TRANEXAMIC ACID injection, solution
tranexamic acid by
Drug Labeling and Warnings
tranexamic acid by is a Prescription medication manufactured, distributed, or labeled by Apollo Pharmaceuticals Inc.. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
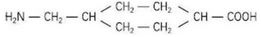
- DESCRIPTION
- FORMULATION
-
CLINICAL PHARMACOLOGY
Tranexamic acid is a competitive inhibitor of plasminogen activation, and at much higher concentrations, a noncompetitive inhibitor of plasmin, i.e., actions similar to aminocaproic acid. Tranexamic acid is about 10 times more potent in vitro than aminocaproic acid.
Tranexamic acid binds more strongly than aminocaproic acid to both the strong and weak receptor sites of the plasminogen molecule in a ratio corresponding to the difference in potency between the compounds. Tranexamic acid in a concentration of 1 mg per mL does not aggregate platelets in vitro.
Tranexamic acid, in concentrations as low as 1 mg per mL, can prolong the thrombin time. However, tranexamic acid in concentrations up to 10 mg per mL in blood showed no influence on the platelet count, the coagulation time, or other coagulation factors in whole blood or citrated blood from normal subjects.
The plasma protein binding of tranexamic acid is about 3% at therapeutic plasma levels and seems to be fully accounted for by its binding to plasminogen. Tranexamic acid does not bind to serum albumin.
After an intravenous dose of 1 g, the plasma concentration time curve shows a triexponential decay with a half-life of about 2 hours for the terminal elimination phase. The initial volume of distribution is about 9 to 12 liters. Urinary excretion is the main route of elimination via glomerular filtration. Overall renal clearance is equal to overall plasma clearance (110 to 116 mL/min), and more than 95% of the dose is excreted in the urine as unchanged drug. Excretion of tranexamic acid is about 90% at 24 hours after intravenous administration of 10 mg per kg body weight.
An antifibrinolytic concentration of tranexamic acid remains in different tissues for about 17 hours, and in the serum, up to seven or eight hours.
Tranexamic acid passes through the placenta. The concentration in cord blood after an intravenous injection of 10 mg per kg to pregnant women is about 30 mg per liter, as high as in the maternal blood. Tranexamic acid diffuses rapidly into joint fluid and the synovial membrane. In the joint fluid, the same concentration is obtained as in the serum. The biological half-life of tranexamic acid in the joint fluid is about three hours.
The concentration of tranexamic acid in a number of other tissues is lower than in blood. In breast milk, the concentration is about one hundredth of the serum peak concentration. Tranexamic acid concentration in cerebrospinal fluid is about one tenth of that of the plasma. The drug passes into the aqueous humor, the concentration being about one tenth of the plasma concentration.
Tranexamic acid has been detected in semen where it inhibits fibrinolytic activity but does not influence sperm migration. - INDICATIONS AND USAGE
-
CONTRAINDICATIONS
Tranexamic Acid Injection is contraindicated:
1. In patients with acquired defective color vision, since this prohibits measuring one endpoint that should be followed as a measure of toxicity (see WARNINGS).
2. In patients with subarachnoid hemorrhage. Anecdotal experience indicates that cerebral edema and cerebral infarction may be caused by Tranexamic Acid Injection in such patients.
3. In patients with active intravascular clotting.
4. In patients with hypersensitivity to tranexamic acid or any of the ingredients. -
WARNINGS
Focal areas of retinal degeneration have developed in cats, dogs, and rats following oral or intravenous tranexamic acid at doses between 250 to 1600 mg/kg/day (6 to 40 times the recommended usual human dose) from 6 days to 1 year. The incidence of such lesions has varied from 25% to 100% of animals treated and was dose-related. At lower doses, some lesions have appeared to be reversible.
Limited data in cats and rabbits showed retinal changes in some animals with doses as low as 126 mg/kg/day (only about 3 times the recommended human dose) administered for several days to two weeks.
No retinal changes have been reported or noted in eye examinations in patients treated with tranexamic acid for weeks to months in clinical trials.
However, visual abnormalities, often poorly characterized, represent the most frequently reported postmarketing adverse reaction in Sweden. For patients who are to be treated continually for longer than several days, an ophthalmological examination, including visual acuity, color vision, eye-ground, and visual fields, is advised, before commencing and at regular intervals during the course of treatment. Tranexamic acid should be discontinued if changes in examination results are found.
Convulsions have been reported in association with tranexamic acid treatment, particularly in patients receiving tranexamic acid during cardiovascular surgery and in patients inadvertently given tranexamic acid into the neuraxial system.
Cases of allergic reaction with use of intravenous tranexamic acid, including anaphylaxis or anaphylactoid reaction have been reported that are suggestive of a causal relationship. -
PRECAUTIONS
General
The dose of Tranexamic Acid Injection should be reduced in patients with renal insufficiency because of the risk of accumulation (see DOSAGE AND ADMINISTRATION).
Ureteral obstruction due to clot formation in patients with upper urinary tract bleeding has been reported in patients treated with Tranexamic Acid Injection.
Venous and arterial thrombosis or thromboembolism has been reported in patients treated with Tranexamic Acid Injection. In addition, cases of central retinal artery and central retinal vein obstruction have been reported.
Patients with a previous history of thromboembolic disease may be at increased risk for venous or arterial thrombosis.
Tranexamic Acid Injection should not be administered concomitantly with Factor IX Complex concentrates or Anti-inhibitor Coagulant concentrates, as the risk of thrombosis may be increased.
Patients with disseminated intravascular coagulation (DIC), who require treatment with Tranexamic Acid Injection, must be under strict supervision of a physician experienced in treating this disorder.
Tranexamic acid may cause dizziness and therefore may influence the ability to drive or use machines.Drug Interactions
No studies of interactions between Tranexamic Acid Injection and other drugs have been conducted.
Carcinogenesis, Mutagenesis, Impairment of Fertility
An increased incidence of leukemia in male mice receiving tranexamic acid in food at a concentration of 4.8% (equivalent to doses as high as 5 g/kg/day) may have been related to treatment. Female mice were not included in this experiment.
Hyperplasia of the biliary tract and cholangioma and adenocarcinoma of the intrahepatic biliary system have been reported in one strain of rats after dietary administration of doses exceeding the maximum tolerated dose for 22 months. Hyperplastic, but not neoplastic, lesions were reported at lower doses. Subsequent long-term dietary administration studies in a different strain of rat, each with an exposure level equal to the maximum level employed in the earlier experiment, have failed to show such hyperplastic / neoplastic changes in the liver. No mutagenic activity has been demonstrated in several in vitro and in vivo test systems.
There are no clinical data to assess the effects of tranexamic acid on fertility.Pregnancy
Reproduction studies performed in mice, rats, and rabbits have not revealed any evidence of impaired fertility or adverse effects on the fetus due to tranexamic acid.
There are no adequate and well-controlled studies in pregnant women. However, tranexamic acid is known to pass the placenta and appears in cord blood at concentrations approximately equal to maternal concentration. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.Nursing Mothers
Tranexamic acid is present in the mother's milk at a concentration of about a hundredth of the corresponding serum levels. Caution should be exercised when Tranexamic Acid Injection is administered to a nursing woman.
Pediatric Use
The drug has had limited use in pediatric patients, principally in connection with tooth extraction. The limited data suggest that dosing instructions for adults can be used for pediatric patients needing Tranexamic Acid Injection therapy.
Geriatric Use
Clinical studies of Tranexamic Acid Injection did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION). -
ADVERSE REACTIONS
Gastrointestinal disturbances (nausea, vomiting, diarrhea) may occur but disappear when the dosage is reduced. Allergic dermatitis, giddiness, and hypotension have been reported occasionally. Hypotension has been observed when intravenous injection is too rapid. To avoid this response, the solution should not be injected more rapidly than 1 mL per minute.
Worldwide Postmarketing Reports
Thromboembolic events (e.g., deep vein thrombosis, pulmonary embolism, cerebral thrombosis, acute renal cortical necrosis, and central retinal artery and vein obstruction) have been rarely reported in patients receiving tranexamic acid for indications other than hemorrhage prevention in patients with hemophilia. Convulsion, chromatopsia, and visual impairment have also been reported. However, due to the spontaneous nature of the reporting of medical events and the lack of controls, the actual incidence and causal relationship of drug and event cannot be determined. Anaphylaxis or anaphylactoid reaction have been reported that are suggestive of a causal relationship (see WARNINGS).
-
OVERDOSAGE
Cases of overdosage of Tranexamic Acid Injection have been reported. Based on these reports, symptoms of overdosage may be gastrointestinal, e.g., nausea, vomiting, diarrhea; hypotensive, e.g., orthostatic symptoms; thromboembolic, e.g., arterial, venous, embolic; neurologic, e.g., visual impairment, convulsions, headache, mental status changes; myoclonus; and rash.
-
DOSAGE AND ADMINISTRATION
Immediately before tooth extraction in patients with hemophilia, administer 10 mg per kg body weight of Tranexamic Acid Injection intravenously together with replacement therapy (see PRECAUTIONS). Following tooth extraction, intravenous therapy, at a dose of 10 mg per kg body weight three to four times daily, may be used for 2 to 8 days.
Note: For patients with moderate to severe impaired renal function, the following dosages are recommended:Serum Creatinine (µmol/L) Tranexamic Acid Intravenous Dosage 120 to 250 (1.36 to 2.83 mg/dL) 10 mg/kg twice daily 250 to 500 (2.83 to 5.66 mg/dL) 10 mg/kg daily 10 mg/kg every 48 hours >500 (>5.66 mg/dL) or 5 mg/kg every 24 hours For intravenous infusion, Tranexamic Acid Injection may be mixed with most solutions for infusion such as electrolyte solutions, carbohydrate solutions, amino acid solutions, and Dextran solutions. Heparin may be added to Tranexamic Acid Injection. Tranexamic Acid Injection should NOT be mixed with blood. The drug is a synthetic amino acid, and should NOT be mixed with solutions containing penicillin.
- HOW SUPPLIED
- STORAGE
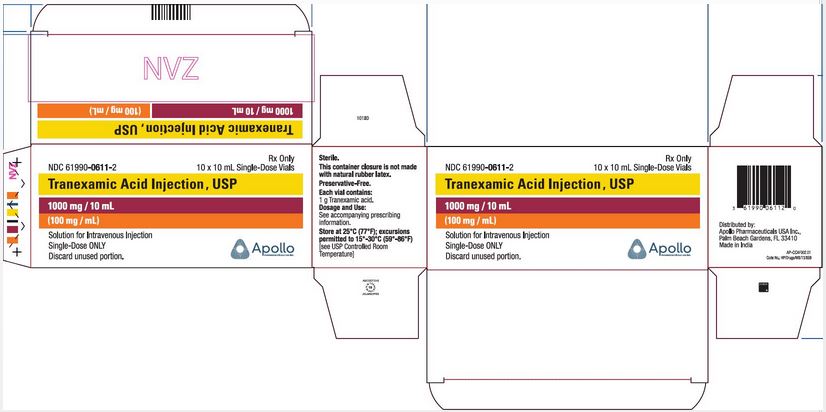
- PRINCIPLE DISPLAY PANEL - 10 x 10 mL Carton Label
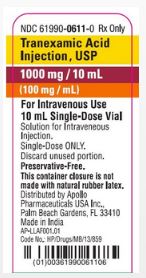
- PRINCIPLE DISPLAY PANEL - 10 mL Single-Dose Vial
-
INGREDIENTS AND APPEARANCE
TRANEXAMIC ACID
tranexamic acid injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 61990-0611 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TRANEXAMIC ACID (UNII: 6T84R30KC1) (TRANEXAMIC ACID - UNII:6T84R30KC1) TRANEXAMIC ACID 100 mg in 1 mL Inactive Ingredients Ingredient Name Strength WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 61990-0611-2 10 in 1 CARTON 09/30/2019 1 NDC: 61990-0611-0 10 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA212676 09/30/2019 Labeler - Apollo Pharmaceuticals Inc. (202959730)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.