MEROPENEM injection, powder, for solution
Meropenem by
Drug Labeling and Warnings
Meropenem by is a Prescription medication manufactured, distributed, or labeled by Sagent Pharmaceuticals. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use MEROPENEM FOR INJECTION safely and effectively. See full prescribing information for MEROPENEM FOR INJECTION
MEROPENEM for Injection, for intravenous use
Initial U.S. Approval: 1996INDICATIONS AND USAGE
Meropenem for Injection is a penem antibacterial indicated for the treatment of:
- Complicated skin and skin structure infections (adult patients and pediatric patients 3 months of age and older only). (1.1)
- Complicated intra-abdominal infections (adult and pediatric patients). (1.2)
- Bacterial meningitis (pediatric patients 3 months of age and older only). (1.3)
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Meropenem for Injection and other antibacterial drugs, Meropenem for Injection should only be used to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria.
DOSAGE AND ADMINISTRATION
- 500 mg every 8 hours by intravenous infusion over 15 to 30 minutes for complicated skin and skin structure infections (cSSSI) for adult patients. When treating infections caused by Pseudomonas aeruginosa, a dose of 1 gram every 8 hours is recommended. (2.1)
- 1 gram every 8 hours by intravenous infusion over 15 minutes to 30 minutes for intra-abdominal infections for adult patients. (2.1)
- 1 gram every 8 hours by intravenous bolus injection (5 mL to 20 mL) over 3 minutes to 5 minutes for adult patients. (2.1)
- Dosage should be reduced in adult patients with renal impairment. (2.2)
Recommended Meropenem for Injection Dosage Schedule for Adult Patients with Renal Impairment Creatinine Clearance (mL/min) Dose (dependent on type of infection) Dosing Interval Greater than 50 Recommended dose (500 mg cSSSI and 1 gram Intra-abdominal) Every 8 hours 26 to 50 Recommended dose Every 12 hours 10 to 25 One-half recommended dose Every 12 hours Less than 10 One-half recommended dose Every 24 hours Pediatric patients 3 months of age and older
- Intravenous infusion is to be given over approximately 15 minutes to 30 minutes.
- Intravenous bolus injection (5 mL to 20 mL) is to be given over approximately 3 minutes to 5 minutes.
- There is no experience in pediatric patients with renal impairment.
* 20 mg/kg (or 1 gram for pediatric patients weighing over 50 kg) every 8 hours is recommended when treating complicated skin and skin structure infections caused by P. aeruginosa. (2.3)
Recommended Meropenem for Injection Dosage Schedule for Pediatric Patients 3 Months of Age and Older with Normal Renal Function (2.3) Type of Infection Dose (mg/kg) Up to a Maximum Dose Dosing Interval Complicated skin and skin structure* 10 500 mg Every 8 hours Intra-abdominal 20 1 gram Every 8 hours Meningitis 40 2 grams Every 8 hours Pediatric patients less than 3 months of age
Intravenous infusion is to be given over 30 minutes.
There is no experience in pediatric patients with renal impairment. GA: gestational age and PNA: postnatal age
Recommended Meropenem for Injection Dosage Schedule for Pediatric Patients Less than 3 Months of Age with Complicated Intra-Abdominal Infections and Normal Renal Function (2.3) Age Group Dose (mg/kg) Dose Interval Infants less than 32 weeks GA and PNA less than 2 weeks 20 Every 12 hours Infants less than 32 weeks GA and PNA 2 weeks and older 20 Every 8 hours Infants 32 weeks and older GA and PNA less than 2 weeks 20 Every 8 hours Infants 32 weeks and older GA and PNA 2 weeks and older 30 Every 8 hours DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
Known hypersensitivity to product components or anaphylactic reactions to β-lactams. (4)
WARNINGS AND PRECAUTIONS
- Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving β-lactams. (5.1)
- Seizures and other adverse CNS experiences have been reported during treatment. (5.2)
- Co-administration of Meropenem for Injection with valproic acid or divalproex sodium reduces the serum concentration of valproic acid potentially increasing the risk of breakthrough seizures. (5.3, 7.2)
- Clostridium difficile-associated diarrhea (ranging from mild diarrhea to fatal colitis) has been reported. Evaluate if diarrhea occurs. (5.4)
- In patients with renal dysfunction, thrombocytopenia has been observed. (5.7)
ADVERSE REACTIONS
Most common adverse reactions (2% or less) are: headache, nausea, constipation, diarrhea, anemia, vomiting, and rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Sagent Pharmaceuticals, Inc. at 1-866-625-1618 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Co-administration of Meropenem for Injection with probenecid inhibits renal excretion of meropenem and is therefore not recommended . (7.1)
- The concomitant use of Meropenem for Injection and valproic acid or divalproex sodium is generally not recommended. Antibacterial drugs other than carbapenems should be considered to treat infections in patients whose seizures are well controlled on valproic acid or divalproex sodium. (5.3, 7.2)
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 5/2017
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Complicated Skin and Skin Structure Infections (Adult Patients and Pediatric Patients 3 Months of Age and Older Only)
1.2 Complicated Intra-abdominal Infections (Adult and Pediatric Patients)
1.3 Bacterial Meningitis (Pediatric Patients 3 Months of Age and Older Only)
1.4 Usage
2 DOSAGE AND ADMINISTRATION
2.1 Adult Patients
2.2 Use in Adult Patients with Renal Impairment
2.3 Use in Pediatric Patients
2.4 Preparation and Administration of Meropenem for Injection
2.5 Compatibility
2.6 Stability and Storage
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
5.2 Seizure Potential
5.3 Risk of Breakthrough Seizures Due to Drug Interaction with Valproic Acid
5.4 Clostridium difficile–associated Diarrhea
5.5 Development of Drug-Resistant Bacteria
5.6 Overgrowth of Nonsusceptible Organisms
5.7 Thrombocytopenia
5.8 Potential for Neuromotor Impairment
6 ADVERSE REACTIONS
6.1 Adverse Reactions from Clinical Trials
6.2 Post-marketing Experience
7 DRUG INTERACTIONS
7.1 Probenecid
7.2 Valproic Acid
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Complicated Skin and Skin Structure Infections
14.2 Complicated Intra-Abdominal Infections
14.3 Bacterial Meningitis
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1 INDICATIONS AND USAGE
1.1 Complicated Skin and Skin Structure Infections (Adult Patients and Pediatric Patients 3 Months of Age and Older Only)
Meropenem for Injection is indicated for the treatment of complicated skin and skin structure infections (cSSSI) due to Staphylococcus aureus (methicillin-susceptible isolates only), Streptococcus pyogenes, Streptococcus agalactiae, viridans group streptococci, Enterococcus faecalis (vancomycin-susceptible isolates only), Pseudomonas aeruginosa, Escherichia coli, Proteus mirabilis, Bacteroides fragilis, and Peptostreptococcus species.
1.2 Complicated Intra-abdominal Infections (Adult and Pediatric Patients)
Meropenem for Injection is indicated for the treatment of complicated appendicitis and peritonitis caused by viridans group streptococci, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Bacteroides fragilis, B. thetaiotaomicron, and Peptostreptococcus species.
1.3 Bacterial Meningitis (Pediatric Patients 3 Months of Age and Older Only)
Meropenem for Injection is indicated for the treatment of bacterial meningitis caused by Haemophilus influenzae, Neisseria meningitidis and penicillin-susceptible isolates of Streptococcus pneumoniae.
Meropenem for Injection has been found to be effective in eliminating concurrent bacteremia in association with bacterial meningitis.
1.4 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Meropenem for Injection and other antibacterial drugs, Meropenem for Injection should only be used to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
-
2 DOSAGE AND ADMINISTRATION
2.1 Adult Patients
The recommended dose of meropenem for injection is 500 mg given every 8 hours for skin and skin structure infections and 1 gram given every 8 hours for intra-abdominal infections. When treating complicated skin and skin structure infections caused by P. aeruginosa, a dose of 1 gram every 8 hours is recommended.
Meropenem for injection should be administered by intravenous infusion over approximately 15 minutes to 30 minutes. Doses of 1 gram may also be administered as an intravenous bolus injection (5 mL to 20 mL) over approximately 3 minutes to 5 minutes.
2.2 Use in Adult Patients with Renal Impairment
Dosage should be reduced in patients with creatinine clearance of 50 mL/min or less. (See dosing table below.)
When only serum creatinine is available, the following formula (Cockcroft and Gault equation)5 may be used to estimate creatinine clearance.
Males: Creatinine Clearance (mL/min) = Weight (kg) x (140 - age)
72 x serum creatinine (mg/dL)Females: 0.85 x above value
Table 1: Recommended Meropenem for Injection Dosage Schedule for Adult Patients with Renal Impairment Creatinine Clearance (mL/min) Dose (dependent on type of infection) Dosing Interval Greater than 50 Recommended dose (500 mg cSSSI and 1 gram Intra-abdominal) Every 8 hours 26 to 50 Recommended dose Every 12 hours 10 to 25 One-half recommended dose Every 12 hours Less than 10 One-half recommended dose Every 24 hours There is inadequate information regarding the use of meropenem for injection in patients on hemodialysis or peritoneal dialysis.
2.3 Use in Pediatric Patients
Pediatric Patients 3 Months of Age and Older
- For pediatric patients 3 months of age and older, the meropenem for injection dose is 10 mg/kg, 20 mg/kg or 40 mg/kg every 8 hours (maximum dose is 2 grams every 8 hours), depending on the type of infection (cSSSI, cIAI, intra-abdominal infection or meningitis). See dosing table 2 below.
- For pediatric patients weighing over 50 kg administer meropenem for injection at a dose of 500 mg every 8 hours for cSSSI, 1 gram every 8 hours for cIAI and 2 grams every 8 hours for meningitis.
- Administer meropenem for injection as an intravenous infusion over approximately 15 minutes to 30 minutes or as an intravenous bolus injection (5 mL to 20 mL) over approximately 3 minutes to 5 minutes.
- There is limited safety data available to support the administration of a 40 mg/kg (up to a maximum of 2 grams) bolus dose.
Table 2: Recommended Meropenem for Injection Dosage Schedule for Pediatric Patients 3 Months of Age and Older with Normal Renal Function There is no experience in pediatric patients with renal impairment.
Type of Infection Dose (mg/kg) Up to a Maximum Dose Dosing Interval Complicated skin and skin structure Infections 10 500 mg Every 8 hours Complicated intra-abdominal Infections 20 1 gram Every 8 hours Meningitis 40 2 grams Every 8 hours When treating cSSSI caused by P. aeruginosa, a dose of 20 mg/kg (or 1 gram for pediatric patients weighing over 50 kg) every 8 hours is recommended.
Pediatric Patients Less Than 3 Months of Age
For pediatric patients (with normal renal function) less than 3 months of age, with complicated intra-abdominal infections, the meropenem for injection dose is based on gestational age (GA) and postnatal age (PNA). See dosing table 3 below. Meropenem for injection should be given as intravenous infusion over 30 minutes.
Table 3: Recommended Meropenem for Injection Dosage Schedule for Pediatric Patients Less than 3 Months of Age with Complicated Intra-Abdominal Infections and Normal Renal Function There is no experience in pediatric patients with renal impairment.
Age Group Dose (mg/kg) Dose Interval Infants less than 32 weeks GA and PNA less than 2 weeks 20 Every 12 hours Infants less than 32 weeks GA and PNA 2 weeks and older 20 Every 8 hours Infants 32 weeks and older GA and PNA less than 2 weeks 20 Every 8 hours Infants 32 weeks and older GA and PNA 2 weeks and older 30 Every 8 hours 2.4 Preparation and Administration of Meropenem for Injection
Important Administration Instructions:
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
For Intravenous Bolus Administration
Re-constitute injection vials (500 mg and 1 gram) with sterile Water for Injection (see table 4 below). Shake to dissolve and let stand until clear.
Table 4: Volume of Sterile Water for Injection for Reconstitution of Injection Vials Vial Size Amount of Diluent
Added (mL)Approximate
Withdrawable Volume (mL)Approximate Average
Concentration
(mg per mL)500 mg 10 10 50 1 gram 20 20 50 For Infusion
- Injection vials (500 mg and 1 gram) may be directly re-constituted with a compatible infusion fluid.
- Alternatively, an injection vial may be re-constituted, then the resulting solution added to an intravenous container and further diluted with an appropriate infusion fluid [see Dosage and Administration (2.5) and (2.6)].
- Do not use flexible container in series connections.
2.5 Compatibility
Compatibility of meropenem for injection with other drugs has not been established. Meropenem for injection should not be mixed with or physically added to solutions containing other drugs.
2.6 Stability and Storage
Freshly prepared solutions of meropenem for injection should be used. However, re-constituted solutions of meropenem for injection maintain satisfactory potency under the conditions described below. Solutions of intravenous meropenem for injection should not be frozen.
Intravenous Bolus Administration
Meropenem for Injection vials re-constituted with sterile Water for Injection for bolus administration (up to 50 mg per mL of meropenem for injection) may be stored for up to 3 hours at up to 25°C (77°F) or for 13 hours at up to 5°C (41°F).
Intravenous Infusion Administration
Solutions prepared for infusion (meropenem for injection concentrations ranging from 1 mg per mL to 20 mg per mL) re-constituted with Sodium Chloride Injection 0.9% may be stored for 1 hour at up to 25°C (77°F) or 15 hours at up to 5°C (41°F).
Solutions prepared for infusion (meropenem for injection concentrations ranging from 1 mg per mL to 20 mg per mL) re-constituted with Dextrose Injection 5% should be used immediately.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving therapy with β-lactams. These reactions are more likely to occur in individuals with a history of sensitivity to multiple allergens.
There have been reports of individuals with a history of penicillin hypersensitivity who have experienced severe hypersensitivity reactions when treated with another β-lactam. Before initiating therapy with meropenem, it is important to inquire about previous hypersensitivity reactions to penicillins, cephalosporins, other β-lactams, and other allergens. If an allergic reaction to meropenem occurs, discontinue the drug immediately.
5.2 Seizure Potential
Seizures and other adverse CNS experiences have been reported during treatment with meropenem. These experiences have occurred most commonly in patients with CNS disorders (e.g., brain lesions or history of seizures) or with bacterial meningitis and/or compromised renal function [see Adverse Reactions (6.1) and Drug Interactions (7.2)].
During clinical investigations, 2904 immunocompetent adult patients were treated for non-CNS infections with the overall seizure rate being 0.7% (based on 20 patients with this adverse event). All meropenem-treated patients with seizures had pre-existing contributing factors. Among these are included prior history of seizures or CNS abnormality and concomitant medications with seizure potential. Dosage adjustment is recommended in patients with advanced age and/or adult patients with creatinine clearance of 50 mL/min or less [see Dosage and Administration (2.2)].
Close adherence to the recommended dosage regimens is urged, especially in patients with known factors that predispose to convulsive activity. Continue anti-convulsant therapy in patients with known seizure disorders. If focal tremors, myoclonus, or seizures occur, evaluate neurologically, placed on anti-convulsant therapy if not already instituted, and re-examine the dosage of meropenem to determine whether it should be decreased or discontinued.
5.3 Risk of Breakthrough Seizures Due to Drug Interaction with Valproic Acid
The concomitant use of meropenem and valproic acid or divalproex sodium is generally not recommended. Case reports in the literature have shown that co-administration of carbapenems, including meropenem, to patients receiving valproic acid or divalproex sodium results in a reduction in valproic acid concentrations. The valproic acid concentrations may drop below the therapeutic range as a result of this interaction, therefore increasing the risk of breakthrough seizures. Increasing the dose of valproic acid or divalproex sodium may not be sufficient to overcome this interaction. Consider administration of antibacterial drugs other than carbapenems to treat infections in patients whose seizures are well controlled on valproic acid or divalproex sodium. If administration of meropenem is necessary, consider supplemental anti-convulsant therapy [see Drug Interactions (7.2)].
5.4 Clostridium difficile–associated Diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including meropenem, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing isolates of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial drug treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.5 Development of Drug-Resistant Bacteria
Prescribing meropenem in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
5.6 Overgrowth of Nonsusceptible Organisms
As with other broad-spectrum antibacterial drugs, prolonged use of meropenem may result in overgrowth of nonsusceptible organisms. Repeated evaluation of the patient is essential. If superinfection does occur during therapy, appropriate measures should be taken.
5.7 Thrombocytopenia
In patients with renal impairment, thrombocytopenia has been observed but no clinical bleeding reported [see Dosage and Administration (2.2), Adverse Reactions (6.1), Use in Specific Populations (8.5) and (8.6), and Clinical Pharmacology (12.3)].
5.8 Potential for Neuromotor Impairment
Alert patients receiving meropenem on an outpatient basis regarding adverse events such as seizures, delirium, headaches and/or paresthesias that could interfere with mental alertness and/or cause motor impairment. Until it is reasonably well established that meropenem is well tolerated, advise patients not to operate machinery or motorized vehicles [see Adverse Reactions (6.1)].
-
6 ADVERSE REACTIONS
The following are discussed in greater detail in other sections of labeling:
- Hypersensitivity Reactions [see Warnings and Precautions (5.1)]
- Seizure Potential [see Warnings and Precautions (5.2)]
- Risk of Breakthrough Seizures Due to Drug Interaction with Valproic Acid [see Warnings and Precautions (5.3)]
- Clostridium difficile – associated Diarrhea [see Warnings and Precautions (5.4)]
- Development of Drug-Resistant Bacteria [see Warnings and Precautions (5.5)]
- Overgrowth of Nonsusceptible Organisms [see Warnings and Precautions (5.6)]
- Thrombocytopenia [see Warnings and Precautions (5.7)]
- Potential for Neuromotor Impairment [see Warnings and Precautions (5.8)]
6.1 Adverse Reactions from Clinical Trials
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Patients:
During clinical investigations, 2904 immunocompetent adult patients were treated for non-CNS infections with meropenem (500 mg or 1 gram every 8 hours). Deaths in 5 patients were assessed as possibly related to meropenem; 36 (1.2%) patients had meropenem discontinued because of adverse events. Many patients in these trials were severely ill and had multiple background diseases, physiological impairments and were receiving multiple other drug therapies. In the seriously ill patient population, it was not possible to determine the relationship between observed adverse events and therapy with meropenem.
The following adverse reaction frequencies were derived from the clinical trials in the 2904 patients treated with meropenem.
Local Adverse Reactions
Local adverse events that were reported with meropenem were as follows:
Inflammation at the injection site 2.4% Injection site reaction 0.9% Phlebitis/thrombophlebitis 0.8% Pain at the injection site 0.4% Edema at the injection site 0.2% Systemic Adverse Reactions
Systemic adverse events that were reported with meropenem occurring in greater than 1% of the patients were diarrhea (4.8%), nausea/vomiting (3.6%), headache (2.3%), rash (1.9%), sepsis (1.6%), constipation (1.4%), apnea (1.3%), shock (1.2%), and pruritus (1.2%).
Additional systemic adverse events that were reported with meropenem and occurring in less than or equal to 1% but greater than 0.1% of the patients are listed below within each body system in order of decreasing frequency:
Bleeding events were seen as follows: gastrointestinal hemorrhage (0.5%), melena (0.3%), epistaxis (0.2%), hemoperitoneum (0.2%).
Body as a Whole: pain, abdominal pain, chest pain, fever, back pain, abdominal enlargement, chills, pelvic pain
Cardiovascular: heart failure, heart arrest, tachycardia, hypertension, myocardial infarction, pulmonary embolus, bradycardia, hypotension, syncope
Digestive System: oral moniliasis, anorexia, cholestatic jaundice/jaundice, flatulence, ileus, hepatic failure, dyspepsia, intestinal obstruction
Hemic/Lymphatic: anemia, hypochromic anemia, hypervolemia
Metabolic/Nutritional: peripheral edema, hypoxia
Nervous System: insomnia, agitation, delirium, confusion, dizziness, seizure, nervousness, paresthesia, hallucinations, somnolence, anxiety, depression, asthenia [see Warnings and Precautions (5.2) and (5.8)]
Respiratory: respiratory disorder, dyspnea, pleural effusion, asthma, cough increased, lung edema
Skin and Appendages: urticaria, sweating, skin ulcer
Urogenital System: dysuria, kidney failure, vaginal moniliasis, urinary incontinence
Adverse Laboratory Changes
Adverse laboratory changes that were reported and occurring in greater than 0.2% of the patients were as follows:
Hepatic: increased alanine transaminase (ALT), aspartate transaminase (AST), alkaline phosphatase, lactate dehydrogenase (LDH), and bilirubin
Hematologic: increased platelets, increased eosinophils, decreased platelets, decreased hemoglobin, decreased hematocrit, decreased white blood cell (WBC), shortened prothrombin time and shortened partial thromboplastin time, leukocytosis, hypokalemia
Renal: increased creatinine and increased blood urea nitrogen (BUN)
Urinalysis: presence of red blood cells
Complicated Skin and Skin Structure Infections
In a study of complicated skin and skin structure infections, the adverse reactions were similar to those listed above. The most common adverse events occurring in greater than 5% of the patients were: headache (7.8%), nausea (7.8%), constipation (7%), diarrhea (7%), anemia (5.5%), and pain (5.1%). Adverse events with an incidence of greater than 1%, and not listed above, include: pharyngitis, accidental injury, gastrointestinal disorder, hypoglycemia, peripheral vascular disorder, and pneumoniae.
Patients with Renal Impairment:
For patients with varying degrees of renal impairment, the incidence of heart failure, kidney failure, seizure and shock reported with meropenem, increased in patients with moderately severe renal impairment (creatinine clearance 10 to 26 mL/min) [see Dosage and Administration (2.2), Warnings and Precautions (5.8), Use in Specific Populations (8.5) and (8.6) and Clinical Pharmacology (12.3)].
Pediatric Patients:
Systemic and Local Adverse Reactions
Pediatric Patients with Serious Bacterial Infections (excluding Bacterial Meningitis):
Meropenem was studied in 515 pediatric patients (3 months to less than 13 years of age) with serious bacterial infections (excluding meningitis, see next section) at dosages of 10 mg/kg to 20 mg/kg every 8 hours. The types of systemic and local adverse events seen in these patients are similar to the adults, with the most common adverse events reported as possibly, probably, or definitely related to meropenem and their rates of occurrence as follows:
Diarrhea 3.5% Rash 1.6% Nausea and Vomiting 0.8% Pediatric Patients with Bacterial Meningitis:
Meropenem was studied in 321 pediatric patients (3 months to less than
17 years of age) with meningitis at a dosage of 40 mg/kg every 8 hours. The types of systemic and local adverse events seen in these patients are similar to the adults, with the most common adverse reactions reported as possibly, probably, or definitely related to meropenem and their rates of occurrence as follows:Diarrhea 4.7% Rash (mostly diaper area moniliasis) 3.1% Oral Moniliasis 1.9% Glossitis 1% In the meningitis studies, the rates of seizure activity during therapy were comparable between patients with no CNS abnormalities who received meropenem and those who received comparator agents (either cefotaxime or ceftriaxone). In the meropenem treated group, 12/15 patients with seizures had late onset seizures (defined as occurring on day 3 or later) versus 7/20 in the comparator arm. The meropenem group had a statistically higher number of patients with transient elevation of liver enzymes.
Pediatric Patients (Neonates and Infants less than 3 months of Age):
Meropenem was studied in 200 neonates and infants less than 3 months of age. The study was open-label, uncontrolled, 98% of the infants received concomitant medications, and the majority of adverse events were reported in neonates less than 32 weeks gestational age and critically ill at baseline, making it difficult to assess the relationship of the adverse events to meropenem.
The adverse reactions seen in these patients that were reported and their rates of occurrence are as follows:
Convulsion 5% Hyperbilirubinemia (conjugated) 4.5% Vomiting 2.5% 6.2 Post-marketing Experience
The following adverse reactions have been identified during post-approval use of meropenem. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Worldwide post-marketing adverse reactions not otherwise listed in the Adverse Reactions from Clinical Trials section of this prescribing information and reported as possibly, probably, or definitely drug related are listed within each body system in order of decreasing severity.
Blood and Lymphatic System Disorders: agranulocytosis, neutropenia, and leukopenia; a positive direct or indirect Coombs test, and hemolytic anemia.
Immune System Disorders: angioedema and drug rash with eosinophilia and systemic symptoms (DRESS syndrome).
Skin and Subcutaneous Disorders: toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme.
-
7 DRUG INTERACTIONS
7.1 Probenecid
Probenecid competes with meropenem for active tubular secretion, resulting in increased plasma concentrations of meropenem. Co-administration of probenecid with meropenem is not recommended.
7.2 Valproic Acid
Case reports in the literature have shown that co-administration of carbapenems, including meropenem, to patients receiving valproic acid or divalproex sodium results in a reduction in valproic acid concentrations. The valproic acid concentrations may drop below the therapeutic range as a result of this interaction, therefore increasing the risk of breakthrough seizures. Although the mechanism of this interaction is unknown, data from in vitro and animal studies suggest that carbapenems may inhibit the hydrolysis of valproic acid's glucuronide metabolite (VPA-g) back to valproic acid, thus decreasing the serum concentrations of valproic acid. If administration of Meropenem for Injection is necessary, then supplemental anti-convulsant therapy should be considered [see Warnings and Precautions (5.3)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B.
There are no adequate and well-controlled studies with meropenem in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Reproductive studies have been performed with meropenem in rats at doses of up to 1000 mg/kg/day, and cynomolgus monkeys at doses of up to 360 mg/kg/day (on the basis of AUC comparisons, approximately 1.8 times and 3.7 times higher, respectively, than human exposure at the usual dose of 1 gram every 8 hours). These studies revealed no evidence of impaired fertility or harm to the fetus due to meropenem, although there were slight changes in fetal body weight at doses of 250 mg/kg/day (on the basis of AUC comparisons, 0.4 times the human exposure at a dose of 1 gram every 8 hours) and above in rats.
8.3 Nursing Mothers
Meropenem has been reported to be excreted in human milk. Caution should be exercised when meropenem is administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of meropenem have been established for pediatric patients 3 months of age and older with complicated skin and skin structure infections and bacterial meningitis, and for pediatric patients of all ages with complicated intra-abdominal infections.
Skin and Skin Structure Infections
Use of meropenem in pediatric patients 3 months of age and older with complicated skin and skin structure infections is supported by evidence from an adequate and well-controlled study in adults and additional data from pediatric pharmacokinetics studies [see Indications and Usage (1.3), Dosage and Administration (2.3), Adverse Reactions (6.1), Clinical Pharmacology (12.3) and Clinical Studies (14.1)].
Intra-abdominal Infections
Use of meropenem in pediatric patients 3 months of age and older with intra-abdominal infections is supported by evidence from adequate and well-controlled studies in adults with additional data from pediatric pharmacokinetics studies and controlled clinical trials in pediatric patients. Use of meropenem in pediatric patients less than 3 months of age with intra-abdominal infections is supported by evidence from adequate and well-controlled studies in adults with additional data from a pediatric pharmacokinetic and safety study [see Indications and Usage (1.2), Dosage and Administration (2.3), Adverse Reactions (6.1), Clinical Pharmacology (12.3) and Clinical Studies (14.2)].
Bacterial Meningitis
Use of meropenem in pediatric patients 3 months of age and older with bacterial meningitis is supported by evidence from adequate and well-controlled studies in the pediatric population [see Indications and Usage (1.3), Dosage and Administration (2.3), Adverse Reactions (6.1), Clinical Pharmacology (12.3) and Clinical Studies (14.3)].
8.5 Geriatric Use
Of the total number of subjects in clinical studies of meropenem, approximately 1100 (30%) were 65 years of age and older, while 400 (11%) were 75 years and older. Additionally, in a study of 511 patients with complicated skin and skin structure infections, 93 (18%) were 65 years of age and older, while 38 (7%) were 75 years and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects; spontaneous reports and other reported clinical experience have not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Meropenem is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with renal impairment. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
A pharmacokinetic study with meropenem in elderly patients has shown a reduction in the plasma clearance of meropenem that correlates with age-associated reduction in creatinine clearance [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
In mice and rats, large intravenous doses of meropenem (2200 mg/kg to 4000 mg/kg) have been associated with ataxia, dyspnea, convulsions, and mortalities.
Intentional overdosing of meropenem is unlikely, although accidental overdosing might occur if large doses are given to patients with reduced renal function. The largest dose of meropenem administered in clinical trials has been 2 grams given intravenously every 8 hours. At this dosage, no adverse pharmacological effects or increased safety risks have been observed.
Limited postmarketing experience indicates that if adverse events occur following overdosage, they are consistent with the adverse event profile described in the Adverse Reactions section and are generally mild in severity and resolve on withdrawal or dose reduction. Consider symptomatic treatments. In individuals with normal renal function, rapid renal elimination takes place. Meropenem and its metabolite are readily dialyzable and effectively removed by hemodialysis; however, no information is available on the use of hemodialysis to treat overdosage.
-
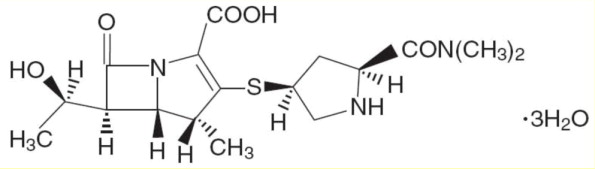
11 DESCRIPTION
Meropenem for Injection, USP is a sterile, pyrogen-free, synthetic, carbapenem antibacterial for intravenous administration. It is (4R,5S,6S)-3-[[(3S,5S)-5-(Dimethylcarbamoyl)-3-pyrrolidinyl]thio]-6-[(1R)-1-hydroxyethyl]-4-methyl-7-oxo-1-azabicyclo[3.2.0]hept-2-ene-2-carboxylic acid trihydrate. Its molecular formula is C17H25N3O5S3H2O with a molecular weight of 437.52. Its structural formula is:
Meropenem for Injection, USP is a white to light yellowish crystalline powder. The solution varies from colorless to yellow depending on the concentration. The pH of freshly constituted solutions is between 7.3 and 8.3. Meropenem is soluble in 5% monobasic potassium phosphate solution, sparingly soluble in water, very slightly soluble in hydrated ethanol, and practically insoluble in acetone or ether.
When re-constituted as instructed, each 1 gram Meropenem for Injection, USP vial will deliver 1 gram of meropenem and 90.2 mg of sodium as sodium carbonate (3.92 mEq). Each 500 mg Meropenem for Injection, USP vial will deliver 500 mg meropenem and 45.1 mg of sodium as sodium carbonate (1.96 mEq) [see Dosage and Administration (2.4)].
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Plasma Concentrations
At the end of a 30 minute intravenous infusion of a single dose of meropenem in healthy volunteers, mean peak plasma concentrations of meropenem are approximately 23 mcg/mL (range 14 to 26) for the 500 mg dose and 49 mcg/mL (range 39 to 58) for the 1 gram dose. A 5 minute intravenous bolus injection of meropenem in healthy volunteers results in mean peak plasma concentrations of approximately 45 mcg/mL (range 18 to 65) for the 500 mg dose and 112 mcg/mL (range 83 to 140) for the 1 gram dose.
Following intravenous doses of 500 mg, mean plasma concentrations of meropenem usually decline to approximately 1 mcg/mL at 6 hours after administration.
No accumulation of meropenem in plasma was observed with regimens using 500 mg administered every 8 hours or 1 gram administered every 6 hours in healthy volunteers with normal renal function.
Distribution
The plasma protein binding of meropenem is approximately 2%.
After a single intravenous dose of meropenem, the highest mean concentrations of meropenem were found in tissues and fluids at 1 hour (0.5 hours to 1.5 hours) after the start of infusion, except where indicated in the tissues and fluids listed in table 5 below.
Table 5: Meropenem Concentrations in Selected Tissues (Highest Concentrations Reported) Tissue Intravenous Dose (gram) Number of Samples Mean [mcg/mL
or mcg/(gram)]1Range [mcg/mL
or mcg/(gram)]1. at 1 hour unless otherwise noted
2. obtained from blister fluid
3. in pediatric patients of age 5 months to 8 years
4. in pediatric patients of age 1 month to 15 years
Endometrium 0.5 7 4.2 1.7 to 10.2 Myometrium 0.5 15 3.8 0.4 to 8.1 Ovary 0.5 8 2.8 0.8 to 4.8 Cervix 0.5 2 7 5.4 to 8.5 Fallopian tube 0.5 9 1.7 0.3 to 3.4 Skin 0.5 22 3.3 0.5 to 12.6 Interstitial fluid2 0.5 9 5.5 3.2 to 8.6 Skin 1 10 5.3 1.3 to 16.7 Interstitial fluid2 1 5 26.3 20.9 to 37.4 Colon 1 2 2.6 2.5 to 2.7 Bile 1 7 14.6 (3 hours) 4 to 25.7 Gall bladder 1 1 — 3.9 Peritoneal fluid 1 9 30.2 7.4 to 54.6 Lung 1 2 4.8 (2 hours) 1.4 to 8.2 Bronchial mucosa 1 7 4.5 1.3 to 11.1 Muscle 1 2 6.1 (2 hours) 5.3 to 6.9 Fascia 1 9 8.8 1.5 to 20 Heart valves 1 7 9.7 6.4 to 12.1 Myocardium 1 10 15.5 5.2 to 25.5 CSF (inflamed) 20 mg/kg3
40 mg/kg48
51.1 (2 hours)
3.3 (3 hours)0.2 to 2.8
0.9 to 6.5CSF (uninflamed) 1 4 0.2 (2 hours) 0.1 to 0.3 Excretion
In subjects with normal renal function, the elimination half-life of meropenem is approximately 1 hour.
Meropenem is primarily excreted unchanged by the kidneys. Approximately 70% (50% to 75%) of the dose is excreted unchanged within 12 hours. A further 28% is recovered as the microbiologically inactive metabolite. Fecal elimination represents only approximately 2% of the dose. The measured renal clearance and the effect of probenecid show that meropenem undergoes both filtration and tubular secretion.
Urinary concentrations of meropenem in excess of 10 mcg/mL are maintained for up to 5 hours after a 500 mg dose.
Specific Populations
Renal Impairment
Pharmacokinetic studies with meropenem in patients with renal impairment have shown that the plasma clearance of meropenem correlates with creatinine clearance. Dosage adjustments are necessary in subjects with renal impairment (creatinine clearance
50 mL/min or less) [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].Meropenem is hemodialyzable. However, there is no information on the usefulness of hemodialysis to treat overdosage [see Overdosage (10)].
Hepatic Impairment
A pharmacokinetic study with meropenem in patients with hepatic impairment has shown no effects of liver disease on the pharmacokinetics of meropenem.
Geriatric Patients
A pharmacokinetic study with meropenem in elderly patients with renal impairment showed a reduction in plasma clearance of meropenem that correlates with age-associated reduction in creatinine clearance.
Pediatric Patients
The pharmacokinetics of meropenem, in pediatric patients 2 years of age or older, are similar to those in adults. The elimination half-life for meropenem was approximately 1.5 hours in pediatric patients of age 3 months to 2 years.
The pharmacokinetics of meropenem in patients less than 3 months of age receiving combination antibacterial drug therapy are given below.
Table 6: Meropenem Pharmacokinetic Parameters in Patients Less Than 3 Months of Age* *Values are derived from a population pharmacokinetic analysis of sparse data
GA less than 32 weeks PNA less than 2 weeks (20 mg/kg
every 12 hours)GA less than 32 weeks PNA 2 weeks or older (20 mg/kg every 8 hours) GA 32 weeks or older PNA less than 2 weeks (20 mg/kg every 8 hours) GA 32 weeks or older PNA 2 weeks or older (30 mg/kg every 8 hours) Overall
CL (L/h/kg) 0.089 0.122 0.135 0.202 0.119 V (L/kg) 0.489 0.467 0.463 0.451 0.468 AUC0-24 (mcg-h/mL) 448 491 445 444 467 Cmax (mcg/mL) 44.3 46.5 44.9 61 46.9 Cmin (mcg/mL) 5.36 6.65 4.84 2.1 5.65 T1/2 (h) 3.82 2.68 2.33 1.58 2.68 Drug Interactions
Probenecid competes with meropenem for active tubular secretion and thus inhibits the renal excretion of meropenem. Following administration of probenecid with meropenem, the mean systemic exposure increased 56% and the mean elimination half-life increased 38%. Co-administration of probenecid with meropenem is not recommended.
12.4 Microbiology
Mechanism of Action
The bactericidal activity of meropenem results from the inhibition of cell wall synthesis. Meropenem penetrates the cell wall of most gram-positive and gram-negative bacteria to reach penicillin-binding-protein (PBP) targets. Meropenem binds to PBPs 2, 3 and 4 of Escherichia coli and Pseudomonas aeruginosa; and PBPs 1, 2 and 4 of Staphylococcus aureus. Bactericidal concentrations (defined as a 3 log10 reduction in cell counts within 12 hours to 24 hours) are typically 1 to 2 times the bacteriostatic concentrations of meropenem, with the exception of Listeria monocytogenes, against which lethal activity is not observed.
Meropenem has significant stability to hydrolysis by β-lactamases, both penicillinases and cephalosporinases produced by gram-positive and gram-negative bacteria.
Meropenem does not have in vitro activity against methicillin-resistant Staphylococcus aureus (MRSA) or methicillin-resistant Staphylococcus epidermidis (MRSE).
Resistance
There are several mechanisms of resistance to carbapenems: 1) decreased permeability of the outer membrane of gram-negative bacteria (due to diminished production of porins) causing reduced bacterial uptake, 2) reduced affinity of the target PBPs, 3) increased expression of efflux pump components, and 4) production of antibacterial drug-destroying enzymes (carbapenemases, metallo-β-lactamases).
Cross-Resistance
Cross-resistance is sometimes observed with isolates resistant to other carbapenems.
Interactions with Other Antibacterial Drugs
In vitro tests show meropenem to act synergistically with aminoglycoside antibacterials against some isolates of Pseudomonas aeruginosa.
Antimicrobial Activity
Meropenem has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections [see Indications and Usage (1)].
Gram-positive bacteria
Enterococcus faecalis (vancomycin-susceptible isolates only)
Staphylococcus aureus (methicillin-susceptible isolates only)
Streptococcus agalactiae
Streptococcus pneumoniae (penicillin-susceptible isolates only)
Streptococcus pyogenes
Viridans group streptococci
Gram-negative bacteria
Escherichia coli
Haemophilus influenzae
Klebsiella pneumoniae
Neisseria meningitidis
Proteus mirabilis
Pseudomonas aeruginosa
Anaerobic bacteria
Bacteroides fragilis
Bacteroides thetaiotaomicron
Peptostreptococcus species
Greater than 90% of the following microorganisms exhibit activity in vitro with a minimum inhibitory concentration (MIC) less than or equal to the meropenem-susceptible breakpoint for organisms of similar genus shown in Table 7. The safety and effectiveness of meropenem in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Gram-positive bacteria
Staphylococcus epidermidis (methicillin-susceptible isolates only)
Gram-negative bacteria
Aeromonas hydrophila
Campylobacter jejuni
Citrobacter freundii
Citrobacter koseri
Enterobacter cloacae
Hafnia alvei
Klebsiella oxytoca
Moraxella catarrhalis
Morganella morganii
Pasteurella multocida
Proteus vulgaris
Serratia marcescens
Anaerobic bacteria
Bacteroides ovatus
Bacteroides uniformis
Bacteroides ureolyticus
Bacteroides vulgatus
Clostridium difficile
Clostridium perfringens
Eggerthella lenta
Fusobacterium species
Parabacteroides distasonis
Porphyromonas asaccharolytica
Prevotella bivia
Prevotella intermedia
Prevotella melaninogenica
Propionibacterium acnes
Susceptibility Test Methods
When available, the clinical microbiology laboratory should provide in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting an antimicrobial drug product for treatment.
Dilution Techniques:
Quantitative methods are used to determine antimicrobial MICs. These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized test method (broth or agar)1,3. The MIC values should be interpreted according to the criteria provided in Table 7.
Diffusion Techniques:
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. The zone size provides an estimate of the susceptibility of bacteria to antimicrobial compounds. The zone size should be determined using a standardized test method2,3 and requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 10 mcg of meropenem to test the susceptibility of microorganisms to meropenem. The disk diffusion interpretive criteria are provided in Table 7.
Anaerobic Techniques:
For anaerobic bacteria, the susceptibility to meropenem as MICs can be determined by a standardized test method.2,4 The MIC values obtained should be interpreted according to the criteria provided in Table 7.
Table 7: Susceptibility Interpretive Criteria for Meropenem S = Susceptible, I = Intermediate, R = Resistant
No interpretative criteria have been established for testing enterococci.
Susceptibility of staphylococci to meropenem may be deduced from testing either cefoxitin or oxacillin.
1. The interpretive criteria for P. aeruginosa are based upon the dosing of 1 gram every 8 hours.
2. The current absence of data on resistant isolates precludes defining any category other than “Susceptible”. If isolates yield MIC results other than susceptible, they should be submitted to a reference laboratory for additional testing.
3. For nonmeningitis isolates of S. pneumoniae a penicillin MIC of ≤ 0.06 mcg/mL or oxacillin zone ≥ 20 mm can predict susceptibility to meropenem. MIC testing should be performed on isolates that do not test as susceptible by either of these methods, and on all meningitis S. pneumoniae isolates.
4. Reliable disk diffusion tests for meropenem do not yet exist for testing streptococci.
5. MIC values using either Brucella blood or Wilkins Chalgren agar (former reference medium) are considered equivalent, Broth microdilution is only recommended for testing the B. fragilis group. MIC values for agar or broth microdilution are considered equivalent for that group.
Minimum Inhibitory
Concentrations (mcg/mL)Disk Diffusion
(zone diameters in mm)Pathogen S I R S I R Enterobacteriaceae ≤ 1 2 ≥ 4 ≥ 23 20 to 22 ≤ 19 Pseudomonas aeruginosa1 ≤ 2 4 ≥ 8 ≥ 19 16 to 18 ≤ 15 Haemophilus influenzae2 ≤ 0.5 — — ≥ 20 — — Neisseria meningitidis2 ≤ 0.25 — — ≥ 30 — — Streptococcus pneumoniae 3,4,5 ≤ 0.25 0.5 ≥ 1 — — — Streptococcus agalactiae and Streptococcus pyogenes 2,4,5 ≤ 0.5 — — — — — Viridians group streptococci ≤ 0.5 — — — — — Anaerobes 5 ≤ 4 8 ≥ 16 — — — A report of Susceptible indicates that the antimicrobial is likely to inhibit growth of the pathogen if the antimicrobial drug reaches the concentration usually achievable at the site of infection. A report of Intermediate indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of Resistant indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the antimicrobial drug reaches concentrations usually achievable at the infection site; other therapy should be selected.
Quality Control
Standardized susceptibility test procedures require the use of quality controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay, and the techniques of the individuals performing the test. Standard meropenem powder should provide the following range of values provided in Table 8.
Table 8: Acceptable Quality Control Ranges for Meropenem 1. Using the Reference Agar Dilution procedure.
Quality Control Strain Minimum Inhibitory Concentrations (MICs = mcg/mL) Disk Diffusion (Zone diameters in mm) Staphylococcus aureus
ATCC 292130.03 to 0.12 — Staphylococcus aureus
ATCC 25923— 29 to 37 Streptococcus pneumoniae
ATCC 496190.03 to 0.25 28 to 35 Enterococcus faecalis
ATCC 292122 to 8 Escherichia coli
ATCC 259220.008 to 0.06 28 to 34 Haemophilus influenzae
ATCC 497660.03 to 0.12 Haemophilus influenzae
ATCC 49247— 20 to 28 Pseudomonas aeruginosa
ATCC 278530.25 to 1 27 to 33 Bacteroides fragilis1
ATCC 252850.03 to 0.25 Bacteroides thetaiotaomicron1
ATCC 297410.125 to 0.5 Eggerthella lenta1
ATCC 430550.125 to 1 Clostridium difficile1
ATCC 7000570.5 to 4 -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenesis:
Genetic toxicity studies were performed with meropenem using the bacterial reverse mutation test, the Chinese hamster ovary HGPRT assay, cultured human lymphocytes cytogenic assay, and the mouse micronucleus test. There was no evidence of mutagenic potential found in any of these tests.
Impairment of Fertility:
Reproductive studies were performed with meropenem in rats at doses up to 1000 mg/kg/day, and cynomolgus monkeys at doses up to 360 mg/kg/day (on the basis of AUC comparisons, approximately 1.8 times and 3.7 times, respectively, to the human exposure at the usual dose of 1 gram every 8 hours). There was no reproductive toxicity seen.
-
14 CLINICAL STUDIES
14.1 Complicated Skin and Skin Structure Infections
Adult patients with complicated skin and skin structure infections including complicated cellulitis, complex abscesses, perirectal abscesses, and skin infections requiring intravenous antimicrobials, hospitalization, and surgical intervention were enrolled in a randomized, multi-center, international, double-blind trial. The study evaluated meropenem at doses of 500 mg administered intravenously every 8 hours and imipenem-cilastatin at doses of 500 mg administered intravenously every 8 hours. The study compared the clinical response between treatment groups in the clinically evaluable population at the follow-up visit (test-of-cure). The trial was conducted in the United States, South Africa, Canada, and Brazil. At enrollment, approximately 37% of the patients had underlying diabetes, 12% had underlying peripheral vascular disease and 67% had a surgical intervention. The study included 510 patients randomized to meropenem and 527 patients randomized to imipenem-cilastatin. Two hundred and sixty one (261) patients randomized to meropenem and 287 patients randomized to imipenem-cilastatin were clinically evaluable. The success rates in the clinically evaluable patients at the follow-up visit were 86% (225/261) in the meropenem arm and 83% (238/287) in imipenem-cilastatin arm.
The success rates for the clinically evaluable population are provided in Table 9.
Table 9: Success Rates at Test-of-Cure Visit for Clinically Evaluable Population with Complicated Skin and Skin Structure Infections 1. n=number of patients with satisfactory response.
2. N=number of patients in the clinically evaluable population or respective subgroup within treatment groups.
Population Meropenem for Injection
n1/N2 (%)Imipenem-cilastatin
n1/N2 (%)Total 225/261 (86) 238/287 (83) Diabetes mellitus 83/97 (86) 76/105 (72) No diabetes mellitus 142/164 (87) 162/182 (89) Less than 65 years of age 190/218 (87) 205/241 (85) 65 years of age or older 35/43 (81) 33/46 (72) Men 130/148 (88) 137/172 (80) Women 95/113 (84) 101/115 (88) The clinical efficacy rates by pathogen are provided in Table 10. The values represent the number of patients clinically cured/number of clinically evaluable patients at the post-treatment follow-up visit, with the percent cure in parentheses (Fully Evaluable analysis set).
Table 10: Clinical Efficacy Rates by Pathogen for Clinically Evaluable Population 1. Patients may have more than one pretreatment pathogen.
2. n=number of patients with satisfactory response.
3. N=number of patients in the clinically evaluable population or subgroup within treatment groups.
4. %= Percent of satisfactory clinical response at follow-up evaluation.
MICROORGANISMS1 Meropenem for Injection
n2/N3 (%)4Imipenem-cilastatin
n2/N3 (%)4Gram-positive aerobes Staphylococcus aureus, methicillin susceptible 82/88 (93) 84/100 (84) Streptococcus pyogenes (Group A) 26/29 (90) 28/32 (88) Streptococcus agalactiae (Group B) 12/17 (71) 16/19 (84) Enterococcus faecalis 9/12 (75) 14/20 (70) Viridans group streptococci 11/12 (92) 5/6 (83) Gram-negative aerobes Escherichia coli 12/15 (80) 15/21 (71) Pseudomonas aeruginosa 11/15 (73) 13/15 (87) Proteus mirabilis 11/13 (85) 6/7 (86) Anaerobes Bacteroides fragilis 10/11 (91) 9/10 (90) Peptostreptococcus species 10/13 (77) 14/16 (88) The proportion of patients who discontinued study treatment due to an adverse event was similar for both treatment groups (meropenem, 2.5% and imipenem-cilastatin, 2.7%).
14.2 Complicated Intra-Abdominal Infections
One controlled clinical study of complicated intra-abdominal infection was performed in the United States where meropenem was compared with clindamycin/tobramycin. Three controlled clinical studies of complicated intra-abdominal infections were performed in Europe; meropenem was compared with imipenem (two trials) and cefotaxime/metronidazole (one trial).
Using strict evaluability criteria and microbiologic eradication and clinical cures at follow-up which occurred 7 or more days after completion of therapy, the presumptive microbiologic eradication/clinical cure rates and statistical findings are provided in Table 11:
Table 11: Presumptive Microbiologic Eradication and Clinical Cure Rates at Test-of-Cure Visit in the Evaluable Population with Complicated Intra-Abdominal Infection Treatment Arm No. evaluable/
No. enrolled (%)Microbiologic
Eradication RateClinical Cure
RateOutcome meropenem 146/516 (28%) 98/146 (67%) 101/146 (69%) imipenem 65/220 (30%) 40/65 (62%) 42/65 (65%) meropenem equivalent to control cefotaxime/
metronidazole26/85 (30%) 22/26 (85%) 22/26 (85%) meropenem not
equivalent to controlclindamycin/
tobramycin50/212 (24%) 38/50 (76%) 38/50 (76%) meropenem equivalent to control The finding that meropenem was not statistically equivalent to cefotaxime/metronidazole may have been due to uneven assignment of more seriously ill patients to the meropenem arm. Currently there is no additional information available to further interpret this observation.
14.3 Bacterial Meningitis
Four hundred forty-six patients (397 pediatric patients 3 months to less than 17 years of age) were enrolled in 4 separate clinical trials and randomized to treatment with meropenem (n=225) at a dose of 40 mg/kg every 8 hours or a comparator drug, i.e., cefotaxime (n=187) or ceftriaxone (n=34), at the approved dosing regimens. A comparable number of patients were found to be clinically evaluable (ranging from 61 to 68%) and with a similar distribution of pathogens isolated on initial CSF culture.
Patients were defined as clinically not cured if any one of the following three criteria were met:
- At the 5 to 7 week post-completion of therapy visit, the patient had any one of the following: moderate to severe motor, behavior or development deficits, hearing loss of greater than 60 decibels in one or both ears, or blindness.
- During therapy the patient's clinical status necessitated the addition of other antibacterial drugs.
- Either during or post-therapy, the patient developed a large subdural effusion needing surgical drainage, or a cerebral abscess, or a bacteriologic relapse.
Using the definition, the following efficacy rates were obtained, per organism (noted in Table 12). The values represent the number of patients clinically cured/number of clinically evaluable patients, with the percent cure in parentheses.
Table 12: Efficacy rates by Pathogen in the Clinically Evaluable Population with Bacterial Meningitis 1. (+) β-lactamase-producing
2. (-/NT) non-β-lactamase-producing or not tested
MICROORGANISMS MEROPENEM FOR INJECTION COMPARATOR S. pneumoniae 17/24 (71) 19/30 (63) H. influenzae (+)1 8/10 (80) 6/6 (100) H. influenzae (-/NT)2 44/59 (75) 44/60 (73) N. meningitidis 30/35 (86) 35/39 (90) Total (including others) 102/131 (78) 108/140 (77) Sequelae were the most common reason patients were assessed as clinically not cured.
Five patients were found to be bacteriologically not cured, 3 in the comparator group (1 relapse and 2 patients with cerebral abscesses) and 2 in the meropenem group (1 relapse and 1 with continued growth of Pseudomonas aeruginosa).
With respect to hearing loss, 263 of the 271 evaluable patients had at least one hearing test performed post-therapy. The following table shows the degree of hearing loss between the meropenem-treated patients and the comparator-treated patients.
Table 13: Hearing Loss at Post-Therapy in the Evaluable Population Treated with Meropenem Degree of Hearing Loss
(in one or both ears)Meropenem
n = 128Comparator
n = 135No loss 61% 56% 20 to 40 decibels 20% 24% Greater than 40 to 60 decibels 8% 7% Greater than 60 decibels 9% 10% -
15 REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically; Approved Standard – Tenth Edition. CLSI document M07-A10, Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2015.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Disk Diffusion Susceptibility Tests; Approved Standard - Twelfth Edition. CLSI document M02-A12, Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2015.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-sixth Informational Supplement, CLSI document M100-S26, Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2016.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; Approved Standard - Eight Edition. CLSI document M11-A8. Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, PA 19087 USA, 2012.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31-41.
-
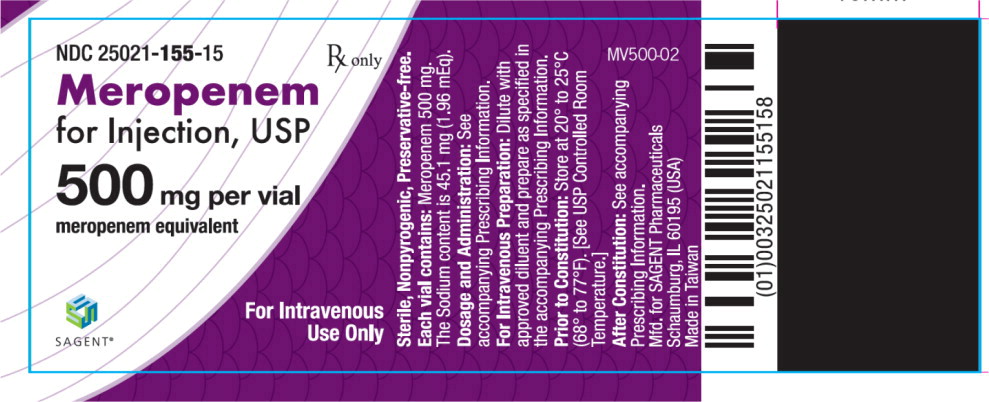
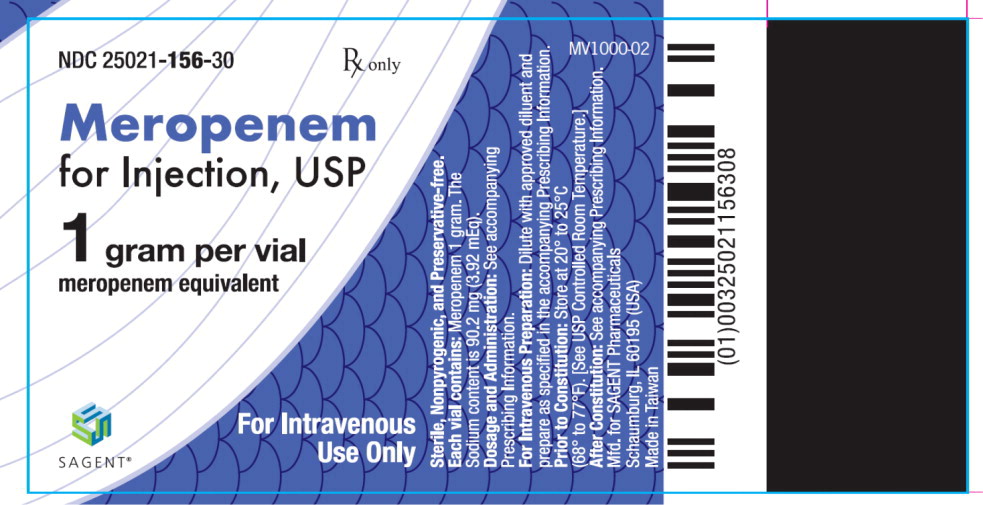
16 HOW SUPPLIED/STORAGE AND HANDLING
Meropenem for Injection, USP is supplied as follows:
NDC Meropenem for Injection Package Factor 25021-155-15 500 mg per vial 10 vials per carton 25021-156-30 1 gram per vial 10 vials per carton Meropenem for Injection, USP is supplied in 20 mL and 30 mL injection vials containing sufficient meropenem to deliver 500 mg or 1 gram for intravenous administration, respectively.
-
17 PATIENT COUNSELING INFORMATION
- Counsel patients that antibacterial drugs including meropenem should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When meropenem is prescribed to treat a bacterial infection, tell patients that although it is common to feel better early in the course of therapy, take the medication exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by meropenem or other antibacterial drugs in the future.
- Counsel patients that diarrhea is a common problem caused by antibacterial drugs which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial drug. If this occurs, patients should contact their physician as soon as possible [see Warnings and Precautions (5.4)].
- Counsel patients to inform their physician if they are taking valproic acid or divalproex sodium. Valproic acid concentrations in the blood may drop below the therapeutic range upon co-administration with meropenem. If treatment with meropenem is necessary and continued, alternative or supplemental anti-convulsant medication to prevent and/or treat seizures may be needed [see Warnings and Precautions (5.3)].
- Patients receiving meropenem on an outpatient basis must be alerted of adverse events such as seizures, delirium, headaches and/or paresthesias that could interfere with mental alertness and/or cause motor impairment. Until it is reasonably well established that meropenem is well tolerated, patients should not operate machinery or motorized vehicles [see Warnings and Precautions (5.8)].
SAGENT®
Mfd. for SAGENT Pharmaceuticals
Schaumburg, IL 60195 (USA)
Made in Taiwan
©2017 Sagent Pharmaceuticals, Inc.May 2017
SAGENT Pharmaceuticals®
- PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
MEROPENEM
meropenem injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-155 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength meropenem (UNII: FV9J3JU8B1) (meropenem anhydrous - UNII:YOP6PX0BAO) meropenem 500 mg Inactive Ingredients Ingredient Name Strength sodium carbonate (UNII: 45P3261C7T) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-155-15 10 in 1 CARTON 01/15/2017 06/30/2020 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA204854 01/15/2017 06/30/2020 MEROPENEM
meropenem injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 25021-156 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength meropenem (UNII: FV9J3JU8B1) (meropenem anhydrous - UNII:YOP6PX0BAO) meropenem 1 g Inactive Ingredients Ingredient Name Strength sodium carbonate (UNII: 45P3261C7T) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 25021-156-30 10 in 1 CARTON 01/15/2017 07/31/2020 1 1 in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA204854 01/15/2017 07/31/2020 Labeler - Sagent Pharmaceuticals (796852890)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.