KIPROFEN™ (Ketoprofen) Capsules
Kiprofen by
Drug Labeling and Warnings
Kiprofen by is a Prescription medication manufactured, distributed, or labeled by Trifluent Pharma LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
KIPROFEN- ketoprofen capsule
Trifluent Pharma LLC
----------
KIPROFEN™ (Ketoprofen) Capsules
Cardiovascular Thrombotic Events
- Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use [see Warningsand Precautions].
- Ketoprofen capsules are contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Contraindicationsand Warnings].
Gastrointestinal Risk
- NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal (GI) events (see Warnings).
1Throughout this package insert, the term NSAID refers to a non-aspirin non-steroidal anti-inflammatory drug.
DESCRIPTION
Ketoprofen is a non-steroidal anti-inflammatory drug. The chemical name for Ketoprofen is 2-(3-benzoylphenyl)-propionic acid with the following structural formula:
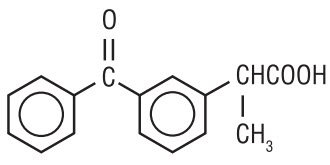
It has a pKa of 5.94 in methanol: water (3:1) and an n-octanol: water partition coefficient of 0.97 (buffer pH 7.4).
Ketoprofen is a white or off-white, odorless, nonhygroscopic, fine to granular powder, melting at about 95°C. It is freely soluble in ethanol, chloroform, acetone, ether and soluble in benzene and strong alkali, but practically insoluble in water at 20°C.
Kiprofen™ Capsules contain 25 mg or 50 mg of Ketoprofen USP for oral administration.
CLINICAL PHARMACOLOGY
Ketoprofen is a non-steroidal anti-inflammatory drug with analgesic and antipyretic properties.
The anti-inflammatory, analgesic and antipyretic properties of ketoprofen have been demonstrated in classical animal and in vitro test systems. In anti-inflammatory models ketoprofen has been shown to have inhibitory effects on prostaglandin and leukotriene synthesis, to have antibradykinin activity, as well as to have lysosomal membrane-stabilizing action. However, its mode of action, like that of other non-steroidal anti-inflammatory drugs, is not fully understood.
Pharmacodynamics
Ketoprofen is a racemate with only the S enantiomer possessing pharmacological activity. The enantiomers have similar concentration time curves and do not appear to interact with one another.
An analgesic effect-concentration relationship for ketoprofen was established in an oral surgery pain study with immediate-release ketoprofen capsules. The effect-site rate constant (k e0) was estimated to be 0.9 hour (95% confidence limits: 0 to 2.1), and the concentration (C e50) of ketoprofen that produced one-half the maximum PID (pain intensity difference) was 0.3 mcg/mL (95% confidence limits: 0.1 to 0.5). Thirty-three (33) to 68% of patients had an onset of action (as measured by reporting some pain relief) within 30 minutes following a single oral dose in postoperative pain and dysmenorrhea studies. Pain relief (as measured by remedication) persisted for up to 6 hours in 26 to 72% of patients in these studies.
Pharmacokinetics
General
The systemic availability (F S) when the oral formulation is compared with IV administration is approximately 90% in humans. For 75 to 200 mg single doses, the area under the curve has been shown to be dose proportional.
Ketoprofen is > 99% bound to plasma proteins, mainly to albumin.
Absorption
Ketoprofen is rapidly and well-absorbed, with peak plasma levels occurring within 0.5 to 2 hours.
When ketoprofen is administered with food, its total bioavailability (AUC) is not altered; however; the rate of absoprtion is slowed.
Food intake reduces C maxby approximately one-half and increases the mean time to peak cencentration (T max) 1.2 hours of fasting subjects (range, 0.5 to 3 hours) to 2.0 hours for fed subjects (range, 0.75 to 3 hours). The fluctuation of plasma peaks may also be influenced by circadian changes in the apborption process.
Concomitant administration of magnesium hydroxide and aluminum hydroxide does not interfere with absorption of ketoprofen from ketoprofen capsules.
Multiple Dosing
Steady-state concentrations of ketoprofen are attained within 24 hours after commencing treatment with immediate-release ketoprofen capsules. In studies with healthy male volunteers, trough levels at 24 hours following administration of immediate-release ketoprofen 50 mg capsules QID for 12 hours were 0.07 mg/L and 0.13 mg/L at 24 hours following administration of immediate-release ketoprofen 75 mg capsules TID for 12 hours. Thus, relative to the peak plasma concentration, the accumulation of ketoprofen after multiple doses of immediate-release ketoprofen capsules is minimal.
The figure below shows a reduction in peak height and area after the second 50 mg dose. This is probably due to a combination of food effects, circadian effects, and plasma sampling times. It is unclear to what extent each factor contributes to the loss of peak height and area.
The shaded area represents ± 1 standard deviation (S.D.) around the mean for immediate-release ketoprofen capsules.

KETOPROFEN PLASMA CONCENTRATIONS IN SUBJECTS RECEIVING KETOPROFEN CAPSULES 50 MG EVERY 4 HOURS FOR 16 HOURS
| Kinetic Parameters | Ketoprofen Capsules (4 × 50 mg) |
|---|---|
|
|
|
| Extent of oral absorption (bioavailability) Fs (%) | ~90 |
| Peak plasma levels C max(mg/L) Fasted Fed | 3.9 ± 1.3 2.4 ± 1.0 |
| Time to peak concentration t max(h) Fasted Fed | 1.2 ± 0.6 2.0 ± 0.8 |
| Area under plasma concentration-time curve AUC 0-24h(mg∙h/L) Fasted Fed | 32.1 ± 7.2 36.6 ± 8.1 |
| Oral-dose clearance CL/F (L/h) | 6.9 ± 0.8 |
| Half-life t 1/2(h) | 2.1 ± 1.2 |
Metabolism
The metabolic fate of ketoprofen is glucuronide conjugation to form an unstable acyl-glucuronide. The glucuronic acid moiety can be converted back to the parent compound. Thus, the metabolite serves as a potential reservoir for parent drug, and this may be important in persons with renal insufficiency, whereby the conjugate may accumulate in the serum and undergo deconjugation back to the parent drug (see Special Populations, Renally Impaired). The conjugates are reported to appear only in trace amounts in plasma in healthy adults, but are higher in elderly subjects-presumably because of reduced renal clearance. It has been demonstrated that in elderly subjects following multiple doses (50 mg every 6 h), the ratio of conjugated to parent ketoprofen AUC was 30% and 3%, respectively, for the S & R enantiomers.
There are no known active metabolites of ketoprofen. Ketoprofen has been shown not to induce drug-metabolizing enzymes.
Elimination
The plasma clearance of ketoprofen is approximately 0.08 L/kg/h with a V dof 0.1 L/kg after IV administration. The elimination half-life of ketoprofen has been reported to be 2.05 ± 0.58 h (Mean ± S.D.) following IV administration from 2 to 4 hours following administration of ketoprofen capsules. In cases of slow drug absorption, the elimination rate is dependent on the absorption rate and thus t 1/2relative to an IV dose appears prolonged.
In a 24 hour period, approximately 80% of an administered dose of ketoprofen is excreted in the urine, primarily as the glucuronide metabolite.
Enterohepatic recirculation of the drug has been postulated, although biliary levels have never been measured to confirm this.
Special Populations
Elderly
Clearance and unbound fraction
The plasma and renal clearance of ketoprofen is reduced in the elderly (mean age, 73 years) compared to a younger normal population (mean age, 27 years). Hence, ketoprofen peak concentration and AUC increase with increasing age. In addition, there is a corresponding increase in unbound fraction with increasing age. Data from one trial suggest that the increase is greater in women than in men. It has not been determined whether age-related changes in absorption among the elderly contribute to the changes in bioavailability of ketoprofen (see Geriatric Use).
In a study conducted with young and elderly men and women, results for subjects older than 75 years of age showed that free drug AUC increased by 40% and C maxincreased by 60% as compared with estimates of the same parameters in young subjects (those younger than 35 years of age; see DOSAGE AND ADMINISTRATION).
Also in the elderly, the ratio of intrinsic clearance/availability decreased by 35% and plasma half-life was prolonged by 26%. This reduction is thought to be due to a decrease in hepatic extraction associated with aging.
Renally Impaired
Studies of the effects of renal-function impairment have been small. They indicate a decrease in clearance in patients with impaired renal function. In 23 patients with renal impairment, free ketoprofen peak concentration was not significantly elevated, but free ketoprofen clearance was reduced from 15 L/kg/h for normal subjects to 7 L/kg/h in patients with mildly impaired renal function, and to 4 L/kg/h in patients with moderately to severely impaired renal function. The elimination t 1/2was prolonged from 1.6 hours in normal subjects to approximately 3 hours in patients with mild renal impairment, and to approximately 5 to 9 hours in patients with moderately to severely impaired renal function.
Hepatically Impaired
For patients with alcoholic cirrhosis, no significant changes in the kinetic disposition of immediate-release ketoprofen capsules were observed relative to age-matched normal subjects: the plasma clearance of drug was 0.07 L/kg/h in 26 hepatically impaired patients. The elimination half-life was comparable to that observed for normal subjects. However, the unbound (biologically active) fraction was approximately doubled, probably due to hypoalbuminemia and high variability which was observed in the pharmacokinetics for cirrhotic patients. Therefore, these patients should be carefully monitored and daily doses of ketoprofen kept at the minimum providing the desired therapeutic effect.
Clinical Trials
Rheumatoid Arthritis and Osteoarthritis
The efficacy of ketoprofen has been demonstrated in patients with rheumatoid arthritis and osteoarthritis. In other trials, ketoprofen demonstrated effectiveness comparable to aspirin, ibuprofen, naproxen, piroxicam, diclofenac, and indomethacin. In some of these studies there were more dropouts due to gastrointestinal side effects among patients on ketoprofen than among patients on other NSAIDs.
In studies with patients with rheumatoid arthritis, ketoprofen was administered in combination with gold salts, antimalarials, low-dose methotrexate, d-penicillamine, and/or corticosteroids with results comparable to those seen with control non-steroidal drugs.
Management of Pain
The effectiveness of immediate-release ketoprofen capsules as a general-purpose analgesic has been studied in standard pain models which have shown the effectiveness of doses of 25 to 150 mg. Doses of 25 mg were superior to placebo. Doses larger than 25 mg generally could not be shown to be significantly more effective, but there was a t endency toward faster onset and greater duration of action with 50 mg, and, in the case of dysmenorrhea, a significantly greater effect overall with 75 mg. Doses greater than 50 to 75 mg did not have increased analgesic effect. Studies in postoperative pain have shown that ketoprofen in doses of 25 to 100 mg was comparable to 650 mg of acetaminophen with 60 mg of codeine, or 650 mg of acetaminophen with 10 mg of oxycodone. Ketoprofen tended to be somewhat slower in onset; peak pain relief was about the same and the duration of the effect tended to be 1 to 2 hours longer, particularly with the higher doses of ketoprofen.
INDICATIONS AND USAGE
Carefully consider the potential benefits and risks of ketoprofen capsules USP and other treatment options before deciding to use ketoprofen capsules USP. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
Ketoprofen capsules USP are indicated for the management of the signs and symptoms of rheumatoid arthritis and osteoarthritis.
Ketoprofen capsules USP are indicated for the management of pain. Ketoprofen capsules USP are also indicated for treatment of primary dysmenorrhea.
CONTRAINDICATIONS
Ketoprofen capsules are contraindicated in patients who have shown hypersensitivity to ketoprofen.
Ketoprofen capsules USP should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic reactions to ketoprofen have been reported in such patients (see WARNINGS, Anaphylactoid Reactionsand PRECAUTIONS, Preexisting Asthma).
Ketoprofen capsules USP are contraindicated in the setting of coronary artery bypass graft (CABG) surgery [see Warnings]
WARNINGS
Cardiovascular Effects
Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as Ketoprofen, increases the risk of serious gastrointestinal (GI) events [see Warnings].
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatments of pain in the first 10-14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG [see Contraindications].
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of Ketoprofen capsules in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If Ketoprofen capsules are used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
Hypertension
NSAIDs, including ketoprofen capsules, can lead to onset of new hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including ketoprofen capsules, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
Heart Failure and Edema
The Coxib and traditional NSAID Trialists' Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of Ketoprofen may blunt the CV effects of several therapeutic agents used to treat these medical conditions [e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers (ARBs)] [see Drug Interactions].
Avoid the use of Ketoprofen capsules in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If Ketoprofen capsules are used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
Gastrointestinal Effects - Risk of Ulceration, Bleeding, and Perforation
NSAIDs, including ketoprofen capsules, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation, of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3 to 6 months, and in about 2 to 4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
NSAIDs should be prescribed with extreme caution in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleedingwho use NSAIDs have a greater than 10 fold increased risk for developing a GI bleed compared to patients with neither of these risk factors. Other factors that increase the risk for GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population.
To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high risk patients, alternate therapies that do not involve NSAIDs should be considered.
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a non-steroidal anti-inflammatory drug may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greater risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE-inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
Advanced Renal Disease
No information is available from controlled clinical studies regarding the use of ketoprofen capsules in patients with advanced renal disease. Therefore, treatment with ketoprofen capsules is not recommended in these patients with advanced renal disease. If ketoprofen capsule therapy must be initiated, close monitoring of the patient's renal function is advisable.
Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur in patients without known prior exposure to ketoprofen capsules. Ketoprofen capsules should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs (see CONTRAINDICATIONSand PRECAUTIONS, Preexisting Asthma). Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Skin Reactions
NSAIDs, including ketoprofen capsules, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) has been reported in patients taking NSAIDs such as ketoprofen capsules. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling. Other clinical manifestations may include hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis. Sometimes symptoms of DRESS may resemble an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its presentation, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, discontinue ketoprofen capsules and evaluate the patient immediately.
Fetal Toxicity
Premature Closure of Fetal Ductus Arteriosus
Avoid use of NSAIDs, including ketoprofen capsules, in pregnant women at about 30 weeks gestation and later. NSAIDs including ketoprofen capsules, increase the risk of premature closure of the fetal ductus arteriosus at approximately this gestational age.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs, including ketoprofen capsules, at about 20 weeks gestation or later in pregnancy may cause fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. Oligohydramnios is often, but not always, reversible with treatment discontinuation. Complications of prolonged oligohydramnios may, for example, include limb contractures and delayed lung maturation. In some postmarketing cases of impaired neonatal renal function, invasive procedures such as exchange transfusion or dialysis were required.
If NSAID treatment is necessary between about 20 weeks and 30 weeks gestation, limit ketoprofen capsules use to the lowest effective dose and shortest duration possible. Consider ultrasound monitoring of amniotic fluid if ketoprofen capsules treatment extends beyond 48 hours. Discontinue ketoprofen capsules if oligohydramnios occurs and follow up according to clinical practice [see PRECAUTIONS; Pregnancy].
PRECAUTIONS
General
Ketoprofen capsules cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to disease exacerbation. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a decision is made to discontinue corticosteroids.
If steroid dosage is reduced or eliminated during therapy, it should be reduced slowly and the patients observed closely for any evidence of adverse effects, including adrenal insufficiency and exacerbation of symptoms of arthritis.
The pharmacological activity of ketoprofen capsules in reducing fever and inflammation may diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
Ketoprofen and other non-steroidal anti-inflammatory drugs cause nephritis in mice and rats associated with chronic administration. Rare cases of interstitial nephritis or nephrotic syndrome have been reported in humans with ketoprofen since it has been marketed.
A second form of renal toxicity has been seen in patients with conditions leading to a reduction in renal blood flow or blood volume, where renal prostaglandins have a supportive role in the maintenance of renal blood flow. In these patients, administration of a non-steroidal anti-inflammatory drug results in a dose-dependent decrease in prostaglandin synthesis and, secondarily, in renal blood flow which may precipitate overt renal failure. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics, and the elderly. Discontinuation of non-steroidal anti-inflammatory drug therapy is typically followed by recovery to the pretreatment state.
Since ketoprofen is primarily eliminated by the kidneys and its pharmacokinetics are altered by renal failure (see CLINICAL PHARMACOLOGY), patients with significantly impaired renal function should be closely monitored, and a reduction of dosage should be anticipated to avoid accumulation of ketoprofen and/or its metabolites (see DOSAGE AND ADMINISTRATION).
Hepatic Effects
Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs including ketoprofen capsules. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice, and fatal fulminant hepatitis, liver necrosis and hepatic failure, some of them with fatal outcomes have been reported.
A patient with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, should be evaluated for evidence of the development of a more severe hepatic reaction while on therapy with ketoprofen capsules. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), ketoprofen capsules should be discontinued.
In patients with chronic liver disease with reduced serum albumin levels, ketoprofen's pharmacokinetics are altered (see CLINICAL PHARMACOLOGY). Such patients should be closely monitored, and a reduction of dosage should be anticipated to avoid high blood levels of ketoprofen and/or its metabolites (see DOSAGE AND ADMINISTRATION).
Hematological Effects
Anemia is sometimes seen in patients receiving NSAIDs, including ketoprofen capsules. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including ketoprofen capsules, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible. Patients receiving ketoprofen capsules who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants, should be carefully monitored.
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and other non-steroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, ketoprofen capsules should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
Information for Patients
Patients should be informed of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. Patients should also be encouraged to read the NSAID Medication Guide that accompanies each prescription dispensed.
-
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see Warnings]. - Ketoprofen capsules, like other NSAIDs, can cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients should be alert for the signs and symptoms of ulcerations and bleeding, and should ask for medical advice when observing any indicative signs or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Patients should be apprised of the importance of this follow-up (see WARNINGS, Gastrointestinal Effects - Risk of Ulceration, Bleeding, and Perforation).
-
Serious Skin Reactions, including DRESS
Advise patients to stop taking ketoprofen capsules immediately if they develop any type of rash or fever and to contact their healthcare provider as soon as possible [see Warnings]. -
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur. [see Warnings]. - Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, patients should be instructed to stop therapy and seek immediate medical therapy.
- Patients should be informed of the signs of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). If these occur, patients should be instructed to seek immediate emergency help (see WARNINGS).
-
Fetal Toxicity
Inform pregnant women to avoid use of ketoprofen capsules and other NSAIDs starting at 30 weeks gestation because of the risk of the premature closing of the fetal ductus arteriosus. If treatment with ketoprofen capsules is needed for a pregnant woman between about 20 to 30 weeks gestation, advise her that she may need to be monitored for oligohydramnios, if treatment continues for longer than 48 hours [see WARNINGS; Fetal Toxicity, PRECAUTIONS; Pregnancy].
NSAIDs are often essential agents in the management of arthritis and have a major role in the treatment of pain, but they also may be commonly employed for conditions which are less serious. Physicians may wish to discuss with their patients the potential risks (see WARNINGS, PRECAUTIONS, and ADVERSE REACTIONS) and likely benefits of NSAID treatment, particularly when the drugs are used for less serious conditions where treatment without NSAIDs may represent an acceptable alternative to both the patient and physician.
Because aspirin causes an increase in the level of unbound ketoprofen, patients should be advised not to take aspirin while taking ketoprofen (see Drug Interactions). It is possible that minor adverse symptoms of gastric intolerance may be prevented by administering ketoprofen capsules with antacids, food, or milk. Because food and milk do affect the rate but not the extent of absorption (see CLINICAL PHARMACOLOGY), physicians may want to make specific recommendations to patients about when they should take ketoprofen in relation to food and/or what patients should do if they experience minor GI symptoms associated with ketoprofen therapy.
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. Patients on long-term treatment with NSAIDs, should have their CBC and a chemistry profile checked periodically. If clinical signs and symptoms consistent with liver or renal disease develop, systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if abnormal liver tests persist or worsen, ketoprofen capsules should be discontinued.
Drug Interactions
The following drug interactions were studied with ketoprofen doses of 200 mg/day. The possibility of increased interaction should be kept in mind when ketoprofen capsule doses greater than 50 mg as a single dose or 200 mg of ketoprofen per day are used concomitantly with highly bound drugs.
ACE-inhibitors
Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE-inhibitors. This interaction should be given consideration in patients taking NSAIDs concomitantly with ACE-inhibitors.
Antacids
Concomitant administration of magnesium hydroxide and aluminum hydroxide does not interfere with the rate or extent of the absorption of ketoprofen administered as ketoprofen capsules.
Aspirin
Ketoprofen does not alter aspirin absorption; however, in a study of 12 normal subjects, concurrent administration of aspirin decreased ketoprofen protein binding and increased ketoprofen plasma clearance from 0.07 L/kg/h without aspirin to 0.11 L/kg/h with aspirin. The clinical significance of these changes is not known; however, as with other NSAIDs, concomitant administration of ketoprofen and aspirin is not generally recommended because of the potential of increased adverse effects.
Diuretics
NSAIDs can reduce the natriuretic effect of furosemide and thiazides in some patients. Hydrochlorothiazide, given concomitantly with ketoprofen, produces a reduction in urinary potassium and chloride excretion compared to hydrochlorothiazide alone. Patients taking diuretics are at a greater risk of developing renal failure secondary to a decrease in renal blood flow caused by prostaglandin inhibition (see PRECAUTIONS). During concomitant therapy with NSAIDs, the patient should be observed closely for signs of renal failure (see WARNINGS, Renal Effects), as well as to assure diuretic efficacy.
Digoxin
In a study in 12 patients with congestive heart failure where ketoprofen and digoxin were concomitantly administered, ketoprofen did not alter the serum levels of digoxin.
Lithium
NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15% and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by the NSAID. Thus, when NSAIDs and lithium are administered concurrently, subjects should be observed carefully for signs of lithium toxicity.
Methotrexate
Ketoprofen, like other NSAIDs, may cause changes in the elimination of methotrexate leading to elevated serum levels of the drug and increased toxicity. NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Caution should be used when NSAIDs are administered concomitantly with methotrexate.
Probenecid
Probenecid increases both free and bound ketoprofen by reducing the plasma clearance of ketoprofen to about one-third, as well as decreasing its protein binding. Therefore, the combination of ketoprofen and probenecid is not recommended.
Warfarin
The effects of warfarin and NSAIDs on GI bleeding are synergistic, such that users of both drugs together have a risk of serious GI bleeding higher than users of either drug alone. In a short-term controlled study in 14 normal volunteers, ketoprofen did not significantly interfere with the effect of warfarin on prothrombin time. Bleeding from a number of sites may be a complication of warfarin treatment and GI bleeding a complication of ketoprofen treatment. Because prostaglandins play an important role in hemostasis and ketoprofen has an effect on platelet function as well (see Drug/Laboratory Test Interactions, Effect on Blood Coagulation), concurrent therapy with ketoprofen and warfarin requires close monitoring of patients on both drugs.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Chronic oral toxicity studies in mice (up to 32 mg/kg/day; 96 mg/m 2/day) did not indicate a carcinogenic potential for ketoprofen. The maximum recommended human therapeutic dose is 300 mg/day for a 60 kg patient with a body surface area of 1.6 m 2, which is 5 mg/kg/day or 185 mg/m 2/day. Thus the mice were treated at 0.5 times the maximum human daily dose based on surface area.
A 2 year carcinogenicity study in rats, using doses up to 6.0 mg/kg/day (36 mg/m 2/day), showed no evidence of tumorigenic potential. All groups were treated for 104 weeks except the females receiving 6.0 mg/kg/day (36 mg/m 2/day) where the drug treatment was terminated in week 81 because of low survival; the remaining rats were sacrificed after week 87. Their survival in the groups treated for 104 weeks was within 6% of the control group. An earlier 2 year study with doses up to 12.5 mg/kg/day (75 mg/m 2/day) also showed no evidence of tumorigenicity, but the survival rate was low and the study was therefore judged inconclusive. Ketoprofen did not show mutagenic potential in the Ames Test. Ketoprofen administered to male rats (up to 9 mg/kg/day; or 54 mg/m 2/day) had no significant effect on reproductive performance or fertility. In female rats administered 6 or 9 mg/kg/day (36 or 54 mg/m 2/day), a decrease in the number of implantation sites has been noted. The dosages of 36 mg/m 2/day in rats represent 0.2 times the maximum recommended human dose of 185 mg/m 2/day (see above).
Abnormal spermatogenesis or inhibition of spermatogenesis developed in rats and dogs at high doses, and a decrease in the weight of the testes occurred in dogs and baboons at high doses.
Pregnancy
Risk Summary
Use of NSAIDs, including ketoprofen capsules, can cause premature closure of the fetal ductus arteriosus and fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. Because of these risks, limit dose and duration of ketoprofen capsules use between about 20 and 30 weeks of gestation, and avoid ketoprofen capsules use at about 30 weeks of gestation and later in pregnancy [see WARNINGS; Fetal Toxicity].
Premature Closure of Fetal Ductus Arteriosus
Use of NSAIDs, including ketoprofen capsules, at about 30 weeks gestation or later in pregnancy increases the risk of premature closure of the fetal ductus arteriosus.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs at about 20 weeks gestation or later in pregnancy has been associated with cases of fetal renal dysfunction leading to oligohydramnios, and in some cases, neonatal renal impairment.
Data from observational studies regarding other potential embryofetal risks of NSAID use in women in the first or second trimesters of pregnancy are inconclusive. In animal reproduction studies ketoprofen administered to mice at doses up to 12 mg/kg/day (36 mg/m 2/day) and rats at doses up to 9 mg/kg/day (54 mg/m 2/day), the approximate equivalent of 0.2 times the maximum recommended therapeutic dose of 185 mg/m 2/day, showed no teratogenic or embryotoxic effects. In separate studies in rabbits, maternally toxic doses were associated with embryotoxicity but not teratogenicity. However, animal reproduction studies are not always predictive of human response. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as ketoprofen, resulted in increased pre- and post-implantation loss. Prostaglandins also have been shown to have an important role in fetal kidney development. In published animal studies, prostaglandin synthesis inhibitors have been reported to impair kidney development when administered at clinically relevant doses.
The estimated background risk of major birth defects and miscarriage for the indicated population(s) is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Premature Closure of Fetal Ductus Arteriosus
Avoid use of NSAIDs in women at about 30 weeks gestation and later in pregnancy, because NSAIDs, including ketoprofen capsules, can cause premature closure of the fetal ductus arteriosus (see WARNINGS; Fetal Toxicity).
Oligohydramnios/Neonatal Renal Impairment
If an NSAID is necessary at about 20 weeks gestation or later in pregnancy, limit the use to the lowest effective dose and shortest duration possible. If ketoprofen capsules treatment extends beyond 48 hours, consider monitoring with ultrasound for oligohydramnios. If oligohydramnios occurs, discontinue ketoprofen capsules and follow up according to clinical practice (see WARNINGS; Fetal Toxicity).
Data
Human Data
Premature Closure of Fetal Ductus Arteriosus
Published literature reports that the use of NSAIDs at about 30 weeks of gestation and later in pregnancy may cause premature closure of the fetal ductus arteriosus.
Oligohydramnios/Neonatal Renal Impairment
Published studies and postmarketing reports describe maternal NSAID use at about 20 weeks gestation or later in pregnancy associated with fetal renal dysfunction leading to oligohydramnios, and in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. In many cases, but not all, the decrease in amniotic fluid was transient and reversible with cessation of the drug. There have been a limited number of case reports of maternal NSAID use and neonatal renal dysfunction without oligohydramnios, some of which were irreversible. Some cases of neonatal renal dysfunction required treatment with invasive procedures, such as exchange transfusion or dialysis.
Methodological limitations of these postmarketing studies and reports include lack of a control group; limited information regarding dose, duration, and timing of drug exposure; and concomitant use of other medications. These limitations preclude establishing a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAID use. Because the published safety data on neonatal outcomes involved mostly preterm infants, the generalizability of certain reported risks to the full-term infant exposed to NSAIDs through maternal use is uncertain.
Labor and Delivery
The effects of ketoprofen on labor and delivery in pregnant women are unknown. Studies in rats have shown ketoprofen at doses of 6 mg/kg (36 mg/m 2/day, approximately equal to 0.2 times the maximum recommended human dose) prolongs pregnancy when given before the onset of labor. Because of the known effects of prostaglandin-inhibiting drugs on the fetal cardiovascular system (closure of ductus arteriosus), use of ketoprofen during late pregnancy should be avoided.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Data on secretion in human milk after ingestion of ketoprofen do not exist. In rats, ketoprofen at doses of 9 mg/kg (54 mg/m 2/day; approximately 0.3 times the maximum human therapeutic dose) did not affect perinatal development. Upon administration to lactating dogs, the milk concentration of ketoprofen was found to be 4 to 5% of the plasma drug level. As with other drugs that are excreted in milk, ketoprofen is not recommended for use in nursing mothers.
Pediatric Use
Safety and effectiveness in pediatric patients below the age of 18 have not been established.
Geriatric Use
As with any NSAIDs, caution should be exercised in treating the elderly (65 years and older). In pharmacokinetic studies, ketoprofen clearance was reduced in older patients receiving ketoprofen capsules, compared with younger patients. Peak ketoprofen concentrations and free drug AUC were increased in older patients (see Special Populations). The glucuronide conjugate of ketoprofen, which can serve as a potential reservoir for the parent drug, is known to be substantially excreted by the kidney. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection. It is recommended that the initial dosage of ketoprofen capsules should be reduced for patients over 75 years of age and it may be useful to monitor renal function (see DOSAGE AND ADMINISTRATION). In addition, the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Elderly patients may be more sensitive to the antiprostaglandin effects of NSAIDs (on the gastrointestinal tract and kidneys) than younger patients (see WARNINGSand PRECAUTIONS). In particular, elderly or debilitated patients who receive NSAID therapy seem to tolerate gastrointestinal ulceration or bleeding less well than other individuals, and most spontaneous reports of fatal GI events are in this population. Therefore, caution should be exercised in treating the elderly, and when individualizing their dosage, extra care should be taken when increasing the dose (see DOSAGE AND ADMINISTRATION).
In ketoprofen capsule clinical studies involving a total of 1540 osteoarthritis or rheumatoid arthritis patients, 369 (24%) were ≥ 65 years of age, and 92 (6%) were ≥ 75 years of age. For ketoprofen capsule acute pain studies, 23 (5%) of 484 patients were ≥ 60 years of age. No overall differences in effectiveness were observed between these patients and younger patients.
ADVERSE REACTIONS
The incidence of common adverse reactions (above 1%) was obtained from a population of 835 ketoprofen-treated patients in double-blind trials lasting from 4 to 54 weeks and in 622 patients treated with ketoprofen extended-release capsules in trials lasting from 4 to 16 weeks.
Minor gastrointestinal side effects predominated; upper gastrointestinal symptoms were more common than lower gastrointestinal symptoms. In crossover trials in 321 patients with rheumatoid arthritis or osteoarthritis, there was no difference in either upper or lower gastrointestinal symptoms between patients treated with 200 mg of ketoprofen extended-release capsules once a day or 75 mg of ketoprofen immediate-release capsules TID (255 mg/day). Peptic ulcer or GI bleeding occurred in controlled clinical trials in less than 1% of 1,076 patients; however, in open label continuation studies in 1,292 patients, the rate was greater than 2%.
The incidence of peptic ulceration in patients on NSAIDs is dependent on many risk factors including age, sex, smoking, alcohol use, diet, stress, concomitant drugs such as aspirin and corticosteroids, as well as the dose and duration of treatment with NSAIDs (see WARNINGS).
Gastrointestinal reactions were followed in frequency by central nervous system side effects, such as headache, dizziness, or drowsiness. The incidence of some adverse reactions appears to be dose-related (see DOSAGE AND ADMINISTRATION). Rare adverse reactions (incidence less than 1%) were collected from one or more of the following sources: foreign reports to manufacturers and regulatory agencies, publications, U.S. clinical trials, and/or U.S. postmarketing spontaneous reports.
Reactions are listed below under body system, then by incidence or number of cases in decreasing incidence.
Incidence Greater Than 1% (Probable Causal Relationship)
Digestive:Dyspepsia (11%), nausea 1, abdominal pain 1, diarrhea 1, constipation 1, flatulence 1, anorexia, vomiting, stomatitis.
Nervous System:Headache 1, dizziness, CNS inhibition (i.e., pooled reports of somnolence, malaise, depression, etc.) or excitation (i.e., insomnia, nervousness, dreams, etc.) 1.
Special Senses:Tinnitus, visual disturbance.
Skin and Appendages:Rash.
Urogenital:Impairment of renal function (edema, increased BUN) 1, signs or symptoms of urinary-tract irritation.
Incidence Less Than 1% (Probable Causal Relationship)
Body as a Whole:Chills, facial edema, infection, pain, allergic reaction, anaphylaxis.
Cardiovascular:Hypertension, palpitation, tachycardia, congestive heart failure, peripheral vascular disease, vasodilation.
Digestive:Appetite increased, dry mouth, eructation, gastritis, rectal hemorrhage, melena, fecal occult blood, salivation, peptic ulcer, gastrointestinal perforation, hematemesis, intestinal ulceration, hepatic dysfunction, hepatitis, cholestatic hepatitis, jaundice.
Hemic:Hypocoagulability, agranulocytosis, anemia, hemolysis, purpura, thrombocytopenia.
Metabolic and Nutritional:Thirst, weight gain, weight loss, hyponatremia.
Musculoskeletal:Myalgia.
Nervous System:Amnesia, confusion, impotence, migraine, paresthesia, vertigo.
Respiratory:Dyspnea, hemoptysis, epistaxis, pharyngitis, rhinitis, bronchospasm, laryngeal edema.
Skin and Appendages:Alopecia, eczema, pruritus, purpuric rash, sweating, urticaria, bullous rash, exfoliative dermatitis, photosensitivity, skin discoloration, onycholysis, toxic epidermal necrolysis, erythema multiforme, Stevens-Johnson syndrome.
Special Senses:Conjunctivitis, conjunctivitis sicca, eye pain, hearing impairment, retinal hemorrhage and pigmentation change, taste perversion.
Urogenital:Menometrorrhagia, hematuria, renal failure, interstitial nephritis, nephrotic syndrome.
To report SUSPECTED ADVERSE REACTIONS, contact Misemer Pharmaceutical, Inc. at 1-662-993-9625 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Incidence Less Than 1% (Causal Relationship Unknown)
The following rare adverse reactions, whose causal relationship to ketoprofen is uncertain, are being listed to serve as alerting information to the physician.
Body as a Whole:Septicemia, shock.
Cardiovascular:Arrhythmias, myocardial infarction.
Digestive:Buccal necrosis, ulcerative colitis, microvesicular steatosis, pancreatitis. Endocrine: Diabetes mellitus (aggravated).
Nervous System:Dysphoria, hallucination, libido disturbance, nightmares, personality disorder, aseptic meningitis.
Urogenital:Acute tubulopathy, gynecomastia
OVERDOSAGE
Signs and symptoms following acute NSAID overdose are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Respiratory depression, coma, or convulsions have occurred following large ketoprofen overdoses. Gastrointestinal bleeding, hypotension, hypertension, or acute renal failure may occur, but are rare.
Patients should be managed by symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. Gut decontamination may be indicated in patients with symptoms seen within 4 hours or following a large overdose (5 to 10 times the usual dose). This should be accomplished via emesis and/or activated charcoal (60 to 100 g in adults, 1 to 2 g/kg in children) with a saline cathartic or sorbitol added to the first dose. Forced diuresis, alkalinization of the urine, hemodialysis or hemoperfusion would probably not be useful due to ketoprofen's high protein binding.
Case reports include twenty-six overdoses: 6 were in children, 16 in adolescents, and 4 in adults. Five of these patients had minor symptoms (vomiting in 4, drowsiness in 1 child). A 12-year-old girl had tonic-clonic convulsions 1 to 2 hours after ingesting an unknown quantity of ketoprofen and 1 or 2 tablets of acetaminophen with hydrocodone. Her ketoprofen level was 1128 mg/L (56 times the upper therapeutic level of 20 mg/L) 3 to 4 hours post ingestion. Full recovery ensued 18 hours after ingestion following management with intubation, diazepam, and activated charcoal. A 45-year-old woman ingested twelve 200 mg extended-release ketoprofen capsules and 375 mL vodka, was treated with emesis and supportive measures 2 hours after ingestion, and recovered completely with her only complaint being mild epigastric pain.
DOSAGE AND ADMINISTRATION
Carefully consider the potential benefits and risks of ketoprofen capsules and other treatment options before deciding to use ketoprofen capsules. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
After observing the response to initial therapy with ketoprofen capsules, the dose and frequency should be adjusted to suit an individual patient's needs.
Concomitant use of ketoprofen capsules and ketoprofen extended-release capsules is not recommended.
If minor side effects appear, they may disappear at a lower dose which may still have an adequate therapeutic effect. If well tolerated but not optimally effective, the dosage may be increased.
Individual patients may show a better response to 300 mg of ketoprofen capsules daily as compared to 200 mg, although in well-controlled clinical trials patients on 300 mg did not show greater mean effectiveness. They did, however, show an increased frequency of upper- and lower-GI distress and headaches. It is of interest that women also had an increased frequency of these adverse effects compared to men. When treating patients with 300 mg/day, the physician should observe sufficient increased clinical benefit to offset potential increased risk.
In patients with mildly impaired renal function, the maximum recommended total daily dose of ketoprofen capsules is 150 mg. In patients with a more severe renal impairment (GFR less than 25 mL/min/1.73 m 2or end-stage renal impairment), the maximum total daily dose of ketoprofen capsules should not exceed 100 mg.
In elderly patients, renal function may be reduced with apparently normal serum creatinine and/or BUN levels. Therefore, it is recommended that the initial dosage of ketoprofen capsules should be reduced for patients over 75 years of age (see Geriatric Use).
It is recommended that for patients with impaired liver function and serum albumin concentration less than 3.5 g/dL, the maximum initial total daily dose of ketoprofen capsules should be 100 mg. All patients with metabolic impairment, particularly those with both hypoalbuminemia and reduced renal function, may have increased levels of free (biologically active) ketoprofen and should be closely monitored. The dosage may be increased to the range recommended for the general population, if necessary, only after good individual tolerance has been ascertained.
Because hypoalbuminemia and reduced renal function both increase the fraction of free drug (biologically active form), patients who have both conditions may be at greater risk of adverse effects. Therefore, it is recommended that such patients also be started on lower doses of ketoprofen capsules and closely monitored.
Rheumatoid Arthritis and Osteoarthritis
The recommended starting dose of ketoprofen capsules in otherwise healthy patients is 75 mg three times or 50 mg four times a day. Smaller doses of ketoprofen capsules should be utilized initially in small individuals or in debilitated or elderly patients. The recommended maximum daily dose of ketoprofen capsules is 300 mg/day.
Dosages higher than 300 mg/day of ketoprofen capsules are not recommended because they have not been studied. Concomitant use of ketoprofen capsules and ketoprofen extended-release capsules is not recommended. Relatively smaller people may need smaller doses.
As with other non-steroidal anti-inflammatory drugs, t he p redominant a dverse e ffects of ketoprofen are gastrointestinal. To attempt to minimize these effects, physicians may wish to prescribe that ketoprofen capsules be taken with antacids, food, or milk. Although food delays the absorption of ketoprofen capsules (see CLINICAL PHARMACOLOGY), in most of the clinical trials ketoprofen was taken with food or milk.
Physicians may want to make specific recommendations to patients about when they should take ketoprofen capsules in relation to food and/or what patients should do if they experience minor GI symptoms associated with ketoprofen capsules.
Management of Pain and Dysmenorrhea
The usual dose of ketoprofen capsules recommended for mild-to-moderate pain and dysmenorrhea is 25 to 50 mg every 6 to 8 hours as necessary. A smaller dose should be utilized initially in small individuals, in debilitated or elderly patients, or in patients with renal or liver disease (see PRECAUTIONS). A larger dose may be tried if the patient's response to a previous dose was less than satisfactory, but doses above 75 mg have not been shown to give added analgesia. Daily doses above 300 mg are not recommended because they have not been adequately studied. Because of its typical non-steroidal anti-inflammatory drug-side-effect profile, including as its principal adverse effect GI side effects (see WARNINGSand ADVERSE REACTIONS), higher doses of ketoprofen capsules should be used with caution and patients receiving them observed carefully.
HOW SUPPLIED
Kiprofen™ (Ketoprofen) Capsules are available as follows:
25 mg: Dark green color cap and body, size "4" imprinted with "KETO 25" on cap with an edible white ink and containing white to off-white crystalline powder supplied as:
| Bottles of 100 | NDC: 73352-504-10 |
50 mg: Light green color cap and body, size "1" imprinted with "KETO 50" on cap with an edible blue ink and containing white to off-white crystalline powder supplied as:
| Bottles of 100 | NDC: 73352-506-10 |
Medication Guide for Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Rx only
What is the most important information I should know about medicines called Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:
-
Increased risk of a heart attack or stroke that can lead to death.This risk may happen early in treatment and may increase:
- with increasing doses of NSAIDs
- with longer use of NSAIDs
Do not take NSAIDs right before or after a heart surgery called a "coronary artery bypass graft (CABG)."
Avoid taking NSAIDs after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack.
-
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
- anytime during use
- without warning symptoms
- that may cause death
The risk of getting an ulcer or bleeding increases with:
- past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs
- taking medicines called "corticosteroids" and "anticoagulants", "SSRIs", or "SNRIs"
- increasing doses of NSAIDS
- longer use of NSAIDs
- smoking
- drinking alcohol
- older age
- poor health
- advanced liver disease
- bleeding problems
NSAIDs should only be used:
- exactly as prescribed
- at the lowest dose possible for your treatment
- for the shortest time needed
What are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps and other types of short-term pain.
Who should not take NSAIDs?
Do not take NSAIDs:
- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs
- right before or after heart bypass surgery
Before taking NSAIDs, tell your healthcare provider about all of your medical conditions, including if you:
- have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant. Taking NSAIDs at about 20 weeks of pregnancy or later may harm your unborn baby. If you need to take NSAIDs for more than 2 days when you are between 20 and 30 weeks of pregnancy, your healthcare provider may need to monitor the amount of fluid in your womb around your baby. You should not take NSAID after about 30 weeks of pregnancy.
- are breastfeeding or plan to breast feed.
Tell your healthcare provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements.NSAIDs and some other medicines can interact with each other and cause serious side effects. Do not start taking any new medicine without talking to your healthcare provider first.
What are the possible side effects of NSAIDs?
NSAIDs can cause serious side effects, including:
See
"What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
- Other side effects of NSAIDs include:stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness
Get emergency help right away if you have any of the following symptoms:
- shortness of breath or trouble breathing
- chest pain
- weakness in one part or side of your body
- slurred speech
- swelling of the face or throat
Stop your NSAID medicine and call your healthcare provider right away if you have any of the following symptoms:
- nausea
- more tired or weaker than usual
- diarrhea
- itching
- your skin or eyes look yellow
- indigestion or stomach pain
- flu-like symptoms
- vomit blood
- there is blood in your bowel movement or it is black and sticky like tar
- unusual weight gain
- skin rash or blisters with fever
- swelling of the arms and legs, hands and feet
If you take too much of your NSAID, call your healthcare provider or get medical help right away.
These are not all the side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Other information about NSAIDs
- Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.
Manufactured for:
Trifluent Pharma
San Antonio, TX 78213
This Medication Guide has been approved by the U.S. Food and Drug Administration.
51UMS0000004US01
Revised: 1/2025
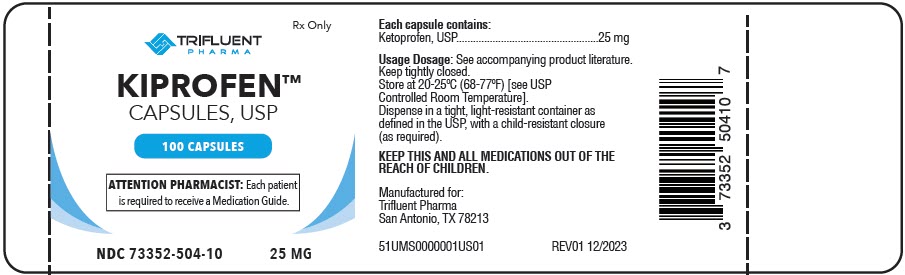
PRINCIPAL DISPLAY PANEL - 25 MG Capsule Bottle Label
TRIFLUENT
PHARMA™
Rx Only
KIPROFEN™
Ketoprofen Capsules, USP
100 CAPSULES
ATTENTION PHARMACIST: Each patient
is required to receive a Medication Guide.
NDC: 73352-504-10
25 MG
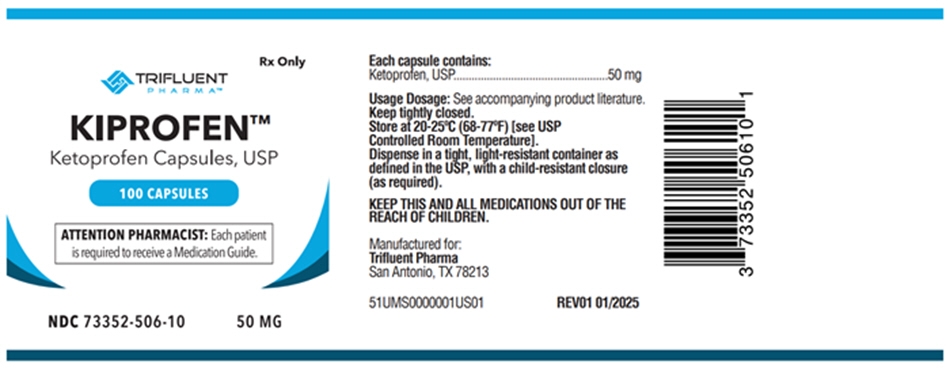
PRINCIPAL DISPLAY PANEL - 50 MG Capsule Bottle Label
TRIFLUENT
PHARMA™
Rx Only
KIPROFEN™
Ketoprofen Capsules, USP
100 CAPSULES
ATTENTION PHARMACIST: Each patient
is required to receive a Medication Guide.
NDC: 73352-506-10
50 MG
| KIPROFEN
ketoprofen capsule |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| KIPROFEN
ketoprofen capsule |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - Trifluent Pharma LLC (117167281) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Misemer Pharmaceuticals | 784121365 | label(73352-504, 73352-506) | |
Trademark Results [Kiprofen]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 KIPROFEN 98326068 not registered Live/Pending |
Real Value Products Corporation 2023-12-21 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.