PHENAZOPYRIDINE HCL tablet
Phenazopyridine HCl by
Drug Labeling and Warnings
Phenazopyridine HCl by is a Prescription medication manufactured, distributed, or labeled by H.J. Harkins Company, Inc., Boca Pharmacal, Inc, Cispharma, Inc. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
-
DESCRIPTION
Phenazopyridine Hydrochloride is a reddish-brown, odorless, slightly bitter, crystalline powder. It has a specific local analgesic effect in the urinary tract, promptly relieving burning and pain.
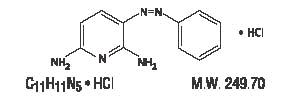
Following is the structural formula:
Phenazopyridine HCl tablets contain the following inactive ingredients: Corn Starch, Croscarmellose Sodium, Hypromellose, Light Mineral Oil, Magnesium Stearate, Microcrystalline Cellulose, Povidone, Pregelatinized Starch, and Silicon Dioxide.
-
CLINICAL PHARMACOLOGY
Phenazopyridine hydrochloride is excreted in the urine where it exerts a topical analgesic effect on the mucosa of the urinary tract. This action helps to relieve pain, burning, urgency and frequency. The precise mechanism of action is unknown.
PHARMACOKINETICS
The pharmacokinetic properties of phenazopyridine hydrochloride have not been determined. Phenazopyridine and its metabolites are rapidly excreted by the kidneys. In a small number of healthy subjects, 90% of a 600 mg/day oral dose of phenazopyridine hydrochloride was eliminated in the urine in 24 hours, 41% as unchanged drug and 49% as metabolites.
-
INDICATIONS AND USAGE
Phenazopyridine HCl is indicated for the symptomatic relief of pain, burning, urgency frequency, and other discomforts arising from irritation of the mucosa of the lower urinary tract caused by infection, trauma, surgery, endoscopic procedures, or the passage of sounds or catheters.
The use of phenazopyridine for relief of symptoms should not delay definitive diagnosis and treatment of causative conditions. The drug should be used for symptomatic relief of pain and not as a substitute for specific surgery or antimicrobial therapy.
Phenazopyridine is compatible with antimicrobial therapy and can help relieve pain and discomfort during the interval before antimicrobial therapy controls the infection.
Treatment of a urinary tract infection with phenazopyridine should not exceed 2 days. There is no evidence that the combined administration of phenazopyridine and an antimicrobial provides greater benefit than administration of the antimicrobial alone after 2 days. (See Dosage and Administration.)
- CONTRAINDICATIONS
-
WARNINGS
Phenazopyridine hydrochloride is reasonably anticipated to be a human carcinogen based on sufficient evidence of carcinogenicity in experimental animals (IARC 1980, 1982, 1987, NCI 1978). When administered in the diet, phenazopyridine hydrochloride increased the incidences of hepatocellular adenomas and carcinomas in female mice and adenomas and adenocarcinomas of the colon and rectum in rats of both sexes.
There is inadequate evidence for the carcinogenicity of phenazopyridine hydrochloride in humans (IARC 1987). In one limited epidemiological study, no significant excess of any cancer was observed among 2,214 patients who received phenazopyridine hydrochloride and were followed for a minimum of 3 years.
-
PRECAUTIONS
General: The patient should be advised that phenazopyridine produces an orange to red color in the urine and feces, and may cause staining. Phenazopyridine may cause discoloration of body fluids and staining of contact lenses has been reported. A yellowish color of the skin or sclera may indicate accumulation of phenazopyridine resulting from impaired renal function and necessitates discontinuance of the drug. It should be noted that a decline in renal function is common in elderly patients. Phenazopyridine may mask pathological conditions and interfere with laboratory test values using colorimetric, spectrophotometric or fluorometric analysis methods.
Cautious use in patients with G-6-PD deficiency is advised since these patients are susceptible to oxidative hemolysis and may have greater potential to develop hemolytic anemia.
Information for Patients: The patient should be advised to take phenazopyridine with or following food or after eating a snack to reduce stomach upset.
The patients should be aware that phenazopyridine causes a reddish orange discoloration of the urine and feces, and may stain clothing. Phenazopyridine may cause discoloration of body fluids and staining of contact lenses has been reported. There have been reports of teeth discoloration when the product has been broken or held in the mouth prior to swallowing.
Patients should be instructed to take phenazopyridine for only 2 days if an antibacterial agent is administered concurrently for the treatment of a urinary tract infection. If symptoms persist beyond those 2 days, the patient should be instructed to contact his or her physician.
Laboratory Tests: Phenazopyridine may interfere with laboratory test values using colorimetric, photometric or fluorometric analysis methods.
Altered urine laboratory test values may include ketone (sodium nitroprusside), bilirubin (foam test, talc-disk-Fouchet-spot test, Franklin's tablet-Fouchet test, p-nitrobenzene diazonium p- toluene sulfonate reagent), diacetic acid (Gerhardt ferric chloride test), free hydrochloric acid, glucose (glucose oxidase tests), 17-hydroxycorticosteroids (modified Glenn-Nelson), 17-ketosteroids (Holtorff Koch modification of Zimmerman), porphyrins, albumin (discolors bromophenol blue test areas of commercial reagent strips, nitric acid ring test), phenolsulfophthalein, urobilinogen (color interference with Ehrlich's reagent), and urinalysis (spectrophotometric or color-based tests). Phenazopyridine also imparts an orange-red color to stools which may interfere with color tests.
Drug Interactions: The interaction of phenazopyridine with other drugs has not been studied in a systematic manner. However, the medical literature to date suggests that no significant interactions have been reported.
Carcinogenesis, Mutagenesis, Impairment of Fertility: Long-term administration of phenazopyridine has been associated with tumors of the large intestine in rats and of the liver in mice. Available epidemiological data are insufficient to evaluate the carcinogenicity of phenazopyridine in humans. In vitro studies indicate that phenazopyridine in the presence of metabolic activation is mutagenic in bacteria and mutagenic and clastogenic in mammalian cells.
Pregnancy Category B: Reproductive studies with phenazopyridine (in combination with sulfacytine) in rats given up to 110 mg/kg/day and in rabbits given up to 39 mg/kg/day during organogenesis revealed no evidence of harm to offspring.
One prospective study in humans demonstrated that phenazopyridine traverses the placenta into the fetal compartment. There are no adequate and well-controlled studies in pregnant women. Therefore, phenazopyridine should be used in pregnant women only if the benefit clearly outweighs the risk.
Nursing Mothers: It is not known whether phenazopyridine or its metabolites are excreted in human milk. Because many drugs are excreted in human milk, a decision should be made to discontinue nursing or to discontinue the drug, taking into account the importance of drug therapy to the mother.
Children: Adequate and well-controlled studies have not been performed in the pediatric population. No pediatric-specific problems have been documented.
-
ADVERSE REACTIONS
The following adverse events have been reported:
CNS: headache.
Gastrointestinal: nausea, vomiting and diarrhea.
Dermatologic and Hypersensitivity: rash, pruritus, discoloration, anaphylactoid-like reaction and hypersensitivity hepatitis.
Hematologic: methemoglobinemia, hemolytic anemia, potential hemolytic agent in G-6-PD deficiency, sulfhemoglobinemia.
Other: visual disturbances, renal and hepatic toxicity usually associated with overdose, renal calculi, jaundice, discoloration of body fluids and aseptic meningitis.
-
OVERDOSAGE
Symptoms: Exceeding the recommended dose in patients with normal renal function or administering the recommended dose to patients with impaired renal function (common in elderly patients) may lead to increased serum levels and toxic reactions. Methemoglobinemia generally follows a massive, acute overdose. Methylene blue, 1 to 2 mg/kg/dose given i.v. as a 1% solution as needed, should cause prompt reduction of the methemoglobinemia and disappearance of the cyanosis which is an aid in diagnosis. Oxidative Heinz body hemolytic anemia also may occur, and "bite cells" (degmacytes) may be present in a chronic overdosage situation. Red blood cell G-6-PD deficiency may predispose to hemolysis; however, hemolysis may occur at normal doses in patients with G-6-PD Mediterranean. Renal toxicity and occasional failure and hepatic impairment may also occur.
Treatment: Treatment is symptomatic and supportive.
- DOSAGE AND ADMINISTRATION
-
HOW SUPPLIED
100 mg Tablets: Supplied in bottles of 100. Reddish-brown, round tablets, debossed “BP 811”.
NDC# 64376-811-01.200 mg Tablets: Supplied in bottles of 100. Reddish-brown, round tablets, debossed “BP 812”.
NDC# 64376-812-01.Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C -30°C (59°-86°F) [See USP Controlled Room Temperature].
Rx Only
Manufactured for:
Boca Pharmacal, Inc. Coral Springs, FL 33065
Ph: 800-354-8460 www.bocapharmacal.com
Rev. 10/12Repacked by:
H.J. Harkins Company, Inc.
Nipomo, CA 93444
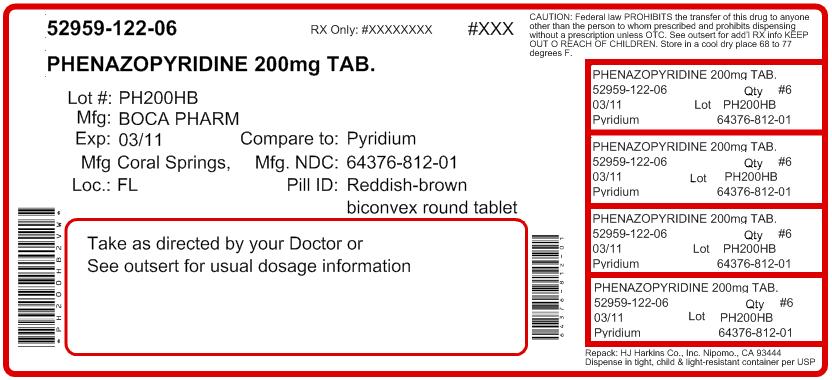
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
PHENAZOPYRIDINE HCL
phenazopyridine hcl tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 52959-122(NDC: 64376-812) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength PHENAZOPYRIDINE HYDROCHLORIDE (UNII: 0EWG668W17) (PHENAZOPYRIDINE - UNII:K2J09EMJ52) PHENAZOPYRIDINE HYDROCHLORIDE 200 mg Inactive Ingredients Ingredient Name Strength HYPROMELLOSES (UNII: 3NXW29V3WO) MINERAL OIL (UNII: T5L8T28FGP) MAGNESIUM STEARATE (UNII: 70097M6I30) POVIDONE (UNII: FZ989GH94E) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) Product Characteristics Color BROWN (Reddish-Brown) Score no score Shape ROUND (Biconvex) Size 10mm Flavor Imprint Code BP;812 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 52959-122-03 3 in 1 BOTTLE 2 NDC: 52959-122-04 4 in 1 BOTTLE 3 NDC: 52959-122-06 6 in 1 BOTTLE 4 NDC: 52959-122-09 9 in 1 BOTTLE 5 NDC: 52959-122-10 10 in 1 BOTTLE 6 NDC: 52959-122-12 12 in 1 BOTTLE 7 NDC: 52959-122-15 15 in 1 BOTTLE 8 NDC: 52959-122-20 20 in 1 BOTTLE 9 NDC: 52959-122-30 30 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date Unapproved drug other 09/10/2010 Labeler - H.J. Harkins Company, Inc. (147681894) Registrant - Boca Pharmacal, Inc (170266089) Establishment Name Address ID/FEI Business Operations Cispharma, Inc 833171445 MANUFACTURE
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.