VENTOLIN HFA- albuterol sulfate aerosol, metered
VENTOLIN by
Drug Labeling and Warnings
VENTOLIN by is a Prescription medication manufactured, distributed, or labeled by Lake Erie Medical DBA Quality Care Products LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use VENTOLIN HFA safely and effectively. See full prescribing information for VENTOLIN HFA.
VENTOLIN HFA (albuterol sulfate) Inhalation Aerosol
FOR ORAL INHALATION
Initial U.S. Approval: 1981INDICATIONS AND USAGE
VENTOLIN HFA is a beta2-adrenergic agonist indicated for:
- Treatment or prevention of bronchospasm in patients aged 4 years and older with reversible obstructive airway disease. (1.1)
- Prevention of exercise-induced bronchospasm in patients aged 4 years and older. (1.2)
DOSAGE AND ADMINISTRATION
- For oral inhalation only. (2)
- Treatment or prevention of bronchospasm in adults and children aged 4 years and older: 2 inhalations every 4 to 6 hours. For some patients, 1 inhalation every 4 hours may be sufficient. (2.1)
- Prevention of exercise-induced bronchospasm in adults and children aged 4 years and older: 2 inhalations 15 to 30 minutes before exercise. (2.2)
- Priming information: Prime VENTOLIN HFA before using for the first time, when the inhaler has not been used for more than 2 weeks, or when the inhaler has been dropped. To prime VENTOLIN HFA, release 4 sprays into the air away from the face, shaking well before each spray. (2.3)
- Cleaning information: At least once a week, wash the actuator with warm water and let it air-dry completely. (2.3)
DOSAGE FORMS AND STRENGTHS
Inhalation Aerosol. Inhaler containing 108 mcg albuterol sulfate (90 mcg albuterol base) as an aerosol formulation for oral inhalation. (3)
CONTRAINDICATIONS
Hypersensitivity to any ingredient. (4)
WARNINGS AND PRECAUTIONS
- Life-threatening paradoxical bronchospasm may occur. Discontinue VENTOLIN HFA immediately and institute alternative therapy. (5.1)
- Need for more doses of VENTOLIN HFA than usual may be a sign of deterioration of asthma and requires reevaluation of treatment. (5.2)
- VENTOLIN HFA is not a substitute for corticosteroids. (5.3)
- Cardiovascular effects may occur. Use with caution in patients sensitive to sympathomimetic drugs and patients with cardiovascular or convulsive disorders. (5.4, 5.7)
- Excessive use may be fatal. Do not exceed recommended dose. (5.5)
- Immediate hypersensitivity reactions may occur. Discontinue VENTOLIN HFA immediately. (5.6)
- Hypokalemia and changes in blood glucose may occur. (5.7, 5.8)
ADVERSE REACTIONS
Most common adverse reactions (incidence greater than or equal to 3%) are throat irritation, viral respiratory infections, upper respiratory inflammation, cough, and musculoskeletal pain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Beta-blockers: Use with caution. May block bronchodilatory effects of beta-agonists and produce severe bronchospasm. (7.1)
- Diuretics: Use with caution. Electrocardiographic changes and/or hypokalemia associated with non–potassium-sparing diuretics may worsen with concomitant beta-agonists. (7.2)
- Digoxin: May decrease serum digoxin levels. Consider monitoring digoxin levels. (7.3)
- Monoamine oxidase inhibitors and tricyclic antidepressants: Use with extreme caution. May potentiate effect of albuterol on vascular system. (7.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
1.1 Bronchospasm
1.2 Exercise-Induced Bronchospasm
2 DOSAGE AND ADMINISTRATION
2.1 Bronchospasm
2.2 Exercise-Induced Bronchospasm
2.3 Administration Information
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Paradoxical Bronchospasm
5.2 Deterioration of Asthma
5.3 Use of Anti-inflammatory Agents
5.4 Cardiovascular Effects
5.5 Do Not Exceed Recommended Dose
5.6 Immediate Hypersensitivity Reactions
5.7 Coexisting Conditions
5.8 Hypokalemia
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Beta-Adrenergic Receptor Blocking Agents
7.2 Non–Potassium-Sparing Diuretics
7.3 Digoxin
7.4 Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.2 Animal Toxicology and/or Pharmacology
14 CLINICAL STUDIES
14.1 Bronchospasm Associated with Asthma
14.2 Exercise-Induced Bronchospasm
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Bronchospasm
For treatment of acute episodes of bronchospasm or prevention of symptoms associated with bronchospasm, the usual dosage for adults and children is 2 inhalations repeated every 4 to 6 hours; in some patients, 1 inhalation every 4 hours may be sufficient. More frequent administration or a greater number of inhalations is not recommended.
2.2 Exercise-Induced Bronchospasm
For prevention of exercise-induced bronchospasm, the usual dosage for adults and children aged 4 years and older is 2 inhalations 15 to 30 minutes before exercise.
2.3 Administration Information
VENTOLIN HFA should be administered by the orally inhaled route only.
Priming: Priming VENTOLIN HFA is essential to ensure appropriate albuterol content in each actuation. Prime VENTOLIN HFA before using for the first time, when the inhaler has not been used for more than 2 weeks, or when the inhaler has been dropped. To prime VENTOLIN HFA, release 4 sprays into the air away from the face, shaking well before each spray.
Cleaning: To ensure proper dosing and to prevent actuator orifice blockage, wash the actuator with warm water and let it air-dry completely at least once a week.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Paradoxical Bronchospasm
VENTOLIN HFA can produce paradoxical bronchospasm, which may be life threatening. If paradoxical bronchospasm occurs following dosing with VENTOLIN HFA, it should be discontinued immediately and alternative therapy should be instituted. It should be recognized that paradoxical bronchospasm, when associated with inhaled formulations, frequently occurs with the first use of a new canister.
5.2 Deterioration of Asthma
Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. If the patient needs more doses of VENTOLIN HFA than usual, this may be a marker of destabilization of asthma and requires reevaluation of the patient and treatment regimen, giving special consideration to the possible need for anti-inflammatory treatment, e.g., corticosteroids.
5.3 Use of Anti-inflammatory Agents
The use of beta-adrenergic agonist bronchodilators alone may not be adequate to control asthma in many patients. Early consideration should be given to adding anti-inflammatory agents, e.g., corticosteroids, to the therapeutic regimen.
5.4 Cardiovascular Effects
VENTOLIN HFA, like all other beta2-adrenergic agonists, can produce clinically significant cardiovascular effects in some patients such as changes in pulse rate or blood pressure. If such effects occur, VENTOLIN HFA may need to be discontinued. In addition, beta-agonists have been reported to produce electrocardiogram (ECG) changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical relevance of these findings is unknown. Therefore, VENTOLIN HFA, like all other sympathomimetic amines, should be used with caution in patients with underlying cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
5.5 Do Not Exceed Recommended Dose
Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs in patients with asthma. The exact cause of death is unknown, but cardiac arrest following an unexpected development of a severe acute asthmatic crisis and subsequent hypoxia is suspected.
5.6 Immediate Hypersensitivity Reactions
Immediate hypersensitivity reactions (e.g., urticaria, angioedema, rash, bronchospasm, hypotension), including anaphylaxis, may occur after administration of VENTOLIN HFA [see Contraindications (4)].
5.7 Coexisting Conditions
VENTOLIN HFA, like other sympathomimetic amines, should be used with caution in patients with convulsive disorders, hyperthyroidism, or diabetes mellitus and in patients who are unusually responsive to sympathomimetic amines. Large doses of intravenous albuterol have been reported to aggravate preexisting diabetes mellitus and ketoacidosis.
5.8 Hypokalemia
Beta-adrenergic agonist medicines may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects [see Clinical Pharmacology (12.1)]. The decrease in serum potassium is usually transient, not requiring supplementation.
-
6 ADVERSE REACTIONS
Use of VENTOLIN HFA may be associated with the following:
- Paradoxical bronchospasm [see Warnings and Precautions (5.1)]
- Cardiovascular effects [see Warnings and Precautions (5.4)]
- Immediate hypersensitivity reactions [see Warnings and Precautions (5.6)]
- Hypokalemia [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data described below reflects exposure to VENTOLIN HFA in 248 subjects treated with VENTOLIN HFA in 3 placebo-controlled clinical trials of 2 to 12 weeks’ duration. The data from adults and adolescents is based upon 2 clinical trials in which 202 subjects with asthma aged 12 years and older were treated with VENTOLIN HFA 2 inhalations 4 times daily for 12 weeks’ duration. The adult/adolescent population was 92 female, 110 male and 163 white, 19 black, 18 Hispanic, 2 other. The data from pediatric subjects are based upon 1 clinical trial in which 46 subjects with asthma aged 4 to 11 years were treated with VENTOLIN HFA 2 inhalations 4 times daily for 2 weeks’ duration. The population was 21 female, 25 male and 25 white, 17 black, 3 Hispanic, 1 other.
Adult and Adolescent Subjects Aged 12 Years and Older: The two 12-week, randomized, double-blind trials in 610 adult and adolescent subjects with asthma that compared VENTOLIN HFA, a CFC 11/12-propelled albuterol inhaler, and an HFA-134a placebo inhaler. Overall, the incidence and nature of the adverse reactions reported for VENTOLIN HFA and a CFC 11/12-propelled albuterol inhaler were comparable. Table 1 lists the incidence of all adverse reactions (whether considered by the investigator to be related or unrelated to drug) from these trials that occurred at a rate of 3% or greater in the group treated with VENTOLIN HFA and more frequently in the group treated with VENTOLIN HFA than in the HFA-134a placebo inhaler group.
Table 1. Adverse Reactions with VENTOLIN HFA with ≥3% Incidence and More Common than Placebo in Adult and Adolescent Subjects Adverse Reaction
Percent of Subjects
VENTOLIN HFA
(n = 202)
%
CFC 11/12-Propelled
Albuterol Inhaler
(n = 207)
%
Placebo HFA-134a
(n = 201)
%
Ear, nose, and throat
- Throat irritation
10
6
7
- Upper respiratory inflammation
5
5
2
Lower respiratory
- Viral respiratory infections
7
4
4
- Cough
5
2
2
Musculoskeletal
- Musculoskeletal pain
5
5
4
Adverse reactions reported by less than 3% of the adult and adolescent subjects receiving VENTOLIN HFA and by a greater proportion of subjects receiving VENTOLIN HFA than receiving HFA-134a placebo inhaler and that have the potential to be related to VENTOLIN HFA include diarrhea, laryngitis, oropharyngeal edema, cough, lung disorders, tachycardia, and extrasystoles. Palpitations and dizziness have also been observed with VENTOLIN HFA.
Pediatric Subjects Aged 4 to 11 Years: Results from the 2-week clinical trial in pediatric subjects with asthma aged 4 to 11 years showed that this pediatric population had an adverse reaction profile similar to that of the adult and adolescent populations.
Three trials have been conducted to evaluate the safety and efficacy of VENTOLIN HFA in subjects between birth and 4 years of age. The results of these trials did not establish the efficacy of VENTOLIN HFA in this age-group [see Use in Specific Populations (8.4)]. Since the efficacy of VENTOLIN HFA has not been demonstrated in children between birth and 48 months of age, the safety of VENTOLIN HFA in this age-group cannot be established. However, the safety profile observed in the pediatric population younger than 4 years was comparable to that observed in the older pediatric subjects and in adults and adolescents. Where adverse reaction incidence rates were greater in subjects younger than 4 years compared with older subjects, the higher incidence rates were noted in all treatment arms, including placebo. These adverse reactions included upper respiratory tract infection, nasopharyngitis, pyrexia, and tachycardia.
6.2 Postmarketing Experience
In addition to adverse reactions reported from clinical trials, the following adverse reactions have been identified during postapproval use of albuterol sulfate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These events have been chosen for inclusion due to either their seriousness, frequency of reporting, or causal connection to albuterol or a combination of these factors.
Cases of paradoxical bronchospasm, hoarseness, arrhythmias (including atrial fibrillation, supraventricular tachycardia), and hypersensitivity reactions (including urticaria, angioedema, rash) have been reported after the use of VENTOLIN HFA.
In addition, albuterol, like other sympathomimetic agents, can cause adverse reactions such as hypokalemia, hypertension, peripheral vasodilatation, angina, tremor, central nervous system stimulation, hyperactivity, sleeplessness, headache, muscle cramps, drying or irritation of the oropharynx, and metabolic acidosis.
-
7 DRUG INTERACTIONS
Other short-acting sympathomimetic aerosol bronchodilators should not be used concomitantly with albuterol. If additional adrenergic drugs are to be administered by any route, they should be used with caution to avoid deleterious cardiovascular effects.
7.1 Beta-Adrenergic Receptor Blocking Agents
Beta-blockers not only block the pulmonary effect of beta-agonists, such as VENTOLIN HFA, but may also produce severe bronchospasm in patients with asthma. Therefore, patients with asthma should not normally be treated with beta-blockers. However, under certain circumstances, there may be no acceptable alternatives to the use of beta-adrenergic blocking agents for these patients; cardioselective beta-blockers could be considered, although they should be administered with caution.
7.2 Non–Potassium-Sparing Diuretics
The ECG changes and/or hypokalemia that may result from the administration of non‑potassium-sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the coadministration of VENTOLIN HFA with non–potassium-sparing diuretics.
7.3 Digoxin
Mean decreases of 16% to 22% in serum digoxin levels were demonstrated after single-dose intravenous and oral administration of albuterol, respectively, to normal volunteers who had received digoxin for 10 days. The clinical relevance of these findings for patients with obstructive airway disease who are receiving inhaled albuterol and digoxin on a chronic basis is unclear. Nevertheless, it would be prudent to carefully evaluate the serum digoxin levels in patients who are currently receiving digoxin and albuterol.
7.4 Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
VENTOLIN HFA should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors or tricyclic antidepressants, or within 2 weeks of discontinuation of such agents, because the action of albuterol on the vascular system may be potentiated.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects: Pregnancy Category C. There are no adequate and well-controlled trials with VENTOLIN HFA or albuterol sulfate in pregnant women. During worldwide marketing experience, various congenital anomalies, including cleft palate and limb defects, have been reported in the offspring of patients being treated with albuterol. Some of the mothers were taking multiple medications during their pregnancies. No consistent pattern of defects can be discerned, and a relationship between albuterol use and congenital anomalies has not been established. Animal reproduction studies in mice and rabbits revealed evidence of teratogenicity. VENTOLIN HFA should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physicians if they become pregnant while taking VENTOLIN HFA.
In a mouse reproduction study, subcutaneously administered albuterol sulfate produced cleft palate formation in 5 of 111 (4.5%) fetuses at exposures less than the maximum recommended human daily inhalation dose (MRHDID) for adults on a mg/m2 basis and in 10 of 108 (9.3%) fetuses at approximately 8 times the MRHDID. Similar effects were not observed at approximately one eleventh of the MRHDID. Cleft palate also occurred in 22 of 72 (30.5%) fetuses from females treated subcutaneously with isoproterenol (positive control).
In a rabbit reproduction study, orally administered albuterol sulfate produced cranioschisis in 7 of 19 fetuses (37%) at approximately 680 times the MRHDID.
In another rabbit study, an albuterol sulfate/HFA-134a formulation administered by inhalation produced enlargement of the frontal portion of the fetal fontanelles at approximately one third of the MRHDID.
Nonteratogenic Effects: A study in which pregnant rats were dosed with radiolabeled albuterol sulfate demonstrated that drug-related material is transferred from the maternal circulation to the fetus.
8.2 Labor and Delivery
There are no well-controlled human trials that have investigated effects of VENTOLIN HFA on preterm labor or labor at term. Because of the potential for beta-agonist interference with uterine contractility, use of VENTOLIN HFA during labor should be restricted to those patients in whom the benefits clearly outweigh the risk.
8.3 Nursing Mothers
Plasma levels of albuterol sulfate and HFA-134a after inhaled therapeutic doses are very low in humans, but it is not known whether the components of VENTOLIN HFA are excreted in human milk. Because of the potential for tumorigenicity shown for albuterol in animal studies and lack of experience with the use of VENTOLIN HFA by nursing mothers, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Caution should be exercised when VENTOLIN HFA is administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of VENTOLIN HFA in children aged 4 years and older have been established based upon two 12-week clinical trials in subjects aged 12 years and older with asthma and one 2-week clinical trial in subjects aged 4 to 11 years with asthma [see Adverse Reactions (6.1), Clinical Studies (14.1)]. The safety and effectiveness of VENTOLIN HFA in children younger than 4 years have not been established. Three trials have been conducted to evaluate the safety and efficacy of VENTOLIN HFA in subjects younger than 4 years and the findings are described below.
Two 4-week randomized, double-blind, placebo-controlled trials were conducted in 163 pediatric subjects aged from birth to 48 months with symptoms of bronchospasm associated with obstructive airway disease (presenting symptoms included: wheeze, cough, dyspnea, or chest tightness). VENTOLIN HFA or placebo HFA was delivered with either an AeroChamber Plus® Valved Holding Chamber or an Optichamber® Valved Holding Chamber with mask 3 times daily. In one trial, VENTOLIN HFA 90 mcg (n = 26), VENTOLIN HFA 180 mcg (n = 25), and placebo HFA (n = 26) were administered to children aged between 24 and 48 months. In the second trial, VENTOLIN HFA 90 mcg (n = 29), VENTOLIN HFA 180 mcg (n = 29), and placebo HFA (n = 28) were administered to children aged between birth and 24 months. Over the 4-week treatment period, there were no treatment differences in asthma symptom scores between the groups receiving VENTOLIN HFA 90 mcg, VENTOLIN HFA 180 mcg, and placebo in either trial.
In a third trial, VENTOLIN HFA was evaluated in 87 pediatric subjects younger than 24 months for the treatment of acute wheezing. VENTOLIN HFA was delivered with an AeroChamber Plus Valved Holding Chamber in this trial. There were no significant differences in asthma symptom scores and mean change from baseline in an asthma symptom score between VENTOLIN HFA 180 mcg and VENTOLIN HFA 360 mcg.
In vitro dose characterization studies were performed to evaluate the delivery of VENTOLIN HFA via holding chambers with attached masks. The studies were conducted with 2 different holding chambers with masks (small and medium size). The in vitro study data when simulating patient breathing suggest that the dose of VENTOLIN HFA presented for inhalation via a valved holding chamber with mask will be comparable to the dose delivered in adults without a spacer and mask per kilogram of body weight (Table 2). However, clinical trials in children younger than 4 years described above suggest that either the optimal dose of VENTOLIN HFA has not been defined in this age-group or VENTOLIN HFA is not effective in this age-group. The safety and effectiveness of VENTOLIN HFA administered with or without a spacer device in children younger than 4 years have not been demonstrated.
Table 2. In Vitro Medication Delivery through AeroChamber Plus® Valved Holding Chamber with a Mask Age
Mask
Flow Rate (L/min)
Holding Time (seconds)
Mean Medication Delivery through AeroChamber Plus (mcg/actuation)
Body Weight 50th Percentile (kg)a
Medication Delivered per Actuation (mcg/kg)b
6 to 12 Months
Small
4.9
0
2
5
10
18.2
19.8
13.8
15.4
7.5-9.9
1.8-2.4
2.0-2.6
1.4-1.8
1.6-2.1
2 to 5 Years
Small
8.0
0
2
5
10
17.8
16.0
16.3
18.3
12.3-18.0
1.0-1.4
0.9-1.3
0.9-1.3
1.0-1.5
2 to 5 Years
Medium
8.0
0
2
5
10
21.1
15.3
18.3
18.2
12.3-18.0
1.2-1.7
0.8-1.2
1.0-1.5
1.0-1.5
>5 Years
Medium
12.0
0
2
5
10
26.8
20.9
19.6
20.3
18.0
1.5
1.2
1.1
1.1
- a Centers for Disease Control growth charts, developed by the National Center for Health Statistics in collaboration with the National Center for Chronic Disease Prevention and Health Promotion (2000). Ranges correspond to the average of the 50 th percentile weight for boys and girls at the ages indicated.
- b A single inhalation of VENTOLIN HFA in a 70-kg adult without use of a valved holding chamber and mask delivers approximately 90 mcg, or 1.3 mcg/kg.
8.5 Geriatric Use
Clinical trials of VENTOLIN HFA did not include sufficient numbers of subjects aged 65 years and older to determine whether older subjects respond differently than younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
-
10 OVERDOSAGE
The expected signs and symptoms with overdosage of albuterol are those of excessive beta-adrenergic stimulation and/or occurrence or exaggeration of any of the signs and symptoms of beta-adrenergic stimulation (e.g., seizures, angina, hypertension or hypotension, tachycardia with rates up to 200 beats/min, arrhythmias, nervousness, headache, tremor, muscle cramps, dry mouth, palpitation, nausea, dizziness, fatigue, malaise, insomnia, hyperglycemia, hypokalemia, metabolic acidosis).
As with all inhaled sympathomimetic medicines, cardiac arrest and even death may be associated with an overdose of VENTOLIN HFA Inhalation Aerosol.
Treatment consists of discontinuation of VENTOLIN HFA together with appropriate symptomatic therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of VENTOLIN HFA.
-
11 DESCRIPTION
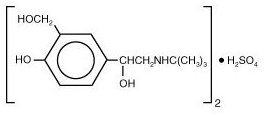
The active component of VENTOLIN HFA is albuterol sulfate, USP, the racemic form of albuterol and a relatively selective beta2-adrenergic bronchodilator. Albuterol sulfate has the chemical name α1-[(tert-butylamino)methyl]-4-hydroxy-m-xylene-α, α′-diol sulfate (2:1)(salt) and the following chemical structure:
Albuterol sulfate is a white crystalline powder with a molecular weight of 576.7, and the empirical formula is (C13H21NO3)2H2SO4. It is soluble in water and slightly soluble in ethanol.
The World Health Organization recommended name for albuterol base is salbutamol.
VENTOLIN HFA is a blue plastic inhaler with a blue strapcap containing a pressurized metered-dose aerosol canister fitted with a counter. Each canister contains a microcrystalline suspension of albuterol sulfate in propellant HFA-134a (1,1,1,2-tetrafluoroethane). It contains no other excipients.
After priming, each actuation of the inhaler delivers 120 mcg of albuterol sulfate, USP in 75 mg of suspension from the valve and 108 mcg of albuterol sulfate, USP from the mouthpiece (equivalent to 90 mcg of albuterol base from the mouthpiece).
Prime VENTOLIN HFA before using for the first time, when the inhaler has not been used for more than 2 weeks, or when the inhaler has been dropped. To prime VENTOLIN HFA, release 4 sprays into the air away from the face, shaking well before each spray.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
In vitro studies and in vivo pharmacologic studies have demonstrated that albuterol has a preferential effect on beta2-adrenergic receptors compared with isoproterenol. Although beta2-adrenoceptors are the predominant adrenergic receptors in bronchial smooth muscle and beta1-adrenoceptors are the predominant receptors in the heart, there are also beta2-adrenoceptors in the human heart comprising 10% to 50% of the total beta-adrenoceptors. The precise function of these receptors has not been established, but their presence raises the possibility that even selective beta2-agonists may have cardiac effects.
Activation of beta2-adrenergic receptors on airway smooth muscle leads to the activation of adenyl cyclase and to an increase in the intracellular concentration of cyclic-3′,5′-adenosine monophosphate (cyclic AMP). This increase of cyclic AMP leads to the activation of protein kinase A, which inhibits the phosphorylation of myosin and lowers intracellular ionic calcium concentrations, resulting in relaxation. Albuterol relaxes the smooth muscles of all airways, from the trachea to the terminal bronchioles. Albuterol acts as a functional antagonist to relax the airway irrespective of the spasmogen involved, thus protecting against all bronchoconstrictor challenges. Increased cyclic AMP concentrations are also associated with the inhibition of release of mediators from mast cells in the airway.
Albuterol has been shown in most controlled clinical trials to have more effect on the respiratory tract, in the form of bronchial smooth muscle relaxation, than isoproterenol at comparable doses while producing fewer cardiovascular effects. Controlled clinical studies and other clinical experience have shown that inhaled albuterol, like other beta-adrenergic agonist drugs, can produce a significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, symptoms, and/or electrocardiographic changes [see Warnings and Precautions (5.4)].
12.3 Pharmacokinetics
The systemic levels of albuterol are low after inhalation of recommended doses. A trial conducted in 12 healthy male and female subjects using a higher dose (1,080 mcg of albuterol base) showed that mean peak plasma concentrations of approximately 3 ng/mL occurred after dosing when albuterol was delivered using propellant HFA-134a. The mean time to peak concentrations (Tmax) was delayed after administration of VENTOLIN HFA (Tmax = 0.42 hours) as compared with CFC-propelled albuterol inhaler (Tmax = 0.17 hours). Apparent terminal plasma half-life of albuterol is approximately 4.6 hours. No further pharmacokinetic trials for VENTOLIN HFA were conducted in neonates, children, or elderly subjects.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year study in Sprague-Dawley rats, albuterol sulfate caused a dose-related increase in the incidence of benign leiomyomas of the mesovarium at and above dietary doses of 2.0 mg/kg (approximately 14 and 6 times the MRHDID for adults and children, respectively, on a mg/m2 basis). In another study this effect was blocked by the coadministration of propranolol, a non-selective beta-adrenergic antagonist. In an 18-month study in CD-1 mice, albuterol sulfate showed no evidence of tumorigenicity at dietary doses of up to 500 mg/kg (approximately 1,700 and 800 times the MRHDID for adults and children, respectively, on a mg/m2 basis). In a 22-month study in Golden hamsters, albuterol sulfate showed no evidence of tumorigenicity at dietary doses of up to 50 mg/kg (approximately 225 and 110 times the MRHDID for adults and children, respectively, on a mg/m2 basis).
Albuterol sulfate was not mutagenic in the Ames test or a mutation test in yeast. Albuterol sulfate was not clastogenic in a human peripheral lymphocyte assay or in an AH1 strain mouse micronucleus assay.
Reproduction studies in rats demonstrated no evidence of impaired fertility at oral doses of albuterol sulfate up to 50 mg/kg (approximately 340 times the MRHDID for adults on a mg/m2 basis).
13.2 Animal Toxicology and/or Pharmacology
Preclinical: Intravenous studies in rats with albuterol sulfate have demonstrated that albuterol crosses the blood-brain barrier and reaches brain concentrations amounting to approximately 5.0% of the plasma concentrations. In structures outside the blood-brain barrier (pineal and pituitary glands), albuterol concentrations were found to be 100 times those in the whole brain.
Studies in laboratory animals (minipigs, rodents, and dogs) have demonstrated the occurrence of cardiac arrhythmias and sudden death (with histologic evidence of myocardial necrosis) when beta-agonists and methylxanthines are administered concurrently. The clinical relevance of these findings is unknown.
Propellant HFA-134a: In animals and humans, propellant HFA-134a was found to be rapidly absorbed and rapidly eliminated, with an elimination half-life of 3 to 27 minutes in animals and 5 to 7 minutes in humans. Time to maximum plasma concentration (Tmax) and mean residence time are both extremely short, leading to a transient appearance of HFA-134a in the blood with no evidence of accumulation.
Propellant HFA-134a is devoid of pharmacological activity except at very high doses in animals (i.e., 380 to 1,300 times the maximum human exposure based on comparisons of area under the plasma concentration versus time curve [AUC] values), primarily producing ataxia, tremors, dyspnea, or salivation. These events are similar to effects produced by the structurally related CFCs, which have been used extensively in metered-dose inhalers.
-
14 CLINICAL STUDIES
14.1 Bronchospasm Associated with Asthma
Adult and Adolescent Subjects Aged 12 Years and Older: The efficacy of VENTOLIN HFA was evaluated in two 12-week, randomized, double-blind, placebo controlled trials in subjects aged 12 years and older with mild to moderate asthma. These trials included a total of 610 subjects (323 males, 287 females). In each trial, subjects received 2 inhalations of VENTOLIN HFA, CFC 11/12-propelled albuterol, or HFA-134a placebo 4 times daily for 12 weeks’ duration. Subjects taking the HFA-134a placebo inhaler also took VENTOLIN HFA for asthma symptom relief on an as-needed basis. Some subjects who participated in these clinical trials were using concomitant inhaled steroid therapy. Efficacy was assessed by serial forced expiratory volume in 1 second (FEV1). In each of these trials, 2 inhalations of VENTOLIN HFA produced significantly greater improvement in FEV1 over the pretreatment value than placebo. Results from the 2 clinical trials are described below.
In a 12-week, randomized, double-blind trial, VENTOLIN HFA (101 subjects) was compared with CFC 11/12-propelled albuterol (99 subjects) and an HFA-134a placebo inhaler (97 subjects) in adolescent and adult subjects aged 12 to 76 years with mild to moderate asthma. Serial FEV1 measurements [shown below as percent change from test-day baseline at Day 1 (n = 297) and at Week 12 (n = 249)] demonstrated that 2 inhalations of VENTOLIN HFA produced significantly greater improvement in FEV1 over the pretreatment value than placebo.
FEV1 as Percent Change from Predose in a Large, 12-Week Clinical Trial
Day 1

Week 12
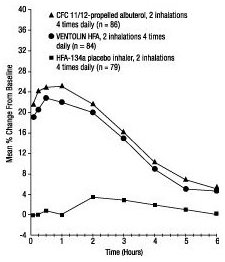
In the responder population (greater than or equal to 15% increase in FEV1 within 30 minutes postdose) treated with VENTOLIN HFA, the mean time to onset of a 15% increase in FEV1 over the pretreatment value was 5.4 minutes, and the mean time to peak effect was 56 minutes. The mean duration of effect as measured by a 15% increase in FEV1 over the pretreatment value was approximately 4 hours. In some subjects, duration of effect was as long as 6 hours.
The second 12-week randomized, double-blind trial was conducted to evaluate the efficacy and safety of switching subjects from CFC 11/12-propelled albuterol to VENTOLIN HFA. During the 3-week run-in phase of the trial, all subjects received CFC 11/12-propelled albuterol. During the double-blind treatment phase, VENTOLIN HFA (91 subjects) was compared to CFC 11/12-propelled albuterol (100 subjects) and an HFA-134a placebo inhaler (95 subjects) in adult and adolescent subjects with mild to moderate asthma. Serial FEV1 measurements demonstrated that 2 inhalations of VENTOLIN HFA produced significantly greater improvement in pulmonary function than placebo. The switching from CFC 11/12-propelled albuterol inhaler to VENTOLIN HFA did not reveal any clinically significant changes in the efficacy profile.
In the 2 adult trials, the efficacy results from VENTOLIN HFA were significantly greater than placebo and were clinically comparable to those achieved with CFC 11/12-propelled albuterol, although small numerical differences in mean FEV1 response and other measures were observed. Physicians should recognize that individual responses to beta-adrenergic agonists administered via different propellants may vary and that equivalent responses in individual patients should not be assumed.
Pediatric Subjects Aged 4 to 11 Years: The efficacy of VENTOLIN HFA was evaluated in one 2-week, randomized, double-blind, placebo-controlled trial in 135 pediatric subjects aged 4 to 11 years with mild to moderate asthma. In this trial, subjects received VENTOLIN HFA, CFC 11/12-propelled albuterol, or HFA-134a placebo. Serial pulmonary function measurements demonstrated that 2 inhalations of VENTOLIN HFA produced significantly greater improvement in pulmonary function than placebo and that there were no significant differences between the groups treated with VENTOLIN HFA and CFC 11/12-propelled albuterol. In the responder population treated with VENTOLIN HFA, the mean time to onset of a 15% increase in peak expiratory flow rate (PEFR) over the pretreatment value was 7.8 minutes, and the mean time to peak effect was approximately 90 minutes. The mean duration of effect as measured by a 15% increase in PEFR over the pretreatment value was greater than 3 hours. In some subjects, duration of effect was as long as 6 hours.
14.2 Exercise-Induced Bronchospasm
One controlled clinical trial in adult subjects with asthma (N = 24) demonstrated that 2 inhalations of VENTOLIN HFA taken approximately 30 minutes prior to exercise significantly prevented exercise-induced bronchospasm (as measured by maximum percentage fall in FEV1 following exercise) compared with an HFA-134a placebo inhaler. In addition, VENTOLIN HFA was shown to be clinically comparable to a CFC 11/12-propelled albuterol inhaler for this indication.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
VENTOLIN HFA Inhalation Aerosol is supplied in the following boxes of 1 as a pressurized aluminum canister fitted with a counter and supplied with a blue plastic actuator with a blue strapcap:
35356-166-08
35356-166-02
35356-166-01
The blue actuator supplied with VENTOLIN HFA should not be used with any other product canisters, and actuators from other products should not be used with a VENTOLIN HFA canister.
VENTOLIN HFA has a counter attached to the canister. The counter starts at 204 or 64 and counts down each time a spray is released. The correct amount of medication in each actuation cannot be assured after the counter reads 000, even though the canister is not completely empty and will continue to operate. The inhaler should be discarded when the counter reads 000 or 12 months after removal from the moisture-protective foil pouch, whichever comes first.
Keep out of reach of children. Avoid spraying in eyes.
Contents Under Pressure: Do not puncture. Do not use or store near heat or open flame. Exposure to temperatures above 120°F may cause bursting. Never throw canister into fire or incinerator.
Store at room temperature between 68°F and 77°F (20°C and 25°C); excursions permitted from 59°F to 86°F (15°C to 30°C) [See USP Controlled Room Temperature]. Store the inhaler with the mouthpiece down. For best results, the inhaler should be at room temperature before use. SHAKE WELL BEFORE EACH SPRAY.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Frequency of Use: Inform patients that the action of VENTOLIN HFA should last up to 4 to 6 hours. Do not use VENTOLIN HFA more frequently than recommended. Instruct patients not to increase the dose or frequency of doses of VENTOLIN HFA without consulting the physician. Instruct patients to seek medical attention immediately if treatment with VENTOLIN HFA becomes less effective for symptomatic relief, symptoms become worse, and/or they need to use the product more frequently than usual.
Priming: Instruct patients to prime VENTOLIN HFA before using for the first time, when the inhaler has not been used for more than 2 weeks, or when the inhaler has been dropped. To prime VENTOLIN HFA, release 4 sprays into the air away from the face, shaking well before each spray.
Cleaning: To ensure proper dosing and to prevent actuator orifice blockage, instruct patients to wash the actuator with warm water and let it air-dry completely at least once a week. Inform patients that detailed cleaning instructions are included in the Patient Information leaflet.
Paradoxical Bronchospasm: Inform patients that VENTOLIN HFA can produce paradoxical bronchospasm. Instruct them to discontinue VENTOLIN HFA if paradoxical bronchospasm occurs.
Concomitant Drug Use: Advise patients that while they are using VENTOLIN HFA, other inhaled drugs and asthma medications should be taken only as directed by the physician.
Common Adverse Effects:Common adverse effects of treatment with inhaled albuterol include palpitations, chest pain, rapid heart rate, tremor, and nervousness.
Pregnancy: Advise patients who are pregnant or nursing to contact their physicians about the use of VENTOLIN HFA.
VENTOLIN is a registered trademark of the GSK group of companies. The other brands listed are trademarks of their respective owners and are not trademarks of the GSK group of companies. The makers of these brands are not affiliated with and do not endorse the GSK group of companies or its products.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2014, the GSK group of companies. All rights reserved.
VNT:9PI
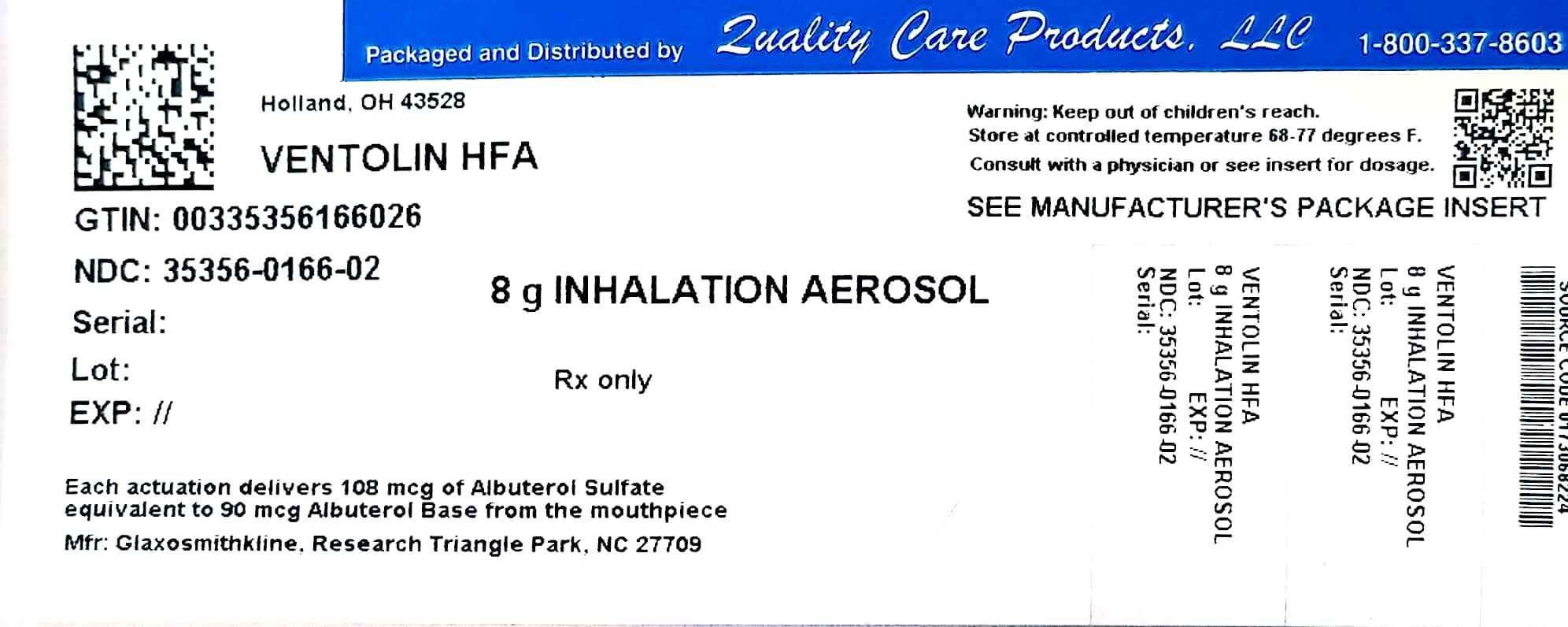
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
VENTOLIN HFA
albuterol sulfate aerosol, meteredProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 35356-166(NDC:0173-0682) Route of Administration RESPIRATORY (INHALATION) Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength ALBUTEROL SULFATE (UNII: 021SEF3731) (ALBUTEROL - UNII:QF8SVZ843E) ALBUTEROL 90 ug Inactive Ingredients Ingredient Name Strength NORFLURANE (UNII: DH9E53K1Y8) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 35356-166-01 1 in 1 CARTON 12/13/2013 12/31/2018 1 200 in 1 INHALER; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 2 NDC: 35356-166-02 1 in 1 CARTON 06/26/2018 2 60 in 1 INHALER; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) 3 NDC: 35356-166-08 1 in 1 CARTON 12/13/2013 12/31/2018 3 60 in 1 INHALER; Type 2: Prefilled Drug Delivery Device/System (syringe, patch, etc.) Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA020983 06/09/2006 Labeler - Lake Erie Medical DBA Quality Care Products LLC (831276758) Establishment Name Address ID/FEI Business Operations Lake Erie Medical DBA Quality Care Products LLC 831276758 relabel(35356-166)
Trademark Results [VENTOLIN]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 VENTOLIN 75017092 2013681 Live/Registered |
GLAXO GROUP LIMITED 1995-11-09 |
 VENTOLIN 73124483 1095668 Live/Registered |
ALLEN & HANBURYS LIMITED 1977-04-27 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.