FABRAZYME- agalsidase beta injection, powder, lyophilized, for solution
Fabrazyme by
Drug Labeling and Warnings
Fabrazyme by is a Prescription medication manufactured, distributed, or labeled by Genzyme Corporation, Genzyme Ireland Limited, Resilience Boston Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use Fabrazyme safely and effectively. See full prescribing information for Fabrazyme.
FABRAZYME (agalsidase beta) for injection, for intravenous use
Initial U.S. Approval: 2003INDICATIONS AND USAGE
Fabrazyme is indicated for use in patients with Fabry disease. Fabrazyme reduces globotriaosylceramide (GL-3) deposition in capillary endothelium of the kidney and certain other cell types. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
For injection: 5 mg or 35 mg lyophilized cake or powder in a single-dose vial for reconstitution (3)
CONTRAINDICATIONS
None. (4)
WARNINGS AND PRECAUTIONS
- Life-threatening anaphylactic and severe allergic reactions have been observed in some patients during Fabrazyme infusions. If severe allergic or anaphylactic reactions occur, immediately discontinue administration of Fabrazyme and provide necessary emergency treatment. Appropriate medical support measures should be readily available when Fabrazyme is administered because of the potential for severe infusion-associated reactions. (5.1)
- Infusion-associated reactions occurred in 59% of patients during Fabrazyme administration in clinical trials. Some reactions were severe. In patients experiencing infusion-associated reactions, pretreatment with an antipyretic and antihistamine is recommended. If an infusion-associated reaction occurs, decreasing the infusion rate, temporarily stopping the infusion, and/or administrating additional antipyretics, antihistamines, and/or steroids may ameliorate the symptoms. (5.2)
- If severe infusion-associated reactions occur, immediate discontinuation of the administration of Fabrazyme should be considered and appropriate medical treatment should be initiated. Severe reactions are generally managed with administration of antihistamines, corticosteroids, intravenous fluids, and/or oxygen as clinically indicated. (5.2)
- Patients with advanced Fabry disease may have compromised cardiac function, which may predispose them to a higher risk of severe complications from infusion-associated reactions, and these patients should be monitored closely during Fabrazyme administration. (5.3)
- Readministration of Fabrazyme to patients who have previously experienced severe or serious allergic reactions to Fabrazyme should be done only after careful consideration of the risks and benefits of continued treatment, and only under the direct supervision of qualified personnel and with appropriate medical support measures readily available. (5.4)
ADVERSE REACTIONS
Most common adverse reactions (≥20% and >2.5% compared to placebo) are: upper respiratory tract infection, chills, pyrexia, headache, cough, paresthesia, fatigue, peripheral edema, dizziness, and rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genzyme at 1-800-745-4447 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2018
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
2.2 Preparation and Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylaxis and Allergic Reactions
5.2 Infusion-associated Reactions
5.3 Compromised Cardiac Function
5.4 Immunogenicity and Rechallenge
5.5 Monitoring: Laboratory Tests
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Immunogenicity
6.3 Postmarketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Responses in Women
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dosage
- The recommended dosage of Fabrazyme is 1 mg/kg body weight infused every two weeks as an intravenous infusion. The initial intravenous infusion rate is no more than 0.25 mg/min (15 mg/hour). Slow the infusion rate in the event of infusion-associated reactions [see Warnings and Precautions (5.2)].
- Administer antipyretics prior to infusion of Fabrazyme [see Warnings and Precautions (5.2)].
- After patient tolerance to the infusion is well established, increase the infusion rate in increments of 0.05 to 0.08 mg/min (increments of 3 to 5 mg/hour) with each subsequent infusion.
- The maximum infusion rate for patients weighing less than 30 kg, is 0.25 mg/minute (15 mg/hour).
- For patients weighing 30 kg or greater, the minimum infusion duration is 1.5 hours (based on individual patient tolerability).
- Patients who have had a positive skin test to Fabrazyme or who have tested positive for anti-Fabrazyme IgE may be successfully rechallenged with Fabrazyme. The initial rechallenge administration should be a low dose at a lower infusion rate, e.g., 1/2 the therapeutic dose (0.5 mg/kg) at 1/25 the initial standard recommended rate (0.01 mg/min). Once a patient tolerates the infusion, the dose may be increased to reach the approved dose of 1 mg/kg and the infusion rate may be increased by slowly titrating upwards (doubled every 30 minutes up to a maximum rate of 0.25 mg/minute), as tolerated.
2.2 Preparation and Administration Instructions
Fabrazyme does not contain any preservatives. Vials are for single use only. Discard any unused product.
Avoid shaking or agitating this product. Do not use filter needles during the preparation of the infusion.
Reconstitution and Dilution (using Aseptic Technique)
- Allow Fabrazyme vials and diluent to reach room temperature prior to reconstitution (approximately 30 minutes). The number of 35 mg and 5 mg vials needed is based on the patient's body weight (kg) and the recommended dose of 1 mg/kg.
Select a combination of 35 mg and 5 mg vials so that the total number of mg is equal to or greater than the patient's number of kg of body weight. - Reconstitute each 35 mg vial of Fabrazyme by slowly injecting 7.2 mL of Sterile Water for Injection, USP down the inside wall of each vial. Roll and tilt each vial gently. Each vial will yield a 5 mg/mL clear, colorless solution (total extractable amount per vial is 35 mg, 7 mL).
Reconstitute each 5 mg vial of Fabrazyme by slowly injecting 1.1 mL of Sterile Water for Injection, USP down the inside wall of each vial. Roll and tilt each vial gently. Each vial will yield a 5 mg/mL clear, colorless solution (total extractable amount per vial is 5 mg, 1 mL). - Visually inspect the reconstituted vials for particulate matter and discoloration. Do not use the reconstituted solution if there is particulate matter or if it is discolored.
- The reconstituted solution should be further diluted with 0.9% Sodium Chloride Injection, USP to a total volume based on patient weight specified in Table 1 below. Prior to adding the volume of reconstituted Fabrazyme required for the patient dose, remove an equal volume of 0.9% Sodium Chloride Injection, USP from the infusion bag.Patient dose (in mg) ÷ 5 mg/mL = Number of mL of reconstituted Fabrazyme required for patient dose
Table 1 Patient Weight (kg) Minimum Total Volume (mL) ≤35 50 35.1–70 100 70.1–100 250 >100 500
Example: Patient dose = 80 mg
80 mg ÷ 5 mg/mL = 16 mL of Fabrazyme
Slowly withdraw the reconstituted solution from each vial up to the total volume required for the patient dose. Inject the reconstituted Fabrazyme solution directly into the Sodium Chloride solution. Do not inject in the airspace within the infusion bag. Discard any vial with unused reconstituted solution. - Gently invert infusion bag to mix the solution, avoiding vigorous shaking and agitation.
- Do not infuse Fabrazyme in the same intravenous line with other products.
- Administer Fabrazyme using an in-line low protein binding 0.2 µm filter.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylaxis and Allergic Reactions
Life-threatening anaphylactic and severe allergic reactions have been observed in patients during Fabrazyme infusions. Reactions have included localized angioedema (including swelling of the face, mouth, and throat), bronchospasm, hypotension, generalized urticaria, dysphagia, rash, dyspnea, flushing, chest discomfort, pruritus, and nasal congestion. Interventions have included cardiopulmonary resuscitation, oxygen supplementation, intravenous fluids, hospitalization, and treatment with inhaled beta-adrenergic agonists, epinephrine, and intravenous corticosteroids.
In clinical trials and postmarketing safety experience with Fabrazyme, approximately 1% of patients developed anaphylactic or severe allergic reactions during Fabrazyme infusion.
If anaphylactic or severe allergic reactions occur, immediately discontinue the administration of Fabrazyme and initiate necessary emergency treatment. Because of the potential for severe allergic reactions, appropriate medical support measures should be readily available when Fabrazyme is administered.
The risks and benefits of readministering Fabrazyme following an anaphylactic or severe allergic reaction should be considered. Extreme care should be exercised, with appropriate medical support measures readily available, if the decision is made to readminister the product [see Warnings and Precautions (5.4) and Clinical Studies (14)].
5.2 Infusion-associated Reactions
In clinical trials with Fabrazyme, 59% of patients experienced infusion-associated reactions during Fabrazyme administration, some of which were severe [see Warnings and Precautions (5.1)]. Severe infusion-associated reactions experienced by more than one patient in clinical studies with Fabrazyme included chills, vomiting, hypotension, and paresthesia. Other infusion-associated reactions included pyrexia, feeling hot or cold, dyspnea, nausea, flushing, headache, fatigue, pruritus, pain in extremity, hypertension, chest pain, throat tightness, abdominal pain, dizziness, tachycardia, nasal congestion, diarrhea, edema peripheral, myalgia, urticaria, bradycardia, and somnolence.
Most patients in clinical trials were pretreated with acetaminophen. In patients experiencing infusion-associated reactions, pretreatment with an antipyretic and antihistamine is recommended. Infusion-associated reactions occurred in some patients after receiving pretreatment with antipyretics, antihistamines, and oral steroids. Infusion-associated reactions tended to decline in frequency with continued use of Fabrazyme. However, infusion-associated reactions may still occur despite extended duration of Fabrazyme treatment. If an infusion-associated reaction occurs, decreasing the infusion rate, temporarily stopping the infusion, and/or administrating additional antipyretics, antihistamines, and/or steroids may ameliorate the symptoms. If severe infusion-associated reactions occur, immediate discontinuation of the administration of Fabrazyme should be considered and appropriate medical treatment should be initiated. Severe reactions are generally managed with administration of antihistamines, corticosteroids, intravenous fluids, and/or oxygen, when clinically indicated. Because of the potential for severe infusion-associated reactions, appropriate medical support measures should be readily available when Fabrazyme is administered. Patients who have experienced infusion-associated reactions should be treated with caution when readministering Fabrazyme.
5.3 Compromised Cardiac Function
Patients with advanced Fabry disease may have compromised cardiac function, which may predispose them to a higher risk of severe complications from infusion-associated reactions [see Warnings and Precautions (5.1, 5.2)]. Patients with compromised cardiac function should be monitored closely if the decision is made to administer Fabrazyme.
5.4 Immunogenicity and Rechallenge
In clinical trials with Fabrazyme, a few patients developed IgE antibodies or skin test reactivity specific to Fabrazyme. Two of six patients in the rechallenge study discontinued treatment with Fabrazyme prematurely due to recurrent infusion-associated reactions. Four serious infusion-associated reactions occurred in three patients during Fabrazyme infusions, including bronchospasm, urticaria, hypotension, and development of Fabrazyme-specific antibodies. Other infusion-associated reactions occurring in more than one patient during the study included rigors, hypertension, nausea, vomiting, and pruritus. Physicians should consider testing for IgE antibodies in patients who experienced suspected allergic reactions and consider the risks and benefits of continued treatment in patients with anti-Fabrazyme IgE antibodies [see Warnings and Precautions (5.1)].
Patients who have had a positive skin test to Fabrazyme or who have tested positive for Fabrazyme-specific IgE antibody have been rechallenged with Fabrazyme using a rechallenge protocol [see Clinical Studies (14)]. Rechallenge of these patients should only occur under the direct supervision of qualified personnel, with appropriate medical support measures readily available [see Dosage and Administration (2.1)].
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in labeling:
- Anaphylaxis and Allergic Reactions [see Warnings and Precautions (5.1)]
- Infusion-associated Reactions [see Warnings and Precautions (5.2)]
- Compromised Cardiac Function [see Warnings and Precautions (5.3)]
- Immunogenicity and Rechallenge [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trial of another drug and may not reflect the rates observed in patients in clinical practice.
The data described below reflect exposure of 80 patients, ages 16 to 61 years, to 1 mg/kg Fabrazyme every two weeks in two separate double-blind, placebo-controlled clinical trials, for periods ranging from 1 to 35 months (mean 15.5 months). All 58 patients enrolled in one of the two studies continued into an open-label extension study of Fabrazyme treatment for up to 54 additional months. Patients were treated with antipyretics and antihistamines prior to the infusions.
Most Common Adverse reactions
Table 2 enumerates adverse reactions that occurred during the double-blind treatment periods of the two placebo-controlled trials (Study 1 and Study 2) [see Clinical Studies (14)]. The most common adverse reactions reported with Fabrazyme were infusion-associated reactions, (Fabrazyme 59% vs placebo 27%) some of which were severe.
Common adverse reactions which occurred in ≥20% of patients treated with Fabrazyme and >2.5% compared to placebo are: upper respiratory tract infection, chills, pyrexia, headache, cough, paresthesia, fatigue, peripheral edema, dizziness and rash.
Table 2: Summary of Common Adverse Reactions* in Clinical Trials of Patients with Fabry Disease Adverse Reaction Fabrazyme
(n=80 )
%Placebo
(n=60)
%- * Reported at rate of at least 5% in Fabrazyme-treated patients and greater than 2.5% compared to placebo-treated patients.
Upper respiratory tract infection 44 30 Chills 43 12 Pyrexia 39 22 Headache 39 28 Cough 33 25 Paresthesia 31 18 Fatigue 24 17 Peripheral edema 21 7 Dizziness 21 8 Rash 20 10 Pain in extremity 19 8 Nasal congestion 19 15 Lower respiratory tract infection 18 7 Pain 16 13 Back pain 16 10 Myalgia 14 5 Hypertension 14 5 Feeling cold 11 2 Pruritus 10 3 Tachycardia 9 3 Sinusitis 9 3 Excoriation 9 2 Increased blood creatinine 9 5 Tinnitus 8 3 Dyspnea 8 2 Respiratory tract congestion 8 2 Toothache 6 3 Pharyngitis 6 2 Fall 6 3 Burning sensation 6 0 Anxiety 6 3 Depression 6 2 Wheezing 6 0 Hypoacusis 5 0 Chest discomfort 5 2 Fungal infection 5 0 Viral infection 5 0 Muscle spasms 5 2 Hot flush 5 0 Serious and/or frequently occurring (≥5% incidence) related adverse reactions based on a pooled analysis of 150 patients treated with Fabrazyme consisted of one or more of the following: chills, pyrexia, feeling hot or cold, dyspnea, nausea, flushing, headache, vomiting, paresthesia, fatigue, pruritus, pain in extremity, hypertension, chest pain, throat tightness, abdominal pain, dizziness, tachycardia, nasal congestion, diarrhea, edema peripheral, myalgia, back pain, pallor, bradycardia, urticaria, hypotension, face edema, rash, and somnolence. The occurrence of somnolence can be attributed to clinical trial specified pretreatment with antihistamines. Most infusion-related reactions requiring intervention were ameliorated with slowing of the infusion rate, temporarily stopping the infusion, and/or administration of antipyretics, antihistamines, or steroids.
Other reported serious adverse events included stroke, pain, ataxia, bradycardia, cardiac arrhythmia, cardiac arrest, decreased cardiac output, vertigo, and nephrotic syndrome. These adverse events also occur as manifestations of Fabry disease; an alteration in frequency or severity cannot be determined from the small numbers of patients studied.
Adverse Reactions in Pediatric Patients
The safety profile of Fabrazyme in pediatric Fabry disease patients, ages 8 to 16 years, was found to be consistent with that seen in adults [see Use in Specific Populations (8.4) and Clinical Studies (14)]. The safety of Fabrazyme in patients younger than 8 years of age has not been evaluated.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other agalsidase products may be misleading.
The following data reflect the percentage of patients whose test results were considered positive for antibodies to Fabrazyme using an ELISA and radioimmunoprecipitation (RIP) assay for antibodies.
Ninety-five of 121 (79%) adult patients and 11 of 16 (69%) pediatric patients (106 of 137, 74% of all patients) treated with Fabrazyme in clinical studies have developed IgG antibodies to Fabrazyme. Most patients who develop IgG antibodies do so within the first three months of exposure. IgG seroconversion in pediatric patients was associated with prolonged half-life of Fabrazyme, a phenomenon rarely observed in adult patients [see Clinical Pharmacology (12.3) and Use in Specific Populations (8.4)]. A possible cause for this prolongation likely pertains to the ability of antibodies to act as "carriers" for their antigens. Among the 14 female patients exposed to Fabrazyme in clinical studies, six (adult patients) developed IgG antibodies to Fabrazyme.
IgG antibodies to Fabrazyme were purified from 15 patients with high antibody titers (≥12,800) and studied for inhibition of in vitro enzyme activity. Under the conditions of this assay, most of these 15 patients had inhibition of in vitro enzyme activity ranging between 21%–74% at one or more time points during the study. Assessment of inhibition of enzyme uptake in cells has not been performed. No general pattern was seen in individual patient reactivity over time. The clinical significance of binding and/or inhibitory antibodies to Fabrazyme is not known. In patients followed in the open-label extension study, reduction of GL-3 in plasma and GL-3 inclusions in superficial skin capillaries was maintained after antibody formation.
Testing for IgE antibodies was performed in approximately 60 patients in clinical trials who experienced moderate to severe infusion-associated reactions or in whom mast cell activation was suspected. Seven of these patients tested positive for Fabrazyme-specific IgE antibodies or had a positive skin test to Fabrazyme. Patients who have had a positive skin test to Fabrazyme, or who have tested positive for Fabrazyme-specific IgE antibodies in clinical trials with Fabrazyme have been rechallenged [see Clinical Studies (14), Warnings and Precautions (5.4), and Dosage and Administration (2.1)].
6.3 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of Fabrazyme. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Cardiovascular: cardiorespiratory arrest, cardiac failure, myocardial infarction, palpitations,
- Infections: sepsis and pneumonia
- Infusion-associated reactions: anaphylaxis [see Warnings and Precautions (5.1)], localized angioedema (including auricular swelling, eye swelling, dysphagia, lip swelling, edema, pharyngeal edema, face swelling, and swollen tongue), and bronchospasm
- General: hyperhidrosis, asthenia, infusion site reaction
- Lymphatic: lymphadenopathy
- Musculoskeletal: arthralgia
- Nasopharyngeal: rhinorrhea
- Neurologic: cerebrovascular accident, hypoesthesia, oral hypoesthesia
- Ophthalmologic: increased lacrimation
- Pulmonary: respiratory failure, hypoxia
- Renal: renal failure
- Dermatologic: erythema
- Vascular: leukocytoclastic vasculitis
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
Pregnant women and women of reproductive potential should be encouraged to enroll in the Fabry patient registry. The registry will monitor the effect of Fabrazyme on pregnant women and their offspring. For more information, visit www.registrynxt.com or call 1-800-745-4447, extension 15500.
Risk Summary
Available data from postmarketing case reports and case series with Fabrazyme use in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes.
Reproduction studies performed in rats at doses up to 68 times the human dose have revealed no evidence of effects on embryo-fetal development (see Data).
The estimated background risk of major birth defects and miscarriage in the indicated population is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal data
The effects of agalsidase beta on embryo-fetal development in rats were evaluated at doses of 3, 10, and 30 mg/kg/day (up to 68 times the human dose of 1 mg/kg every 2 weeks on a body surface area basis) during gestation days 7 to 17. Hepatocellular necrosis consistent with accumulation of test article was evident in maternal livers in the 10 and 30 mg/kg/day groups (23 and 68 times the human dose on a body surface area basis). There were no adverse effects of agalsidase beta on embryo-fetal development in rats.
8.2 Lactation
Risk Summary
There are no data on the presence of agalsidase beta in either human or animal milk, the effects of the drug on the breastfed infant, or on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Fabrazyme and any potential adverse effects on the breastfed child from Fabrazyme or from the underlying maternal condition.
Lactating women with Fabry disease treated with Fabrazyme should be encouraged to enroll in the Fabry registry [see Use in Specific Populations (8.1)].
8.4 Pediatric Use
The safety and effectiveness of Fabrazyme have been established in pediatric patients 8 years of age and older. Use of Fabrazyme in this age group is supported by evidence from a multinational, multicenter, uncontrolled, open-label study in 16 pediatric patients with Fabry disease (14 males, 2 females) ages 8 to 16 years [see Clinical Studies (14)].
The safety and effectiveness of Fabrazyme have not been established in pediatric patients less than 8 years of age.
8.5 Geriatric Use
Clinical studies of Fabrazyme did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
8.6 Responses in Women
Fabry disease is an X-linked genetic disorder. However, some heterozygous women will develop signs and symptoms of Fabry disease due to the variability of the X-chromosome inactivation within cells.
A total of 12 adult female patients with Fabry disease were enrolled in two separate randomized, double-blind, placebo-controlled clinical studies with Fabrazyme, and two female pediatric patients with Fabry disease, ages 11 years, were evaluated in an open-label, uncontrolled pediatric study [see Use in Specific Populations (8.4) and Clinical Studies (14)]. Although the safety and efficacy data available in female patients in these clinical studies are limited, there is no indication that female patients respond differently to Fabrazyme compared to males.
-
10 OVERDOSAGE
There have been no reports of overdose with Fabrazyme. In clinical trials, patients received doses up to 3 mg/kg body weight. The adverse reactions experienced by patients who received treatment with 3 mg/kg were similar to the adverse reactions experienced by patients who received treatment with 1 mg/kg.
-
11 DESCRIPTION
Agalsidase beta is a recombinant human α-galactosidase A enzyme with the same amino acid sequence as the native enzyme. Purified agalsidase beta is a homodimeric glycoprotein with a molecular weight of approximately 100 kD. The mature protein is comprised of two subunits of 398 amino acids (approximately 51 kD), each of which contains three N-linked glycosylation sites. α-galactosidase A catalyzes the hydrolysis of globotriaosylceramide (GL-3) and other α-galactyl-terminated neutral glycosphingolipids, such as galabiosylceramide and blood group B substances to ceramide dihexoside and galactose. The specific activity of agalsidase beta is approximately 70 U/mg (one unit is defined as the amount of activity that results in the hydrolysis of 1 µmole of a synthetic substrate, p-nitrophenyl-α-D-galactopyranoside, per minute under the assay conditions).
Agalsidase beta is produced by recombinant DNA technology in a Chinese hamster ovary mammalian cell expression system.
Fabrazyme (agalsidase beta) for injection is intended for intravenous infusion. It is supplied as a sterile, nonpyrogenic, preservative-free, white to off-white, lyophilized cake or powder for reconstitution with Sterile Water for Injection, USP. Each 35 mg vial contains 37 mg of agalsidase beta, as well as 222 mg mannitol, 20.4 mg sodium phosphate monobasic monohydrate, and 59.2 mg sodium phosphate dibasic heptahydrate. Following reconstitution as directed, 35 mg of agalsidase beta (7 mL) may be extracted from each 35 mg vial.
Each 5 mg vial contains 5.5 mg of agalsidase beta, as well as 33.0 mg mannitol, 3.0 mg sodium phosphate monobasic monohydrate, and 8.8 mg sodium phosphate dibasic heptahydrate. Following reconstitution as directed, 5 mg of agalsidase beta (1 mL) may be extracted from each 5 mg vial.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fabry disease is an X-linked genetic disorder of glycosphingolipid metabolism. Deficiency of the lysosomal enzyme α-galactosidase A leads to progressive accumulation of glycosphingolipids, predominantly GL-3, in many body tissues, starting early in life and continuing over decades. Clinical manifestations of Fabry disease include renal failure, cardiomyopathy, and cerebrovascular accidents. Accumulation of GL-3 in renal endothelial cells may play a role in renal failure.
Fabrazyme is intended to provide an exogenous source of α-galactosidase A in Fabry disease patients. Nonclinical and clinical studies evaluating a limited number of cell types indicate that Fabrazyme will catalyze the hydrolysis of glycosphingolipids, including GL-3.
12.2 Pharmacodynamics
In a placebo-controlled study conducted in patients with Fabry disease after intravenous administration of 1 mg/kg of Fabrazyme every two weeks for 20 weeks, a reduction of GL-3 was observed in the capillary endothelium (vasculature) of kidney, heart, and skin as determined by histological assessment, and in plasma as determined by ELISA [see Clinical Studies (14)].
12.3 Pharmacokinetics
Plasma pharmacokinetic profiles of Fabrazyme were characterized at 0.3, 1, and 3 mg/kg in adult patients with Fabry disease. The area under the plasma concentration-time curve (AUC∞) and the clearance (CL) did not increase proportionately with increasing doses, demonstrating that the enzyme follows non-linear pharmacokinetics (Table 3). Plasma pharmacokinetic profiles were also characterized in adult patients with Fabry disease given 1 mg/kg Fabrazyme every 14 days for a total of 11 infusions. Refer to Table 3 below for more details.
In 15 pediatric Fabry patients (ranging in age from 8 to 16 years old and weighing between 27.1 to 64.9 kg) who were dosed with 1 mg/kg every 14 days, Fabrazyme pharmacokinetics were not weight-dependent (Table 3). Fabrazyme concentrations were about five times higher after IgG seroconversion, without any detectable impact on GL-3 clearance.
IgG seroconversion in pediatric patients was associated with prolonged half-life and plasma concentrations of Fabrazyme, a phenomenon rarely observed in adult patients. A possible cause for this prolongation likely pertains to the ability of antibodies to potentially act as "carriers" for their antigens [see Adverse Reactions (6.2) and Use in Specific Populations (8.4)].
Table 3: Fabrazyme Pharmacokinetic Summary Dose Regimen Mean Infusion Length
(min)Infusion number
(n=patients)AUC(0–∞)
µg min/mLCmax
µg/mLHalf-life
minCL
mL/min/kgVss*
mL/kgAll data reported as the mean ± standard deviation. - * Vss = volume of distribution at steady state
Study FB9702-01: Phase 1/2 Study in Adult Patients with Fabry Disease 0.3 mg/kg q14 days × 5 132 1 (n=3) 79 ± 24 0.6 ± 0.2 92 ± 27 4.1 ± 1.2 225 ± 62 128 5 (n=3) 74 ± 30 0.6 ± 0.2 78 ± 67 4.6 ± 2.2 330 ± 231 1 mg/kg q14 days × 5 115 1 (n=3) 496 ± 137 5.0 ± 1.1 67 ± 12 2.1 ± 0.7 112 ± 13 120 5 (n=2) 466 ± 382 4.74 ± 4.3 45 ± 3 3.2 ± 2.6 243 ± 236 3 mg/kg q14 days × 5 129 1 (n=2) 4168 ± 1401 29.7 ± 14.6 102 ± 4 0.8 ± 0.3 81 ± 45 300 5 (n=2) 4327 ± 2074 19.8 ± 5.8 87 ± 21 0.8 ± 0.4 165 ± 80 Study AGAL-1-002-98: Phase 3 Study in Adult Patients with Fabry Disease 1 mg/kg q14 days × 11 280 1–3 (n=11) 649 ± 226 3.5 ± 1.6 89 ± 20 1.8 ± 0.8 120 ± 80 280 7 (n=11) 372 ± 223 2.1 ± 1.14 82 ± 25 4.9 ± 5.6 570 ± 710 300 11 (n=11) 784 ± 521 3.5 ± 2.2 119 ± 49 2.3 ± 2.2 280 ± 230 Study AGAL-016-01: Phase 2 Study in Pediatric Patients with Fabry Disease 1 mg/kg q14 days × 24 208 1 (n=8–9) 344 ± 307 2.2 ± 1.9 86 ± 27 5.8 ± 4.6 1097 ± 912 111 12 (n=15) 1007 ± 688 4.9 ± 2.4 130 ± 41 1.6 ± 1.2 292 ± 185 108 24 (n=9–10) 1238 ± 547 7.1 ± 4.4 151 ± 59 1.1 ± 0.8 247 ± 146 -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
There are no animal or human studies to assess the carcinogenic or mutagenic potential of Fabrazyme. A study to evaluate the effects of agalsidase beta on fertility and general reproduction was performed in male and female rats at doses up to 10 mg/kg/day (23 times the human dose, on a body surface area basis). There were no adverse effects of agalsidase beta on fertility and early embryonic development in rats.
-
14 CLINICAL STUDIES
The safety and efficacy of Fabrazyme were assessed in four clinical studies in patients with Fabry disease.
Study 1 was a randomized, double-blind, placebo-controlled, multinational, multicenter study of 58 Fabry patients (56 males and 2 females), ages 16 to 61 years, all naive to enzyme replacement therapy. Patients received either 1 mg/kg of Fabrazyme or placebo every two weeks for five months (20 weeks) for a total of 11 infusions. All patients were pretreated with acetaminophen and an antihistamine to decrease or prevent infusion-associated reactions. Oral steroids were an additional option to the pretreatment regimen for patients who exhibited severe or recurrent infusion-associated reactions. The primary efficacy endpoint of GL-3 inclusions in renal interstitial capillary endothelial cells, was assessed by light microscopy and was graded on an inclusion severity score ranging from 0 (normal or near normal) to 3 (severe inclusions).
A GL-3 inclusion score of 0 was achieved in 20 of 29 (69%) patients treated with Fabrazyme compared to 0 of 29 treated with placebo (p<0.001). Similar reductions in GL-3 inclusions were observed in the capillary endothelium of the heart and skin (Table 4). No differences between groups in symptoms or renal function were observed during this five-month study.
Table 4: Reduction of GL-3 Inclusions to Normal or Near Normal Levels (0 Score) in the Capillary Endothelium of the Kidney, Heart, and Skin 5 Months of the Controlled Study 6 Months of the Open-label Extension Study Placebo
(n=29)Fabrazyme
(n=29)Placebo/Fabrazyme
(n=29)*Fabrazyme/Fabrazyme
(n=29)*- * Results reported where biopsies were available
Kidney 0/29 20/29 24/24 23/25 Heart 1/29 21/29 13/18 19/22 Skin 1/29 29/29 25/26 26/27 All 58 patients in Study 1 participated in an open-label extension study of Fabrazyme at 1 mg/kg every two weeks, which continued for an additional 54 months. At the end of six months of open-label treatment, most patients achieved a GL-3 inclusion score of 0 in capillary endothelium (Table 4). GL-3 was decreased to normal or near normal levels in mesangial cells, glomerular capillary endothelium, interstitial cells, and non-capillary endothelium. GL-3 deposition was still present in vascular smooth muscle cells, tubular epithelium and podocytes, at variably reduced levels. Forty-four of the 58 patients completed 54 months of the open-label extension study. Thirty-six of these 44 patients underwent follow-up skin biopsy, and 31 of these patients showed sustained GL-3 clearance in the capillary endothelium of the skin. Follow-up heart and kidney biopsies were assessed in only 8 of the 44 patients, which showed sustained GL-3 clearance in the capillary endothelium of the kidney in 8 patients, and sustained GL-3 clearance in the capillary endothelium of the heart in 6 patients. Plasma GL-3 levels were reduced to normal levels (≤7.03 µg/mL determined by LC/MS/MS) and remained at normal levels after up to 60 months of treatment. The reduction of GL-3 inclusions suggests that Fabrazyme may ameliorate disease expression; however, the relationship of GL-3 inclusion reduction to specific clinical manifestations of Fabry disease has not been established.
Study 2 was a randomized (2:1 Fabrazyme to placebo), double-blind, placebo-controlled, multinational, multicenter study of 82 patients (72 males and 10 females), ages 20 to 72 years, all naive to enzyme replacement therapy. Patients received either 1 mg/kg of Fabrazyme or placebo every two weeks for up to a maximum of 35 months (median 18.5 months). There was significant difference in postbaseline plasma GL-3 levels in the Fabrazyme-treated patients compared to placebo. The reduction in plasma GL-3 levels in the Fabrazyme group compared to the placebo group was significant at one year (p<0.0001) and at two years (p=0.0019). Fourteen patients (8 in Fabrazyme-treated and 6 in placebo) had skin biopsies at first infusion and final visit. All Fabrazyme-treated patients had capillary endothelium and deep vessel endothelium scores of zero at the final visit. Four (4) of 6 placebo patients had non-zero capillary endothelium scores (p=0.0150), and 6 of 6 had non-zero deep vessel endothelium scores (p=0.0003).
Sixty-seven patients who participated in Study 2 were subsequently entered into an open-label extension study in which all patients received 1 mg/kg of Fabrazyme every two weeks for up to a maximum of 18 months. There was a statistically significant reduction in mean plasma GL-3 levels with durability in effect through the additional 18 months of treatment in the extension study from pretreatment baseline.
Study 3 (Pediatric Study) was an open-label, uncontrolled, multinational, multicenter study to evaluate safety, pharmacokinetics, and pharmacodynamics of Fabrazyme treatment in 16 pediatric patients with Fabry disease (14 males, 2 females), who were ages 8 to 16 years at first treatment. All patients received Fabrazyme 1 mg/kg every two weeks for up to 48 weeks. At baseline, all 14 males had elevated plasma GL-3 levels (i.e., >7.03 µg/mL), whereas the two female patients had normal plasma GL-3 levels. Twelve of the 14 male patients, and no female patients, had GL-3 inclusions observed in the capillary endothelium on skin biopsies at baseline. At Weeks 24 and 48 of treatment, all 14 males had plasma GL-3 within the normal range. The 12 male patients with GL-3 inclusions in capillary endothelium at baseline achieved GL-3 inclusion scores of 0 at Weeks 24 and 48 of treatment. The two female patients' plasma GL-3 levels remained normal through study Week 48.
No new safety concerns were identified in pediatric patients in this study, and the overall safety and efficacy profile of Fabrazyme treatment in pediatric patients was found to be consistent with that seen in adults. Immunologic responses in pediatric patients may differ from those in adults, as IgG seroconversion in pediatric patients was associated with prolonged half-life concentrations of Fabrazyme, a phenomenon rarely observed in adult patients [see Clinical Pharmacology (12.3), Adverse Reactions (6.2), and Use in Specific Populations (8.4)].
Study 4 was an open-label, rechallenge study to evaluate the safety of Fabrazyme treatment in patients who had a positive skin test to Fabrazyme or who had tested positive for Fabrazyme-specific IgE antibodies. In this study, six adult male patients, who had experienced multiple or recurrent infusion-associated reactions during previous clinical trials with Fabrazyme, were rechallenged with Fabrazyme administered as a graded infusion, for up to 52 weeks of treatment [see Warnings and Precautions (5.4)]. The initial two rechallenge doses of Fabrazyme were administered as a 0.5 mg/kg dose per week at an initial infusion rate of 0.01 mg/min for the first 30 minutes (1/25th the usually recommended maximum infusion rate). The infusion rate was doubled every 30 minutes thereafter, as tolerated, for the remainder of the infusion up to a maximum rate of 0.25 mg/min. If the patient tolerated the infusion, the dose was increased to 1 mg/kg every two weeks (usually recommended dose), and the infusion rate was increased by slow titration upwards [see Dosage and Administration (2.1)]. Four of the six patients treated in this study received at least 26 weeks of study medication, and two patients discontinued prematurely due to recurrent infusion-associated reactions [see Warnings and Precautions (5.4)].
-
16 HOW SUPPLIED/STORAGE AND HANDLING
Fabrazyme (agalsidase beta) for injection is supplied as a sterile, nonpyrogenic, white to off-white lyophilized cake or powder in single-dose vials.
35 mg vial: NDC: 58468-0040-1
5 mg vial: NDC: 58468-0041-1
Refrigerate vials of Fabrazyme at 2°C to 8°C (36°F to 46°F). Do not use Fabrazyme after the expiration date on the vial.
This product contains no preservatives. Reconstituted and diluted solutions of Fabrazyme should be used immediately. If immediate use is not possible, the reconstituted and diluted solution may be stored for up to 24 hours at 2°C to 8°C (36°F to 46°F) [see Dosage and Administration (2.2)].
-
17 PATIENT COUNSELING INFORMATION
Inform patients that a Registry has been established in order to better understand the variability and progression of Fabry disease in the population as a whole and in women [see Use in Specific Populations (8.1)], and to monitor and evaluate long-term treatment effects of Fabrazyme. The Registry will also monitor the effect of Fabrazyme on pregnant women and their offspring. Encourage patients to participate. Advise patients that their participation is voluntary and may involve long-term follow-up. For more information, visit www. registrynxt.com or call 1-800-745-4447, extension 15500.
- SPL UNCLASSIFIED SECTION
-
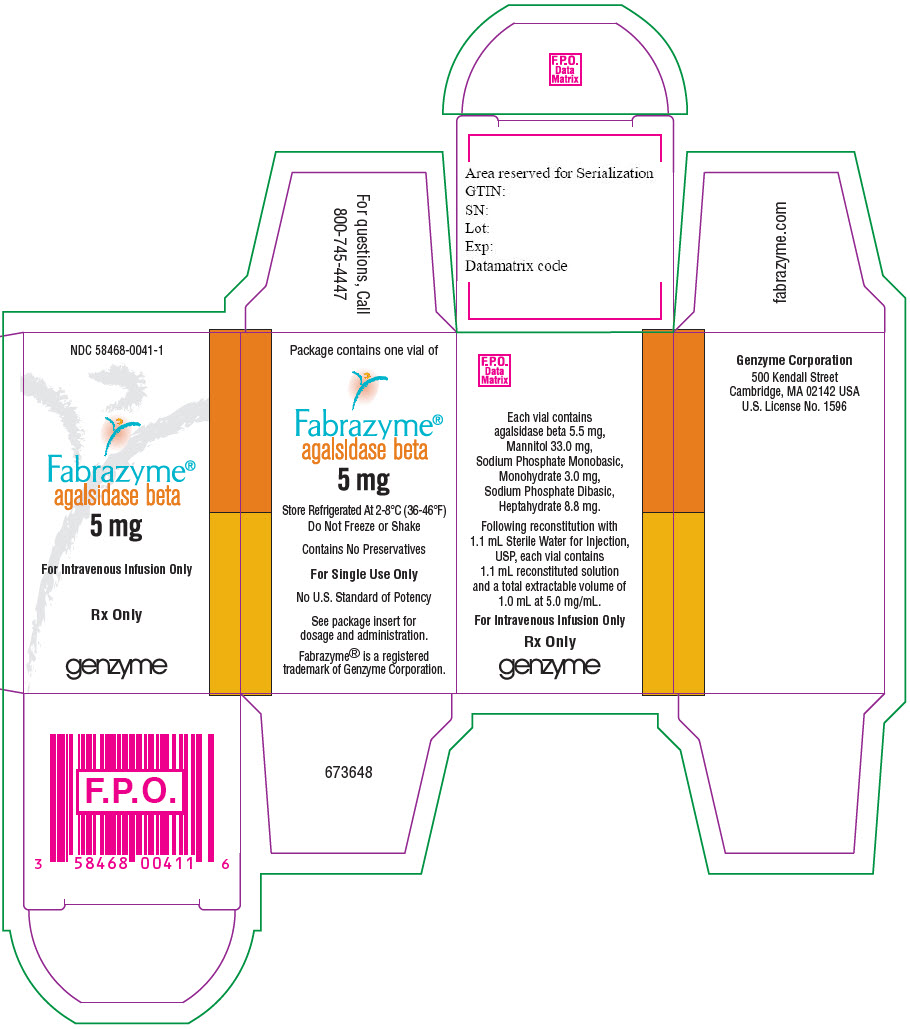
PRINCIPAL DISPLAY PANEL - 5 mg Vial Carton
NDC: 58468-0041-1 Rx only
Fabrazyme®
agalsidase beta5 mg
For Intravenous Infusion Only
One single-dose vial
Discard unused portion
SANOFI GENZYME
-
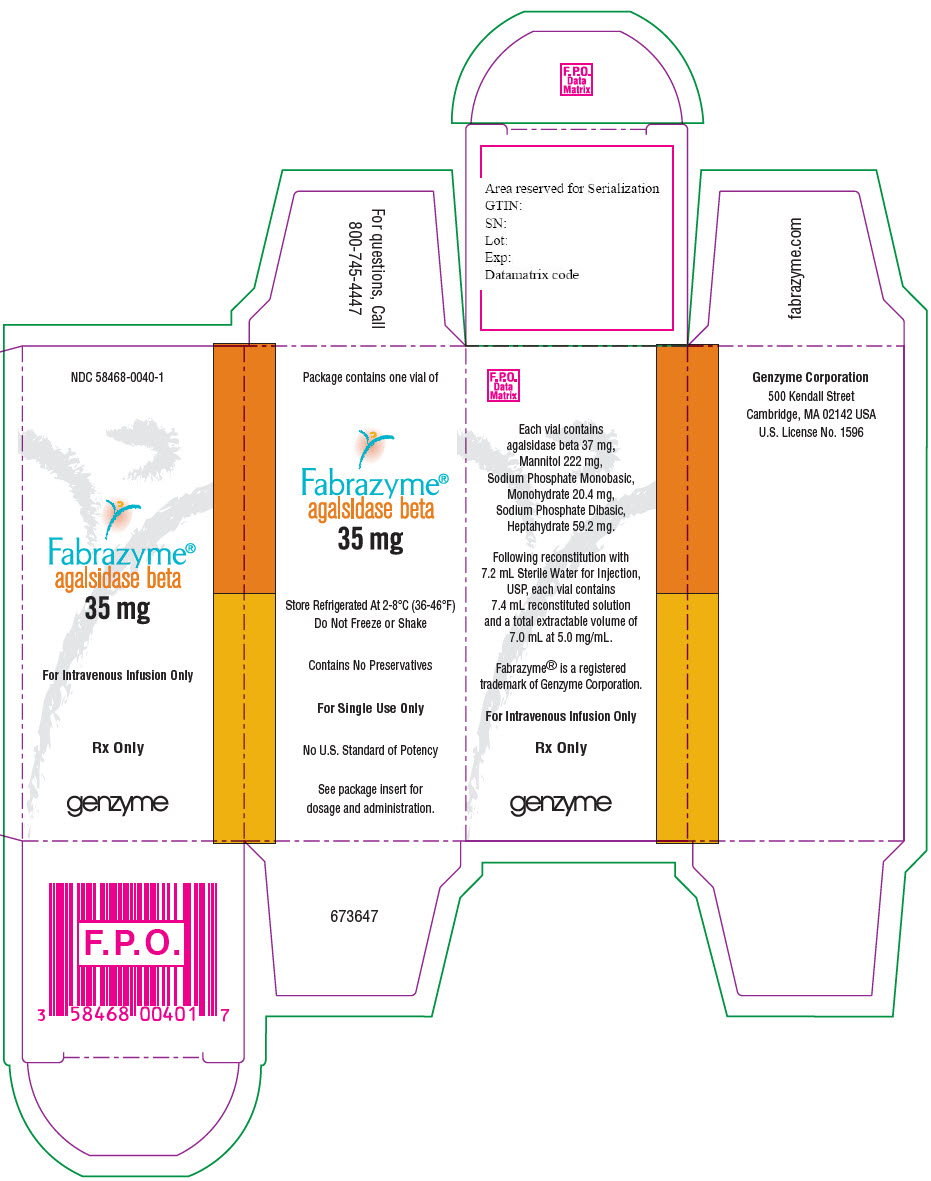
PRINCIPAL DISPLAY PANEL - 35 mg Vial Carton
NDC: 58468-0040-1 Rx only
Fabrazyme®
agalsidase beta35 mg
For Intravenous Infusion Only
One single-dose vial
Discard unused portion
SANOFI GENZYME
-
INGREDIENTS AND APPEARANCE
FABRAZYME
agalsidase beta injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 58468-0041 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AGALSIDASE BETA (UNII: RZD65TSM9U) (AGALSIDASE BETA - UNII:RZD65TSM9U) AGALSIDASE BETA 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 33 mg in 1 mL SODIUM PHOSPHATE, MONOBASIC, MONOHYDRATE (UNII: 593YOG76RN) 3 mg in 1 mL SODIUM PHOSPHATE, DIBASIC, HEPTAHYDRATE (UNII: 70WT22SF4B) 8.8 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 58468-0041-1 1 in 1 CARTON 12/17/2008 1 1 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103979 12/17/2008 FABRAZYME
agalsidase beta injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 58468-0040 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength AGALSIDASE BETA (UNII: RZD65TSM9U) (AGALSIDASE BETA - UNII:RZD65TSM9U) AGALSIDASE BETA 5 mg in 1 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 222 mg in 1 mL SODIUM PHOSPHATE, MONOBASIC, MONOHYDRATE (UNII: 593YOG76RN) 20.4 mg in 1 mL SODIUM PHOSPHATE, DIBASIC, HEPTAHYDRATE (UNII: 70WT22SF4B) 59.2 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 58468-0040-1 1 in 1 CARTON 12/17/2008 1 7 mL in 1 VIAL, GLASS; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA103979 12/17/2008 Labeler - Genzyme Corporation (025322157) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 926029653 ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 968278916 API MANUFACTURE(58468-0040, 58468-0041) , ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 050424395 LABEL(58468-0040, 58468-0041) , PACK(58468-0040, 58468-0041) , ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Hospira, Inc. 030606222 MANUFACTURE(58468-0040, 58468-0041) , ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 968278874 API MANUFACTURE(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 968278932 API MANUFACTURE(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 943130096 API MANUFACTURE(58468-0040, 58468-0041) , ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 034378252 ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 968302658 ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Corporation 078456891 ANALYSIS(58468-0040, 58468-0041) Establishment Name Address ID/FEI Business Operations Genzyme Ireland 985127419 MANUFACTURE(58468-0040, 58468-0041) , ANALYSIS(58468-0040, 58468-0041) , LABEL(58468-0040, 58468-0041) , PACK(58468-0040, 58468-0041)
Trademark Results [Fabrazyme]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 FABRAZYME 75844246 2528286 Live/Registered |
GENZYME THERAPEUTIC PRODUCTS LIMITED PARTNERSHIP 1999-11-10 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.