OXALIPLATIN injection, solution
Oxaliplatin by
Drug Labeling and Warnings
Oxaliplatin by is a Prescription medication manufactured, distributed, or labeled by Ingenus Pharmaceuticals, LLC, Ingenus Pharmaceuticals GmbH. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use OXALIPLATIN INJECTION safely and effectively.
See full prescribing information for OXALIPLATIN INJECTION.
OXALIPLATIN injection, for intravenous use
Initial U.S. Approval: 2002WARNING:ANAPHYLACTIC REACTIONS
See full prescribing information for complete boxed warning.
Anaphylactic reactions to oxaliplatin have been reported, and may occur within minutes of oxaliplatin administration. Epinephrine, corticosteroids, and antihistamines have been employed to alleviate symptoms. (5.1)
RECENT MAJOR CHANGES
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
- Administer oxaliplatin injection in combination with 5-fluorouracil/leucovorin every 2 weeks. (2.1):
- Day 1: Oxaliplatin injection 85 mg/m2intravenous infusion in 250 to 500 mL 5% Dextrose Injection and leucovorin 200 mg/ m2intravenous infusion in 5% Dextrose Injection both given over 120 minutes at the same time in separate bags using a Y-line, followed by 5-fluorouracil 400 mg/m2intravenous bolus given over 2 to 4 minutes, followed by 5-fluorouracil 600 mg/m2intravenous infusion in 500 mL 5% Dextrose Injection (recommended) as a 22-hour continuous infusion.
- Day 2: Leucovorin 200 mg/m2intravenous infusion over 120 minutes, followed by 5-fluorouracil 400 mg/m2intravenous bolus given over 2 to 4 minutes, followed by 5-fluorouracil 600 mg/m2intravenous infusion in 500 mL 5% Dextrose Injection (recommended) as a 22-hour continuous infusion.
- Reduce the dose of oxaliplatin injection to 75 mg/m2(adjuvant setting) or 65 mg/m2(advanced colorectal cancer) (2.2):
- if there are persistent Grade 2 neurosensory events that do not resolve.
- after recovery from Grade 3/4 gastrointestinal toxicities (despite prophylactic treatment) or grade 4 neutropenia, or febrile neutropenia, or Grade 3/4 thrombocytopenia. Delay next dose until neutrophils ≥ 1.5 x 109/L and platelets ≥ 75 x 109/L.
- For patients with severe renal impairment (creatinine clearance < 30 mL/min), the initial recommended dose is 65 mg/m2 (2.2):
- Discontinue oxaliplatin injection, USP if there are persistent Grade 3 neurosensory events. (2.2):
- Never prepare a final dilution with a sodium chloride solution or other chloride-containing solutions. (2.3)
DOSAGE FORMS AND STRENGTHS
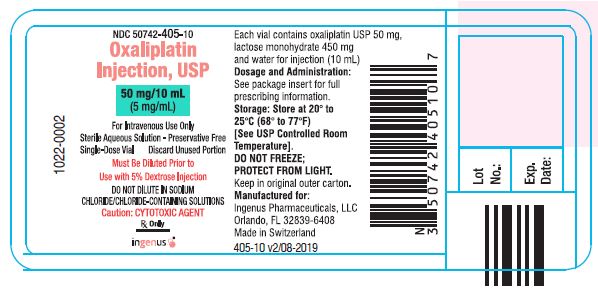
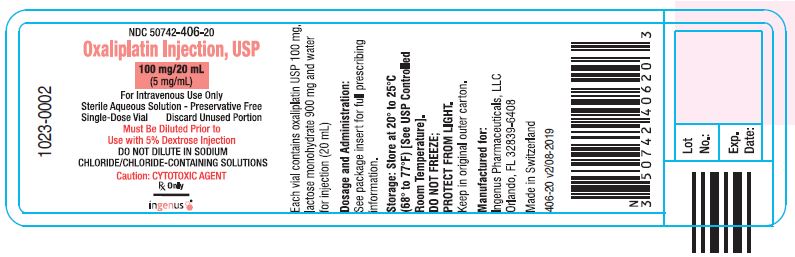
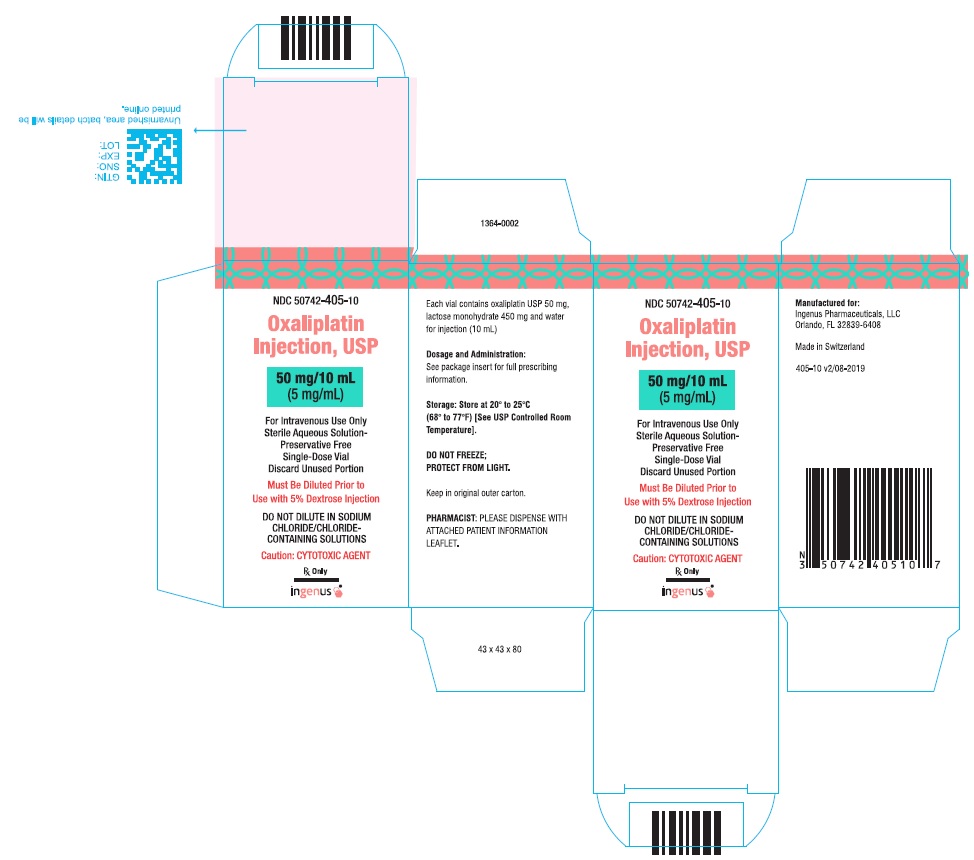
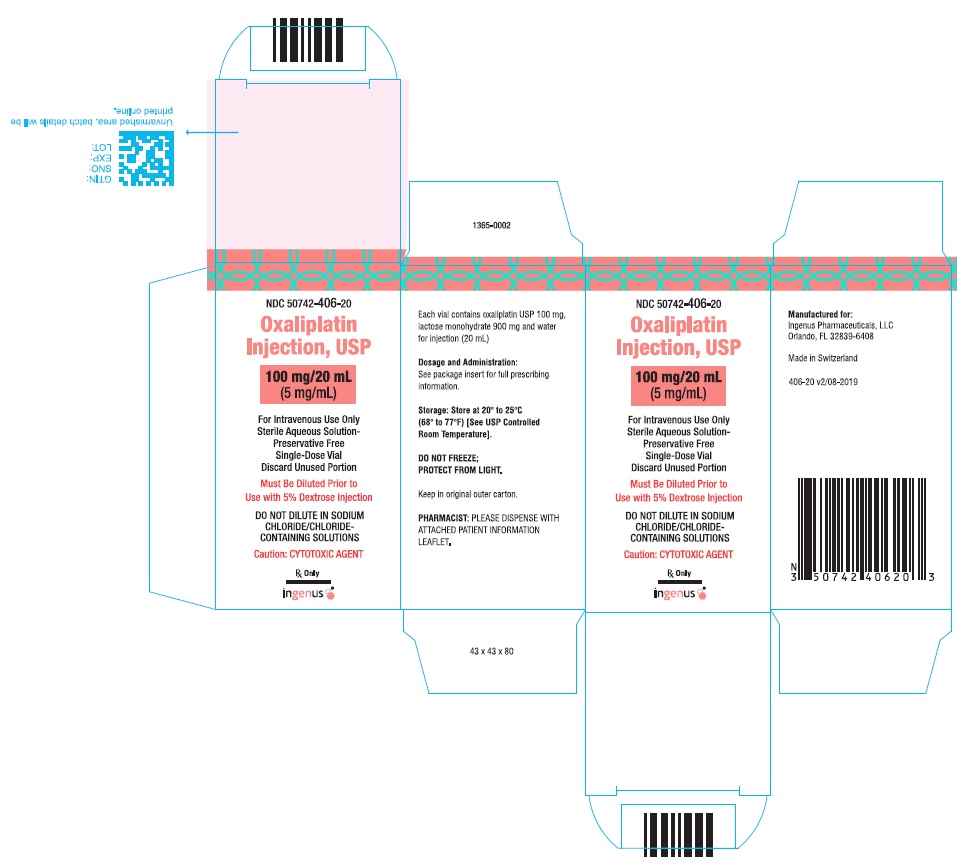
Single-dose vials of 50 mg or 100 mg oxaliplatin as a sterile, preservative-free, aqueous solution at a concentration of 5 mg/mL. (3)
WARNINGS AND PRECAUTIONS
- Allergic Reactions: Monitor for development of rash, urticaria, erythema, pruritus, bronchospasm, and hypotension. (5.1)
- Neuropathy: Reduce the dose or discontinue oxaliplatin if necessary. (5.2)
- Severe Neutropenia: Delay oxaliplatin until neutrophils are ≥1.5 x 109/L. Withhold oxaliplatin for sepsis. (5.3)
- Pulmonary Toxicity: May need to discontinue oxaliplatin until interstitial lung disease or pulmonary fibrosis are excluded. (5.4)
- Hepatotoxicity: Monitor liver function tests. (5.5)
- Cardiovascular Toxicity: Correct hypokalemia or hypomagnesemia prior to initiating oxaliplatin. (5.6)
- Rhabdomyolysis: Discontinue oxaliplatin if rhabdomyolysis occurs. (5.7)
- Pregnancy. Fetal harm can occur when administered to a pregnant woman. Women should be apprised of the potential harm to the fetus. (5.8, 8.1)
ADVERSE REACTIONS
Most common adverse reactions (incidence ≥ 40%) were peripheral sensory neuropathy, neutropenia, thrombocytopenia, anemia, nausea, increase in transaminases and alkaline phosphatase, diarrhea, emesis, fatigue and stomatitis. Other adverse reactions, including serious adverse reactions, have been reported. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Ingenus Pharmaceuticals, LLC at 1-877-748-1970 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2019
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: ANAPHYLACTIC REACTIONS
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosage
2.2 Dose Modification Recommendations
2.3 Preparation of Infusion Solution
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Allergic Reactions
5.2 Neurologic Toxicity
5.3 Severe Neutropenia
5.4 Pulmonary Toxicity
5.5 Hepatotoxicity
5.6 Cardiovascular Toxicity
5.7 Rhabdomyolysis
5.8 Use in Pregnancy
5.9 Recommended Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Patients With Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Combination Adjuvant Therapy With Oxaliplatin and Infusional 5-Fluorouracil/Leucovorin in Patients With Colon Cancer
14.2 Combination Therapy With Oxaliplatin and 5-Fluorouracil/Leucovorin in Patients Previously Untreated for Advanced Colorectal Cancer
14.3 Combination Therapy With Oxaliplatin and 5-Fluorouracil/Leucovorin in Previously Treated Patients With Advanced Colorectal Cancer
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
16.3 Handling and Disposal
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: ANAPHYLACTIC REACTIONS
Anaphylactic reactions to oxaliplatin have been reported, and may occur within minutes of oxaliplatin administration. Epinephrine, corticosteroids, and antihistamines have been employed to alleviate symptoms of anaphylaxis [see Warnings and Precautions (5.1)].
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
Oxaliplatin Injection should be administered under the supervision of a qualified physician experienced in the use of cancer chemotherapeutic agents. Appropriate management of therapy and complications is possible only when adequate diagnostic and treatment facilities are readily available.
2.1 Dosage
Administer oxaliplatin in combination with 5-fluorouracil/leucovorin every 2 weeks. For advanced disease, treatment is recommended until disease progression or unacceptable toxicity. For adjuvant use, treatment is recommended for a total of 6 months (12 cycles):
Day 1: Oxaliplatin 85 mg/m2 intravenous infusion in 250 to 500 mL 5% Dextrose Injection and leucovorin 200 mg/m2 intravenous infusion in 5% Dextrose Injection both given over 120 minutes at the same time in separate bags using a Y-line, followed by 5-fluorouracil 400 mg/m2 intravenous bolus given over 2 to 4 minutes, followed by 5-fluorouracil 600 mg/m2 intravenous infusion in 500 mL 5% Dextrose Injection (recommended) as a 22 hour continuous infusion.
Day 2: Leucovorin 200 mg/m2 intravenous infusion over 120 minutes, followed by 5-fluorouracil 400 mg/m2 intravenous bolus given over 2 to 4 minutes, followed by 5-fluorouracil 600 mg/m2 intravenous infusion in 500 mL 5% Dextrose Injection (recommended) as a 22 hour continuous infusion.
Figure 1
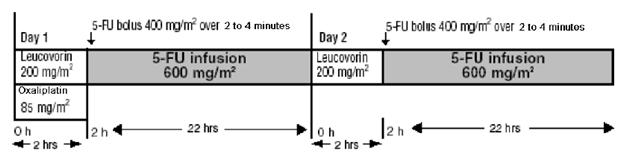
The administration of oxaliplatin does not require prehydration. Premedication with antiemetics, including 5-HT3 blockers with or without dexamethasone, is recommended.
For information on 5-fluorouracil and leucovorin, see the respective package inserts.
2.2 Dose Modification Recommendations
Prior to subsequent therapy cycles, patients should be evaluated for clinical toxicities and recommended laboratory tests [see Warnings and Precautions (5.6)]. Prolongation of infusion time for oxaliplatin from 2 hours to 6 hours may mitigate acute toxicities. The infusion times for 5-fluorouracil and leucovorin do not need to be changed.
Adjuvant Therapy in Patients With Stage III Colon Cancer
Neuropathy and other toxicities were graded using the NCI CTC scale version 1 [see Warnings and Precautions (5.2)]
For patients who experience persistent Grade 2 neurosensory events that do not resolve, a dose reduction of oxaliplatin to 75 mg/m2 should be considered. For patients with persistent Grade 3 neurosensory events, discontinuing therapy should be considered. The infusional 5 fluorouracil/leucovorin regimen need not be altered.
A dose reduction of oxaliplatin to 75 mg/m2 and infusional 5-fluorouracil to 300 mg/m2 bolus and 500 mg/m2 22 hour infusion is recommended for patients after recovery from Grade 3/4 gastrointestinal (despite prophylactic treatment) or Grade 4 neutropenia, or febrile neutropenia, or Grade 3/4 thrombocytopenia. The next dose should be delayed until: neutrophils ≥ 1.5 x 109/L and platelets ≥ 75 x 109/L.
Dose Modifications in Therapy in Previously Untreated and Previously Treated Patients With Advanced Colorectal Cancer
Neuropathy was graded using a study-specific neurotoxicity scale [see Warnings and Precautions (5.2)].Other toxicities were graded by the NCI CTC, Version 2.
For patients who experience persistent Grade 2 neurosensory events that do not resolve, a dose reduction of oxaliplatin to 65 mg/m2 should be considered. For patients with persistent Grade 3 neurosensory events, discontinuing therapy should be considered. The 5-fluorouracil/leucovorin regimen need not be altered.
A dose reduction of oxaliplatin to 65 mg/m2 and 5-fluorouracil by 20% (300 mg/m2 bolus and 500 mg/m2 22 hour infusion) is recommended for patients after recovery from Grade 3/4 gastrointestinal (despite prophylactic treatment), or Grade 4 neutropenia, or febrile neutropenia, or Grade 3/4 thrombocytopenia. The next dose should be delayed until: neutrophils ≥ 1.5 x 109/L and platelets ≥ 75 x 109/L.
Dose Modifications in Therapy for Patients With Renal Impairment
In patients with normal renal function or mild to moderate renal impairment, the recommended dose of oxaliplatin is 85 mg/m2. In patients with severe renal impairment, the initial recommended oxaliplatin dose should be reduced to 65 mg/m2[see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
2.3 Preparation of Infusion Solution
Do not freeze and protect from light the concentrated solution.
A final dilution must never be performed with a sodium chloride solution or other chloride-containing solutions.
The solution must be further diluted in an infusion solution of 250 to 500 mL of 5% Dextrose Injection.
After dilution with 250 to 500 mL of 5% Dextrose Injection, the shelf life is 6 hours at room temperature [20°to 25°C (68°to 77°F)] or up to 24 hours under refrigeration [2° to 8°C (36° to 46°F)]. After final dilution, protection from light is not required.
Oxaliplatin is incompatible in solution with alkaline medications or media (such as basic solutions of 5-fluorouracil) and must not be mixed with these or administered simultaneously through the same infusion line. The infusion line should be flushed with 5% Dextrose Injection prior to administration of any concomitant medication.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration and discarded if present.
Needles or intravenous administration sets containing aluminum parts that may come in contact with oxaliplatin should not be used for the preparation or mixing of the drug. Aluminum has been reported to cause degradation of platinum compounds.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Oxaliplatin should not be administered to patients with a history of known allergy to oxaliplatin or other platinum compounds [see Warnings and Precautions (5.1)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Allergic Reactions
See Boxed Warning
Grade 3/4 hypersensitivity, including anaphylactic/anaphylactoid reactions, to oxaliplatin has been observed in 2% to 3% of colon cancer patients. These allergic reactions which can be fatal, can occur within minutes of administration and at any cycle, and were similar in nature severity to those reported with other platinum-containing compounds, such as rash, urticaria, erythema, pruritus, and, rarely, brnchospasm and hypotension. The symptoms associated with hypersensitivity reactions reported in previously untreated patients were urticaria, pruritus, flushing of the face, diarrhea associated with oxaliplatin infusion, shorntness of breath, bronchospasm, diaphoresis, chest pains, hypotension, disorientation and syncope. These reactions are usually managed with standard epinephrine, corticosteroid, antihistamine therapy, and required discontinuation of therapy. Rechallenge is contraindicated in these patients [see contraindications (4)]. Drug-related deaths associated with platinum compounds from anaphylaxis have been reported.
5.2 Neurologic Toxicity
Oxaliplatin is associated with two types of neuropathy.
An acute, reversible, primarily peripheral, sensory neuropathy that is of early onset, occurring within hours or one to two days of dosing, that resolves within 14 days, and that frequently recurs with further dosing. The symptoms may be precipitated or exacerbated by exposure to cold temperature or cold objects and they usually present as transient paresthesia, dysesthesia and hypoesthesia in the hands, feet, perioral area, or throat. Jaw spasm, abnormal tongue sensation, dysarthria, eye pain, and a feeling of chest pressure have also been observed. The acute, reversible pattern of sensory neuropathy was observed in about 56% of study patients who received oxaliplatin with 5-fluorouracil/leucovorin. In any individual cycle acute neurotoxicity was observed in approximately 30% of patients. In adjuvant patients the median cycle of onset for Grade 3 peripheral sensory neuropathy was 9 in the previously treated patients the median number of cycles administered on the oxaliplatin with 5-fluorouracil/leucovorin combination arm was 6.
An acute syndrome of pharyngolaryngeal dysesthesia seen in 1% to 2% (Grade 3/4) of patients previously untreated for advanced colorectal cancer, and the previously treated patients, is characterized by subjective sensations of dysphagia or dyspnea, without any laryngospasm or bronchospasm (no stridor or wheezing). Ice (mucositis prophylaxis) should be avoided during the infusion of oxaliplatin because cold temperature can exacerbate acute neurological symptoms.
A persistent (> 14 days), primarily peripheral, sensory neuropathy that is usually characterized by paresthesias, dysesthesias, hypoesthesias, but may also include deficits in proprioception that can interfere with daily activities (e.g., writing, buttoning, swallowing, and difficulty walking from impaired proprioception). These forms of neuropathy occurred in 48% of the study patients receiving oxaliplatin with 5-fluorouracil/leucovorin. Persistent neuropathy can occur without any prior acute neuropathy event. The majority of the patients (80%) who developed Grade 3 persistent neuropathy progressed from prior Grade 1 or 2 events. These symptoms may improve in some patients upon discontinuation of oxaliplatin.
In the adjuvant colon cancer trial, neuropathy was graded using a prelisted module derived from the Neuro-Sensory section of the National Cancer Institute Common Toxicity Criteria (NCI CTC) scale, Version 1, as follows:
Table 1 – NCI CTC Grading for Neuropathy in Adjuvant Patients Grade
Definition
Grade 0
No change or none
Grade 1
Mild paresthesias, loss of deep tendon reflexes
Grade 2
Mild or moderate objective sensory loss, moderate paresthesias
Grade 3
Severe objective sensory loss or paresthesias that interfere with function
Grade 4
Not applicable
Peripheral sensory neuropathy was reported in adjuvant patients treated with the oxaliplatin combination with a frequency of 92% (all grades) and 13% (Grade 3). At the 28 day follow-up after the last treatment cycle, 60% of all patients had any grade (Grade 1 = 40%, Grade 2 = 16%, Grade 3 = 5%) peripheral sensory neuropathy decreasing to 39% at 6 months follow-up (Grade 1 = 31%, Grade 2 = 7%, Grade 3 = 1%) and 21% at 18 months of follow-up (Grade 1 = 17%, Grade 2 = 3%, Grade 3 = 1%).
In the advanced colorectal cancer studies, neuropathy was graded using a study-specific neurotoxicity scale, which was different from the NCI CTC scale, Version 2 (see below).
Table 2 - Grading Scale for Paresthesias/Dysesthesias in Advanced Colorectal Cancer Patients Grade
Definition
Grade 1
Resolved and did not interfere with functioning
Grade 2
Interfered with function but not daily activities
Grade 3
Pain or functional impairment that interfered with daily activities
Grade 4
Persistent impairment that is disabling or life-threatening
Overall, neuropathy was reported in patients previously untreated for advanced colorectal cancer in 82% (all grades) and 19% (Grade 3/4), and in the previously treated patients in 74% (all grades) and 7% (Grade 3/4) events. Information regarding reversibility of neuropathy was not available from the trial for patients who had not been previously treated for colorectal cancer.
Reversible Posterior Leukoencephalopathy Syndrome
Reversible Posterior Leukoencephalopathy Syndrome (RPLS, also known as PRES, Posterior Reversible Encephalopathy Syndrome) has been observed in clinical trials (< 0.1%) and postmarketing experience. Signs and symptoms of RPLS could be headache, altered mental functioning, seizures, abnormal vision from blurriness to blindness, associated or not with hypertension [see Adverse Reactions (6.2)]. Diagnosis of RPLS is based upon confirmation by brain imaging.
5.3 Severe Neutropenia
Grade 3 or 4 neutropenia occurred in 41 to 44% of patients with colorectal cancer treated with oxaliplatin in combination with 5-flurouracil (5-FU) and leucovorin compared to 5% with 5-FU plus leucovorin alone. Sepsis, neutropenic sepsis and septic shock have been reported in patients treated with oxaliplatin, including fatal outcomes [seeAdverse Reactions (6.1)].
Delay oxaliplatin until neutrophils are ≥ 1.5 x 109/L. Withhold oxaliplatin for sepsis or septic shock. Dose reduce oxaliplatin after recovery from Grade 4 neutropenia or febrile neutropenia [see Dosage and Administration (2.2)].
5.4 Pulmonary Toxicity
Oxaliplatin has been associated with pulmonary fibrosis (< 1% of study patients), which may be fatal. The combined incidence of cough and dyspnea was 7.4% (any grade) and < 1% (Grade 3) with no Grade 4 events in the oxaliplatin plus infusional 5-fluorouracil/leucovorin arm compared to 4.5% (any grade) and no Grade 3 and 0.1% Grade 4 events in the infusional 5-fluorouracil/leucovorin alone arm in adjuvant colon cancer patients. In this study, one patient died from eosinophilic pneumonia in the oxaliplatin combination arm. The combined incidence of cough, dyspnea and hypoxia was 43% (any grade) and 7% (Grade 3 and 4) in the oxaliplatin plus 5-fluorouracil/leucovorin arm compared to 32% (any grade) and 5% (Grade 3 and 4) in the irinotecan plus 5-fluorouracil/leucovorin arm of unknown duration for patients with previously untreated colorectal cancer. In case of unexplained respiratory symptoms such as non-productive cough, dyspnea, crackles, or radiological pulmonary infiltrates, oxaliplatin should be discontinued until further pulmonary investigation excludes interstitial lung disease or pulmonary fibrosis.
5.5 Hepatotoxicity
Hepatotoxicity as evidenced in the adjuvant study, by increase in transaminases (57% vs. 34%) and alkaline phosphatase (42% vs. 20%) was observed more commonly in the oxaliplatin combination arm than in the control arm. The incidence of increased bilirubin was similar on both arms. Changes noted on liver biopsies include: peliosis, nodular regenerative hyperplasia or sinusoidal alterations, perisinusoidal fibrosis, and veno-occlusive lesions. Hepatic vascular disorders should be considered, and if appropriate, should be investigated in case of abnormal liver function test results or portal hypertension, which cannot be explained by liver metastases [see Clinical Trials Experience (6.1)].
5.6 Cardiovascular Toxicity
QT prolongation and ventricular arrhythmias including fatal Torsade de Pointes have been reported in postmarketing experiences following oxaliplatin administration. ECG monitoring is recommended if therapy is initiated in patients with congestive heart failure, bradyarrhythmias, drugs known to prolong the QT interval, including Class Ia and III antiarrhythmics, and electrolyte abnormalities. Correct hypokalemia or hypomagnesemia prior to initiating oxaliplatin and monitor these electrolytes periodically during therapy. Avoid oxaliplatin in patients with congenital long QT syndrome [see Adverse Reactions (6.2)].
5.7 Rhabdomyolysis
Rhabdomyolysis, including fatal cases, has been reported in patients treated with oxaliplatin. Discontinue oxaliplatin if any signs or symptoms of rhabdomyolysis occur [see Adverse Reactions (6.2)].
5.8 Use in Pregnancy
Oxaliplatin may cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies of oxaliplatin in pregnant women. Women of childbearing potential should be advised to avoid becoming pregnant while receiving treatment with oxaliplatin [see Use in Specific Populations (8.1)].
5.9 Recommended Laboratory Tests
Standard monitoring of the white blood cell count with differential, hemoglobin, platelet count, and blood chemistries (including ALT, AST, bilirubin and creatinine) is recommended before each oxaliplatin cycle [see Dosage and Administration (2)].
There have been reports while on study and from post-marketing surveillance of prolonged prothrombin time and INR occasionally associated with hemorrhage in patients who received oxaliplatin plus 5-fluorouracil/leucovorin while on anticoagulants. Patients receiving oxaliplatin plus 5-fluorouracil/leucovorin and requiring oral anticoagulants may require closer monitoring.
-
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Anaphylaxis and Allergic reactions [see Boxed Warning, Warnings and Precautions (5.1) ]
- Neuropathy [see Warnings and Precautions (5.2) ]
- Severe Neutropenia [see Warnings and Precautions (5.3) ]
- Pulmonary Toxicities [see Warnings and Precautions (5.4) ]
- Hepatotoxicity [see Warnings and Precautions (5.5) ]
- Cardiovascular Toxicities [see Warnings and Precautions (5.6) ]
- Rhabdomyolysis [see Warnings and Precautions (5.7) ]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
More than 1100 patients with Stage II or III colon cancer and more than 4,000 patients with advanced colorectal cancer have been treated in clinical studies with oxaliplatin. The most common adverse reactions in patients with Stage II or III colon cancer receiving adjuvant therapy were peripheral sensory neuropathy, neutropenia, thrombocytopenia, anemia, nausea, increase in transaminases and alkaline phosphatase, diarrhea, emesis, fatigue and stomatitis. The most common adverse reactions in previously untreated and treated patients were peripheral sensory neuropathies, fatigue, neutropenia, nausea, emesis, and diarrhea [see Warnings and Precautions(5)]
Combination Adjuvant Therapy With Oxaliplatin and Infusional 5-Fluorouracil/Leucovorin in Patients With Colon Cancer
One thousand one hundred and eight patients with Stage II or III colon cancer, who had undergone complete resection of the primary tumor, have been treated in a clinical study with oxaliplatin in combination with infusional 5-fluorouracil/leucovorin [see Clinical Studies(14)] The incidence of Grade 3 or 4 adverse reactions was 70% on the oxaliplatin combination arm, and 31% on the infusional 5-fluorouracil/leucovorin arm. The adverse reactions in this trial are shown in the tables below. Discontinuation of treatment due to adverse reactions occurred in 15% of the patients receiving oxaliplatin and infusional 5-fluorouracil/leucovorin. Both 5 fluorouracil/leucovorin and oxaliplatin are associated with gastrointestinal or hematologic adverse reactions. When oxaliplatin is administered in combination with infusional 5 fluorouracil/leucovorin, the incidence of these events is increased.
The incidence of death within 28 days of last treatment, regardless of causality, was 0.5% (n = 6) in both the oxaliplatin combination and infusional 5-fluorouracil/leucovorin arms, respectively. Deaths within 60 days from initiation of therapy were 0.3% (n = 3) in both the oxaliplatin combination and infusional 5-fluorouracil/leucovorin arms, respectively. On the oxaliplatin combination arm, 3 deaths were due to sepsis/neutropenic sepsis, 2 from intracerebral bleeding and one from eosinophilic pneumonia. On the 5-fluorouracil/leucovorin arm, one death was due to suicide, 2 from Stevens-Johnson syndrome (1 patient also had sepsis), 1 unknown cause, 1 anoxic cerebral infarction and 1 probable abdominal aorta rupture.
The following table provides adverse reactions reported in the adjuvant therapy colon cancer clinical trial [see Clinical Studies(14)] by body system and decreasing order of frequency in the oxaliplatin and infusional 5-fluorouracil/leucovorin arm for events with overall incidences ≥ 5% and for NCI Grade 3/4 events with incidences ≥ 1%.
Table 3 - Adverse Reactions Reported in Patients With Colon Cancer Receiving Adjuvant Treatment (≥ 5% of all patients and with ≥ 1% NCI Grade 3/4 events) 1 Includes thrombosis related to the catheter
Oxaliplatin + 5-FU/LV
N = 1108
5-FU/LV
N = 1111
Adverse Reaction
(WHO/Pref)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
Any Event
100
70
99
31
Allergy/Immunology
Allergic Reaction
10
3
2
< 1
Constitutional Symptoms/Pain
Fatigue
44
4
38
1
Abdominal Pain
18
1
17
2
Dermatology/Skin
Skin Disorder
32
2
36
2
Injection Site Reaction1
11
3
10
3
Gastrointestinal
Nausea
74
5
61
2
Diarrhea
56
11
48
7
Vomiting
47
6
24
1
Stomatitis
42
3
40
2
Anorexia
13
1
8
<1
Fever/Infection
Fever
27
1
12
1
Infection
25
4
25
3
Neurology
Overall Peripheral Sensory Neuropathy
92
12
16
<1
The following table provides adverse reactions reported in the adjuvant therapy colon cancer clinical trial [see Clinical Studies (14)] by body system and decreasing order of frequency in the oxaliplatin and infusional 5-fluorouracil/leucovorin arm for events with overall incidences ≥ 5% but with incidences < 1% NCI Grade 3/4 events.
Table 4 -Adverse Reactions Reported in Patients With Colon Cancer Receiving Adjuvant Treatment (≥ 5% of all patients, but with < 1% NCI Grade 3/4 events) Adverse Reaction
Oxaliplatin + 5-FU/LV
N = 1108
5-FU/LV
N = 1111
(WHO/Pref)
All Grades (%)
All Grades (%)
Allergy/Immunology
Rhinitis
6
8
Constitutional Symptoms/Pain/Ocular/Visual
Epistaxis
16
12
Weight Increase
10
10
Conjunctivitis
9
15
Headache
7
5
Dyspnea
5
3
Pain
5
5
Lacrimation Abnormal
4
12
Dermatology/Skin
Alopecia
30
28
Gastrointestinal
Constipation
22
19
Taste Perversion
12
8
Dyspepsia
8
5
Metabolic
Phosphate Alkaline Increased
42
20
Neurology
Sensory Disturbance
8
1
Although specific events can vary, the overall frequency of adverse reactions was similar in men and women and in patients < 65 and ≥ 65 years. However, the following Grade 3/4 events were more common in females: diarrhea, fatigue, granulocytopenia, nausea and vomiting. In patients ≥ 65 years old, the incidence of Grade 3/4 diarrhea and granulocytopenia was higher than in younger patients. Insufficient subgroup sizes prevented analysis of safety by race. The following additional adverse reactions, were reported in ≥ 2% and < 5% of the patients in the oxaliplatin and infusional 5-fluorouracil/leucovorin combination arm (listed in decreasing order of frequency): pain, leukopenia, weight decrease, coughing.
The number of patients who developed secondary malignancies was similar; 62 in the oxaliplatin combination arm and 68 in the infusional 5-fluorouracil/leucovorin arm. An exploratory analysis showed that the number of deaths due to secondary malignancies was 1.96% in the oxaliplatin combination arm and 0.98% in infusional 5-fluorouracil/leucovorin arm. In addition, the number of cardiovascular deaths was 1.4% in the oxaliplatin combination arm as compared to 0.7% in the infusional 5-fluorouracil/leucovorin arm. Clinical significance of these findings is unknown.
Patients Previously Untreated for Advanced Colorectal Cancer
Two hundred and fifty-nine patients were treated in the oxaliplatin and 5-fluorouracil/leucovorin combination arm of the randomized trial in patients previously untreated for advanced colorectal cancer [see Clinical Studies(14)] The adverse reaction profile in this study was similar to that seen in other studies and the adverse reactions in this trial are shown in the tables below.
Both 5-fluorouracil and oxaliplatin are associated with gastrointestinal and hematologic adverse reactions. When oxaliplatin is administered in combination with 5-fluorouracil, the incidence of these events is increased.
The incidence of death within 30 days of treatment in the previously untreated for advanced colorectal cancer study, regardless of causality, was 3% with the oxaliplatin and 5-fluorouracil/leucovorin combination, 5% with irinotecan plus 5-fluorouracil/leucovorin, and 3% with oxaliplatin plus irinotecan. Deaths within 60 days from initiation of therapy were 2.3% with the oxaliplatin and 5-fluorouracil/leucovorin combination, 5.1% with irinotecan plus 5-fluorouracil/leucovorin, and 3.1% with oxaliplatin plus irinotecan.
The following table provides adverse reactions reported in the previously untreated for advanced colorectal cancer study [see Clinical Studies(14)] by body system and decreasing order of frequency in the oxaliplatin and 5-fluorouracil/leucovorin combination arm for events with overall incidences ≥ 5% and for Grade 3/4 events with incidences ≥ 1%.
Table 5 -Adverse Reactions Reported in Patients Previously Untreated for Advanced Colorectal Cancer Clinical Trial (≥ 5% of all patients and with ≥ 1% NCI Grade 3/4 events) * Not otherwise specified
** Absolute neutrophil count
Adverse Reaction
(WHO/Pref)
Oxaliplatin + 5-FU/LV
N = 259
Irinotecan + 5FU/LV
N = 256
Oxaliplatin + Irinotecan
N = 258
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
Any Event
99
82
98
70
99
76
Allergy/Immunology
Hypersensitivity
12
2
5
0
6
1
Cardiovascular
Thrombosis
6
5
6
6
3
3
Hypotension
5
3
6
3
4
3
Constitutional Symptoms/Pain/Ocular/Visual
Fatigue
70
7
58
11
66
16
Abdominal Pain
29
8
31
7
39
10
Myalgia
14
2
6
0
9
2
Pain
7
1
5
1
6
1
Vision abdominal
5
0
2
1
6
1
Neuralgia
5
0
0
0
2
1
Dermatology/Skin
Skin reaction – hand/foot
7
1
2
1
1
0
Injection site reaction
6
0
1
0
4
1
Gastrointestinal
Nausea
71
6
67
15
83
19
Diarrhea
56
12
65
29
76
25
Vomiting
41
4
43
13
64
23
Stomatitis
38
0
25
1
19
1
Anorexia
35
2
25
4
27
5
Constipation
32
4
27
2
21
2
Diarrhea-colostomy
13
2
16
7
16
3
Gastrointestinal NOS*
5
2
4
2
3
2
Hematology/Infection
Infection normal ANC**
10
4
5
1
7
2
Infection low ANC**
8
8
12
11
9
8
Lymphopenia
6
2
4
1
5
2
Febrile neutropenia
4
4
15
14
12
11
Hepatic/Metabolic/Laboratory/Renal
Hyperglycemia
14
2
11
3
12
3
Hypokalemia
11
3
7
4
6
2
Dehydration
9
5
16
11
14
7
Hypoalbuminemia
8
0
5
2
9
1
Hyponatremia
8
2
7
4
4
1
Urinary frequency
5
1
2
1
3
1
Neurology
Overall Neuropathy
82
19
18
2
69
7
Paresthesias
77
18
16
2
62
6
Pharyngo-laryngeal dysesthesias
38
2
1
0
28
1
Neuro-sensory
12
1
2
0
9
1
Neuro NOS*
1
0
1
0
1
0
Pulmonary
Cough
35
1
25
2
17
1
Dyspnea
18
7
14
3
11
2
Hiccups
5
1
2
0
3
2
The following table provides adverse reactions reported in the previously untreated for advanced colorectal cancer study [see Clinical Studies (14)] by body system and decreasing order of frequency in the oxaliplatin and 5-fluorouracil/leucovorin combination arm for events with overall incidences ≥ 5% but with incidences < 1% NCI Grade 3/4 events.
Table 6 -Adverse Reactions Reported in Patients Previously Untreated for Advanced Colorectal Cancer Clinical Trial (≥ 5% of all patients but with < 1% NCI Grade 3/4 events) * Absolute neutrophil count
Oxaliplatin + 5-FU/LV N = 259
Irinotecan + 5-FU/LV N = 256
Oxaliplatin + Irinotecan N = 258
Adverse Reaction
(WHO/Pref)
All Grades
(%)
All Grades
(%)
All Grades
(%)
Allergy/Immunology
Rash
11
4
7
Rhinitis allergic
10
6
6
Cardiovascular
Edema
15
13
10
Constitutional Symptoms/Pain/Ocular/Visual
Headache
13
6
9
Weight Loss
11
9
11
Epistaxis
10
2
2
Tearing
9
1
2
Rigors
8
2
7
Dysphasia
5
3
3
Sweating
5
6
12
Arthralgia
5
5
8
Dermatology/Skin
Alopecia
38
44
67
Flushing
7
2
5
Pruritis
6
4
2
Dry Skin
6
2
5
Gastrointestinal
Taste perversion
14
6
8
Dyspepsia
12
7
5
Flatulence
9
6
5
Mouth Dryness
5
2
3
Hematology/Infection
Fever Normal ANC*
16
9
9
Hepatic/Metabolic/Laboratory/Renal
Hypocalcemia
7
5
4
Elevated Creatinine
4
4
5
Neurology
Insomnia
13
9
11
Depression
9
5
7
Dizziness
8
6
10
Anxiety
5
2
6
Adverse reactions were similar in men and women and in patients < 65 and ≥ 65 years, but older patients may have been more susceptible to diarrhea, dehydration, hypokalemia, leukopenia, fatigue and syncope. The following additional adverse reactions, at least possibly related to treatment and potentially important, were reported in ≥ 2% and < 5% of the patients in the oxaliplatin and 5-fluorouracil/leucovorin combination arm (listed in decreasing order of frequency): metabolic, pneumonitis, catheter infection, vertigo, prothrombin time, pulmonary, rectal bleeding, dysuria, nail changes, chest pain, rectal pain, syncope, hypertension, hypoxia, unknown infection, bone pain, pigmentation changes, and urticaria.
Previously Treated Patients with Advanced Colorectal Cancer
Four hundred and fifty patients (about 150 receiving the combination of oxaliplatin and 5-fluorouracil/leucovorin) were studied in a randomized trial in patients with refractory and relapsed colorectal cancer [see Clinical Studies (14)]. The adverse reaction profile in this study was similar to that seen in other studies and the adverse reactions in this trial are shown in the tables below.
Thirteen percent of patients in the oxaliplatin and 5-fluorouracil/leucovorin combination arm and 18% in the 5-fluorouracil/leucovorin arm of the previously treated study had to discontinue treatment because of adverse effects related to gastrointestinal, or hematologic adverse reactions, or neuropathies. Both 5-fluorouracil and oxaliplatin are associated with gastrointestinal and hematologic adverse reactions. When oxaliplatin is administered in combination with 5-fluorouracil, the incidence of these events is increased.
The incidence of death within 30 days of treatment in the previously treated study, regardless of causality, was 5% with the oxaliplatin and 5-fluorouracil/leucovorin combination, 8% with oxaliplatin alone, and 7% with 5-fluorouracil/leucovorin. Of the 7 deaths that occurred on the oxaliplatin and 5-fluorouracil/leucovorin combination arm within 30 days of stopping treatment, 3 may have been treatment related, associated with gastrointestinal bleeding or dehydration.
The following table provides adverse reactions reported in the previously treated study [see Clinical Studies (14)]. by body system and in decreasing order of frequency in the oxaliplatin and 5-fluorouracil/leucovorin combination arm for events with overall incidences ≥ 5% and for Grade 3/4 events with incidences ≥ 1%. This table does not include hematologic and blood chemistry abnormalities; these are shown separately below.
Table 7 -Adverse Reactions Reported in Previously Treated Colorectal Cancer Clinical Trial (≥ 5% of all patients and with ≥ 1% NCI Grade 3/4 events) 5-FU/LV
(N = 142)
Oxaliplatin
(N = 153)
Oxaliplatin + 5-FU/LV
(N = 150)
Adverse Reaction
(WHO/Pref)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
Any Event
98
41
100
46
99
73
Cardiovascular
Dyspnea
11
2
13
7
20
4
Coughing
9
0
11
0
19
1
Edema
13
1
10
1
15
1
Thromboembolism
4
2
2
1
9
8
Chest Pain
4
1
5
1
8
1
Constitutional Symptoms/Pain
Fatigue
52
6
61
9
68
7
Back Pain
16
4
11
0
19
3
Pain
9
3
14
3
15
2
Dermatology/Skin
Injection Site Reaction
5
1
9
0
10
3
Gastrointestinal
Diarrhea
44
3
46
4
67
11
Nausea
59
4
64
4
65
11
Vomiting
27
4
37
4
40
9
Stomatitis
32
3
14
0
37
3
Abdominal Pain
31
5
31
7
33
4
Anorexia
20
1
20
2
29
3
Gastroesophageal Reflux
3
0
1
0
5
2
Hematology/Infection
Fever
23
1
25
1
29
1
Febrile Neutropenia
1
1
0
0
6
6
Hepatic/Metabolic/Laboratory/Renal
Hypokalemia
3
1
3
2
9
4
Dehydration
6
4
5
3
8
3
Neurology
Neuropathy
17
0
76
7
74
7
Acute
10
0
65
5
56
2
Persistent
9
0
43
3
48
6
The following table provides adverse reactions reported in the previously treated study [see Clinical Studies (14)] by body system and in decreasing order of frequency in the oxaliplatin and 5-fluorouracil/leucovorin combination arm for events with overall incidences ≥ 5% but with incidences < 1% NCI Grade 3/4 events.
Table 8 -Adverse Reactions Reported in Previously Treated Colorectal Cancer Clinical Trial (≥ 5% of all patients but with < 1% NCI Grade 3/4 events) 5-FU/LV
N = 142
Oxaliplatin
(N = 153)
Oxaliplatin + 5-FU/LV
(N = 150)
Adverse Reaction
(WHO/Pref)
All Grades
(%)
All Grades
(%)
All Grades
(%)
Allergy/Immunology
Rhinitis
4
6
15
Allergic Reaction
1
3
10
Rash
5
5
9
Cardiovascular
Peripheral Edema
11
5
10
Constitutional Symptoms/Pain/Ocular/Visual
Headache
8
13
17
Arthralgia
10
7
10
Epistaxis
1
2
9
Abnormal Lacrimation
6
1
7
Rigors
6
9
7
Dermatology/Skin
Hand-Foot Syndrome
13
1
11
Flushing
2
3
10
Alopecia
3
3
7
Gastrointestinal
Constipation
23
31
32
Dyspepsia
10
7
14
Taste Perversion
1
5
13
Mucositis
10
2
7
Flatulence
6
3
5
Hepatic/Metabolic/Laboratory/Renal
Hematuria
4
0
6
Dysuria
1
1
6
Neurology
Dizziness
8
7
13
Insomnia
4
11
9
Pulmonary
Upper Resp Tract Infection
4
7
10
Pharygitis
10
2
9
Hiccup
0
2
5
Adverse reactions were similar in men and women and in patients < 65 and ≥ 65 years, but older patients may have been more susceptible to dehydration, diarrhea, hypokalemia and fatigue. The following additional adverse reactions, at least possibly related to treatment and potentially important, were reported in ≥ 2% and < 5% of the patients in the oxaliplatin and 5-fluorouracil/leucovorin combination arm (listed in decreasing order of frequency): anxiety, myalgia, erythematous rash, increased sweating, conjunctivitis, weight decrease, dry mouth, rectal hemorrhage, depression, ataxia, ascites, hemorrhoids, muscle weakness, nervousness, tachycardia, abnormal micturition frequency, dry skin, pruritus, hemoptysis, purpura, vaginal hemorrhage, melena, somnolence, pneumonia, proctitis, involuntary muscle contractions, intestinal obstruction, gingivitis, tenesmus, hot flashes, enlarged abdomen, urinary incontinence.
Hematologic Changes
The following tables list the hematologic changes occurring in ≥ 5% of patients, based on laboratory values and NCI grade, with the exception of those events occurring in adjuvant patients and anemia in the patients previously untreated for advanced colorectal cancer, respectively, which are based on AE reporting and NCI grade alone.
Table 9 - Adverse Hematologic Reactions in Patients with Colon Cancer Receiving Adjuvant Therapy (≥ 5% of patients) Hematology
Parameter
Oxaliplatin + 5-FU/LV
(N = 1108)
5-FU/LV
(N = 1111)
All Grades (%)
Grade 3/4
All Grades (%)
Grade 3/4
Anemia
76
1
67
<1
Neutropenia
79
41
40
5
Thrombocytopenia
77
2
19
<1
Table 10 -Adverse Hematologic Reactions in Patients Previously Untreated for Advanced Colorectal Cancer (≥ 5% of patients) Hematology
Parameter
Oxaliplatin + 5-FU/LV
N = 259
Irinotecan + 5-FU/LV
N = 256
Oxaliplatin + Irinotecan
N = 258
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
Anemia
27
3
28
4
25
3
Leukopenia
85
20
84
23
76
24
Neutropenia
81
53
77
44
71
36
Thrombocytopenia
71
5
26
2
44
4
Table 11 -Adverse Hematologic Reactions in Previously Treated Patients (≥ 5% of patients) Hematology
Parameter
5-FU/LV
(N = 142)
Oxaliplatin
(N = 153)
Oxaliplatin + 5-FU/LV
(N = 150)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
Anemia
68
2
64
1
81
2
Leukopenia
34
1
13
0
76
19
Neutropenia
25
5
7
0
73
44
Thrombocytopenia
20
0
30
3
64
4
Thrombocytopenia was frequently reported with the combination of oxaliplatin and infusional 5-fluorouracil/leucovorin. The incidence of all hemorrhagic events in the adjuvant and previously treated patients was higher on the oxaliplatin combination arm compared to the infusional 5-fluorouracil/leucovorin arm. These events included gastrointestinal bleeding, hematuria, and epistaxis. In the adjuvant trial, two patients died from intracerebral hemorrhages.
The incidence of Grade 3/4 thrombocytopenia was 2% in adjuvant patients with colon cancer. In patients treated for advanced colorectal cancer the incidence of Grade 3/4 thrombocytopenia was 3% to 5%, and the incidence of these events was greater for the combination of oxaliplatin and 5-fluorouracil/leucovorin over the irinotecan plus 5-fluorouracil/leucovorin or 5-fluorouracil/leucovorin control groups. Grade 3/4 gastrointestinal bleeding was reported in 0.2% of adjuvant patients receiving oxaliplatin and 5-fluorouracil/leucovorin. In the previously untreated patients, the incidence of epistaxis was 10% in the oxaliplatin and 5-fluorouracil/leucovorin arm, and 2% and 1%, respectively, in the irinotecan plus 5-fluorouracil/leucovorin or irinotecan plus oxaliplatin arms.
Neutropenia
Neutropenia was frequently observed with the combination of oxaliplatin and 5-fluorouracil/leucovorin, with Grade 3 and 4 events reported in 29% and 12% of adjuvant patients with colon cancer, respectively. In the adjuvant trial, 3 patients died from sepsis/neutropenic sepsis. Grade 3 and 4 events were reported in 35% and 18% of the patients previously untreated for advanced colorectal cancer, respectively. Grade 3 and 4 events were reported in 27% and 17% of previously treated patients, respectively. In adjuvant patients the incidence of either febrile neutropenia (0.7%) or documented infection with concomitant Grade 3/4 neutropenia (1.1%) was 1.8% in the oxaliplatin and 5-fluorouracil/leucovorin arm. The incidence of febrile neutropenia in the patients previously untreated for advanced colorectal cancer was 15% (3% of cycles) in the irinotecan plus 5-fluorouracil/leucovorin arm and 4% (less than 1% of cycles) in the oxaliplatin and 5-fluorouracil/leucovorin combination arm. Additionally, in this same population, infection with Grade 3 or 4 neutropenia was 12% in the irinotecan plus 5-fluorouracil/leucovorin, and 8% in the oxaliplatin and 5-fluorouracil/leucovorin combination. The incidence of febrile neutropenia in the previously treated patients was 1% in the 5-fluorouracil/leucovorin arm and 6% (less than 1% of cycles) in the oxaliplatin and 5-fluorouracil/leucovorin combination arm.
Gastrointestinal
In patients receiving the combination of oxaliplatin plus infusional 5-fluorouracil/leucovorin for adjuvant treatment for colon cancer the incidence of Grade 3/4 nausea and vomiting was greater than those receiving infusional 5-fluorouracil/leucovorin alone (see table). In patients previously untreated for advanced colorectal cancer receiving the combination of oxaliplatin and 5-fluorouracil/leucovorin, the incidence of Grade 3 and 4 vomiting and diarrhea was less compared to irinotecan plus 5-fluorouracil/leucovorin controls (see table). In previously treated patients receiving the combination of oxaliplatin and 5-fluorouracil/leucovorin, the incidence of Grade 3 and 4 nausea, vomiting, diarrhea, and mucositis/stomatitis increased compared to 5-fluorouracil/leucovorin controls (see table).
The incidence of gastrointestinal adverse reactions in the previously untreated and previously treated patients appears to be similar across cycles. Premedication with antiemetics, including 5-HT3 blockers, is recommended. Diarrhea and mucositis may be exacerbated by the addition of oxaliplatin to 5-fluorouracil/leucovorin, and should be managed with appropriate supportive care. Since cold temperature can exacerbate acute neurological symptoms, ice (mucositis prophylaxis) should be avoided during the infusion of oxaliplatin.
Dermatologic
Oxaliplatin did not increase the incidence of alopecia compared to 5-fluorouracil/leucovorin alone. No complete alopecia was reported. The incidence of Grade 3/4 skin disorders was 2% in both the oxaliplatin plus infusional 5-fluorouracil/leucovorin and the infusional 5-fluorouracil/leucovorin alone arms in the adjuvant colon cancer patients. The incidence of hand-foot syndrome in patients previously untreated for advanced colorectal cancer was 2% in the irinotecan plus 5-fluorouracil/leucovorin arm and 7% in the oxaliplatin and 5-fluorouracil/leucovorin combination arm. The incidence of hand-foot syndrome in previously treated patients was 13% in the 5-fluorouracil/leucovorin arm and 11% in the oxaliplatin and 5-fluorouracil/leucovorin combination arm.
Intravenous Site Reactions
Extravasation, in some cases including necrosis, has been reported.
Injection site reaction, including redness, swelling, and pain, has been reported.
Anticoagulation and Hemorrhage
There have been reports while on study and from postmarketing surveillance of prolonged prothrombin time and INR occasionally associated with hemorrhage in patients who received oxaliplatin plus 5-fluorouracil/leucovorin while on anticoagulants. Patients receiving oxaliplatin plus 5-fluorouracil/leucovorin and requiring oral anticoagulants may require closer monitoring.
Renal
About 5% to 10% of patients in all groups had some degree of elevation of serum creatinine. The incidence of Grade 3/4 elevations in serum creatinine in the oxaliplatin and 5-fluorouracil/leucovorin combination arm was 1% in the previously treated patients. Serum creatinine measurements were not reported in the adjuvant trial.
Hepatic
Hepatotoxicity (defined as elevation of liver enzymes) appears to be related to oxaliplatin combination therapy [see Warnings and Precautions(5.6)] The following tables list the clinical chemistry changes associated with hepatic toxicity occurring in ≥ 5% of patients, based on adverse reactions reported and NCI CTC grade for adjuvant patients and patients previously untreated for advanced colorectal cancer, laboratory values and NCI CTC grade for previously treated patients.
Table 12 -Adverse Hepatic Reactions in Patients With Stage II or III Colon Cancer Receiving Adjuvant Therapy (≥ 5% of patients)
Oxaliplatin + 5-FU/LV
(N = 1108)
5-FU/LV
(N = 1111)
Hepatic Parameter
All Grades (%)
Grade 3/4
All Grades (%)
Grade 3/4
Increase in transaminases
57
2
34
1
ALP increased
42
<1
20
<1
Bilirubinaemia
20
4
20
5
Table 13 -Adverse Hepatic – Clinical Chemistry Abnormalities in Patients Previously Untreated for Advanced Colorectal Cancer (≥ 5% of Patients)
Oxaliplatin + 5-FU/LV
N=259
Irinotecan + 5-FU/LV
N = 256
Oxaliplatin + Irinotecan
N = 258
Clinical
Chemistry
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade ¾
(%)
ALT (SGPT-ALAT)
6
1
2
0
5
2
AST (SGOT-ASAT)
17
1
2
1
11
1
Alkaline Phosphatase
16
0
8
0
14
2
Total Bilirubin
6
1
3
1
3
2
Table 14 -Adverse Hepatic – Clinical Chemistry Abnormalities in Previously Treated Patients (≥ 5% of Patients)
5-FU/LV
(N = 142)
Oxaliplatin
(N = 153)
Oxaliplatin
+ 5-FU/LV (N = 150)
Clinical
Chemistry
All Grades
(%)
Grade ¾
(%)
All Grades
(%)
Grade 3/4
(%)
All Grades
(%)
Grade 3/4
(%)
ALT (SGPT-ALAT)
28
3
36
1
31
0
AST (SGOT-ASAT)
39
2
54
4
47
0
Total Bilirubin
22
6
13
5
13
1
The incidence of thromboembolic events in adjuvant patients with colon cancer was 6% (1.8% Grade 3/4) in the infusional 5-fluorouracil/leucovorin arm and 6% (1.2% Grade 3/4) in the oxaliplatin and infusional 5-fluorouracil/leucovorin combined arm, respectively. The incidence was 6% and 9% of the patients previously untreated for advanced colorectal cancer and previously treated patients in the oxaliplatin and 5-fluorouracil/leucovorin combination arm, respectively.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of oxaliplatin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a whole:
angioedema, anaphylactic shock
Cardiovascular disorders:
QT prolongation leading to ventricular arrhythmias including fatal Torsade de Pointes
Central and peripheral nervous system disorders:
loss of deep tendon reflexes, dysarthria, Lhermitte's sign, cranial nerve palsies, fasciculations, convulsion, Reversible Posterior Leukoencephalopathy Syndrome (RPLS, also known as PRES).
Hearing and vestibular system disorders:
Deafness
Infections:
septic shock, including fatal outcomes
Infusion reactions/hypersensitivity:
laryngospasm
Liver and gastrointestinal system disorders:
severe diarrhea/vomiting resulting in hypokalemia, colitis (including Clostridium difficile diarrhea), metabolic acidosis; ileus; intestinal obstruction, pancreatitis; veno-occlusive disease of liver also known as sinusoidal obstruction syndrome, and perisinusoidal fibrosis which rarely may progress.
Platelet, bleeding, and clotting disorders:
immuno-allergic thrombocytopenia
prolongation of prothrombin time and of INR in patients receiving anticoagulants
Red blood cell disorders:
hemolytic uremic syndrome, immuno-allergic hemolytic anemia
Renal disorders:
Acute tubular necrosis, acute interstitial nephritis and acute renal failure
Respiratory system disorders:
pulmonary fibrosis, and other interstitial lung diseases (sometimes fatal)
Vision disorders:
decrease of visual acuity, visual field disturbance, optic neuritis and transient vision loss (reversible following therapy discontinuation)
-
7 DRUG INTERACTIONS
No specific cytochrome P-450-based drug interaction studies have been conducted. No pharmacokinetic interaction between 85 mg/m2 oxaliplatin and 5-fluorouracil/leucovorin has been observed in patients treated every 2 weeks. Increases of 5-fluorouracil plasma concentrations by approximately 20% have been observed with doses of 130 mg/m2 oxaliplatin dosed every 3 weeks. Because platinum-containing species are eliminated primarily through the kidney, clearance of these products may be decreased by coadministration of potentially nephrotoxic compounds; although, this has not been specifically studied [see Clinical Pharmacology (12.3)]
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Based on direct interaction with DNA, oxaliplatin may cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies of oxaliplatin in pregnant women. Reproductive toxicity studies in rats demonstrated adverse effects on fertility and embryo-fetal development at maternal doses that were below the recommended human dose based on body surface area. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant and use effective contraception while receiving treatment with oxaliplatin.
Pregnant rats were administered oxaliplatin at less than one-tenth the recommended human dose based on body surface area during gestation days 1 to 5 (pre-implantation), 6 to 10, or 11 to 16 (during organogenesis). Oxaliplatin caused developmental mortality (increased early resorptions) when administered on days 6 to 10 and 11 to 16 and adversely affected fetal growth (decreased fetal weight, delayed ossification) when administered on days 6 to 10. Administration of oxaliplatin to male and female rats prior to mating resulted in 97% post-implantation loss in animals that received approximately one-seventh the recommended human dose based on the body surface area.
8.3 Nursing Mothers
It is not known whether oxaliplatin or its derivatives are excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from oxaliplatin, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The effectiveness of oxaliplatin in children has not been established. Oxaliplatin has been tested in 2 Phase 1 and 2 Phase 2 trials in 235 patients ages 7 months to 22 years with solid tumors (see below) and no significant activity observed.
In a Phase 1/2 study, oxaliplatin was administered as a 2-hour intravenous infusion on Days 1, 8 and 15 every 4 weeks (1 cycle), for a maximum of 6 cycles, to 43 patients with refractory or relapsed malignant solid tumors, mainly neuroblastoma and osteosarcoma. Twenty eight pediatric patients in the Phase 1 study received oxaliplatin at 6 dose levels starting at 40 mg/m2 with escalation to 110 mg/m2. The dose limiting toxicity (DLT) was sensory neuropathy at the 110 mg/m2 dose. Fifteen patients received oxaliplatin at a dose of 90 mg/m2 intravenous in the Phase 2 portion of the study. At this dose, paresthesia (60%, G3/4: 7%), fever (40%, G3/4: 7%) and thrombocytopenia (40%, G3/4: 27%) were the main adverse reactions. No responses were observed.
In a second Phase 1 study, oxaliplatin was administered to 26 pediatric patients as a 2-hour intravenous infusion on day 1 every 3 weeks (1 cycle) at 5 dose levels starting at 100 mg/m2 with escalation to 160 mg/m2, for a maximum of 6 cycles. In a separate cohort, oxaliplatin 85 mg/m2 was administered on day 1 every 2 weeks, for a maximum of 9 doses. Patients had metastatic or unresectable solid tumors mainly neuroblastoma and ganglioneuroblastoma. No responses were observed. The DLT was sensory neuropathy at the 160 mg/m2 dose. Based on these studies, oxaliplatin 130 mg/m2 as a 2-hour intravenous infusion on day 1 every 3 weeks (1 cycle) was used in subsequent Phase 2 studies. A dose of 85 mg/m2 on day 1 every 2 weeks was also found to be tolerable.
In one Phase 2 study, 43 pediatric patients with recurrent or refractory embryonal CNS tumors received oxaliplatin 130 mg/m2 every 3 weeks for a maximum of 12 months in absence of progressive disease or unacceptable toxicity. In patients < 10 kg the oxaliplatin dose used was 4.3 mg/kg. The most common adverse reactions reported were leukopenia (67%, G3/4: 12%), anemia (65%, G3/4: 5%), thrombocytopenia (65%, G3/4: 26%), vomiting (65%, G3/4: 7%), neutropenia (58%, G3/4: 16%) and sensory neuropathy (40%, G3/4: 5%). One partial response was observed.
In a second Phase 2 study, 123 pediatric patients with recurrent solid tumors, including neuroblastoma, osteosarcoma, Ewing sarcoma or peripheral PNET, ependymoma, rhabdomyosarcoma, hepatoblastoma, high grade astrocytoma, brain stem glioma, low grade astrocytoma, malignant germ cell tumor and other tumors of interest received oxaliplatin 130 mg/m2 every 3 weeks for a maximum of 12 months or 17 cycles. In patients ≤ 12 months old the oxaliplatin dose used was 4.3 mg/kg. The most common adverse reactions reported were sensory neuropathy (52%, G3/4: 12%), thrombocytopenia (37%, G3/4: 17%), anemia (37%, G3/4: 9%), vomiting (26%, G3/4: 4%), ALT increased (24%, G3/4: 6%), AST increased (24%, G3/4: 2%), and nausea (23%, G3/4: 3%). Two partial responses were observed.
The pharmacokinetic parameters of ultrafiltrable platinum have been evaluated in 105 pediatric patients during the first cycle. The mean clearance in pediatric patients estimated by the population pharmacokinetic analysis was 4.7 L/h. The inter-patient variability of platinum clearance in pediatric cancer patients was 41%. Mean platinum pharmacokinetic parameters in ultrafiltrate were Cmax of 0.75 ± 0.24 mcg/mL, AUC0-48 of 7.52 ± 5.07 mcgh/mL and AUCinf of 8.83 ± 1.57 mcgh/mL at 85 mg/m2 of oxaliplatin and Cmax of 1.10 ± 0.43 mcg/mL, AUC0-48 of 9.74 ± 2.52 mcgh/mL and AUCinf of 17.3 ± 5.34 mcgh/mL at 130 mg/m2 of oxaliplatin.
8.5 Geriatric Use
No significant effect of age on the clearance of ultrafilterable platinum has been observed.
In the adjuvant therapy colon cancer randomized clinical trial, [see Clinical Studies (14)] 723 patients treated with oxaliplatin and infusional 5-fluorouracil/leucovorin were < 65 years and 400 patients were ≥ 65 years.
A descriptive subgroup analysis demonstrated that the improvement in DFS for the oxaliplatin combination arm compared to the infusional 5-fluorouracil/leucovorin alone arm appeared to be maintained across genders. The effect of oxaliplatin in patients ≥ 65 years of age was not conclusive. Insufficient subgroup sizes prevented analysis by race.
Patients ≥ 65 years of age receiving the oxaliplatin combination therapy experienced more Grade 3 to 4 granulocytopenia than patients < 65 years of age (45% versus 39%).
In the previously untreated for advanced colorectal cancer randomized clinical trial [see Clinical Studies (14)] of oxaliplatin, 160 patients treated with oxaliplatin and 5-fluorouracil/leucovorin were < 65 years and 99 patients were ≥ 65 years. The same efficacy improvements in response rate, time to tumor progression, and overall survival were observed in the ≥ 65 year old patients as in the overall study population. In the previously treated for advanced colorectal cancer randomized clinical trial [see Clinical Studies (14)] of oxaliplatin, 95 patients treated with oxaliplatin and 5-fluorouracil/leucovorin were < 65 years and 55 patients were ≥ 65 years. The rates of overall adverse reactions, including Grade 3 and 4 events, were similar across and within arms in the different age groups in all studies. The incidence of diarrhea, dehydration, hypokalemia, leukopenia, fatigue and syncope were higher in patients ≥ 65 years old. No adjustment to starting dose was required in patients ≥ 65 years old.
8.6 Patients With Renal Impairment
The exposure (AUC) of unbound platinum in plasma ultrafiltrate tends to increase in renally impaired patients [see Pharmacokinetics (12.3). Caution and close monitoring should be exercised when oxaliplatin is administered to patients with renal impairment. The starting oxaliplatin dose does not need to be reduced in patients with mild (creatinine clearance = 50 to 80 mL/min) or moderate (creatinine clearance = 30 to 49 mL/min) renal impairment. However, the starting dose of oxaliplatin should be reduced in patients with severe renal impairment (creatinine clearance < 30 mL/min) [see Dosage and Administration (2.2)].
-
10 OVERDOSAGE
There is no known antidote for oxaliplatin overdose. In addition to thrombocytopenia, the anticipated complications of an oxaliplatin overdose include hypersensitivity reaction, myelosuppression, nausea, vomiting, diarrhea and neurotoxicity.
Several cases of overdoses have been reported with oxaliplatin. Adverse reactions observed were Grade 4 thrombocytopenia (< 25,000/mm3) without any bleeding, anemia, sensory neuropathy such as paresthesia, dysesthesia, laryngospasm and facial muscle spasms, gastrointestinal disorders such as nausea, vomiting, stomatitis, flatulence, abdomen enlarged and Grade 4 intestinal obstruction, Grade 4 dehydration, dyspnea, wheezing, chest pain, respiratory failure, severe bradycardia and death.
Patients suspected of receiving an overdose should be monitored, and supportive treatment should be administered. The maximum dose of oxaliplatin that has been administered in a single infusion is 825 mg.
-
11 DESCRIPTION
Oxaliplatin Injection, USP is an antineoplastic agent with the chemical name of cis-[(1R,2R)-1,2-cyclohexanediamine-N,N'] [oxalato(2-)-O,O'] platinum. Oxaliplatin is an organoplatinum complex in which the platinum atom is complexed with 1,2-diaminocyclohexane(DACH) and with an oxalate ligand as a leaving group.
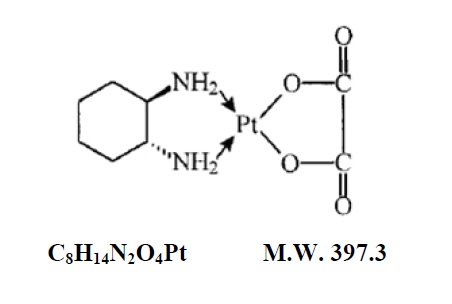
Oxaliplatin is slightly soluble in water at 6 mg/mL, very slightly soluble in methanol, and practically insoluble in ethanol and acetone.
Oxaliplatin Injection, USP is supplied in vials containing 50 mg or 100 mg of oxaliplatin as a sterile, preservative-free, aqueous solution at a concentration of 5 mg/mL. Lactose monohydrate are present as inactive ingredient at 450 mg and 900 mg in the 50 mg and 100 mg dosage strengths, respectively. Water for Injection, USP is also present as an inactive ingredient.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Oxaliplatin undergoes nonenzymatic conversion in physiologic solutions to active derivatives via displacement of the labile oxalate ligand. Several transient reactive species are formed, including monoaquo and diaquo DACH platinum, which covalently bind with macromolecules. Both inter-and intrastrand Pt-DNA crosslinks are formed. Crosslinks are formed between the N7 positions of two adjacent guanines (GG), adjacent adenine-guanines (AG), and guanines separated by an intervening nucleotide (GNG). These crosslinks inhibit DNA replication and transcription. Cytotoxicity is cell-cycle nonspecific.
In vivo studies have shown antitumor activity of oxaliplatin against colon carcinoma. In combination with 5-fluorouracil, oxaliplatin exhibits in vitro and in vivo antiproliferative activity greater than either compound alone in several tumor models [HT29 (colon), GR (mammary), and L1210 (leukemia)].
12.3 Pharmacokinetics
The reactive oxaliplatin derivatives are present as a fraction of the unbound platinum in plasma ultrafiltrate. The decline of ultrafilterable platinum levels following oxaliplatin administration is triphasic, characterized by two relatively short distribution phases (t 1/2α; 0.43 hours and t1/2β; 16.8 hours) and a long terminal elimination phase (t1/2γ; 391 hours). Pharmacokinetic parameters obtained after a single 2-hour intravenous infusion of oxaliplatin at a dose of 85 mg/m2 expressed as ultrafilterable platinum were Cmax of 0.814 mcg/mL and volume of distribution of 440 L.
Interpatient and intrapatient variability in ultrafilterable platinum exposure (AUC 0-48hr) assessed over 3 cycles was moderate to low (23% and 6%, respectively). A pharmacodynamic relationship between platinum ultrafiltrate levels and clinical safety and effectiveness has not been established.
Distribution
At the end of a 2-hour infusion of oxaliplatin, approximately 15% of the administered platinum is present in the systemic circulation. The remaining 85% is rapidly distributed into tissues or eliminated in the urine. In patients, plasma protein binding of platinum is irreversible and is greater than 90%. The main binding proteins are albumin and gamma-globulins. Platinum also binds irreversibly and accumulates (approximately 2-fold) in erythrocytes, where it appears to have no relevant activity. No platinum accumulation was observed in plasma ultrafiltrate following 85 mg/m2 every two weeks.
Metabolism
Oxaliplatin undergoes rapid and extensive nonenzymatic biotransformation. There is no evidence of cytochrome P450-mediated metabolism in vitro.
Up to 17 platinum-containing derivatives have been observed in plasma ultrafiltrate samples from patients, including several cytotoxic species (monochloro DACH platinum, dichloro DACH platinum, and monoaquo and diaquo DACH platinum) and a number of noncytotoxic, conjugated species.
Elimination
The major route of platinum elimination is renal excretion. At five days after a single 2-hour infusion of oxaliplatin, urinary elimination accounted for about 54% of the platinum eliminated, with fecal excretion accounting for only about 2%. Platinum was cleared from plasma at a rate (10 to 17 L/h) that was similar to or exceeded the average human glomerular filtration rate (GFR; 7.5 L/h). There was no significant effect of gender on the clearance of ultrafilterable platinum. The renal clearance of ultrafilterable platinum is significantly correlated with GFR.
Pharmacokinetics in Special Populations
Pediatric
[See Use in Specific Patient Populations (8.4) ]
Renal Impairment
A study was conducted in 38 patients with advanced GI cancer and varying degrees of renal impairment. Patients in the normal (creatinine clearance (CrCL) > 80 mL/min, N = 11), mild (CrCL = 50 to 80 mL/min, N = 13), and moderate (CrCL = 30 to 49 mL/min, N = 10) groups were treated with 85 mg/m2 oxaliplatin and those in the severe (CrCL < 30 mL/min, N = 4) group were treated with 65 mg/m2 oxaliplatin. The mean AUC of unbound platinum was 40%, 95%, and 342% higher in the mild, moderate, and severe groups, respectively, than in the normal group. Mean Cmax of unbound platinum appeared to be similar among the normal, mild and moderate renal function groups, but was 38% higher in the severe group than in the normal group. Caution should be exercised in renally impaired patients [see Use in Specific Patient Populations (8.6) ] The starting dose of oxaliplatin should be reduced in patients with severe renal impairment [see Dosage and Administration (2.2)]
Drug-Drug Interactions
No pharmacokinetic interaction between 85 mg/m2 of oxaliplatin and infusional 5-fluorouracil has been observed in patients treated every 2 weeks, but increases of 5-fluorouracil plasma concentrations by approximately 20% have been observed with doses of 130 mg/m2 of oxaliplatin administered every 3 weeks. In vitro, platinum was not displaced from plasma proteins by the following medications: erythromycin, salicylate, sodium valproate, granisetron, and paclitaxel. In vitro, oxaliplatin is not metabolized by, nor does it inhibit, human cytochrome P450 isoenzymes. No P450-mediated drug-drug interactions are therefore anticipated in patients. Since platinum-containing species are eliminated primarily through the kidney, clearance of these products may be decreased by co-administration of potentially nephrotoxic compounds, although this has not been specifically studied.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of oxaliplatin. Oxaliplatin was not mutagenic to bacteria (Ames test) but was mutagenic to mammalian cells in vitro (L5178Y mouse lymphoma assay). Oxaliplatin was clastogenic both in vitro (chromosome aberration in human lymphocytes) and in vivo (mouse bone marrow micronucleus assay).
In a fertility study, male rats were given oxaliplatin at 0, 0.5, 1, or 2 mg/kg/day for five days every 21 days for a total of three cycles prior to mating with females that received two cycles of oxaliplatin on the same schedule. A dose of 2 mg/kg/day (less than one-seventh the recommended human dose on a body surface area basis) did not affect pregnancy rate, but caused developmental mortality (increased early resorptions, decreased live fetuses, decreased live births) and delayed growth (decreased fetal weight).
Testicular damage, characterized by degeneration, hypoplasia, and atrophy, was observed in dogs administered oxaliplatin at 0.75 mg/kg/day x 5 days every 28 days for three cycles. A no effect level was not identified. This daily dose is approximately one-sixth of the recommended human dose on a body surface area basis.
-
14 CLINICAL STUDIES
14.1 Combination Adjuvant Therapy With Oxaliplatin and Infusional 5-Fluorouracil/Leucovorin in Patients With Colon Cancer
An international, multicenter, randomized study compared the efficacy and evaluated the safety of oxaliplatin in combination with an infusional schedule of 5-fluorouracil/leucovorin to infusional 5-fluorouracil/leucovorin alone, in patients with Stage II (Dukes' B2) or III (Dukes' C) colon cancer who had undergone complete resection of the primary tumor. The primary objective of the study was to compare the 3 year disease-free survival (DFS) in patients receiving oxaliplatin and infusional 5-fluorouracil/leucovorin to those receiving 5-fluorouracil/leucovorin alone. Patients were to be treated for a total of 6 months (i.e., 12 cycles). A total of 2246 patients were randomized; 1123 patients per study arm. Patients in the study had to be between 18 and 75 years of age, have histologically proven Stage II (T3 to T4 N0 M0; Dukes' B2) or III (any T N1 to 2 M0; Dukes' C) colon carcinoma (with the inferior pole of the tumor above the peritoneal reflection, i.e., ≥ 15 cm from the anal margin) and undergone (within 7 weeks prior to randomization) complete resection of the primary tumor without gross or microscopic evidence of residual disease. Patients had to have had no prior chemotherapy, immunotherapy or radiotherapy, and have an ECOG performance status of 0, 1, or 2 (KPS ≥ 60%), absolute neutrophil count (ANC) > 1.5 x 109/L, platelets ≥ 100 x 109/L, serum creatinine ≤ 1.25 x ULN total bilirubin < 2 x ULN, AST/ALT < 2 x ULN and carcino-embyrogenic antigen (CEA) < 10 ng/mL. Patients with preexisting peripheral neuropathy (NCI Grade ≥ 1) were ineligible for this trial.
The following table shows the dosing regimens for the two arms of the study.
Table 15 -Dosing Regimens in Adjuvant Therapy Study Treatment Arm
Dose
Regimen
Oxaliplatin + 5-FU/LV
(FOLFOX4) (N = 1123)
Day 1: Oxaliplatin: 85 mg/m2 (2-hour infusion) + LV: 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
Day 2: LV: 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
every 2 weeks
12 cycles
5-FU/LV (N = 1123)
Day 1: LV: 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
Day 2: LV: 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
every 2 weeks
12 cycles
The following tables show the baseline characteristics and dosing of the patient population entered into this study. The baseline characteristics were well balanced between arms.
Table 16 -Patient Characteristics in Adjuvant Therapy Study Oxaliplatin + Infusional 5-FU/LV
N = 1123
Infusional 5-FU/LV
N = 1123
Sex: Male (%)
56.1
52.4
Female (%)
43.9
47.6
Median age (years)
61
60
< 65 Years of age (%)
64.4
66.2
≥ 65 Years of age (%)
35.6
33.8
Karnofsky Performance Status (KPS) (%)
100
29.7
30.5
90
52.2
53.9
80
4.4
3.3
70
13.2
11.9
≤ 60
0.6
0.4
Primary Site (%)
Colon including cecum
54.6
54.4
Sigmoid
31.9
33.8
Recto sigmoid
12.9
10.9
Other including rectum
0.6
0.9
Bowel Obstructions (%)
Yes
17.9
19.3
Perforations (%)
Yes
6.9
6.9
Stage at Randomization (%)
II (T = 3,4 N = 0, M = 0)
40.1
39.9
III (T = any, N = 1,2, M = 0)
59.6
59.3
IV (T = any, N = any, M =1)
0.4
0.8
Staging – T (%)
T1
0.5
0.7
T2
4.5
4.8
T3
76
75.9
T4
19
18.5
Staging – N (%)
N0
40.2
39.9
N1
39.4
39.4
N2
20.4
20.7
Staging – M (%)
M1
0.4
0.8
Table 17 -Dosing in Adjuvant Therapy Study
Oxaliplatin + Infusional 5-FU/LV
N = 1108
Infusional 5-FU/LV
N = 1111
Median Relative Dose Intensity (%)
5-FU
84.4
97.7
Oxaliplatin
80.5
N/A
Median Number of Cycles
12
12
Median Number of cycles with Oxaliplatin
11
N/A
The following table and figures summarize the disease-free survival (DFS) results in the overall randomized population and in patients with Stage II and III disease based on an ITT analysis. The median duration of follow-up was approximately 77 months.
Table 18 – Summary of DFS Analysis – ITT Analysis Data cut off for disease free survival 1 June 2006
* Disease-free survival at 5 years
** A hazard ratio of less than 1 favors oxaliplatin + infusional 5–fluorouracil/leucovorin
Parameter
Oxaliplatin + Infusional 5-FU/LV
Infusional 5-FU/LV
Overall
N
1123
1123
Number of events – relapse or death (%)
304
(27.1)
360
(32.1)
Disease-free survival % [95% CI]*
73.3
[70.7, 76]
67.4
[64.6, 70.2]
Hazard ratio [95% CI]**
0.80 [0.68, 0.93]
Stratified logrank test
p = 0.003
Stage III (Dukes' C)
N
672
675
Number of events – relapse or death (%)
226
(33.6)
271
(40.1)
Disease-free survival % [95% CI]*
66.4
[62.7, 70]
58.9
[55.2, 62.7]
Hazard ratio [95% CI]**
0.78
[0.65, 0.93]
Logrank test
p = 0.005
Stage II (Dukes' B2)
N
451
448
Number of events – relapse or death (%)
78 (17.3)
89 (19.9)
Disease-free survival % [95% CI]*
83.7
[80.2, 87.1]
79.9
[76.2, 83.7]
Hazard ratio [95% CI]**
0.84
[0.62, 1.14]
Logrank test
p = 0.258
In the overall and Stage III colon cancer populations DFS was statistically significantly improved in the oxaliplatin combination arm compared to infusional 5-fluorouracil/leucovorin alone. However, a statistically significant improvement in DFS was not noted in Stage II patients.
Figure 2 shows the DFS Kaplan-Meier curves for the comparison of oxaliplatin and infusional 5-fluorouracil/leucovorin combination and infusional 5-fluorouracil/leucovorin alone for the overall population (ITT analysis).
Figure 3 shows the DFS Kaplan-Meier curves for the comparison of oxaliplatin and infusional 5-fluorouracil/leucovorin combination and infusional 5-fluorouracil/leucovorin alone in stage III patients.
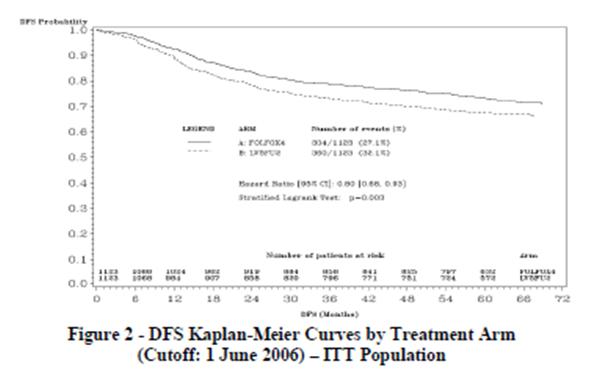
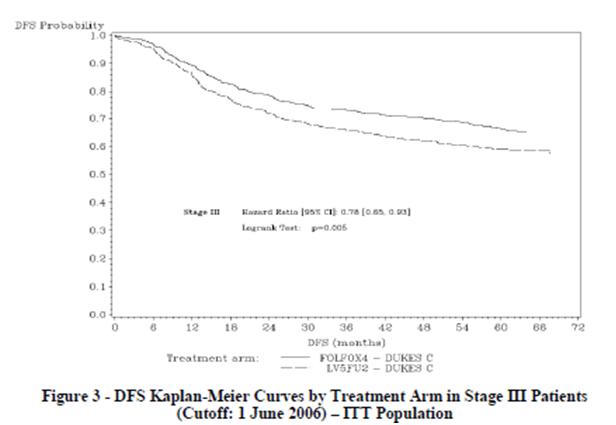
The following table summarizes the overall survival (OS) results in the overall randomized population and in patients with stage II and III disease, based on the ITT analysis.
Table 19 -Summary of OS Analysis -ITT Analysis Data cut off for overall survival 16 January 2007
* A hazard ratio of less than 1 favors oxaliplatin + infusional 5-fluorouracil/leucovorin
Parameter
Oxaliplatin + Infusional
5-FU/LV
Infusional 5-FU/LV
Overall
N
1123
1123
Number of death events (%)
245 (21.8)
283 (25.2)
Hazard ratio* [95% CI]
0.84 [0.71, 1]
Stage III (Dukes' C)
N
672
675
Number of death events (%)
182 (27.1)
220 (32.6)
Hazard ratio* [95% CI]
0.80 [0.65, 0.97]
Stage II (Dukes' B2)
N
451
448
Number of death events (%)
63 (14)
63 (14.1)
Hazard ratio* [95% CI]
1 [0.70, 1.41]
14.2 Combination Therapy With Oxaliplatin and 5-Fluorouracil/Leucovorin in Patients Previously Untreated for Advanced Colorectal Cancer
A North American, multicenter, open-label, randomized controlled study was sponsored by the National Cancer Institute (NCI) as an intergroup study led by the North Central Cancer Treatment Group (NCCTG). The study had 7 arms at different times during its conduct, four of which were closed due to either changes in the standard of care, toxicity, or simplification. During the study, the control arm was changed to irinotecan plus 5-fluorouracil/leucovorin. The results reported below compared the efficacy and safety of two experimental regimens, oxaliplatin in combination with infusional 5-fluorouracil/leucovorin and a combination of oxaliplatin plus irinotecan, to an approved control regimen of irinotecan plus 5-fluorouracil/leucovorin in 795 concurrently randomized patients previously untreated for locally advanced or metastatic colorectal cancer. After completion of enrollment, the dose of irinotecan plus 5-fluorouracil/leucovorin was decreased due to toxicity. Patients had to be at least 18 years of age, have known locally advanced, locally recurrent, or metastatic colorectal adenocarcinoma not curable by surgery or amenable to radiation therapy with curative intent, histologically proven colorectal adenocarcinoma, measurable or evaluable disease, with an ECOG performance status 0, 1, or 2. Patients had to have granulocyte count ≥ 1.5 x 109/L, platelets ≥ 100 x 109/L, hemoglobin ≥ 9 gm/dL, creatinine ≤ 1.5 x ULN, total bilirubin ≤ 1.5 mg/dL, AST ≤ 5 x ULN, and alkaline phosphatase ≤ 5 x ULN. Patients may have received adjuvant therapy for resected Stage II or III disease without recurrence within 12 months. The patients were stratified for ECOG performance status (0, 1 vs. 2), prior adjuvant chemotherapy (yes vs. no), prior immunotherapy (yes vs. no), and age (< 65 vs. ≥ 65 years). Although no post study treatment was specified in the protocol, 65% to 72% of patients received additional post study chemotherapy after study treatment discontinuation on all arms. Fifty-eight percent of patients on the oxaliplatin plus 5-fluorouracil/leucovorin arm received an irinotecan-containing regimen and 23% of patients on the irinotecan plus 5-fluorouracil/leucovorin arm received oxaliplatin-containing regimens. Oxaliplatin was not commercially available during the trial.
The following table presents the dosing regimens of the three arms of the study.
Table 20 -Dosing Regimens in Patients Previously Untreated for Advanced Colorectal Cancer Clinical Trial Treatment Arm
Dose
Regimen
Oxaliplatin + 5-FU/LV (FOLFOX4) (N = 267)
Day 1: Oxaliplatin: 85 mg/m2 (2-hour infusion) + LV 200 mg/m2 (2-hour infusion),
Followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
Day 2: LV 200 mg/m2 (2 hour infusion), followed by 5-FU: 400 mg/m2 (bolus),
600 mg/m2 (22-hour infusion)
every 2 weeks
Irinotecan + 5-FU/LV (IFL) (N = 264)
Day 1: Irinotecan 125 mg/m2 as a 90 min infusion + LV 20 mg/m2 as a 15 minute
Infusion or intravenous push, followed by 5-FU 500 mg/m2
intravenous bolus weekly x 4
every 6 weeks
Oxaliplatin + Irinotecan (IROX) (N = 264)
Day 1: Oxaliplatin: 85 mg/m2 intravenous (2 hourinfusion) + irinotecan 200 mg/m2
intravenous over 30 minutesevery 3 weeks
The following table presents the demographics of the patient population entered into this study.
Table 21 -Patient Demographics in Patients Previously Untreated for Advanced Colorectal Cancer Clinical Trial
Oxaliplatin + 5-FU/LV
N = 267
Irinotecan + 5-FU/LV
N = 264
Oxaliplatin + Irinotecan N = 264
Sex: Male (%)
58.8
65.2
61
Female (%)
41.2
34.8
39
Median age (years)
61
61
61
< 65 Years of age (%)
61
62
63
≥ 65 Years of age (%)
39
38
37
ECOG (%)
0 to 1
94.4
95.5
94.7
2
5.6
4.5
5.3
Involved organs (%)
Colon only
0.7
0.8
0.4
Liver only
39.3
44.3
39
Liver + other
41.2
38.6
40.9
Lung only
6.4
3.8
5.3
Other (including lymph nodes)
11.6
11
12.9
Not reported
0.7
1.5
1.5
Prior radiation (%)
3
1.5
3
Prior surgery (%)
74.5
79.2
81.8
Prior adjuvant (%)
15.7
14.8
15.2
The length of a treatment cycle was 2 weeks for the oxaliplatin and 5-fluorouracil/leucovorin regimen; 6 weeks for the irinotecan plus 5-fluorouracil/leucovorin regimen; and 3 weeks for the oxaliplatin plus irinotecan regimen. The median number of cycles administered per patient was 10 (23.9 weeks) for the oxaliplatin and 5-fluorouracil/leucovorin regimen, 4 (23.6 weeks) for the irinotecan plus 5-fluorouracil/leucovorin regimen, and 7 (21 weeks) for the oxaliplatin plus irinotecan regimen. Patients treated with the oxaliplatin and 5-fluorouracil/leucovorin combination had a significantly longer time to tumor progression based on investigator assessment, longer overall survival, and a significantly higher confirmed response rate based on investigator assessment compared to patients given irinotecan plus 5-fluorouracil/leucovorin. The following table summarizes the efficacy results.
Table 22 -Summary of Efficacy * Compared to irinotecan plus 5-fluorouracil/leucovorin (IFL) arm
** Based on all patients with measurable disease at baseline
The numbers in the response rate and TTP analysis are based on unblinded investigator assessment.
*** A hazard ratio of less than 1 favors oxaliplatin + infusional 5-fluorouracil/leucovorin
Oxaliplatin + 5-FU/LV
N = 267
Irinotecan + 5-FU/LV
N = 264
Oxaliplatin + Irinotecan
N = 264
Survival (ITT)
Number of deaths N (%)
155 (58.1)
192 (72.7)
175 (66.3)
Median survival (months)
19.4
14.6
17.6
Hazard Ratio and (95% confidence interval)
0.65 (0.53 to 0.80)*
P-value
< 0.0001*
-
-
TTP (ITT, investigator assessment)
Percentage of progressors
82.8
81.8
89.4
Median TTP (months)
8.7
6.9
6.5
Hazard Ratio and (95% confidence interval)***
0.74 (0.61 to 0.89)*
P-value
0.0014*
-
-
Response Rate (investigator assessment)**
Patients with measurable disease
210
212
215
Complete response N (%)
13 (6.2)
5 (2.4)
7 (3.3)
Partial response N (%)
82 (39)
64 (30.2)
67 (31.2)
Complete and partial response N (%)
95 (45.2)
69 (32.5)
74 (34.4)
95% Confidence interval
(38.5 to 52)
(26.2 to 38.9)
(28.1 to 40.8)
P-value
0.0080*
-
-
Figure 4 illustrates the Kaplan-Meier survival curves for the comparison of oxaliplatin and 5-fluorouracil/leucovorin combination and oxaliplatin plus irinotecan to irinotecan plus 5-fluorouracil/leucovorin.
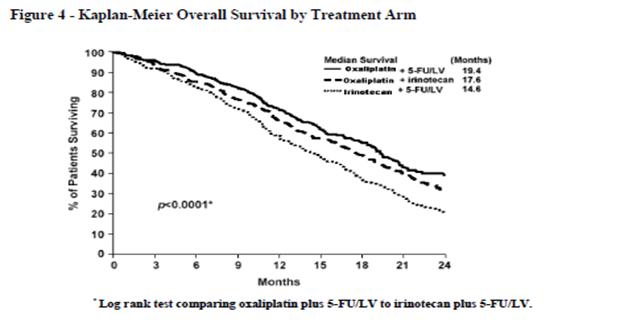
A descriptive subgroup analysis demonstrated that the improvement in survival for oxaliplatin plus 5-fluorouracil/leucovorin compared to irinotecan plus 5-fluorouracil/leucovorin appeared to be maintained across age groups, prior adjuvant therapy, and number of organs involved. An estimated survival advantage in oxaliplatin plus 5-fluorouracil/leucovorin versus irinotecan plus 5-fluorouracil/leucovorin was seen in both genders; however it was greater among women than men. Insufficient subgroup sizes prevented analysis by race.
14.3 Combination Therapy With Oxaliplatin and 5-Fluorouracil/Leucovorin in Previously Treated Patients With Advanced Colorectal Cancer
A multicenter, open-label, randomized, three-arm controlled study was conducted in the U.S. and Canada comparing the efficacy and safety of oxaliplatin in combination with an infusional schedule of 5-fluorouracil/leucovorin to the same dose and schedule of 5-fluorouracil/leucovorin alone and to single agent oxaliplatin in patients with advanced colorectal cancer who had relapsed/progressed during or within 6 months of first-line therapy with bolus 5fluorouracil/leucovorin and irinotecan. The study was intended to be analyzed for response rate after 450 patients were enrolled. Survival will be subsequently assessed in all patients enrolled in the completed study. Accrual to this study is complete, with 821 patients enrolled. Patients in the study had to be at least 18 years of age, have unresectable, measurable, histologically proven colorectal adenocarcinoma, with a Karnofsky performance status > 50%. Patients had to have SGOT(AST) and SGPT(ALT) ≤ 2x the institution's upper limit of normal (ULN), unless liver metastases were present and documented at baseline by CT or MRI scan, in which case ≤ 5x ULN was permitted. Patients had to have alkaline phosphatase ≤ 2x the institution's ULN, unless liver metastases were present and documented at baseline by CT or MRI scan, in which cases ≤ 5x ULN was permitted. Prior radiotherapy was permitted if it had been completed at least 3 weeks before randomization.
The dosing regimens of the three arms of the study are presented in the table below.
Table 23 -Dosing Regimens in Refractory and Relapsed Colorectal Cancer Clinical Trial Treatment Arm
Dose
Regimen
Oxaliplatin + 5-FU/LV
(N = 152)
Day 1: Oxaliplatin: 85 mg/m2 (2hour infusion) + LV 200 mg/m2 (2- hour infusion), followed by 5FU: 400 mg/m2 (bolus), 600 mg/m2
(22-hour infusion)
Day 2: LV 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
every 2 weeks
5-FU/LV
(N = 151)
Day 1: LV 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
Day 2: LV 200 mg/m2 (2-hour infusion), followed by 5-FU: 400 mg/m2 (bolus), 600 mg/m2 (22-hour infusion)
every 2 weeks
Oxaliplatin
(N = 156)
Day 1: Oxaliplatin 85 mg/m2 (2-hour infusion)
every 2 weeks
Patients entered into the study for evaluation of response must have had at least one unidimensional lesion measuring ≥ 20mm using conventional CT or MRI scans, or ≥ 10mm using a spiral CT scan. Tumor response and progression were assessed every 3 cycles (6 weeks) using the Response Evaluation Criteria in Solid Tumors (RECIST) until radiological documentation of progression or for 13 months following the first dose of study drug(s), whichever came first. Confirmed responses were based on two tumor assessments separated by at least 4 weeks.
The demographics of the patient population entered into this study are shown in the table below.
Table 24 -Patient Demographics in Refractory and Relapsed Colorectal Cancer Clinical Trial 5-FU/LV
(N = 151)
Oxaliplatin
(N = 156)
Oxaliplatin + 5-FU/LV (N = 152)
Sex: Male (%)
54.3
60.9
57.2
Female (%)
45.7
39.1
42.8
Median age (years)
60
61
59
Range
21 to 80
27 to 79
22 to 88
Race (%)
Caucasian
87.4
84.6
88.8
Black
7.9
7.1
5.9
Asian
1.3
2.6
2.6
Other
3.3
5.8
2.6
KPS (%)
70 to 100
94.7
92.3
95.4
50 to 60
2.6
4.5
2
Not reported
2.6
3.2
2.6
Prior radiotherapy (%)
25.2
19.2
25
Prior pelvic radiation (%)
18.5
13.5
21.1
Number of metastatic sites (%)
1
27.2
31.4
25.7
≥ 2
72.2
67.9
74.3
Liver Involvement (%)
Liver only
22.5
25.6
18.4
Liver + other
60.3
59
53.3
The median number of cycles administered per patient was 6 for the oxaliplatin and 5-fluorouracil/leucovorin combination and 3 each for 5-fluorouracil/leucovorin alone and oxaliplatin alone.
Patients treated with the combination of oxaliplatin and 5-fluorouracil/leucovorin had an increased response rate compared to patients given 5-fluorouracil/leucovorin or oxaliplatin alone. The efficacy results are summarized in the tables below.
Table 25 -Response Rates (ITT Analysis) Best Response
5-FU/LV
(N = 151)
Oxaliplatin
(N = 156)
Oxaliplatin + 5-FU/LV (N = 152)
CR
0
0
0
PR
0
2 (1%)
13 (9%)
p-value
0.0002 for 5-FU/LV vs. Oxaliplatin + 5-FU/LV
95% CI
0 to 2.4%
0.2 to 4.6%
4.6 to 14.2%
Table 26 -Summary of Radiographic Time to Progression* * This is not an ITT analysis. Events were limited to radiographic disease progression documented by independent review of radiographs. Clinical progression was not included in this analysis, and 18% of patients were excluded from the analysis based on unavailability of the radiographs for independent review.
Arm
5-FU/LV
(N = 151)
Oxaliplatin
(N = 156)
Oxaliplatin + 5-FU/LV (N = 152)
No. of Progressors
74
101
50
No. of patients with no radiological evaluation beyond baseline
22
(15%)
16
(10%)
17
(11%)
Median TTP (months)
2.7
1.6
4.6
95% CI
1.8 to 3
1.4 to 2.7
4.2 to 6.1
At the time of the interim analysis 49% of the radiographic progression events had occurred. In this interim analysis an estimated 2-month increase in median time to radiographic progression was observed compared to 5-fluorouracil/leucovorin alone.
Of the 13 patients who had tumor response to the combination of oxaliplatin and 5-fluorouracil/leucovorin, 5 were female and 8 were male, and responders included patients < 65 years old and ≥ 65 years old. The small number of non-Caucasian participants made efficacy analyses in these populations uninterpretable.
-
15 REFERENCES
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. (2006) ASHP Guidelines on Handling Hazardous Drugs.
- Polovich, M., White, J. M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd. ed.) Pittsburgh, PA: Oncology Nursing Society.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Oxaliplatin Injection, USP is supplied in clear, glass, single-use vials with gray elastomeric stoppers and aluminum flip-off seals containing 50 mg or 100 mg of oxaliplatin as a sterile, preservative-free, aqueous solution at a concentration of 5 mg/mL. Water for injection and lactose monohydrate are present as inactive ingredients.
NDC 50742-405-10
50 mg single-use vial with flip-off seal individually packaged in a carton.
NDC 50742-406-20
100 mg single-use vial with flip-off seal individually packaged in a carton.
16.2 Storage
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
DO NOT FREEZE.
PROTECT FROM LIGHT.
Keep in original outer carton.
16.3 Handling and Disposal
As with other potentially toxic anticancer agents, care should be exercised in the handling and preparation of infusion solutions prepared from oxaliplatin. The use of gloves is recommended. If a solution of oxaliplatin contacts the skin, wash the skin immediately and thoroughly with soap and water. If oxaliplatin contacts the mucous membranes, flush thoroughly with water.
Procedures for the handling and disposal of anticancer drugs should be considered. Several guidelines on the subject have been published [see References (15))]. There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
-
17 PATIENT COUNSELING INFORMATION
- To expect side effects of oxaliplatin, particularly its neurologic effects, both the acute, reversible effects and the persistent neurosensory toxicity. Patients should be informed that the acute neurosensory toxicity may be precipitated or exacerbated by exposure to cold or cold objects.
- To avoid cold drinks, use of ice, and should cover exposed skin prior to exposure to cold temperature or cold objects.
- Of the risk of low blood cell counts and to contact their physician immediately should fever, particularly if associated with persistent diarrhea, or evidence of infection develop.
- To contact their physician if persistent vomiting, diarrhea, signs of dehydration, cough or breathing difficulties occur, or signs of allergic reaction appear.
- To exercise caution when driving and using machines. No studies on the effects of the ability to operate cars and machines have been performed; however, oxaliplatin treatment resulting in an increase risk of dizziness, nausea and vomiting, and other neurologic symptoms that affect gait and balance may lead to a minor or moderate influence on the ability to drive and use machines.
- Of the potential effects of vision abnormalities, in particular transient vision loss (reversible following therapy discontinuation), which may affect patients' ability to drive and use machines.
Ingenus Pharmaceuticals, LLC
Orlando, FL 32839-6408
Made in Switzerland
Revised: 03/2019
Patient Information
OXALIPLATIN (ox al″ i pla′ tin)
Injection
for intravenous use
Read this Patient Information leaflet carefully before you start receiving oxaliplatin. There may be new information. It will help you learn more about oxaliplatin. This leaflet does not take the place of talking to your doctor about your medical condition or your treatment. Ask your doctor about any questions you have.
What is the most important information I should know about oxaliplatin?
Oxaliplatin can cause serious allergic reactions, including allergic reactions that may cause death. Oxaliplatin is a platinum base medicine. Serious allergic reactions including death can happen in people who take oxaliplatin and who have had previous allergic reactions to platinum medicines. Serious allergic reactions can happen within a few minutes of your infusion or any time during your treatment with oxaliplatin.
Get emergency help right away if you:
Have trouble breathing.
Feel like your throat is closing up.
Call your doctor right away if you have any of the following signs or symptoms of an allergic reaction:
Rash sudden Cough
flushed face dizziness or feel faint
hives sweating
itching chest pain
swelling of your lips or tongue
See "What are the possible side effects of oxaliplatin?" for information about other serious side effects.
What is oxaliplatin?
Oxaliplatin is an anti-cancer (chemotherapy) medicine that is used with other anti-cancer medicines called 5-fluorouracil and leucovorin to treat people with:
Stage III colon cancer after surgery to remove the tumor
advanced colon or rectal cancer (colo-rectal cancer).
It is not known if oxaliplatin is effective in children.
Who should not receive oxaliplatin?
Do not receive oxaliplatin if you are allergic to any of the ingredients in oxaliplatin injection or other medicines that contain platinum. See the end of this leaflet for a complete list of the ingredients in oxaliplatin injection. Ask your doctor if you are not sure if you take a medicine that contains platinum.
What should I tell my doctor before receiving oxaliplatin?
Before receiving oxaliplatin, tell your doctor about all of your medical conditions, including if you:
have an infection
have lung, liver, or kidney problems
have or had heart problems such as an abnormal heart test called an electrocardiogram (ECG or EKG), a condition called long QT syndrome, an irregular or slow heartbeat, or a family history of heart problems.
have had changes in the level of certain blood salt (electrolytes) levels, including potassium, magnesium, and calcium
are pregnant or plan to become pregnant. Oxaliplatin may harm your unborn baby. Females who are able to become pregnant should avoid becoming pregnant and should use effective birth control during treatment with oxaliplatin.
are breastfeeding or plan to breastfeed. It is not known if oxaliplatin passes into your breast milk. You and your doctor should decide if you will receive oxaliplatin or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of them and show it to your doctor and pharmacist when you get a new medicine.
How will I receive oxaliplatin?
Oxaliplatin is given to you into your vein through an intravenous (IV) tube.
Your doctor will prescribe oxaliplatin in a dose that is right for you.
Your doctor may change how often you receive oxaliplatin, your dose, or how long your infusion will take.
You and your doctor will decide how many oxaliplatin treatments you will receive.
It is very important that you do exactly what your doctor and nurse tell you to do.
Some medicines may be given to you before oxaliplatin to help prevent nausea and vomiting.
Each treatment course is given to you over 2 days. You will receive oxaliplatin on the first day only.
There are usually 14 days between each chemotherapy treatment course.
It is important for you to keep all of your medical appointments. Call your doctor if you miss an appointment. There may be special instructions for you.
Treatment Day 1:
Oxaliplatin and leucovorin will be given through a thin plastic tube into a vein (intravenous infusion or IV) and given for 2 hours. You will be watched by a healthcare provider during this time.
Right after the oxaliplatin and leucovorin are given, 2 doses of 5-fluorouracil will be given. The first dose is given right away into your IV tube. The second dose will be given into your IV tube over the next 22 hours, using a pump device.
Treatment Day 2:
You will not get oxaliplatin on Day 2. Leucovorin and 5-fluorouracil will be given the same way as on Day 1. The 5-fluorouracil will be given through your IV with a pump. If you have any problems with the pump or the tube, call your doctor, your nurse, or the person who is responsible for your pump. Do not let anyone other than a healthcare provider touch your infusion pump or tubing.
What should I avoid while receiving oxaliplatin?
Avoid cold temperatures and cold objects. Cover your skin if you must go outside in cold temperatures.
Do not drink cold drinks or use ice cubes in drinks.
Do not put ice or ice packs on your body.
Oxaliplatin can cause dizziness, vision problems, or vision loss that can affect your ability to drive or use machines. You should not drive or operate machinery if you develop these symptoms while receiving oxaliplatin.
See "How can I reduce the side effects caused by cold temperatures?" for more information.
Talk with your doctor and nurse about your level of activity during treatment with oxaliplatin. Follow their instructions.
What are the possible side effects of oxaliplatin? Oxaliplatin can cause serious side effects, including:
See " What is the most important information I should know about oxaliplatin? "
Nerve problems. Oxaliplatin can affect how your nerves work and make you feel. Nerve problems may happen with the first treatment or within two days after your treatment of oxaliplatin. Nerve problems may last a short time (acute) or may become persistent. Symptoms may improve after stopping treatment with oxaliplatin. Exposure to cold or cold objects may cause or worsen nerve problems. Tell your doctor right away if you get any signs of nerve problems, including:
o very sensitive to cold temperatures and cold objects
o trouble breathing, swallowing, or saying words, jaw tightness, odd feelings in your tongue, or chest pressure
o pain, tingling, burning (pins and needles, numb feeling) in your hands, feet, or around your mouth or throat, which may cause problems walking or performing activities of daily living.
For information on ways to lessen or help with the nerve problems, see the end of this leaflet, "How can I reduce the side effects caused by cold temperatures?"
Reversible Posterior Leukoencephalopathy (RPLS). RPLS is a rare condition that affects the brain. Tell your doctor right away if you have any of the following signs and symptoms of RPLS:
o headache
o confusion or a change in the way you think
o seizures
o vision problems, such as blurriness or vision loss
Low white blood cell counts (neutropenia). Oxaliplatin can cause low white blood cells counts. Low blood cell counts are common with oxaliplatin and can lead to serious infection and death. Tell your doctor right away if you have a fever greater than 100.9oF (38.3°C) or a prolonged fever greater than 100.4oF (38°C) for more than one hour (febrile neutropenia). Call your doctor right away if you get any of the following signs of infection:
o chills or shivering o cough that brings up mucus
o pain on swallowing o burning or pain on urination
o sore throat o redness or swelling at intravenous site
o persistent diarrhea
Lung problems (interstitial fibrosis). Oxaliplatin can cause lung problems that may lead to death. Tell your doctor right away if you get a dry cough and have trouble breathing (shortness of breath) before your next treatment. These may be signs of a serious lung disease.
Liver problems (hepatotoxicity). Your doctor will do blood tests to check your liver.
Heart problems. Oxaliplatin can cause heart problems that have led to death. Your doctor may do blood and heart tests during treatment with oxaliplatin if you have certain heart problem. If you faint (lose consciousness) or have an irregular heartbeat or chest pain during treatment with oxaliplatin, tell your doctor right away as this may be a sign of a serious heart condition.
Muscle problems. Oxaliplatin can cause muscle damage (rhabdomyolysis) which can lead to death. Tell your doctor right away if you have muscle pain and swelling, along with weakness, fever, or red brown urine.
Harm to an unborn baby. See " What should I tell my doctor before treatment with oxaliplatin? "
The most common side effects of oxaliplatin include:
Numbness, pain, tingling, and/or burning along the nerves
Low white blood cells (neutropenia)
Low platelet count (important for clotting and to control bleeding)
Low red blood cells (blood cells that carry oxygen to the tissues)
Nausea
Changes in liver function tests
Diarrhea
Vomiting
Tiredness
Mouth sores
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of oxaliplatin. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How can I reduce the side effects caused by cold temperatures?
Cover yourself with a blanket while you are getting your oxaliplatin infusion.
Do not breathe deeply when exposed to cold air.
Wear warm clothing in cold weather at all times. Cover your mouth and nose with a scarf or a pull-down cap (ski cap) to warm the air that goes to your lungs.
Wear gloves when taking things from the freezer or refrigerator.
Drink fluids warm or at room temperature.
Always drink through a straw.
Do not use ice chips if you have nausea or mouth sores. Ask your doctor about what you can use.
Be aware that most metals are cold to touch, especially in the winter. These include your car door and mailbox. Wear gloves to touch cold objects.
Do not run the air-conditioning at high levels in the house or in the car in hot weather.
If your body gets cold, warm-up the affected part. If your hands get cold, wash them with warm water.
Always let your healthcare provider or doctor know before your next treatment how well you did since your last visit. Your doctor may have other useful tips for helping you with these side effects.
General information about the safe and effective use of oxaliplatin
Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. This Patient Information leaflet summarizes the most important information about oxaliplatin. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about oxaliplatin that is written for health professionals.
What are the ingredients in oxaliplatin?
Active ingredient: oxaliplatin
Concentrate for solution for infusion inactive ingredients: lactose monohydrate, and water for injection.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Ingenus Pharmaceuticals, LLC
Orlando, FL 32839-6408
Made in Switzerland
Revised: 03/2019
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
OXALIPLATIN
oxaliplatin injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50742-405 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXALIPLATIN (UNII: 04ZR38536J) (OXALIPLATIN - UNII:04ZR38536J) OXALIPLATIN 50 mg in 10 mL Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) 450 mg in 10 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50742-405-10 1 in 1 CARTON 10/29/2018 1 10 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207562 10/29/2018 OXALIPLATIN
oxaliplatin injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 50742-406 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength OXALIPLATIN (UNII: 04ZR38536J) (OXALIPLATIN - UNII:04ZR38536J) OXALIPLATIN 100 mg in 20 mL Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) 900 mg in 20 mL WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 50742-406-20 1 in 1 CARTON 10/29/2018 1 20 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA207562 10/29/2018 Labeler - Ingenus Pharmaceuticals, LLC (833250017) Registrant - Ingenus Pharmaceuticals, LLC (833250017) Establishment Name Address ID/FEI Business Operations Ingenus Pharmaceuticals GmbH 482730327 ANALYSIS(50742-405, 50742-406) , LABEL(50742-405, 50742-406) , MANUFACTURE(50742-405, 50742-406) , PACK(50742-405, 50742-406) , STERILIZE(50742-405, 50742-406)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.