SEZABY- phenobarbital sodium injection
SEZABY by
Drug Labeling and Warnings
SEZABY by is a Prescription medication manufactured, distributed, or labeled by Sun Pharmaceutical Industries, Inc., Sun Pharmaceutical Medicare Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SEZABY safely and effectively. See full prescribing information for SEZABY.
SEZABY™ (phenobarbital sodium) for injection, for intravenous use, CIV
Initial U.S. Approval: 2022WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; DEPENDENCE AND WITHDRAWAL REACTIONS AFTER USE OF SEZABY FOR A LONGER DURATION THAN RECOMMENDED; and ABUSE, MISUSE, AND ADDICTION WITH UNAPPROVED USE IN ADOLESCENTS AND ADULTS
See full prescribing information for complete boxed warning.
- Concomitant use of phenobarbital products, including SEZABY, and opioids may result in profound sedation, respiratory depression, coma, and death. If a decision is made to use concomitantly, limit dosages and durations to the minimum required, and monitor patients for respiratory depression and sedation. (5.1, 7.3)
- Although SEZABY is indicated only for short-term use (1, 2), if used for a longer duration than recommended, abrupt discontinuation or rapid dosage reduction may precipitate acute withdrawal reactions, which can be life-threatening. For patients receiving SEZABY for a longer duration than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue SEZABY. (5.2)
- SEZABY is not approved for use in adolescents or adults. The unapproved use of SEZABY in adolescents and adults exposes them to risks of abuse, misuse, and addiction, which can lead to overdose or death. (5.3)
INDICATIONS AND USAGE
SEZABY is a barbiturate indicated for the treatment of neonatal seizures in term and preterm infants. (1)
DOSAGE AND ADMINISTRATION
- Loading Dose: 20 mg/kg is administered by intravenous infusion over 15 minutes into a large peripheral vein. If clinically indicated, at least 15 minutes after completion of the initial loading dose, a second loading dose may be administered over the subsequent 15 minutes as 20 mg/kg for term infants or 10 mg/kg or 20 mg/kg for preterm infants. The maximum total loading dose is 40 mg/kg. (2.1)
-
Maintenance Dosage: starting 8 to 12 hours after first loading dose:
4.5 mg/kg/day given in 2 or 3 divided doses (i.e., 1.5 mg/kg every 8 hours or 2.25 mg/kg every 12 hours) up to 5 days. (2.1). - Must be reconstituted with 10 mL 0.9 % Sodium Chloride Injection, USP prior to administration. See additional preparation and administration instructions in the Full Prescribing Information. (2.3)
DOSAGE FORMS AND STRENGTHS
For injection: 100 mg of phenobarbital sodium lyophilized powder in a single-dose vial for reconstitution (3)
CONTRAINDICATIONS
- Acute porphyrias (4)
- Hypersensitivity to phenobarbital or other barbiturates (4)
WARNINGS AND PRECAUTIONS
- Respiratory Depression or Insufficiency: Abnormal respiration has been observed; careful respiratory monitoring is recommended during and after treatment. (5.4)
- Serious Dermatologic Reactions: Serious and sometimes fatal hypersensitivity reactions, including toxic epidermal necrolysis and Stevens-Johnson syndrome, have been reported. SEZABY should be discontinued at the first sign of a rash, unless the rash is clearly not drug related. (5.5)
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan hypersensitivity: DRESS can be fatal or life-threatening. If signs or symptoms of DRESS are present, evaluate the patient immediately. Discontinue if an alternative etiology cannot be established. (5.6)
- Infusion Site Reactions: SEZABY may cause tissue damage with necrosis; avoid perivascular extravasation or intra-arterial injection. Stop SEZABY if evidence of pain, swelling, discoloration, or temperature change in limb. (5.9)
- QT Prolongation: Avoid concomitant use of SEZABY in patients who are at significant risk of developing torsade de pointes and with products that may increase the risk of the QTc interval prolongation or products that may increase concentrations of SEZABY. (5.10)
ADVERSE REACTIONS
The most common adverse reactions (incidence > 5% patients overall) are abnormal respiration, sedation, feeding disorder, and hypotension. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sun Pharmaceutical Industries, Inc. at 1-800-818-4555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- CYP2C9, 2C19, 2E1, UGT Inhibitors: Closely monitor and decrease SEZABY dosage, if needed. (7.1)
- CYP3A4, 2B6, 2C, UGT Substrates: Substrate dosage adjustment may be needed. (7.1)
- CNS depressants: Closely monitor for sedation and respiratory depression. (7.2)
- Drugs that Prolong the QT Interval: Avoid concomitant use. (7.3)
Revised: 12/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; DEPENDENCE AND WITHDRAWAL REACTIONS AFTER USE OF SEZABY FOR A LONGER DURATION THAN RECOMMENDED; and ABUSE, MISUSE AND ADDICTION WITH UNAPPROVED USE IN ADOLESCENTS AND ADULTS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage and Administration
2.2 Reconstitution and Additional Administration Instructions
2.3 Storage of Reconstituted Solution
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risks from Concomitant Use with Opioids
5.2 Dependence and Withdrawal Reactions After Use of SEZABY for a Longer Duration Than Recommended
5.3 Abuse, Misuse, and Addiction with Unapproved Use in Adolescents and Adults
5.4 Respiratory Depression or Insufficiency
5.5 Serious Dermatologic Reactions
5.6 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
5.7 Hypersensitivity Reactions
5.8 Exacerbation of Porphyria
5.9 Infusion Site Reactions
5.10 QT Prolongation
5.11 Embryofetal Toxicity with Unapproved Use in Adolescents and Adults
5.12 Neonatal Adverse Reactions from Unapproved Maternal Phenobarbital Use
5.13 Sedation, Respiratory Depression, and Withdrawal in Neonates Exposed to Phenobarbital Through Breast Milk
5.14 Suicidal Behavior and Ideation with Unapproved Use in Adolescents and Adults
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Cytochrome P450- or Uridine 5’-diphospho-glucuronosyltransferase (UGT)-Based Interactions
7.2 CNS Depressants
7.3 Drugs that Prolong QT Interval
8 USE IN SPECIFIC POPULATIONS
8.4 Pediatric Use
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; DEPENDENCE AND WITHDRAWAL REACTIONS AFTER USE OF SEZABY FOR A LONGER DURATION THAN RECOMMENDED; and ABUSE, MISUSE AND ADDICTION WITH UNAPPROVED USE IN ADOLESCENTS AND ADULTS
Risks from Concomitant Use with Opioids
Concomitant use of phenobarbital products, including SEZABY, and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. If a decision is made for concomitant use of these drugs, limit dosages and durations to the minimum required, and follow patients for signs and symptoms of respiratory depression and sedation [see Warnings and Precautions (5.1) and Drug Interactions (7.3)].
Dependence and Withdrawal Reactions After Use of SEZABY for a Longer Duration than Recommended
The continued use of phenobarbital may lead to clinically significant physical dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily dose. Although SEZABY is indicated only for short-term use [see Indications and Usage (1) and Dosage and Administration (2)], if used for a longer duration than recommended, abrupt discontinuation or rapid dosage reduction of SEZABY may precipitate acute withdrawal reactions, which can be life-threatening. For patients receiving SEZABY for longer duration than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue SEZABY [see Warnings and Precautions (5.2)].
Abuse, Misuse, and Addiction with Unapproved Use in Adolescents and Adults
SEZABY is not approved for use in adolescents or adults. The unapproved use of SEZABY, in adolescents and adults exposes them to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of phenobarbital commonly involve concomitant use of other drugs, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes [see Warnings and Precaution (5.3)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage and Administration
The recommended dosage of SEZABY in neonates consists of a loading dose(s) followed by maintenance dosage (see Table 1). Administer SEZABY by intravenous infusion (over 15 minutes) into a large peripheral vein to avoid local tissue toxicity [see Warnings and Precautions (5.9)]. SEZABY is for intravenous use only.
Table 1: Recommended Dosage of SEZABY for Neonatal Seizures
Loading Dose (maximum total loading dose is 40 mg/kg)
First loading dose
20 mg/kg
Second loading dose
(If clinically indicated)1
Preterm Infants
10 mg/kg or 20 mg/kg [see Clinical Pharmacology (12.3)]
Term Infants
20 mg/kg
Maintenance Dosage (total daily dose is 4.5 mg/kg/day and the total duration is up to 5 days)
Initiate 8 to 12 hours after first loading dose
Option 1
1.5 mg/kg every 8 hours
Option 2
2.25 mg/kg every 12 hours
1If seizures persist or recur any time 15 minutes after completion of the initial loading dose, administer a second loading dose. (Administer the second loading dose no sooner than 15 minutes after completion of the first loading dose.)
2.2 Reconstitution and Additional Administration Instructions
- Determine the number of vials to be reconstituted based on the patient’s weight and recommended dose.
- Aseptically reconstitute the lyophilized powder in the vial using 10 mL of 0.9% Sodium Chloride Injection, USP.
- Swirl the vial gently until contents are completely dissolved.
- The reconstituted solution contains 100 mg per 10 mL (10 mg/mL) of phenobarbital sodium.
- Inspect the vial visually for particulate matter and discoloration prior to administration (the reconstituted solution is clear, colorless, and free from visible particulate matter).
- Discard the reconstituted solution if it is discolored or contains foreign particles.
- Withdraw the appropriate volume from the reconstituted vial for intravenous infusion and administer immediately [see Dosage and Administration (2.3)].
- Discard any unused portion of the reconstituted solution left in the vial [see Description (11)].
2.3 Storage of Reconstituted Solution
If the reconstituted solution is not administered immediately, place the vial back in the original carton to protect it from light and store at either room temperature at 20°C to 25°C (68°F to 77°F) for a maximum of 8 hours or in the refrigerator at 2°C to 8°C (36°F to 46°F) for a maximum of 24 hours. Discard any unused portion of the reconstituted solution after the recommended storage duration.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Risks from Concomitant Use with Opioids
Concomitant use of phenobarbital products, including SEZABY, and opioids may result in profound sedation, respiratory depression, coma, and death [see Drug Interactions (7.3)].
Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. If a decision is made for concomitant use of these drugs, limit dosages and durations to the minimum required, and follow patients for signs and symptoms of respiratory depression and sedation. Practitioners administering SEZABY must have the skills necessary to manage serious cardiorespiratory adverse reactions, including skills in airway management.
5.2 Dependence and Withdrawal Reactions After Use of SEZABY for a Longer Duration Than Recommended
The continued use of phenobarbital may lead to clinically significant physical dependence. Although SEZABY is indicated only for short-term use [see Indications and Usage (1) and Dosage and Administration (2)], if used for a longer duration than recommended, abrupt discontinuation or rapid dosage reduction of SEZABY may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) [see Drug Abuse and Dependence (9.3)].
To reduce the risk of withdrawal reactions in patients receiving SEZABY for a longer duration than recommended, use a gradual taper to discontinue SEZABY (a patient-specific plan should be used to taper the dose). Patients at an increased risk of withdrawal adverse reactions after phenobarbital discontinuation or rapid dosage reduction include those who received higher dosages, or those who had longer durations of use.
5.3 Abuse, Misuse, and Addiction with Unapproved Use in Adolescents and Adults
SEZABY is not approved for use in adolescents or adults. The unapproved use of SEZABY in adolescents and adults exposes them to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of barbiturates, including phenobarbital, often (but not always) involve the use of doses exceeding the doses used in clinical practice and commonly involve concomitant use of other drugs, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death [see Drug Abuse and Dependence (9.2)].
5.4 Respiratory Depression or Insufficiency
In Study 1, 25% of patients treated with phenobarbital developed abnormal respiration [see Adverse Reactions (6.1) and Clinical Studies (14)]. Careful respiratory monitoring is needed during and after the administration of SEZABY.
5.5 Serious Dermatologic Reactions
Serious and sometimes fatal dermatologic reactions, including toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS), have been reported with the use of phenobarbital.
SEZABY should be discontinued at the first sign of a rash, unless the rash is clearly not drug related. If signs or symptoms suggest SJS/TEN, use of SEZABY should not be resumed and alternative therapy should be considered. If a rash occurs, the patient should be evaluated for signs and symptoms of Drug Reaction with Eosinophilia and Systemic Symptoms [see Warnings and Precautions (5.6)].
5.6 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as multiorgan hypersensitivity, has been reported in patients taking antiepileptic drugs, including phenobarbital. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling, in association with other organ system involvement, such as hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis sometimes resembling an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its expression, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident.
If such signs or symptoms are present, the patient should be evaluated immediately. SEZABY should be discontinued if an alternative etiology for the signs or symptoms cannot be established.
5.7 Hypersensitivity Reactions
Phenobarbital-associated hypersensitivity reactions may include symptoms and signs such as rash, fever, facial or limb edema, and lymphadenopathy.
SEZABY is contraindicated in patients who have experienced hypersensitivity to phenobarbital or other barbiturates. Additionally, consider alternatives to structurally similar drugs such as carboxamides (e.g., carbamazepine) and hydantoins (e.g., phenytoin) in these same patients. Similarly, if there is a history of hypersensitivity reactions to these structurally similar drugs in the patient or immediate family members, consider alternatives to SEZABY. If signs or symptoms of hypersensitivity reactions are present in a patient treated with SEZABY, the patient should be evaluated immediately and SEZABY should be discontinued if an alternative etiology for the signs or symptoms cannot be established.
5.8 Exacerbation of Porphyria
SEZABY may precipitate acute attacks in patients with acute porphyrias. These episodes may be life-threatening, and include symptoms and signs such as anxiety, confusion, limb or abdominal pain, hyponatremia, seizures, and muscle weakness. Therefore, SEZABY is contraindicated in patients with acute porphyrias [see Contraindications (4)].
5.9 Infusion Site Reactions
SEZABY is highly alkaline [see Description (11)]. Therefore, extreme care should be taken to avoid perivascular extravasation or intra-arterial injection. Extravascular injection may cause local tissue damage with subsequent necrosis; consequences of intraarterial injection may vary from transient pain to gangrene of the limb. Any evidence of pain, swelling, discoloration, or temperature change in the limb warrants stopping the injection.
5.10 QT Prolongation
SEZABY may prolong the QT interval [see Clinical Pharmacology (12.2)].
Avoid use of SEZABY in patients who are at significant risk of developing torsade de pointes, including those with congenital long QT syndrome, uncontrolled or significant cardiac disease, recent myocardial infarction, heart failure, unstable angina, bradyarrhythmias, AV block, aortic stenosis, or uncontrolled hypothyroidism. If use cannot be avoided in these patients, collect ECGs during treatment at specified intervals as clinically indicated, and monitor serum electrolytes and correct abnormalities.
Avoid the concomitant use of products that may increase the risk of QTc interval prolongation or products that may increase concentrations of phenobarbital [see Drug Interactions (7.3)]. If concomitant use of a product that also prolongs the QTc interval or that increases SEZABY concentrations is unavoidable, monitor patients for increased risk of QTc interval prolongation.
5.11 Embryofetal Toxicity with Unapproved Use in Adolescents and Adults
SEZABY is not approved for use in adolescents or adults. Based on findings from prospective controlled trials, cohort studies, pregnancy registries, and randomized controlled-trials, phenobarbital can cause fetal harm when administered during pregnancy. Data from observational studies suggest an increased risk of major congenital malformations in infants of mothers who received phenobarbital during pregnancy.
5.12 Neonatal Adverse Reactions from Unapproved Maternal Phenobarbital Use
SEZABY is not approved for use in adolescents or adults. Phenobarbital crosses the placenta and may produce respiratory depression, hypotonia, and sedation in neonates of mothers who received phenobarbital during pregnancy. The use of SEZABY late in pregnancy can result in the following adverse reactions in neonates:
- Sedation (respiratory depression, lethargy, hypotonia) and/or
- Withdrawal reactions (hyperreflexia, irritability, restlessness, tremors, inconsolable crying and feeding difficulties).
Neonatal coagulation defects have also been reported within the first 24 hours in neonates exposed to phenobarbital during pregnancy.
5.13 Sedation, Respiratory Depression, and Withdrawal in Neonates Exposed to Phenobarbital Through Breast Milk
SEZABY is not approved for use in adolescents or adults. Phenobarbital is present and may accumulate in breast milk. Phenobarbital has been detected in some neonates exposed to breast milk from phenobarbital-treated mothers. There are reports of sedation, respiratory depression and withdrawal in infants exposed to phenobarbital through breast milk.
5.14 Suicidal Behavior and Ideation with Unapproved Use in Adolescents and Adults
SEZABY is not approved for use in adolescents or adults. Antiepileptic drugs (AEDs) increase the risk of suicidal thoughts or behavior in adolescents and adults.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that adult patients randomized to one of the AEDs had approximately twice the risk (adjusted relative risk 1.8, 95% confidence interval [CI]: 1.2, 2.7) of suicidal thinking or behavior compared to adult patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated adult patients was 0.43%, compared to 0.24% among 16,029 placebo-treated adult patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 adult patients treated. There were four suicides in drug-treated adult patients in the trials and none in placebo-treated adult patients, but the number was too small to allow any conclusion about AED effect on suicide.
The increased risk of suicidal thoughts or behavior in adults with AEDs was observed as early as one week after starting AED treatment and persisted for the duration of treatment assessed.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Risks from Concomitant Use with Opioids [see Warnings and Precautions (5.1)]
- Dependence and Withdrawal Reactions After Use of SEZABY for a Longer Duration Than Recommended [see Warnings and Precautions (5.2)]
- Abuse, Misuse, and Addiction with Unapproved Use in Adolescents and Adults [see Warnings and Precautions (5.3)]
- Respiratory Depression or Insufficiency [see Warnings and Precautions (5.4)]
- Serious Dermatologic Reactions [see Warnings and Precautions (5.5)]
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity [see Warnings and Precautions (5.6)]
- Hypersensitivity [see Warnings and Precautions (5.7)]
- Exacerbation of Porphyria [see Warnings and Precautions (5.8)]
- Injection Site Reactions [see Warnings and Precautions (5.9)]
- QT Prolongation [see Warnings and Precautions (5.10)]
- Embryofetal Toxicity with Unapproved Use in Adolescents and Adults [see Warnings and Precautions (5.11)]
- Neonatal Adverse Reactions from Unapproved Maternal Phenobarbital Use [see Warnings and Precautions (5.12)]
- Sedation, Respiratory Depression, and Withdrawal in Neonates Exposed to Phenobarbital Through Breast Milk [see Warnings and Precautions (5.13)]
- Suicidal Behavior and Ideation with Unapproved use in Adolescents and Adults [see Warnings and Precautions (5.14)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The Study 1 was a multicenter, randomized, double-blind, active-controlled study in neonates who were experiencing seizures [see Clinical Studies (14)]. Patients were infants younger than 14 days of age with gestational ages between 36 and 44 weeks. Overall, 106 neonates (51 female and 55 male) were randomized to receive either phenobarbital (N=42) or levetiracetam (N=64) as their initial treatment. Patients received up to two 15-minute infusions of their initially assigned treatment (loading dose(s)) followed by maintenance treatment of up to 5 days. Mean durations of phenobarbital and levetiracetam treatments were 4.3 and 4 days, respectively.
Table 2 summarizes the adverse reactions that occurred in 2% or more of neonates in Study 1. Incidences are displayed for neonates who received phenobarbital only and for neonates who received levetiracetam only. Because patients in Study 1 were neonates, adverse reactions that are verbally reported could not be assessed in this study.
Table 2: Adverse Reactions That Occurred in At Least 2% of Neonates Overall in Study 1 by Treatment Received
Phenobarbital
(N = 32)*
%
Levetiracetam
(N = 19)
%
Respiration abnormal
25
5
Sedation
16
5
Feeding disorder
16
5
Hypotension
16
0
Bradycardia
3
0
Hyponatremia
3
0
Sepsis
3
0
* Fifty-five neonates received both phenobarbital and levetiracetam and they had a similar adverse reaction profile as neonates who received only phenobarbital.
6.2 Postmarketing Experience
The following adverse reactions associated with the use of phenobarbital in neonates were identified in the literature. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Cardiovascular System: Bradycardia, patent ductus arteriosus
- Dermatologic Reactions: Eczema
- Hepatic: Abnormal liver function
- Musculoskeletal: Hypotonia, absent deep tendon reflexes
- Nervous System: Impaired consciousness, neurological impairment
- Renal: Abnormal kidney function
- Respiratory System: Bronchial secretion, respiratory depression
-
7 DRUG INTERACTIONS
7.1 Cytochrome P450- or Uridine 5’-diphospho-glucuronosyltransferase (UGT)-Based Interactions
The drug interaction information in Table 3 is based upon published literature in non-neonatal populations, in vitro studies, and the mechanistic knowledge of phenobarbital metabolic pathways [see Clinical Pharmacology (12.3)]. Although the data from the published literature regarding these drug interactions are from non-neonatal populations and the magnitude of the potential drug interactions in neonates have not been characterized, this information still warrants consideration given the potential impact of these possible drug interactions on the safety and efficacy of phenobarbital and CYP2B6, 2C9, 2C19, or UGT substrates in neonates.
Table 3: Drug Interactions with SEZABY
Effects of Other Drugs on SEZABY
CYP2C9, 2C19, 2E1, Uridine 5'-diphospho-glucuronosyltransferases (UGT) Inhibitors or Inducers
Prevention or Management
Closely monitor for adverse reactions (e.g., over sedation, prolonged QTc interval, etc.) when used concomitantly with inhibitors of these enzymes and reduced efficacy (e.g., breakthrough seizure) when used with inducers of these enzymes. Consider titration of the SEZABY maintenance dosage accordingly if concomitant use is unavoidable.
Clinical Effect(s)
Phenobarbital is a substrate of CYP2C9, CYP2C19, CYP2E1, and UGTs [see Clinical Pharmacology (12.3)]. It is likely that concomitant use will result in an increase in phenobarbital exposure when used with these inhibitors and a reduction when used with these inducers, which may increase the risk of SEZABY adverse reactions or reduce efficacy, respectively when concomitant use in neonates.
Effects of Other Drugs on Sezaby
CYP3A, 2B6, 2C(s), UGTs Substrates
Prevention or Management
Closely monitor neonates when SEZABY is used concurrently with substrates of these enzymes and consider increasing the dosage of the substrate accordingly, unless otherwise advised in its Prescribing Information, if concomitant use is unavoidable.
Clinical Effect(s)
Phenobarbital is an inducer of CYP3A, CYP2B6, CYP2C(s), and UGT(s) [see Clinical Pharmacology (12.3)]. It is likely that concomitant use in neonates will result in a decrease in the exposure of these substrates, which may reduce efficacy.
7.2 CNS Depressants
Closely monitor for signs of sedation and respiratory depression with concomitant use of SEZABY with other CNS depressants, including opioids [see Warnings and Precautions (5.1)].
Phenobarbital may cause sedation and respiratory depression [see Warnings and Precautions (5.4) and Adverse Reactions (6.1)]. Other products that may also cause these adverse reactions may have additive pharmacologic effect and may increase the risk of sedation and respiratory depression.
7.3 Drugs that Prolong QT Interval
SEZABY may prolong the QT interval [see Warnings and Precautions (5.10) and Clinical Pharmacology (12.2)]. Other products that may also prolong the QTc interval may have additive effects, and products that may increase concentrations of phenobarbital [see Drug Interactions (7.1)] may increase the QT prolongation risk; therefore, avoid concomitant use of SEZABY and these products. If concomitant use of a product that also prolongs the QTc interval or that increases SEZABY concentrations is unavoidable, monitor patients for increased risk of QTc interval prolongation.
-
8 USE IN SPECIFIC POPULATIONS
8.4 Pediatric Use
The safety and effectiveness of SEZABY have been established for the treatment of neonatal seizures in term and preterm infants, and the information on this use is discussed throughout the labeling.
Juvenile Animal Studies
In published studies, administration of antiepileptic drugs, including phenobarbital, to neonatal rats during the period of synaptogenesis has been reported to result in widespread apoptotic neurodegeneration in the developing brain and neurobehavioral deficits that persist into adulthood at doses associated with plasma exposures similar to those anticipated at the doses proposed for humans. The synaptogenetic period in rats is generally thought to correspond in humans to the third trimester of pregnancy through the first 3 to 4 years of life.
In rodents, exposure to phenobarbital during the neonatal period has been reported in published literature to result in permanent alterations in male and female reproductive function. Administration of phenobarbital to neonatal rats or hamsters resulted in disruption of testosterone secretory profiles and estrous cyclicity, changes in steroidogenesis, altered sexual behavior, and impaired fertility in adulthood.
-
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
SEZABY is a barbiturate and a CNS depressant with a potential for misuse, abuse, and addiction with unapproved use in adolescents and adults.
Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects. Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a health care provider or for whom it was not prescribed. Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence. Even taking barbiturates as prescribed may put patients at risk for abuse and misuse of their medication. Abuse and misuse of barbiturates, including phenobarbital, may lead to addiction.
Abuse and misuse of barbiturates often (but not always) involve the use of doses exceeding the doses used in clinical practice and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death. Barbiturates, including phenobarbital, are often sought by individuals who abuse drugs and other substances, and by individuals with addictive disorders [see Warnings and Precautions (5.3)].
Symptoms of acute intoxication with barbiturates include unsteady gait, slurred speech, and sustained nystagmus. Mental signs of chronic intoxication include confusion, poor judgment, irritability, insomnia, and somatic complaints. The use of phenobarbital alone can result in death; however, death is more often associated with phenobarbital use in the context of polysubstance use (especially with other CNS depressants, such as opioids and alcohol).
9.3 Dependence
Physical Dependence
SEZABY may produce physical dependence. Physical dependence is a state that develops as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug. Abrupt discontinuation or rapid dosage reduction of SEZABY may precipitate acute withdrawal reactions, including seizures, which can be life-threatening. Patients at an increased risk of withdrawal adverse reactions after SEZABY discontinuation or rapid dosage reduction include those administered higher dosages (i.e., higher and/or more frequent doses) and those who have had longer durations of use [see Warnings and Precautions (5.2)].
Symptoms of barbiturate withdrawal, including with phenobarbital, can be severe and may cause life threatening seizures or death.
- Minor withdrawal symptoms may appear 8 to 12 hours after the last barbiturate dose. These symptoms usually appear in the following order: anxiety, muscle twitching, tremor of hands and fingers, progressive weakness, dizziness, distortion in visual perception, nausea, vomiting, insomnia, and orthostatic hypotension.
- Major withdrawal symptoms (convulsions and delirium) may occur within 16 hours and last up to 5 days after abrupt cessation of barbiturates.
The intensity of withdrawal symptoms gradually declines over a period of approximately 15 days.
To reduce the risk of withdrawal reactions in patients using SEZABY for longer durations than recommended, use a gradual taper to discontinue SEZABY over an extended period of time (weeks to months) [see Warnings and Precautions (5.2)].
Tolerance
Tolerance to barbiturates may develop after continued use. Tolerance is a physiological state characterized by a reduced response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was once obtained at a lower dose). As tolerance to barbiturates develops, the amount needed to maintain the same level of intoxication increases; tolerance to a fatal dosage, however, does not increase more than two-fold. As this occurs, the margin between an intoxicating dosage and a fatal dosage becomes smaller.
-
10 OVERDOSAGE
Overdosage of barbiturates, including phenobarbital, is characterized by central nervous system depression ranging from drowsiness to coma.
- In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthria, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia.
- Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur.
- In severe overdosage cases, patients may develop respiratory depression and coma.
- Overdosage of barbiturates, particularly in combination with other CNS depressants (including alcohol and opioids) may be fatal [see Warnings and Precautions (5.3)].
- Markedly elevated blood pressure, heart rate, or respiratory rate raise the concern that additional drugs are involved in the overdosage.
In managing SEZABY overdosage, employ general supportive measures, including intravenous fluids, pressors, and airway maintenance. Consider contacting a poison center (1-800-221-2222) or a medical toxicologist for additional overdosage management recommendations.
-
11 DESCRIPTION
Phenobarbital is a barbiturate. Chemically, phenobarbital sodium is 2,4,6(1H,3H,5H)-Pyrimidinetrione, 5-ethyl-5-phenyl-, monosodium salt and has the following structural formula:
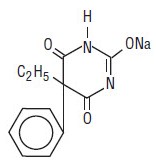
C12H11N2NaO3 MW 254.22
The sodium salt of phenobarbital occurs as a white, slightly bitter powder, crystalline granules or flaky crystals; it is very soluble in water, soluble in alcohol and practically insoluble in ether or chloroform.
SEZABY (phenobarbital sodium) for injection, for intravenous use, is supplied as sterile white to off white lyophilized powder in a 10 mL tubular glass vial. Each single-dose vial contains 100 mg of phenobarbital sodium, USP (equivalent to 91.35 mg of phenobarbital). The pH range is 9.20-10.00. SEZABY does not contain benzyl alcohol or propylene glycol.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism of action for phenobarbital for the treatment of neonatal seizures is not fully understood, but it is thought to involve potentiation of synaptic inhibition through an action on the GABAA receptor.
12.2 Pharmacodynamics
Phenobarbital exposure-response relationships and the time course of pharmacodynamic response of phenobarbital in neonates are unknown.
Cardiac Electrophysiology
The effect of SEZABY on the QTc interval has not been adequately characterized. Nonclinical data suggest a potential for phenobarbital to inhibit the hERG potassium cardiac ionic channel, and QTc prolongation was reported in the literature in adult patients with post-stroke seizures at a mean phenobarbital dose of 130 mg (approximately 1.5 times the recommended loading dose in an average 4.4 kg neonate at 4 weeks) [see Indications and Usage (1), Dosage and Administration (2.1), and Warnings and Precautions (5.10)].
12.3 Pharmacokinetics
Mean (± standard deviation) total (bound + unbound) phenobarbital concentrations were evaluated (see Table 4) in term infants younger than 14 days old with gestational ages between 36 and 44 weeks who received either one loading dose (20 mg/kg) or two loading doses (20 mg/kg each) based upon seizure persistence or reoccurrence [see Clinical Studies 14)]. The loading dose(s) was followed by a maintenance dosage of 1.5 mg/kg every 8 hours (total daily dose 4.5 mg/kg/day).
A clinically significant difference between term and preterm infants in phenobarbital PK following the first SEZABY loading dose was not predicted. A second loading dose of either 10 mg/kg or 20 mg/kg of phenobarbital in preterm infants is expected to result in similar plasma concentrations compared to a second loading dose of 20 mg/kg in term infants. In addition, administration of a phenobarbital maintenance dosage of 1.5 mg/kg every 8 hours or 2.25 mg/kg every 12 hours is not expected to result in a clinically significant difference in total phenobarbital plasma concentrations.
Table 4: Observed Phenobarbital Concentration Following Intravenous Phenobarbital Administration in Study 1
Time (Hours)
Phenobarbital Concentration (mcg/mL)
One Loading Dose Followed by the Maintenance Dosage
Two Loading Doses1 Followed by the Maintenance Dosage
1
23 (± 2.7)
26 (± 5.8)
24
23 (± 1.3)
39 (± 9.1)
48
25 (± 1.8)
39 (± 8.2)
1 Second loading dose administered if seizures persisted or reoccurred more than 15 minutes after the first infusion
Elimination
Published literature reports that the elimination t1/2 of phenobarbital in neonates is approximately 1 week.
Metabolism
Published literature reports that phenobarbital is primarily metabolized by CYP2C9 and to a lesser extent by CYP2C19, CYP2E1, and UGTs. At birth, expression of CYP2C9 is negligible, which results in the longer half-life in neonates compared to older populations in the published literature.
Specific Populations
There are no clinically significant differences in pharmacokinetics of phenobarbital in neonates administered therapeutic hypothermia. The effect of sex, race, ethnicity, renal impairment, or hepatic impairment on phenobarbital pharmacokinetics in neonates is unknown.
Drug Interaction Studies
Clinical Studies and Published Literature
No dedicated clinical studies have been conducted in neonates that evaluated the effect of concomitant use of SEZABY with:
CYP2C9, 2C19, 2E1, or UGT inhibitors or inducers on phenobarbital pharmacokinetics
CYP2B6, 2C9, 2C19, or UGT substrates on the pharmacokinetics of these substrates
Published literature regarding these interactions in non-neonatal populations should not be used to estimate the magnitude of the change in phenobarbital exposure in neonates due to differences in the expression of CYP2C9 and possibly other phenobarbital metabolic enzymes in term and preterm infants.
Midazolam: Published literature reports a 2.3-fold increase in the clearance of midazolam (CYP3A substrate) with concurrent use with phenobarbital in 68 neonates with hypoxic ischemic encephalopathy [see Drug Interactions (7.1)].
Theophylline or Chloramphenicol: Published literature reports no change in theophylline or chloramphenicol clearance with concomitant use of phenobarbital in neonates.
In Vitro Studies
Cytochrome P450 (CYP) Enzymes: Phenobarbital is an inhibitor of CYP2B6, CYP2C8, CYP2C9, CYP2C19, and CYP3A4. Phenobarbital is an inducer of CYP3A4, CYP2B6, and CYP2Cs [see Drug Interactions (7.1)].
Uridine diphosphate (UDP)-glucuronosyl transferase (UGT) Enzymes: Phenobarbital is an inhibitor of UGT1A1 and UGT2B7. Published literature reports that phenobarbital is an inducer for UGTs [see Drug Interactions (7.1)].
Transporter Systems: Phenobarbital is an inhibitor of BCRP, OAT1, OAT3, OCT2, OATP1B1, MATE1, and MATE2K. Phenobarbital is not a substrate of OAT1, OAT3, OCT2, OATP1B1, OATP1B3, MATE1, or MATE2K transporters.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Phenobarbital is a rodent carcinogen that has been demonstrated to produce hepatocellular adenomas and carcinomas in rats and mice following lifetime administration.
Mutagenesis
The genotoxic potential of phenobarbital has not been adequately assessed.
Impairment of Fertility
In a published study, administration of phenobarbital (subcutaneous doses up to 60 mg/kg/day) to adult rats prior to and during mating and continuing throughout pregnancy was reported to produce no adverse effects on fertility.
-
14 CLINICAL STUDIES
The effectiveness of phenobarbital for the treatment of neonatal seizures was established in a randomized, double-blind, active-controlled study in neonates who were experiencing seizures (Study 1; NCT01720667). Patients were neonates younger than 14 days of age with gestational ages between 36 and 44 weeks. Fifty-two percent of patients were male. Fifty-six percent of patients were White, 9% were Native Hawaiian or other Pacific Islander, 5% were Black or African American, 5% were Asian, 4% were mixed race, 1% were American Indian or Alaska Native, and 22% were identified as other, or were missing or unknown. Twenty-six percent of patients were Hispanic or Latino, 60% were not Hispanic or Latino, and 14% were not reported, missing, or unknown.
Eligible patients who experienced electrographically-confirmed seizures were randomized to receive either intravenous phenobarbital (N=42) or levetiracetam (N=64).
- Patients received an initial 15-minute infusion (loading dose) of either 20 mg/kg phenobarbital or 40 mg/kg levetiracetam.
- If electroencephalographic seizures persisted or recurred any time 15 minutes after the initial infusion completion, an additional infusion of the same treatment was administered (the second loading dose was 20 mg/kg infused over 15 minutes for both drugs).
- After loading dose(s) of phenobarbital or levetiracetam were administered, maintenance dosing of that treatment was administered regardless of whether seizures subsided. Maintenance regimens of 1.5 mg/kg/dose of phenobarbital and/or 10 mg/kg/dose of levetiracetam were administered via infusion every 8 hours and continued for up to 5 days. Mean durations of phenobarbital and levetiracetam treatments were 4.3 and 4 days, respectively.
- If seizures persisted or recurred any time 15 minutes after the second loading dose was completed, the patient also received alternate treatment.
The primary endpoint in Study 1 was the percentage of neonates whose seizures were terminated for at least 24 hours without the need for a second drug for the treatment of their seizures. A total of 94 patients who had neurophysiologist-confirmed seizures were included in the efficacy analysis.
Efficacy Results
A statistically significantly greater percentage of phenobarbital-treated patients met Study 1’s primary efficacy endpoint, compared to levetiracetam-treated patients. Table 5 presents the results of the trial’s primary and secondary efficacy analyses.
Table 5: Seizure Efficacy Results in Neonates (Study 1)
Phenobarbital
(N=33)Levetiracetam
(N=61)P-value*
Primary Endpoint
Percentage of patients with seizure termination > 24 hours1
73%
25%
<0.001
Secondary Endpoints
Percentage of patients with seizure termination > 48 hours1
55%
13%
<0.001
Percentage of patients with seizure termination > 1 hour1
85%
43%
<0.001**
1 Without need for a second drug to treat seizures
N = Total number of patients in each treatment group.
*P-value was based on two-sided Fisher’s Exact Test for categorical variables comparing phenobarbital and levetiracetam groups.
**Nominal: not controlled for Type I error
The outcome of 11 patients who had missing data (3 in the phenobarbital group and 8 in the levetiracetam group) was imputed as not successfully terminating seizures.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
SEZABY (phenobarbital sodium) for injection is supplied as a sterile white to off-white, lyophilized powder in single-dose clear glass vials containing 100 mg of phenobarbital sodium.
Carton Contents
NDC
One 100 mg single-dose vial
NDC: 62756-301-01
The vial stopper is not made with natural rubber latex.
16.2 Storage and Handling
Store unopened vials of SEZABY in original cartons at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [see USP Controlled Room Temperature]. Retain in the original carton until use to protect from light.
For information on storage of the reconstituted SEZABY, see Dosage and Administration (2.3).
Manufactured by:
Sun Pharmaceutical Medicare Ltd.,
Baska Ujeti Road, Ujeti,
Halol -389350, Gujarat, India
Distributed by:
Sun Pharmaceutical Industries, Inc.,
Cranbury, NJ 08512
ISS. 02/2023
5237784
SEZABY is a trademark of Sun Pharma Advanced Research Company Ltd., used under license
-
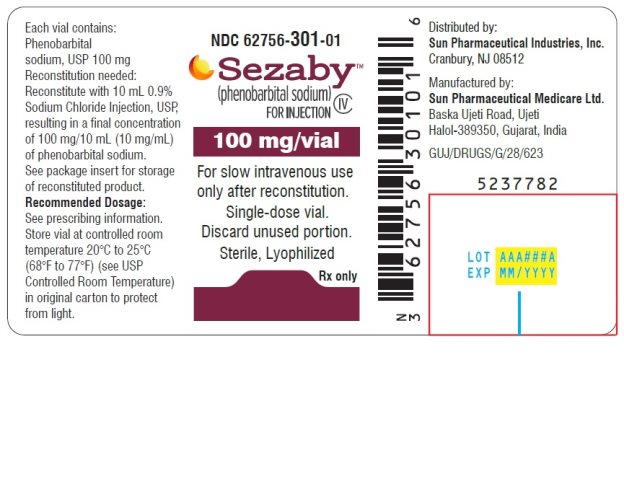
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL - Vial Label
NDC: 62756-301-01
SezabyTM (phenobarbital sodium) for injection CIV
100 mg/vial
For slow intravenous use only after reconstitution.
Single-dose vial.
Discard unused portion.
Sterile, Lyophilized
Rx only
-
Package/Label Display Panel – Carton Label
NDC: 62756-301-01
SezabyTM (phenobarbital sodium) for injection CIV
100 mg/vial
For slow intravenous use only after reconstitution.
Single-dose vial.
Discard unused portion.
Sterile, Lyophilized
Rx only

-
INGREDIENTS AND APPEARANCE
SEZABY
phenobarbital sodium injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 62756-301 Route of Administration INTRAVENOUS DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHENOBARBITAL SODIUM (UNII: SW9M9BB5K3) (PHENOBARBITAL - UNII:YQE403BP4D) PHENOBARBITAL SODIUM 100 mg Product Characteristics Color WHITE (white to off-white) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 62756-301-01 1 in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product 12/26/2022 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215910 12/25/2022 Labeler - Sun Pharmaceutical Industries, Inc. (146974886) Establishment Name Address ID/FEI Business Operations Sun Pharmaceutical Medicare Limited 725420835 manufacture(62756-301) , analysis(62756-301)
Trademark Results [SEZABY]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SEZABY 97098882 not registered Live/Pending |
Sun Pharma Advanced Research Company Limited 2021-10-29 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.