ZOSYN IN GALAXY CONTAINERS- piperacillin sodium and tazobactam sodium injection, solution
Zosyn by
Drug Labeling and Warnings
Zosyn by is a Prescription medication manufactured, distributed, or labeled by Wyeth Pharmaceuticals Inc., a subsidiary of Pfizer Inc., Baxter Healthcare Corporation. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
SPL UNCLASSIFIED SECTION
To reduce the development of drug-resistant bacteria and maintain the effectiveness of ZOSYN® (piperacillin and tazobactam) injection and other antibacterial drugs, ZOSYN (piperacillin and tazobactam) should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
-
DESCRIPTION
ZOSYN (piperacillin and tazobactam injection) in Galaxy® Containers (PL 2040 Plastic) is a sterile injectable antibacterial combination product consisting of the semisynthetic antibiotic piperacillin sodium and the β-lactamase inhibitor tazobactam sodium for intravenous administration.
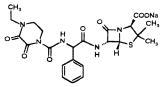
Piperacillin sodium is derived from D(-)-α-aminobenzyl-penicillin. The chemical name of piperacillin sodium is sodium (2S,5R,6R)-6-[(R)-2-(4-ethyl-2,3-dioxo-1-piperazine-carboxamido)-2-phenylacetamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylate. The chemical formula is C23H26N5NaO7S and the molecular weight is 539.5. The chemical structure of piperacillin sodium is:
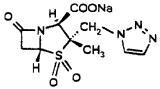
Tazobactam sodium, a derivative of the penicillin nucleus, is a penicillanic acid sulfone. Its chemical name is sodium (2S,3S,5R)-3-methyl-7-oxo-3-(1H-1,2,3-triazol-1-ylmethyl)-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylate-4,4-dioxide. The chemical formula is C10H11N4NaO5S and the molecular weight is 322.3. The chemical structure of tazobactam sodium is:
ZOSYN in the Galaxy Container (PL 2040 Plastic) is a frozen, iso-osmotic, sterile, non-pyrogenic premixed solution. The components and dosage formulations are given in the table below:
TABLE 1 ZOSYN IN GALAXY CONTAINERS (PL 2040 PLASTIC) PREMIXED FROZEN SOLUTION Component* Function Dosage Formulations 2.25 g/50 mL 3.375 g/50 mL 4.5 g/100 mL *Piperacillin and tazobactam are present in the formulation as sodium salts. Dextrose hydrous, sodium citrate dihydrate, and edetate disodium dihydrate amounts are approximate. Piperacillin active ingredient 2 g 3 g 4 g Tazobactam β-lactamase
inhibitor250 mg 375 mg 500 mg Dextrose Hydrous osmolality adjusting agent 1 g 350 mg 2 g Sodium Citrate Dihydrate buffering agent 100 mg 150 mg 200 mg Edetate Disodium Dihydrate metal chelator 0.5 mg 0.75 mg 1 mg Water for Injection solvent q.s. 50 mL q.s. 50 mL q.s. 100 mL The pH has been adjusted between 5.5 to 6.8 with sodium bicarbonate and hydrochloric acid.
The solution is intended for intravenous use only.
The plastic container is fabricated from a specially designed multilayer plastic, PL 2040. Solutions are in contact with the polyethylene layer of this container and can leach out certain chemical components of the plastic in very small amounts within the expiration period. The suitability of the plastic has been confirmed in tests in animals according to the USP biological tests for plastic containers, as well as by tissue culture toxicity studies.
The approximate total sodium content for ZOSYN in Galaxy Containers is 5.58 mEq (128 mg) per 50 mL in the 2.25 g dose, 8.38 mEq (192 mg) per 50 mL in the 3.375 g dose, and 11.17 mEq (256 mg) per 100 mL in the 4.5 g dose.
-
CLINICAL PHARMACOLOGY
Adults
Peak plasma concentrations of piperacillin and tazobactam are attained immediately after completion of an intravenous infusion of ZOSYN. Piperacillin plasma concentrations, following a 30-minute infusion of ZOSYN, were similar to those attained when equivalent doses of piperacillin were administered alone, with mean peak plasma concentrations of approximately 134 μg/mL, 242 μg/mL, and 298 μg/mL for the 2.25 g, 3.375 g, and 4.5 g ZOSYN (piperacillin/tazobactam) doses, respectively. The corresponding mean peak plasma concentrations of tazobactam were 15 μg/mL, 24 μg/mL, and 34 μg/mL, respectively.
Following a 30-minute I.V. infusion of 3.375 g ZOSYN every 6 hours, steady-state plasma concentrations of piperacillin and tazobactam were similar to those attained after the first dose. In like manner, steady-state plasma concentrations were not different from those attained after the first dose when 2.25 g or 4.5 g doses of ZOSYN were administered via 30-minute infusions every 6 hours. Steady-state plasma concentrations after 30-minute infusions every 6 hours are provided in Table 2.
Following single or multiple ZOSYN doses to healthy subjects, the plasma half-life of piperacillin and of tazobactam ranged from 0.7 to 1.2 hours and was unaffected by dose or duration of infusion.
Piperacillin is metabolized to a minor microbiologically active desethyl metabolite. Tazobactam is metabolized to a single metabolite that lacks pharmacological and antibacterial activities. Both piperacillin and tazobactam are eliminated via the kidney by glomerular filtration and tubular secretion. Piperacillin is excreted rapidly as unchanged drug with 68% of the administered dose excreted in the urine. Tazobactam and its metabolite are eliminated primarily by renal excretion with 80% of the administered dose excreted as unchanged drug and the remainder as the single metabolite. Piperacillin, tazobactam, and desethyl piperacillin are also secreted into the bile.
Both piperacillin and tazobactam are approximately 30% bound to plasma proteins. The protein binding of either piperacillin or tazobactam is unaffected by the presence of the other compound. Protein binding of the tazobactam metabolite is negligible.
Piperacillin and tazobactam are widely distributed into tissues and body fluids including intestinal mucosa, gallbladder, lung, female reproductive tissues (uterus, ovary, and fallopian tube), interstitial fluid, and bile. Mean tissue concentrations are generally 50% to 100% of those in plasma. Distribution of piperacillin and tazobactam into cerebrospinal fluid is low in subjects with non-inflamed meninges, as with other penicillins.
After the administration of single doses of piperacillin/tazobactam to subjects with renal impairment, the half-life of piperacillin and of tazobactam increases with decreasing creatinine clearance. At creatinine clearance below 20 mL/min, the increase in half-life is twofold for piperacillin and fourfold for tazobactam compared to subjects with normal renal function. Dosage adjustments for ZOSYN are recommended when creatinine clearance is below 40 mL/min in patients receiving the usual recommended daily dose of ZOSYN. (See DOSAGE AND ADMINISTRATION section for specific recommendations for the treatment of patients with renal insufficiency.)
Hemodialysis removes 30% to 40% of a piperacillin/tazobactam dose with an additional 5% of the tazobactam dose removed as the tazobactam metabolite. Peritoneal dialysis removes approximately 6% and 21% of the piperacillin and tazobactam doses, respectively, with up to 16% of the tazobactam dose removed as the tazobactam metabolite. For dosage recommendations for patients undergoing hemodialysis, see DOSAGE AND ADMINISTRATION section.
The half-life of piperacillin and of tazobactam increases by approximately 25% and 18%, respectively, in patients with hepatic cirrhosis compared to healthy subjects. However, this difference does not warrant dosage adjustment of ZOSYN due to hepatic cirrhosis.
TABLE 2 STEADY STATE MEAN PLASMA CONCENTRATIONS IN ADULTS AFTER 30-MINUTE INTRAVENOUS INFUSION OF PIPERACILLIN/TAZOBACTAM EVERY 6 HOURS PIPERACILLIN ** Numbers in parentheses are coefficients of variation (CV%). Plasma Concentrations**
(µg/mL)AUC**
(μghr/mL)Piperacillin/
Tazobactam
DoseaNo. of
Evaluable
Subjects30 min 1 hr 2 hr 3 hr 4 hr 6 hr AUC0-6 2.25 g 8 134 (14) 57 (14) 17.1 (23) 5.2 (32) 2.5 (35) 0.9
(14)b131 (14) 3.375 g 6 242 (12) 106 (8) 34.6 (20) 11.5 (19) 5.1 (22) 1.0 (10) 242 (10) 4.5 g 8 298 (14) 141 (19) 46.6 (28) 16.4 (29) 6.9 (29) 1.4 (30) 322 (16)
TAZOBACTAM
Plasma Concentrations**
(µg/mL)AUC**
(μghr/mL)Piperacillin/
Tazobactam
DoseaNo. of
Evaluable
Subjects30 min 1 hr 2 hr 3 hr 4 hr 6 hr AUC0-6 2.25 g 8 14.8 (14) 7.2 (22) 2.6 (30) 1.1 (35) 0.7
(6)c<0.5 16.0 (21) 3.375 g 6 24.2 (14) 10.7 (7) 4.0 (18) 1.4 (21) 0.7
(16)b<0.5 25.0 (8) 4.5 g 8 33.8 (15) 17.3 (16) 6.8 (24) 2.8 (25) 1.3
(30)<0.5 39.8 (15) Pediatrics
Piperacillin and tazobactam pharmacokinetics were studied in pediatric patients 2 months of age and older. The clearance of both compounds is slower in the younger patients compared to older children and adults.
In a population PK analysis, estimated clearance for 9 month-old to 12 year-old patients was comparable to adults, with a population mean (SE) value of 5.64 (0.34) mL/min/kg. The piperacillin clearance estimate is 80% of this value for pediatric patients 2 - 9 months old. In patients younger than 2 months of age, clearance of piperacillin is slower compared to older children; however, it is not adequately characterized for dosing recommendations. The population mean (SE) for piperacillin distribution volume is 0.243 (0.011) L/kg and is independent of age.
Microbiology
Piperacillin sodium exerts bactericidal activity by inhibiting septum formation and cell wall synthesis of susceptible bacteria. In vitro, piperacillin is active against a variety of gram-positive and gram-negative aerobic and anaerobic bacteria. Tazobactam sodium has little clinically relevant in vitro activity against bacteria due to its reduced affinity to penicillin-binding proteins. It is, however, a β-lactamase inhibitor of the Richmond-Sykes class III (Bush class 2b & 2b') penicillinases and cephalosporinases. It varies in its ability to inhibit class II and IV (2a & 4) penicillinases. Tazobactam does not induce chromosomally-mediated β-lactamases at tazobactam concentrations achieved with the recommended dosage regimen.
Piperacillin/tazobactam has been shown to be active against most strains of the following microorganisms both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Aerobic and facultative gram-positive microorganisms:
Staphylococcus aureus (excluding methicillin and oxacillin-resistant isolates)
Aerobic and facultative gram-negative microorganisms:
Haemophilus influenzae (excluding β-lactamase negative, ampicillin-resistant isolates)
Pseudomonas aeruginosa (given in combination with an aminoglycoside to which the isolate is susceptible)
Gram-negative anaerobes:
Bacteroides fragilis group (B. fragilis, B. ovatus, B. thetaiotaomicron, and B. vulgatus)
The following in vitro data are available, but their clinical significance is unknown.
At least 90% of the following microorganisms exhibit in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for piperacillin/tazobactam. However, the safety and effectiveness of piperacillin/tazobactam in treating clinical infections due to these bacteria have not been established in adequate and well-controlled clinical trials.
Aerobic and facultative gram-positive microorganisms:
Enterococcus faecalis (ampicillin or penicillin-susceptible isolates only)
Staphylococcus epidermidis (excluding methicillin and oxacillin-resistant isolates)
Streptococcus pneumoniae† (penicillin-susceptible isolates only)
Susceptibility Testing Methods
As is recommended with all antimicrobials, the results of in vitro susceptibility tests, when available, should be provided to the physician as periodic reports, which describe the susceptibility profile of nosocomial and community—acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial.
Dilution Techniques:
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of piperacillin and tazobactam powders.1,2 MIC values should be determined using serial dilutions of piperacillin combined with a fixed concentration of 4 μg/mL tazobactam. The MIC values obtained should be interpreted according to criteria provided in Table 3.
Diffusion Technique:
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure1,3 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 100 μg of piperacillin and 10 μg of tazobactam to test the susceptibility of microorganisms to piperacillin/tazobactam. The disk diffusion interpreted criteria are provided in Table 3.
Anaerobic Techniques
For anaerobic bacteria, the susceptibility to piperacillin/tazobactam can be determined by the reference agar dilution method.4
TABLE 3 SUSCEPTIBILITY INTERPRETIVE CRITERIA FOR PIPERACILLIN/TAZOBACTAM Susceptibility Test Result Interpretive Criteria a These interpretive criteria for Haemophilus influenzae are applicable only to tests performed using Haemophilus Test Medium inoculated with a direct colony suspension and incubated at 35°C in ambient air for 20 to 24 hours. Minimal Inhibitory Concentration
(MIC in µg/mL)Disk Diffusion
(Zone Diameter in mm)Pathogen S I R S I R
Enterobacteriaceae and Acinetobacter baumanii
≤ 16 32 - 64 ≥ 128 ≥ 21 18 - 20 ≤ 17
Haemophilus influenzaea
≤ 1 - ≥ 2 ≥ 21 - -
Pseudomonas aeruginosa
≤ 64 - ≥ 128 ≥ 18 - ≤ 17
Staphylococcus aureus
≤ 8 - ≥ 16 ≥ 18 - ≤ 17
Bacteroides fragilis group≤ 32 64 ≥ 128 - - - A report of S (“Susceptible”) indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of I (“Intermediate”) indicates that the results should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone, which prevents small, uncontrolled technical factors from causing major discrepancies in interpretation. A report of R (“Resistant”) indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be considered.
Quality Control
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the procedures.1,2,3,4 Standard piperacillin/tazobactam powder should provide the following ranges of values noted in Table 4. Quality control microorganisms are specific strains of microorganisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within the microorganism; the specific strains used for microbiological quality control are not clinically significant.
TABLE 4 ACCEPTABLE QUALITY CONTROL RANGES FOR PIPERACILLIN/TAZOBACTAM TO BE USED IN VALIDATION OF SUSCEPTIBILITY TEST RESULTS Acceptable Quality Control Ranges a This quality control range for Haemophilus influenzae is applicable only to tests performed using Haemophilus Test Medium inoculated with a direct colony suspension and incubated at 35°C in ambient air for 20 to 24 hours. b The quality control ranges for Bacteroides fragilis and Bacteroides thetaiotaomicron are applicable only to tests performed using the agar dilution method. QC Strain Minimum Inhibitory
Concentration
Range (MIC in µg/mL)Disk Diffusion
Zone Diameter
Ranges in mm
Escherichia coli
ATCC 259221 - 4 24 - 30
Escherichia coli
ATCC 352180.5 - 2 24 - 30
Pseudomonas aeruginosa
ATCC 278531 - 8 25 - 33
Haemophilus influenzaea
ATCC 492470.06 - 0.5 33-38
Staphylococcus aureus
ATCC 292130.25 - 2 -
Staphylococcus aureus
ATCC 25923- 27 - 36
Bacteroides fragilisb
ATCC 252850.12 - 0.5 -
Bacteroides thetaiotaomicronb
ATCC 297414 - 16 - -
INDICATIONS AND USAGE
ZOSYN is indicated for the treatment of patients with moderate to severe infections caused by piperacillin-resistant, piperacillin/tazobactam-susceptible, β-lactamase producing strains of the designated microorganisms in the specified conditions listed below:
Appendicitis (complicated by rupture or abscess) and peritonitis caused by piperacillin-resistant, β‑lactamase producing strains of Escherichia coli or the following members of the Bacteroides fragilis group: B. fragilis, B. ovatus, B. thetaiotaomicron, or B. vulgatus. The individual members of this group were studied in less than 10 cases.
Uncomplicated and complicated skin and skin structure infections, including cellulitis, cutaneous abscesses, and ischemic/diabetic foot infections caused by piperacillin-resistant, β‑lactamase producing strains of Staphylococcus aureus.
Postpartum endometritis or pelvic inflammatory disease caused by piperacillin-resistant, β‑lactamase producing strains of Escherichia coli.
Community-acquired pneumonia (moderate severity only) caused by piperacillin-resistant, β‑lactamase producing strains of Haemophilus influenzae.
Nosocomial pneumonia (moderate to severe) caused by piperacillin-resistant, β-lactamase producing strains of Staphylococcus aureus and by piperacillin/tazobactam-susceptible Acinetobacter baumanii, Haemophilus influenzae, Klebsiella pneumoniae, and Pseudomonas aeruginosa. (Nosocomial pneumonia caused by P. aeruginosa should be treated in combination with an aminoglycoside.) (See DOSAGE AND ADMINISTRATION.)
ZOSYN is indicated only for the specified conditions listed above. Infections caused by piperacillin-susceptible organisms, for which piperacillin has been shown to be effective, are also amenable to ZOSYN treatment due to its piperacillin content. The tazobactam component of this combination product does not decrease the activity of the piperacillin component against piperacillin-susceptible organisms. Therefore, the treatment of mixed infections caused by piperacillin-susceptible organisms and piperacillin-resistant, β-lactamase producing organisms susceptible to ZOSYN should not require the addition of another antibiotic. (See DOSAGE AND ADMINISTRATION.)
ZOSYN is useful as presumptive therapy in the indicated conditions prior to the identification of causative organisms because of its broad spectrum of bactericidal activity against gram-positive and gram-negative aerobic and anaerobic organisms.
Appropriate cultures should usually be performed before initiating antimicrobial treatment in order to isolate and identify the organisms causing infection and to determine their susceptibility to ZOSYN. Antimicrobial therapy should be adjusted, if appropriate, once the results of culture(s) and antimicrobial susceptibility testing are known.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of ZOSYN (piperacillin and tazobactam) injection and other antibacterial drugs, ZOSYN (piperacillin and tazobactam) should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
- CONTRAINDICATIONS
-
WARNINGS
SERIOUS AND OCCASIONALLY FATAL HYPERSENSITIVITY (ANAPHYLACTIC/ANAPHYLACTOID) REACTIONS (INCLUDING SHOCK) HAVE BEEN REPORTED IN PATIENTS RECEIVING THERAPY WITH PENICILLINS INCLUDING ZOSYN. THESE REACTIONS ARE MORE LIKELY TO OCCUR IN INDIVIDUALS WITH A HISTORY OF PENICILLIN HYPERSENSITIVITY OR A HISTORY OF SENSITIVITY TO MULTIPLE ALLERGENS. THERE HAVE BEEN REPORTS OF INDIVIDUALS WITH A HISTORY OF PENICILLIN HYPERSENSITIVITY WHO HAVE EXPERIENCED SEVERE REACTIONS WHEN TREATED WITH CEPHALOSPORINS. BEFORE INITIATING THERAPY WITH ZOSYN, CAREFUL INQUIRY SHOULD BE MADE CONCERNING PREVIOUS HYPERSENSITIVITY REACTIONS TO PENICILLINS, CEPHALOSPORINS, OR OTHER ALLERGENS. IF AN ALLERGIC REACTION OCCURS, ZOSYN SHOULD BE DISCONTINUED AND APPROPRIATE THERAPY INSTITUTED. SERIOUS ANAPHYLACTIC/ANAPHYLACTOID REACTIONS (INCLUDING SHOCK) REQUIRE IMMEDIATE EMERGENCY TREATMENT WITH EPINEPHRINE. OXYGEN, INTRAVENOUS STEROIDS, AND AIRWAY MANAGEMENT, INCLUDING INTUBATION, SHOULD ALSO BE ADMINISTERED AS INDICATED.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including ZOSYN, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis, have been reported in patients receiving ZOSYN (see ADVERSE REACTIONS). If patients develop a skin rash they should be monitored closely and ZOSYN discontinued if lesions progress.
-
PRECAUTIONS
General
Bleeding manifestations have occurred in some patients receiving β-lactam antibiotics, including piperacillin. These reactions have sometimes been associated with abnormalities of coagulation tests such as clotting time, platelet aggregation, and prothrombin time, and are more likely to occur in patients with renal failure. If bleeding manifestations occur, ZOSYN should be discontinued and appropriate therapy instituted.
The possibility of the emergence of resistant organisms that might cause superinfections should be kept in mind. If this occurs, appropriate measures should be taken.
As with other penicillins, patients may experience neuromuscular excitability or convulsions if higher than recommended doses are given intravenously (particularly in the presence of renal failure).
ZOSYN in Galaxy Containers contains a monosodium salt of piperacillin, a monosodium salt of tazobactam, and sodium from other formulation components. The approximate total sodium content for ZOSYN in Galaxy Containers is 5.58 mEq (128 mg) per 50 mL in the 2.25 g dose, 8.38 mEq (192 mg) per 50 mL in the 3.375 g dose, and 11.17 mEq (256 mg) per 100 mL in the 4.5 g dose. This should be considered when treating patients requiring restricted salt intake. Periodic electrolyte determinations should be performed in patients with low potassium reserves, and the possibility of hypokalemia should be kept in mind with patients who have potentially low potassium reserves and who are receiving cytotoxic therapy or diuretics. As with other semisynthetic penicillins, piperacillin therapy has been associated with an increased incidence of fever and rash in cystic fibrosis patients.
In patients with creatinine clearance ≤ 40 mL/min and dialysis patients (hemodialysis and CAPD), the intravenous dose should be adjusted to the degree of renal function impairment. (See DOSAGE AND ADMINISTRATION.)
Prescribing ZOSYN (piperacillin and tazobactam) in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs, including ZOSYN, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When ZOSYN is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by ZOSYN or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Laboratory Tests
Periodic assessment of hematopoietic function should be performed, especially with prolonged therapy, i.e., ≥ 21 days. (See ADVERSE REACTIONS, Adverse Laboratory Events.)
Drug Interactions
Aminoglycosides
The mixing of beta-lactam antibiotics with aminoglycosides in vitro can result in substantial inactivation of the aminoglycoside. However, amikacin and gentamicin have been shown to be compatible in vitro with reformulated ZOSYN containing EDTA supplied in vials or bulk pharmacy containers in certain diluents at specific concentrations for a simultaneous Y-site infusion. (See DOSAGE AND ADMINISTRATION.) Reformulated ZOSYN containing EDTA is not compatible with tobramycin for simultaneous coadministration via Y-site infusion.
The inactivation of aminoglycosides in the presence of penicillin-class drugs has been recognized. It has been postulated that penicillin-aminoglycoside complexes form; these complexes are microbiologically inactive and of unknown toxicity. Sequential administration of ZOSYN with tobramycin to patients with normal renal function and mild to moderate renal impairment has been shown to modestly decrease serum concentrations of tobramycin but does not significantly affect tobramycin pharmacokinetics. When aminoglycosides are administered in combination with piperacillin to patients with end-stage renal disease requiring hemodialysis, the concentrations of the aminoglycosides (especially tobramycin) may be significantly altered and should be monitored. Since aminoglycosides are not equally susceptible to inactivation by piperacillin, consideration should be given to the choice of the aminoglycoside when administered in combination with piperacillin to these patients.
Probenecid
Probenecid administered concomitantly with ZOSYN prolongs the half-life of piperacillin by 21% and of tazobactam by 71%.
Heparin
Coagulation parameters should be tested more frequently and monitored regularly during simultaneous administration of high doses of heparin, oral anticoagulants, or other drugs that may affect the blood coagulation system or the thrombocyte function.
Vecuronium
Piperacillin when used concomitantly with vecuronium has been implicated in the prolongation of the neuromuscular blockade of vecuronium. ZOSYN could produce the same phenomenon if given along with vecuronium. Due to their similar mechanism of action, it is expected that the neuromuscular blockade produced by any of the non-depolarizing muscle relaxants could be prolonged in the presence of piperacillin. (See package insert for vecuronium bromide.)
Methotrexate
Limited data suggests that coadministration of methotrexate and piperacillin may reduce the clearance of methotrexate due to competition for renal secretion. The impact of tazobactam on the elimination of methotrexate has not been evaluated. If concurrent therapy is necessary, serum concentrations of methotrexate as well as the signs and symptoms of methotrexate toxicity should be frequently monitored.
Drug/Laboratory Test Interactions
As with other penicillins, the administration of ZOSYN may result in a false-positive reaction for glucose in the urine using a copper-reduction method (CLINITEST®). It is recommended that glucose tests based on enzymatic glucose oxidase reactions (such as DIASTIX® or TES-TAPE) be used.
There have been reports of positive test results using the Bio-Rad Laboratories Platelia Aspergillus EIA test in patients receiving piperacillin/tazobactam injection who were subsequently found to be free of Aspergillus infection. Cross-reactions with non-Aspergillus polysaccharides and polyfuranoses with the Bio-Rad Laboratories Platelia Aspergillus EIA test have been reported.
Therefore, positive test results in patients receiving piperacillin/tazobactam should be interpreted cautiously and confirmed by other diagnostic methods.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term carcinogenicity studies in animals have not been conducted with piperacillin/tazobactam, piperacillin, or tazobactam.
Piperacillin/Tazobactam
Piperacillin/tazobactam was negative in microbial mutagenicity assays at concentrations up to 14.84/1.86 μg/plate. Piperacillin/tazobactam was negative in the unscheduled DNA synthesis (UDS) test at concentrations up to 5689/711 μg/mL. Piperacillin/tazobactam was negative in a mammalian point mutation (Chinese hamster ovary cell HPRT) assay at concentrations up to 8000/1000 μg/mL. Piperacillin/tazobactam was negative in a mammalian cell (BALB/c-3T3) transformation assay at concentrations up to 8/1 μg/mL. In vivo, piperacillin/tazobactam did not induce chromosomal aberrations in rats dosed I.V. with 1500/187.5 mg/kg; this dose is similar to the maximum recommended human daily dose on a body-surface-area basis (mg/m2).
Piperacillin
Piperacillin was negative in microbial mutagenicity assays at concentrations up to 50 μg/plate. There was no DNA damage in bacteria (Rec assay) exposed to piperacillin at concentrations up to 200 μg/disk. Piperacillin was negative in the UDS test at concentrations up to 10,000 μg/mL. In a mammalian point mutation (mouse lymphoma cells) assay, piperacillin was positive at concentrations ≥2500 μg/mL. Piperacillin was negative in a cell (BALB/c-3T3) transformation assay at concentrations up to 3000 μg/mL. In vivo, piperacillin did not induce chromosomal aberrations in mice at I.V. doses up to 2000 mg/kg/day or rats at I.V. doses up to 1500 mg/kg/day. These doses are half (mice) or similar (rats) to the maximum recommended human daily dose based on body-surface area (mg/m2). In another in vivo test, there was no dominant lethal effect when piperacillin was administered to rats at I.V. doses up to 2000 mg/kg/day, which is similar to the maximum recommended human daily dose based on body-surface area (mg/m2). When mice were administered piperacillin at I.V. doses up to 2000 mg/kg/day, which is half the maximum recommended human daily dose based on body-surface area (mg/m2), urine from these animals was not mutagenic when tested in a microbial mutagenicity assay. Bacteria injected into the peritoneal cavity of mice administered piperacillin at I.V. doses up to 2000 mg/kg/day did not show increased mutation frequencies.
Tazobactam
Tazobactam was negative in microbial mutagenicity assays at concentrations up to 333 μg/plate. Tazobactam was negative in the UDS test at concentrations up to 2000 μg/mL. Tazobactam was negative in a mammalian point mutation (Chinese hamster ovary cell HPRT) assay at concentrations up to 5000 μg/mL. In another mammalian point mutation (mouse lymphoma cells) assay, tazobactam was positive at concentrations ≥3000 μg/mL. Tazobactam was negative in a cell (BALB/c-3T3) transformation assay at concentrations up to 900 μg/mL. In an in vitro cytogenetics (Chinese hamster lung cells) assay, tazobactam was negative at concentrations up to 3000 μg/mL. In vivo, tazobactam did not induce chromosomal aberrations in rats at I.V. doses up to 5000 mg/kg, which is 23 times the maximum recommended human daily dose based on body-surface area (mg/m2).
Pregnancy
Teratogenic effects—Pregnancy Category B
Piperacillin/tazobactam
Reproduction studies have been performed in rats and have revealed no evidence of impaired fertility due to piperacillin/tazobactam administered up to a dose which is similar to the maximum recommended human daily dose based on body-surface area (mg/m2).
Teratology studies have been performed in mice and rats and have revealed no evidence of harm to the fetus due to piperacillin/tazobactam administered up to a dose which is 1 to 2 times and 2 to 3 times the human dose of piperacillin and tazobactam, respectively, based on body-surface area (mg/m2).
Piperacillin
Reproduction and teratology studies have been performed in mice and rats and have revealed no evidence of impaired fertility or harm to the fetus due to piperacillin administered up to a dose which is half (mice) or similar (rats) to the maximum recommended human daily dose based on body-surface area (mg/m2).
Tazobactam
Reproduction studies have been performed in rats and have revealed no evidence of impaired fertility due to tazobactam administered at doses up to 3 times the maximum recommended human daily dose based on body-surface area (mg/m2).
Teratology studies have been performed in mice and rats and have revealed no evidence of harm to the fetus due to tazobactam administered at doses up to 6 and 14 times, respectively, the human dose based on body-surface area (mg/m2). In rats, tazobactam crosses the placenta. Concentrations in the fetus are less than or equal to 10% of those found in maternal plasma.
There are, however, no adequate and well-controlled studies with the piperacillin/tazobactam combination or with piperacillin or tazobactam alone in pregnant women. Because animal reproduction studies are not always predictive of the human response, this drug should be used during pregnancy only if clearly needed.
Nursing Mothers
Piperacillin is excreted in low concentrations in human milk; tazobactam concentrations in human milk have not been studied. Caution should be exercised when ZOSYN is administered to a nursing woman.
Pediatric Use
Use of ZOSYN in pediatric patients 2 months of age or older with appendicitis and/or peritonitis is supported by evidence from well-controlled studies and pharmacokinetic studies in adults and in pediatric patients. This includes a prospective, randomized, comparative, open-label clinical trial with 542 pediatric patients 2-12 years of age with complicated intra-abdominal infections, in which 273 pediatric patients received piperacillin/tazobactam. Safety and efficacy in pediatric patients less than 2 months of age have not been established (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
There are no dosage recommendations for ZOSYN in pediatric patients with impaired renal function.
Geriatric Use
Patients over 65 years are not at an increased risk of developing adverse effects solely because of age. However, dosage should be adjusted in the presence of renal insufficiency. (See DOSAGE AND ADMINISTRATION.)
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
The approximate total sodium content for ZOSYN in Galaxy Containers is 5.58 mEq (128 mg) per 50 mL in the 2.25 g dose, 8.38 mEq (192 mg) per 50 mL in the 3.375 g dose, and 11.17 mEq (256 mg) per 100 mL in the 4.5 g dose. At the usual recommended doses, patients would receive approximately 790 to 1050 mg/day (33.5 to 44.6 mEq) of sodium. The geriatric population may respond with a blunted natriuresis to salt loading. This may be clinically important with regard to such diseases as congestive heart failure.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
-
ADVERSE REACTIONS
Adverse Events From Clinical Trials
During the initial clinical investigations, 2621 patients worldwide were treated with ZOSYN in phase 3 trials. In the key North American clinical trials (n=830 patients), 90% of the adverse events reported were mild to moderate in severity and transient in nature. However, in 3.2% of the patients treated worldwide, ZOSYN was discontinued because of adverse events primarily involving the skin (1.3%), including rash and pruritus; the gastrointestinal system (0.9%), including diarrhea, nausea, and vomiting; and allergic reactions (0.5%).
Adverse local reactions that were reported, irrespective of relationship to therapy with ZOSYN, were phlebitis (1.3%), injection site reaction (0.5%), pain (0.2%), inflammation (0.2%), thrombophlebitis (0.2%), and edema (0.1%).
Based on patients from the North American trials (n=1063), the events with the highest incidence in patients, irrespective of relationship to ZOSYN therapy, were diarrhea (11.3%); headache (7.7%); constipation (7.7%); nausea (6.9%); insomnia (6.6%); rash (4.2%), including maculopapular, bullous, urticarial, and eczematoid; vomiting (3.3%); dyspepsia (3.3%); pruritus (3.1%); stool changes (2.4%); fever (2.4%); agitation (2.1%); pain (1.7%); moniliasis (1.6%); hypertension (1.6%); dizziness (1.4%); abdominal pain (1.3%); chest pain (1.3%); edema (1.2%); anxiety (1.2%); rhinitis (1.2%); and dyspnea (1.1%).
Additional adverse systemic clinical events reported in 1.0% or less of the patients in the initial North American trials are listed below within each body system.
Autonomic nervous system—hypotension, ileus, syncope
Body as a whole—rigors, back pain, malaise
Cardiovascular—tachycardia, including supraventricular and ventricular; bradycardia; arrhythmia, including atrial fibrillation, ventricular fibrillation, cardiac arrest, cardiac failure, circulatory failure, myocardial infarction
Central nervous system—tremor, convulsions, vertigo
Gastrointestinal—melena, flatulence, hemorrhage, gastritis, hiccough, ulcerative stomatitis
Pseudomembranous colitis was reported in one patient during the clinical trials. The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment. (see WARNINGS.)
Hearing and Vestibular system—tinnitus
Metabolic and Nutritional—symptomatic hypoglycemia, thirst
Musculoskeletal—myalgia, arthralgia
Platelets, Bleeding, Clotting—mesenteric embolism, purpura, epistaxis, pulmonary embolism (see PRECAUTIONS, General.)
Psychiatric—confusion, hallucination, depression
Reproductive, Female—leukorrhea, vaginitis
Respiratory—pharyngitis, pulmonary edema, bronchospasm, coughing
Skin and Appendages—genital pruritus, diaphoresis
Special senses—taste perversion
Urinary—retention, dysuria, oliguria, hematuria, incontinence
Vascular (extracardiac)—flushing
Nosocomial Pneumonia Trials
In a completed study of nosocomial lower respiratory tract infections, 222 patients were treated with ZOSYN in a dosing regimen of 4.5 g every 6 hours in combination with an aminoglycoside and 215 patients were treated with imipenem/cilastatin (500 mg/500 mg q6h) in combination with an aminoglycoside. In this trial, treatment-emergent adverse events were reported by 402 patients, 204 (91.9%) in the piperacillin/tazobactam group and 198 (92.1%) in the imipenem/cilastatin group. Twenty-five (11.0%) patients in the piperacillin/tazobactam group and 14 (6.5%) in the imipenem/cilastatin group (p > 0.05) discontinued treatment due to an adverse event.
In this study of ZOSYN in combination with an aminoglycoside, adverse events that occurred in more than 1% of patients and were considered by the investigator to be drug-related were: diarrhea (17.6%), fever (2.7%), vomiting (2.7%), urinary tract infection (2.7%), rash (2.3%), abdominal pain (1.8%), generalized edema (1.8%), moniliasis (1.8%), nausea (1.8%), oral moniliasis (1.8%), BUN increased (1.8%), creatinine increased (1.8%), peripheral edema (1.8%), abdomen enlarged (1.4%), headache (1.4%), constipation (1.4%), liver function tests abnormal (1.4%), thrombocythemia (1.4%), excoriations (1.4%), and sweating (1.4%).
Drug-related adverse events reported in 1% or less of patients in the nosocomial pneumonia study of ZOSYN with an aminoglycoside were: acidosis, acute kidney failure, agitation, alkaline phosphatase increased, anemia, asthenia, atrial fibrillation, chest pain, CNS depression, colitis, confusion, convulsion, cough increased, thrombocytopenia, dehydration, depression, diplopia, drug level decreased, dry mouth, dyspepsia, dysphagia, dyspnea, dysuria, eosinophilia, fungal dermatitis, gastritis, glossitis, grand mal convulsion, hematuria, hyperglycemia, hypernatremia, hypertension, hypertonia, hyperventilation, hypochromic anemia, hypoglycemia, hypokalemia, hyponatremia, hypophosphatemia, hypoxia, ileus, injection site edema, injection site pain, injection site reaction, kidney function abnormal, leukocytosis, leukopenia, local reaction to procedure, melena, pain, prothrombin decreased, pruritus, respiratory disorder, SGOT increased, SGPT increased, sinus bradycardia, somnolence, stomatitis, stupor, tremor, tachycardia, ventricular extrasystoles, and ventricular tachycardia.
In a previous nosocomial pneumonia study conducted with a dosing regimen of 3.375 g given every 4 hours with an aminoglycoside, the following adverse events, irrespective of drug relationship, were observed: diarrhea (20%); constipation (8.4%); agitation (7.1%); nausea (5.8%); headache (4.5%); insomnia (4.5%); oral thrush (3.9%); erythematous rash (3.9%); anxiety (3.2%); fever (3.2%); pain (3.2%); pruritus (3.2%); hiccough (2.6%); vomiting (2.6%); dyspepsia (1.9%); edema (1.9%); fluid overload (1.9%); stool changes (1.9%); anorexia (1.3%); cardiac arrest (1.3%); confusion (1.3%); diaphoresis (1.3%); duodenal ulcer (1.3%); flatulence (1.3%); hypertension (1.3%); hypotension (1.3%); inflammation at injection site (1.3%); pleural effusion (1.3%); pneumothorax (1.3%); rash, not otherwise specified (1.3%); supraventricular tachycardia (1.3%); thrombophlebitis (1.3%); and urinary incontinence (1.3%).
Adverse events irrespective of drug relationship observed in 1% or less of patients in the above study with ZOSYN and an aminoglycoside included: aggressive reaction (combative), angina, asthenia, atelectasis, balanoposthitis, cerebrovascular accident, chest pain, conjunctivitis, deafness, dyspnea, earache, ecchymosis, fecal incontinence, gastric ulcer, gout, hemoptysis, hypoxia, pancreatitis, perineal irritation/pain, urinary tract infection with trichomonas, vitamin B12 deficiency anemia, xerosis, and yeast in urine.
Pediatrics
Studies of ZOSYN in pediatric patients suggest a similar safety profile to that seen in adults. In a prospective, randomized, comparative, open-label clinical trial of pediatric patients with severe intra-abdominal infections (including appendicitis and/or peritonitis), 273 patients were treated with ZOSYN (112.5 mg/kg every 8 hours) and 269 patients were treated with cefotaxime (50 mg/kg) plus metronidazole (7.5 mg/kg) every 8 hours. In this trial, treatment-emergent adverse events were reported by 146 patients, 73 (26.7%) in the ZOSYN group and 73 (27.1%) in the cefotaxime/metronidazole group. Six patients (2.2%) in the ZOSYN group and 5 patients (1.9%) in the cefotaxime/metronidazole group discontinued due to an adverse event.
In this study, adverse events that were reported in more than 1% of patients, irrespective of relationship to therapy with ZOSYN, were: diarrhea (7.0%), fever (4.8%), vomiting (3.7%), local reaction (3.3%), abscess (2.2%), sepsis (2.2%), abdominal pain (1.8%), infection (1.8%), bloody diarrhea (1.1%), pharyngitis (1.5%), constipation (1.1%), and SGOT increase (1.1%).
Adverse events reported in 1% or less of pediatric patients receiving ZOSYN are consistent with adverse events reported in adults.
Additional controlled studies in pediatric patients showed a similar safety profile as that described above.
Post-Marketing Experience
Additional adverse events reported from worldwide marketing experience with ZOSYN, occurring under circumstances where causal relationship to ZOSYN is uncertain:
Gastrointestinal—hepatitis, cholestatic jaundice
Hematologic—hemolytic anemia, anemia, thrombocytosis, agranulocytosis, pancytopenia
Immune––hypersensitivity reactions, anaphylactic/anaphylactoid reactions (including shock)
Infections––candidal superinfections
Renal—interstitial nephritis, renal failure
Skin and Appendages—erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis
Post-marketing experience with ZOSYN in pediatric patients suggests a similar safety profile to that seen in adults.
Adverse Laboratory Events (Seen During Clinical Trials)
Of the studies reported, including that of nosocomial lower respiratory tract infections in which a higher dose of ZOSYN was used in combination with an aminoglycoside, changes in laboratory parameters, without regard to drug relationship, include:
Hematologic—decreases in hemoglobin and hematocrit, thrombocytopenia, increases in platelet count, eosinophilia, leukopenia, neutropenia. The leukopenia/neutropenia associated with ZOSYN administration appears to be reversible and most frequently associated with prolonged administration, i.e., ≥ 21 days of therapy. These patients were withdrawn from therapy; some had accompanying systemic symptoms (e.g., fever, rigors, chills).
Coagulation—positive direct Coombs' test, prolonged prothrombin time, prolonged partial thromboplastin time
Hepatic—transient elevations of AST (SGOT), ALT (SGPT), alkaline phosphatase, bilirubin
Renal—increases in serum creatinine, blood urea nitrogen
Urinalysis—proteinuria, hematuria, pyuria
Additional laboratory events include abnormalities in electrolytes (i.e., increases and decreases in sodium, potassium, and calcium), hyperglycemia, decreases in total protein or albumin, blood glucose decreased, gamma-glutamyltransferase increased, hypokalemia, and bleeding time prolonged.
The following adverse reaction has also been reported for PIPRACIL® (piperacillin for injection):
Skeletal—prolonged muscle relaxation (see PRECAUTIONS, Drug Interactions.)
Piperacillin therapy has been associated with an increased incidence of fever and rash in cystic fibrosis patients.
-
OVERDOSAGE
There have been post-marketing reports of overdose with piperacillin/tazobactam. The majority of those events experienced, including nausea, vomiting, and diarrhea, have also been reported with the usual recommended dosages. Patients may experience neuromuscular excitability or convulsions if higher than recommended doses are given intravenously (particularly in the presence of renal failure).
Treatment should be supportive and symptomatic according to the patient's clinical presentation. Excessive serum concentrations of either piperacillin or tazobactam may be reduced by hemodialysis. Following a single 3.375 g dose of piperacillin/tazobactam, the percentage of piperacillin and tazobactam dose removed by hemodialysis was approximately 31% and 39%, respectively. (See CLINICAL PHARMACOLOGY.)
-
DOSAGE AND ADMINISTRATION
ZOSYN should be administered by intravenous infusion over 30 minutes.
The usual daily dose of ZOSYN for adults is 3.375 g every six hours totaling 13.5 g (12.0 g piperacillin/1.5 g tazobactam).
Nosocomial Pneumonia
Initial presumptive treatment of patients with nosocomial pneumonia should start with ZOSYN at a dosage of 4.5 g every six hours plus an aminoglycoside, totaling 18.0 g (16.0 g piperacillin/2.0 g tazobactam). Treatment with the aminoglycoside should be continued in patients from whom Pseudomonas aeruginosa is isolated. If Pseudomonas aeruginosa is not isolated, the aminoglycoside may be discontinued at the discretion of the treating physician.
Due to the in vitro inactivation of the aminoglycoside by beta-lactam antibiotics, ZOSYN and the aminoglycoside are recommended for separate administration. ZOSYN and the aminoglycoside should be reconstituted, diluted, and administered separately when concomitant therapy with aminoglycosides is indicated. (See PRECAUTIONS, Drug Interactions.)
In circumstances where coadministration via Y-site is necessary, reformulated ZOSYN containing EDTA supplied in Galaxy containers is compatible for simultaneous coadministration via Y-site infusion only with the following aminoglycosides under the following conditions:
The following compatibility information does not apply to the ZOSYN (piperacillin/tazobactam) formulation not containing EDTA. This information does not apply to ZOSYN in vials or bulk pharmacy containers. Refer to the package insert for ZOSYN vials or bulk pharmacy containers for instructions.
TABLE 5 Aminoglycoside ZOSYN Dose
(grams)Aminoglycoside Concentration Range*
(mg/mL)Acceptable
DiluentsAmikacin 2.25, 3.375,
4.51.75 – 7.5 0.9% Sodium Chloride or 5% Dextrose Gentamicin 2.25, 3.375, 4.5 0.7 – 3.32 0.9% Sodium Chloride or 5% Dextrose *The concentration ranges in Table 5 are based on administration of the aminoglycoside in divided doses (10-15 mg/kg/day in two daily doses for amikacin and 3-5 mg/kg/day in three daily doses for gentamicin). Administration of amikacin or gentamicin in a single daily dose or in doses exceeding those stated above via Y-site with ZOSYN containing EDTA has not been evaluated. See package insert for each aminoglycoside for complete Dosage and Administration instructions.
ZOSYN is not compatible with tobramycin for simultaneous coadministration via Y-site infusion. Compatibility of ZOSYN with other aminoglycosides has not been established. Only the concentration and diluents for amikacin or gentamicin with the dosages of ZOSYN listed above have been established as compatible for coadministration via Y-site infusion. Simultaneous coadministration via Y-site infusion in any manner other than listed above may result in inactivation of the aminoglycoside by ZOSYN.
Renal Insufficiency
In patients with renal insufficiency (Creatinine Clearance ≤ 40 mL/min), the intravenous dose of ZOSYN should be adjusted to the degree of actual renal function impairment. In patients with nosocomial pneumonia receiving concomitant aminoglycoside therapy, the aminoglycoside dosage should be adjusted according to the recommendations of the manufacturer. The recommended daily doses of ZOSYN for patients with renal insufficiency are as follows:
Recommended Dosing of ZOSYN in Patients with Normal Renal Function and Renal Insufficiency (As total grams piperacillin/tazobactam) Renal Function
(Creatinine Clearance,
mL/min)All Indications (except nosocomial pneumonia) Nosocomial Pneumonia >40 mL/min 3.375 q 6 h 4.5 q 6 h 20-40 mL/min* 2.25 q 6 h 3.375 q 6 h <20 mL/min* 2.25 q 8 h 2.25 q 6 h Hemodialysis** 2.25 q 12 h 2.25 q 8 h CAPD 2.25 q 12 h 2.25 q 8 h * Creatinine clearance for patients not receiving hemodialysis
** 0.75 g should be administered following each hemodialysis session on hemodialysis daysFor patients on hemodialysis, the maximum dose is 2.25 g every twelve hours for all indications other than nosocomial pneumonia and 2.25 g every eight hours for nosocomial pneumonia. Since hemodialysis removes 30% to 40% of the administered dose, an additional dose of 0.75 g ZOSYN should be administered following each dialysis period on hemodialysis days. No additional dosage of ZOSYN is necessary for CAPD patients.
Duration of Therapy
The usual duration of ZOSYN treatment is from seven to ten days. However, the recommended duration of ZOSYN treatment of nosocomial pneumonia is 7 to 14 days. In all conditions, the duration of therapy should be guided by the severity of the infection and the patient's clinical and bacteriological progress.
Pediatric Patients
For children with appendicitis and/or peritonitis 9 months of age or older, weighing up to 40 kg, and with normal renal function, the recommended ZOSYN dosage is 100 mg piperacillin/12.5 mg tazobactam per kilogram of body weight, every 8 hours. For pediatric patients between 2 months and 9 months of age, the recommended ZOSYN dosage based on pharmacokinetic modeling, is 80 mg piperacillin/10 mg tazobactam per kilogram of body weight, every 8 hours (see PRECAUTIONS, General, Pediatric Use and CLINICAL PHARMACOLOGY). Pediatric patients weighing over 40 kg and with normal renal function should receive the adult dose. There are no dosage recommendations for ZOSYN in pediatric patients with impaired renal function.
ZOSYN in Galaxy containers should not be used in pediatric patients who require less than the full adult dose of ZOSYN in order to prevent unintentional overdose. The other available formulations of ZOSYN can be used in this population.
DIRECTIONS FOR USE OF ZOSYN (PIPERACILLIN AND TAZOBACTAM INJECTION) IN GALAXY CONTAINERS (PL 2040 PLASTIC)
ZOSYN Injection (PL 2040 Plastic) is to be administered using sterile equipment after thawing to room temperature.
Zosyn containg EDTA is compatible for co-administration via a Y-site intravenous tube with Lactated Ringer's injection, USP.
Administer by infusion over a period of at least 30 minutes. During the infusion it is desirable to discontinue the primary infusion solution.
ZOSYN should not be mixed with other drugs in a syringe or infusion bottle since compatibility has not been established.
ZOSYN is not chemically stable in solutions that contain only sodium bicarbonate and solutions that significantly alter the pH.
ZOSYN should not be added to blood products or albumin hydrolysates.
- STORAGE
-
THAWING OF PLASTIC CONTAINER
Thaw frozen container at room temperature 20°C to 25°C [68°F to 77°F] or under refrigeration (2°C to 8°C [36°F to 46°F]). DO NOT FORCE THAW BY IMMERSION IN WATER BATHS OR BY MICROWAVE IRRADIATION.
Check for minute leaks by squeezing container firmly. If leaks are detected, discard solution as sterility may be impaired.
The container should be visually inspected. Components of the solution may precipitate in the frozen state and will dissolve upon reaching room temperature with little or no agitation. Potency is not affected. Agitate after solution has reached room temperature. If after visual inspection the solution remains cloudy or if an insoluble precipitate is noted or if any seals or outlet ports are not intact, the container should be discarded.
The thawed solution is stable for 14 days under refrigeration (2°C to 8°C [36°F to 46°F]) or 24 hours at room temperature 20°C to 25°C [68°F to 77°F]. DO NOT REFREEZE THAWED ANTIBIOTICS.
DO NOT ADD SUPPLEMENTARY MEDICATION.
UNUSED PORTIONS OF ZOSYN SHOULD BE DISCARDED.
CAUTION: Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is complete.
Preparation for administration:
- Suspend container from eyelet support.
- Remove protector from outlet port at bottom of container.
- Attach administration set. Refer to complete directions accompanying set.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
-
HOW SUPPLIED
ZOSYN (piperacillin and tazobactam injection) in Galaxy Container (PL 2040 Plastic) is supplied as a frozen, iso-osmotic, sterile, nonpyrogenic solution in single-dose plastic containers as follows:
2.25 g (piperacillin sodium equivalent to 2 g piperacillin/tazobactam sodium equivalent to 0.25 g tazobactam) in 50 mL. Each container has 5.58 mEq (128 mg) of sodium. Supplied 24/box—NDC: 0206-2409-02
3.375 g (piperacillin sodium equivalent to 3 g piperacillin/tazobactam sodium equivalent to 0.375 g tazobactam) in 50 mL. Each container has 8.38 mEq (192 mg) of sodium. Supplied 24/box—NDC: 0206-2411-02
4.5 g (piperacillin sodium equivalent to 4 g piperacillin/tazobactam sodium equivalent to 0.5 g tazobactam) in 100 mL. Each container has 11.17 mEq (256 mg) of sodium. Supplied 12/box—NDC: 0206-2413-02
Store at or below -20°C (-4°F). [See DOSAGE AND ADMINISTRATION, DIRECTIONS FOR USE OF ZOSYN (PIPERACILLIN AND TAZOBACTAM INJECTION) IN GALAXY CONTAINERS (PL 2040 PLASTIC).]
Also Available
ZOSYN (piperacillin and tazobactam for injection, USP) is also supplied as follows:
2.25 g single-dose vial containing piperacillin sodium equivalent to 2 g of piperacillin and tazobactam sodium equivalent to 0.25 g of tazobactam. Each vial contains 5.58 mEq (128 mg) of sodium. Supplied 10/box—NDC: 0206-2404-02
3.375 g single-dose vial containing piperacillin sodium equivalent to 3 g of piperacillin and tazobactam sodium equivalent to 0.375 g of tazobactam. Each vial contains 8.38 mEq (192 mg) of sodium. Supplied 10/box—NDC: 0206-2405-02
4.5 g single-dose vial containing piperacillin sodium equivalent to 4 g of piperacillin and tazobactam sodium equivalent to 0.5 g of tazobactam. Each vial contains 11.17 mEq (256 mg) of sodium. Supplied 10/box—NDC: 0206-2408-02
Also Available
ZOSYN (piperacillin and tazobactam for injection, USP) is also supplied as a powder in the pharmacy bulk vial as follows:
40.5 g pharmacy-bulk vial containing piperacillin sodium equivalent to 36 grams of piperacillin and tazobactam sodium equivalent to 4.5 grams of tazobactam. Each pharmacy-bulk vial contains 100.4 mEq (2,304 mg) of sodium. NDC: 0206-2416-01
ZOSYN (piperacillin and tazobactam for injection, USP) vials should be stored at controlled room temperature 20°C to 25°C (68°F to 77°F) prior to reconstitution.
-
REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; 21st Informational Supplement. CLSI document M100-S21. CLSI, 940 West Valley Rd., Suite 1400, Wayne, PA 19087, 2011
- CLSI. Methods for Dilution Antimicrobial Susceptibility Test for Bacteria that Grow Aerobically; Approved Standard – 8th ed. CLSI document M07-A8, 2009.
- CLSI. Performance Standards for Antimicrobial Disk Susceptibility Test; Approved Standard – 10th ed. CLSI document M02-A10, 2009.
- CLSI. Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; Approved Standard – 7th ed. CLSI document M11-A7, 2007
DIASTIX is a registered trademark of Bayer Healthcare LLC.
CLINITEST is a registered trademark of Siemens Healthcare Diagnostics Inc.
Galaxy is a registered trademark of Baxter International Inc.

This product's label may have been updated. For current package insert and further product information, please visit www.pfizer.com or call our medical communications department toll-free at 1‑800‑438‑1985. 
Distributed by Wyeth Pharmaceuticals Inc., a subsidiary of Pfizer Inc.
Manufactured by Baxter Healthcare Corporation, Deerfield, IL 60015

Novation and NOVAPLUS are registered trademarks of Novation LLC.
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 2.25 G SINGLE DOSE CONTAINER
NDC: 0206-2409-01
(Piperacillin and Tazobactam Injection)
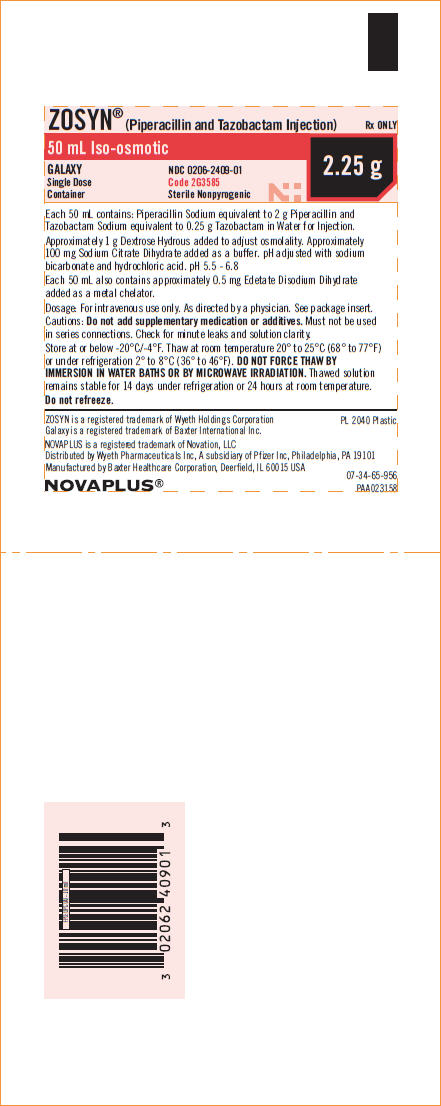
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 2.25 G - LABEL UNIT
NDC: 0206-2409-02
(Piperacillin and Tazobactam Injection)
12 – 50 mL Single Dose Containers
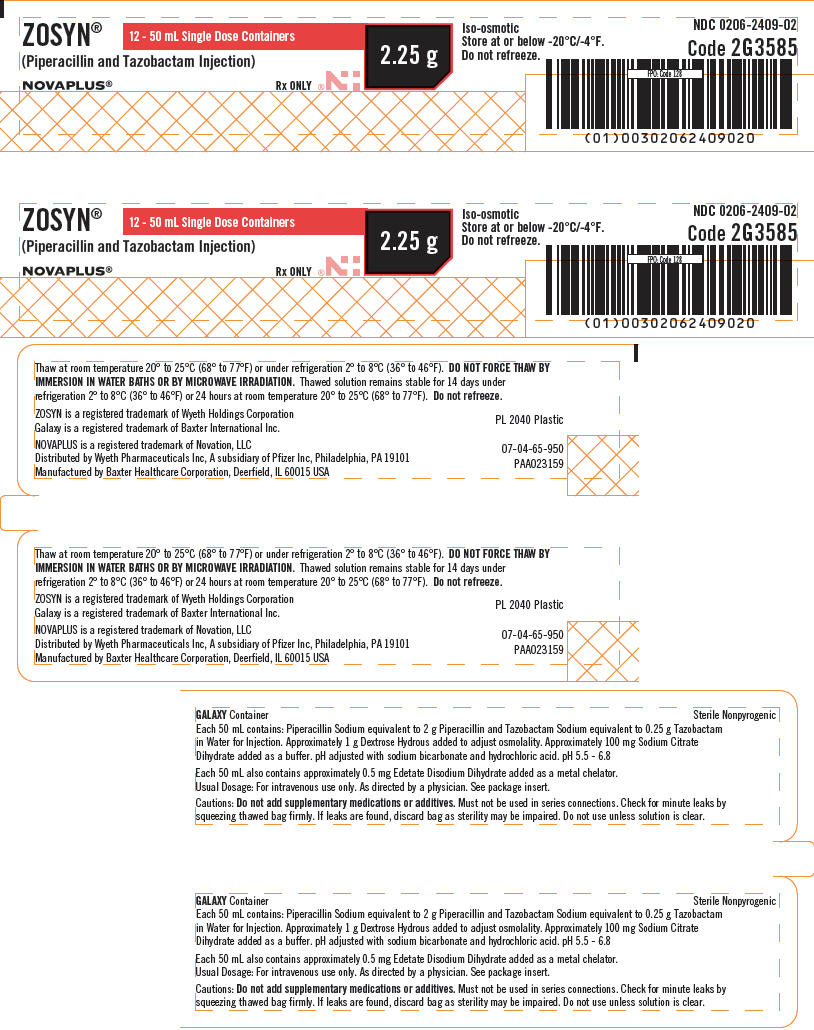
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 3.375 G - SINGLE DOSE CONTAINER
NDC: 0206-2411-01
(Piperacillin and Tazobactam Injection)
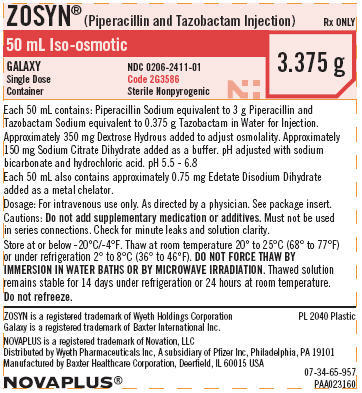
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 3.375 G - LABEL UNIT
NDC: 0206-2411-02
(Piperacillin and Tazobactam Injection)
12 – 50 mL Single Dose Containers
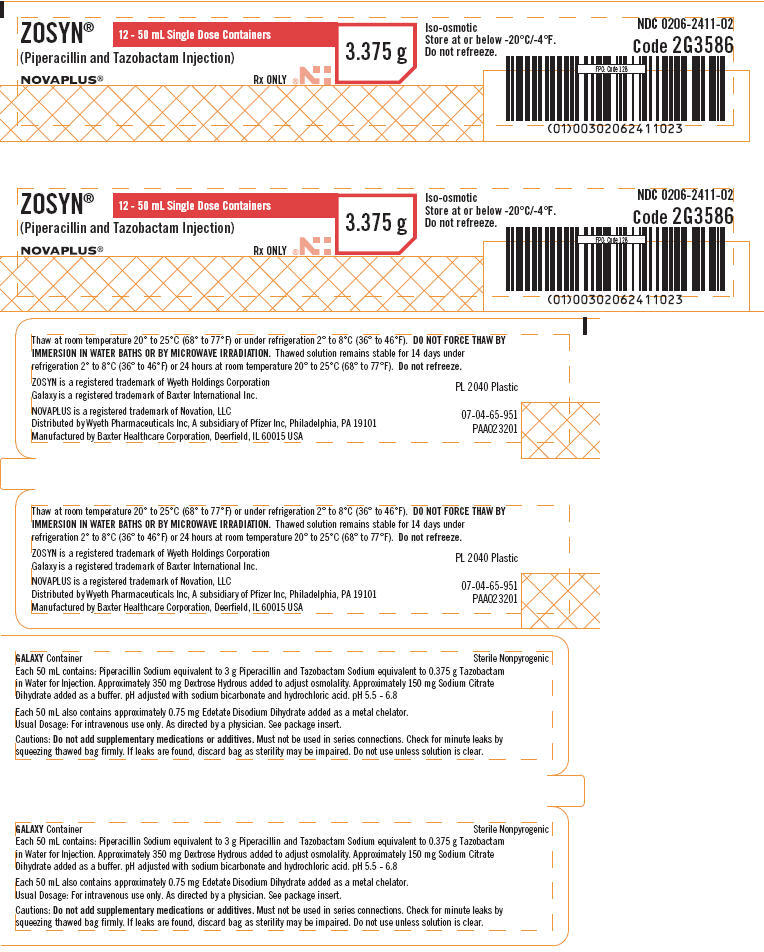
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 4.5 G - SINGLE DOSE CONTAINER
NDC: 0206-2413-01
(Piperacillin and Tazobactam Injection)
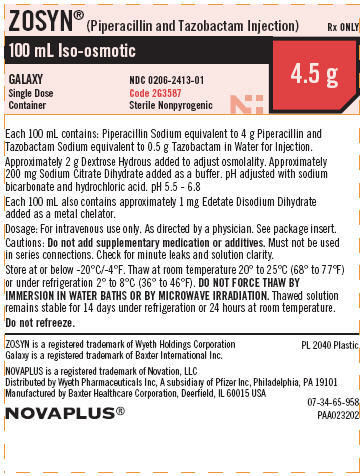
-
PRINCIPAL DISPLAY PANEL
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - 4.5 G - LABEL UNIT
NDC: 0206-2413-02
(Piperacillin and Tazobactam Injection)
6 – 100 mL Single Dose Containers
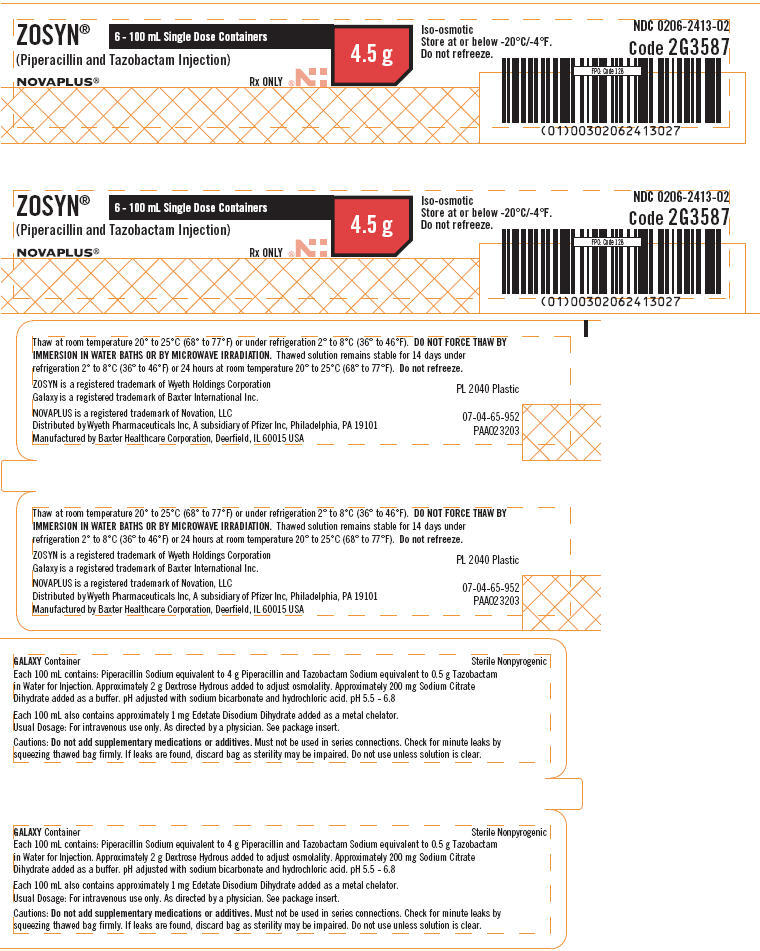
-
INGREDIENTS AND APPEARANCE
ZOSYN IN GALAXY CONTAINERS
piperacillin sodium and tazobactam sodium injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0206-2409 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PIPERACILLIN SODIUM (UNII: M98T69Q7HP) (PIPERACILLIN ANHYDROUS - UNII:9I628532GX) PIPERACILLIN ANHYDROUS 2 g in 50 mL TAZOBACTAM SODIUM (UNII: UXA545ABTT) (TAZOBACTAM - UNII:SE10G96M8W) TAZOBACTAM 250 mg in 50 mL Inactive Ingredients Ingredient Name Strength DEXTROSE MONOHYDRATE (UNII: LX22YL083G) 1 g in 50 mL SODIUM CITRATE (UNII: 1Q73Q2JULR) 100 mg in 50 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.5 mg in 50 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0206-2409-02 24 in 1 BOX 1 NDC: 0206-2409-01 50 mL in 1 BAG Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050750 03/01/1998 ZOSYN IN GALAXY CONTAINERS
piperacillin sodium and tazobactam sodium injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0206-2411 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PIPERACILLIN SODIUM (UNII: M98T69Q7HP) (PIPERACILLIN ANHYDROUS - UNII:9I628532GX) PIPERACILLIN ANHYDROUS 3 g in 50 mL TAZOBACTAM SODIUM (UNII: UXA545ABTT) (TAZOBACTAM - UNII:SE10G96M8W) TAZOBACTAM 375 mg in 50 mL Inactive Ingredients Ingredient Name Strength SODIUM BICARBONATE (UNII: 8MDF5V39QO) HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) DEXTROSE MONOHYDRATE (UNII: LX22YL083G) 350 mg in 50 mL SODIUM CITRATE (UNII: 1Q73Q2JULR) 150 mg in 50 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 0.75 mg in 50 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0206-2411-02 24 in 1 BOX 1 NDC: 0206-2411-01 50 mL in 1 BAG Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050750 03/01/1998 ZOSYN IN GALAXY CONTAINERS
piperacillin sodium and tazobactam sodium injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0206-2413 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PIPERACILLIN SODIUM (UNII: M98T69Q7HP) (PIPERACILLIN ANHYDROUS - UNII:9I628532GX) PIPERACILLIN ANHYDROUS 4 g in 100 mL TAZOBACTAM SODIUM (UNII: UXA545ABTT) (TAZOBACTAM - UNII:SE10G96M8W) TAZOBACTAM 500 mg in 100 mL Inactive Ingredients Ingredient Name Strength SODIUM BICARBONATE (UNII: 8MDF5V39QO) HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) DEXTROSE MONOHYDRATE (UNII: LX22YL083G) 2 g in 100 mL EDETATE DISODIUM (UNII: 7FLD91C86K) 1 mg in 100 mL SODIUM CITRATE (UNII: 1Q73Q2JULR) 200 mg in 100 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0206-2413-02 12 in 1 BOX 1 NDC: 0206-2413-01 100 mL in 1 BAG Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA050750 03/01/1998 Labeler - Wyeth Pharmaceuticals Inc., a subsidiary of Pfizer Inc. (828831441) Establishment Name Address ID/FEI Business Operations Baxter Healthcare Corporation 194684502 ANALYSIS(0206-2413, 0206-2411, 0206-2409) , MANUFACTURE(0206-2413, 0206-2411, 0206-2409)
Trademark Results [Zosyn]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ZOSYN 74400770 1915777 Live/Registered |
WYETH HOLDINGS LLC 1993-06-11 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.