RIASTAP- fibrinogen human injection, powder, lyophilized, for solution
RiaSTAP by
Drug Labeling and Warnings
RiaSTAP by is a Other medication manufactured, distributed, or labeled by CSL Behring GmbH. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use RiaSTAP® safely and effectively. See full prescribing information for RiaSTAP.
RiaSTAP, Fibrinogen Concentrate (Human)
Lyophilized Powder for Solution for Intravenous Injection
Initial U.S. Approval: 2009INDICATIONS AND USAGE
RiaSTAP, Fibrinogen Concentrate (Human) is a human blood coagulation factor indicated for the treatment of acute bleeding episodes in patients with congenital fibrinogen deficiency, including afibrinogenemia and hypofibrinogenemia. (1)
DOSAGE AND ADMINISTRATION
For intravenous use only.
-
Dose (mg/kg body weight) =
[Target level (mg/dL) - measured level (mg/dL)]
1.7 (mg/dL per mg/kg body weight) - Dose when fibrinogen level is unknown: 70 mg/kg body weight. (2.1)
- Monitoring of patient's fibrinogen level is recommended during treatment. A target fibrinogen level of 100 mg/dL should be maintained until hemostasis is obtained. (2.1)
- Injection rate should not exceed 5 mL per minute. (2.3)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
Known anaphylactic or severe systemic reactions to human plasma-derived products (4)
WARNINGS AND PRECAUTIONS
- Monitor patients for early signs of anaphylaxis or hypersensitivity reactions and if necessary, discontinue administration and institute appropriate treatment. (5.1)
- Thrombotic events have been reported in patients receiving RiaSTAP. Weigh the benefits of administration versus the risks of thrombosis. (5.2)
- Because RiaSTAP is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. (5.3)
ADVERSE REACTIONS
- The most serious adverse reactions observed are thrombotic episodes (pulmonary embolism, myocardial infarction, deep vein thrombosis) and anaphylactic reactions. (6)
- The most common adverse reactions observed in clinical studies (frequency >1%) were fever and headache. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact CSL Behring at 1-866-915-6958 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
USE IN SPECIFIC POPULATIONS
- Pediatric: Shorter half-life and faster clearance than in adults has been observed. (8.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 4/2019
-
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Congenital Fibrinogen Deficiency
2.2 Preparation and Reconstitution
2.3 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
5.2 Thrombosis
5.3 Transmissible Infectious Agents
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamic Action
12.3 Pharmacokinetics
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For intravenous use only.
2.1 Treatment of Congenital Fibrinogen Deficiency
RiaSTAP dosing, duration of dosing and frequency of administration should be individualized based on the extent of bleeding, laboratory values, and the clinical condition of the patient.
RiaSTAP dose when baseline fibrinogen level is known.
Dose should be individually calculated for each patient based on the target plasma fibrinogen level based on the type of bleeding, actual measured plasma fibrinogen level and body weight, using the following formula [see Clinical Pharmacology (12.3)]:
[Target level (mg/dL) - measured level (mg/dL)] 1.7 (mg/dL per mg/kg body weight) RiaSTAP dose when baseline fibrinogen level is not known.
If the patient's fibrinogen level is not known, the recommended dose is 70 mg per kg of body weight administered intravenously.
Monitor patient's fibrinogen level during treatment with RiaSTAP. Maintain a target fibrinogen level of 100 mg/dL until hemostasis is obtained.
2.2 Preparation and Reconstitution
The procedures below are provided as general guidelines for preparation and reconstitution of RiaSTAP.
Use aseptic technique when preparing and reconstituting RiaSTAP.
Reconstitute RiaSTAP at room temperature as follows:
- Remove the cap from the product vial to expose the central portion of the rubber stopper.
- Clean the surface of the rubber stopper with an antiseptic solution and allow it to dry.
- Using an appropriate transfer device or syringe, transfer 50 mL of Sterile Water for Injection into the product vial.
- Gently swirl the product vial to ensure the product is fully dissolved. Do not shake the vial.
After reconstitution, the RiaSTAP solution should be colorless and clear to slightly opalescent. Inspect visually for particulate matter and discoloration prior to administration. Do not use if the solution is cloudy or contains particulates. Discard partially used vials.
RiaSTAP is stable for 8 hours after reconstitution when stored at 20-25°C; administer within this time period.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
RiaSTAP is contraindicated in patients with known anaphylactic or severe systemic reactions to human plasma-derived products [see Description (11)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
Allergic reactions may occur. If signs or symptoms of anaphylaxis or hypersensitivity reactions (including hives, generalized urticaria, tightness of the chest, wheezing, hypotension) occur, immediately discontinue administration [see Patient Counseling Information (17)]. The treatment required depends on the nature and severity of the reaction.
5.2 Thrombosis
Thrombosis may occur spontaneously in patients with congenital fibrinogen deficiency with or without the use of fibrinogen replacement therapy.1 Thromboembolic events have been reported in patients treated with RiaSTAP. Weigh the benefits of RiaSTAP administration versus the risk of thrombosis. Monitor patients receiving RiaSTAP for signs and symptoms of thrombosis [see Patient Counseling Information (17)].
5.3 Transmissible Infectious Agents
Because RiaSTAP is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. The risk that such products will transmit an infectious agent has been reduced by screening plasma donors for prior exposure to certain viruses, by testing for the presence of certain current virus infections, and by a process demonstrated to inactivate and/or remove certain viruses during manufacturing [see Description (11)]. Despite these measures, such products may still potentially transmit disease. There is also the possibility that unknown infectious agents may be present in such products [see Patient Counseling Information (17)]. All infections thought by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to CSL Behring Pharmacovigilance at 1-866-915-6958.
-
6 ADVERSE REACTIONS
The most serious adverse reactions reported in clinical studies or through postmarketing surveillance following RiaSTAP treatment are thromboembolic episodes, including myocardial infarction, pulmonary embolism, deep vein thrombosis, arterial thrombosis, and allergic-anaphylactic reactions.
The most common adverse reactions observed in more than one subject in clinical studies (frequency >1%) were fever and headache.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in practice.
6.2 Postmarketing Experience
Because postmarketing reporting of adverse reactions is voluntary and from a population of uncertain size, it is not always possible to reliably estimate the frequency of these reactions or establish a causal relationship to product exposure.
The following adverse reactions, identified by system organ class, have shown a possible causal relationship with RiaSTAP.
- Allergic-anaphylactic reactions: anaphylaxis, dyspnea, rash
- Cardiovascular: thromboembolic complications such as myocardial infarction, pulmonary embolism, and deep vein thrombosis [see Warnings and Precautions (5.2)]
- General/Body as a Whole: chills, nausea, vomiting
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no studies of RiaSTAP use in pregnant women. Animal reproduction studies have not been conducted with RiaSTAP. It is not known whether RiaSTAP can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. RiaSTAP should be used during pregnancy only if clearly needed. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
8.2 Lactation
Risk Summary
There is no information regarding the presence of RiaSTAP in human milk, its effects on the breastfed infant, or its effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for RiaSTAP and any potential adverse effects on the breastfed infant from RiaSTAP or from the underlying maternal condition.
8.4 Pediatric Use
RiaSTAP studies have included subjects below the age of 16 years. In the pharmacokinetic study [see Clinical Pharmacology (12.3)], 2 children aged 8 and 11 years and 3 adolescents aged 12, 14 and 16 years were studied. Subjects <16 years of age (n = 4) had shorter half-life (69.9 ± 8.5 h) and faster clearance (0.7 ± 0.1 mg/L) compared with adults (half-life: 82.3 ± 20.0 h, clearance: 0.53 ± 0.1 mg/L). The number of subjects <16 years of age in this study limits statistical interpretation.
-
11 DESCRIPTION
RiaSTAP is a sterile, heat-treated, lyophilized fibrinogen (coagulation factor I) concentrate powder manufactured from pooled human plasma.
Fibrinogen (factor I) is a soluble plasma glycoprotein with a molecular weight of about 340 kDa. The native molecule is a dimer and consists of three pairs of polypeptide chains (Aα, Bβ and γ). Fibrinogen is a physiological substrate of three enzymes: thrombin, factor XIIIa, and plasmin.
Each vial contains 900 to 1300 mg fibrinogen, 400 to 700 mg human albumin, 375 to 660 mg L-arginine hydrochloride, 200 to 350 mg sodium chloride and 50 to 100 mg sodium citrate. Sodium hydroxide and hydrochloric acid may have been used to adjust the pH. The pH of the reconstituted RiaSTAP is in a range of 6.5 to 7.5.
Viral Clearance
All plasma used in the manufacture of RiaSTAP is tested using serological assays for hepatitis B surface antigen and for antibodies to Human Immunodeficiency Virus (HIV)-1/2 and Hepatitis C Virus (HCV). As an additional safety measure, the plasma is tested with Nucleic Acid Testing (NAT) for Hepatitis B Virus (HBV), HCV and HIV-1 and found to be non-reactive (negative). The plasma is also screened for Hepatitis A Virus (HAV) and Human Parvovirus B19 (B19V) by NAT. Only plasma that passed virus screening is used for production, and the limit for B19V in the fractionation pool is set not to exceed 104 IU of B19V DNA per mL.
RiaSTAP is manufactured from cryoprecipitate into a glycine precipitate, which is then further purified by multiple precipitation/adsorption steps. The manufacturing process has been demonstrated to reduce the risk of virus transmission in an additive manner: cryoprecipitation, heat treatment (+60ºC for 20 hours in an aqueous solution), two subsequent glycine precipitation steps (initial and main glycine precipitation steps), and lyophilization. These steps have been validated independently in a series of in vitro experiments for their capacity to inactivate and/or remove both enveloped and non-enveloped viruses. The results of virus clearance validation studies for RiaSTAP manufacturing process are summarized in Table 1.
Table 1. Cumulative (Log10) Virus Reduction Factors for RiaSTAP Manufacturing Step Virus Reduction Factor (log10) Enveloped viruses Non-enveloped viruses HIV* BVDV† WNV‡ PRV§ HAV¶ CPV# Studies using human parvovirus B19, which are considered experimental in nature, have demonstrated a virus reduction factor of ≥4.5 log10 by heat treatment n.d. not determined - * HIV, human immunodeficiency virus, a model for HIV-1 and HIV-2
- † BVDV, bovine viral diarrhea virus, a model for Hepatitis C virus (HCV) and West Nile Virus (WNV)
- ‡ WNV, West Nile virus
- § PRV, Pseudorabies virus, a model for large enveloped DNA viruses
- ¶ HAV, Hepatitis A virus
- # CPV, canine parvovirus, a model for B19V
Cryoprecipitation n.d. n.d. n.d. 1.6 n.d. 1.9 Heat Treatment ≥5.7 ≥9.1 ≥8.3 5.4 5.9 1.4 Glycine precipitations
(two subsequent steps)3.9 2.1 n.d. 1.8 1.0 1.6 Lyophilization n.d. n.d. n.d. n.d. 1.7 n.d. Cumulative virus reduction (log10) ≥9.6 ≥11.2 ≥8.3 8.8 8.6 4.9 -
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
During the coagulation process, thrombin cleaves the Aα and Bβ chains releasing fibrinopeptides A and B (FPA and FPB, respectively).2 FPA is separated rapidly and the remaining molecule is a soluble fibrin monomer (fibrin I). The slower removal of FPB results in formation of fibrin II that is capable of polymerization that occurs by aggregation of fibrin monomers.2 The resulting fibrin is stabilized in the presence of calcium ions and by activated factor XIII, which acts as a transglutaminase. Factor XIIIa-induced cross-linking of fibrin polymers renders the fibrin clot more elastic and more resistant to fibrinolysis.3 Cross-linked fibrin is the end result of the coagulation cascade, and provides tensile strength to a primary hemostatic platelet plug and structure to the vessel wall.
12.2 Pharmacodynamic Action
Administration of RiaSTAP to patients with congenital fibrinogen deficiency replaces missing or low levels of coagulation factor. Normal levels are in the range of 200 to 450 mg/dL.4
12.3 Pharmacokinetics
A prospective, open label, uncontrolled, multicenter pharmacokinetic study was conducted in 5 females and 9 males with congenital fibrinogen deficiency (afibrinogenemia), ranging in age from 8 to 61 years (2 children, 3 adolescents, 9 adults). Each subject received a single intravenous dose of 70 mg/kg RiaSTAP. Blood samples were collected to determine fibrinogen activity at baseline and up to 14 days after infusion. The pharmacokinetic parameters of RiaSTAP are summarized in Table 2.
No statistically relevant difference in fibrinogen activity was observed between males and females. Subjects <16 years of age (n=4) had shorter half-life (69.9 ± 8.5 h) and faster clearance (0.73 ± 0.14 mg/L) compared with subjects ≥16 years of age (half-life of 82.5 ± 20.0 h and clearance of 0.53 ± 0.07 mg/L). The number of subjects <16 years of age in this study limits statistical interpretation.
The incremental in vivo recovery (IVR) was determined from levels obtained up to 4 hours post-infusion. The median incremental IVR was 1.7 mg/dL (range 1.30 – 2.73 mg/dL) increase per mg/kg. The median in vivo recovery indicates that a dose of 70 mg/kg will increase fibrinogen plasma concentration in patients by approximately 120 mg/dL.
The pharmacokinetic analysis using fibrinogen antigen data (ELISA) was concordant with the fibrinogen activity (Clauss assay).
Table 2. Pharmacokinetic Parameters (n=14) for Fibrinogen Activity Parameters Mean ± SD (range) Half-life [hours] 78.7 ± 18.13 (55.73-117.26) Cmax [mg/dL] 140 ± 27 (100-210) AUC for dose of 70 mg/kg [mg*hr/mL] 124.3 ± 24.16 (81.73-156.40) Clearance [mL/h/kg] 0.59 ± 0.13 (0.45-0.86) Mean residence time [hours] 92.8 ± 20.11 (66.14-126.44) Volume of distribution at steady state [mL/kg] 52.7 ± 7.48 (36.22-67.67) -
14 CLINICAL STUDIES
The efficacy of RiaSTAP is based on maximum clot firmness, a measure of clot structural integrity that reflects the underlying effectiveness of the fibrinogen present to form a fibrin clot. A pharmacokinetic study evaluated single-dose PK [see Clinical Pharmacology (12.3)] and maximum clot firmness (MCF) in subjects with afibrinogenemia. MCF was determined by thromboelastometry (ROTEM) testing and was used to demonstrate functional activity of replacement fibrinogen when a fixed dose of RiaSTAP was administered. Clot firmness is a functional parameter that depends on activation of coagulation, fibrinogen content of the sample and polymerization/crosslinking of the fibrin network. Thromboelastometry has been shown to be a functional marker for assessment of fibrinogen content and for effects of fibrinogen supplementation on clinical efficacy.5
For each subject, MCF was determined before (baseline) and one hour after single dose administration of RiaSTAP. RiaSTAP was found to be effective in increasing clot firmness in subjects with congenital fibrinogen deficiency (afibrinogenemia) as measured by thromboelastometry. The study results demonstrated that MCF values were significantly higher after administration of RiaSTAP than at baseline (see Table 3). Mean change from pre-infusion to 1 hour post-infusion was 8.9 mm in the primary analysis (9.9 mm for subjects <16years old and 8.5 mm for subjects ≥16 to <65 years old). Mean change in MCF values closely approximated levels expected from adding known amounts of fibrinogen to plasma in vitro.6
Table 3. MCF [mm] (ITT population) Time point n Mean ± SD Median (range) MCF = maximum clot firmness; mm = millimeter; ITT = intention-to-treat. - * p-value was <0.0001.
- † The mean change was set to 0 for 2 subjects with missing MCF data.
Pre-infusion 13 0 ± 0 0 (0-0) 1 hour post-infusion 13 10.3 ± 2.7 10.0 (6.5-16.5) Mean change (primary analysis)* 15† 8.9 ± 4.4 9.5 (0-16.5) -
15 REFERENCES
- Peyvandi F, Haertal S, Knaub S, et al. Incidence of bleeding symptoms in 100 patients with inherited afibrinogenemia or hypofibrinogenemia. J Thromb Haemost 2006; 4:1634-7.
- Kreuz W, Meili E, Peter-Salonen K, et al. Pharmacokinetic properties of a pasteurized fibrinogen concentrate. Transfusion and Apheresis Science 2005; 32:239-46.
- Colman R, Clowes A, George J, et al. Overview of Hemostasis. In: Hemostasis and Thrombosis: Basic Principles and Clinical Practice (5th ed.). Colman R, Clowes A, George J, Goldhaber S, Marder VJ (eds.). Lippincott Williams & Wilkins, Philadelphia 2006:11-14.
- Kreuz W, Meili E, Peter-Salonen K, et al. Efficacy and tolerability of a pasteurized human fibrinogen concentrate in patients with congenital fibrinogen deficiency. Transfusion and Apheresis Science 2005; 32:247-253.
- Fries D, Innerhofer P, Reif C, et al. The Effect of Fibrinogen Substitution on Reversal of Dilutional Coagulopathy: An In Vitro Model. Anesth Analg 2006; 102:347-351.
- Kalina U, Stöhr HA, Bickhard H, et. al. Rotational thromboelastography for monitoring of fibrinogen concentrate therapy in fibrinogen deficiency. Blood Coagulation and Fibrinolysis. 2008; 19:777-783.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
- RiaSTAP is supplied in a single-use vial.
- Each carton contains one vial of RiaSTAP.
- Components are not made with natural rubber latex.
- RiaSTAP contains no preservative.
- The actual potency of fibrinogen concentrate in milligram (mg) is stated on each RiaSTAP vial label and carton.
The product presentation includes a package insert and the following component:
Presentation Carton NDC Number Component 900-1300 mg 63833-891-51 RiaSTAP in a single-use vial (NDC: 63833-891-90) -
17 PATIENT COUNSELING INFORMATION
-
Allergic Reactions
Inform patients of the early signs of allergic or hypersensitivity reactions to RiaSTAP, including hives, chest tightness, wheezing, hypotension, and anaphylaxis. Advise them to notify their physician immediately if they experience any of these symptoms [see Warnings and Precautions (5.1)].
-
Thrombosis
Inform patients that thrombosis with or without embolization has been reported with the use of RiaSTAP. Any symptoms of thrombotic events such as unexplained pleuritic, chest and/or leg pain or edema, hemoptysis, dyspnea, tachypnea or unexplained neurologic symptoms should be reported to their physician immediately [see Warnings and Precautions (5.2)].
-
Transmissible Infectious Agents
Inform patients that RiaSTAP is made from human plasma (part of the blood) and may carry a risk of transmitting infectious agents e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. Explain that the risk of transmitting an infection agent using RiaSTAP has been reduced by screening plasma donors, testing the donated plasma for certain virus infections, and incorporating a process demonstrated to inactivate and/or remove certain viruses during manufacturing. Symptoms of possible virus infection include headache, fever, nausea, vomiting, weakness, malaise, diarrhea, or, in the case of hepatitis, jaundice [see Warnings and Precautions (5.3)].
-
- SPL UNCLASSIFIED SECTION
-
PRINCIPAL DISPLAY PANEL - 50 mL Vial Label
NDC: 63833-891-90
Fibrinogen Concentrate
(Human)
RiaSTAP®For Intravenous
Administration OnlyManufactured by:
CSL Behring GmbH
35041 Marburg, Germany
US License No. 1765Distributed by:
CSL Behring LLC
Kankakee, IL 60901 USA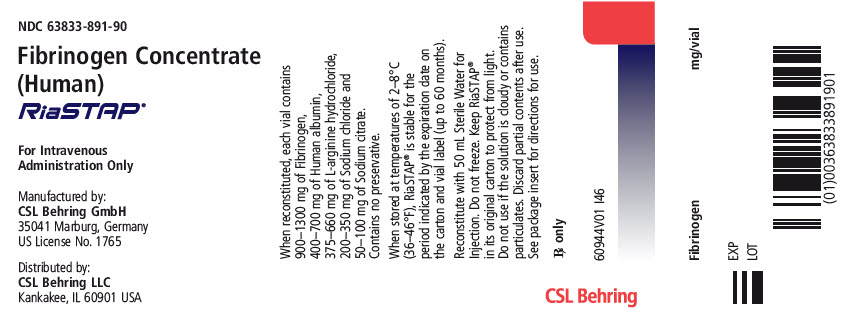
-
PRINCIPAL DISPLAY PANEL - 50 mL Vial Carton
NDC: 63833-891-51
One Vial
Fibrinogen Concentrate (Human)
RiaSTAP®
One single-use vial containing
900 mg – 1300 mg of lyophilized
fibrinogen for reconstitution.For Intravenous Administration Only
CSL Behring

-
INGREDIENTS AND APPEARANCE
RIASTAP
fibrinogen human injection, powder, lyophilized, for solutionProduct Information Product Type PLASMA DERIVATIVE Item Code (Source) NDC: 63833-891 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FIBRINOGEN HUMAN (UNII: N94833051K) (FIBRINOGEN HUMAN - UNII:N94833051K) FIBRINOGEN HUMAN 1300 mg in 50 mL Inactive Ingredients Ingredient Name Strength Albumin Human (UNII: ZIF514RVZR) 700 mg in 50 mL arginine hydrochloride (UNII: F7LTH1E20Y) 660 mg in 50 mL Sodium chloride (UNII: 451W47IQ8X) 350 mg in 50 mL Sodium citrate, unspecified form (UNII: 1Q73Q2JULR) 100 mg in 50 mL Water (UNII: 059QF0KO0R) Sodium hydroxide (UNII: 55X04QC32I) hydrochloric acid (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 63833-891-51 1 in 1 CARTON 1 NDC: 63833-891-90 50 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125317 01/16/2009 Labeler - CSL Behring GmbH (326530474) Establishment Name Address ID/FEI Business Operations CSL Behring GmbH 326530474 MANUFACTURE(63833-891)
Trademark Results [RiaSTAP]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 RIASTAP 77892481 3852693 Live/Registered |
CSL Behring GmbH 2009-12-14 |
 RIASTAP 77434377 3655552 Live/Registered |
CSL Behring GmbH 2008-03-28 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.