the treatment of status epilepticus because therapeutic phenytoin concentrations may not be reached as quickly as with intravenous administration.
Nonemergent Loading and Maintenance Dosing
Because of the risks of cardiac and local toxicity associated with intravenous fosphenytoin, oral phenytoin should be used whenever possible.
The loading dose of fosphenytoin is 10 to 20 mg PE/kg given intravenous or intramuscular. The rate of administration for intravenous fosphenytoin should be no greater than 150 mg PE/min. Continuous monitoring of the electrocardiogram, blood pressure, and respiratory function is essential and the patient should be observed throughout the period where maximal serum phenytoin concentrations occur (approximately 20 minutes after the end of fosphenytoin infusion).
The initial daily maintenance dose of fosphenytoin is 4 to 6 mg PE/kg/day in divided doses.
Intramuscular or Intravenous Substitution for Oral Phenytoin Therapy
When treatment with oral phenytoin is not possible, fosphenytoin can be substituted for oral phenytoin at the same total daily dose.
Phenytoin sodium capsules are approximately 90% bioavailable by the oral route. Phenytoin, supplied as fosphenytoin, is 100% bioavailable by both the intramuscular and intravenous routes. For this reason, plasma phenytoin concentrations may increase modestly when intramuscular or intravenous fosphenytoin is substituted for oral phenytoin sodium therapy.
The rate of administration for intravenous fosphenytoin should be no greater than 150 mg PE/min.
In controlled trials, intramuscular fosphenytoin was administered as a single daily dose utilizing either 1 or 2 injection sites. Some patients may require more frequent dosing.
Dosing in Special Populations
Patients with Renal or Hepatic Disease: Due to an increased fraction of unbound phenytoin in patients with renal or hepatic disease, or in those with hypoalbuminemia, the interpretation of total phenytoin plasma concentrations should be made with caution (see CLINICAL PHARMACOLOGY, Special Populations). Unbound phenytoin concentrations may be more useful in these patient populations. After intravenous fosphenytoin administration to patients with renal and/or hepatic disease, or in those with hypoalbuminemia, fosphenytoin clearance to phenytoin may be increased without a similar increase in phenytoin clearance. This has the potential to increase the frequency and severity of adverse events (see PRECAUTIONS).
Elderly Patients: Age does not have a significant impact on the pharmacokinetics of fosphenytoin following fosphenytoin administration. Phenytoin clearance is decreased slightly in elderly patients and lower or less frequent dosing may be required.
Pediatric: The safety and efficacy of fosphenytoin in pediatric patients have not been established.
-
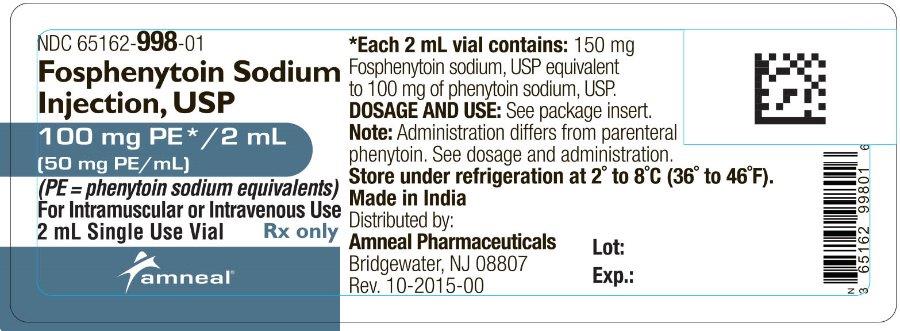
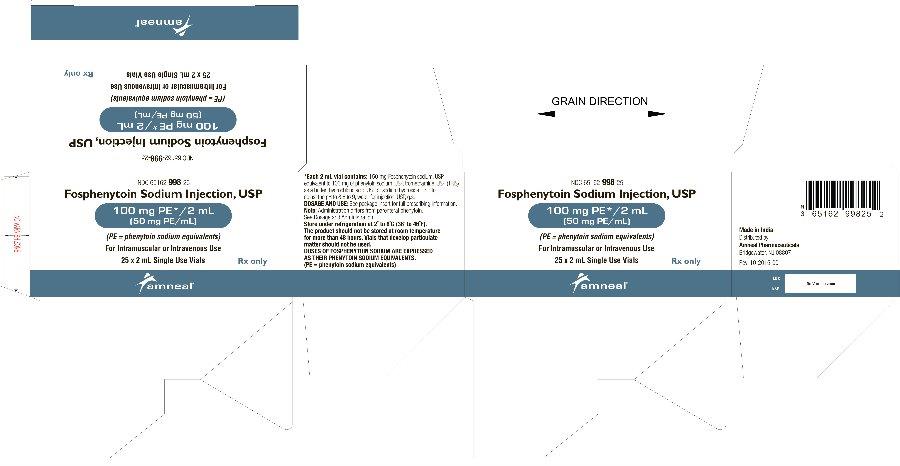
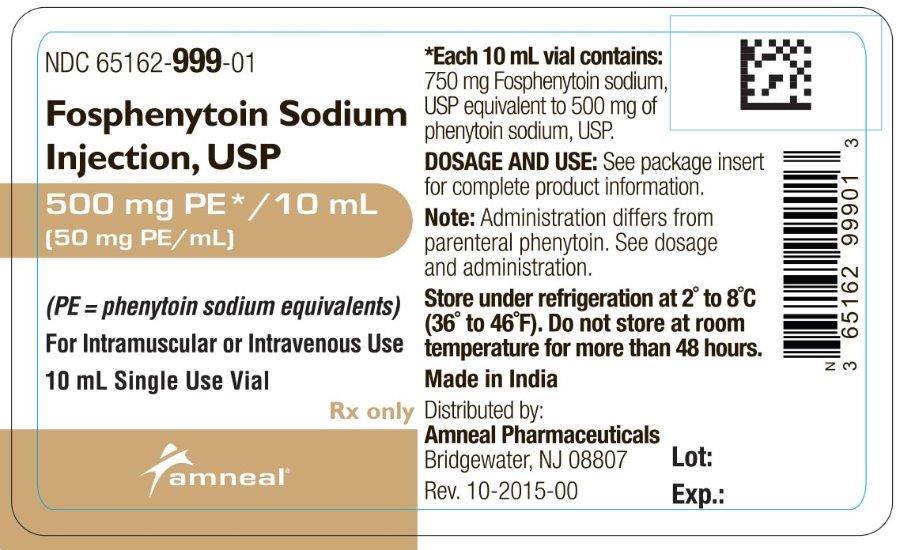
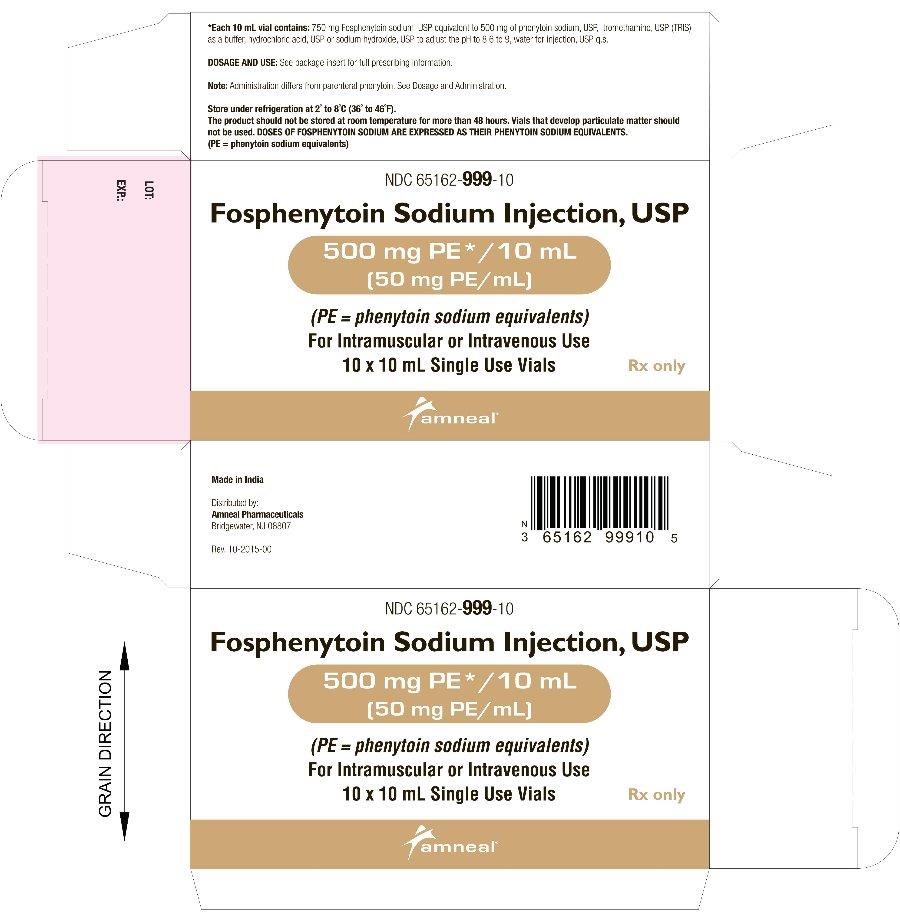
HOW SUPPLIED
Fosphenytoin Sodium Injection, USP is supplied as follows:
10 mL per vial [NDC: 65162-999-01] — Each 10 mL vial contains Fosphenytoin Sodium, USP 750 mg equivalent to 500 mg of phenytoin sodium, USP: (Packages of 10 - NDC: 65162-999-10).
2 mL per vial [NDC: 65162-998-01] — Each 2 mL vial contains Fosphenytoin Sodium, USP 150 mg equivalent to 100 mg of phenytoin sodium, USP: (Packages of 25 - NDC: 65162-998-25).
Both sizes of vials contain Tromethamine, USP (TRIS), Hydrochloric Acid, NF, or Sodium Hydroxide, NF, and Water for Injection, USP.
Fosphenytoin sodium should always be prescribed in phenytoin sodium equivalents (PE) (see DOSAGE AND ADMINISTRATION).
1.5 mg of fosphenytoin sodium is equivalent to 1 mg phenytoin sodium, and is referred to as 1 mg PE. The amount and concentration of fosphenytoin is always expressed in terms of mg of phenytoin sodium equivalents (PE). Fosphenytoin’s weight is expressed as phenytoin sodium equivalents to avoid the need to perform molecular weight-based adjustments when substituting fosphenytoin for phenytoin or vice versa.
Store under refrigeration at 2°C to 8°C (36°F to 46°F). The product should not be stored at room temperature for more than 48 hours. Vials that develop particulate matter should not be used.
Brands listed are the trademarks of their respective owners.
Made in India
Distributed by:
Amneal Pharmaceuticals
Bridgewater, NJ 08807Rev. 10-2015-03
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FOSPHENYTOIN SODIUM
fosphenytoin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65162-998 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FOSPHENYTOIN SODIUM (UNII: 7VLR55452Z) (PHENYTOIN - UNII:6158TKW0C5) PHENYTOIN SODIUM 50 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) TROMETHAMINE (UNII: 023C2WHX2V) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Product Characteristics Color YELLOW (clear, colorless to pale yellow) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65162-998-25 25 in 1 CARTON 1 NDC: 65162-998-01 2 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078476 05/17/2013 FOSPHENYTOIN SODIUM
fosphenytoin sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 65162-999 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FOSPHENYTOIN SODIUM (UNII: 7VLR55452Z) (PHENYTOIN - UNII:6158TKW0C5) PHENYTOIN SODIUM 50 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) TROMETHAMINE (UNII: 023C2WHX2V) HYDROCHLORIC ACID (UNII: QTT17582CB) SODIUM HYDROXIDE (UNII: 55X04QC32I) Product Characteristics Color YELLOW (clear, colorless to pale yellow) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 65162-999-10 10 in 1 CARTON 1 NDC: 65162-999-01 2 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078476 05/17/2013 Labeler - Amneal Pharmaceuticals of New York, LLC (123797875) Establishment Name Address ID/FEI Business Operations Strides Arcolab Limited 918513263 ANALYSIS(65162-998, 65162-999) , MANUFACTURE(65162-998, 65162-999) , PACK(65162-998, 65162-999)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.