AMVUTTRA- vutrisiran injection
AMVUTTRA by
Drug Labeling and Warnings
AMVUTTRA by is a Prescription medication manufactured, distributed, or labeled by Alnylam Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use AMVUTTRA® safely and effectively. See full prescribing information for AMVUTTRA.
AMVUTTRA (vutrisiran) injection, for subcutaneous use
Initial U.S. Approval: 2022RECENT MAJOR CHANGES
Indication and Usage (1) 3/2025 INDICATIONS AND USAGE
AMVUTTRA is a transthyretin-directed small interfering RNA indicated for the treatment of:
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Injection: 25 mg/0.5 mL in a single-dose prefilled syringe. (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
Reduced serum vitamin A levels and recommended supplementation: Supplement with the recommended daily allowance of vitamin A. Refer to an ophthalmologist if ocular symptoms suggestive of vitamin A deficiency occur. (5.1)
ADVERSE REACTIONS
The most common adverse reactions (≥5%) were pain in extremity, arthralgia, dyspnea, and vitamin A decreased. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Alnylam Pharmaceuticals at 1-877-256-9526 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Polyneuropathy of Hereditary Transthyretin-mediated Amyloidosis
1.2 Cardiomyopathy of Wild-type or Hereditary Transthyretin-mediated Amyloidosis
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Reduced Serum Vitamin A Levels and Recommended Supplementation
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.6 Immunogenicity
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Polyneuropathy of Hereditary Transthyretin-mediated Amyloidosis
14.2 Cardiomyopathy of Wild-type or Hereditary Transthyretin-mediated Amyloidosis
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Polyneuropathy of Hereditary Transthyretin-mediated Amyloidosis
AMVUTTRA is indicated for the treatment of the polyneuropathy of hereditary transthyretin-mediated amyloidosis (hATTR-PN) in adults.
1.2 Cardiomyopathy of Wild-type or Hereditary Transthyretin-mediated Amyloidosis
AMVUTTRA is indicated for the treatment of the cardiomyopathy of wild-type or hereditary transthyretin-mediated amyloidosis (ATTR-CM) in adults to reduce cardiovascular mortality, cardiovascular hospitalizations and urgent heart failure visits.
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
The recommended dosage of AMVUTTRA is 25 mg administered by subcutaneous injection once every 3 months [see Dosage and Administration (2.2)].
2.2 Administration Instructions
AMVUTTRA is for subcutaneous use only and should be administered by a healthcare professional.
Preparation and Administration
- 1.
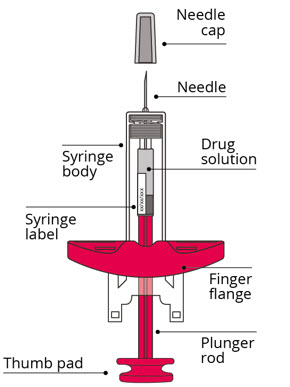
Prepare the syringe
If stored cold, allow the syringe to warm to room temperature for 30 minutes prior to use.
Remove the syringe from the packaging by gripping the syringe body.- Do not touch the plunger rod until ready to inject.
Check the following:- Syringe is not damaged, such as cracked or leaking
- Needle cap is attached to the syringe
- Expiration date on syringe label
- Do not use the syringe if any issues are found while checking the syringe.
- 2.
Choose and prepare the injection site
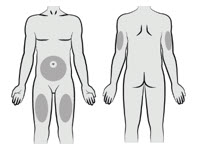
Choose an injection site from the following areas: the abdomen, thighs, or upper arms.
Avoid the following:- 5-cm area around the navel
- Scar tissue or areas that are reddened, inflamed, or swollen
- 3.
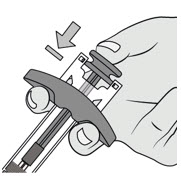
Prepare the syringe for injection
Hold the syringe body with one hand. Pull the needle cap straight off with other hand and dispose of needle cap immediately. It is normal to see a drop of liquid at the tip of the needle.- Do not touch the needle or let it touch any surface.
- Do not recap the syringe.
- Do not use the syringe if it is dropped.

- 4.
Perform the injection
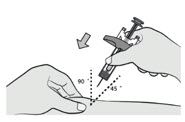
Pinch the cleaned skin.
Fully insert the needle into the pinched skin at a 45°-90° angle.
-
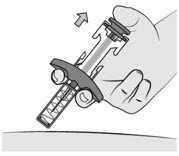
Inject all of the medication.
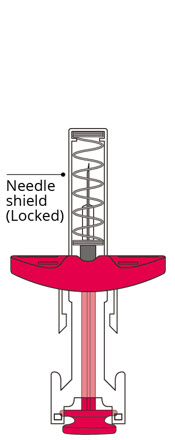
- Push the plunger rod as far as it will go to administer the dose and activate the needle shield.
-
Release the plunger rod to allow the needle shield to cover the needle.
- Do not block plunger rod movement.
- 5.
Dispose of the syringe
Immediately dispose of the used syringe into a sharps container.
- 1.
Prepare the syringe
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Reduced Serum Vitamin A Levels and Recommended Supplementation
AMVUTTRA treatment leads to a decrease in serum vitamin A levels [see Adverse Reactions (6.1) and Clinical Pharmacology (12.2)].
Supplementation at the recommended daily allowance of vitamin A is advised for patients taking AMVUTTRA. Higher doses than the recommended daily allowance of vitamin A should not be given to try to achieve normal serum vitamin A levels during treatment with AMVUTTRA, as serum vitamin A levels do not reflect the total vitamin A in the body.
Patients should be referred to an ophthalmologist if they develop ocular symptoms suggestive of vitamin A deficiency (e.g., night blindness).
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Reduced Serum Vitamin A Levels and Recommended Supplementation [see Warnings and Precautions (5.1)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of AMVUTTRA cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Two Phase 3 randomized, multi-center studies evaluated the safety of AMVUTTRA in 448 transthyretin-mediated amyloidosis (ATTR) patients, including 122 patients with hATTR-PN (HELIOS-A) and 326 patients with ATTR-CM (HELIOS-B) [see Clinical Studies (14)]. In both studies, patients were instructed to take the recommended daily allowance of vitamin A [see Warnings and Precautions (5.1)].
Polyneuropathy of Hereditary Transthyretin-mediated Amyloidosis
In HELIOS-A, 118 patients received at least 18 months of treatment. The mean duration of treatment was 18.8 months (range: 1.7 to 19.4 months). The median patient age at baseline was 60 years and 65% of the patients were male. Seventy percent of AMVUTTRA-treated patients were Caucasian, 17% were Asian, 3% were Black, and 9% were reported as Other. Forty-four percent of patients had the Val30Met mutation in the transthyretin gene; the remaining patients had one of 21 other mutations. At baseline, 70% of patients were in Stage 1 of the disease and 30% were in Stage 2.
The most common adverse reactions (at least 5%) were pain in extremity, arthralgia, dyspnea, and vitamin A decreased (see Table 1).
Seventy-four percent of patients treated with AMVUTTRA had normal vitamin A levels at baseline, and 98% of those with a normal baseline developed low vitamin A levels. In some cases, the decreased vitamin A level was reported as an adverse reaction (see Table 1).
Table 1: Adverse Reactions Reported in at least 5% of Patients Treated with AMVUTTRA in HELIOS-A Adverse Reaction AMVUTTRA
N=122
%- * Comprised of several similar terms
- † Percentage only reflects those reported as an adverse reaction
Pain in extremity* 15 Arthralgia* 11 Dyspnea* 7 Vitamin A decreased† 7 In HELIOS-A, two serious adverse reactions of atrioventricular (AV) heart block (1.6%) occurred in patients treated with AMVUTTRA, including one case of complete AV block.
Injection site reactions were reported in 5 (4%) patients treated with AMVUTTRA. Reported symptoms included bruising, erythema, pain, pruritus, and warmth. Injection site reactions were mild and transient.
Cardiomyopathy of Wild-type or Hereditary Transthyretin-mediated Amyloidosis
In HELIOS-B, safety was evaluated in 654 patients with ATTR-CM, which included 257 patients treated with AMVUTTRA for ≥30 months, and 77 patients treated with AMVUTTRA for ≥36 months [see Clinical Studies (14)]. No new safety issues were identified. Eighty-two percent of patients treated with AMVUTTRA had normal vitamin A levels at baseline, and 80% of those with a normal baseline developed low vitamin A levels.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no available data on AMVUTTRA use in pregnant women to inform a drug-associated risk of adverse developmental outcomes. AMVUTTRA treatment leads to a decrease in serum vitamin A levels, and vitamin A supplementation is advised for patients taking AMVUTTRA. Vitamin A is essential for normal embryofetal development; however, excessive levels of vitamin A are associated with adverse developmental effects. The effects on the fetus of a reduction in maternal serum TTR caused by AMVUTTRA and of vitamin A supplementation are unknown [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.2)].
In animal studies, subcutaneous administration of vutrisiran to pregnant rats resulted in developmental toxicity (reduced fetal body weight and embryofetal mortality) at doses associated with maternal toxicity (see Data).
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Data
Animal Data
Subcutaneous administration of vutrisiran (0, 3, 10, or 30 mg/kg/day) to pregnant rats during the period of organogenesis resulted in embryofetal mortality at the high dose and reduced fetal body weight at the mid and high doses, which were associated with maternal toxicity.
Subcutaneous administration of vutrisiran (0, 3, 10, or 30 mg/kg/day) to pregnant rabbits resulted in no adverse effects on embryofetal development.
Subcutaneous administration of vutrisiran (0, 5, 10, or 20 mg/kg) to pregnant rats every 6 days throughout pregnancy and lactation resulted in no adverse developmental effects on the offspring.
8.2 Lactation
Risk Summary
There is no information regarding the presence of vutrisiran in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for AMVUTTRA and any potential adverse effects on the breastfed infant from AMVUTTRA or from the underlying maternal condition.
8.5 Geriatric Use
No dose adjustment is required in patients ≥65 years of age [see Clinical Pharmacology (12.3)]. In HELIOS-A, a total of 46 (38%) patients ≥65 years of age, including 7 (6%) patients ≥75 years of age, received AMVUTTRA In HELIOS-B, a total of 299 (92%) patients ≥65 years old, including 203 (62%) ≥75 years old, received AMVUTTRA. No overall differences in safety or effectiveness were observed between these patients and younger patients.
8.6 Renal Impairment
No dose adjustment is recommended in patients with mild or moderate renal impairment (estimated glomerular filtration rate [eGFR] ≥30 to <90 mL/min/1.73 m2) [see Clinical Pharmacology (12.3)]. AMVUTTRA has not been studied in patients with severe renal impairment or end-stage renal disease.
8.7 Hepatic Impairment
No dose adjustment is recommended in patients with mild (total bilirubin ≤1 × ULN and AST >1 × ULN, or total bilirubin >1.0 to 1.5 × ULN and any AST) or moderate (total bilirubin >1.5 to 3 × ULN and any AST) hepatic impairment [see Clinical Pharmacology (12.3)]. AMVUTTRA has not been studied in patients with severe hepatic impairment.
-
11 DESCRIPTION
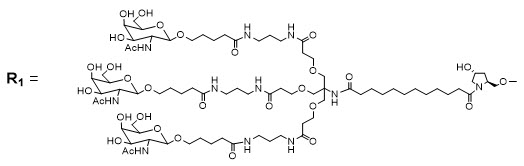
AMVUTTRA contains vutrisiran, a chemically modified double-stranded small interfering ribonucleic acid (siRNA) that targets mutant and wild-type transthyretin (TTR) messenger RNA (mRNA) and is covalently linked to a ligand containing three N-acetylgalactosamine (GalNAc) residues to enable delivery of the siRNA to hepatocytes.
The structural formula of vutrisiran sodium is presented below.
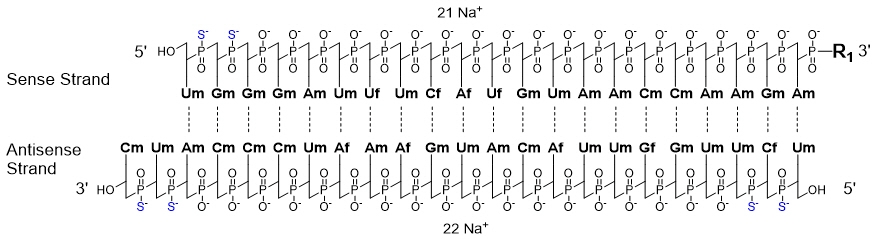
Dashed lines denote Watson-Crick base pairing
The molecular formula of vutrisiran sodium is C530H672F9N171Na43O323P43S6 with a molecular weight of 17,290 Da. The molecular formula of the free acid is C530H715F9N171O323P43S6 with a molecular weight of 16,345 Da.
AMVUTTRA is supplied as a sterile, preservative-free, clear, colorless-to-yellow solution for subcutaneous injection. Each 0.5 mL of solution contains 25 mg of vutrisiran (equivalent to 26.5 mg vutrisiran sodium), 0.2 mg sodium phosphate monobasic dihydrate, 0.7 mg sodium phosphate dibasic dihydrate, 3.2 mg sodium chloride, water for injection, and sodium hydroxide and/or phosphoric acid to adjust the pH to ~7.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Vutrisiran is a double-stranded siRNA-GalNAc conjugate that causes degradation of mutant and wild-type TTR mRNA through RNA interference, which results in a reduction of serum TTR protein and TTR protein deposits in tissues.
12.2 Pharmacodynamics
The pharmacodynamic effects of AMVUTTRA were evaluated in patients with hATTR-PN and ATTR-CM, treated with 25 mg AMVUTTRA administered by subcutaneous injection once every 3 months.
Polyneuropathy of Hereditary Transthyretin-mediated Amyloidosis
In HELIOS-A [see Clinical Studies (14)], vutrisiran reduced mean serum TTR at steady state by 83%. Similar TTR reductions were observed regardless of Val30Met genotype status, weight, sex, age, or race.
Vutrisiran also reduced the mean steady state serum vitamin A by 62% over 9 months [see Warnings and Precautions (5.1)].
Cardiomyopathy of Wild-type (wt) or Hereditary Transthyretin-mediated Amyloidosis (hATTR)
In HELIOS-B, the mean serum TTR reduction profile was similar with that observed in HELIOS-A, and consistent across the subgroups studied (age, sex, race, body weight, anti-drug antibody [ADA] status, ATTR disease type (wtATTR versus hATTR), NYHA class, and baseline tafamidis use).
Vutrisiran reduced the mean steady state serum vitamin A by 65% over 36 months. [see Warnings and Precautions (5.1)].
12.3 Pharmacokinetics
The pharmacokinetic (PK) properties of AMVUTTRA were evaluated following a single dose in healthy subjects and multiple doses in patients with hATTR amyloidosis, as summarized in Table 2.
Table 2: Pharmacokinetic Parameters of Vutrisiran Vutrisiran AUCinf = area under the concentration-time curve from the time of dosing extrapolated to infinity; AUClast = area under the concentration-time curve from the time of dosing to the last measurable concentration; Cmax = maximum plasma concentration; CV = coefficient of variation; RSE = relative standard error; Tmax = time to maximum concentration; Vd/F = apparent volume of distribution - * After 25 mg every 3 months dosage in hATTR amyloidosis patients
- † After 25 mg single dose in healthy subjects
- ‡ Based on population PK model estimation
- § Vutrisiran plasma protein binding was concentration-dependent and decreased with increasing vutrisiran concentrations (from 78% at 0.5 mcg/mL to 19% at 50 mcg/mL)
- ¶ After single subcutaneous vutrisiran dose from 5 to 300 mg (i.e., 0.2 to 12 times the recommended dose) in healthy subjects
General Information Dose Proportionality Vutrisiran Cmax showed dose proportional increase while AUClast and AUCinf were slightly more than dose proportional following single subcutaneous doses ranging from 5 to 300 mg (i.e., 0.2 to 12 times the recommended dose) Accumulation No accumulation of vutrisiran was observed in plasma after repeated every 3 months dosage* Absorption Tmax [Median (Range)] 4 (0.17, 12.0) hours† Distribution Estimated Vd/F (%RSE) 10.1 (5.8) L‡ Protein Binding 80%§ Organ Distribution Vutrisiran distributes primarily to the liver after subcutaneous dosing Elimination Half-Life [Median (Range)] 5.2 (2.2, 6.4) hours† Apparent Clearance [Median (Range)] 21.4 (19.8, 30) L/hour† Metabolism Primary Pathway Vutrisiran is metabolized by endo- and exonucleases to short nucleotide fragments of varying sizes within the liver Excretion Primary Pathway The mean fraction of unchanged vutrisiran eliminated in urine was approximately 19.4% at the recommended dose of 25 mg. The mean renal clearance of vutrisiran ranged from 4.5 to 5.7 L/hour¶ Specific Populations
No clinically significant differences in the pharmacokinetics of vutrisiran were observed based on age, sex, race, mild and moderate renal impairment (eGFR≥30 to <90 mL/min/1.73 m2), or mild (total bilirubin ≤1 × ULN and AST >1 × ULN, or total bilirubin >1.0 to 1.5 × ULN and any AST) and moderate (total bilirubin >1.5 to 3 × ULN and any AST) hepatic impairment. Vutrisiran has not been studied in patients with severe renal impairment, end-stage renal disease, severe hepatic impairment, or in patients with prior liver transplant.
Drug Interaction Studies
No clinical drug-drug interaction studies have been performed with vutrisiran. In vitro studies suggest that vutrisiran is not a substrate or inhibitor of cytochrome P450 enzymes. Vutrisiran is not expected to cause drug-drug interactions by inducing CYP enzymes or modulating the activities of drug transporters.
12.6 Immunogenicity
The observed incidence of anti-drug antibody (ADA, including neutralizing antibody) is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of ADA in the studies described below with the incidence of ADA in the other studies, including those of AMVUTTRA or of other siRNA products.
In HELIOS-A and HELIOS-B studies, 3 (2.5%) and 1 (0.3%) patient treated with AMVUTTRA, respectively, developed transient, low titer anti-drug antibodies. The available data are limited to make definitive conclusions regarding the effect of anti-drug antibodies on pharmacokinetics or pharmacodynamics of AMVUTTRA.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Subcutaneous administration of vutrisiran to male mice (0, 2, 6, or 13 mg/kg once every 4 weeks) for 100 weeks and to female mice (0, 3, 9, or 18 mg/kg once every 4 weeks) for 98 weeks resulted in no increase in tumors.
Subcutaneous administration of vutrisiran to male rats (0, 4, 7.5, or 15 mg/kg once every 4 weeks or 15 mg/kg once every 12 weeks) for 99 weeks and to female rats (0, 6, 12.5, or 25 mg/kg once every 4 weeks or 25 mg/kg once every 12 weeks) for 86-87 weeks resulted in no increase in tumors.
-
14 CLINICAL STUDIES
14.1 Polyneuropathy of Hereditary Transthyretin-mediated Amyloidosis
The efficacy of AMVUTTRA was evaluated in a randomized, open-label clinical trial in adult patients with hATTR-PN (HELIOS-A; NCT03759379). Patients were randomized 3:1 to receive 25 mg of AMVUTTRA subcutaneously once every 3 months (N=122), or 0.3 mg/kg patisiran intravenously every 3 weeks (N=42) as a reference group. Ninety-seven percent of AMVUTTRA-treated patients and 93% of patisiran-treated patients completed at least 9 months of the assigned treatment.
Efficacy assessments were based on a comparison of the AMVUTTRA arm of HELIOS-A with an external placebo group in another study (NCT01960348) composed of a comparable population of adult patients with polyneuropathy caused by hATTR amyloidosis.
The primary efficacy endpoint was the change from baseline to Month 9 in modified Neuropathy Impairment Score +7 (mNIS+7). The mNIS+7 is an objective assessment of neuropathy and comprises the NIS and Modified +7 composite scores. In the version of the mNIS+7 used in the trial, the NIS objectively measures deficits in cranial nerve function, muscle strength, and reflexes, and the +7 assesses postural blood pressure, quantitative sensory testing, and peripheral nerve electrophysiology. The mNIS+7 has a total score range from 0 to 304 points, with higher scores representing a greater severity of disease.
The clinical meaningfulness of effects on the mNIS+7 was assessed by the change from baseline to Month 9 in Norfolk Quality of Life-Diabetic Neuropathy (QoL-DN) total score. The Norfolk QoL-DN scale is a patient-reported assessment that evaluates the subjective experience of neuropathy in the following domains: physical functioning/large fiber neuropathy, activities of daily living, symptoms, small fiber neuropathy, and autonomic neuropathy. The Norfolk QoL-DN has a total score range from -4 to 136, with higher scores representing greater impairment.
Additional endpoints were gait speed, as measured by the 10-meter walk test (10MWT), and modified body mass index (mBMI).
Treatment with AMVUTTRA in HELIOS-A resulted in statistically significant improvements in the mNIS+7, Norfolk QoL-DN total score, and 10-meter walk test at Month 9 compared to placebo in the external study (p<0.001) [Table 3, Figure 1, and Figure 3]. The distributions of changes in mNIS+7 and Norfolk QoL-DN total scores from baseline to Month 9 by percent of patients are shown in Figure 2 and Figure 4, respectively.
The change from baseline to Month 9 in modified body mass index nominally favored AMVUTTRA [Table 3].
Table 3: Clinical Efficacy Results (Comparison of AMVUTTRA Treatment in HELIOS-A to an External Placebo Control*) Endpoint† Baseline, Mean (SD) Change from Baseline to Month 9, LS Mean (SEM) AMVUTTRA-Placebo* Treatment Difference, LS Mean
(95% CI)p-value AMVUTTRA
N=122
(HELIOS-A)Placebo*
N=77
(NCT01960348)AMVUTTRA
(HELIOS-A)Placebo*
(NCT01960348)CI = confidence interval; LS mean = least squares mean; mBMI = modified body mass index; mNIS = modified Neuropathy Impairment Score; QoL-DN = Quality of Life-Diabetic Neuropathy; SD = standard deviation; SEM = standard error of the mean - * External placebo group from another randomized controlled trial (NCT01960348)
- † All endpoints analyzed using the analysis of covariance (ANCOVA) with multiple imputation (MI) method)
- ‡ A lower number indicates less impairment/fewer symptoms
- § A higher number indicates less disability/less impairment
- ¶ mBMI: nominal p-value; body mass index (BMI; kg/m2) multiplied by serum albumin (g/L).
mNIS+7‡ 60.6 (36.0) 74.6 (37.0) -2.2 (1.4) 14.8 (2.0) -17.0
(-21.8, -12.2)p<0.001 Norfolk
QoL-DN‡47.1 (26.3) 55.5 (24.3) -3.3 (1.7) 12.9 (2.2) -16.2
(-21.7, -10.8)p<0.001 10-meter walk test (m/sec)§ 1.01 (0.39) 0.79 (0.32) 0 (0.02) -0.13 (0.03) 0.13
(0.07, 0.19)p<0.001 mBMI¶ 1058 (234) 990 (214) 7.6 (7.9) -60.2 (10.1) 67.8
(43.0, 92.6)p<0.001 A decrease in mNIS+7 indicates improvement
Δ indicates between-group treatment difference, shown as the LS mean difference (95% CI) for AMVUTTRA – placebo- * External placebo group from another randomized controlled trial (NCT01960348)
Figure 1: Change from Baseline in mNIS+7
(Comparison of AMVUTTRA Treatment in HELIOS-A to an External Placebo Control*)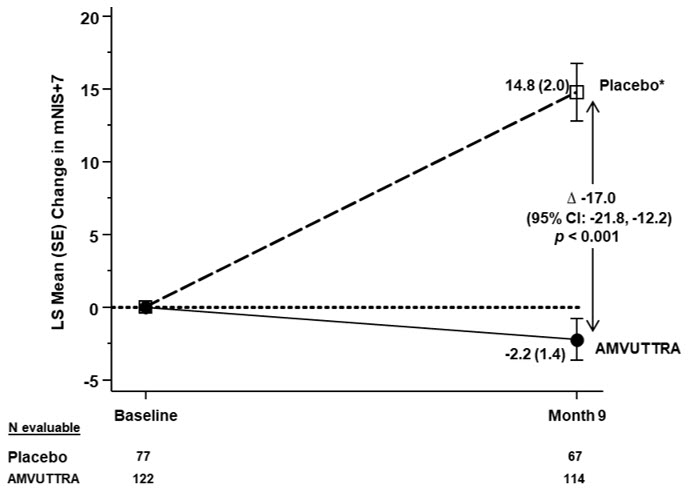
Categories are mutually exclusive; patients who died before 9 months are summarized in the "Death" category only - * External placebo group from another randomized controlled trial (NCT01960348)
Figure 2: Histogram of mNIS+7 Change from Baseline at Month 9
(Comparison of AMVUTTRA Treatment in HELIOS-A to an External Placebo Control*)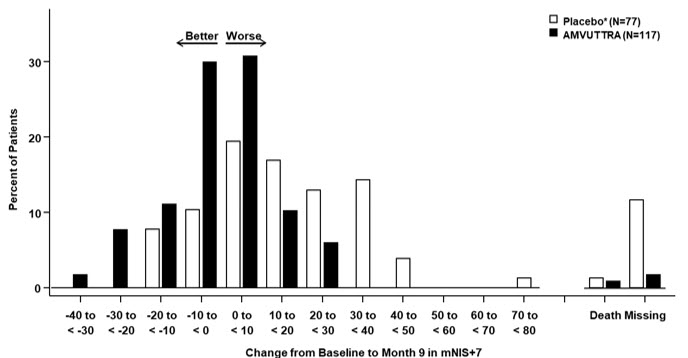
A decrease in Norfolk QoL-DN score indicates improvement
Δ indicates between-group treatment difference, shown as the LS mean difference (95% CI) for AMVUTTRA – placebo- * External placebo group from another randomized controlled trial (NCT01960348)
Figure 3: Change from Baseline in Norfolk QoL-DN Total Score
(Comparison of AMVUTTRA Treatment in HELIOS-A to an External Placebo Control*)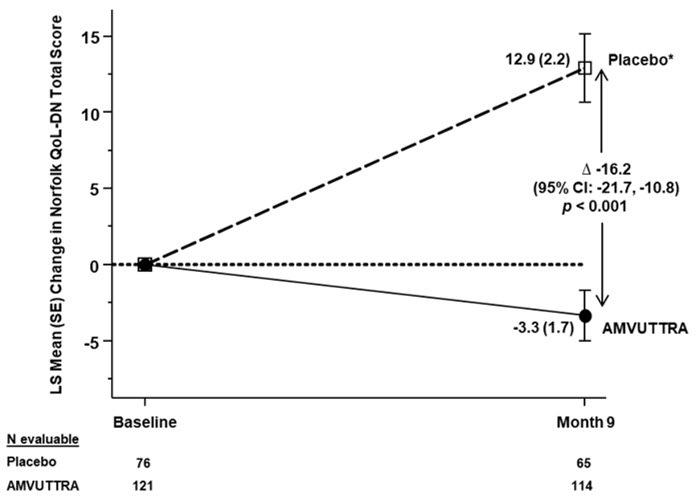
Categories are mutually exclusive; patients who died before 9 months are summarized in the "Death" category only - * External placebo group from another randomized controlled trial (NCT01960348)
Figure 4: Histogram of Norfolk QoL-DN Total Score Change from Baseline at Month 9
(Comparison of AMVUTTRA Treatment in HELIOS-A to an External Placebo Control*)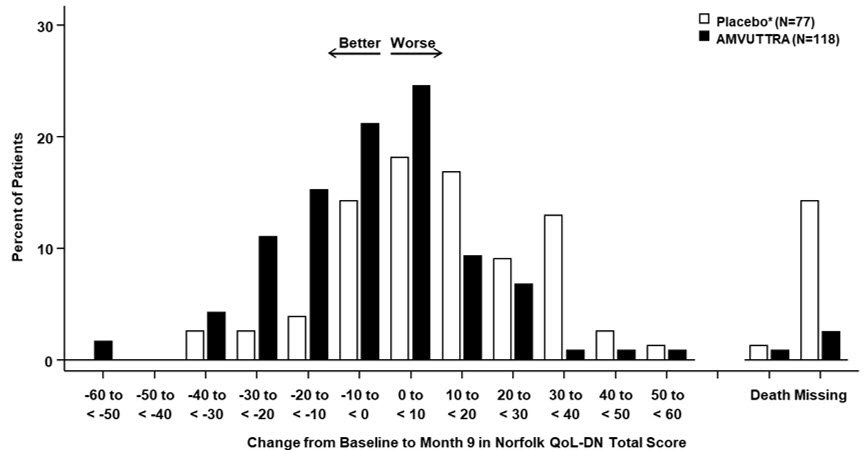
Patients receiving AMVUTTRA in HELIOS-A experienced similar improvements relative to those in the external placebo group in mNIS+7 and Norfolk QoL-DN total score across all subgroups including age, sex, race, region, NIS score, Val30Met genotype status, and disease stage.
14.2 Cardiomyopathy of Wild-type or Hereditary Transthyretin-mediated Amyloidosis
The efficacy of AMVUTTRA was evaluated in a multicenter, international, randomized, double-blind, placebo-controlled trial (HELIOS-B, NCT04153149) in 654 adult patients with wild-type or hereditary ATTR-CM. Patients were randomized 1:1 to receive 25 mg of AMVUTTRA (n=326) subcutaneously once every 3 months, or matching placebo (n=328).
Treatment assignment was stratified by baseline tafamidis use (yes versus no), ATTR disease type (wtATTR or hATTR amyloidosis), and by baseline New York Heart Association (NYHA) Class I or II and age <75 years versus all other. At baseline, 40% of patients were on tafamidis. The mean age of study participants was 75 years, 93% were male, 84% were White, 7% were Black or African American, 6% were Asian, 2% did not report race and 1% were race other, 88% had wild-type ATTR, 13% were NYHA Class I, 78% were NYHA Class II, and 9% NYHA Class III. No significant imbalance in baseline characteristics was observed between the two treatment groups.
Participants were permitted to initiate open-label tafamidis during the study. A total of 85 participants initiated tafamidis: 44 (22%) in the AMVUTTRA arm and 41 (21%) in the placebo arm. The median time to initiation of tafamidis for these 85 participants was 18 months.
The primary efficacy endpoint was the composite outcome of all-cause mortality and recurrent CV events (CV hospitalizations and urgent heart failure [UHF] visits) during the double-blind treatment period of up to 36 months, evaluated in the overall population and in the monotherapy population (defined as patients not receiving tafamidis at study baseline).
AMVUTTRA led to significant reduction in the risk of all-cause mortality and recurrent CV events compared to placebo in the overall and monotherapy population of 28% and 33%, respectively (Table 4). The majority of the deaths (77%) were CV-related. A Kaplan-Meier curve illustrating time to first CV event or all-cause mortality is presented in Figure 5.
Both components of the primary composite endpoint individually contributed to the treatment effect in the overall and monotherapy population (Table 4).
Table 4: Primary Composite Endpoint and its Individual Components in HELIOS-B Endpoint Overall population Monotherapy population AMVUTTRA
(N=326)Placebo
(N=328)AMVUTTRA
(N=196)Placebo
(N=199)Abbreviations: CI=confidence interval; CV=cardiovascular; UHF=urgent heart failure.
Heart transplantation and left ventricular assist device placement are treated as death. Deaths after study discontinuation are included in the all-cause mortality component analysis.- * Primary composite endpoint defined as: composite outcome of all-cause mortality and recurrent CV events. Primary analysis included at least 33 months (and up to 36 months) follow-up on all patients.
- † Hazard Ratio (95% CI) and p-value are based on a modified Andersen-Gill model.
- ‡ Hazard Ratio (95% CI) is based on a Cox proportional hazard model.
Primary composite endpoint* Hazard Ratio (95% CI)†
p-value†0.72 (0.55, 0.93)
0.010.67 (0.49, 0.93)
0.02Components of the Primary Composite Endpoint All-cause mortality Hazard Ratio (95% CI)‡ 0.69 (0.49, 0.98) 0.71 (0.47, 1.06) CV hospitalizations and UHF visits Hazard Ratio (95% CI)† 0.73 (0.55, 0.96) 0.67 (0.47, 0.96) Figure 5: Time to All-Cause Mortality or First CV Event (Overall population) Abbreviations: CI=confidence interval; CV=cardiovascular; HR = hazard ratio.
Heart transplantation and left ventricular assist device placement are treated as death. HR and 95% CI are based on a Cox proportional hazard model. First CV event = First CV hospitalization or urgent heart failure visit after randomization.
Results from the subgroup analysis for the primary composite endpoint were consistent across prespecified subgroups in the overall population (Figure 6) and monotherapy population.
Figure 6: Subgroup Analyses of the Primary Composite Endpoint (Overall Population) Abbreviations: ATTR = transthyretin amyloidosis; CI = confidence interval; hATTR = hereditary transthyretin amyloidosis; HR = hazard ratio; NT-pro-BNP = N-terminal prohormone of B-type natriuretic peptide; NYHA = New York Heart Association; wtATTR = wild-type transthyretin amyloidosis.
HR and 95% CI are based on modified Andersen-Gill model analyses.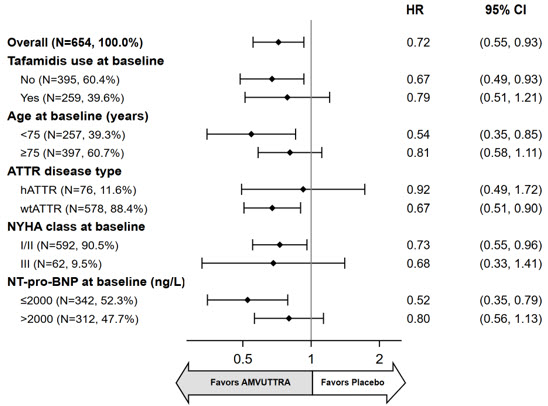
The treatment effect of AMVUTTRA on functional capacity and health status were assessed by the change from baseline to Month 30 in distance walked on 6-Minute Walk Test (6-MWT), and the Kansas City Cardiomyopathy Questionnaire-Overall Summary (KCCQ-OS) score, respectively.
At Month 30, the LS mean difference in change from baseline in distance walked on 6-MWT was 22 (95% CI: 8, 35; p=0.002) meters and 25 (95% CI: 7, 44; p=0.006) meters favoring AMVUTTRA over placebo in the overall population and monotherapy population, respectively.
At Month 30, the LS mean difference in the change from baseline in KCCQ-OS was 6 (95% CI: 2, 9; p=0.001) and 8 (95% CI: 4, 13; p=0.0003) favoring AMVUTTRA over placebo in the overall population and monotherapy population respectively.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
AMVUTTRA is a sterile, preservative-free, clear, colorless-to-yellow solution for subcutaneous injection. AMVUTTRA is supplied as 25 mg/0.5 mL solution in a single-dose 1-mL prefilled syringe made from Type I glass with stainless steel 29-gauge needle with a needle shield. The prefilled syringe components are not made with natural rubber latex.
AMVUTTRA is available in cartons containing one single-dose prefilled syringe each.
The NDC is: 71336-1003-1.
-
17 PATIENT COUNSELING INFORMATION
Recommended Vitamin A Supplementation
Inform patients that AMVUTTRA treatment leads to a decrease in serum vitamin A levels. Instruct patients to take the recommended daily allowance of vitamin A. Advise patients to contact their healthcare provider if they experience ocular symptoms suggestive of vitamin A deficiency (e.g., night blindness) and refer them to an ophthalmologist if they develop these symptoms [see Warnings and Precautions (5.1)].
Pregnancy
Instruct patients that if they are pregnant or plan to become pregnant while taking AMVUTTRA they should inform their healthcare provider. Inform patients of the potential risk to the fetus, including that AMVUTTRA treatment leads to a decrease in serum vitamin A levels [see Use in Specific Populations (8.1) and Clinical Pharmacology (12.2)].
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 25 mg/0.5 mL Syringe Carton
NDC: 71336-1003-1
amvuttra ™
(vutrisiran) injection25 mg/0.5 mL
For Subcutaneous Injection by
Healthcare Professional OnlyRx Only
Do not use if
seal is broken1 x 25 mg single-dose
prefilled syringe
-
INGREDIENTS AND APPEARANCE
AMVUTTRA
vutrisiran injectionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 71336-1003 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength VUTRISIRAN SODIUM (UNII: 28O0WP6Z1P) (VUTRISIRAN - UNII:GB4I2JI8UI) VUTRISIRAN 25 mg in 0.5 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Sodium hydroxide (UNII: 55X04QC32I) Phosphoric acid (UNII: E4GA8884NN) SODIUM PHOSPHATE, MONOBASIC, DIHYDRATE (UNII: 5QWK665956) SODIUM PHOSPHATE, DIBASIC, DIHYDRATE (UNII: 94255I6E2T) Sodium chloride (UNII: 451W47IQ8X) Product Characteristics Color YELLOW (clear, colorless-to-yellow) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 71336-1003-1 1 in 1 CARTON 06/13/2022 1 0.5 mL in 1 SYRINGE, GLASS; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA215515 06/13/2022 Labeler - Alnylam Pharmaceuticals, Inc. (115524410)
Trademark Results [AMVUTTRA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 AMVUTTRA 97057480 not registered Live/Pending |
Alnylam Pharmaceuticals, Inc. 2021-10-03 |
 AMVUTTRA 97057473 not registered Live/Pending |
Alnylam Pharmaceuticals, Inc. 2021-10-03 |
 AMVUTTRA 90151672 not registered Live/Pending |
Alnylam Pharmaceuticals, Inc. 2020-09-01 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.