LIDOCAINE HYDROCHLORIDE- lidocaine hydrochloride injection, solution
Lidocaine hydrochloride by
Drug Labeling and Warnings
Lidocaine hydrochloride by is a Prescription medication manufactured, distributed, or labeled by Camber Pharmaceuticals, Inc., Aspiro Pharma Limited. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LIDOCAINE HYDROCHLORIDE INJECTION safely and effectively. See full prescribing information for LIDOCAINE HYDROCHLORIDE INJECTION.
LIDOCAINE HYDROCHLORIDE injection, for infiltration and nerve block
Initial U.S. Approval: 1948INDICATIONS AND USAGE
Lidocaine hydrochloride injection contains lidocaine, an amide local anesthetic. Lidocaine hydrochloride injection is indicated in adult and pediatric patients for the production of local or regional anesthesia or analgesia for surgery, dental, and oral surgery procedures, diagnostic and therapeutic procedures, and for obstetrical procedures. For each type of block indicated to produce local or regional anesthesia or analgesia, specific concentrations and presentations are recommended. ( 1, 2.2)
DOSAGE AND ADMINISTRATION
See Full Prescribing Information for recommended dosages and administration information for adult and pediatric patients (2)
DOSAGE FORMS AND STRENGTHS
Lidocaine hydrochloride injection: 1%, 2% (3)
CONTRAINDICATIONS
Known hypersensitivity to any local anesthetic agent of the amide-type or to other components of lidocaine hydrochloride injection. (4)
WARNINGS AND PRECAUTIONS
Dose-Related Toxicity:Monitor cardiovascular and respiratory vital signs and patient’s state of consciousness after injection of lidocaine hydrochloride injection ( 5.1)
Methemoglobinemia:Cases of methemoglobinemia have been reported in association with local anesthetics use. See full prescribing information for more details on managing these risks. ( 5.2)
Chondrolysis with Intra-Articular Infusion:Avoid Intra-articular infusions as there have been post-marketing reports of chondrolysis in patients receiving such infusion. ( 5.4)
Allergic-Type Reactions to Sulfites in Lidocaine Hydrochloride Injection and Anaphylactic Reactions:Lidocaine hydrochloride injection without epinephrine does not contain sodium metabisulfite ( 5.6)
Risk of Systemic Toxicities with Unintended Intravascular or Intrathecal Injection:Unintended intravascular or intrathecal injection may be associated with systemic toxicities, including CNS or cardiorespiratory depression and coma, progression ultimately to respiratory arrest. Aspirate for blood prior to each dose of lidocaine hydrochloride injection ( 5.7)ADVERSE REACTIONS
Most common adverse reactions are as follows:
Central Nervous System: Lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest. ( 6)
Cardiovascular System: Bradycardia, hypotension, and cardiovascular collapse. ( 6)
Allergic: Cutaneous lesions, urticaria, edema or anaphylactoid reactions. ( 6)
Neurologic: Positional headaches, hypotension and backache. ( 6)
Hematologic: Methemoglobinemia. ( 6)
To report SUSPECTED ADVERSE REACTIONS, contact Aspiro Pharma Limited at 1-866-495-1995 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
DRUG INTERACTIONS
Local Anesthetics:The toxic effects of local anesthetics are additive. Monitor for neurologic and cardiovascular effects when additional local anesthetics are administered ( 7.1)
Monoamine Oxidase Inhibitors and Tricyclic Antidepressants:Administration of lidocaine hydrochloride to patients receiving monoamine oxidase inhibitors or tricyclic antidepressants may produce severe, prolonged hypertension Concurrent use of these agents should generally be avoided ( 5.5, 7.2)
Ergot-type Oxytocic drugs:Concurrent administration of lidocaine hydrochloride and ergot-type oxytocic drugs may cause severe, persistent hypertension or cerebrovascular accidents ( 5.5, 7.3)
Nonselective Beta-Adrenergic Antagonists:Administration of lidocaine hydrochloride in patients receiving nonselective beta-adrenergic antagonist may cause severe hypertension and bradycardia. Concurrent use of these agents should generally be avoided. ( 5.5, 7.4)
Drugs Associated with Methemoglobinemia:Patients are at increased risk of developing methemoglobinemia when concurrently exposed to nitrates, nitrites, local anesthetics, antineoplastic agents, antibiotics, antimalarials, anticonvulsants and other drugs ( 7.5).
Geriatric Use:Elderly patients should be given reduced doses commensurate with their age and physical condition ( 8.5)
Hepatic Impairment:consider reduced dosing and increased monitoring for local anesthetic systemic toxicity in patients with hepatic impairment ( 8.6)See 17 for PATIENT COUNSELING INFORMATION.
Revised: 4/2025
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
2.2 Recommended Concentrations and Dosages of Lidocaine Hydrochloride Injection in adults
2.6 Maximum Recommend Dosage
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Dose Related Toxicity
5.2 Methemoglobinemia
5.3 Antimicrobial Preservatives in Multiple-Dose Vials
5.4 Chondrolysis with Intra-Articular Infusion
5.5 Risk of Adverse Reactions Due to Drug Interactions with Lidocaine Hydrochloride Injection
5.6 Allergic-Type Reactions to Sulfites in Lidocaine Hydrochloride Injection and Anaphylactic Reactions
5.7 Risk of Systemic Toxicities with Unintended Intravascular or Intrathecal Injection
5.8 Risk of Toxicity in Patients with Hepatic Impairment
5.9 Risk of Use in Patients with Impaired Cardiovascular Function
5.12 Risk of Adverse Reactions with Use in the Head and Neck Area
5.13 Familial Malignant Hyperthermia
5.14 Risk of Respiratory Arrest with Use in Ophthalmic Surgery
5.16 Drug/Laboratory Test Interactions
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 Local Anesthetics
7.2 Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
7.3 Ergot-Type Oxytocic Drugs
7.4 Nonselective Beta-Adrenergic Antagonists
7.5 Drugs Associated with Methemoglobinemia
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
17.1 Allergic Type Reactions
17.3 Methemoglobinemia
- * Sections or subsections omitted from the full prescribing information are not listed.
- BOXED WARNING (What is this?)
-
1 INDICATIONS AND USAGE
Lidocaine hydrochloride injection is indicated in adult and pediatric patients for the production of local or regional anesthesia or analgesia for surgery, dental, and oral surgery procedures, diagnostic and therapeutic procedures, and for obstetrical procedures. Specific concentrations and presentations of lidocaine hydrochloride injection are recommended for each type of block indicated to produce local or regional anesthesia or analgesia [see Dosage and Administration (2.2)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Information
Lidocaine hydrochloride injection is not recommended for intrathecal use.
Avoid use of lidocaine hydrochloride injection solutions containing antimicrobial preservatives (i.e., multiple-dose vials) for epidural or caudal anesthesia [see Warnings and Precautions (5.3)].
Visually inspect this product for particulate matter and discoloration prior to administration whenever solution and container permit. Lidocaine hydrochloride injection is clear, colorless solution. Do not administer solution which is discolored or contain particulate matter.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever the solution and container permit. Solution which is discolored (e.g., pinkish or darker than slightly yellow) or which contain particulate matter or precipitate should not be administered.
Mixing or the prior or intercurrent use of any other local anesthetic with lidocaine hydrochloride injection is not recommended because of insufficient data on the clinical use of such mixtures.
Administration Precautions
Lidocaine hydrochloride injection is to be administered in carefully adjusted dosages by or under the supervision of experienced clinicians who are well versed in the diagnosis and management of dose-related toxicity and other acute emergencies which might arise from the block to be employed.
Use lidocaine hydrochloride injection only if the following are immediately available: oxygen, cardiopulmonary resuscitative equipment and drugs, and the personnel resources needed for proper management of toxic reactions and related emergencies [see Warnings and Precautions (5.1), Adverse Reactions (6), Overdosage (10)] .
The toxic effects of local anesthetics are additive. Monitor for neurologic and cardiovascular effects related to local anesthetic systemic toxicity when additional local anesthetics are administered with lidocaine hydrochloride injection [see Warnings and Precautions (5.1), Drug Interactions (7.1), Overdosage (10)] .
Aspirate for blood prior to injecting lidocaine hydrochloride injection, both the initial dose and all subsequent doses, to avoid intravascular or intrathecal injection. However, a negative aspiration for blood does not ensure against an intravascular injection [see Warnings and Precautions (5.7)] .
Avoid rapid injection of a large volume of lidocaine hydrochloride injection and use fractional (incremental) doses when feasible.
During major regional nerve blocks, such as those of the brachial plexus or lower extremity, the patient should have an indwelling intravenous catheter to assure adequate intravenous access. The lowest dosage of lidocaine hydrochloride injection that results in effective anesthesia should be used to avoid high plasma levels and serious adverse reactions.
Perform careful and constant monitoring of cardiovascular and respiratory (adequacy of oxygenation and ventilation) vital signs and the patient’s level of consciousness after each local anesthetic injection.
Use lidocaine hydrochloride injection in carefully restricted quantities in areas of the body supplied by end arteries or having otherwise compromised blood supply such as digits, nose, external ear, or penis [see Warnings and Precautions (5.10)].2.2 Recommended Concentrations and Dosages of Lidocaine Hydrochloride Injection in adults
The dosage of lidocaine hydrochloride injection administered varies with the anesthetic procedure, the area to be anesthetized, the vascularity of the tissues, the number of neuronal segments to be blocked, the depth of anesthesia and degree of muscle relaxation required, the duration of anesthesia desired, individual tolerance, and the physical condition of the patient. Administer the smallest dosage and concentration required to produce the desired result.
The types of block and recommended lidocaine hydrochloride injection concentrations are shown in Table 1. The dosages suggested in this table are for normal healthy adults and refer to the use of epinephrine-free solutions. Consider administration of solutions containing epinephrine when large volumes are required.
Table 1: Recommended Dosages in Adults
Procedure
Lidocaine Hydrochloride Injection
(without epinephrine)
Conc (%)
Vol (mL)
Total Dose (mg)
Infiltration
Percutaneous
Peripheral Nerve Blocks, e.g.,
Brachial
Dental
Intercostal
Paravertebral
Pudendal (each side)
Paracervical
0.5 or 1
1.5
2
1
1
1
1 to 60
15 to 20
1 to 5
3
3 to 5
10
5 to 300
225 to 300
20 to 100
30
30 to 50
100
Obstetrical analgesia (each side)
Sympathetic Nerve Blocks, e.g.,
Cervical (stellate ganglion)
Lumbar
1
1
1
10
5
5 to 10
100
50
50 to 100
The above suggested concentrations and volumes serve only as a guide. Other volumes and concentrations may be used provided the total maximum recommended dose is not exceeded [see Dosage and Administration (2.5)].
These recommended doses serve only as a guide to the amount of local anesthetic required for most indicated procedures. The actual volumes and concentrations to be used depend on a number of factors such as type and extent of surgical procedure, depth of anesthesia and degree of muscular relaxation required, duration of anesthesia required, and the physical condition of the patient. In all cases, the lowest concentration and smallest dose that will produce the desired result should be given. The maximum dosage limit within the recommended dosage range must be individualized in each case after evaluating the size and physical status of the patient, as well as the anticipated rate of systemic absorption from a particular injection site.2.6 Maximum Recommend Dosage
Adults
For normal healthy adults, the maximum individual dose should not exceed 4.5 mg/kg of body weight, and in general it is recommended that the maximum total dose does not exceed 300 mg.
The maximum recommended dose per 90 minute period of lidocaine hydrochloride for paracervical block in obstetrical patients and non-obstetrical patients is 200 mg total. One half of the total dose is usually administered to each side. Inject slowly, five minutes between sides [see Pregnancy (8.1)].
Pediatric Patients
A maximum dose of lidocaine hydrochloride injection for children varies based on age and weight. For children over 3 years of age with a normal lean body mass and normal body development, the maximum dose is determined by the child’s age and weight. For example, in a child of 5 years weighing approximately 23 kg, the dose of lidocaine hydrochloride should not exceed approximately 75 mg to 100 mg (3.3 mg/kg to 4.4 mg/kg).
-
3 DOSAGE FORMS AND STRENGTHS
Lidocaine hydrochloride Injection, USP is a clear, colorless solution available as:
1% (200 mg per 20 mL) (10 mg per mL), 20 mL multiple-dose vials
1% (500 mg per 50 mL) (10 mg per mL), 50 mL multiple-dose vials
2% (400 mg per 20 mL) (20 mg per mL), 20 mL multiple-dose vials
2% (1000 mg per 50 mL) (20 mg per mL), 50 mL multiple-dose vials - 4 CONTRAINDICATIONS
-
5 WARNINGS AND PRECAUTIONS
5.1 Dose Related Toxicity
The safety and effectiveness of lidocaine hydrochloride depend on proper dosage, correct technique, adequate precautions, and readiness for emergencies. Careful and constant monitoring of cardiovascular and respiratory (adequacy of ventilation) vital signs and the patient's state of consciousness should be performed after injection of lidocaine hydrochloride solution.
Possible early warning signs of central nervous system (CNS) toxicity are restlessness, anxiety, incoherent speech, lightheadedness, numbness and tingling of the mouth and lips, metallic taste, tinnitus, dizziness, blurred vision, tremors, twitching, CNS depression, or drowsiness. Delay in proper management of dose-related toxicity, underventilation from any cause, and/or altered sensitivity may lead to the development of acidosis, cardiac arrest, and, possibly, death.
During major regional nerve blocks, such as those of the brachial plexus or lower extremity, the patient should have an indwelling intravenous catheter to assure adequate intravenous access. Use the lowest dosage of lidocaine hydrochloride injection that results in effective anesthesia to avoid high plasma levels and serious adverse effects. Avoid rapid injection of a large volume of lidocaine hydrochloride solution and administer fractional (incremental) doses when feasible.
Injection of repeated doses of lidocaine hydrochloride injection may cause significant increases in plasma levels with each repeated dose due to slow accumulation of the drug or its metabolites, or to slow metabolic degradation. Tolerance to elevated blood levels varies with the status of the patient. Debilitated, elderly patients and acutely ill patients should be given reduced doses commensurate with their age and physical status.
5.2 Methemoglobinemia
Cases of methemoglobinemia have been reported in association with local anesthetic use. Although all patients are at risk for methemoglobinemia, patients with glucose-6-phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing clinical manifestations of the condition [see Drug Interactions ( 7.5)]. If local anesthetics must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended.
Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure and are characterized by a cyanotic skin discoloration and abnormal coloration of the blood. Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue lidocaine hydrochloride and any other oxidizing agents. Depending on the severity of the symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. More severe symptoms may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
5.3 Antimicrobial Preservatives in Multiple-Dose Vials
Avoid use of lidocaine hydrochloride solutions containing antimicrobial preservatives (i.e., those supplied in multiple-dose vials) for epidural or caudal anesthesia because safety has not been established with such use.
5.4 Chondrolysis with Intra-Articular Infusion
Intra-articular infusions of local anesthetics following arthroscopic and other surgical procedures is an unapproved use, and there have been post-marketing reports of chondrolysis in patients receiving such infusions. The majority of reported cases of chondrolysis have involved the shoulder joint; cases of gleno-humeral chondrolysis have been described in pediatric and adult patients following intra-articular infusions of local anesthetics with and without epinephrine for periods of 48 to 72 hours. There is insufficient information to determine whether shorter infusion periods are not associated with these findings. The time of onset of symptoms, such as joint pain, stiffness and loss of motion can be variable, but may begin as early as the 2nd month after surgery. Currently, there is no effective treatment for chondrolysis; patients who experienced chondrolysis have required additional diagnostic and therapeutic procedures and some required arthroplasty or shoulder replacement.
5.5 Risk of Adverse Reactions Due to Drug Interactions with Lidocaine Hydrochloride Injection
Risk of Severe, Persistent Hypertension Due to Drug Interactions Between Lidocaine Hydrochloride and Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
Administration of lidocaine hydrochloride in patients receiving monoamine oxidase inhibitors (MAOI), or tricyclic antidepressants may result in severe, prolonged hypertension. Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful monitoring of the patient's hemodynamic status is essential [see Drug Interactions (7.2)].
Risk of Severe, Persistent Hypertension or Cerebrovascular Accidents Due to Drug Interactions Between Lidocaine Hydrochloride and Ergot-Type Oxytocic Drugs
Concurrent administration of lidocaine hydrochloride and ergot-type oxytocic drugs may cause severe, persistent hypertension or cerebrovascular accidents. Avoid use of lidocaine hydrochloride concomitantly with ergot-type oxytocic drugs [see Drug Interactions (7.3)].
Risk of Hypertension and Bradycardia Due to Drug Interactions Between Lidocaine Hydrochloride and Nonselective Beta-Adrenergic Antagonists
Administration of lidocaine hydrochloride in patients receiving nonselective beta-adrenergic antagonists may cause severe hypertension and bradycardia. Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful monitoring of the patient's blood pressure and heart rate is essential [see Drug Interactions (7.4)]
5.6 Allergic-Type Reactions to Sulfites in Lidocaine Hydrochloride Injection and Anaphylactic Reactions
Lidocaine hydrochloride injection without epinephrine does not contain sodium metabisulfite.
Anaphylactic reactions may occur following administration of lidocaine hydrochloride [see Adverse Reactions (6)] . Lidocaine hydrochloride should be used with caution in persons with known drug sensitivities. Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross-sensitivity to lidocaine hydrochloride.5.7 Risk of Systemic Toxicities with Unintended Intravascular or Intrathecal Injection
Unintended intravascular or intrathecal injection of lidocaine hydrochloride may be associated with systemic toxicities, including CNS or cardiorespiratory depression and coma, progressing ultimately to respiratory arrest. Unintentional intrathecal injection during the intended performance of nerve blocks near the vertebral column has resulted in underventilation or apnea ("Total or High Spinal"). A high spinal has been characterized by paralysis of the legs, loss of consciousness, respiratory paralysis, and bradycardia [see Adverse Reactions (6)].
Aspirate for blood before injecting lidocaine hydrochloride injection, both the initial dose and all subsequent doses, to avoid intravascular injection. However, a negative aspiration for blood does not ensure against an intravascular injection.
5.8 Risk of Toxicity in Patients with Hepatic Impairment
Because amide local anesthetics such as lidocaine are metabolized by the liver, consider reduced dosing and increased monitoring for lidocaine systemic toxicity in patients with moderate to severe hepatic impairment who are treated with lidocaine hydrochloride injection, especially with repeat doses [see Use in Specific Populations (8.6)].
5.9 Risk of Use in Patients with Impaired Cardiovascular Function
Lidocaine hydrochloride injection should also be given in reduced doses in patients with impaired cardiovascular function since they may be less able to compensate for functional changes associated with the prolongation of A-V conduction produced by these drugs. Monitor patients closely for blood pressure, heart rate, and ECG changes.
5.12 Risk of Adverse Reactions with Use in the Head and Neck Area
Small doses of local anesthetics (e.g., lidocaine hydrochloride) injected into the head and neck area, including retrobulbar, dental and stellate ganglion blocks, may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. The injection procedures require the utmost care. Confusion, convulsions, respiratory depression and/or respiratory arrest, and cardiovascular stimulation or depression have been reported. These reactions may be due to intra- arterial injection of the local anesthetic with retrograde flow to the cerebral circulation. They may also be due to puncture of the dural sheath of the optic nerve during retrobulbar block with diffusion of any local anesthetic along the subdural space to the midbrain. Monitor circulation and respiration and constantly observe patients receiving lidocaine hydrochloride injection blocks. Resuscitative equipment and drugs, and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded [see Dosage and Administration (2.2)].
5.13 Familial Malignant Hyperthermia
Many drugs used during the conduct of anesthesia are considered potential triggering agents for familial malignant hyperthermia. Since it is not known whether amide-type local anesthetics may trigger this reaction and since the need for supplemental general anesthesia cannot be predicted in advance, it is suggested that a standard protocol for the management of malignant hyperthermia should be available. Early unexplained signs of tachycardia, tachypnea, labile blood pressure and metabolic acidosis may precede temperature elevation. Successful outcome is dependent on early diagnosis, prompt discontinuance of the suspect triggering agent(s) and institution of treatment, including oxygen therapy, indicated supportive measures and dantrolene (consult dantrolene sodium intravenous package insert before using).
5.14 Risk of Respiratory Arrest with Use in Ophthalmic Surgery
Clinicians who perform retrobulbar blocks should be aware that there have been reports of respiratory arrest following local anesthetic injection. Prior to retrobulbar block (e.g., with lidocaine hydrochloride), as with all other regional procedures, resuscitative equipment and drugs, and personnel to manage respiratory arrest or depression, convulsions, and cardiac stimulation or depression should be immediately available [see Warnings and Precautions (5.14)] . As with other anesthetic procedures, patients should be constantly monitored following ophthalmic blocks for signs of these adverse reactions, which may occur following relatively low total doses.
5.16 Drug/Laboratory Test Interactions
The intramuscular injection of lidocaine hydrochloride may result in an increase in creatine phosphokinase levels. Thus, the use of this enzyme determination, without isoenzyme separation, as a diagnostic test for the presence of acute myocardial infarction may be compromised by the intramuscular injection of lidocaine hydrochloride.
-
6 ADVERSE REACTIONS
The following clinically significant adverse reactions have been reported and described in the Warnings and Precautions section of the labeling:
Dose-Related Toxicity [see Warnings and Precautions (5.1)]
Methemoglobinemia [see Warnings and Precautions (5.2)]
Chondrolysis with Intra-Articular Infusion [see Warnings and Precautions (5.4)]
Severe, Persistent Hypertension, Cerebrovascular Accidents, and Bradycardia Due to Drug Interactions [see Warnings and Precautions (5.5)]
Allergic-Type Reactions [see Warnings and Precautions (5.6)]
Systemic Toxicities with Unintended Intravascular or Intrathecal Injection [see Warnings and Precautions (5.7)]
Respiratory Arrest Following Retrobulbar Block [see Warnings and Precautions (5.14)]
The following adverse reactions from voluntary reports or clinical studies have been reported with lidocaine or lidocaine and epinephrine. Because many of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse reactions to lidocaine hydrochloride are characteristic of those associated with other amide-type local anesthetic. A major cause of adverse reactions to this group of drugs is excessive plasma levels, which may be due to overdosage, unintentional intravascular injection, or slow metabolic degradation.
The most commonly encountered acute adverse reactions that demand immediate counter measures were related to the CNS and the cardiovascular system. These adverse reactions were generally dose-related and due to high plasma levels which may have resulted from overdosage, rapid absorption from the injection site, diminished tolerance, or from unintentional intravascular injection of the local anesthetic solution. In addition to systemic does-related toxicity, unintentional intrathecal injection of drug during the intended performance of caudal or lumbar epidural block or nerve blocks near the vertebral column (especially in the head and neck region) has resulted in underventilation or apnea (“Total or High Spinal”). Also, hypertension due to loss of sympathetic tone and respiratory paralysis or underventilation due to cephalad extension of the motor level of anesthesia have occurred. This has led to secondary cardiac arrest when untreated.
When used for dental injections, paresthesia of the lips, tongue, and oral tissues have been reported. Persistent paresthesia lasting weeks to months and, in some instances, lasting greater than one year, have also been reported.
Nervous System Disorders
Adverse reactions were characterized by excitation and/or depression of the central nervous system and included lightheadedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest.
The incidences of adverse reactions associated with the use of local anesthetics may be related to the total dose of local anesthetic administered and are also dependent upon the particular drug used, the route of administration and the physical status of the patient. In a prospective review of 10,440 patients who received lidocaine hydrochloride for spinal anesthesia, the incidences of adverse reactions were reported to be about 3 percent each for positional headaches, hypotension and backache; 2 percent for shivering; and less than 1 percent each for peripheral nerve symptoms, nausea, respiratory inadequacy and double vision.
Persistent motor, sensory and/or autonomic (sphincter control) deficit of some lower spinal segments with slow recovery (several months) or incomplete recovery have been reported in rare instances when caudal or lumbar epidural block has been attempted. Backache and headache have also been noted following use of these anesthetic procedures.
There have been reported cases of permanent injury to extraocular muscles requiring surgical repair following retrobulbar administration.
Neurologic effects following other procedures or routes of administration have included persistent anesthesia, paresthesia, weakness, paralysis, all with slow, incomplete, or no recovery.
Convulsions:Incidence varied with the procedure used and the total dose administered. The incidences of adverse neurologic reactions associated with the use of local anesthetics may be related to the total dose of local anesthetic administered and are also dependent upon the particular drug used, the route of administration, and the physical status of the patient.
Cardiac Disorders:High doses or unintentional intravascular injection have led to high plasma levels and related depression of the myocardium, decreased cardiac output, heartblock, hypotension, bradycardia, ventricular arrhythmias, including ventricular tachycardia and ventricular fibrillation, and cardiac arrest [see Warnings and Precautions (5.9)].
Immune System Disorders
Allergic reactions are characterized by cutaneous lesions, urticaria, edema or anaphylactoid reactions. Allergic reactions may occur as a result of sensitivity either to local anesthetic agents or to the methylparaben used as a preservative in the multiple dose vials. [see Warnings and Precautions (5.6)].
There have been no reports of cross sensitivity between lidocaine hydrochloride and procainamide or between lidocaine hydrochloride and quinidine.
Hematologic
Methemoglobinemia [See Warnings and Precautions (5.2)]. -
7 DRUG INTERACTIONS
7.1 Local Anesthetics
The toxic effects of local anesthetics are additive. If coadministration of other local anesthetics with lidocaine hydrochloride cannot be avoided, monitor patients for neurologic and cardiovascular effects related to local anesthetic systemic toxicity [see Warnings and Precautions (5.1)].
7.2 Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
The administration of lidocaine hydrochloride to patients receiving monoamine oxidase inhibitors or tricyclic antidepressants may produce severe, prolonged hypertension. Concurrent use of these agents should generally be avoided. In situation when concurrent therapy is necessary, careful monitoring of the patient’s hemodynamic status is essential [see Warnings and Precautions (5.5)].
7.3 Ergot-Type Oxytocic Drugs
Concurrent administration of vasopressor drugs (for the treatment of hypotension related to obstetric blocks) and ergot-type oxytocic drugs may cause severe, persistent hypertension or cerebrovascular accidents. Avoid use of lidocaine hydrochloride concomitantly with ergot-type oxytocic drugs [see Warnings and Precautions (5.5)].
7.4 Nonselective Beta-Adrenergic Antagonists
Administration of lidocaine hydrochloride in patients receiving nonselective beta-adrenergic antagonists may cause severe hypertension and bradycardia. Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful monitoring of the patient's blood pressure and heart rate is essential [see Warnings and Precautions (5.5)].
7.5 Drugs Associated with Methemoglobinemia
Patients that are administered local anesthetics may be at increased risk of developing methemoglobinemia when concurrently exposed to the following oxidizing agents:
Class
Examples
Nitrates/Nitrites
nitroglycerin, nitroprusside, nitric oxide, nitrous oxide
Local anesthetics
articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine
Antineoplastic agents
cyclophosphamide, flutamide, rasburicase, ifosfamide, hydroxyurea
Antibiotics
dapsone, sulphonamides, nitrofurantoin, para-aminosalicylic acid
Antimalarials
chloroquine, primaquine
Anticonvulsants
phenytoin, sodium valproate, phenobarbital
Other drugs
acetaminophen, metoclopramide, quinine, sulfasalazine
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available published data and decades of clinical use with lidocaine hydrochloride in pregnant women have not identified any drug- associated risk for major birth defects, miscarriage, or other adverse maternal or fetal outcomes. Local anesthetics may cause varying degrees of toxicity to the mother and fetus and adverse reactions include alterations of the central nervous system, peripheral vascular tone and cardiac function (see Clinical Considerations).
In a published animal reproduction study, pregnant rats administered lidocaine by continuous subcutaneous infusion at a dose approximately 9.6 times the maximum recommended human dose (MRHD) of 500 mg in Xylocaine during the period of organogenesis resulted in lower fetal body weights [ see Data].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. In the United States general population, the estimated background risks of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15%to 20%, respectively.
Clinical Considerations
Maternal adverse reactions
Maternal hypotension has resulted from regional anesthesia. Local anesthetics produce vasodilation by blocking sympathetic nerves. Therefore, during treatment of systemic toxicity, maternal hypotension or fetal bradycardia following regional block, the parturient should be maintained in the left lateral decubitus position if possible or manual displacement of the uterus off the great vessels be accomplished. Elevating the patient’s legs will also help prevent decreases in blood pressure. The fetal heart rate also should be monitored continuously, and electronic fetal monitoring is highly advisable.
Labor or delivery
Local anesthetics rapidly cross the placenta, and when used for epidural, paracervical, pudendal or caudal block anesthesia, can cause varying degrees of maternal, fetal and neonatal toxicity [see Clinical Pharmacology (12.3)]. The incidence and degree of toxicity depend upon the procedure performed, the type and amount of drug used, and the technique of drug administration. Adverse reactions in the parturient, fetus and neonate involve alterations of the central nervous system, peripheral vascular tone and cardiac function. However, dosage recommendations for spinal anesthesia are much lower than dosage recommendations for other major blocks.
Spinal anesthesia may alter the forces of parturition through changes in uterine contractility or maternal expulsive efforts. Spinal anesthesia has also been reported to prolong the second stage of labor by removing the parturient’s reflex urge to bear down or by interfering with motor function. The use of obstetrical anesthesia may increase the need for forceps assistance. The use of some local anesthetic drug products during labor and delivery may be followed by diminished muscle strength and tone for the first day or two of life.
Data
Animal Data
Reproduction studies have been performed in rats at doses up to 6.6 times the human dose and have revealed no evidence of harm to the fetus caused by lidocaine hydrochloride.
In a published study, lidocaine administered to pregnant rats by continuous subcutaneous infusion during the period of organogenesis at 100, 250, and 500 mg/kg/day, did not produce any structural abnormalities, but did result in lower fetal weights at 500 mg/kg/day dose (approximately 9.6 times the maximum recommended human dose [MRHD] of 500 mg lidocaine on a mg/m 2basis) in the absence of maternal toxicity.8.2 Lactation
Risk Summary
Published data report the presence of lidocaine and its metabolites in human milk in low amounts, along with poor oral bioavailability. There are no data on the effect of lidocaine on the breastfed infant or the effect on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for lidocaine hydrochloride injection and any potential adverse effects on the breastfed child from lidocaine hydrochloride injection or from the underlying maternal condition.8.4 Pediatric Use
Dosages in children should be reduced, commensurate with age, body weight and physical condition [see Dosage and Administration (2.6)].
8.5 Geriatric Use
Elderly patients should be given reduced doses commensurate with their age and physical condition. [see Dosage and Administration (2.6)].
8.6 Hepatic Impairment
Amide-type local anesthetics such as lidocaine are metabolized by the liver. Patients with severe hepatic impairment, because of their inability to metabolize local anesthetics normally, are at greater risk of developing toxic plasma concentrations and potentially local anesthetic systemic toxicity. Therefore, consider reduced dosing and increased monitoring for local anesthetic systemic toxicity in patients with hepatic impairment treated with lidocaine hydrochloride injection, especially with repeat doses [see Warnings and Precautions (5.8)]
-
10 OVERDOSAGE
Clinical Presentation
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics or to unintended subarachnoid injection of local anesthetic solution [see Warnings and Precautions (5.1)and see Adverse Reactions (6)].
Management
The first consideration is prevention, best accomplished by careful and constant monitoring of cardiovascular and respiratory vital signs and the patient’s state of consciousness after each local anesthetic injection. At the first sign of change, oxygen should be administered.
The first step in the management of convulsions, as well as underventilation or apnea due to unintended subarachnoid injection of drug solution, consists of immediate attention to the maintenance of a patent airway and assisted or controlled ventilation with oxygen and a delivery system capable of permitting immediate positive airway pressure by mask. Immediately after the institution of these ventilatory measures, the adequacy of the circulation should be evaluated, keeping in mind that drugs used to treat convulsions sometimes depress the circulation when administered intravenously. Should convulsions persist despite adequate respiratory support, and if the status of the circulation permits, a benzodiazepine (such as diazepam) may be administered intravenously. The clinician should be familiar, prior to the use of local anesthetics, with these anticonvulsant drugs. Supportive treatment of circulatory depression may require administration of intravenous fluids and, when appropriate, a vasopressor as directed by the clinical situation (e.g., ephedrine).
If not treated immediately, both convulsions and cardiovascular depression can result in hypoxia, acidosis, bradycardia, arrhythmias and cardiac arrest. Underventilation or apnea due to unintentional subarachnoid injection of local anesthetic solution may produce these same signs and also lead to cardiac arrest if ventilatory support is not instituted. If cardiac arrest should occur, standard cardiopulmonary resuscitative measures should be instituted.
Endotracheal intubation, employing drugs and techniques familiar to the clinician, may be indicated, after initial administration of oxygen by mask, if difficulty is encountered in the maintenance of a patent airway or if prolonged ventilatory support (assisted or controlled) is indicated.
Dialysis is of negligible value in the treatment of acute overdosage with lidocaine hydrochloride. -
11 DESCRIPTION
Lidocaine hydrochloride injection contains lidocaine hydrochloride, an amide local anesthetic, as the active pharmaceutical ingredient. The route of administration for lidocaine hydrochloride is by injection, for infiltration, nerve block, use. Multiple dose vials contain methylparaben and they should not be used for caudal and lumbar epidural blocks.
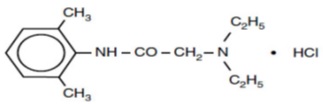
Lidocaine hydrochloride, is chemically designated as acetamide, 2-(diethylamino)-N-(2,6-dimethylphenyl)-, monohydrochloride and has the molecular weight of 270.8 g/mol. Lidocaine hydrochloride molecular formula is C 14H 22N 2O HCl, and has the following structural formula:
Lidocaine hydrochloride injection in multiple dose vials is a sterile, nonpyrogenic, isotonic, clear, colorless solution containing lidocaine hydrochloride and sodium chloride. Each mL contains 1 mg methylparaben as an antiseptic preservative. The pH of these solutions is adjusted to approximately 6.5 (5.0 to 7.0) with sodium hydroxide and hydrochloric acid.
Ingredients
Strength
1%
2%
Amount (Per mL)
Amount (Per mL)
Lidocaine Hydrochloride (Anhydrous)
10 mg £
20 mg µ
Sodium Chloride
7 mg
6 mg
Methylparaben
1 mg
1 mg
Sodium Hydroxide
Added for pH Adjustment to approximately 6.5 (5.0 to 7.0)
Hydrochloric Acid
£ Quantity is equivalent to 10.66 mg/mL Lidocaine Hydrochloride, USP (Monohydrate).
μ Quantity is equivalent to 21.33 mg/mL Lidocaine Hydrochloride, USP (Monohydrate).
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Lidocaine hydrochloride stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses thereby effecting local anesthetic action.
12.2 Pharmacodynamics
Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. With central neural blockade these changes may be attributable to block of autonomic fibers, a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system, and/or the beta-adrenergic receptor stimulating action of epinephrine when present. The net effect is normally a modest hypotension when the recommended dosages are not exceeded.
Factors such as acidosis and the use of CNS stimulants and depressants affect the CNS levels of lidocaine hydrochloride required to produce overt systemic effects. Objective adverse manifestations become increasingly apparent with increasing venous plasma levels above 6 mcg free base per mL.12.3 Pharmacokinetics
Systemic plasma levels of lidocaine following lidocaine hydrochloride do not correlate with local efficacy.
Absorption
Information derived from diverse formulations, concentrations and usages reveals that lidocaine hydrochloride is completely absorbed following parenteral administration, its rate of absorption depending, for example, upon various factors such as the site of administration and the presence or absence of a vasoconstrictor agent. Except for intravascular administration, the highest blood levels are obtained following intercostal nerve block and the lowest after subcutaneous administration.
Distribution
The plasma binding of lidocaine hydrochloride is dependent on drug concentration, and the fraction bound decreases with increasing concentration. At concentrations of 1 to 4 mcg of free base per mL 60 to 80 percent of lidocaine hydrochloride is protein bound. Binding is also dependent on the plasma concentration of the alpha-1-acid glycoprotein.
Lidocaine hydrochloride crosses the blood-brain and placental barriers, presumably by passive diffusion.
Elimination
The elimination half-life of lidocaine hydrochloride following an intravenous bolus injection is typically 1.5 to 2 hours.
Metabolism
Lidocaine hydrochloride is metabolized rapidly by the liver, and biotransformation includes oxidative N-dealkylation, ring hydroxylation, cleavage of the amide linkage, and conjugation. N-dealkylation, a major pathway of biotransformation, yields the metabolites monoethylglycinexylidide and glycinexylidide. The pharmacological/toxicological actions of these metabolites are similar to, but less potent than, those of lidocaine hydrochloride.
Excretion
Approximately 90% of lidocaine hydrochloride administered is excreted in the form of various metabolites, and less than 10% is excreted unchanged by the kidneys. The primary metabolite in urine is a conjugate of 4-hydroxy-2,6-dimethylaniline.
Specific Populations
Patients with Hepatic Impairment
Because of the rapid rate at which lidocaine hydrochloride is metabolized, any condition that affects liver function may alter lidocaine HCl kinetics. The half-life may be prolonged two-fold or more in patients with liver dysfunction.
Patients with Renal Impairment
Renal dysfunction does not affect lidocaine hydrochloride kinetics but may increase the accumulation of metabolites. -
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Studies of lidocaine hydrochloride in animals to evaluate the carcinogenic potential have not been conducted.
Mutagenesis
Studies of lidocaine hydrochloride in animals to evaluate the mutagenic potential have not been conducted.
Impairment of Fertility
In a published study, female Sprague-Dawley rats were treated subcutaneously with lidocaine via osmotic pumps starting two weeks prior to mating, and reproductive effects were assessed. Rats dosed up to the high dose of 500 mg/kg/day (approximately 45 times the MRDD on a mg/m 2basis) showed no effects on copulatory rate, pregnancy rate, numbers of corpora lutea, or implantations. -
16 HOW SUPPLIED/STORAGE AND HANDLING
Storage:Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Protect from light.
Lidocaine Hydrochloride Injection, USP is a sterile, nonpyrogenic, clear, colorless, isotonic solution and is supplied as follows:
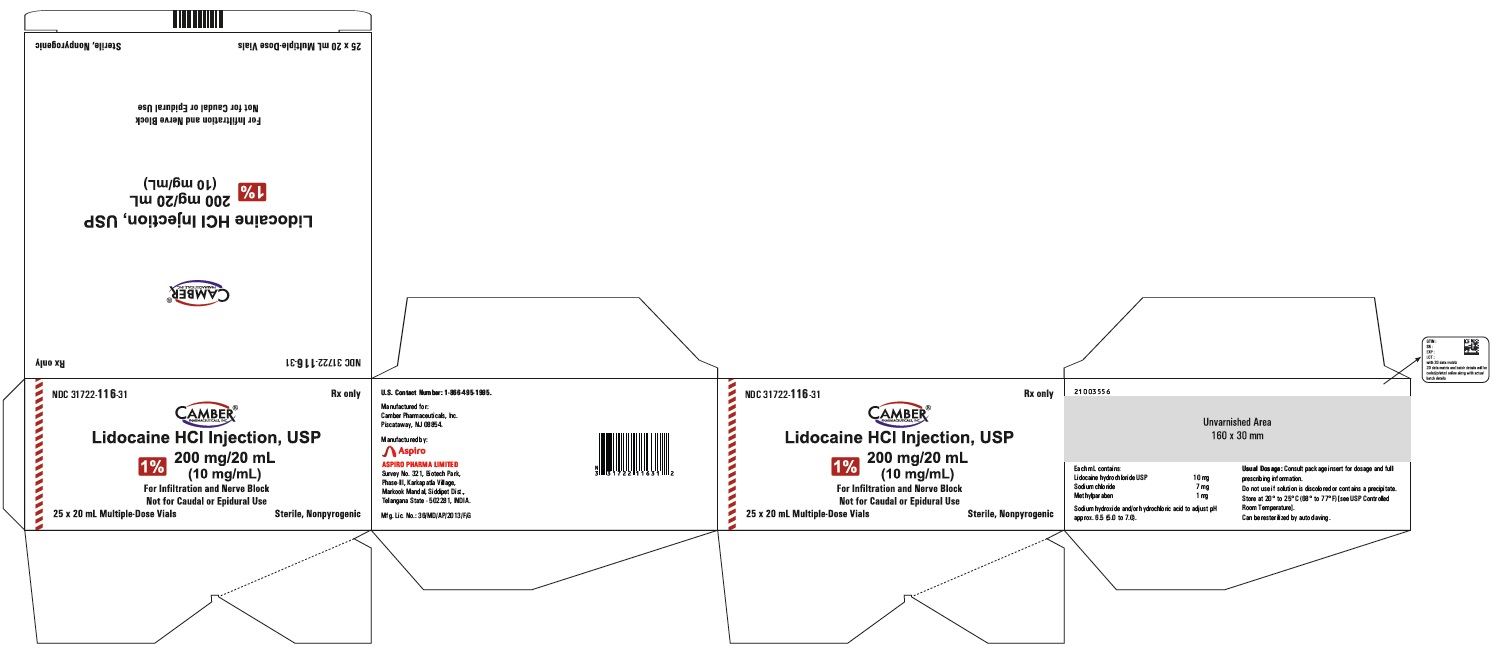
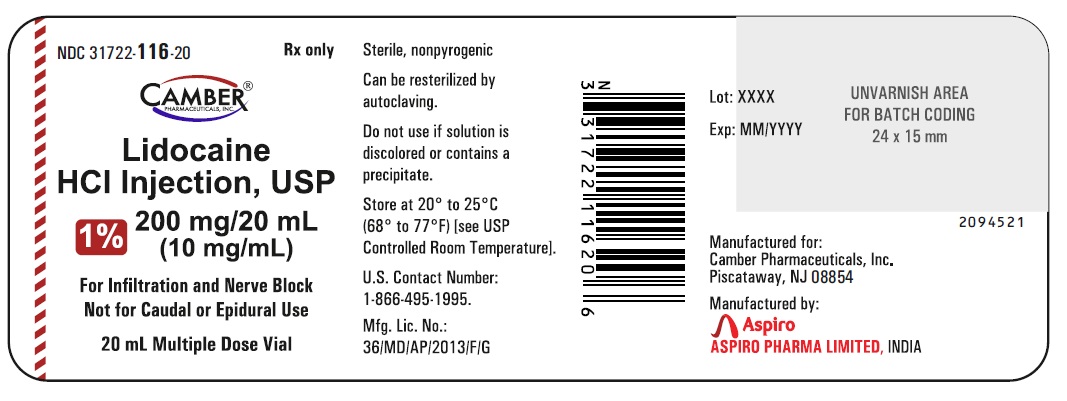
Lidocaine Hydrochloride Injection USP, 1% (10 mg/mL):
10 x 20 mL Multiple-Dose Vials NDC: 31722-116-32
25 x 20 mL Multiple-Dose Vials NDC: 31722-116-31
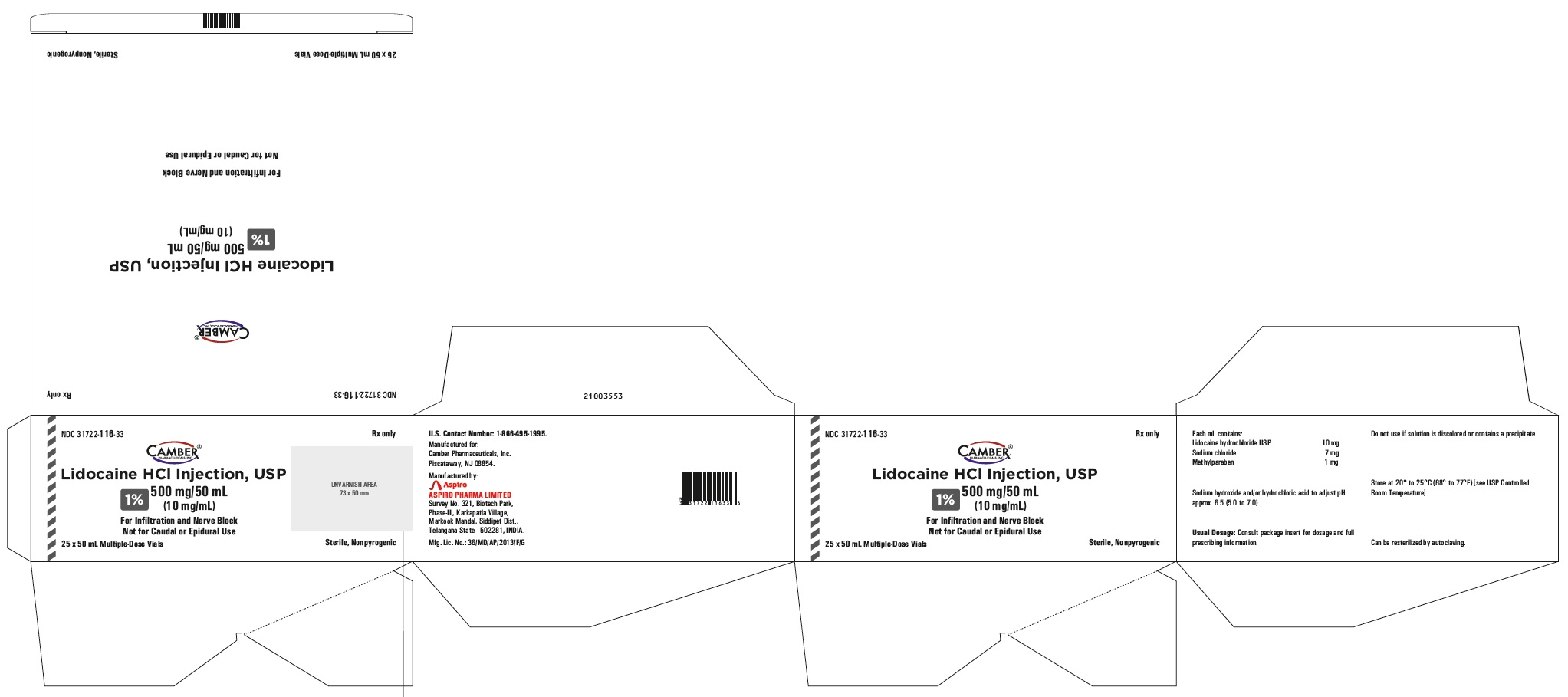
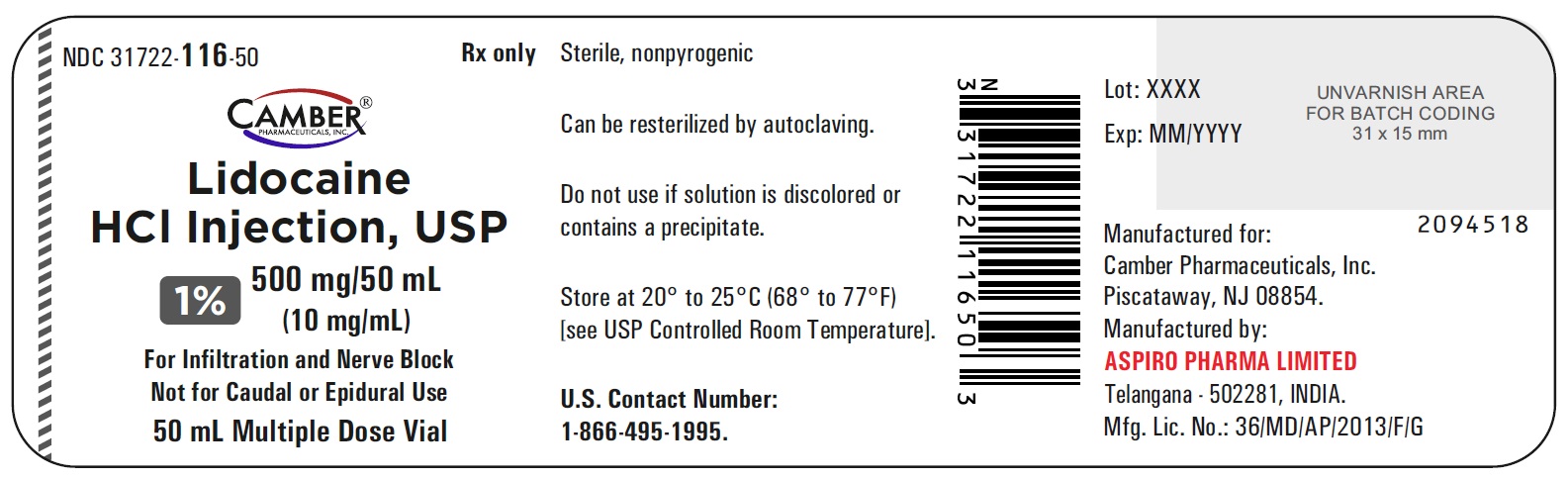
10 x 50 mL Multiple-Dose Vials NDC: 31722-116-34
25 x 50 mL Multiple-Dose Vials NDC: 31722-116-33
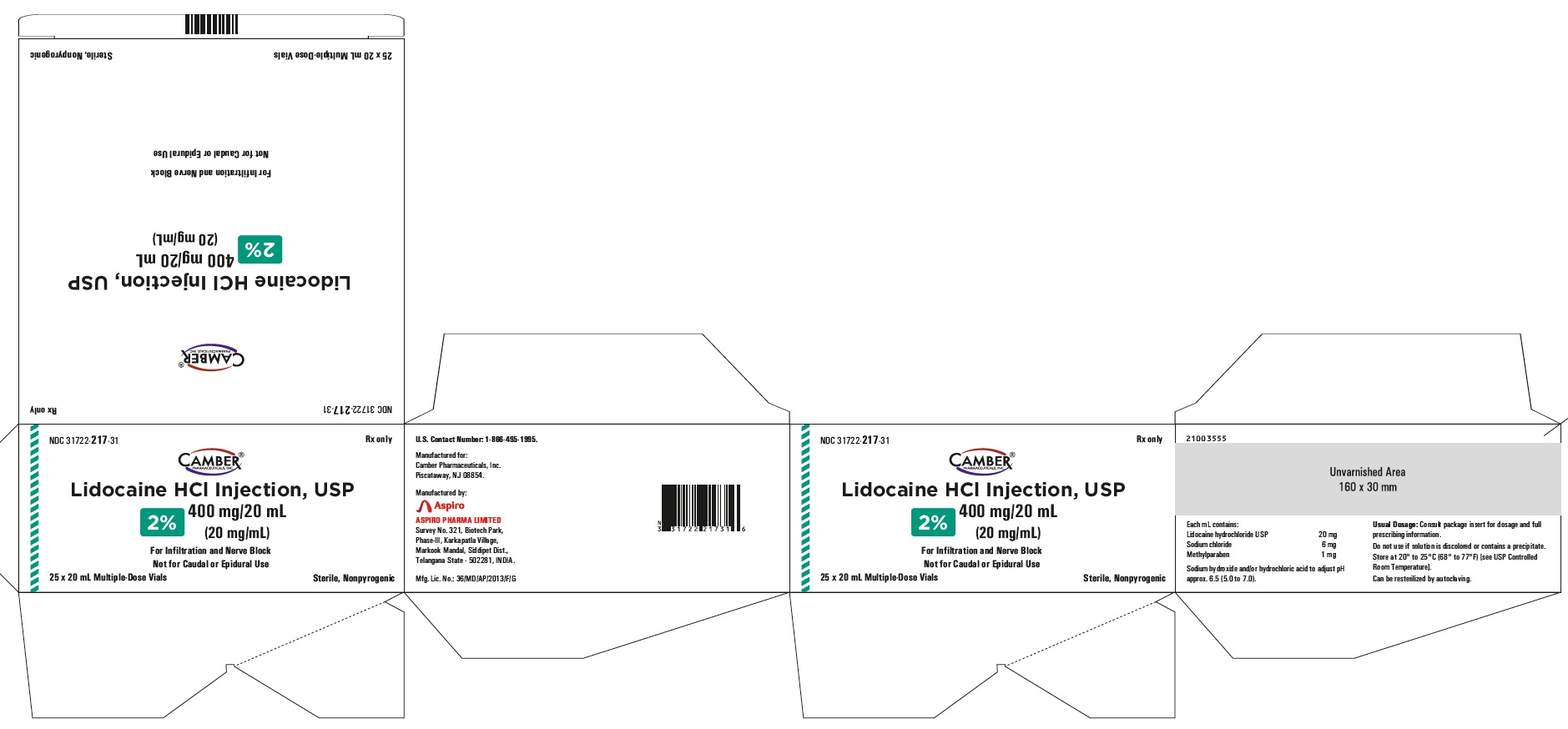
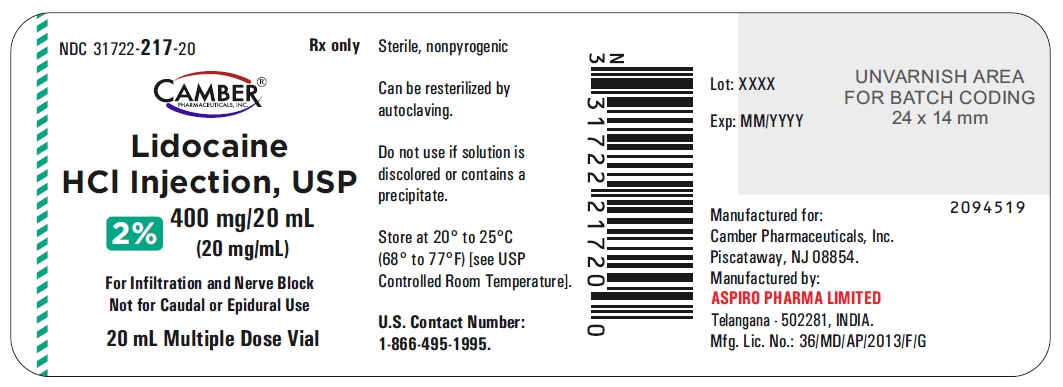
Lidocaine Hydrochloride Injection USP, 2% (20 mg/mL):
25 x 20 mL Multiple-Dose Vials NDC: 31722-217-31
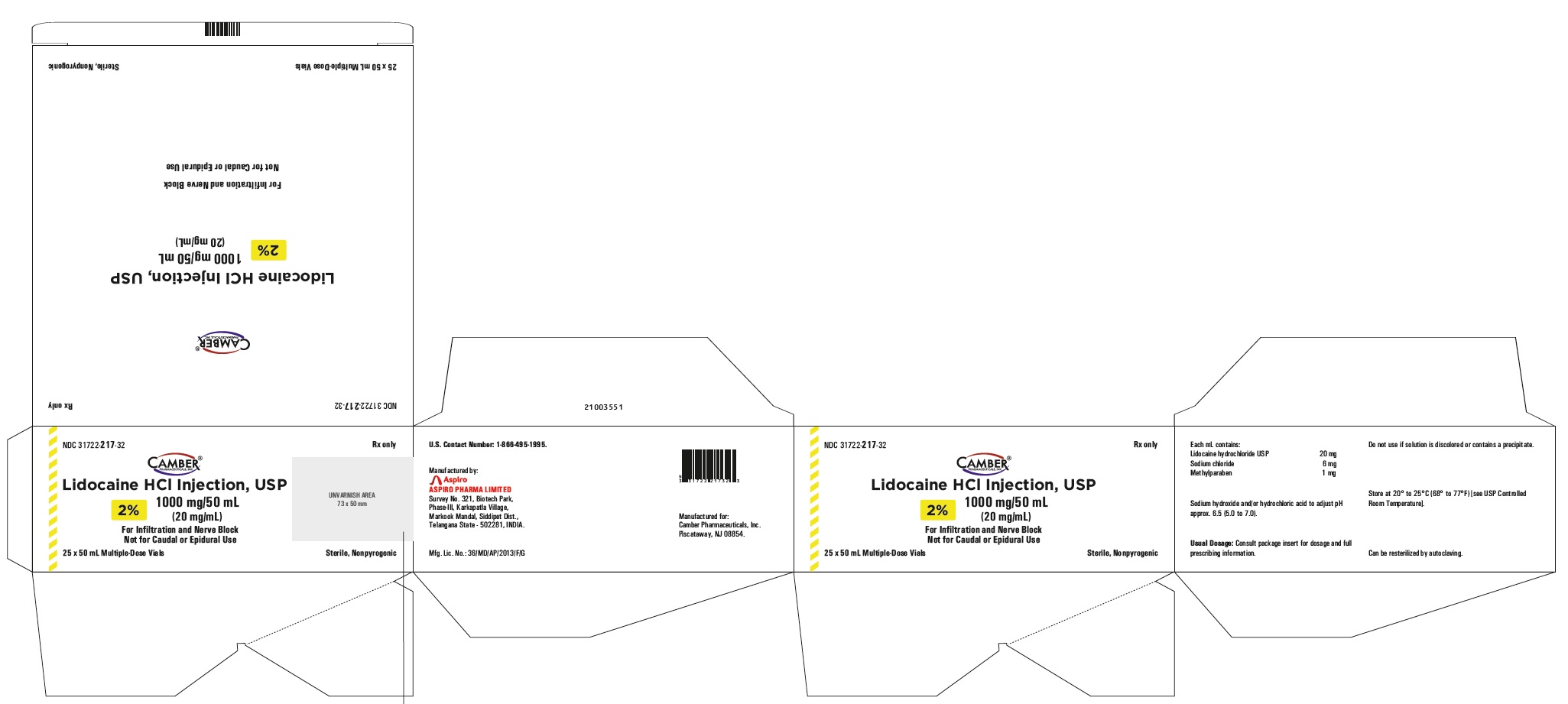
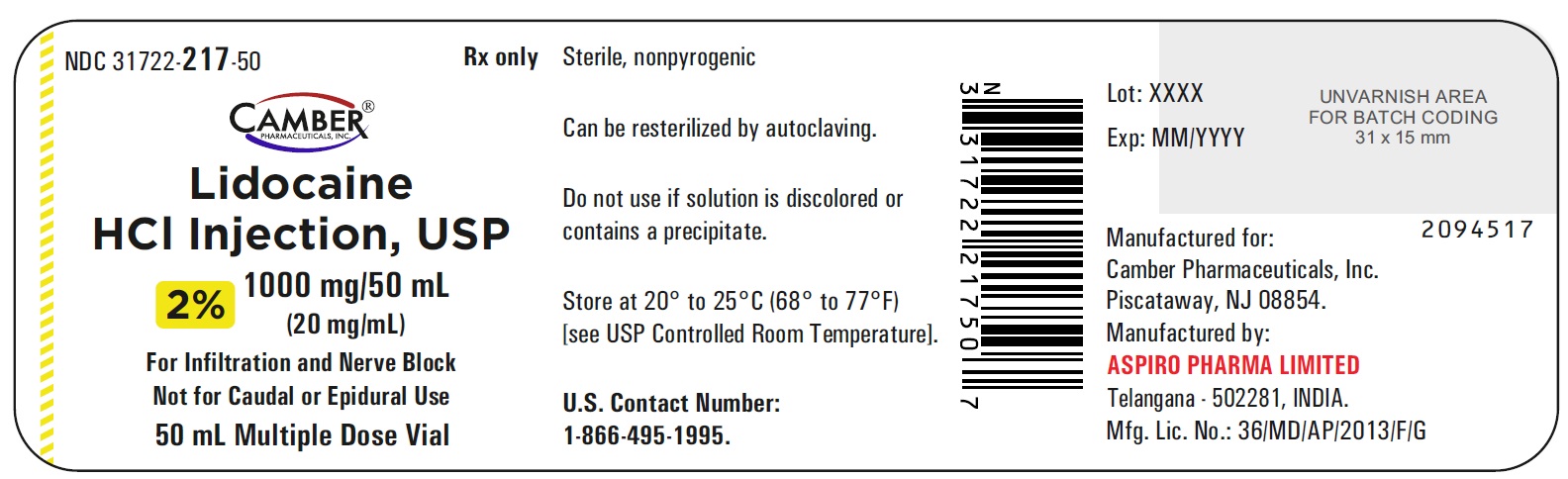
10 x 50 mL Multiple-Dose Vials NDC: 31722-217-33
25 x 50 mL Multiple-Dose Vials NDC: 31722-217-32 -
17 PATIENT COUNSELING INFORMATION
17.1 Allergic Type Reactions
Assess if the patient has had allergic-type reactions to amide-type local anesthetics or to other formulation ingredients, such as the antimicrobial preservative methylparaben contained in multiple-dose vials [see Contraindications (4), Warnings and Precautions (5.6), Adverse Reactions (6)].
17.3 Methemoglobinemia
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue [see Warnings and Precautions (5.2)].

Manufactured for:
Camber Pharmaceuticals, Inc.,
Piscataway, NJ 08854Manufactured by:

Aspiro Pharma Limited
Survey No. 321, Biotech Park, Phase – III
Karkapatla Village, Markook (Mandal)
Siddipet, Telangana-502281, India.
Revised: 04/2025 - PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
LIDOCAINE HYDROCHLORIDE
lidocaine hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 31722-116 Route of Administration INFILTRATION, PERINEURAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LIDOCAINE HYDROCHLORIDE ANHYDROUS (UNII: EC2CNF7XFP) (LIDOCAINE - UNII:98PI200987) LIDOCAINE HYDROCHLORIDE ANHYDROUS 10 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 7 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) METHYLPARABEN (UNII: A2I8C7HI9T) 1 mg in 1 mL SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 31722-116-31 25 in 1 CARTON 11/08/2021 1 NDC: 31722-116-20 20 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 2 NDC: 31722-116-32 10 in 1 CARTON 12/13/2023 2 NDC: 31722-116-20 20 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 3 NDC: 31722-116-34 10 in 1 CARTON 12/13/2023 3 NDC: 31722-116-50 50 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 4 NDC: 31722-116-33 25 in 1 CARTON 12/13/2023 4 NDC: 31722-116-50 50 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214336 11/08/2021 LIDOCAINE HYDROCHLORIDE
lidocaine hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 31722-217 Route of Administration INFILTRATION, PERINEURAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength LIDOCAINE HYDROCHLORIDE ANHYDROUS (UNII: EC2CNF7XFP) (LIDOCAINE - UNII:98PI200987) LIDOCAINE HYDROCHLORIDE ANHYDROUS 20 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 6 mg in 1 mL HYDROCHLORIC ACID (UNII: QTT17582CB) WATER (UNII: 059QF0KO0R) METHYLPARABEN (UNII: A2I8C7HI9T) 1 mg in 1 mL SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 31722-217-31 25 in 1 CARTON 12/13/2023 1 NDC: 31722-217-20 20 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 2 NDC: 31722-217-33 10 in 1 CARTON 12/13/2023 2 NDC: 31722-217-50 50 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product 3 NDC: 31722-217-32 25 in 1 CARTON 12/13/2023 3 NDC: 31722-217-50 50 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA214336 11/08/2021 Labeler - Camber Pharmaceuticals, Inc. (826774775) Establishment Name Address ID/FEI Business Operations Aspiro Pharma Limited 872341023 manufacture(31722-116, 31722-217)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.