VALSARTAN AND HYDROCHLOROTHIAZIDE tablet, film coated
Valsartan and Hydrochlorothiazide by
Drug Labeling and Warnings
Valsartan and Hydrochlorothiazide by is a Prescription medication manufactured, distributed, or labeled by REMEDYREPACK INC.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use valsartan and hydrochlorothiazide tablets, USP, safely and effectively. See full prescribing information for valsartan and hydrochlorothiazide tablets USP.
VALSARTAN and HYDROCHLOROTHIAZIDE tablets USP, for oral use
Initial U.S. Approval: 1998WARNING: FETAL TOXICITY
See full prescribing information for complete boxed warning.
- When pregnancy is detected, discontinue valsartan and hydrochlorothiazide tablets as soon as possible. (5.1)
- Drugs that act directly on the renin-angiotensin system can cause injury and death to the developing fetus. (5.1)
INDICATIONS AND USAGE
Valsartan and hydrochlorothiazide tablets, USP are the combination tablet of valsartan, an angiotensin II receptor blocker (ARB) and hydrochlorothiazide (HCTZ), a diuretic.
Valsartan and hydrochlorothiazide tablets, USP are indicated for the treatment of hypertension, to lower blood pressure :
In patients not adequately controlled with monotherapy ( 1)
As initial therapy in patients likely to need multiple drugs to achieve their blood pressure goals ( 1)
Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
Tablets (valsartan/HCTZ mg): 80/12.5, 160/12.5, 160/25, 320/12.5, 320/25 ( 3)
CONTRAINDICATIONS
Anuria; Hypersensitivity to any sulfonamide-derived drugs or any component; Do not coadminister aliskiren with valsartan and hydrochlorothiazide tablets in patients with diabetes ( 4)
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
The most common reasons for discontinuation of therapy with valsartan and hydrochlorothiazide were headache and dizziness. The only adverse experience that occurred in ≥2% of patients treated with valsartan and hydrochlorothiazide and at a higher incidence than placebo was nasopharyngitis (2.4% vs. 1.9%) ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Macleods Pharma USA, Inc., at 1-888-943-3210 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.DRUG INTERACTIONS
- Antidiabetic drugs: Dosage adjustment of antidiabetic may be required ( 7)
- Cholestyramine and colestipol: Reduced absorption of thiazides ( 12.3)
- Lithium: Increase risk of lithium toxicity. Monitor serum lithium concentrations during concurrent use. ( 7)
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): May increase risk of renal impairment. Can reduce diuretic, natriuretic and antihypertensive effects of diuretics. ( 7)
- Dual inhibition of the renin-angiotensin system: Increased risk of renal impairment, hypotension, and hyperkalemia ( 7)
USE IN SPECIFIC POPULATIONS
Nursing Mothers: Nursing or drug should be discontinued ( 8.3)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 5/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING:FETAL TOXICITY
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 General Considerations
2.2 Add-On Therapy
2.3 Replacement Therapy
2.4 Initial Therapy
2.5 Use with Other Antihypertensive Drugs
3 DOSAGE FORMS & STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Fetal Toxicity
5.2 Hypotension in Volume- and/or Salt-Depleted Patients
5.3 Impaired Renal Function
5.4 Hypersensitivity Reaction
5.5 Systemic Lupus Erythematosus
5.6 Lithium Interaction
5.7 Potassium Abnormalities
5.8 Acute Myopia and Secondary Angle-Closure Glaucoma
5.9 Metabolic Disturbances
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
13.3 Developmental Toxicity Studies
14 CLINICAL STUDIES
14.1 Hypertension
14.2 Initial Therapy - Hypertension
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- BOXED WARNING (What is this?)
-
1 INDICATIONS AND USAGE
Valsartan and hydrochlorothiazide tablets, USP are indicated for the treatment of hypertension, to lower blood pressure. Lowering blood pressure reduces the risk of fatal and nonfatal cardiovascular events, primarily strokes and myocardial infarctions. These benefits have been seen in controlled trials of antihypertensive drugs from a wide variety of pharmacologic classes, including hydrochlorothiazide and the ARB class to which valsartan principally belongs. There are no controlled trials demonstrating risk reduction with valsartan and hydrochlorothiazide tablets, USP.
Control of high blood pressure should be part of comprehensive cardiovascular risk management, including, as appropriate, lipid control, diabetes management, antithrombotic therapy, smoking cessation, exercise, and limited sodium intake. Many patients will require more than 1 drug to achieve blood pressure goals. For specific advice on goals and management, see published guidelines, such as those of the National High Blood Pressure Education Program’s Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC).
Numerous antihypertensive drugs, from a variety of pharmacologic classes and with different mechanisms of action, have been shown in randomized controlled trials to reduce cardiovascular morbidity and mortality, and it can be concluded that it is blood pressure reduction, and not some other pharmacologic property of the drugs, that is largely responsible for those benefits. The largest and most consistent cardiovascular outcome benefit has been a reduction in the risk of stroke, but reductions in myocardial infarction and cardiovascular mortality have also been seen regularly.
Elevated systolic or diastolic pressure causes increased cardiovascular risk, and the absolute risk increase per mmHg is greater at higher blood pressures, so that even modest reductions of severe hypertension can provide substantial benefit. Relative risk reduction from blood pressure reduction is similar across populations with varying absolute risk, so the absolute benefit is greater in patients who are at higher risk independent of their hypertension (for example, patients with diabetes or hyperlipidemia), and such patients would be expected to benefit from more aggressive treatment to a lower blood pressure goal.
Some antihypertensive drugs have smaller blood pressure effects (as monotherapy) in black patients, and many antihypertensive drugs have additional approved indications and effects (e.g., on angina, heart failure, or diabetic kidney disease). These considerations may guide selection of therapy.
Add-On Therapy
Valsartan and hydrochlorothiazide tablets, USP may be used in patients whose blood pressure is not adequately controlled on monotherapy.
Replacement Therapy
Valsartan and hydrochlorothiazide tablets, USP may be substituted for the titrated components.
Initial Therapy
Valsartan and hydrochlorothiazide tablets, USP may be used as initial therapy in patients who are likely to need multiple drugs to achieve blood pressure goals.
The choice of valsartan and hydrochlorothiazide tablets, USP as initial therapy for hypertension should be based on an assessment of potential benefits and risks.
Patients with stage 2 hypertension are at a relatively high risk for cardiovascular events (such as strokes, heart attacks, and heart failure), kidney failure, and vision problems, so prompt treatment is clinically relevant. The decision to use a combination as initial therapy should be individualized and should be shaped by considerations such as baseline blood pressure, the target goal and the incremental likelihood of achieving goal with a combination compared to monotherapy. Individual blood pressure goals may vary based upon the patient's risk.
Data from the high dose multifactorial trial [see Clinical Studies ( 14.1)]provides estimates of the probability of reaching a target blood pressure with valsartan and hydrochlorothiazide tablets, USP compared to valsartan or hydrochlorothiazide monotherapy. The figures below provide estimates of the likelihood of achieving systolic or diastolic blood pressure control with valsartan and hydrochlorothiazide tablets, USP 320/25 mg, based upon baseline systolic or diastolic blood pressure. The curve of each treatment group was estimated by logistic regression modeling. The estimated likelihood at the right tail of each curve is less reliable due to small numbers of subjects with high baseline blood pressures.
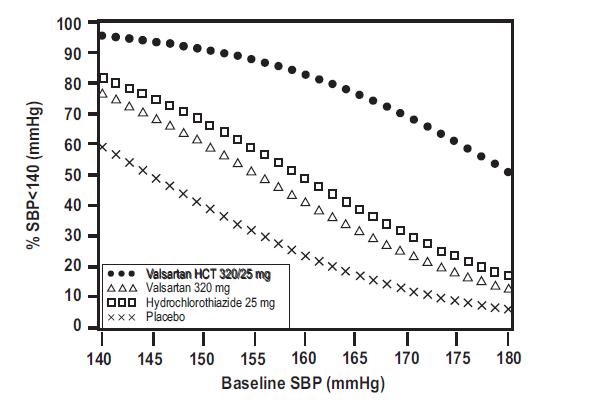
Figure 1: Probability of Achieving Systolic Blood Pressure <140 mmHg at Week 8
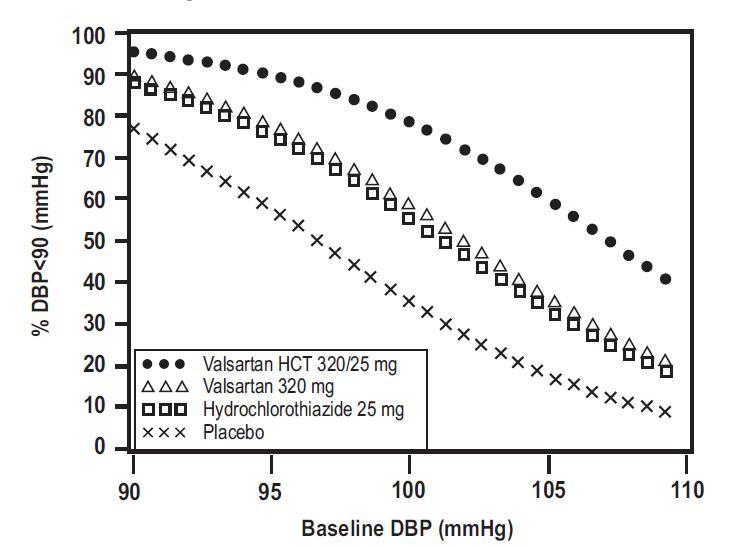
Figure 2: Probability of Achieving Diastolic Blood Pressure <90 mmHg at Week 8
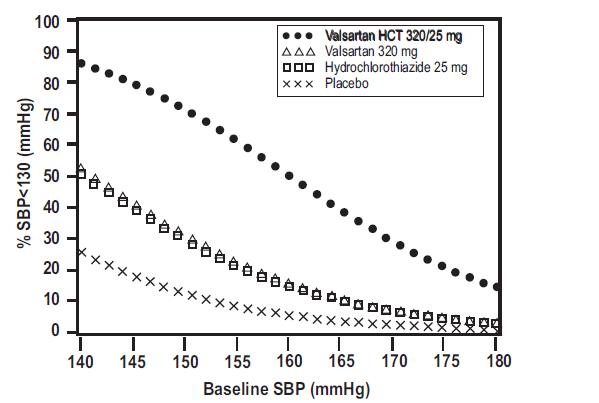
Figure 3: Probability of Achieving Systolic Blood Pressure <130 mmHg at Week 8
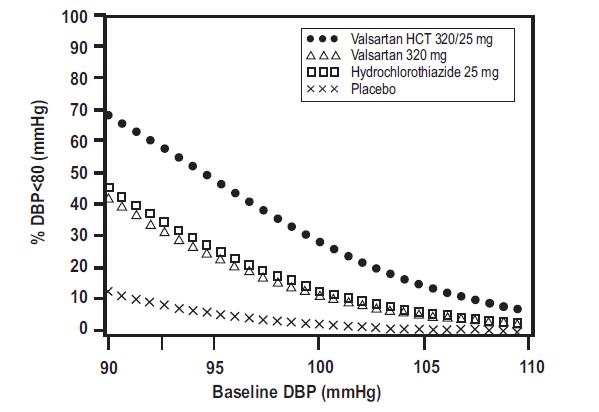
Figure 4: Probability of Achieving Diastolic Blood Pressure <80 mmHg at Week 8
For example, a patient with a baseline blood pressure of 160/100 mmHg has about a 41% likelihood of achieving a goal of <140 mmHg (systolic) and 60% likelihood of achieving <90 mmHg (diastolic) on valsartan alone and the likelihood of achieving these goals on HCTZ alone is about 50% (systolic) or 57% (diastolic). The likelihood of achieving these goals on valsartan and hydrochlorothiazide tablets, USP rises to about 84% (systolic) or 80% (diastolic). The likelihood of achieving these goals on placebo is about 23% (systolic) or 36% (diastolic).
-
2 DOSAGE AND ADMINISTRATION
2.1 General Considerations
The usual starting dose is valsartan and hydrochlorothiazide tablets 160/12.5 mg once daily. The dosage can be increased after 1 to 2 weeks of therapy to a maximum of one 320/25 tablet once daily as needed to control blood pressure [see Clinical Studies ( 14.2)]. Maximum antihypertensive effects are attained within 2 to 4 weeks after a change in dose.
2.2 Add-On Therapy
A patient whose blood pressure is not adequately controlled with valsartan (or another ARB) alone or hydrochlorothiazide alone may be switched to combination therapy with valsartan and hydrochlorothiazide tablets.
A patient who experiences dose-limiting adverse reactions on either component alone may be switched to valsartan and hydrochlorothiazide tablets containing a lower dose of that component in combination with the other to achieve similar blood pressure reductions. The clinical response to valsartan and hydrochlorothiazide tablets should be subsequently evaluated and if blood pressure remains uncontrolled after 3 to 4 weeks of therapy, the dose may be titrated up to a maximum of 320/25 mg.
2.3 Replacement Therapy
Valsartan and hydrochlorothiazide tablets may be substituted for the titrated components.
2.4 Initial Therapy
Valsartan and hydrochlorothiazide tablets are not recommended as initial therapy in patients with intravascular volume depletion [see Warnings and Precautions ( 5.2)].
-
3 DOSAGE FORMS & STRENGTHS
80/12.5 mg tablets, debossed with "L16" on side and plain on other side
160/12.5 mg tablets, debossed with "L17" on side and plain on other side
160/25 mg tablets, debossed with "L18" on side and plain on other side
320/12.5 mg tablets, debossed with "L19" on side and plain on other side
320/25 mg tablets, debossed with "L20" on side and plain on other side
-
4 CONTRAINDICATIONS
Valsartan and hydrochlorothiazide tablets, USP are contraindicated in patients who are hypersensitive to any component of this product.
Because of the hydrochlorothiazide component, this product is contraindicated in patients with anuria or hypersensitivity to other sulfonamide-derived drugs.
Do not coadminister aliskiren with valsartan and hydrochlorothiazide tablets in patients with diabetes [See Drug Interactions (7)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Fetal Toxicity
Pregnancy Category D
Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue Valsartan and hydrochlorothiazide tablets as soon as possible [see Use in Specific Populations (8.1)].
Intrauterine exposure to thiazide diuretics is associated with fetal or neonatal jaundice, thrombocytopenia, and possibly other adverse reactions that have occurred in adults
5.2 Hypotension in Volume- and/or Salt-Depleted Patients
Excessive reduction of blood pressure was rarely seen (0.7%) in patients with uncomplicated hypertension treated with valsartan and hydrochlorothiazide tablets in controlled trials. In patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients receiving high doses of diuretics, symptomatic hypotension may occur. This condition should be corrected prior to administration of valsartan and hydrochlorothiazide tablets, or the treatment should start under close medical supervision.
If hypotension occurs, the patient should be placed in the supine position and, if necessary, given an intravenous infusion of normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
5.3 Impaired Renal Function
Changes in renal function including acute renal failure can be caused by drugs that inhibit the renin-angiotensin system and by diuretics. Patients whose renal function may depend in part on the activity of the renin-angiotensin system (e.g., patients with renal artery stenosis, chronic kidney disease, severe congestive heart failure, or volume depletion) may be at particular risk of developing acute renal failure on valsartan and hydrochlorothiazide tablets. Monitor renal function periodically in these patients. Consider withholding or discontinuing therapy in patients who develop a clinically significant decrease in renal function on valsartan and hydrochlorothiazide tablets [See Drug Interactions ( 7)].
5.4 Hypersensitivity Reaction
Hydrochlorothiazide: Hypersensitivity reactions to hydrochlorothiazide may occur in patients with or without a history of allergy or bronchial asthma, but are more likely in patients with such a history.
5.5 Systemic Lupus Erythematosus
Hydrochlorothiazide: Thiazide diuretics have been reported to cause exacerbation or activation of systemic lupus erythematosus.
5.6 Lithium Interaction
Increases in serum lithium concentrations and lithium toxicity have been reported with concomitant use of valsartan or thiazide diuretics. Monitor lithium levels in patients receiving valsartan HCT and lithium. [See Drug Interactions ( 7)].
5.7 Potassium Abnormalities
Valsartan – Hydrochlorothiazide: In the controlled trials of various doses of valsartan and hydrochlorothiazide tablets the incidence of hypertensive patients who developed hypokalemia (serum potassium <3.5 mEq/L) was 3.0%; the incidence of hyperkalemia (serum potassium >5.7 mEq/L) was 0.4%.
Hydrochlorothiazide can cause hypokalemia and hyponatremia. Hypomagnesemia can result in hypokalemia which appears difficult to treat despite potassium repletion. Drugs that inhibit the renin-angiotensin system can cause hyperkalemia. Monitor serum electrolytes periodically.
If hypokalemia is accompanied by clinical signs (e.g. muscular weakness, paresis, or ECG alterations), valsartan and hydrochlorothiazide tablets should be discontinued. Correction of hypokalemia and any coexisting hypomagnesemia is recommended prior to the initiation of thiazides.
Some patients with heart failure have developed increases in potassium with valsartan therapy. These effects are usually minor and transient, and they are more likely to occur in patients with pre-existing renal impairment. Dosage reduction and/or discontinuation of the diuretic and/or valsartan may be required [see Adverse Reactions ( 6.1)].
5.8 Acute Myopia and Secondary Angle-Closure Glaucoma
Hydrochlorothiazide, a sulfonamide, can cause an idiosyncratic reaction, resulting in acute transient myopia and acute angle-closure glaucoma. Symptoms include acute onset of decreased visual acuity or ocular pain and typically occur within hours to weeks of drug initiation. Untreated acute angle-closure glaucoma can lead to permanent vision loss. The primary treatment is to discontinue hydrochlorothiazide as rapidly as possible. Prompt medical or surgical treatments may need to be considered if the intraocular pressure remains uncontrolled. Risk factors for developing acute angle-closure glaucoma may include a history of sulfonamide or penicillin allergy.
5.9 Metabolic Disturbances
Hydrochlorothiazide
Hydrochlorothiazide may alter glucose tolerance and raise serum levels of cholesterol and triglycerides.
Hydrochlorothiazide may raise the serum uric acid level due to reduced clearance of uric acid and may cause or exacerbate hyperuricemia and precipitate gout in susceptible patients.
Hydrochlorothiazide decreases urinary calcium excretion and may cause elevations of serum calcium. Monitor calcium levels in patients with hypercalcemia receiving valsartan and hydrochlorothiazide tablets.
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reactions rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Hypertension
Valsartan and hydrochlorothiazide tablets, USP have been evaluated for safety in more than 5,700 patients, including over 990 treated for over 6 months, and over 370 for over 1 year. Adverse experiences have generally been mild and transient in nature and have only infrequently required discontinuation of therapy. The overall incidence of adverse reactions with valsartan and hydrochlorothiazide tablets was comparable to placebo.
The overall frequency of adverse reactions was neither dose-related nor related to gender, age, or race. In controlled clinical trials, discontinuation of therapy due to side effects was required in 2.3% of valsartan-hydrochlorothiazide patients and 3.1% of placebo patients. The most common reasons for discontinuation of therapy with valsartan and hydrochlorothiazide tablets were headache and dizziness.
The only adverse reaction that occurred in controlled clinical trials in at least 2% of patients treated with valsartan and hydrochlorothiazide tablets and at a higher incidence in valsartan-hydrochlorothiazide (n=4372) than placebo (n=262) patients was nasopharyngitis (2.4% vs. 1.9%).
Dose-related orthostatic effects were seen in fewer than 1% of patients. In individual trials, a dose-related increase in the incidence of dizziness was observed in patients treated with valsartan and hydrochlorothiazide tablets.
Other adverse reactions that have been reported with valsartan-hydrochlorothiazide (>0.2% of valsartan-hydrochlorothiazide patients in controlled clinical trials) without regard to causality, are listed below:
Cardiovascular: Palpitations and tachycardia
Ear and Labyrinth: Tinnitus and vertigo
Gastrointestinal: Dyspepsia, diarrhea, flatulence, dry mouth, nausea, abdominal pain, abdominal pain upper, and vomiting
General and Administration Site Conditions: Asthenia, chest pain, fatigue, peripheral edema and pyrexia
Infections and Infestations: Bronchitis, bronchitis acute, influenza, gastroenteritis, sinusitis, upper respiratory tract infection and urinary tract infection
Investigations: Blood urea increased
Musculoskeletal: Arthralgia, back pain, muscle cramps, myalgia, and pain in extremity
Nervous System: Dizziness postural, paresthesia, and somnolence
Psychiatric: Anxiety and insomnia
Renal and Urinary: Pollakiuria
Reproductive System: Erectile dysfunction
Respiratory, Thoracic and Mediastinal: Dyspnea, cough, nasal congestion, pharyngolaryngeal pain and sinus congestion
Skin and Subcutaneous Tissue: Hyperhidrosis and rash
Vascular: Hypotension
Other reported reactions seen less frequently in clinical trials included abnormal vision, anaphylaxis, bronchospasm, constipation, depression, dehydration, decreased libido, dysuria, epistaxis, flushing, gout, increased appetite, muscle weakness, pharyngitis, pruritus, sunburn, syncope, and viral infection.
Initial Therapy - Hypertension
In a clinical study in patients with severe hypertension (diastolic blood pressure ≥110 mmHg and systolic blood pressure ≥140 mmHg), the overall pattern of adverse reactions reported through 6 weeks of follow-up was similar in patients treated with valsartan and hydrochlorothiazide tablets as initial therapy and in patients treated with valsartan as initial therapy. Comparing the groups treated with valsartan and hydrochlorothiazide tablets (force-titrated to 320/25 mg) and valsartan (force-titrated to 320 mg), dizziness was observed in 6% and 2% of patients, respectively. Hypotension was observed in 1% of those patients receiving valsartan and hydrochlorothiazide tablets and 0% of patients receiving valsartan. There were no reported cases of syncope in either treatment group. Laboratory changes with valsartan and hydrochlorothiazide tablets as initial therapy in patients with severe hypertension were similar to those reported with valsartan and hydrochlorothiazide tablets in patients with less severe hypertension [ see Clinical Studies (14.2) and Drug Interactions ( 7)].
Valsartan: In trials in which valsartan was compared to an ACE inhibitor with or without placebo, the incidence of dry cough was significantly greater in the ACE inhibitor group (7.9%) than in the groups who received valsartan (2.6%) or placebo (1.5%). In a 129-patient trial limited to patients who had had dry cough when they had previously received ACE inhibitors, the incidences of cough in patients who received valsartan, hydrochlorothiazide, or lisinopril were 20%, 19%, 69% respectively (p <0.001).
Other reported reactions seen less frequently in clinical trials included chest pain, syncope, anorexia, vomiting, and angioedema.
Hydrochlorothiazide: Other adverse reactions not listed above that have been reported with hydrochlorothiazide, without regard to causality, are listed below:
Body As A Whole: weakness
Digestive: pancreatitis, jaundice (intrahepatic cholestatic jaundice), sialadenitis, cramping, gastric irritation
Hematologic: aplastic anemia, agranulocytosis, leukopenia, hemolytic anemia, thrombocytopenia
Hypersensitivity: purpura, photosensitivity, urticaria, necrotizing angiitis (vasculitis and cutaneous vasculitis), fever, respiratory distress including pneumonitis and pulmonary edema, anaphylactic reactions
Metabolic: hyperglycemia, glycosuria, hyperuricemia
Musculoskeletal: muscle spasm
Nervous System/Psychiatric: restlessness
Renal: renal failure, renal dysfunction, interstitial nephritis
Skin: erythema multiforme including Stevens-Johnson syndrome, exfoliative dermatitis including toxic epidermal necrolysis
Special Senses: transient blurred vision, xanthopsia
Clinical Laboratory Test Findings
In controlled clinical trials, clinically important changes in standard laboratory parameters were rarely associated with administration of valsartan and hydrochlorothiazide tablets.
Creatinine/Blood Urea Nitrogen (BUN): Minor elevations in creatinine and BUN occurred in 2% and 15% respectively, of patients taking valsartan and hydrochlorothiazide tablets and 0.4% and 6% respectively, given placebo in controlled clinical trials.
Hemoglobin and Hematocrit: Greater than 20% decreases in hemoglobin and hematocrit were observed in less than 0.1% of valsartan and hydrochlorothiazide tablets patients, compared with 0% in placebo-treated patients.
Liver Function Tests: Occasional elevations (greater than 150%) of liver chemistries occurred in valsartan and hydrochlorothiazide tablets -treated patients.
Neutropenia: Neutropenia was observed in 0.1% of patients treated with valsartan and hydrochlorothiazide tablets and 0.4% of patients treated with placebo.
6.2 Postmarketing Experience
The following additional adverse reactions have been reported in valsartan or valsartan/ hydrochlorothiazide postmarketing experience. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity: There are rare reports of angioedema. Some of these patients previously experienced angioedema with other drugs including ACE inhibitors. Valsartan and hydrochlorothiazide tablets should not be re-adminitered to patients who have had angioedema.
Digestive: Elevated liver enzymes and very rare reports of hepatitis
Renal: Impaired renal function
Clinical Laboratory Tests: Hyperkalemia
Dermatologic: Alopecia, bullous dermatitis
Vascular: Vasculitis
Nervous System: Syncope
Rare cases of rhabdomyolysis have been reported in patients receiving angiotensin II receptor blockers.
Hydrochlorothiazide:
The following additional adverse reactions have been reported in post-marketing experience with hydrochlorothiazide:
Acute renal failure, renal disorder, aplastic anemia, erythema multiforme, pyrexia, muscle spasm, asthenia, acute angle-closure glaucoma, bone marrow failure, worsening of diabetes control, hypokalemia, blood lipids increased, hyponatremia, hypomagnesemia, hypercalcemia, hypochloremic alkalosis, impotence, and visual impairment.
Pathological changes in the parathyroid gland of patients with hypercalcemia and hypophosphatemia have been observed in a few patients on prolonged thiazide therapy. If hypercalcemia occurs, further diagnostic evaluation is necessary.
-
7 DRUG INTERACTIONS
Valsartan-Hydrochlorothiazide:
Lithium: Increases in serum lithium concentrations and lithium toxicity have been reported during concomitant administration of lithium with angiotensin II receptor antagonists or thiazides. Monitor lithium levels in patients taking valsartan HCT.
Valsartan: No clinically significant pharmacokinetic interactions were observed when valsartan was coadministered with amlodipine, atenolol, cimetidine, digoxin, furosemide, glyburide, hydrochlorothiazide, or indomethacin. The valsartan-atenolol combination was more antihypertensive than either component, but it did not lower the heart rate more than atenolol alone.
Coadministration of valsartan and warfarin did not change the pharmacokinetics of valsartan or the time-course of the anticoagulant properties of warfarin.
CYP 450 Interactions:In vitro metabolism studies indicate that CYP 450 mediated drug interactions between valsartan and co-administered drugs are unlikely because of low extent of metabolism [see Clinical Pharmacology ( 12.3)].
Transporters: The results from an in vitro study with human liver tissue indicate that valsartan is a substrate of the hepatic uptake transporter OATP1B1 and the hepatic efflux transporter MRP2. Coadministration of inhibitors of the uptake transporter (rifampin, cyclosporine) or efflux transporter (ritonavir) may increase the systemic exposure to valsartan
Non-Steroidal Anti-Inflammatory Agents including Selective Cyclooxygenase-2 Inhibitors (COX-2 Inhibitors): In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, coadministration of NSAIDs, including selective COX-2 inhibitors, with angiotensin II receptor antagonists, including valsartan, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible. Monitor renal function periodically in patients receiving valsartan and NSAID therapy.
The antihypertensive effect of angiotensin II receptor antagonists, including valsartan may be attenuated by NSAIDs including selective COX-2 inhibitors.
Potassium: Concomitant use of valsartan with other agents that block the renin-angiotensin system, potassium-sparing diuretics (e.g. spironolactone, triamterene, amiloride), potassium supplements, salt substitutes containing potassium or other drugs that may increase potassium levels (e.g., heparin) may lead to increases in serum potassium and in heart failure patients to increases in serum creatinine. If comedication is considered necessary, monitoring of serum potassium is advisable.
Dual Blockade of the Renin-Angiotensin System (RAS): Dual blockade of the RAS with angiotensin receptor blockers, ACE inhibitors, or aliskiren is associated with increased risks of hypotension, hyperkalemia, and changes in renal function (including acute renal failure) compared to monotherapy. Most patients receiving the combination of two RAS inhibitors do not obtain any additional benefit compared to monotherapy. In general, avoid combined use of RAS inhibitors. Closely monitor blood pressure, renal function and electrolytes in patients on valsartan and hydrochlorothiazide tablets and other agents that affect the RAS.
Do not coadminister aliskiren with valsartan and hydrochlorothiazide tablets in patients with diabetes. Avoid use of aliskiren with valsartan and hydrochlorothiazide tablets in patients with renal impairment (GFR <60 ml/min).
Hydrochlorothiazide: When administered concurrently, the following drugs may interact with thiazide diuretics:
Antidiabetic Drugs (oral agents and insulin ) - Dosage adjustment of the antidiabetic drug may be required.
Nonsteroidal Anti-inflammatory Drugs (NSAIDS and COX-2 selective inhibitors) - When valsartan and hydrochlorothiazide tablets and nonsteroidal anti-inflammatory agents are used concomitantly, the patient should be observed closely to determine if the desired effect of the diuretic is obtained.
Carbamazepine – May lead to symptomatic hyponatremia.
Ion exchange resins: Staggering the dosage of hydrochlorothiazide and ion exchange resins (e.g., cholestyramine, colestipol) such that hydrochlorothiazide is administered at least 4 hours before or 4-6 hours after the administration of resins would potentially minimize the interaction.
[see Clinical Pharmacology ( 12.3)].
Cyclosporine: Concomitant treatment with cyclosporine may increase the risk of hyperuricemia and gout-type complications.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D
Use of drugs that act on the renin-angiotensin system during the second and third trimesters of pregnancy reduces fetal renal function and increases fetal and neonatal morbidity and death. Resulting oligohydramnios can be associated with fetal lung hypoplasia and skeletal deformations. Potential neonatal adverse effects include skull hypoplasia, anuria, hypotension, renal failure, and death. When pregnancy is detected, discontinue valsartan and hydrochlorothiazide tablets as soon as possible. These adverse outcomes are usually associated with use of these drugs in the second and third trimester of pregnancy. Most epidemiologic studies examining fetal abnormalities after exposure to antihypertensive use in the first trimester have not distinguished drugs affecting the renin-angiotensin system from other antihypertensive agents. Appropriate management of maternal hypertension during pregnancy is important to optimize outcomes for both mother and fetus.
In the unusual case that there is no appropriate alternative to therapy with drugs affecting the renin-angiotensin system for a particular patient, apprise the mother of the potential risk to the fetus. Perform serial ultrasound examinations to assess the intra-amniotic environment. If oligohydramnios is observed, discontinue valsartan and hydrochlorothiazide tablets, unless it is considered lifesaving for the mother. Fetal testing may be appropriate, based on the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury. Closely observe infants with histories of in utero exposure to valsartan and hydrochlorothiazide tablets for hypotension, oliguria, and hyperkalemia [ see Use in Specific Populations ( 8.4)].
Hydrochlorothiazide
Thiazides can cross the placenta, and concentrations reached in the umbilical vein approach those in the maternal plasma. Hydrochlorothiazide, like other diuretics, can cause placental hypoperfusion. It accumulates in the amniotic fluid, with reported concentrations up to 19 times higher than in umbilical vein plasma. Use of thiazides during pregnancy is associated with a risk of fetal or neonatal jaundice or thrombocytopenia. Since they do not prevent or alter the course of EPH (Edema, Proteinuria, Hypertension) gestosis (pre-eclampsia), these drugs should not be used to treat hypertension in pregnant women. The use of hydrochlorothiazide for other indications (e.g. heart disease) in pregnancy should be avoided.8.3 Nursing Mothers
It is not known whether valsartan is excreted in human milk. Valsartan was excreted into the milk of lactating rats; however, animal breast milk drug levels may not accurately reflect human breast milk levels. Hydrochlorothiazide is excreted in human breast milk. Because many drugs are excreted into human milk and because of the potential for adverse reactions in nursing infants from valsartan and hydrochlorothiazide tablets, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness of valsartan and hydrochlorothiazide tablets in pediatric patients have not been established.
Neonates with a history of in utero exposure to valsartan and hydrochlorothiazide tablets:
If oliguria or hypotension occurs, direct attention toward support of blood pressure and renal perfusion. Exchange transfusions or dialysis may be required as a means of reversing hypotension and/or substituting for disordered renal function.8.5 Geriatric Use
In the controlled clinical trials of valsartan and hydrochlorothiazide tablets, 764 (17.5%) patients treated with valsartan-hydrochlorothiazide were ≥65 years and 118 (2.7%) were ≥75 years. No overall difference in the efficacy or safety of valsartan-hydrochlorothiazide was observed between these patients and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
Safety and effectiveness of valsartan and hydrochlorothiazide tablets in patients with severe renal impairment (CrCl ≤ 30 mL/min) have not been established. No dose adjustment is required in patients with mild (CrCl 60-90 mL/min) or moderate (CrCl 30-60) renal impairment.
8.7 Hepatic Impairment
Valsartan
No dose adjustment is necessary for patients with mild-to-moderate liver disease. No dosing recommendations can be provided for patients with severe liver disease.
Hydrochlorothiazide
Minor alterations of fluid and electrolyte balance may precipitate hepatic coma in patients with impaired hepatic function or progressive liver disease.
-
10 OVERDOSAGE
Valsartan – Hydrochlorothiazide: Limited data are available related to overdosage in humans. The most likely manifestations of overdosage would be hypotension and tachycardia; bradycardia could occur from parasympathetic (vagal) stimulation. Depressed level of consciousness, circulatory collapse and shock have been reported. If symptomatic hypotension should occur, supportive treatment should be instituted.
Valsartan is not removed from the plasma by dialysis.
The degree to which hydrochlorothiazide is removed by hemodialysis has not been established. The most common signs and symptoms observed in patients are those caused by electrolyte depletion (hypokalemia, hypochloremia, hyponatremia) and dehydration resulting from excessive diuresis. If digitalis has also been administered, hypokalemia may accentuate cardiac arrhythmias.
In rats and marmosets, single oral doses of valsartan up to 1524 and 762 mg/kg in combination with hydrochlorothiazide at doses up to 476 and 238 mg/kg, respectively, were very well tolerated without any treatment-related effects. These no adverse effect doses in rats and marmosets, respectively, represent 46.5 and 23 times the maximum recommended human dose (MRHD) of valsartan and 188 and 113 times the MRHD of hydrochlorothiazide on a mg/m2 basis. (Calculations assume an oral dose of 320 mg/day valsartan in combination with 25 mg/day hydrochlorothiazide and a 60-kg patient.)
Valsartan: Valsartan was without grossly observable adverse effects at single oral doses up to 2000 mg/kg in rats and up to 1000 mg/kg in marmosets, except for salivation and diarrhea in the rat and vomiting in the marmoset at the highest dose (60 and 31 times, respectively, the MRHD on a mg/m 2 basis). (Calculations assume an oral dose of 320 mg/day and a 60-kg patient.)
Hydrochlorothiazide: The oral LD 50 of hydrochlorothiazide is greater than 10 g/kg in both mice and rats, which represents 2027 and 4054 times, respectively, the MRHD on a mg/m2 basis. (Calculations assume an oral dose of 25 mg/day and a 60-kg patient.) -
11 DESCRIPTION
Valsartan and hydrochlorothiazide tablets, USP are a combination of valsartan, an orally active, specific angiotensin II receptor blocker (ARB) acting on the AT 1 receptor subtype, and hydrochlorothiazide, a diuretic.
Valsartan, a nonpeptide molecule, is chemically described as N-(1-oxopentyl)-N-[[2′-(1H-tetrazol-5-yl)[1,1′-biphenyl]-4-yl]methyl]-L-Valine. Its empirical formula is C 24H 29N 5O 3, its molecular weight is 435.5, and its structural formula is
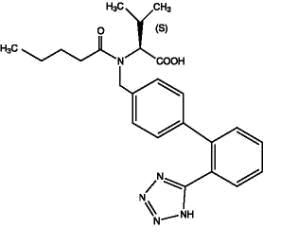
Valsartan is a white to practically white fine powder. It is soluble in ethanol and methanol and slightly soluble in water.
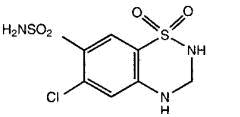
Hydrochlorothiazide USP is a white, or practically white, practically odorless, crystalline powder. It is slightly soluble in water; freely soluble in sodium hydroxide solution, in n-butylamine, and in dimethylformamide; sparingly soluble in methanol; and insoluble in ether, in chloroform, and in dilute mineral acids. Hydrochlorothiazide is chemically described as 6-chloro-3,4-dihydro-2H-1,2,4-benzothiadiazine-7-sulfonamide 1,1-dioxide.
Hydrochlorothiazide is a thiazide diuretic. Its empirical formula is C 7H 8ClN 3O 4S 2, its molecular weight is 297.73, and its structural formula is
Valsartan and hydrochlorothiazide tablets, USP, are formulated for oral administration to contain valsartan and hydrochlorothiazide, USP 80/12.5 mg, 160/12.5 mg, 160/25 mg, 320/12.5 mg and 320/25 mg. The inactive ingredients of the tablets are colloidal silicon dioxide, crospovidone, hydroxypropyl methylcellulose, iron oxides, magnesium stearate, microcrystalline cellulose, polyethylene glycol, talc, and titanium dioxide.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin-converting enzyme (ACE, kininase II). Angiotensin II is the principal pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation, and renal reabsorption of sodium. Valsartan blocks the vasoconstrictor and aldosterone-secreting effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT 1 receptor in many tissues, such as vascular smooth muscle and the adrenal gland. Its action is therefore independent of the pathways for angiotensin II synthesis.
There is also an AT 2 receptor found in many tissues, but AT 2 is not known to be associated with cardiovascular homeostasis. Valsartan has much greater affinity (about 20,000-fold) for the AT 1 receptor than for the AT 2 receptor. The primary metabolite of valsartan is essentially inactive with an affinity for the AT 1 receptor about one 200th that of valsartan itself.
Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is widely used in the treatment of hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction also catalyzed by ACE. Because valsartan does not inhibit ACE (kininase II) it does not affect the response to bradykinin. Whether this difference has clinical relevance is not yet known. Valsartan does not bind to or block other hormone receptors or ion channels known to be important in cardiovascular regulation.
Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and angiotensin II circulating levels do not overcome the effect of valsartan on blood pressure.
Hydrochlorothiazide is a thiazide diuretic. Thiazides affect the renal tubular mechanisms of electrolyte reabsorption, directly increasing excretion of sodium and chloride in approximately equivalent amounts. Indirectly, the diuretic action of hydrochlorothiazide reduces plasma volume, with consequent increases in plasma renin activity, increases in aldosterone secretion, increases in urinary potassium loss, and decreases in serum potassium. The renin-aldosterone link is mediated by angiotensin II, so coadministration of an angiotensin II receptor antagonist tends to reverse the potassium loss associated with these diuretics.
The mechanism of the antihypertensive effect of thiazides is unknown.
12.2 Pharmacodynamics
Valsartan: Valsartan inhibits the pressor effect of angiotensin II infusions. An oral dose of 80 mg inhibits the pressor effect by about 80% at peak with approximately 30% inhibition persisting for 24 hours. No information on the effect of larger doses is available.
Removal of the negative feedback of angiotensin II causes a 2- to 3-fold rise in plasma renin and consequent rise in angiotensin II plasma concentration in hypertensive patients. Minimal decreases in plasma aldosterone were observed after administration of valsartan; very little effect on serum potassium was observed.
Hydrochlorothiazide: After oral administration of hydrochlorothiazide, diuresis begins within 2 hours, peaks in about 4 hours and lasts about 6 to 12 hours.
Drug Interactions
Hydrochlorothiazide:
Alcohol, barbiturates, or narcotics: Potentiation of orthostatic hypotension may occur.
Skeletal muscle relaxants: Possible increased responsiveness to muscle relaxants such as curare derivatives.
Digitalis glycosides: Thiazide-induced hypokalemia or hypomagnesemia may predispose the patient to digoxin toxicity.
12.3 Pharmacokinetics
Valsartan: Valsartan peak plasma concentration is reached 2 to 4 hours after dosing. Valsartan shows bi-exponential decay kinetics following intravenous administration, with an average elimination half-life of about 6 hours. Absolute bioavailability for the capsule formulation is about 25% (range 10%-35%). Food decreases the exposure (as measured by AUC) to valsartan by about 40% and peak plasma concentration (C max) by about 50%. AUC and C max values of valsartan increase approximately linearly with increasing dose over the clinical dosing range. Valsartan does not accumulate appreciably in plasma following repeated administration.
Hydrochlorothiazide: The estimated absolute bioavailability of hydrochlorothiazide after oral administration is about 70%. Peak plasma hydrochlorothiazide concentrations (C max) are reached within 2 to 5 hours after oral administration. There is no clinically significant effect of food on the bioavailability of hydrochlorothiazide.
Hydrochlorothiazide binds to albumin (40 to 70%) and distributes into erythrocytes. Following oral administration, plasma hydrochlorothiazide concentrations decline bi-exponentially, with a mean distribution half-life of about 2 hours and an elimination half-life of about 10 hours.
Valsartan and hydrochlorothiazide tablets: Valsartan and hydrochlorothiazide tablets may be administered with or without food.
Distribution
Valsartan: The steady state volume of distribution of valsartan after intravenous administration is small (17 L), indicating that valsartan does not distribute into tissues extensively. Valsartan is highly bound to serum proteins (95%), mainly serum albumin.
Metabolism
Valsartan: The primary metabolite, accounting for about 9% of dose, is valeryl 4-hydroxy valsartan. In vitro metabolism studies involving recombinant CYP 450 enzymes indicated that the CYP 2C9 isoenzyme is responsible for the formation of valeryl-4-hydroxy valsartan. Valsartan does not inhibit CYP 450 isozymes at clinically relevant concentrations. CYP 450 mediated drug interaction between valsartan and co-administered drugs are unlikely because of the low extent of metabolism.
Hydrochlorothiazide: Is not metabolized.
Excretion
Valsartan: Valsartan, when administered as an oral solution, is primarily recovered in feces (about 83% of dose) and urine (about 13% of dose). The recovery is mainly as unchanged drug, with only about 20% of dose recovered as metabolites.
Following intravenous administration, plasma clearance of valsartan is about 2 L/h and its renal clearance is 0.62 L/h (about 30% of total clearance).
Hydrochlorothiazide:
About 70% of an orally administered dose of hydrochlorothiazide is eliminated in the urine as unchanged drug.
Special Populations
Geriatric: Exposure (measured by AUC) to valsartan is higher by 70% and the half-life is longer by 35% in the elderly than in the young. A limited amount of data suggest that the systemic clearance of hydrochlorothiazide is reduced in both healthy and hypertensive elderly subjects compared to young healthy volunteers.
Gender: Pharmacokinetics of valsartan does not differ significantly between males and females.
Race: Pharmacokinetic differences due to race have not been studied.
Renal Insufficiency: There is no apparent correlation between renal function (measured by creatinine clearance) and exposure (measured by AUC) to valsartan in patients with different degrees of renal impairment. Valsartan has not been studied in patients with severe impairment of renal function (creatinine clearance <10 mL/min). Valsartan is not removed from the plasma by hemodialysis.
In a study in individuals with impaired renal function, the mean elimination half-life of hydrochlorothiazide was doubled in individuals with mild/moderate renal impairment (30 < CrCl < 90 mL/min) and tripled in severe renal impairment (≤ 30 mL/min), compared to individuals with normal renal function (CrCl > 90 mL/min) [see Use in Specific Populations ( 8.6)].
Hepatic Insufficiency: On average, patients with mild-to-moderate chronic liver disease have twice the exposure (measured by AUC values) to valsartan of healthy volunteers (matched by age, sex, and weight) [see Use in Specific Populations ( 8.7)].
Drug Interactions
Hydrochlorothiazide:
Drugs that alter gastrointestinal motility: The bioavailability of thiazide-type diuretics may be increased by anticholinergic agents (e.g. atropine, biperiden), apparently due to a decrease in gastrointestinal motility and the stomach emptying rate. Conversely, pro-kinetic drugs may decrease the bioavailability of thiazide diuretics.
Cholestyramine: In a dedicated drug interaction study, administration of cholestyramine 2 hours before hydrochlorothiazide resulted in a 70% reduction in exposure to hydrochlorothiazide. Further, administration of hydrochlorothiazide 2 hours before cholestyramine resulted in 35% reduction in exposure to hydrochlorothiazide.
Antineoplastic agents (e.g. cyclophosphamide, methotrexate): Concomitant use of thiazide diuretics may reduce renal excretion of cytotoxic agents and enhance their myelosuppressive effects. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Valsartan-Hydrochlorothiazide: No carcinogenicity, mutagenicity or fertility studies have been conducted with the combination of valsartan and hydrochlorothiazide. However, these studies have been conducted for valsartan as well as hydrochlorothiazide alone. Based on the preclinical safety and human pharmacokinetic studies, there is no indication of any adverse interaction between valsartan and hydrochlorothiazide.
Valsartan: There was no evidence of carcinogenicity when valsartan was administered in the diet to mice and rats for up to 2 years at doses up to 160 and 200 mg/kg/day, respectively. These doses in mice and rats are about 2.6 and 6 times, respectively, the MRHD on a mg/m 2 basis. (Calculations assume an oral dose of 320 mg/day and a 60-kg patient.)
Mutagenicity assays did not reveal any valsartan-related effects at either the gene or chromosome level. These assays included bacterial mutagenicity tests with Salmonella (Ames) and E. coli; a gene mutation test with Chinese hamster V79 cells; a cytogenetic test with Chinese hamster ovary cells; and a rat micronucleus test.
Valsartan had no adverse effects on the reproductive performance of male or female rats at oral doses up to 200 mg/kg/day. This dose is about 6 times the MRHD on a mg/m 2 basis. (Calculations assume an oral dose of 320 mg/day and a 60-kg patient.)
Hydrochlorothiazide: Two-year feeding studies in mice and rats conducted under the auspices of the National Toxicology Program (NTP) uncovered no evidence of a carcinogenic potential of hydrochlorothiazide in female mice (at doses of up to approximately 600 mg/kg/day) or in male and female rats (at doses of up to approximately 100 mg/kg/day). The NTP, however, found equivocal evidence for hepatocarcinogenicity in male mice.
Hydrochlorothiazide was not genotoxic in vitro in the Ames mutagenicity assay of Salmonella Typhimurium strains TA 98, TA 100, TA 1535, TA 1537, and TA 1538 and in the Chinese Hamster Ovary (CHO) test for chromosomal aberrations, or in vivo in assays using mouse germinal cell chromosomes, Chinese hamster bone marrow chromosomes, and the Drosophila sex-linked recessive lethal trait gene. Positive test results were obtained only in the in vitro CHO Sister Chromatid Exchange (clastogenicity) and in the Mouse Lymphoma Cell (mutagenicity) assays, using concentrations of hydrochlorothiazide from 43 to 1300 mcgm/mL, and in the Aspergillus Nidulans non-disjunction assay at an unspecified concentration.
Hydrochlorothiazide had no adverse effects on the fertility of mice and rats of either sex in studies wherein these species were exposed, via their diet, to doses of up to 100 and 4 mg/kg, respectively, prior to mating and throughout gestation. These doses of hydrochlorothiazide in mice and rats represent 19 and 1.5 times, respectively, the MRHD on a mg/m 2 basis. (Calculations assume an oral dose of 25 mg/day and a 60-kg patient.)
13.3 Developmental Toxicity Studies
Valsartan-Hydrochlorothiazide: There was no evidence of teratogenicity in mice, rats, or rabbits treated orally with valsartan at doses up to 600, 100 and 10 mg/kg/day, respectively, in combination with hydrochlorothiazide at doses up to 188, 31 and 3 mg/kg/day. These non-teratogenic doses in mice, rats and rabbits, respectively, represent 9, 3.5 and 0.5 times the MRHD of valsartan and 38, 13 and 2 times the MRHD of hydrochlorothiazide on a mg/m 2 basis. (Calculations assume an oral dose of 320 mg/day valsartan in combination with 25 mg/day hydrochlorothiazide and a 60-kg patient.)
Fetotoxicity was observed in association with maternal toxicity in rats and rabbits at valsartan doses of ≥200 and 10 mg/kg/day, respectively, in combination with hydrochlorothiazide doses of ≥63 and 3 mg/kg/day. Fetotoxicity in rats was considered to be related to decreased fetal weights and included fetal variations of sternebrae, vertebrae, ribs and/or renal papillae. Fetotoxicity in rabbits included increased numbers of late resorptions with resultant increases in total resorptions, postimplantation losses and decreased number of live fetuses. The no observed adverse effect doses in mice, rats and rabbits for valsartan were 600, 100 and 3 mg/kg/day, respectively, in combination with hydrochlorothiazide doses of 188, 31 and 1 mg/kg/day. These no adverse effect doses in mice, rats and rabbits, respectively, represent 9, 3 and 0.18 times the MRHD of valsartan and 38, 13 and 0.5 times the MRHD of hydrochlorothiazide on a mg/m 2 basis. (Calculations assume an oral dose of 320 mg/day valsartan in combination with 25 mg/day hydrochlorothiazide and a 60-kg patient.)
Valsartan: No teratogenic effects were observed when valsartan was administered to pregnant mice and rats at oral doses up to 600 mg/kg/day and to pregnant rabbits at oral doses up to 10 mg/kg/day. However, significant decreases in fetal weight, pup birth weight, pup survival rate, and slight delays in developmental milestones were observed in studies in which parental rats were treated with valsartan at oral, maternally toxic (reduction in body weight gain and food consumption) doses of 600 mg/kg/day during organogenesis or late gestation and lactation. In rabbits, fetotoxicity (i.e., resorptions, litter loss, abortions, and low body weight) associated with maternal toxicity (mortality) was observed at doses of 5 and 10 mg/kg/day. The no observed adverse effect doses of 600, 200 and 2 mg/kg/day in mice, rats and rabbits represent 9, 6 and 0.1 times, respectively, the MRHD on a mg/m 2 basis. (Calculations assume an oral dose of 320 mg/day and a 60-kg patient.)
Hydrochlorothiazide: Under the auspices of the National Toxicology Program, pregnant mice and rats that received hydrochlorothiazide via gavage at doses up to 3000 and 1000 mg/kg/day, respectively, on gestation days 6 through 15 showed no evidence of teratogenicity. These doses of hydrochlorothiazide in mice and rats represent 608 and 405 times, respectively, the MRHD on a mg/m 2 basis. (Calculations assume an oral dose of 25 mg/day and a 60-kg patient.)
-
14 CLINICAL STUDIES
14.1 Hypertension
Valsartan-Hydrochlorothiazide: In controlled clinical trials including over 7600 patients, 4372 patients were exposed to valsartan (80, 160 and 320 mg) and concomitant hydrochlorothiazide (12.5 and 25 mg). Two factorial trials compared various combinations of 80/12.5 mg, 80/25 mg, 160/12.5 mg, 160/25 mg, 320/12.5 mg and 320/25 mg with their respective components and placebo. The combination of valsartan and hydrochlorothiazide resulted in additive placebo-adjusted decreases in systolic and diastolic blood pressure at trough of 14-21/8-11 mmHg at 80/12.5 mg to 320/25 mg, compared to 7-10/4-5 mmHg for valsartan 80 mg to 320 mg and 5-11/2-5 mmHg for hydrochlorothiazide 12.5 mg to 25 mg, alone.
Three other controlled trials investigated the addition of hydrochlorothiazide to patients who did not respond adequately to valsartan 80 mg to valsartan 320 mg, resulted in the additional lowering of systolic and diastolic blood pressure by approximately 4-12/2-5 mmHg.
The maximal antihypertensive effect was attained 4 weeks after the initiation of therapy, the first time point at which blood pressure was measured in these trials.
In long-term follow-up studies (without placebo control) the effect of the combination of valsartan and hydrochlorothiazide appeared to be maintained for up to two years. The antihypertensive effect is independent of age or gender. The overall response to the combination was similar for black and non-black patients.
There was essentially no change in heart rate in patients treated with the combination of valsartan and hydrochlorothiazide in controlled trials.
There are no trials of the valsartan and hydrochlorothiazide combination tablet demonstrating reductions in cardiovascular risk in patients with hypertension, but the hydrochlorothiazide component and several ARBs, which are the same pharmacological class as the valsartan component, have demonstrated such benefits.
Valsartan: The antihypertensive effects of valsartan were demonstrated principally in 7 placebo-controlled, 4- to 12-week trials (one in patients over 65) of dosages from 10 to 320 mg/day in patients with baseline diastolic blood pressures of 95-115. The studies allowed comparison of once-daily and twice-daily regimens of 160 mg/day; comparison of peak and trough effects; comparison (in pooled data) of response by gender, age, and race; and evaluation of incremental effects of hydrochlorothiazide.
Administration of valsartan to patients with essential hypertension results in a significant reduction of sitting, supine, and standing systolic and diastolic blood pressure, usually with little or no orthostatic change.
In most patients, after administration of a single oral dose, onset of antihypertensive activity occurs at approximately 2 hours, and maximum reduction of blood pressure is achieved within 6 hours. The antihypertensive effect persists for 24 hours after dosing, but there is a decrease from peak effect at lower doses (40 mg) presumably reflecting loss of inhibition of angiotensin II. At higher doses, however (160 mg), there is little difference in peak and trough effect. During repeated dosing, the reduction in blood pressure with any dose is substantially present within 2 weeks, and maximal reduction is generally attained after 4 weeks. In long-term follow-up studies (without placebo control) the effect of valsartan appeared to be maintained for up to 2 years. The antihypertensive effect is independent of age, gender or race. The latter finding regarding race is based on pooled data and should be viewed with caution, because antihypertensive drugs that affect the renin-angiotensin system (that is, ACE inhibitors and angiotensin II blockers) have generally been found to be less effective in low-renin hypertensives (frequently blacks) than in high-renin hypertensives (frequently whites). In pooled, randomized, controlled trials of valsartan that included a total of 140 blacks and 830 whites, valsartan and an ACE-inhibitor control were generally at least as effective in blacks as whites. The explanation for this difference from previous findings is unclear.
Abrupt withdrawal of valsartan has not been associated with a rapid increase in blood pressure.
The 7 studies of valsartan monotherapy included over 2000 patients randomized to various doses of valsartan and about 800 patients randomized to placebo. Doses below 80 mg were not consistently distinguished from those of placebo at trough, but doses of 80, 160 and 320 mg produced dose-related decreases in systolic and diastolic blood pressure, with the difference from placebo of approximately 6-9/3-5 mmHg at 80-160 mg and 9/6 mmHg at 320 mg.
Patients with an inadequate response to 80 mg once daily were titrated to either 160 mg once daily or 80 mg twice daily, which resulted in a comparable response in both groups.
In another 4-week study, 1876 patients randomized to valsartan 320 mg once daily had an incremental blood pressure reduction 3/1 mmHg lower than did 1900 patients randomized to valsartan 160 mg once daily.
In controlled trials, the antihypertensive effect of once daily valsartan 80 mg was similar to that of once daily enalapril 20 mg or once daily lisinopril 10 mg.
There was essentially no change in heart rate in valsartan-treated patients in controlled trials.
14.2 Initial Therapy - Hypertension
The safety and efficacy of valsartan and hydrochlorothiazide tablets as initial therapy for patients with severe hypertension (defined as a sitting diastolic blood pressure ≥110 mmHg and systolic blood pressure ≥140 mmHg off all antihypertensive therapy) was studied in a 6-week multicenter, randomized, double-blind study. Patients were randomized to either valsartan and hydrochlorothiazide tablets (valsartan and hydrochlorothiazide 160/12.5 mg once daily) or to valsartan (160 mg once daily) and followed for blood pressure response. Patients were force-titrated at 2-week intervals. Patients on combination therapy were subsequently titrated to 160/25 mg followed by 320/25 mg valsartan/hydrochlorothiazide. Patients on monotherapy were subsequently titrated to 320 mg valsartan followed by a titration to 320 mg valsartan to maintain the blind.
The study randomized 608 patients, including 261 (43%) females, 147 (24%) blacks, and 75 (12%) ≥65 years of age. The mean blood pressure at baseline for the total population was 168/112 mmHg. The mean age was 52 years. After 4 weeks of therapy, reductions in systolic and diastolic blood pressure were 9/5 mmHg greater in the group treated with valsartan and hydrochlorothiazide tablets compared to valsartan. Similar trends were seen when the patients were grouped according to gender, race or age.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Valsartan and hydrochlorothiazide tablets, USP, are available as non-scored tablets containing valsartan/hydrochlorothiazide 80/12.5 mg, 160/12.5 mg, 160/25 mg, 320/12.5 mg and 320/25 mg. Strengths are available as follows.
80/12.5 mg Tablet - Light orange, oval shaped biconvex film coated tablets debossed with "L16" on side and plain on other side.
Bottles of 90 NDC: 33342-074-10
Bottles of 1000 NDC: 33342-074-44
160/12.5 mg Tablet - Dark red, oval shaped biconvex film coated tablets debossed with "L17" on side and plain on other side.
Bottles of 90 NDC: 33342-075-10
Bottles of 500 NDC: 33342-075-15
160/25 mg Tablet - Brown orange, oval shaped biconvex film coated tablets debossed with "L18" on side and plain on other side.
Bottles of 90 NDC: 33342-076-10
Bottles of 500 NDC: 33342-076-15
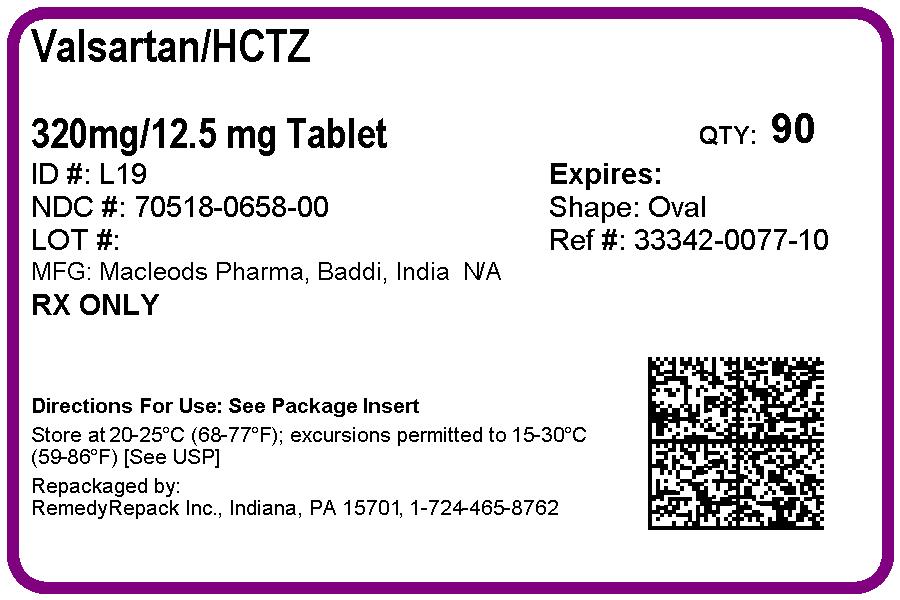
320/12.5 mg Tablet - Pink, oval shaped biconvex film coated tablets debossed with "L19" on side and plain on other side.
Bottles of 90 NDC: 33342-077-10
Bottles of 500 NDC: 33342-077-15
320/25 mg Tablet - Yellow, oval shaped biconvex film coated tablets debossed with "L20" on side and plain on other side.
Bottles of 90 NDC: 33342-078-10
Bottles of 500 NDC: 33342-078-15
Store at 20º to 25ºC (68º to 77ºF); excursions permitted to 15º to 30ºC (59º to 86ºF) [see USP Controlled Room Temperature].
Protect from moisture
Dispense in tight container (USP).
-
17 PATIENT COUNSELING INFORMATION
Information for Patients
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Pregnancy: Female patients of childbearing age should be told about the consequences of exposure to valsartan and hydrochlorothiazide tablets during pregnancy. Discuss treatment options with women planning to become pregnant. Patients should be asked to report pregnancies to their physicians as soon as possible.
Symptomatic Hypotension: A patient receiving valsartan and hydrochlorothiazide tablets should be cautioned that lightheadedness can occur, especially during the first days of therapy, and that it should be reported to the prescribing physician. The patients should be told that if syncope occurs, valsartan and hydrochlorothiazide tablets should be discontinued until the physician has been consulted.
All patients should be cautioned that inadequate fluid intake, excessive perspiration, diarrhea, or vomiting can lead to an excessive fall in blood pressure, with the same consequences of lightheadedness and possible syncope.
Potassium Supplements: A patient receiving valsartan and hydrochlorothiazide tablets should be told not to use potassium supplements or salt substitutes containing potassium without consulting the prescribing physician.
Manufactured for:
Macleods Pharma USA, Inc.,
Plainsboro, NJ 08536Manufactured by:
Macleods Pharmaceutical Limited
Daman (U.T.) INDIA
OR
Manufactured by :
Macleods Pharmaceuticals Ltd.
Baddi, Himachal Pradesh, INDIARevised: 05/2016
PM01467304
OR
PM02216401
FDA-Approved Patient Labeling
PATIENT INFORMATION
Valsartan and Hydrochlorothiazide Tablets, USP
(val sar' tan and hye'' droe klor'' oh thye' a zide)
Read the Patient Information that comes with valsartan and hydrochlorothiazide tablets before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your doctor about your condition and treatment. If you have any questions about valsartan and hydrochlorothiazide tablets, ask your doctor or pharmacist.
What is the most important information I should know about valsartan and hydrochlorothiazide tablets?
Valsartan and hydrochlorothiazide tablets can cause harm or death to an unborn baby. Talk to your doctor about other ways to lower your blood pressure if you plan to become pregnant. If you get pregnant while taking valsartan and hydrochlorothiazide tablets, tell your doctor right away.
What are Valsartan and hydrochlorothiazide tablets?
Valsartan and hydrochlorothiazide tablets contain 2 prescription medicines:
1. valsartan, an angiotensin receptor blocker (ARB)
2. hydrochlorothiazide (HCTZ), a water pill (diuretic)
Valsartan and hydrochlorothiazide tablets may be used to lower high blood pressure (hypertension) in adults-
when 1 medicine to lower your high blood pressure is not enough
as the first medicine to lower high blood pressure if your doctor decides you are likely to need more than 1 medicine.
Valsartan and hydrochlorothiazide tablets have not been studied in children under 18 years of age.
Who should not take valsartan and hydrochlorothiazide tablets?
Do not take valsartan and hydrochlorothiazide tablets if you:
are allergic to any of the ingredients in valsartan and hydrochlorothiazide tablets. See the end of this leaflet for a complete list of ingredients in valsartan and hydrochlorothiazide tablets.
make less urine due to kidney problems
are allergic to medicines that contain sulfonamides
What should I tell my doctor before taking valsartan and hydrochlorothiazide tablets?
Tell your doctor about all your medical conditions including if you:
are pregnant or plan to become pregnant. See "What is the most important information I should know about valsartan and hydrochlorothiazide tablets?"
are breastfeeding. Valsartan and hydrochlorothiazide passes into breast milk. You should choose either to take valsartan and hydrochlorothiazide tablets or breastfeed, but not both.
have liver problems
have kidney problems
have or had gallstones
have Lupus
have low levels of potassium (with or without symptoms such as muscle weakness, muscle spasms, abnormal heart rhythm) or magnesium in your blood
have high levels of calcium in your blood (with or without symptoms such as nausea, vomiting, constipation, stomach pain, frequent urination, thirst, muscle weakness and twitching).
have high levels of uric acid in the blood.
have ever had a reaction called angioedema, to another blood pressure medication. Angioedema causes swelling of the face, lips, tongue, throat and may cause difficulty breathing.
Tell your doctor about all the medicines you take including prescription and nonprescription medicines, vitamins and herbal supplements. Some of your other medicines and valsartan and hydrochlorothiazide tablets could affect each other, causing serious side effects. Especially, tell your doctor if you take:
other medicines for high blood pressure or a heart problem
water pills (diuretics)
potassium supplements. Your doctor may check the amount of potassium in your blood periodically.
a salt substitute. Your doctor may check the amount of potassium in your blood periodically.
antidiabetic medicines including insulin
narcotic pain medicines
sleeping pills
lithium, a medicine used in some types of depression (Eskalith ®, Lithobid ®, Lithium Carbonate, Lithium Citrate)
aspirin or other medicines called non-steroidal anti-inflammatory Drugs (NSAIDs), like ibuprofen or naproxen
digoxin or other digitalis glycosides (a heart medicine)
muscle relaxants (medicines used during operations)
certain cancer medicines, like cyclophosphamide or methotrexate
certain antibiotics (rifamycin group), a drug used to protect against transplant rejection (cyclosporin) or an antiretroviral drug used to treat HIV/AIDS infection (ritonavir). These drugs may increase the effect of valsartan.
Ask your doctor if you are not sure if you are taking 1 of these medicines.
Know the medicines you take. Keep a list of your medicines with you to show to your doctor and pharmacist when a new medicine is prescribed. Talk to your doctor or pharmacist before you start taking any new medicine. Your doctor or pharmacist will know what medicines are safe to take together.
How should I take valsartan and hydrochlorothiazide tablets?
Take valsartan and hydrochlorothiazide tablets exactly as prescribed by your doctor. Your doctor may change your dose if needed.
Take valsartan and hydrochlorothiazide tablets once each day.
Valsartan and hydrochlorothiazide tablets can be taken with or without food.
If you miss a dose, take it as soon as you remember. If it is close to your next dose, do not take the missed dose. Just take the next dose at your regular time.
If you take too much valsartan and hydrochlorothiazide tablets, call your doctor or Poison Control Center, or go to the nearest hospital emergency room.
What should I avoid while taking valsartan and hydrochlorothiazide tablets?
You should not take valsartan and hydrochlorothiazide tablets during pregnancy. See "What is the most important information I should know about valsartan and hydrochlorothiazide tablets?"
What are the possible side effects of valsartan and hydrochlorothiazide tablets?
Valsartan and hydrochlorothiazide tablets may cause serious side effects including:
Harm to an unborn baby causing injury and even death. See "What is the most important information I should know about valsartan and hydrochlorothiazide tablets?"
Low blood pressure (hypotension). Low blood pressure is most likely to happen if you:
o take water pills
o are on a low salt diet
o get dialysis treatments
o have heart problems
o get sick with vomiting or diarrhea
o drink alcohol
Lie down if you feel faint or dizzy. Call your doctor right away.
Allergic reactions. People with and without allergy problems or asthma who take valsartan and hydrochlorothiazide tablets may get allergic reactions.
Worsening of Lupus. Hydrochlorothiazide, 1 of the medicines in valsartan and hydrochlorothiazide tablets may cause Lupus to become active or worse.
Fluid and electrolyte (salt) problems. Tell your doctor about any of the following signs and symptoms of fluid and electrolyte problems:
dry mouth
thirst
lack of energy (lethargic)
weakness
drowsiness
restlessness
confusion
seizures
muscle pain or cramps
muscle fatigue
very low urine output
fast heartbeat
nausea and vomiting
Kidney problems. Kidney problems may become worse in people that already have kidney disease. Some people will have changes on blood tests for kidney function and may need a lower dose of valsartan and hydrochlorothiazide tablets. Call your doctor if you get swelling in your feet, ankles, or hands, or unexplained weight gain. If you have heart failure, your doctor should check your kidney function before prescribing valsartan and hydrochlorothiazide tablets.
Skin rash. Call your doctor right away if you have an unusual skin rash.
Eye Problems. One of the medicines in valsartan and hydrochlorothiazide tablets can cause eye problems that may lead to vision loss. Symptoms of eye problems can happen within hours to weeks of starting valsartan and hydrochlorothiazide tablets. Tell your doctor right away if you have:
decrease in vision
eye pain
Other side effects were generally mild and brief. They generally have not caused patients to stop taking valsartan and hydrochlorothiazide tablets.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of valsartan and hydrochlorothiazide tablets. For a complete list, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How do I store valsartan and hydrochlorothiazide tablets?
Store valsartan and hydrochlorothiazide tablets at room temperature between 59ºF to 86ºF (15ºC to 30ºC).
Keep valsartan and hydrochlorothiazide tablets in a closed container in a dry place.
Keep valsartan and hydrochlorothiazide tablets and all medicines out of the reach of children.
General information about valsartan and hydrochlorothiazide tablets
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use valsartan and hydrochlorothiazide tablets for a condition for which it was not prescribed. Do not give valsartan and hydrochlorothiazide tablets to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about valsartan and hydrochlorothiazide tablets. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about valsartan and hydrochlorothiazide tablets that is written for health professionals. For more information about valsartan and hydrochlorothiazide tablets, call 1-888-943-3210.
What are the ingredients in valsartan and hydrochlorothiazide tablets?
Active ingredients: Valsartan and hydrochlorothiazide
Inactive ingredients: colloidal silicon dioxide, crospovidone, hydroxypropyl methylcellulose, iron oxides, magnesium stearate, microcrystalline cellulose, polyethylene glycol, talc, and titanium dioxide.
What is high blood pressure (hypertension)?
Blood pressure is the force in your blood vessels when your heart beats and when your heart rests. You have high blood pressure when the force is too much. Valsartan and hydrochlorothiazide tablets can help your blood vessels relax and reduce the amount of water in your body so your blood pressure is lower. Medicines that lower blood pressure lower your risk of having a stroke or heart attack.
High blood pressure makes the heart work harder to pump blood throughout the body and causes damage to the blood vessels. If high blood pressure is not treated, it can lead to stroke, heart attack, heart failure, kidney failure, and vision problems.
Eskalith ® and Lithobid ® are registered trademarks of Noven Pharmaceuticals, Inc
Manufactured for:
Macleods Pharma USA, Inc.,
Plainsboro, NJ 08536Manufactured by:
Macleods Pharmaceutical Limited
Daman (U.T.) INDIAOR
Manufactured by :
Macleods Pharmaceuticals Ltd.
Baddi, Himachal Pradesh, INDIARevised: 05/2016
PM01467304
OR
PM02216401 - SPL PATIENT PACKAGE INSERT
-
PRINCIPAL DISPLAY PANEL
DRUG: Valsartan and Hydrochlorothiazide
GENERIC: Valsartan and Hydrochlorothiazide
DOSAGE: TABLET, FILM COATED
ADMINSTRATION: ORAL
NDC: 70518-0658-0
COLOR: pink
SHAPE: OVAL
SCORE: No score
SIZE: 21 mm
IMPRINT: L19
PACKAGING: 90 in 1 BOTTLE, PLASTIC
ACTIVE INGREDIENT(S):
- HYDROCHLOROTHIAZIDE 12.5mg in 1
- VALSARTAN 320mg in 1
INACTIVE INGREDIENT(S):
- FERRIC OXIDE RED
- TITANIUM DIOXIDE
- HYPROMELLOSES
- FERROSOFERRIC OXIDE
- TALC
- CROSPOVIDONE
- MAGNESIUM STEARATE
- POLYETHYLENE GLYCOLS
- CELLULOSE, MICROCRYSTALLINE
- SILICON DIOXIDE
-
INGREDIENTS AND APPEARANCE
VALSARTAN AND HYDROCHLOROTHIAZIDE
valsartan and hydrochlorothiazide tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 70518-0658(NDC:33342-077) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength VALSARTAN (UNII: 80M03YXJ7I) (VALSARTAN - UNII:80M03YXJ7I) VALSARTAN 320 mg HYDROCHLOROTHIAZIDE (UNII: 0J48LPH2TH) (HYDROCHLOROTHIAZIDE - UNII:0J48LPH2TH) HYDROCHLOROTHIAZIDE 12.5 mg Inactive Ingredients Ingredient Name Strength FERRIC OXIDE RED (UNII: 1K09F3G675) CROSPOVIDONE (UNII: 68401960MK) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) HYPROMELLOSES (UNII: 3NXW29V3WO) FERROSOFERRIC OXIDE (UNII: XM0M87F357) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color pink Score no score Shape OVAL (Biconvex) Size 21mm Flavor Imprint Code L19 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 70518-0658-0 90 in 1 BOTTLE, PLASTIC; Type 0: Not a Combination Product 08/01/2017 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA203145 08/01/2017 Labeler - REMEDYREPACK INC. (829572556)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.