SCENESSE- afamelanotide implant
SCENESSE by
Drug Labeling and Warnings
SCENESSE by is a Prescription medication manufactured, distributed, or labeled by CLINUVEL INC.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use SCENESSE safely and effectively. See full prescribing information for SCENESSE.
SCENESSE® (afamelanotide) implant, for subcutaneous use.
Initial U.S. Approval: 2019INDICATIONS AND USAGE
SCENESSE is a melanocortin 1 receptor (MC1-R) agonist indicated to increase pain free light exposure in adult patients with a history of phototoxic reactions from erythropoietic protoporphyria (EPP)
DOSAGE AND ADMINISTRATION
- SCENESSE should be administered by a healthcare professional who is proficient in the subcutaneous implantation procedure and has completed training prior to administration.
- Insert a single implant, containing 16 mg of afamelanotide, using an SFM Implantation Cannula or other implantation devices that have been determined by the manufacturer to be suitable for implantation of SCENESSE.
- Administer SCENESSE subcutaneously every 2 months.
DOSAGE FORMS AND STRENGTHS
Implant: 16 mg of afamelanotide.
WARNINGS AND PRECAUTIONS
Skin monitoring: May induce darkening of pre-existing nevi and ephelides due to its pharmacological effect. A regular full body skin examination (twice yearly) is recommended to monitor all nevi and other skin abnormalities.
ADVERSE REACTIONS
The most common adverse reactions (incidence > 2%) are implant site reaction, nausea, oropharyngeal pain, cough, fatigue, dizziness, skin hyperpigmentation, somnolence, melanocytic nevus, respiratory tract infection, non-acute porphyria, and skin irritation.
To report SUSPECTED ADVERSE REACTIONS, contact CLINUVEL INC. at 1-888-288-2031 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Revised: 10/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
Important Dosage and Administration Information
Instructions for Implantation of SCENESSE
Skin Monitoring
Clinical Trials Experience
Pregnancy
Lactation
Pediatric Use
Geriatric Use
Descripton
Mechanism of Action
Pharmacodynamics
Pharmacokinetics
Carcinogenesis, Mutagenesis, Impairment of Fertility
- * Sections or subsections omitted from the full prescribing information are not listed.
- INDICATIONS & USAGE
-
Important Dosage and Administration Information
SCENESSE should be administered by a health care professional. All healthcare professionals should be proficient in the subcutaneous implantation procedure and have completed the training program provided by CLINUVEL prior to administration of the SCENESSE implant [ see Dosage and Administration]. Additional information, including a video, is available at http://www.clinuvel.com/US-HCP. The additional information has not been evaluated or approved by the FDA.
A single SCENESSE implant is inserted subcutaneously above the anterior supra-iliac crest every 2 months.
Use the SFM Implantation Cannula to implant SCENESSE. Contact CLINUVEL INC. for other implantation devices that have been determined by the manufacturer to be suitable for implantation of SCENESSE.
Maintain sun and light protection measures during treatment with SCENESSE to prevent phototoxic reactions related to EPP.Instructions for Implantation of SCENESSE
Insert a single SCENESSE implant (containing 16 mg of afamelanotide) subcutaneously above the anterior supra-iliac crest.
Implant SCENESSE observing an aseptic technique. The following equipment is needed for the implant insertion:- SCENESSE implant
- SFM Implantation Cannula; use of a device that has not been determined to be suitable could result in damage to the SCENESSE implant [ see Dosage and Administration].
- Sterile gloves
- Local anesthetic, needle and syringe
- Blunt forceps suitable for removing the SCENESSE implant from the glass vial and placement of the SCENESSE implant
- Sterile gauze, adhesive bandage, pressure bandage
Step 1
- Take the carton containing SCENESSE out of the refrigerator to allow the product to gradually warm up to ambient temperature.
- Remove the seal and stopper from the glass vial containing SCENESSE. Remove the implant from the vial using the blunt forceps under aseptic conditions and place the implant on a sterile gauze.
Step 2
Put the patient in a comfortable reclined supine position.
Identify the insertion site 3-4 cm above the anterior supra-iliac crest and disinfect the skin surface.
Step 3 (optional)
Anesthetize the area of insertion (puncture) if deemed necessary and in consultation with the patient.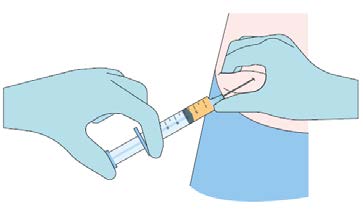
Step 4
While pinching the skin of the insertion site, insert the cannula with the bevel facing upwards (away from the abdomen) at a 30-45° angle into the subcutaneous layer.
Advance the cannula 2 cm into the subcutaneous layer.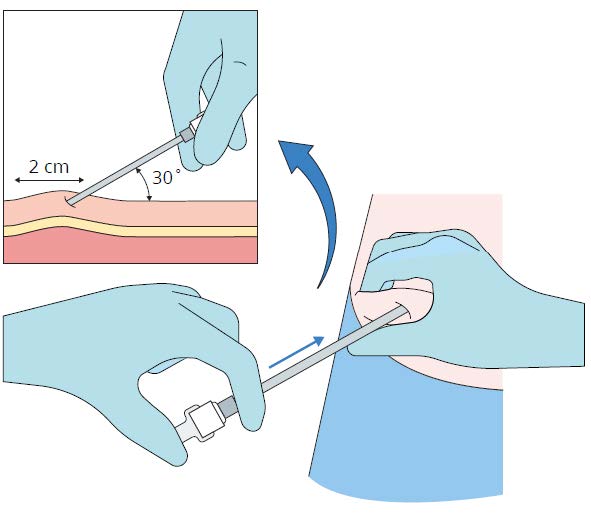
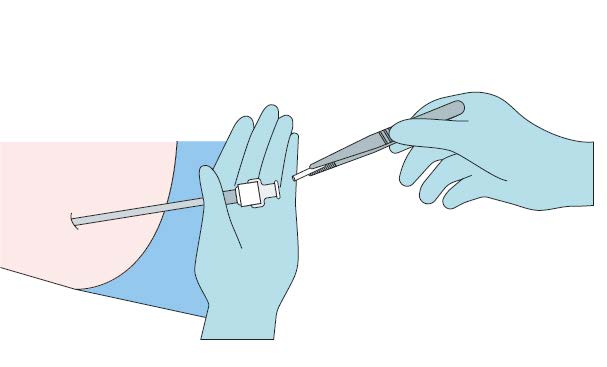
Step 5- Remove the stylet (obturator) from the cannula maintaining aseptic precautions.
- Load the implant into the cannula.
- Using the stylet (obturator) gently push the implant down the full length of the cannula’s shaft.
Step 6
Apply pressure to the site of the implant while removing the stylet (obturator) and the cannula. Verify that no implant or
implant portion remains in the cannula.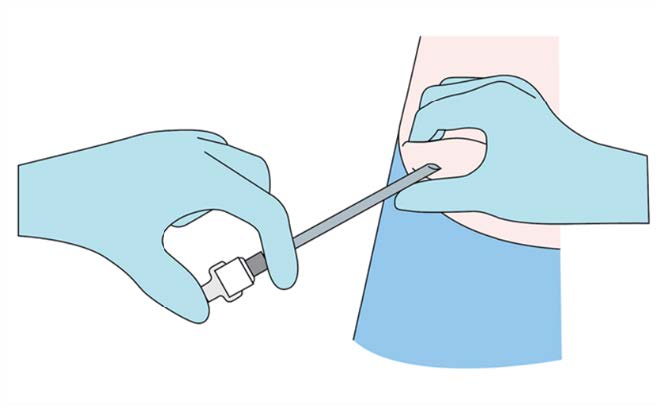
Step 7
Verify the correct insertion and placement of the implant by palpating the skin overlying the implant.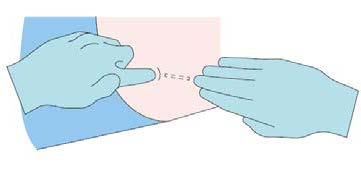
Step 8
Apply dressing to the insertion site. Leave dressing in place for 24 hours.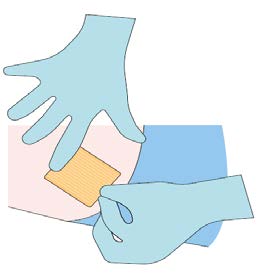
Step 9
Monitor the patient for 30 minutes after the implant administration.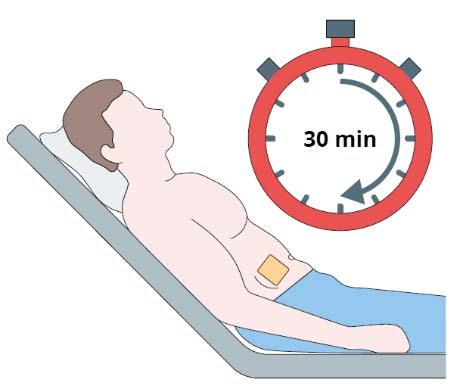
- DOSAGE FORMS & STRENGTHS
- CONTRAINDICATIONS
- Skin Monitoring
-
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of SCENESSE was evaluated in 3 randomized, multicenter, prospective, vehicle controlled clinical trials (Study CUV029, Study CUV030, and Study CUV039) involving 244 adult subjects with erythropoietic protoporphyria (EPP) without significant liver involvement. Subjects received subcutaneous SCENESSE implants containing 16 mg of afamelanotide every 2 months. A total of 125 subjects received SCENESSE and 119 subjects received vehicle implants.Table 1 summarizes the adverse reactions that occurred in more than 2% of subjects.
Table 1: Adverse Reactions Occurring in More Than 2% of Subjects with EPP Through Month 6 (Studies CUV039, CUV030, and CUV029).
Table 1: Adverse Reactions Occurring in More Than 2% of Subjects with EPP Through Month 6 (Studies CUV039, CUV030, and CUV029) Adverse Reaction SCENESSE
n (%)
N = 125Vehicle
n (%)
N = 119Implant site reaction 1 26 (21%) 12 (10%) Nausea 24 (19%) 17 (14%) Oropharyngeal pain 9 (7%) 6 (5%) Cough 8 (6%) 4 (3%) Fatigue 7 (6%) 3 (3%) Skin hyperpigmentation 2 5 (4%) 0 (0%) Dizziness 5 (4%) 4 (3%) Melanocytic nevus 5 (4%) 2 (2%) Respiratory tract infection 5 (4%) 3 (3%) Somnolence 3 (2%) 1 (1%) Non-acute porphyria 2 (2%) 0 (0%) Skin irritation 2 (2%) 0 (0%) 1: Implant site reaction includes: implant site bruising, discoloration, erythema, hemorrhage, hypertrophy, irritation, nodule, pain, pruritus, swelling;
injection site bruising and erythema; and expelled implant.
2: Skin hyperpigmentation includes skin hyperpigmentation, pigmentation lip (subject also had skin hyperpigmentation), and pigmentation disorder.
Specific Adverse Reactions
Implant Site Reactions: Implant site reactions were more common in the SCENESSE group (21%) compared to the vehicle
group (10%). In the SCENESSE group, the most common implant site reaction was implant site discoloration (10%). -
Pregnancy
Risk Summary
There are no data on SCENESSE use in pregnant women to evaluate for any drug associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcome.
In animal reproductive and development toxicity studies, no adverse developmental effects were observed with afamelanotide administration during the period of organogenesis to pregnant rats at subcutaneous doses up to 12 times the maximum recommended human dose (MRHD) ( see Data).All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In embryofetal development studies in Sprague Dawley and Lister Hooded rats, afamelanotide was administered subcutaneously to pregnant rats at doses of 0.2, 2, or 20 mg/kg/day throughout the period of organogenesis. No adverse embryofetal developmental effects were observed at doses up to 20 mg/kg/day (12 times the MRHD, based on a body surface area comparison).
In a pre- and post-natal development study in Sprague Dawley rats, afamelanotide was administered subcutaneously at doses of 0.2, 2, or 20 mg/kg/day during the period of organogenesis through lactation. No treatment-related effects were observed at doses up to 20 mg/kg/day (12 times the MRHD, based on a body surface area comparison).Lactation
Risk Summary
There are no data on the presence of afamelanotide or any of its metabolites in human or animal milk, the effects on the breastfed infant, or the effect on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for SCENESSE and any potential adverse effects on the breastfed infant from SCENESSE or from the underlying maternal condition.Pediatric Use
The safety and effectiveness of SCENESSE have not been established in pediatric patients.
Geriatric Use
There were 10 subjects 65 years old and over in the clinical studies for EPP [ see Clinical Studies]. Of the 125 subjects treated with SCENESSE in these studies, 4 (3%) were 65 years of age and older. Clinical studies of SCENESSE did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
-
Descripton
SCENESSE (afamelanotide) implant is a controlled-release dosage form for subcutaneous administration. Afamelanotide is a melanocortin 1 receptor (MC1-R) agonist. The active ingredient afamelanotide acetate is a synthetic peptide containing 13 amino acids with molecular formula C 78H 111N 21O 19 xC 2H 4O 2 (3 ≤ x ≤ 4). The molecular weight of afamelanotide is 1646.85 (anhydrous free base). Afamelanotide acetate has the following structure:
Ac-Ser-Tyr-Ser-Nle-Glu-His-(D)Phe-Arg-Trp-Gly-Lys-Pro-Val-NH 2 xCH 3COOH.
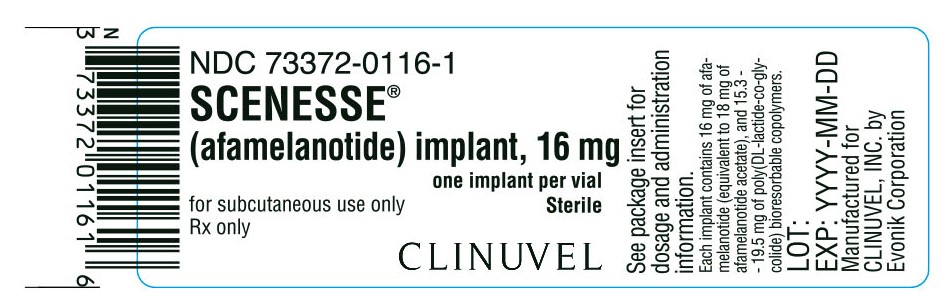
Afamelanotide is a white to off-white powder, freely soluble in water. Each SCENESSE implant contains 16 mg of afamelanotide (equivalent to 18 mg of afamelanotide acetate), and 15.3-19.5 mg of poly (DL-lactide-co-glycolide).
SCENESSE implant is a single, solid white to off-white, bioresorbable and sterile rod approximately 1.7 cm in length and 1.45 mm in diameter. The implant core comprises of the drug substance admixed with a poly (DL-lactide-co-glycolide) bioresorbable copolymer. -
Mechanism of Action
Afamelanotide is a synthetic tridecapeptide and a structural analog of α-melanocyte stimulating hormone (α-MSH).
Afamelanotide is a melanocortin receptor agonist and binds predominantly to MC1-R.Pharmacodynamics
Afamelanotide increases production of eumelanin in the skin independently of exposure to sunlight or artificial UV light sources.
Pharmacokinetics
The pharmacokinetics of afamelanotide following administration of a single subcutaneous implant of SCENESSE were evaluated in 12 healthy adults. High variability was observed in the plasma concentrations of afamelanotide and for most subjects (9 out of 12), the last measurable afamelanotide concentration was at 96 hours post-dose. The mean ± SD C max and AUC 0-inf were 3.7 ± 1.3 ng/mL and 138.9 ± 42.6 hr*ng/mL, respectively.
Absorption
The median T max was 36 hr.
Elimination
The apparent half-life of afamelanotide is approximately 15 hr when administered subcutaneously in a controlled release
implant.Metabolism
Afamelanotide may undergo hydrolysis. However, its metabolic profile has not been fully characterized.
Specific Populations
The effect of renal or hepatic impairment on the pharmacokinetics of afamelanotide is unknown.
Drug Interaction Studies
No drug interaction studies were conducted with afamelanotide.
-
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with SCENESSE.
Afamelanotide was negative in the Ames test, in vitro mouse lymphoma assay, and in vivo mouse bone marrow micronucleus assay.No effects on male or female fertility and reproductive performance were observed in rats at subcutaneous doses up to 20 mg/kg/day afamelanotide (12 times the MRHD, based on a body surface area comparison).
-
CLINICAL STUDIES
Three vehicle-controlled, parallel-group clinical trials of SCENESSE were conducted in subjects with EPP. Of these trials, two trials (Study CUV039, NCT 01605136, and Study CUV029, NCT 00979745) were designed to assess exposure to direct sunlight on days with no phototoxic pain. The two trials differed in the number of days of follow-up, the time windows within a day in which time spent outdoors was recorded, and how the amount of time spent in direct sunlight on each day was characterized. The subjects enrolled in these trials were primarily Caucasian (98%), the mean age was 40 years (range 18 to 74 years), and 53% of subjects were male and 47% were female.
Study CUV039 enrolled 93 subjects, of whom 48 received SCENESSE (16 mg of afamelanotide administered subcutaneously every 2 months), 45 received vehicle. Subjects received three implants and were followed for 180 days. On each study day, subjects recorded the number of hours spent in direct sunlight between 10 am and 6 pm, the number of hours spent in shade between 10 am and 6 pm, and whether they experienced any phototoxic pain that day. The primary endpoint was the total number of hours over 180 days spent in direct sunlight between 10 am and 6 pm on days with no pain. The median total number of hours over 180 days spent in direct sunlight between 10 am and 6 pm on days with no pain was 64.1 hours for subjects receiving SCENESSE and 40.5 hours for subjects receiving vehicle.
Study CUV029 enrolled 74 subjects, of whom 38 received SCENESSE (16 mg of afamelanotide administered subcutaneously every 2 months), 36 received vehicle. Subjects received five implants and were followed for 270 days. On each study day, subjects recorded the number of hours spent outdoors between 10 am and 3 pm, whether “most of the day” was spent in direct sunlight, shade, or a combination of both, and whether they experienced any phototoxic pain that day.
The primary endpoint was the total number of hours over 270 days spent outdoors between 10 am and 3 pm on days with no pain for which “most of the day” was spent in direct sunlight. This analysis does not include sun exposure on days for which subjects reported spending time in a combination of both direct sunlight and shade. The median total number of hours over 270 days spent outdoors between 10 am and 3 pm on days with no pain for which “most of the day” was spent in direct sunlight was 6.0 hours for subjects in the SCENESSE group and 0.75 hours for subjects in the vehicle group. -
HOW SUPPLIED
SCENESSE (afamelanotide) implant, 16 mg, for subcutaneous administration (NDC: 73372-0116-1) is supplied in a Type I amber glass vial sealed with a PTFE coated rubber stopper. Each vial contains one afamelanotide implant and is packaged individually in a cardboard box. SCENESSE implant is a solid white to off-white, bioresorbable and sterile rod approximately 1.7 cm in length and 1.45 mm in diameter.
Store in a refrigerator at 2°C – 8°C (36°F-46°F). Protect from light.
SCENESSE implants are not supplied with an implantation device for subcutaneous administration [ see Dosage and Administration]. -
88436-1 - Section Title Not Found In Database
Concomitant Measures
Advise patients to maintain sun and light protection measures during treatment with SCENESSE to prevent phototoxic reactions related to EPP.
Skin Monitoring
Advise patients that darkening of pre-existing nevi and ephelides may occur with use of SCENESSE. A full body skin examination is recommended twice yearly to monitor pre-existing and new skin pigmentary lesions.
Expelled Implant
Advise patients to contact their healthcare provider if the implant is expelled.Dressing removal
Advise patients that the dressing can be removed after 24 hours.
Insertion Site Care and Monitoring
Advise patients to monitor the insertion site after dressing removal and to report any reaction observed at the site to their healthcare provider. - PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
SCENESSE
afamelanotide implantProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 73372-0116 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AFAMELANOTIDE (UNII: QW68W3J66U) (AFAMELANOTIDE - UNII:QW68W3J66U) AFAMELANOTIDE 16 mg in 16 mg Product Characteristics Color white (white to off-white) Score Shape Size 17mm Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 73372-0116-1 1 in 1 CARTON 12/31/2019 1 1 mg in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA210797 12/31/2019 Labeler - CLINUVEL INC. (937954977)
Trademark Results [SCENESSE]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 SCENESSE 79229902 5724241 Live/Registered |
Clinuvel Pharmaceuticals Limited 2018-02-13 |
 SCENESSE 79088813 4008201 Dead/Cancelled |
Clinuvel Pharmaceuticals Limited 2010-05-10 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.