EMTRIVA- emtricitabine capsule
Emtriva by
Drug Labeling and Warnings
Emtriva by is a Prescription medication manufactured, distributed, or labeled by Excella GmbH. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use EMTRIVA safely and effectively. See full prescribing information for EMTRIVA.
EMTRIVA (emtricitabine) capsule for oral use
EMTRIVA (emtricitabine) solution for oral use
Initial U.S. Approval: 2003WARNINGS: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH STEATOSIS and POST TREATMENT EXACERBATION OF HEPATITIS B
See full prescribing information for complete boxed warning.
- Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogs. (5.1)
- Emtriva is not approved for the treatment of chronic Hepatitis B virus (HBV) infection. Severe acute exacerbations of Hepatitis B have been reported in patients who have discontinued EMTRIVA. Hepatic function should be monitored closely in patients coinfected with HIV-1 and HBV. If appropriate, initiation of anti-Hepatitis B therapy may be warranted. (5.2)
INDICATIONS AND USAGE
EMTRIVA, a nucleoside analog HIV-1 reverse transcriptase inhibitor, is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection. (1)
DOSAGE AND ADMINISTRATION
- EMTRIVA may be taken without regard to food. (2.1)
- Adult Patients (18 years of age and older) (2.2):
- EMTRIVA capsules: one 200 mg capsule administered once daily orally.
- EMTRIVA oral solution: 240 mg (24 mL) administered once daily orally.
- Pediatric Patients (0–3 months of age) (2.3):
- EMTRIVA oral solution: 3 mg/kg administered once daily orally.
- Pediatric Patients (3 months through 17 years) (2.4):
- EMTRIVA oral solution: 6 mg/kg up to a maximum of 240 mg (24 mL) administered once daily orally.
- EMTRIVA capsules: for children weighing more than 33 kg who can swallow an intact capsule, one 200 mg capsule administered once daily orally.
- Dose interval adjustment in adult patients with renal impairment (2.5):
Creatinine Clearance (mL/min) Formulation ≥50
mL/min30–49
mL/min15–29
mL/min<15 mL/min
or on hemodialysis*- * Hemodialysis Patients: If dosing on day of dialysis, give dose after dialysis.
Capsule
(200 mg)200 mg every
24 hours200 mg every
48 hours200 mg every
72 hours200 mg
every 96 hoursOral Solution
(10 mg/mL)240 mg every
24 hours
(24 mL)120 mg every
24 hours
(12 mL)80 mg every
24 hours
(8 mL)60 mg every
24 hours
(6 mL)CONTRAINDICATIONS
EMTRIVA is contraindicated in patients with previously demonstrated hypersensitivity to any of the components of the products. (4)
WARNINGS AND PRECAUTIONS
- Products with same active ingredient: Do not use with other emtricitabine-containing products (e.g., ATRIPLA and TRUVADA). (5.3)
- Redistribution/accumulation of body fat: Observed in patients receiving antiretroviral therapy. (5.5)
- Immune reconstitution syndrome: May necessitate further evaluation and treatment. (5.6)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥10%) are headache, diarrhea, nausea, fatigue, dizziness, depression, insomnia, abnormal dreams, rash, abdominal pain, asthenia, increased cough, and rhinitis. Skin hyperpigmentation was very common (≥10%) in pediatric patients. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Gilead Sciences, Inc. at 1-800-GILEAD-5 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2009
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNINGS: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH STEATOSIS and POST TREATMENT EXACERBATION OF HEPATITIS B
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose
2.2 Adult Patients (18 years of age and older)
2.3 Pediatric Patients (0–3 months of age)
2.4 Pediatric Patients (3 months through 17 years)
2.5 Dose Adjustment in Adult Patients with Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Lactic Acidosis/Severe Hepatomegaly with Steatosis
5.2 Patients Coinfected with HIV-1 and HBV
5.3 Coadministration with Related Products
5.4 New Onset or Worsening Renal Impairment
5.5 Fat Redistribution
5.6 Immune Reconstitution Syndrome
6 ADVERSE REACTIONS
6.1 Adverse Reactions from Clinical Trials Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients with Impaired Renal Function
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Treatment-Naive Adult Patients
14.2 Treatment-Experienced Adult Patients
14.3 Pediatric Patients
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Information for Patients
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNINGS: LACTIC ACIDOSIS/SEVERE HEPATOMEGALY WITH STEATOSIS and POST TREATMENT EXACERBATION OF HEPATITIS B
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogs alone or in combination with other antiretrovirals [See Warnings and Precautions (5.1)].
EMTRIVA is not approved for the treatment of chronic hepatitis B virus (HBV) infection and the safety and efficacy of EMTRIVA have not been established in patients coinfected with HBV and HIV-1. Severe acute exacerbations of hepatitis B have been reported in patients who have discontinued EMTRIVA. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who are coinfected with HIV-1 and HBV and discontinue EMTRIVA. If appropriate, initiation of anti-hepatitis B therapy may be warranted [See Warnings and Precautions (5.2)].
-
1 INDICATIONS AND USAGE
EMTRIVA® is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection.
Additional important information regarding the use of EMTRIVA for the treatment of HIV-1 Infection:
- EMTRIVA should not be coadministered with ATRIPLA®, TRUVADA®, or lamivudine-containing products [See Warnings and Precautions (5.3)].
- In treatment-experienced patients, the use of EMTRIVA should be guided by laboratory testing and treatment history [See Clinical Pharmacology (12.4)].
-
2 DOSAGE AND ADMINISTRATION
2.2 Adult Patients (18 years of age and older)
- EMTRIVA capsules: one 200 mg capsule administered once daily orally.
- EMTRIVA oral solution: 240 mg (24 mL) administered once daily orally.
2.3 Pediatric Patients (0–3 months of age)
- EMTRIVA oral solution: 3 mg/kg administered once daily orally.
2.4 Pediatric Patients (3 months through 17 years)
- EMTRIVA oral solution: 6 mg/kg up to a maximum of 240 mg (24 mL) administered once daily orally.
- EMTRIVA capsules: for children weighing more than 33 kg who can swallow an intact capsule, one 200 mg capsule administered once daily orally.
2.5 Dose Adjustment in Adult Patients with Renal Impairment
Significantly increased drug exposures were seen when EMTRIVA was administered to patients with renal impairment [See Clinical Pharmacology (12.3)]. Therefore, the dosing interval or dose of EMTRIVA should be adjusted in patients with baseline creatinine clearance <50 mL/min using the following guidelines (see Table 1). The safety and effectiveness of these dose adjustment guidelines have not been clinically evaluated. Therefore, clinical response to treatment and renal function should be closely monitored in these patients.
Table 1 Dose Adjustment in Adult Patients with Renal Impairment Creatinine Clearance (mL/min) Formulation ≥50 mL/min 30–49 mL/min 15–29 mL/min <15 mL/min
or on hemodialysis*- * Hemodialysis Patients: If dosing on day of dialysis, give dose after dialysis
Capsule
(200 mg)200 mg every
24 hours200 mg every
48 hours200 mg every
72 hours200 mg
every
96 hoursOral Solution
(10 mg/mL)240 mg every
24 hours
(24 mL)120 mg every
24 hours
(12 mL)80 mg every
24 hours
(8 mL)60 mg every
24 hours
(6 mL)Although there are insufficient data to recommend a specific dose adjustment of EMTRIVA in pediatric patients with renal impairment, a reduction in the dose and/or an increase in the dosing interval similar to adjustments for adults should be considered.
-
3 DOSAGE FORMS AND STRENGTHS
EMTRIVA is available as capsules and oral solution.
EMTRIVA capsules, containing 200 mg of emtricitabine, are size 1 hard gelatin capsules with a blue cap and white body, printed with "200 mg" in black on the cap and "GILEAD" and the corporate logo in black on the body.
EMTRIVA oral solution is a clear, orange to dark orange liquid containing 10 mg of emtricitabine per mL.
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Lactic Acidosis/Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogs alone or in combination, including emtricitabine and other antiretrovirals. A majority of these cases have been in women. Obesity and prolonged nucleoside exposure may be risk factors. Particular caution should be exercised when administering nucleoside analogs to any patient with known risk factors for liver diseases; however, cases have also been reported in patients with no known risk factors. Treatment with EMTRIVA should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
5.2 Patients Coinfected with HIV-1 and HBV
It is recommended that all patients with HIV-1 be tested for the presence of chronic Hepatitis B virus (HBV) before initiating antiretroviral therapy. EMTRIVA is not approved for the treatment of chronic HBV infection and the safety and efficacy of EMTRIVA have not been established in patients coinfected with HBV and HIV-1. Severe acute exacerbations of Hepatitis B have been reported in patients after the discontinuation of EMTRIVA. In some patients infected with HBV and treated with EMTRIVA, the exacerbations of hepatitis B were associated with liver decompensation and liver failure. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who are coinfected with HIV-1 and HBV and discontinue EMTRIVA. If appropriate, initiation of anti-Hepatitis B therapy may be warranted.
5.3 Coadministration with Related Products
EMTRIVA is a component of TRUVADA (a fixed-dose combination of emtricitabine and tenofovir disoproxil fumarate) and ATRIPLA (a fixed-dose combination of efavirenz, emtricitabine, and tenofovir disoproxil fumarate). EMTRIVA should not be coadministered with TRUVADA or ATRIPLA. Due to similarities between emtricitabine and lamivudine, EMTRIVA should not be coadministered with other drugs containing lamivudine, including Combivir (lamivudine/zidovudine), Epivir or Epivir-HBV (lamivudine), Epzicom (abacavir sulfate/lamivudine), or Trizivir (abacavir sulfate/lamivudine/zidovudine).
5.4 New Onset or Worsening Renal Impairment
Emtricitabine is principally eliminated by the kidney. Reduction of the dosage of EMTRIVA is recommended for patients with impaired renal function [See Dosage and Administration (2.5) and Clinical Pharmacology (12.3)].
5.5 Fat Redistribution
Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and "cushingoid appearance" have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
5.6 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including EMTRIVA. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections [such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia (PCP), or tuberculosis], which may necessitate further evaluation and treatment.
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in other sections of the labeling:
- Lactic acidosis/severe hepatomegaly with steatosis [See Boxed Warning, Warnings and Precautions (5.1)].
- Severe acute exacerbations of Hepatitis B [See Boxed Warning, Warnings and Precautions (5.2)].
- Immune reconstitution syndrome [See Warnings and Precautions (5.6)]
6.1 Adverse Reactions from Clinical Trials Experience
Adult Patients
More than 2,000 adult patients with HIV-1 infection have been treated with EMTRIVA alone or in combination with other antiretroviral agents for periods of 10 days to 200 weeks in clinical trials.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The most common adverse reactions (incidence ≥10%, any severity) identified from any of the 3 large controlled clinical trials include headache, diarrhea nausea, fatigue, dizziness, depression, insomnia, abnormal dreams, rash, abdominal pain, asthenia, increased cough, and rhinitis.
Studies 301A and 303 - Treatment Emergent Adverse Reactions: The most common adverse reactions that occurred in patients receiving EMTRIVA with other antiretroviral agents in clinical studies 301A and 303 were headache, diarrhea, nausea, and rash, which were generally of mild to moderate severity. Approximately 1% of patients discontinued participation in the clinical studies due to these events. All adverse reactions were reported with similar frequency in EMTRIVA and control treatment groups with the exception of skin discoloration which was reported with higher frequency in the EMTRIVA treated group.
Skin discoloration, manifested by hyperpigmentation on the palms and/or soles was generally mild and asymptomatic. The mechanism and clinical significance are unknown.
A summary of EMTRIVA treatment emergent clinical adverse reactions in studies 301A and 303 is provided in Table 2.
Table 2 Selected Treatment-Emergent Adverse Reactions (All Grades, Regardless of Causality) Reported in ≥3% of EMTRIVA-Treated Patients in Either Study 301A or 303 (0–48 Weeks) 303 301A EMTRIVA
+ ZDV/d4T
+ NNRTI/PI
(N=294)Lamivudine
+ ZDV/d4T
+ NNRTI/PI
(N=146)EMTRIVA
+ didanosine + efavirenz
(N=286)Stavudine
+ didanosine
+ efavirenz
(N=285)- * Rash event includes rash, pruritus, maculopapular rash, urticaria, vesiculobullous rash, pustular rash, and allergic reaction.
Body as a Whole Abdominal pain 8% 11% 14% 17% Asthenia 16% 10% 12% 17% Headache 13% 6% 22% 25% Digestive System Diarrhea 23% 18% 23% 32% Dyspepsia 4% 5% 8% 12% Nausea 18% 12% 13% 23% Vomiting 9% 7% 9% 12% Musculoskeletal Arthralgia 3% 4% 5% 6% Myalgia 4% 4% 6% 3% Nervous System Abnormal dreams 2% <1% 11% 19% Depressive disorders 6% 10% 9% 13% Dizziness 4% 5% 25% 26% Insomnia 7% 3% 16% 21% Neuropathy/peripheral neuritis 4% 3% 4% 13% Paresthesia 5% 7% 6% 12% Respiratory Increased cough 14% 11% 14% 8% Rhinitis 18% 12% 12% 10% Skin Rash event* 17% 14% 30% 33% Studies 301A and 303 - Laboratory Abnormalities:
Laboratory abnormalities in these studies occurred with similar frequency in the EMTRIVA and comparator groups. A summary of Grade 3 and 4 laboratory abnormalities is provided in Table 3 below.
Table 3 Treatment-Emergent Grade 3/4 Laboratory Abnormalities Reported in ≥1% of EMTRIVA-Treated Patients in Either Study 301A or 303 303 301A EMTRIVA
+ ZDV/d4T
+ NNRTI/PI
(N=294)Lamivudine
+ ZDV/d4T
+ NNRTI/PI
(N=146)EMTRIVA
+ Didanosine
+ Efavirenz
(N=286)Stavudine
+ Didanosine
+ Efavirenz
(N=285)- * ULN = Upper limit of normal
Percentage with grade 3 or grade 4 laboratory abnormality 31% 28% 34% 38% ALT (>5.0 × ULN*) 2% 1% 5% 6% AST (>5.0 × ULN) 3% <1% 6% 9% Bilirubin (>2.5 × ULN) 1% 2% <1% <1% Creatine kinase
(>4.0 × ULN)11% 14% 12% 11% Neutrophils (<750 mm3) 5% 3% 5% 7% Pancreatic amylase
(>2.0 × ULN)2% 2% <1% 1% Serum amylase
(>2.0 × ULN)2% 2% 5% 10% Serum glucose
<40 or >250 mg/dL)3% 3% 2% 3% Serum lipase
(>2.0 × ULN)<1% <1% 1% 2% Triglycerides
(>750 mg/dL)10% 8% 9% 6% Study 934 - Treatment Emergent Adverse Reactions: In Study 934, 511 antiretroviral-naïve patients received either VIREAD + EMTRIVA administered in combination with efavirenz (N=257) or zidovudine/lamivudine administered in combination with efavirenz (N=254). Adverse reactions observed in this study were generally consistent with those seen in previous studies in treatment-experienced or treatment-naïve patients (Table 4).
Table 4 Selected Treatment-Emergent Adverse Reactions* (Grades 2–4) Reported in ≥5% in Any Treatment Group in Study 934 (0–144 Weeks) TDF† + EMTRIVA + EFV AZT/3TC + EFV N=257 N=254 - * Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
- † From Weeks 96 to 144 of the study, patients received TRUVADA with efavirenz in place of VIREAD + EMTRIVA with efavirenz.
- ‡ Rash event includes rash, exfoliative rash, rash generalized, rash macular, rash maculo-papular, rash pruritic, and rash vesicular.
Gastrointestinal Disorder Diarrhea 9% 5% Nausea 9% 7% Vomiting 2% 5% General Disorders and Administration Site Condition Fatigue 9% 8% Infections and Infestations Sinusitis 8% 4% Upper respiratory tract infections 8% 5% Nasopharyngitis 5% 3% Nervous System Disorders Headache 6% 5% Dizziness 8% 7% Psychiatric Disorders Depression 9% 7% Insomnia 5% 7% Skin and Subcutaneous Tissue Disorders Rash event‡ 7% 9% Study 934 – Laboratory Abnormalities: Significant laboratory abnormalities observed in this study are shown in Table 5.
Table 5 Significant Laboratory Abnormalities Reported in ≥1% of Patients in Any Treatment Group in Study 934 (0–144 Weeks) TDF* + EMTRIVA + EFV AZT/3TC + EFV N=257 N=254 - * From Weeks 96 to 144 of the study, patients received TRUVADA with efavirenz in place of VIREAD + EMTRIVA with efavirenz.
Any ≥ Grade 3 Laboratory Abnormality 30% 26% Fasting Cholesterol (>240 mg/dL) 22% 24% Creatine Kinase
(M: >990 U/L)
(F: >845 U/L)9% 7% Serum Amylase (>175 U/L) 8% 4% Alkaline Phosphatase (>550 U/L) 1% 0% AST
(M: >180 U/L)
(F: >170 U/L)3% 3% ALT
(M: >215 U/L)
(F: >170 U/L)2% 3% Hemoglobin (<8.0 mg/dL) 0% 4% Hyperglycemia (>250 mg/dL) 2% 1% Hematuria (>75 RBC/HPF) 3% 2% Glycosuria (3+) <1% 1% Neutrophils (<750/mm3) 3% 5% Fasting Triglycerides (>750 mg/dL) 4% 2% Pediatric Patients
Assessment of adverse reactions is based on data from Study 203, an open label, uncontrolled study of 116 HIV-1-infected pediatric patients who received emtricitabine through 48 weeks. The adverse reaction profile in pediatric patients was generally comparable to that observed in clinical studies of EMTRIVA in adult patients [See Adverse Reactions (6.1)]. Hyperpigmentation was more frequent in children. Additional adverse reactions identified from this study include anemia.
Selected treatment-emergent adverse events, regardless of causality, reported in patients during 48 weeks of treatment were the following: infection (44%), hyperpigmentation (32%), increased cough (28%), vomiting (23%), otitis media (23%), rash (21%), rhinitis (20%), diarrhea (20%), fever (18%), pneumonia (15%), gastroenteritis (11%), abdominal pain (10%), and anemia (7%). Treatment-emergent grade 3/4 laboratory abnormalities were experienced by 9% of pediatric patients, including amylase >2.0 × ULN (n=4), neutrophils <750/mm3 (n=3), ALT >5 × ULN (n=2), elevated CPK (>4 × ULN) (n=2) and one patient each with elevated bilirubin (>3.0 × ULN), elevated GGT (>10 × ULN), elevated lipase (>2.5 × ULN), decreased hemoglobin (<7 g/dL), and decreased glucose (<40 mg/dL).
-
7 DRUG INTERACTIONS
The potential for drug interactions with EMTRIVA has been studied in combination with zidovudine, indinavir, stavudine, famciclovir, and tenofovir disoproxil fumarate. There were no clinically significant drug interactions for any of these drugs Drug interactions studies are described elsewhere in the labeling [See Clinical Pharmacology (12.3)]
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B
The incidence of fetal variations and malformations was not increased in embryofetal toxicity studies performed with emtricitabine in mice at exposures (AUC) approximately 60-fold higher and in rabbits at approximately 120-fold higher than human exposures at the recommended daily dose. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, EMTRIVA should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Nursing Mothers: The Centers for Disease Control and Prevention recommend that HIV-1-infected mothers not breast-feed their infants to avoid risking postnatal transmission of HIV-1. It is not known whether emtricitabine is excreted in human milk. Because of both the potential for HIV-1 transmission and the potential for serious adverse reactions in nursing infants, mothers should be instructed not to breast-feed if they are receiving EMTRIVA.
8.4 Pediatric Use
The safety and efficacy of emtricitabine in patients between 3 months and 21 years of age is supported by data from three open-label, non-randomized clinical studies in which emtricitabine was administered to 169 HIV-1 infected treatment-naive and experienced (defined as virologically suppressed on a lamivudine containing regimen for which emtricitabine was substituted for lamivudine) subjects [See Clinical Studies(14.3)].
The pharmacokinetics of emtricitabine were studied in 20 neonates born to HIV-1-positive mothers [See Clinical Studies (14.3)]. All neonates were HIV-1 negative at the end of the study; the efficacy of emtricitabine in preventing or treating HIV-1 could not be determined.
8.5 Geriatric Use
Clinical studies of EMTRIVA did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. In general, dose selection for the elderly patient should be cautious, keeping in mind the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Patients with Impaired Renal Function
It is recommended that the dose or dosing interval for EMTRIVA be modified in patients with creatinine clearance <50 mL/min or in patients who require dialysis [See Dosage and Administration (2.5)].
-
10 OVERDOSAGE
There is no known antidote for EMTRIVA. Limited clinical experience is available at doses higher than the therapeutic dose of EMTRIVA. In one clinical pharmacology study single doses of emtricitabine 1200 mg were administered to 11 patients. No severe adverse reactions were reported.
The effects of higher doses are not known. If overdose occurs the patient should be monitored for signs of toxicity, and standard supportive treatment applied as necessary.
Hemodialysis treatment removes approximately 30% of the emtricitabine dose over a 3-hour dialysis period starting within 1.5 hours of emtricitabine dosing (blood flow rate of 400 mL/min and a dialysate flow rate of 600 mL/min). It is not known whether emtricitabine can be removed by peritoneal dialysis.
-
11 DESCRIPTION
EMTRIVA is the brand name of emtricitabine, a synthetic nucleoside analog with activity against human immunodeficiency virus type 1 (HIV-1) reverse transcriptase.
The chemical name of emtricitabine is 5-fluoro-1-(2R,5S)-[2-(hydroxymethyl)-1,3-oxathiolan-5-yl]cytosine. Emtricitabine is the (-) enantiomer of a thio analog of cytidine, which differs from other cytidine analogs in that it has a fluorine in the 5-position.
It has a molecular formula of C8H10FN3O3S and a molecular weight of 247.24. It has the following structural formula:
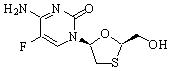
Emtricitabine is a white to off-white powder with a solubility of approximately 112 mg/mL in water at 25 °C. The log P for emtricitabine is -0.43 and the pKa is 2.65.
EMTRIVA is available as capsules or as an oral solution.
EMTRIVA capsules are for oral administration. Each capsule contains 200 mg of emtricitabine and the inactive ingredients, crospovidone, magnesium stearate, microcrystalline cellulose, and povidone.
EMTRIVA oral solution is for oral administration. One milliliter (1 mL) of EMTRIVA oral solution contains 10 mg of emtricitabine in an aqueous solution with the following inactive ingredients: cotton candy flavor, FD&C yellow No. 6, edetate disodium, methylparaben, and propylparaben (added as preservatives), sodium phosphate (monobasic), propylene glycol, water, and xylitol (added as a sweetener). Sodium hydroxide and hydrochloric acid may be used to adjust pH.
-
12 CLINICAL PHARMACOLOGY
12.3 Pharmacokinetics
Adult Subjects
The pharmacokinetics of emtricitabine were evaluated in healthy volunteers and HIV-1-infected individuals. Emtricitabine pharmacokinetics are similar between these populations.
Figure 1 shows the mean steady-state plasma emtricitabine concentration-time profile in 20 HIV-1-infected subjects receiving EMTRIVA capsules.
Figure 1 Mean (± 95% CI) Steady-State Plasma Emtricitabine Concentrations in HIV-1-Infected Adults (N=20)
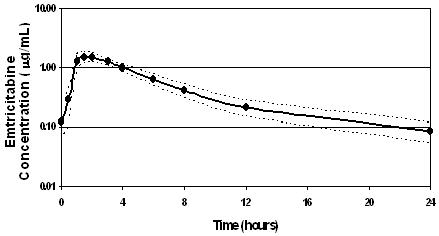
Absorption
Emtricitabine is rapidly and extensively absorbed following oral administration with peak plasma concentrations occurring at 1–2 hours post-dose. Following multiple dose oral administration of EMTRIVA capsules to 20 HIV-1-infected subjects, the (mean ± SD) steady-state plasma emtricitabine peak concentration (Cmax) was 1.8 ± 0.7 µg/mL and the area-under the plasma concentration-time curve over a 24-hour dosing interval (AUC) was 10.0 ± 3.1 µg∙hr/mL. The mean steady state plasma trough concentration at 24 hours post-dose was 0.09 µg/mL. The mean absolute bioavailability of EMTRIVA capsules was 93% while the mean absolute bioavailability of EMTRIVA oral solution was 75%. The relative bioavailability of EMTRIVA oral solution was approximately 80% of EMTRIVA capsules.
The multiple dose pharmacokinetics of emtricitabine are dose proportional over a dose range of 25–200 mg.
Distribution
In vitro binding of emtricitabine to human plasma proteins was <4% and independent of concentration over the range of 0.02–200 µg/mL. At peak plasma concentration, the mean plasma to blood drug concentration ratio was ~1.0 and the mean semen to plasma drug concentration ratio was ~4.0.
Metabolism
In vitro studies indicate that emtricitabine is not an inhibitor of human CYP450 enzymes. Following administration of 14C-emtricitabine, complete recovery of the dose was achieved in urine (~86%) and feces (~14%). Thirteen percent (13%) of the dose was recovered in urine as three putative metabolites. The biotransformation of emtricitabine includes oxidation of the thiol moiety to form the 3'-sulfoxide diastereomers (~9% of dose) and conjugation with glucuronic acid to form 2'-O-glucuronide (~4% of dose). No other metabolites were identifiable.
Elimination
The plasma emtricitabine half-life is approximately 10 hours. The renal clearance of emtricitabine is greater than the estimated creatinine clearance, suggesting elimination by both glomerular filtration and active tubular secretion. There may be competition for elimination with other compounds that are also renally eliminated.
Effects of Food on Oral Absorption
EMTRIVA capsules and oral solution may be taken with or without food. Emtricitabine systemic exposure (AUC) was unaffected while Cmax decreased by 29% when EMTRIVA capsules were administered with food (an approximately 1000 kcal high-fat meal). Emtricitabine systemic exposure (AUC) and Cmax were unaffected when 200 mg EMTRIVA oral solution was administered with either a high-fat or low-fat meal.
Special Populations
Race, Gender
The pharmacokinetics of emtricitabine were similar in adult male and female patients and no pharmacokinetic differences due to race have been identified.
Pediatric Patients
The pharmacokinetics of emtricitabine at steady state were determined in 77 HIV-1-infected children, and the pharmacokinetic profile was characterized in four age groups (Table 6). The emtricitabine exposure achieved in children receiving a daily dose of 6 mg/kg up to a maximum of 240 mg oral solution or a 200 mg capsule is similar to exposures achieved in adults receiving a once-daily dose of 200 mg.
The pharmacokinetics of emtricitabine were studied in 20 neonates born to HIV-1-positive mothers. Each mother received prenatal and intrapartum combination antiretroviral therapy. Neonates received up to 6 weeks of zidovudine prophylactically after birth. The neonates were administered two short courses of emtricitabine oral solution (each 3 mg/kg once daily × 4 days) during the first 3 months of life. The AUC observed in neonates who received a daily dose of 3 mg/kg of emtricitabine was similar to the AUC observed in pediatric patients ≥3 months to 17 years who received a daily dose of emtricitabine as a 6 mg/kg oral solution up to 240 mg or as a 200 mg capsule (Table 6).
Table 6 Mean ± SD Pharmacokinetic Parameters by Age Groups for Pediatric Patients and Neonates Receiving EMTRIVA Capsules or Oral Solution HIV-1-exposed Neonates HIV-1-infected Pediatric Patients Age 0–3 mo
(N=20)*3–24 mo
(N=14)25 mo–6 yr
(N=19)7–12yr
(N=17)13–17 yr
(N=27)- * Two pharmacokinetic evaluations were conducted in 20 neonates over the first 3 months of life. Median (range) age of infant on day of pharmacokinetic evaluation was 26 (5–81) days.
- † Mean (range)
Formulation Capsule (n) 0 0 0 10 26 Oral Solution (n) 20 14 19 7 1 Dose (mg/kg)† 3.1 (2.9–3.4) 6.1 (5.5–6.8) 6.1 (5.6–6.7) 5.6 (3.1–6.6) 4.4 (1.8–7.0) Cmax (µg/mL) 1.6 ± 0.6 1.9 ± 0.6 1.9 ± 0.7 2.7 ± 0.8 2.7 ± 0.9 AUC (µg∙hr/mL) 11.0 ± 4.2 8.7 ± 3.2 9.0 ± 3.0 12.6 ± 3.5 12.6 ± 5.4 T1/2 (hr) 12.1 ± 3.1 8.9 ± 3.2 11.3 ± 6.4 8.2 ± 3.2 8.9 ± 3.3 Geriatric Patients
The pharmacokinetics of emtricitabine have not been fully evaluated in the elderly.
Patients with Impaired Renal Function
The pharmacokinetics of emtricitabine are altered in patients with renal impairment [See Warnings and Precautions (5.4)]. In adult patients with creatinine clearance <50 mL/min or with end-stage renal disease (ESRD) requiring dialysis, Cmax and AUC of emtricitabine were increased due to a reduction in renal clearance (Table 7). It is recommended that the dosing interval for EMTRIVA be modified in adult patients with creatinine clearance <50 mL/min or in adult patients with ESRD who require dialysis [See Dosage and Administration (2.5)]. The effects of renal impairment on emtricitabine pharmacokinetics in pediatric patients are not known.
Table 7 Mean ± SD Pharmacokinetic Parameters in Adult Patients with Varying Degrees of Renal Function Creatinine Clearance (mL/min) >80
(N=6)50–80
(N=6)30–49
(N=6)<30
(N=5)ESRD*
<30
(N=5)- * ESRD patients requiring dialysis
- † NA = Not Applicable
Baseline creatinine clearance (mL/min) 107 ± 21 59.8 ± 6.5 40.9 ± 5.1 22.9 ± 5.3 8.8 ± 1.4 Cmax (µg/mL) 2.2 ± 0.6 3.8 ± 0.9 3.2 ± 0.6 2.8 ± 0.7 2.8 ± 0.5 AUC (µg∙hr/mL) 11.8 ± 2.9 19.9 ± 1.2 25.1 ± 5.7 33.7± 2.1 53.2 ± 9.9 CL/F (mL/min) 302 ± 94 168 ± 10 138 ± 28 99 ± 6 64 ± 12 CLr (mL/min) 213 ± 89 121 ± 39 69 ± 32 30 ± 11 NA† Hemodialysis: Hemodialysis treatment removes approximately 30% of the emtricitabine dose over a 3-hour dialysis period starting within 1.5 hours of emtricitabine dosing (blood flow rate of 400 mL/min and a dialysate flow rate of 600 mL/min). It is not known whether emtricitabine can be removed by peritoneal dialysis.
Assessment of Drug Interactions
At concentrations up to 14-fold higher than those observed in vivo, emtricitabine did not inhibit in vitro drug metabolism mediated by any of the following human CYP isoforms: CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2C19, CYP2D6, and CYP3A4. Emtricitabine did not inhibit the enzyme responsible for glucuronidation (uridine-5'-disphosphoglucuronyl transferase). Based on the results of these in vitro experiments and the known elimination pathways of emtricitabine, the potential for CYP mediated interactions involving emtricitabine with other medicinal products is low.
EMTRIVA has been evaluated in healthy volunteers in combination with tenofovir disoproxil fumarate (DF), zidovudine, indinavir, famciclovir, and stavudine. Tables 8 and 9 summarize the pharmacokinetic effects of coadministered drug on emtricitabine pharmacokinetics and effects of emtricitabine on the pharmacokinetics of coadministered drug.
Table 8 Drug Interactions: Change in Pharmacokinetic Parameters for Emtricitabine in the Presence of the Coadministered Drug* Coadministered Drug Dose of Coadministered Drug (mg) Emtricitabine Dose (mg) N % Change of Emtricitabine Pharmacokinetic Parameters† (90% CI) Cmax AUC Cmin - * All interaction studies conducted in healthy volunteers.
- †
↑ = Increase; ↓ = Decrease;
 = No Effect; NA = Not Applicable
= No Effect; NA = Not ApplicableTenofovir DF 300 once daily x 7 days 200 once daily × 7 days 17 

↑ 20
(↑ 12 to ↑ 29)Zidovudine 300 twice daily × 7 days 200 once daily × 7 days 27 


Indinavir 800 × 1 200 × 1 12 

NA Famciclovir 500 × 1 200 × 1 12 

NA Stavudine 40 × 1 200 × 1 6 

NA Table 9 Drug Interactions: Change in Pharmacokinetic Parameters for Coadministered Drug in the Presence of Emtricitabine* Coadministered Drug Dose of Coadministered Drug (mg) Emtricitabine Dose (mg) N % Change of Coadministered Drug Pharmacokinetic Parameters† (90% CI) Cmax AUC Cmin - * All interaction studies conducted in healthy volunteers.
- †
↑ = Increase; ↓ = Decrease;
 = No Effect; NA = Not Applicable
= No Effect; NA = Not ApplicableTenofovir DF 300 once daily × 7 days 200 once daily × 7 days 17 


Zidovudine 300 twice daily × 7 days 200 once daily × 7 days 27 ↑ 17
(↑ 0 to ↑ 38)↑ 13
(↑ 5 to↑ 20)
Indinavir 800 × 1 200 × 1 12 

NA Famciclovir 500 × 1 200 × 1 12 

NA Stavudine 40 × 1 200 × 1 6 

NA 12.4 Microbiology
Mechanism of Action
Emtricitabine, a synthetic nucleoside analog of cytidine, is phosphorylated by cellular enzymes to form emtricitabine 5'-triphosphate. Emtricitabine 5'-triphosphate inhibits the activity of the HIV-1 reverse transcriptase by competing with the natural substrate deoxycytidine 5'-triphosphate and by being incorporated into nascent viral DNA which results in chain termination. Emtricitabine 5'-triphosphate is a weak inhibitor of mammalian DNA polymerase α, β, ε, and mitochondrial DNA polymerase γ.
Antiviral Activity
The antiviral activity in cell culture of emtricitabine against laboratory and clinical isolates of HIV-1 was assessed in lymphoblastoid cell lines, the MAGI-CCR5 cell line, and peripheral blood mononuclear cells. The 50% effective concentration (EC50) value for emtricitabine was in the range of 0.0013–0.64 µM (0.0003–0.158 µg/mL). In drug combination studies of emtricitabine with nucleoside reverse transcriptase inhibitors (abacavir, lamivudine, stavudine, tenofovir, zalcitabine, zidovudine), non-nucleoside reverse transcriptase inhibitors (delavirdine, efavirenz, nevirapine), and protease inhibitors (amprenavir, nelfinavir, ritonavir, saquinavir), additive to synergistic effects were observed. Emtricitabine displayed antiviral activity in cell culture against HIV-1 clades A, B, C, D, E, F, and G (EC50 values ranged from 0.007–0.075 µM) and showed strain specific activity against HIV-2 (EC50 values ranged from 0.007–1.5 µM).
The in vivo activity of emtricitabine was evaluated in two clinical trials in which 101 patients were administered 25–400 mg a day of EMTRIVA as monotherapy for 10–14 days. A dose-related antiviral effect was observed, with a median decrease from baseline in plasma HIV-1 RNA of 1.3 log10 at a dose of 25 mg once daily and 1.7 log10 to 1.9 log10 at a dose of 200 mg once daily or twice daily.
Resistance
Emtricitabine-resistant isolates of HIV-1 have been selected in cell culture and in vivo. Genotypic analysis of these isolates showed that the reduced susceptibility to emtricitabine was associated with a substitution in the HIV-1 reverse transcriptase gene at codon 184 which resulted in an amino acid substitution of methionine by valine or isoleucine (M184V/I).
Emtricitabine-resistant isolates of HIV-1 have been recovered from some patients treated with emtricitabine alone or in combination with other antiretroviral agents. In a clinical study of treatment-naive patients treated with EMTRIVA, didanosine, and efavirenz [See Clinical Studies (14.1)], viral isolates from 37.5% of patients with virologic failure showed reduced susceptibility to emtricitabine. Genotypic analysis of these isolates showed that the resistance was due to M184V/I substitutions in the HIV-1 reverse transcriptase gene.
In a clinical study of treatment-naive patients treated with either EMTRIVA, VIREAD, and efavirenz or zidovudine/lamivudine and efavirenz [See Clinical Studies (14.1)], resistance analysis was performed on HIV-1 isolates from all confirmed virologic failure patients with >400 copies/mL of HIV-1 RNA at Week 144 or early discontinuation. Development of efavirenz resistance-associated substitutions occurred most frequently and was similar between the treatment arms. The M184V amino acid substitution, associated with resistance to EMTRIVA and lamivudine, was observed in 2/19 analyzed patient isolates in the EMTRIVA + VIREAD group and in 10/29 analyzed patient isolates in the lamivudine/zidovudine group. Through 144 weeks of Study 934, no patients have developed a detectable K65R substitution in their HIV-1 as analyzed through standard genotypic analysis.
Cross Resistance
Cross-resistance among certain nucleoside analog reverse transcriptase inhibitors has been recognized. Emtricitabine-resistant isolates (M184V/I) were cross-resistant to lamivudine and zalcitabine but retained sensitivity in cell culture to didanosine, stavudine, tenofovir, zidovudine, and NNRTIs (delavirdine, efavirenz, and nevirapine). HIV-1 isolates containing the K65R substitution, selected in vivo by abacavir, didanosine, tenofovir, and zalcitabine, demonstrated reduced susceptibility to inhibition by emtricitabine. Viruses harboring substitutions conferring reduced susceptibility to stavudine and zidovudine (M41L, D67N, K70R, L210W, T215Y/F, K219Q/E) or didanosine (L74V) remained sensitive to emtricitabine. HIV-1 containing the K103N substitution associated with resistance to NNRTIs was susceptible to emtricitabine.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In long-term oral carcinogenicity studies of emtricitabine, no drug-related increases in tumor incidence were found in mice at doses up to 750 mg/kg/day (26 times the human systemic exposure at the therapeutic dose of 200 mg/day) or in rats at doses up to 600 mg/kg/day (31 times the human systemic exposure at the therapeutic dose).
Emtricitabine was not genotoxic in the reverse mutation bacterial test (Ames test), mouse lymphoma or mouse micronucleus assays.
Emtricitabine did not affect fertility in male rats at approximately 140-fold or in male and female mice at approximately 60-fold higher exposures (AUC) than in humans given the recommended 200 mg daily dose. Fertility was normal in the offspring of mice exposed daily from before birth (in utero) through sexual maturity at daily exposures (AUC) of approximately 60-fold higher than human exposures at the recommended 200 mg daily dose.
-
14 CLINICAL STUDIES
14.1 Treatment-Naive Adult Patients
Study 934
Data through 144 weeks are reported for Study 934, a randomized, open-label, active-controlled multicenter study comparing EMTRIVA + VIREAD administered in combination with efavirenz versus zidovudine/lamivudine fixed-dose combination administered in combination with efavirenz in 511 antiretroviral-naive patients. From Weeks 96 to 144 of the study, patients received emtricitabine + tenofovir disoproxil fumarate (tenofovir DF) with efavirenz in place of EMTRIVA + tenofovir DF with efavirenz. Patients had a mean age of 38 years (range 18–80), 86% were male, 59% were Caucasian and 23% were Black. The mean baseline CD4+ cell count was 245 cells/mm3 (range 2–1191) and median baseline plasma HIV-1 RNA was 5.01 log10 copies/mL (range 3.56–6.54). Patients were stratified by baseline CD4+ cell count (< or ≥200 cells/mm3); 41% had CD4+ cell counts <200 cells/mm3 and 51% of patients had baseline viral loads >100,000 copies/mL. Treatment outcomes through 48 and 144 weeks for those patients who did not have efavirenz resistance at baseline are presented in Table 10.
Table 10 Outcomes of Randomized Treatment at Week 48 and 144 (Study 934) Outcomes Week 48 Week 144 EMTRIVA
+TDF
+EFV
(N=244)AZT/3TC
+EFV
(N=243)EMTRIVA
+TDF
+EFV
(N=227)*AZT/3TC
+EFV
(N=229)*- * Patients who were responders at Week 48 or Week 96 (HIV-1 RNA <400 copies/mL) but did not consent to continue study after Week 48 or Week 96 were excluded from analysis.
- † Patients achieved and maintained confirmed HIV-1 RNA <400 copies/mL through Weeks 48 and 144.
- ‡ Includes confirmed viral rebound and failure to achieve confirmed <400 copies/mL through Weeks 48 and 144.
- § Includes lost to follow-up, patient withdrawal, noncompliance, protocol violation and other reasons.
Responder† 84% 73% 71% 58% Virologic failure‡ 2% 4% 3% 6% Rebound 1% 3% 2% 5% Never suppressed 0% 0% 0% 0% Change in antiretroviral regimen 1% 1% 1% 1% Death <1% 1% 1% 1% Discontinued due to adverse event 4% 9% 5% 12% Discontinued for other reasons§ 10% 14% 20% 22% Through Week 48, 84% and 73% of patients in the EMTRIVA + tenofovir DF group and the zidovudine/lamivudine group, respectively, achieved and maintained HIV-1 RNA <400 copies/mL (71% and 58% through Week 144). The difference in the proportion of patients who achieved and maintained HIV-1 RNA <400 copies/mL through 48 weeks largely results from the higher number of discontinuations due to adverse events and other reasons in the zidovudine/lamivudine group in this open-label study. In addition, 80% and 70% of patients in the EMTRIVA + tenofovir DF group and the zidovudine/lamivudine group, respectively, achieved and maintained HIV-1 RNA <50 copies/mL through Week 48 (64% and 56% through Week 144). The mean increase from baseline in CD4+ cell count was 190 cells/mm3 in the EMTRIVA + tenofovir DF group and 158 cells/mm3 in the zidovudine/lamivudine group at Week 48 (312 and 271 cells/mm3 at Week 144).
Through 48 weeks, 7 patients in the EMTRIVA + tenofovir DF group and 5 patients in the zidovudine/lamivudine group experienced a new CDC Class C event (10 and 6 patients through 144 weeks).
Study 301A
Study 301A was a 48 week double-blind, active-controlled multicenter study comparing EMTRIVA (200 mg once daily) administered in combination with didanosine and efavirenz versus stavudine, didanosine and efavirenz in 571 antiretroviral naive adult patients. Patients had a mean age of 36 years (range 18–69), 85% were male, 52% Caucasian, 16% African-American and 26% Hispanic. Patients had a mean baseline CD4+ cell count of 318 cells/mm3 (range 5–1317) and a median baseline plasma HIV-1 RNA of 4.9 log10 copies/mL (range 2.6–7.0). Thirty-eight percent of patients had baseline viral loads >100,000 copies/mL and 31% had CD4+ cell counts <200 cells/mL. Treatment outcomes are presented in Table 11 below.
Table 11 Outcomes of Randomized Treatment at Week 48 (Study 301A) Outcomes EMTRIVA
+ Didanosine
+ Efavirenz
(N=286)Stavudine
+ Didanosine
+ Efavirenz
(N=285)- * Patients achieved and maintained confirmed HIV RNA <400 copies/mL (<50 copies/mL) through Week 48.
- † Includes patients who failed to achieve virologic suppression or rebounded after achieving virologic suppression.
- ‡ Includes lost to follow-up, patient withdrawal, non-compliance, protocol violation and other reasons.
Responder* 81% (78%) 68% (59%) Virologic Failure† 3% 11% Death 0% <1% Study Discontinuation Due to Adverse Event 7% 13% Study Discontinuation for Other Reasons‡ 9% 8% The mean increase from baseline in CD4+ cell count was 168 cells/mm3 for the EMTRIVA arm and 134 cells/mm3 for the stavudine arm.
Through 48 weeks in the EMTRIVA group, 5 patients (1.7%) experienced a new CDC Class C event, compared to 7 patients (2.5%) in the stavudine group.
14.2 Treatment-Experienced Adult Patients
Study 303
Study 303 was a 48 week, open-label, active-controlled multicenter study comparing EMTRIVA (200 mg once daily) to lamivudine, in combination with stavudine or zidovudine and a protease inhibitor or NNRTI in 440 adult patients who were on a lamivudine-containing triple-antiretroviral drug regimen for at least 12 weeks prior to study entry and had HIV-1 RNA ≤400 copies/mL.
Patients were randomized 1:2 to continue therapy with lamivudine (150 mg twice daily) or to switch to EMTRIVA (200 mg once daily). All patients were maintained on their stable background regimen. Patients had a mean age of 42 years (range 22–80), 86% were male, 64% Caucasian, 21% African-American and 13% Hispanic. Patients had a mean baseline CD4+ cell count of 527 cells/mm3 (range 37–1909), and a median baseline plasma HIV-1 RNA of 1.7 log10 copies/mL (range 1.7–4.0).
The median duration of prior antiretroviral therapy was 27.6 months. Treatment outcomes are presented in Table 12 below.
Table 12 Outcomes of Randomized Treatment at Week 48 (Study 303) Outcomes EMTRIVA
+ ZDV/d4T
+ NNRTI/PI
(N=294)Lamivudine
+ ZDV/d4T
+ NNRTI/PI
(N=146)- * Patients achieved and maintained confirmed HIV RNA <400 copies/mL (<50 copies/mL) through Week 48.
- † Includes patients who failed to achieve virologic suppression or rebounded after achieving virologic suppression.
- ‡ Includes lost to follow-up, patient withdrawal, non-compliance, protocol violation and other reasons.
Responder* 77% (67%) 82% (72%) Virologic Failure† 7% 8% Death 0% <1% Study Discontinuation Due to Adverse Event 4% 0% Study Discontinuation for Other Reasons‡ 12% 10% The mean increase from baseline in CD4+ cell count was 29 cells/mm3 for the EMTRIVA arm and 61 cells/mm3 for the lamivudine arm.
Through 48 weeks, in the EMTRIVA group 2 patients (0.7%) experienced a new CDC Class C event, compared to 2 patients (1.4%) in the lamivudine group.
14.3 Pediatric Patients
In three open-label, non-randomized clinical studies, emtricitabine was administered to 169 HIV-1 infected treatment-naive and experienced (defined as virologically suppressed on a lamivudine containing regimen for which emtricitabine was substituted for lamivudine) patients between 3 months and 21 years of age. Patients received once-daily EMTRIVA oral solution (6 mg/kg to a maximum of 240 mg/day) or EMTRIVA capsules (a single 200 mg capsule once daily) in combination with at least two other antiretroviral agents.
Patients had a mean age of 7.9 years (range 0.3–21), 49% were male, 15% Caucasian, 61% Black and 24% Hispanic. Patients had a median baseline HIV-1 RNA of 4.6 log10 copies/mL (range 1.7–6.4) and a mean baseline CD4+ cell count of 745 cells/mm3 (range 2–2650). Through 48 weeks of therapy, the overall proportion of patients who achieved and sustained an HIV-1 RNA <400 copies/mL was 86%, and <50 copies/mL was 73%. The mean increase from baseline in CD4+ cell count was 232 cells/mm3 (-945, +1512). The adverse reaction profile observed during these clinical trials was similar to that of adult patients, with the exception of the occurrence of anemia and higher frequency of hyperpigmentation in children [See Adverse Reactions (6)].
The pharmacokinetics of emtricitabine were studied in 20 neonates born to HIV-1-positive mothers. Each mother received prenatal and intrapartum combination antiretroviral therapy. Neonates received up to 6 weeks of zidovudine prophylactically after birth. The neonates were administered two short courses of emtricitabine oral solution (each 3 mg/kg once daily × 4 days) during the first 3 months of life. Emtricitabine exposures in neonates were similar to the exposures achieved in patients >3 months to 17 years [See Clinical Pharmacology (12.3)]. During the two short dosing periods on emtricitabine there were no safety issues identified in the treated neonates. All neonates were HIV-1 negative at the end of the study; the efficacy of emtricitabine in preventing or treating HIV-1 could not be determined.
-
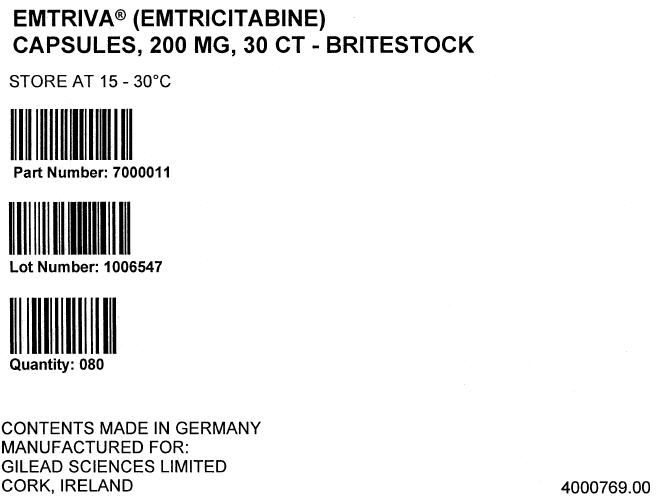
16 HOW SUPPLIED/STORAGE AND HANDLING
Capsules
The size 1 hard gelatin capsules with a blue cap and white body contain 200 mg of emtricitabine, are printed with "200 mg" in black on the cap and "GILEAD" and the corporate logo in black on the body, and are available in unit of use bottles (closed with induction sealed child-resistant closures) of:
- 30 capsules (NDC 61958–0601–1).
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (17.2)
17.1 Information for Patients
Patients should be advised that:
- EMTRIVA is not a cure for HIV-1 infection and patients may continue to experience illnesses associated with HIV-1 infection, including opportunistic infections. Patients should remain under the care of a physician when using EMTRIVA.
- The use of EMTRIVA has not been shown to reduce the risk of transmission of HIV-1 to others through sexual contact or blood contamination.
- The long term effects of EMTRIVA are unknown.
- EMTRIVA capsules and oral solution are for oral ingestion only.
- It is important to take EMTRIVA with combination therapy on a regular dosing schedule to avoid missing doses.
- Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported. Treatment with EMTRIVA should be suspended in any patient who develops clinical symptoms suggestive of lactic acidosis or pronounced hepatotoxicity (including nausea, vomiting, unusual or unexpected stomach discomfort, and weakness) [See Warnings and Precautions (5.1)].
- Patients with HIV-1 should be tested for Hepatitis B virus (HBV) before initiating antiretroviral therapy.
- Severe acute exacerbations of Hepatitis B have been reported in patients who are coinfected with HBV and HIV-1 and have discontinued EMTRIVA.
- EMTRIVA should not be coadministered with other drugs containing lamivudine, including Combivir (lamivudine/zidovudine), Epivir or Epivir-HBV (lamivudine), Epzicom (abacavir sulfate/lamivudine), or Trizivir (abacavir sulfate/lamivudine/zidovudine) [See Warnings and Precautions (5.3)].
- Dose or dosing interval of EMTRIVA may need adjustment in patients with renal impairment [See Dosage and Administration (2.5)].
-
PATIENT PACKAGE INSERT
EMTRIVA® (em-treev'-ah) capsules
EMTRIVA oral solution
Generic name: emtricitabine (em tri SIT uh bean)
Read the Patient Information that comes with EMTRIVA before you start using it and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
You should stay under a healthcare provider's care when taking EMTRIVA. Do not change or stop your medicine without first talking with your healthcare provider. Talk to your healthcare provider or pharmacist if you have any questions about EMTRIVA.
What is the most important information I should know about EMTRIVA?
- Some people who have taken medicines like EMTRIVA (a nucleoside analog) have developed a serious condition called lactic acidosis (buildup of an acid in the blood). Lactic acidosis can be a medical emergency and may need to be treated in the hospital. Call your healthcare provider right away if you get the following signs of lactic acidosis.
- You feel very weak or tired.
- You have unusual (not normal) muscle pain.
- You have trouble breathing.
- You have stomach pain with nausea and vomiting.
- You feel cold, especially in your arm and legs.
- You feel dizzy or lightheaded.
- You have a fast or irregular heartbeat.
-
Some people who have taken medicines like EMTRIVA have developed serious liver problems called hepatotoxicity, with liver enlargement (hepatomegaly) and fat in the liver (steatosis). Call your healthcare provider right away if you get the following signs of liver problems.
- Your skin or the white part of your eyes turns yellow (jaundice).
- Your urine turns dark.
- Your bowel movements (stools) turn light in color.
- You don't feel like eating food for several days or longer.
- You feel sick to your stomach (nausea).
- You have lower stomach area (abdominal) pain.
- You may be more likely to get lactic acidosis or liver problems if you are female, very overweight (obese), or have been taking nucleoside analog medicines, like EMTRIVA, for a long time.
- If you are also infected with the Hepatitis B Virus (HBV), you need close medical follow-up for several months after stopping treatment with EMTRIVA. Follow-up includes medical exams and blood tests to check for HBV that is getting worse. Patients with HBV infection, who take EMTRIVA and then stop it, may get "flare-ups" of their hepatitis. A "flare-up" is when the disease suddenly returns in a worse way than before.
What is EMTRIVA?
EMTRIVA is a type of medicine called an HIV-1 (human immunodeficiency virus) nucleoside reverse transcriptase inhibitor (NRTI). EMTRIVA is always used with other anti-HIV-1 medicines to treat people with HIV-1 infection. EMTRIVA is for adults and children, but has not been studied fully in adults over age 65.
HIV infection destroys CD4+ T cells, which are important to the immune system. The immune system helps fight infection. After a large number of T cells are destroyed, acquired immune deficiency syndrome (AIDS) develops.
EMTRIVA helps to block HIV-1 reverse transcriptase, a chemical in your body (enzyme) that is needed for HIV-1 to multiply. EMTRIVA may lower the amount of HIV-1 in the blood (viral load). EMTRIVA may also help to increase the number of T cells called CD4+ cells. Lowering the amount of HIV-1 in the blood lowers the chance of death or infections that happen when your immune system is weak (opportunistic infections).
EMTRIVA does not cure HIV-1 infection or AIDS. The long-term effects of EMTRIVA are not known at this time. People taking EMTRIVA may still get opportunistic infections or other conditions that happen with HIV-1 infection. Opportunistic infections are infections that develop because the immune system is weak. Some of these conditions are pneumonia, herpes virus infections, and Mycobacterium avium complex (MAC) infections. It is very important that you see your healthcare provider regularly while taking EMTRIVA.
EMTRIVA does not lower your chance of passing HIV-1 to other people through sexual contact, sharing needles, or being exposed to your blood. For your health and the health of others, it is important to always practice safer sex by using a latex or polyurethane condom or other barrier to lower the chance of sexual contact with semen, vaginal secretions, or blood. Never use or share dirty needles.
Who should not take EMTRIVA?
- Do not take EMTRIVA if you are allergic to EMTRIVA or any of its ingredients. The active ingredient is emtricitabine. See the end of this leaflet for a complete list of ingredients.
- Do not take EMTRIVA if you are already taking ATRIPLA®, TRUVADA®, Combivir, Epivir, Epivir-HBV, Epzicom, or Trizivir because these medicines contain the same or similar active ingredients.
What should I tell my healthcare provider before taking EMTRIVA?
Tell your healthcare provider
- If you are pregnant or planning to become pregnant. We do not know if EMTRIVA can harm your unborn child. You and your healthcare provider will need to decide if EMTRIVA is right for you. If you use EMTRIVA while you are pregnant, talk to your healthcare provider about how you can be on the EMTRIVA Antiviral Pregnancy Registry.
- If you are breast-feeding. You should not breast feed if you are HIV-positive because of the chance of passing the HIV virus to your baby. Also, it is not known if EMTRIVA can pass into your breast milk and if it can harm your baby. If you are a woman who has or will have a baby, talk with your healthcare provider about the best way to feed your baby.
- If you have kidney problems. You may need to take EMTRIVA less often.
- If you have any liver problems including Hepatitis B Virus infection.
- Tell your healthcare provider about all your medical conditions.
- Tell your healthcare provider about all the medicines you take such as prescription and non-prescription medicines and dietary supplements. Keep a complete list of all the medicines that you take. Make a new list when medicines are added or stopped. Give copies of this list to all of your healthcare providers and pharmacist every time you visit or fill a prescription.
How should I take EMTRIVA?
- Take EMTRIVA by mouth exactly as your healthcare provider prescribed it. Follow the directions from your healthcare provider, exactly as written on the label.
- Dosing in adults: The usual dose of EMTRIVA is 1 capsule once a day.
- Dosing in children: The child's doctor will calculate the right dose of EMTRIVA (oral solution or capsule) based on the child's weight.
- EMTRIVA is always used with other anti-HIV-1 medicines.
- EMTRIVA may be taken with or without a meal. Food does not affect how EMTRIVA works.
- If you forget to take EMTRIVA, take it as soon as you remember that day. Do not take more than 1 dose of EMTRIVA in a day. Do not take 2 doses at the same time. Call your healthcare provider or pharmacist if you are not sure what to do. It is important that you do not miss any doses of EMTRIVA or your other anti-HIV-1 medicines.
- When your EMTRIVA supply starts to run low, get more from your healthcare provider or pharmacy. This is very important because the amount of virus in your blood may increase if the medicine is stopped for even a short time. The virus may develop resistance to EMTRIVA and become harder to treat.
- Stay under a healthcare provider's care when taking EMTRIVA. Do not change your treatment or stop treatment without first talking with your healthcare provider.
- If you take too much EMTRIVA, call your local poison control center or emergency room right away.
What should I avoid while taking EMTRIVA?
- Do not breast-feed. See "What should I tell my healthcare provider before taking EMTRIVA?" Talk with your healthcare provider about the best way to feed your baby.
- Avoid doing things that can spread HIV-1 infection since EMTRIVA doesn't stop you from passing the HIV-1 infection to others.
- Do not share needles or other injection equipment.
- Do not share personal items that can have blood or body fluids on them, like toothbrushes or razor blades.
- Do not have any kind of sex without protection. Always practice safer sex by using a latex or polyurethane condom or other barrier to reduce the chance of sexual contact with semen, vaginal secretions, or blood.
What are the possible side effects of EMTRIVA?
EMTRIVA may cause the following serious side effects (See "What is the most important information I should know about EMTRIVA?"):
- lactic acidosis (buildup of an acid in the blood). Lactic acidosis can be a medical emergency and may need to be treated in the hospital. Call your doctor right away if you get signs of lactic acidosis. (See "What is the most important information I should know about EMTRIVA?")
- serious liver problems (hepatotoxicity), with liver enlargement (hepatomegaly) and fat in the liver (steatosis). Call your healthcare provider right away if you get any signs of liver problems. (See "What is the most important information I should know about EMTRIVA?")
- "flare-ups" of Hepatitis B Virus infection, in which the disease suddenly returns in a worse way than before, can occur if you stop taking EMTRIVA. EMTRIVA is not for the treatment of Hepatitis B Virus (HBV) infection.
Other side effects with EMTRIVA when used with other anti-HIV-1 medicines Include:
- Changes in body fat have been seen in some patients taking EMTRIVA and other anti-HIV-1 medicines. These changes may include increased amount of fat in the upper back and neck ("buffalo hump"), breast, and around the main part of your body (trunk). Loss of fat from the legs, arms and face may also happen. The cause and long term health effects of these conditions are not known at this time.
The most common side effects of EMTRIVA used with other anti-HIV-1 medicines are headache, diarrhea, and nausea. Other side effects include allergic reaction, dizziness, sleeping problems, abnormal dreams, vomiting, indigestion, stomach pain, pain, weakness and rash. Skin discoloration may also happen with EMTRIVA.
There have been other side effects in patients taking EMTRIVA. However, these side effects may have been due to other medicines that patients were taking or to HIV-1 itself. Some of these side effects can be serious.
This list of side effects is not complete. If you have questions about side effects, ask your healthcare provider or pharmacist. You should report any new or continuing symptoms to your healthcare provider right away. Your healthcare provider may be able to help you manage these side effects.
How do I store EMTRIVA?
- Keep EMTRIVA and all other medicines out of reach of children.
- Store EMTRIVA capsules between 59 °F and 86 °F (15 °C to 30 °C).
- Store EMTRIVA oral solution in a refrigerator between 36 °F and 46 °F (2–8 °C). Do not freeze. Alternatively, the product may be stored at room temperature for up to 3 months and any remaining solution in the bottle must be discarded after the 3 months.
- Do not keep your medicine in places that are too hot or cold.
- Do not keep medicine that is out of date or that you no longer need. If you throw any medicines away make sure that children will not find them.
General information about EMTRIVA:
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use EMTRIVA for a condition for which it was not prescribed. Do not give EMTRIVA to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about EMTRIVA. If you would like more information, talk with your doctor. You can ask your healthcare provider or pharmacist for information about EMTRIVA that is written for health professionals. For more information, you may also call 1-800-GILEAD5.
What are the ingredients of EMTRIVA?
Active Ingredient: emtricitabine
Inactive Ingredients for EMTRIVA capsules: crospovidone, magnesium stearate, microcrystalline cellulose, and povidone.
Inactive Ingredients for EMTRIVA oral solution: Cotton candy flavor, FD&C yellow No. 6, edetate disodium, methylparaben and propylparaben, sodium phosphate (monobasic), propylene glycol, water, and xylitol. Sodium hydroxide and hydrochloric acid may be used to adjust pH.
Rx Only
May 2008
EMTRIVA, TRUVADA, and VIREAD are trademarks of Gilead Sciences, Inc. ATRIPLA is a trademark of Bristol-Myers Squibb & Gilead Sciences, LLC. All other trademarks referenced herein are the property of their respective owners.
21-500-896-GS-014
- Some people who have taken medicines like EMTRIVA (a nucleoside analog) have developed a serious condition called lactic acidosis (buildup of an acid in the blood). Lactic acidosis can be a medical emergency and may need to be treated in the hospital. Call your healthcare provider right away if you get the following signs of lactic acidosis.
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
EMTRIVA
emtricitabine capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 46014-0601 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength emtricitabine (UNII: G70B4ETF4S) (emtricitabine - UNII:G70B4ETF4S) emtricitabine 200 mg Product Characteristics Color WHITE (white opaque body with ligh-blue cap) Score no score Shape CAPSULE Size 19mm Flavor Imprint Code 200;mg;GILEAD Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 46014-0601-1 30 in 1 BOTTLE, PLASTIC Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021500 07/02/2003 Labeler - Excella GmbH (329809800)
Trademark Results [Emtriva]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 EMTRIVA 78239710 2852092 Live/Registered |
Gilead Sciences, Inc. 2003-04-18 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.