METHENAMINE MANDELATE tablet, film coated
Methenamine Mandelate by
Drug Labeling and Warnings
Methenamine Mandelate by is a Prescription medication manufactured, distributed, or labeled by Method Pharmaceuticals, LLC. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Methenamine mandelate, USP, a urinary antibacterial agent, is the chemical combination of mandelic acid with methenamine. Methenamine mandelate, USP is available for oral use as film-coated tablets.
Methenamine mandelate tablets, USP contain 500 mg methenamine mandelate and the following inactive ingredients: microcrystalline cellulose, croscarmellose sodium, silicon dioxide, magnesium stearate, FD&C Blue #2, polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide.
-
CLINICAL PHARMACOLOGY
Methenamine mandelate, USP is readily absorbed but remains essentially inactive until it is excreted by the kidneys and concentrated in the urine. An acid urine is essential for antibacterial action, with maximum efficacy occurring at pH 5.5 or less. In an acid urine, mandelic acid exerts its antibacterial action and also contributes to the acidification of the urine. Mandelic acid is excreted both by glomerular filtration and tubular excretion. The methenamine component is hydrolyzed in acid urine to ammonia and to the bactericidal agent formaldehyde.
Proportionally less formaldehyde is released as urinary pH approaches 6.0 and insufficient quantities are released above this level for therapeutic response. There is equally effective antibacterial activity against both gram-positive and gram-negative organisms, since the antibacterial action of mandelic acid and formaldehyde is nonspecific. There are reports that methenamine mandelate, USP is ineffective in some infections with Proteus vulgaris and urea-splitting strains of Pseudomonas aeruginosa and A aerogenes. Since urea-splitting strains may raise the pH of the urine, particular attention to supplementary acidification is required. However, results in any single case will depend to a large extent on the underlying pathology and the overall management.
-
INDICATIONS AND USAGE
Methenamine mandelate, USP is indicated for the suppression or elimination of bacteriuria associated with pyelonephritis, cystitis, and other chronic urinary tract infections; also those neurologic diseases leading to an infected residual urine. When used as recommended, methenamine mandelate, USP is particularly suitable for long-term therapy because of its safety and because resistance to the nonspecific bactericidal action of formaldehyde does not develop. Pathogens resistant to other antibacterial agents may respond to methenamine mandelate, USP because of the nonspecific effect of formaldehyde formed in an acid urine.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of methenamine mandelate, USP and other antibacterial drugs, methenamine mandelate, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria.
Prophylactic Use Rationale: Urine is a good culture medium for many urinary pathogens. Inoculation by a few organisms (relapse or reinfection) may lead to bacteriuria in susceptible individuals. Thus, the rationale of management in recurring urinary tract infection (bacteriuria) is to change the urine from a growth-supporting to a growth-inhibiting medium. There is a growing body of evidence that long-term administration of methenamine mandelate, USP can prevent the recurrence of bacteriuria in patients with chronic pyelonephritis.
Therapeutic Use Rationale: Methenamine mandelate, USP helps to sterilize the urine, and in some situations in which underlying pathologic conditions prevent sterilization by any means, it can help to suppress the bacteriuria. Methenamine mandelate, USP should not be used alone for acute infections with parenchymal involvement causing systemic symptoms such as chills and fever. A thorough diagnostic investigation as a part of the overall management of the urinary tract infection should accompany the use of methenamine mandelate, USP.
- CONTRAINDICATIONS
-
WARNINGS
Methenamine mandelate, USP should be avoided in patients with gout because it may precipitate urate crystals in their urine. A similar situation may arise in patients with a predisposition to the formation of uric acid stones.
Methenamine preparations should not be given to patients taking sulfonamides because some sulfonamides may form an insoluble precipitate with formaldehyde in the urine.
-
PRECAUTIONS
General
Dysuria may occur (usually at higher than recommended dosage). This can be controlled by reducing the dosage and the acidification. When urine acidification is contraindicated or unattainable (as with some urea-splitting bacteria), the drug is not recommended.
Large doses of methenamine (8 g daily for 3 to 4 weeks) have caused bladder irritation, painful and frequent micturition, albuminuria, and gross hematuria.
Information for Patients
To assure an acidic pH, patients should be instructed to restrict or avoid milk products and antacids containing sodium carbonate or bicarbonate.
Laboratory Tests
As with all urinary tract infections, the efficacy of therapy should be monitored by repeated urine cultures. Urinary pH monitoring is required to assure an acidic
urinary pH (below 5.5).
Drug Interactions
Formaldehyde and sulfamethizole form an insoluble precipitate in acid urine; therefore, methenamine mandelate, USP should not be administered concurrently with sulfamethizole or other sulfonamides. Concurrent use of salicylates may lead to increased serum salicylate levels since excretion of salicylates is reduced in acidified urine.
Drug/Laboratory Test Interactions
Formaldehyde interferes with fluorometric procedures for determination of urinary catecholamines and vanillylmandelic acid (VMA), causing erroneously high results. Formaldehyde also causes falsely decreased urine estriol levels by reacting with estriol when acid hydrolysis techniques are used; estriol determinations which use enzymatic hydrolysis are unaffected by formaldehyde.
Formaldehyde causes falsely elevated 17-hydroxycorticosteroid levels when the Porter-Silber method is used and falsely decreased 5-hydroxyindoleacetic acid (5HIAA) levels by inhibiting color development when nitrosonaphthol methods are used.
CARCINOGENESIS AND MUTAGENESIS
Methenamine was evaluated for mutagenicity in the Ames Salmonella/mammalian microsome test. Five strains of Salmonella typhimurium (TA98, TA100, TA1535, TA1537 and TA1538) and a strain of Escherichia coli (WP2uvrA) were used. At a dose of 10,000 ug/plate methenamine showed mutagenic activity in Salmonella typhimurium TA98 and TA100 by metabolic activation and also showed mutagenic activity in TA98 without microsomal activation.
In one large study, no evidence of carcinogenicity was found following long-term oral administration of methenamine 1.25 g/kg/day to rats (104 weeks) and mice (60 weeks).
Pregnancy
Teratogenic Effects. Pregnancy Category C.
Animal reproduction studies have not been conducted with methenamine mandelate, USP. It is also not known whether methenamine mandelate, USP can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Since methenamine is known to cross the placental barrier, methenamine mandelate, USP should be given to a pregnant woman only if the potential benefit outweighs the risk.
- ADVERSE REACTIONS
- OVERDOSAGE
- DOSAGE AND ADMINISTRATION
-
HOW SUPPLIED
Methenamine Mandelate Tablets, USP 500 mg are blue, oval, film-coated, debossed with “M460”. Supplied in bottles of 100 (NDC: 58657-460-01)
Dispense in a tight, light-resistant container as defined in the USP.
Store at 25°C (77°F); excursions permitted between 15°-30°C (59°-86°F). [See USP Controlled Room Temperature.]
Rx only
Marketed by:
Method Pharmaceuticals, LLC
Fort Worth, TX 76118
1-877-250-3427Rev. 06/18
-
PRINCIPAL DISPLAY PANEL
NDC: 58657-460-01
Methenamine
Mandelate
Tablets USP
URINARY ANTIBACTERIAL
500 mg
Rx Only
100 Tablets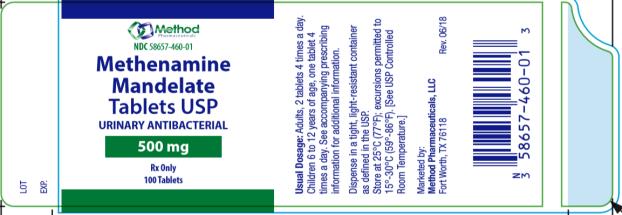
-
INGREDIENTS AND APPEARANCE
METHENAMINE MANDELATE
methenamine mandelate tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC: 58657-460 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METHENAMINE MANDELATE (UNII: 695N30CINR) (METHENAMINE - UNII:J50OIX95QV) METHENAMINE MANDELATE 500 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) SILICON DIOXIDE (UNII: ETJ7Z6XBU4) MAGNESIUM STEARATE (UNII: 70097M6I30) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) POLYETHYLENE GLYCOL, UNSPECIFIED (UNII: 3WJQ0SDW1A) POLYVINYL ALCOHOL, UNSPECIFIED (UNII: 532B59J990) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) Product Characteristics Color blue Score no score Shape OVAL Size 15mm Flavor Imprint Code M460 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC: 58657-460-01 100 in 1 BOTTLE; Type 0: Not a Combination Product 07/19/2018 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date unapproved drug other 07/19/2018 Labeler - Method Pharmaceuticals, LLC (060216698)
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.