ZINPLAVA- bezlotoxumab injection, solution
ZINPLAVA by
Drug Labeling and Warnings
ZINPLAVA by is a Prescription medication manufactured, distributed, or labeled by Merck Sharp & Dohme Corp.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ZINPLAVA safely and effectively. See full prescribing information for ZINPLAVA.
ZINPLAVA™ (bezlotoxumab) injection, for intravenous use
Initial U.S. Approval: 2016INDICATIONS AND USAGE
ZINPLAVA is a human monoclonal antibody that binds to Clostridium difficile toxin B, indicated to reduce recurrence of Clostridium difficile infection (CDI) in patients 18 years of age or older who are receiving antibacterial drug treatment of CDI and are at a high risk for CDI recurrence. (1)
Limitation of Use:ZINPLAVA is not indicated for the treatment of CDI. ZINPLAVA is not an antibacterial drug. ZINPLAVA should only be used in conjunction with antibacterial drug treatment of CDI. (1)
DOSAGE AND ADMINISTRATION
- Administer ZINPLAVA during antibacterial drug treatment for CDI. (2.1)
- The recommended dose is a single dose of 10 mg/kg administered as an intravenous infusion over 60 minutes. (2.2)
- Dilute prior to intravenous infusion. Administer via a low-protein binding 0.2 micron to 5 micron in-line or add-on filter. See Full Prescribing Information for dilution and administration instructions. (2.3)
DOSAGE FORMS AND STRENGTHS
Injection: 1,000 mg/40 mL (25 mg/mL) solution in a single-dose vial. (3)
CONTRAINDICATIONS
None (4)
WARNINGS AND PRECAUTIONS
Heart Failure: Was reported more commonly in ZINPLAVA-treated patients with a history of congestive heart failure (CHF) in the two Phase 3 clinical trials. In patients with a history of CHF, ZINPLAVA should be reserved for use when the benefit outweighs the risk. (5.1)
ADVERSE REACTIONS
Most common adverse reactions (reported in ≥4% of patients) included nausea, pyrexia, and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2016
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
2.2 Dosing Recommendations in Adults
2.3 Preparation and Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Heart Failure
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
ZINPLAVA™ is indicated to reduce recurrence of Clostridium difficile infection (CDI) in patients 18 years of age or older who are receiving antibacterial drug treatment of CDI and are at a high risk for CDI recurrence.
Limitation of Use:
ZINPLAVA is not indicated for the treatment of CDI. ZINPLAVA is not an antibacterial drug. ZINPLAVA should only be used in conjunction with antibacterial drug treatment of CDI. [See Dosage and Administration (2.1).]
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Administration Instructions
Administer ZINPLAVA during antibacterial drug treatment for CDI.
2.2 Dosing Recommendations in Adults
The recommended dose of ZINPLAVA is a single dose of 10 mg/kg administered as an intravenous infusion over 60 minutes. The safety and efficacy of repeat administration of ZINPLAVA in patients with CDI have not been studied.
2.3 Preparation and Administration
Preparation of Diluted Solution
- ZINPLAVA must be diluted prior to intravenous infusion.
- Prepare the diluted solution immediately after removal of the vial(s) from refrigerated storage, or the vial(s) may be stored at room temperature protected from light for up to 24 hours prior to preparation of the diluted solution.
- Inspect vial contents for discoloration and particulate matter prior to dilution. ZINPLAVA is a clear to moderately opalescent, colorless to pale yellow solution. Do not use the vial if the solution is discolored or contains visible particles.
- Do not shake the vial.
- Withdraw the required volume from the vial(s) based on the patient's weight (in kg) and transfer into an intravenous bag containing either 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP to prepare a diluted solution with a final concentration ranging from 1 mg/mL to 10 mg/mL. Mix diluted solution by gentle inversion. Do not shake.
- Discard vial(s) and all unused contents.
Storage of Diluted Solution
- The product does not contain preservative. The diluted solution of ZINPLAVA may be stored either at room temperature for up to 16 hours or under refrigeration at 2°C to 8°C (36°F to 46°F) for up to 24 hours. If refrigerated, allow the intravenous bag to come to room temperature prior to use.
- These time limits include storage of the infusion solution in the intravenous bag through the duration of infusion.
- Do not freeze the diluted solution.
Administration
- Administer the diluted solution as an intravenous infusion over 60 minutes using a sterile, non-pyrogenic, low-protein binding 0.2 micron to 5 micron in-line or add-on filter.
- The diluted solution can be infused via a central line or peripheral catheter. Do not administer ZINPLAVA as an intravenous push or bolus.
- Do not co-administer other drugs simultaneously through the same infusion line.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Heart Failure
Heart failure was reported more commonly in the two Phase 3 clinical trials in ZINPLAVA-treated patients compared to placebo-treated patients. These adverse reactions occurred primarily in patients with underlying congestive heart failure (CHF). In patients with a history of CHF, 12.7% (15/118) of ZINPLAVA-treated patients and 4.8% (5/104) of placebo-treated patients had the serious adverse reaction of heart failure during the 12-week study period [see Adverse Reactions (6.1)]. Additionally, in patients with a history of CHF, there were more deaths in ZINPLAVA-treated patients, 19.5% (23/118) than in placebo-treated patients, 12.5% (13/104) during the 12-week study period. The causes of death varied and included cardiac failure, infections, and respiratory failure.
In patients with a history of CHF, ZINPLAVA should be reserved for use when the benefit outweighs the risk.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of ZINPLAVA was evaluated in two placebo-controlled, Phase 3 trials (Trial 1 n= 390 and Trial 2 n= 396). Patients received a single 10 mg/kg intravenous infusion of ZINPLAVA and concomitant standard of care antibacterial drugs (metronidazole, vancomycin or fidaxomicin) for CDI (SoC). Adverse reactions reported within the first 4 weeks after ZINPLAVA was administered are described for the pooled Phase 3 trial population of 786 patients. The median age of patients receiving ZINPLAVA was 65 years (range 18 to 100), 50% were age 65 years or older, 56% were female, and 83% were white.
The most common adverse reactions following treatment with ZINPLAVA (reported in ≥4% of patients within the first 4 weeks of infusion and with a frequency greater than placebo) were nausea, pyrexia, and headache (see Table 1).
Table 1: Adverse Reactions Reported in ≥4% of ZINPLAVA-Treated Patients with CDI and at a Frequency Greater than Placebo in Trial 1 and Trial 2*,† Adverse Reaction ZINPLAVA with SoC‡
N=786
%Placebo with SoC‡
N=781
%- * All patients as treated population, defined as all randomized patients who received a dose of study medication, by treatment received
- † Adverse reactions reported within 4 weeks of administration of ZINPLAVA or placebo
- ‡ SoC = Standard of Care antibacterial drugs (metronidazole or vancomycin or fidaxomicin) for CDI
Gastrointestinal disorders Nausea 7% 5% General disorders and administration site conditions Pyrexia 5% 3% Nervous system disorders Headache 4% 3% Serious adverse reactions occurring within 12 weeks following infusion were reported in 29% of ZINPLAVA-treated patients and 33% of placebo-treated patients. Heart failure was reported as a serious adverse reaction in 2.3% of the ZINPLAVA-treated patients and 1.0% of the placebo-treated patients [see Warnings and Precautions (5.1)].
One patient discontinued the ZINPLAVA infusion due to ventricular tachyarrhythmia that occurred 30 minutes after the start of the infusion.
Mortality rates were 7.1% and 7.6% in ZINPLAVA-treated patients and placebo-treated patients, respectively, during the 12-week follow-up period.
Infusion Related Reactions
Overall, 10% of ZINPLAVA-treated patients experienced one or more infusion specific adverse reactions on the day of, or the day after, the infusion compared to 8% of placebo-treated patients. Infusion specific adverse reactions reported in ≥0.5% of patients receiving ZINPLAVA and at a frequency greater than placebo were nausea (3%), fatigue (1%), pyrexia (1%), dizziness (1%), headache (2%), dyspnea (1%) and hypertension (1%). Of these patients, 78% and 20% of patients experienced mild and moderate adverse reactions, respectively. These reactions resolved within 24 hours following onset.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity following administration of ZINPLAVA. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to bezlotoxumab in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
Following treatment with ZINPLAVA in Trial 1 and Trial 2, none of the 710 evaluable patients tested positive for treatment-emergent anti-bezlotoxumab antibodies.
-
7 DRUG INTERACTIONS
Since ZINPLAVA is eliminated by catabolism, no metabolic drug-drug interactions are expected [see Clinical Pharmacology (12.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Adequate and well controlled studies with ZINPLAVA have not been conducted in pregnant women. No animal reproductive and developmental studies have been conducted with bezlotoxumab.
The background risk of major birth defects and miscarriage for the indicated population is unknown; however, the background risk in the U.S. general population of major birth defects is 2-4% and of miscarriage is 15-20% of clinically recognized pregnancies.
8.2 Lactation
Risk Summary
There is no information regarding the presence of bezlotoxumab in human milk, the effects on the breast-fed infant, or the effects on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ZINPLAVA and any potential adverse effects on the breastfed child from ZINPLAVA or from the underlying maternal condition.
8.4 Pediatric Use
Safety and efficacy of ZINPLAVA in patients below 18 years of age have not been established.
8.5 Geriatric Use
Of the 786 patients treated with ZINPLAVA, 50% were 65 years of age and over, and 27% were 75 years of age and over. No overall differences in safety and efficacy were observed between these subjects and younger subjects [see Clinical Studies (14)]. No dose adjustment is necessary for patients ≥65 years of age [see Clinical Pharmacology (12.3)].
- 10 OVERDOSAGE
-
11 DESCRIPTION
Bezlotoxumab is a human monoclonal antibody that binds to C. difficile toxin B and neutralizes its effects. Bezlotoxumab is an IgG1 immunoglobulin with an approximate molecular weight of 148.2 kDa.
ZINPLAVA (bezlotoxumab) Injection is a sterile, preservative-free, clear to moderately opalescent, colorless to pale yellow solution that requires dilution for intravenous infusion. The product is provided in a 50 mL vial that contains 1000 mg of bezlotoxumab in 40 mL of solution. Each mL of solution contains bezlotoxumab (25 mg), citric acid monohydrate (0.8 mg), diethylenetriaminepentaacetic acid (0.0078 mg), polysorbate 80 (0.25 mg), sodium chloride (8.77 mg), sodium citrate dihydrate (4.75 mg), and Water for Injection, USP. The vial may contain sodium hydroxide to adjust the pH to 6.0.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
ZINPLAVA (bezlotoxumab) is a human monoclonal antibody that binds to C. difficile toxin B and neutralizes its effects [see Microbiology (12.4)].
12.3 Pharmacokinetics
The pharmacokinetics of bezlotoxumab were studied in 1515 CDI patients in two Phase 3 trials (Trial 1 and Trial 2). Based on a population PK analysis, the geometric mean (%CV) clearance of bezlotoxumab was 0.317 L/day (41%), with a mean volume of distribution of 7.33 L (16%), and elimination half-life (t½) of approximately 19 days (28%). After a single intravenous dose of 10 mg/kg bezlotoxumab, geometric mean AUC0-INF and Cmax were 53000 mcg∙h/mL and 185 mcg/mL, respectively, in the patients with CDI. The clearance of bezlotoxumab increased with increasing body weight; the resulting exposure differences are adequately addressed by the administration of a weight-based dose. Bezlotoxumab is eliminated by catabolism.
Patients with Renal Impairment
The effect of renal impairment on the pharmacokinetics of bezlotoxumab was evaluated in patients with mild (eGFR 60 to <90 mL/min/1.73 m2), moderate (eGFR 30 to <60 mL/min/1.73 m2), or severe (eGFR 15 to <30 mL/min/1.73 m2) renal impairment, or with end stage renal disease (eGFR <15 mL/min/1.73 m2), as compared to patients with normal (eGFR ≥90 mL/min/1.73 m2) renal function. No clinically meaningful differences in the exposure of bezlotoxumab were found between patients with renal impairment and patients with normal renal function.
Patients with Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of bezlotoxumab was evaluated in patients with hepatic impairment (defined as having two or more of the following: [1] albumin ≤3.1 g/dL; [2] ALT ≥2× ULN; [3] total bilirubin ≥1.3× ULN; or [4] mild, moderate or severe liver disease as reported by the Charlson Co-morbidity Index), as compared to patients with normal hepatic function. No clinically meaningful differences in the exposure of bezlotoxumab were found between patients with hepatic impairment and patients with normal hepatic function.
12.4 Microbiology
Mechanism of Action
Bezlotoxumab is a human monoclonal antibody that binds C. difficile toxin B with an equilibrium dissociation constant (Kd) of <1×10-9M. Bezlotoxumab inhibits the binding of toxin B and prevents its effects on mammalian cells. Bezlotoxumab does not bind to C. difficile toxin A.
Activity In Vitro
Bezlotoxumab binds to an epitope on toxin B that is conserved across reported strains of C. difficile, although amino acid sequence variation within the epitope does occur. In vitro studies in cell-based assays using Vero cells or Caco-2 cells, suggest that bezlotoxumab neutralizes the toxic effects of toxin B.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
The safety and efficacy of ZINPLAVA were investigated in two randomized, double-blind, placebo-controlled, multicenter, Phase 3 trials (Trial 1 and Trial 2) in patients receiving Standard of Care antibacterial drugs for treatment of CDI (SoC). Randomization was stratified by SoC (metronidazole, vancomycin, or fidaxomicin) and hospitalization status (inpatient vs. outpatient) at the time of study entry.
Enrolled patients were 18 years of age or older and had a confirmed diagnosis of CDI, which was defined as diarrhea (passage of 3 or more loose bowel movements in 24 or fewer hours) and a positive stool test for toxigenic C. difficile from a stool sample collected no more than 7 days before study entry. Patients were excluded if surgery for CDI was planned, or if they had uncontrolled chronic diarrheal illness. Patients received a 10- to 14-day course of oral SoC and a single infusion of ZINPLAVA or placebo was administered during the course of SoC. Patients on oral vancomycin or oral fidaxomicin could have also received intravenous metronidazole. Choice of SoC was at the discretion of the health care provider. The day of the infusion of ZINPLAVA or placebo in relation to the start of SoC ranged from the day prior to the start of SoC to 14 days after the start of SoC with the median being day 3 of SoC.
In Trial 1, 403 patients were randomized to receive ZINPLAVA and 404 patients were randomized to receive placebo. In Trial 2, 407 subjects were randomized to receive ZINPLAVA and 399 patients were randomized to receive placebo. The Full Analysis Set (FAS) was a subset of all randomized subjects with exclusions for: (i) not receiving infusion of study medication; (ii) not having a positive local stool test for toxigenic C. difficile; (iii) not receiving protocol defined standard of care therapy within a 1 day window of the infusion. The baseline characteristics of the 1554 patients randomized to ZINPLAVA or placebo in the FAS were similar across treatment arms and in Trial 1 and Trial 2. The median age was 65 years, 85% were white, 57% were female, and 68% were inpatients. A similar proportion of patients received oral metronidazole (48%) or oral vancomycin (48%) and 4% of the patients received oral fidaxomicin as their SoC.
The following risk factors associated with a high risk of CDI recurrence or CDI-related adverse outcomes were present in the study population: 51% were ≥65 years of age, 39% received one or more systemic antibacterial drugs (during the 12-week follow-up period), 28% had one or more episodes of CDI within the six months prior to the episode under treatment (15% had two or more episodes prior to the episode under treatment), 21% were immunocompromised and 16% presented at study entry with clinically severe CDI (as defined by a Zar score of ≥21). A hypervirulent strain (ribotypes 027, 078 or 244) was isolated in 22% of patients who had a positive baseline culture, of which 87% (189 of 217 strains) were ribotype 027.
Patients were assessed for clinical cure of the presenting CDI episode, defined as no diarrhea for 2 consecutive days following the completion of a ≤14 day SoC regimen. Patients who achieved clinical cure were then assessed for recurrence of CDI through 12 weeks following administration of the infusion of ZINPLAVA or placebo. CDI recurrence was defined as the development of a new episode of diarrhea associated with a positive stool test for toxigenic C. difficile following clinical cure of the presenting CDI episode. Sustained clinical response was defined as clinical cure of the presenting CDI episode and no CDI recurrence through 12 weeks after infusion. Table 2 contains the results for Trial 1 and Trial 2.
Table 2: Efficacy Results Through 12 Weeks After Infusion (Trial 1 and Trial 2, Full Analysis Set*) Trial ZINPLAVA with SoC† Placebo with SoC† Adjusted Difference
(95% CI)‡n (%) n (%) n (%) = Number (percentage) of subjects in the analysis population meeting the criteria for endpoint N = Number of subjects included in the analysis population - * Full Analysis Set = a subset of all randomized subjects with exclusions for: (i) did not receive infusion of study medication; (ii) did not have a positive local stool test for toxigenic C. difficile; (iii) did not receive protocol defined standard of care therapy within a 1 day window of the infusion
- † SoC = Standard of Care antibacterial drugs (metronidazole or vancomycin or fidaxomicin) for CDI
- ‡ Adjusted difference of ZINPLAVA-placebo (95% confidence interval) based on Miettinen and Nurminen method stratified by SoC antibacterial drugs (metronidazole vs. vancomycin vs. fidaxomicin) and hospitalization status (inpatient vs. outpatient).
1 N=386 N=395 Sustained clinical response 232 (60.1) 218 (55.2) 4.8 (-2.1, 11.7) Reasons for failure to achieve sustained clinical response: Clinical failure 87 (22.5) 68 (17.2) Recurrence 67 (17.4) 109 (27.6) 2 N=395 N=378 Sustained clinical response 264 (66.8) 197 (52.1) 14.6 (7.7, 21.4) Reasons for failure to achieve sustained clinical response: Clinical failure 69 (17.5) 84 (22.2) Recurrence 62 (15.7) 97 (25.7) In Trial 1, the clinical cure rate of the presenting CDI episode was lower in the ZINPLAVA arm as compared to the placebo arm and in Trial 2, the clinical cure rate was lower in the placebo arm compared to the ZINPLAVA arm. Patients in the ZINPLAVA and placebo arms who did not achieve clinical cure of the presenting CDI episode (no diarrhea for 2 consecutive days following the completion of a ≤14 day SoC regimen) received a mean of 18 to 19 days of SoC and had a mean of 4 additional days of diarrhea following completion of SoC. Additional analyses showed that by 3 weeks post study drug infusion the clinical cure rates of the presenting CDI episode were similar between treatment arms.
Efficacy results in patients at high risk for CDI recurrence (i.e., patients aged 65 years and older, with a history of CDI in the past 6 months, immunocompromised state, severe CDI at presentation, or C. difficile ribotype 027) were consistent with the efficacy results in the overall trial population in Trials 1 and 2.
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ZINPLAVA Injection: is a sterile, preservative-free, clear to moderately opalescent, colorless to pale yellow solution and is supplied in the following packaging configuration:
Carton (NDC: 0006-3025-00) containing one (1) single-dose vial of ZINPLAVA 1,000 mg/40 mL (25 mg/mL).
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Concurrent Antibacterial Therapy
Inform patients that ZINPLAVA does not take the place of their antibacterial treatment for their CDI infection. They must continue their antibacterial treatment as directed [see Indications and Usage (1) and Dosage and Administration (2.1)].
-
SPL UNCLASSIFIED SECTION
Manufactured by: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USA
U.S. License No. 0002At:
MSD Ireland (Carlow)
County Carlow, IrelandFor patent information: www.merck.com/product/patent/home.html
Copyright © 2016 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All rights reserved.uspi-mk6072-iv-1610r000
-
PATIENT PACKAGE INSERT
Patient Information
ZINPLAVA™ (zin-PLAH-va)
(bezlotoxumab)
injection, for intravenous useWhat you need to know about ZINPLAVA - Before you receive ZINPLAVA, be sure you understand what it is for and how it is given.
- ZINPLAVA helps decrease the risk of C-diff (Clostridium difficile infection) from coming back by working with the antibiotic that you are taking to treat your C-diff. ZINPLAVA does not replace the antibiotic. ZINPLAVA is not an antibiotic.
- Keep taking your antibiotic for your C-diff as directed by your doctor.
- If you have questions about ZINPLAVA, ask your doctor or pharmacist.
- Keep this Patient Information for ZINPLAVA so you can read it again.
What is ZINPLAVA?ZINPLAVA is a prescription medicine used to help decrease the risk of C-diff from coming back in people 18 years of age or older who are taking an antibiotic for C-diff and who have a high risk of C-diff coming back.
C-diff is a bacterial infection that can damage your colon and cause stomach pain and severe diarrhea. When people get C-diff, they often take an antibiotic to get rid of the infection. Even when treated by an antibiotic, C-diff can come back within weeks to months. ZINPLAVA helps to decrease the risk of the infection from coming back. It works when given along with the antibiotic that you are taking to treat C-diff.
How will I receive ZINPLAVA?- You will receive ZINPLAVA into your vein through an IV (intravenously).
- You do not need to do anything to prepare for receiving ZINPLAVA.
- You will receive ZINPLAVA in 1 dose and it will take about 1 hour.
- If you miss your appointment, call your doctor right away to reschedule it.
Is ZINPLAVA right for me? Children - It is not known if ZINPLAVA is safe and effective in children under 18 years old.
Pregnancy
- If you are pregnant or trying to get pregnant, tell your doctor before you receive ZINPLAVA.
- It is not known if ZINPLAVA will harm your baby while you are pregnant.
- You and your doctor should decide together if you will receive ZINPLAVA.
Breastfeeding
- If you are breastfeeding or plan to breastfeed, tell your doctor before you receive ZINPLAVA.
- It is not known if ZINPLAVA gets in your breast milk and will be passed to your baby.
- You and your doctor should decide together if you will receive ZINPLAVA.
Medical Conditions
- Tell your doctor about any medical conditions you have now or have had before.
- Make sure to tell your doctor if you have or have had congestive heart failure (CHF).
Other Medicines
- Tell your doctor about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side effects of ZINPLAVA? ZINPLAVA may cause serious side effects, including: - Heart failure. Heart failure may happen in people who receive ZINPLAVA and can be serious. People with a history of congestive heart failure (CHF) who received ZINPLAVA had a higher rate of heart failure and death than those who did not receive ZINPLAVA.
Common side effects of ZINPLAVA:
The most common side effects that may happen on the day of or the day after receiving ZINPLAVA:- nausea
- headache
- fever
- feeling tired
- shortness of breath
- feeling dizzy
- high blood pressure
The most common side effects that may happen up to four weeks after receiving ZINPLAVA: - nausea
- fever
- headache
If you have any side effect that bothers you or does not go away, tell your doctor.
There may be other side effects to ZINPLAVA that are not listed. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of ZINPLAVA.Medicines are sometimes prescribed for purposes other than those listed in the Patient Information. You can ask your pharmacist or doctor for information about ZINPLAVA that is written for doctors.
What if I have questions?- Call your doctor.
- Call Merck, the company that makes ZINPLAVA, at 1-800-444-2080.
- Go to the website – www.ZINPLAVA.com
You can also find the full prescribing information written for doctors at www.ZINPLAVA.com
What are the ingredients in ZINPLAVA? The active ingredient is: bezlotoxumab
The inactive ingredients are: citric acid monohydrate, diethylenetriaminepentaacetic acid, polysorbate 80, sodium chloride, sodium citrate dihydrate, and water for injection, USP. ZINPLAVA may also contain sodium hydroxide.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Manufactured by: Merck Sharp & Dohme Corp., a subsidiary of
MERCK & CO., INC., Whitehouse Station, NJ 08889, USAU.S. License No. 0002
At:
MSD Ireland (Carlow)
County Carlow, Ireland
For patent information: www.merck.com/product/patent/home.html
Copyright © 2016 Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
All rights reserved.
Issued: 10/2016
usppi-mk6072-iv-1610r000 -
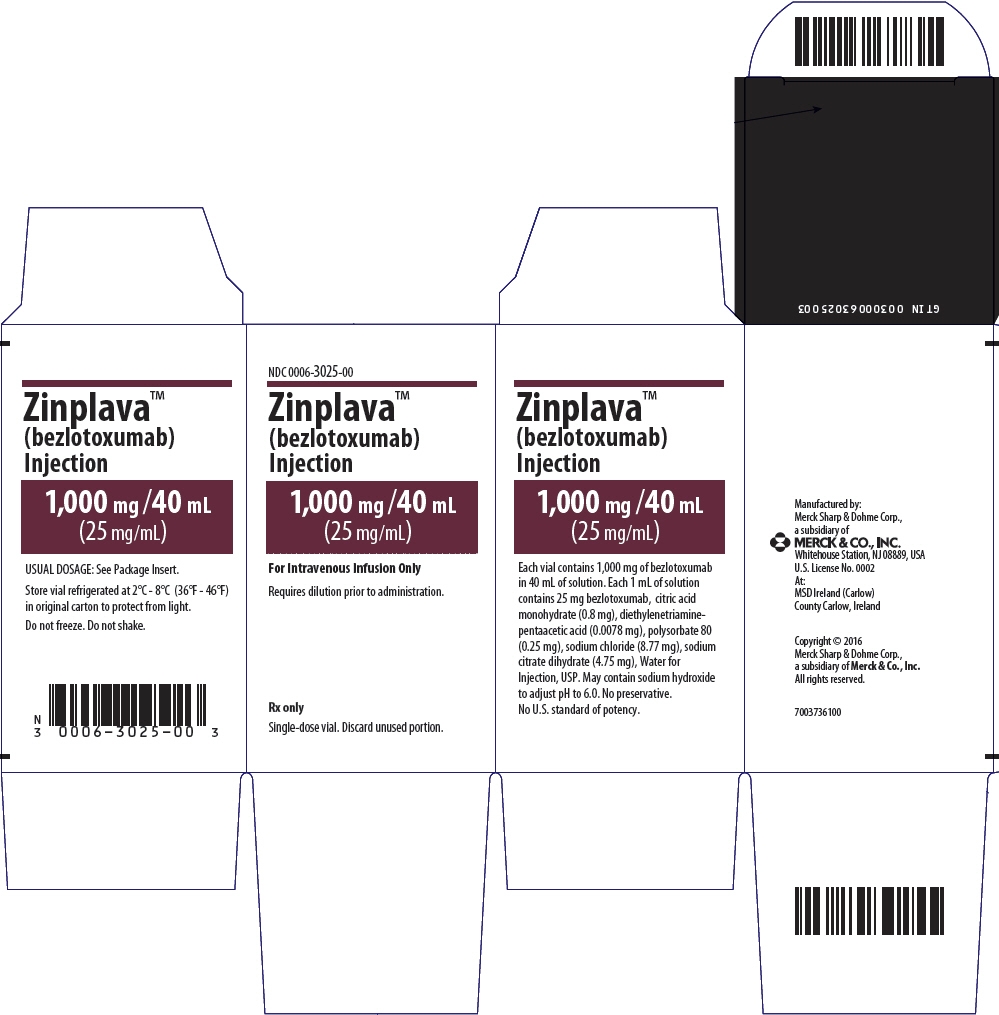
PRINCIPAL DISPLAY PANEL - 1,000 mg/40 mL Vial Carton
NDC: 0006-3025-00
Zinplava™
(bezlotoxumab)
Injection1,000 mg /40 mL
(25 mg/mL)For Intravenous Infusion Only
Requires dilution prior to administration.
Rx only
Single-dose vial. Discard unused portion.
-
INGREDIENTS AND APPEARANCE
ZINPLAVA
bezlotoxumab injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 0006-3025 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength bezlotoxumab (UNII: 4H5YMK1H2E) (bezlotoxumab - UNII:4H5YMK1H2E) bezlotoxumab 25 mg in 1 mL Inactive Ingredients Ingredient Name Strength CITRIC ACID MONOHYDRATE (UNII: 2968PHW8QP) 0.8 mg in 1 mL PENTETIC ACID (UNII: 7A314HQM0I) 0.0078 mg in 1 mL POLYSORBATE 80 (UNII: 6OZP39ZG8H) 0.25 mg in 1 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 8.77 mg in 1 mL TRISODIUM CITRATE DIHYDRATE (UNII: B22547B95K) 4.75 mg in 1 mL WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) Product Characteristics Color YELLOW (clear to moderately opalescent, colorless to pale yellow) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 0006-3025-00 1 in 1 CARTON 10/21/2016 1 NDC: 0006-3025-01 40 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA761046 10/21/2016 Labeler - Merck Sharp & Dohme Corp. (001317601)
Trademark Results [ZINPLAVA]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 ZINPLAVA 86884102 5360500 Live/Registered |
Merck Sharp & Dohme Corp. 2016-01-22 |
 ZINPLAVA 86884098 5360499 Live/Registered |
Merck Sharp & Dohme Corp. 2016-01-22 |
 ZINPLAVA 86851397 not registered Dead/Abandoned |
Merck Sharp & Dohme Corp. 2015-12-16 |
 ZINPLAVA 86607706 5209883 Live/Registered |
Merck Sharp & Dohme Corp. 2015-04-23 |
 ZINPLAVA 86239391 not registered Dead/Abandoned |
Merck Sharp & Dohme Corp. 2014-04-01 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.