CYCLOSPORINE by Lupin Pharmaceuticals, Inc. CYCLOSPORINE emulsion
CYCLOSPORINE by
Drug Labeling and Warnings
CYCLOSPORINE by is a Prescription medication manufactured, distributed, or labeled by Lupin Pharmaceuticals, Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CYCLOSPORINE OPHTHALMIC EMULSION, 0.05% safely and effectively. See full prescribing information for CYCLOSPORINE OPHTHALMIC EMULSION, 0.05%.
CYCLOSPORINE OPHTHALMIC EMULSION, 0.05%
For topical ophthalmic use
Initial U.S. Approval: 1983
INDICATIONS AND USAGE
Cyclosporine ophthalmic emulsion, 0.05% is a calcineurin inhibitor immunosuppressant indicated to increase tear production in patients whose tear production is presumed to be suppressed due to ocular inflammation associated with keratoconjunctivitis sicca. Increased tear production was not seen in patients currently taking topical anti-inflammatory drugs or using punctal plugs. (1)
DOSAGE AND ADMINISTRATION
Instill one drop of cyclosporine ophthalmic emulsion, 0.05% twice a day in each eye approximately 12 hours apart. (2)
DOSAGE FORMS AND STRENGTHS
Cyclosporine ophthalmic emulsion 0.5 mg/mL (3)
CONTRAINDICATIONS
- Hypersensitivity (4)
WARNINGS AND PRECAUTIONS
- To avoid the potential for eye injury and contamination, be careful not to touch the vial tip to your eye or other surfaces. (5.1)
ADVERSE REACTIONS
The most common adverse reaction following the use of cyclosporine ophthalmic emulsion, 0.05% was ocular burning (17%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Lupin Pharmaceuticals Inc., at 1-800-399-2561 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.See 17 for PATIENT COUNSELING INFORMATION.
Revised: 9/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Potential for Eye Injury and Contamination
5.2 Use with Contact Lenses
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-marketing Experience
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- * Sections or subsections omitted from the full prescribing information are not listed.
-
1
INDICATIONS AND USAGE
Cyclosporine ophthalmic emulsion, 0.05% is indicated to increase tear production in patients whose tear production is presumed to be suppressed due to ocular inflammation associated with keratoconjunctivitis sicca. Increased tear production was not seen in patients currently taking topical anti-inflammatory drugs or using punctal plugs.
-
2
DOSAGE AND ADMINISTRATION
Invert the unit dose vial a few times to obtain a uniform, white, opaque emulsion before using. Instill one drop of cyclosporine ophthalmic emulsion, 0.05% twice a day in each eye approximately 12 hours apart. Cyclosporine ophthalmic emulsion, 0.05% can be used concomitantly with lubricant eye drops, allowing a 15-minute interval between products. Discard vial immediately after use.
- 3 DOSAGE FORMS AND STRENGTHS
- 4 CONTRAINDICATIONS
-
5
WARNINGS AND PRECAUTIONS
5.1 Potential for Eye Injury and Contamination
Be careful not to touch the vial tip to your eye or other surfaces to avoid potential for eye injury and contamination.
5.2 Use with Contact Lenses
Cyclosporine ophthalmic emulsion, 0.05% should not be administered while wearing contact lenses. Patients with decreased tear production typically should not wear contact lenses. If contact lenses are worn, they should be removed prior to the administration of the emulsion. Lenses may be reinserted 15 minutes following administration of cyclosporine ophthalmic emulsion, 0.05%.
-
6
ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling:
- Potential for Eye Injury and Contamination [see Warnings and Precautions (5.1)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials, the most common adverse reaction following the use of cyclosporine ophthalmic emulsion, 0.05% was ocular burning (17%).
Other reactions reported in 1% to 5% of patients included conjunctival hyperemia, discharge, epiphora, eye pain, foreign body sensation, pruritus, stinging, and visual disturbance (most often blurring).
6.2 Post-marketing Experience
The following adverse reactions have been identified during post approval use of cyclosporine ophthalmic emulsion, 0.05%. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Reported reactions have included: hypersensitivity (including eye swelling, urticaria, rare cases of severe angioedema, face swelling, tongue swelling, pharyngeal edema, and dyspnea); and superficial injury of the eye (from the vial tip touching the eye during administration).
-
8
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Clinical administration of cyclosporine ophthalmic emulsion, 0.05% is not detected systemically following topical ocular administration [see Clinical Pharmacology (12.3)], and maternal use is not expected to result in fetal exposure to the drug. Oral administration of cyclosporine to pregnant rats or rabbits did not produce teratogenicity at clinically relevant doses [see Data].
Data
Animal Data
At maternally toxic doses (30 mg/kg/day in rats and 100 mg/kg/day in rabbits), cyclosporine oral solution (USP) was teratogenic as indicated by increased pre- and postnatal mortality, reduced fetal weight and skeletal retardations. These doses (normalized to body surface area) are 5,000 and 32,000 times greater, respectively, than the daily recommended human dose of one drop (approximately 28 mcL) of cyclosporine ophthalmic emulsion, 0.05% twice daily into each eye of a 60 kg person (0.001 mg/kg/day), assuming that the entire dose is absorbed. No evidence of embryofetal toxicity was observed in rats or rabbits receiving cyclosporine during organogenesis at oral doses up to 17 mg/kg/day or 30 mg/kg/day, respectively. These doses in rats and rabbits are approximately 3,000 and 10,000 times greater, respectively, than the daily recommended human dose.
An oral dose of 45 mg/kg/day cyclosporine administered to rats from Day 15 of pregnancy until Day 21 postpartum produced maternal toxicity and an increase in postnatal mortality in offspring. This dose is 7,000 times greater than the daily recommended human dose. No adverse effects in dams or offspring were observed at oral doses up to 15 mg/kg/day (2,000 times greater than the daily recommended human dose).
8.2 Lactation
Risk Summary
Cyclosporine is known to appear in human milk following systemic administration, but its presence in human milk following topical treatment has not been investigated. Although blood concentrations are undetectable following topical administration of cyclosporine ophthalmic emulsion, 0.05% [see Clinical Pharmacology (12.3)], caution should be exercised when cyclosporine ophthalmic emulsion, 0.05% is administered to a nursing woman. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for cyclosporine ophthalmic emulsion, 0.05% and any potential adverse effects on the breast-fed child from cyclosporine.
-
11
DESCRIPTION
Cyclosporine ophthalmic emulsion, 0.05% contains a topical calcineurin inhibitor immunosuppressant with anti-inflammatory effects. Cyclosporine’s chemical name is Cyclo[[E-(2S,3R,4R)-3-hydroxy-4-methyl-2-(methylamino)-6-octenoyl]-L-2-aminobutyryl-N-methylglycyl-N-methyl-L-leucyl-L-valyl-N-methyl-L-leucyl-L-alanyl-D-alanyl-N-methyl-L-leucyl-N-methyl-L-leucyl-N-methyl-L-valyl] and it has the following structure:
Structural Formula
![The following structure for Cyclosporine ophthalmic emulsion, 0.05% contains a topical calcineurin inhibitor immunosuppressant with anti-inflammatory effects. Cyclosporine’s chemical name is Cyclo[[E-(2S,3R,4R)-3-hydroxy-4-methyl-2-(methylamino)-6-octenoyl]-L-2-aminobutyryl-N-methylglycyl-N-methyl-L-leucyl-L-valyl-N-methyl-L-leucyl-L-alanyl-D-alanyl-N-methyl-L-leucyl-N-methyl-L-leucyl-N-methyl-L-valyl]](https://fda.report/DailyMed/9aca2026-af86-4e97-925e-c202b87c46ac/cyclosporine-ophthalmic-emulsion---lupin-01.jpg)
Formula: C62H111N11O12 Mol. Wt.: 1202.6
Cyclosporine is a fine white powder. Cyclosporine ophthalmic emulsion, 0.05% appears as a white opaque to slightly translucent homogeneous emulsion. It has an osmolality of 230 to 320 mOsmol/kg and a pH of 6.5-8.0. Each mL of cyclosporine ophthalmic emulsion contains: Active: cyclosporine 0.05%. Inactives: glycerin; castor oil; polysorbate 80; carbomer copolymer type A; purified water; and sodium hydroxide to adjust pH.
-
12
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Cyclosporine is an immunosuppressive agent when administered systemically.
In patients whose tear production is presumed to be suppressed due to ocular inflammation associated with keratoconjunctivitis sicca, cyclosporine emulsion is thought to act as a partial immunomodulator. The exact mechanism of action is not known.
12.3 Pharmacokinetics
Blood cyclosporine A concentrations were measured using a specific high pressure liquid chromatography-mass spectrometry assay. Blood concentrations of cyclosporine, in all the samples collected, after topical administration of cyclosporine ophthalmic emulsion, 0.05%, twice daily, in humans for up to 12 months, were below the quantitation limit of 0.1 ng/mL. There was no detectable drug accumulation in blood during 12 months of treatment with cyclosporine ophthalmic emulsion, 0.05%.
-
13
NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Systemic carcinogenicity studies were conducted in male and female mice and rats. In the 78-week oral (diet) mouse study, at doses of 1, 4, and 16 mg/kg/day, evidence of a statistically significant trend was found for lymphocytic lymphomas in females, and the incidence of hepatocellular carcinomas in mid-dose males significantly exceeded the control value.
In the 24-month oral (diet) rat study, conducted at 0.5, 2, and 8 mg/kg/day, pancreatic islet cell adenomas significantly exceeded the control rate in the low dose level. The hepatocellular carcinomas and pancreatic islet cell adenomas were not dose related. The low doses in mice and rats are approximately 80 times greater (normalized to body surface area) than the daily recommended human dose of one drop (approximately 28 mcL) of 0.05% cyclosporine ophthalmic emulsion twice daily into each eye of a 60 kg person (0.001 mg/kg/day), assuming that the entire dose is absorbed.
Mutagenesis
Cyclosporine has not been found to be mutagenic/genotoxic in the Ames Test, the V79-HGPRT Test, the micronucleus test in mice and Chinese hamsters, the chromosome-aberration tests in Chinese hamster bone-marrow, the mouse dominant lethal assay, and the DNA-repair test in sperm from treated mice. A study analyzing sister chromatid exchange (SCE) induction by cyclosporine using human lymphocytes in vitro gave indication of a positive effect (i.e., induction of SCE).
Impairment of Fertility
No impairment in fertility was demonstrated in studies in male and female rats receiving oral doses of cyclosporine up to 15 mg/kg/day (approximately 2,000 times the human daily dose of 0.001 mg/kg/day normalized to body surface area) for 9 weeks (male) and 2 weeks (female) prior to mating.
-
14
CLINICAL STUDIES
Four multicenter, randomized, adequate and well-controlled clinical studies were performed in approximately 1,200 patients with moderate to severe keratoconjunctivitis sicca. Cyclosporine ophthalmic emulsion, 0.05% demonstrated statistically significant increases in Schirmer wetting of 10 mm versus vehicle at six months in patients whose tear production was presumed to be suppressed due to ocular inflammation. This effect was seen in approximately 15% of cyclosporine ophthalmic emulsion, 0.05%-treated patients versus approximately 5% of vehicle-treated patients. Increased tear production was not seen in patients currently taking topical anti-inflammatory drugs or using punctal plugs.
No increase in bacterial or fungal ocular infections was reported following administration of cyclosporine ophthalmic emulsion, 0.05%.
-
16
HOW SUPPLIED/STORAGE AND HANDLING
Cyclosporine ophthalmic emulsion, 0.05% is packaged in sterile, preservative-free single-use vials. Each vial contains 0.4 mL fill in a 0.9 mL LDPE vial; 30 or 60 vials are packaged in a polypropylene tray with an aluminum peelable lid. The entire contents of each tray (30 vials or 60 vials) must be dispensed intact.
30 Vials 0.4 mL each - NDC: 68180-214-30
60 Vials 0.4 mL each - NDC: 68180-214-60
Storage: Store at 15°-25 °C (59°-77 °F).
-
17
PATIENT COUNSELING INFORMATION
Handling the Container
Advise patients to not allow the tip of the vial to touch the eye or any surface, as this may contaminate the emulsion. Advise patients to not touch the vial tip to their eye to avoid the potential for injury to the eye [see Warnings and Precautions (5.1)].
Use with Contact Lenses
Cyclosporine ophthalmic emulsion, 0.05% should not be administered while wearing contact lenses. Patients with decreased tear production typically should not wear contact lenses. Advise patients that if contact lenses are worn, they should be removed prior to the administration of the emulsion. Lenses may be reinserted 15 minutes following administration of cyclosporine ophthalmic emulsion, 0.05% [see Warnings and Precautions (5.2)].
Administration
Advise patients that the emulsion from one individual single-use vial is to be used immediately after opening for administration to one or both eyes, and the remaining contents should be discarded immediately after administration.
Manufactured for:
Lupin Pharmaceuticals, Inc.
Naples, FL 34108
United StatesManufactured by:
Allergan Sales, LLC,
Waco, TX 76712
USA© 2024 AbbVie. All rights reserved.
v2.0USPI0214AG
-
PRINCIPAL DISPLAY PANEL
NDC: 68180-214-30
Cyclosporine Ophthalmic Emulsion
0.05%
Preservative-Free
Sterile
30 Single-Use Vials
(0.4 mL each)
Rx only
LUPIN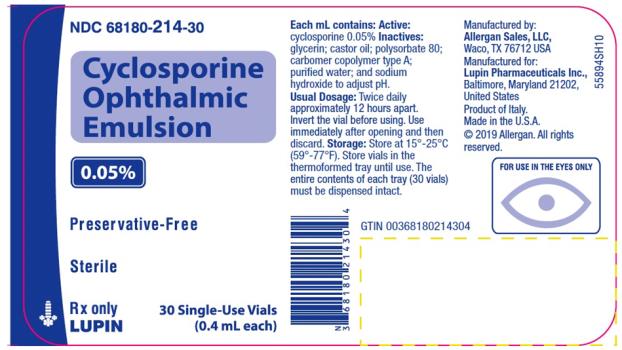
-
PRINCIPAL DISPLAY PANEL
NDC: 68180-214-60
Cyclosporine Ophthalmic Emulsion
0.05%
Preservative-Free
Sterile
One Month Supply
60 Single-Use Vials
(0.4 mL each)
Rx only
LUPIN
-
INGREDIENTS AND APPEARANCE
CYCLOSPORINE
cyclosporine emulsionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 68180-214 Route of Administration OPHTHALMIC Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CYCLOSPORINE (UNII: 83HN0GTJ6D) (CYCLOSPORINE - UNII:83HN0GTJ6D) CYCLOSPORINE 0.5 mg in 1 mL Inactive Ingredients Ingredient Name Strength GLYCERIN (UNII: PDC6A3C0OX) CASTOR OIL (UNII: D5340Y2I9G) POLYSORBATE 80 (UNII: 6OZP39ZG8H) CARBOMER COPOLYMER TYPE A (UNII: 71DD5V995L) WATER (UNII: 059QF0KO0R) SODIUM HYDROXIDE (UNII: 55X04QC32I) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 68180-214-30 30 in 1 TRAY 05/11/2022 1 0.4 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product 2 NDC: 68180-214-60 60 in 1 TRAY 05/11/2022 2 0.4 mL in 1 VIAL, SINGLE-USE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA authorized generic NDA050790 05/11/2022 Labeler - Lupin Pharmaceuticals, Inc. (089153071)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.