TRIFENA™ PATCH – Diclofenac Sodium, Lidocaine, Menthol Patch Trifluent Pharma, LLC
Trifena by
Drug Labeling and Warnings
Trifena by is a Prescription medication manufactured, distributed, or labeled by Trifluent Pharma LLC, Dr Sabharwals Wound Care. Drug facts, warnings, and ingredients follow.
Drug Details [pdf]
TRIFENA- diclofenac, lidocaine, menthol patch
Trifluent Pharma LLC
Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here.
----------
TRIFENA™ PATCH – Diclofenac Sodium, Lidocaine, Menthol Patch
Trifluent Pharma, LLC
Trifena™ Patch - Diclofenac Sodium, Lidocaine, Menthol
Trifena™ Topical Patch
(Diclofenac Sodium, USP 1.2%, Lidocaine, USP 4%, Menthol, USP 5%)
Rx only
WARNING: RISK OF SERIOUS CARDIOVASCULAR AND GASTROINTESTINAL EVENTS
Cardiovascular Risk
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs) may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS) . Trifena™ patch is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see CONTRAINDICATIONSand WARNINGS) .
Gastrointestinal Risk
- NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events (See PRECAUTIONSand WARNINGS) .
DESCRIPTION
Trifena™ patch (Diclofenac Sodium, USP 1.2%; Lidocaine, USP 4%; Menthol, USP 5%) is a topical pain relief patch comprised of adhesive material containing local pain reliever 1.2% diclofenac sodium, local anesthetic lidocaine 4%, and local analgesic menthol 5%.
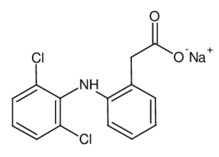
Diclofenac sodium, USP is a benzeneacetic acid derivative, designated chemically as 2-[(2,6- dichlorophenyl)amino] benzeneacetic acid, monosodium salt. The structural formula is:
Lidocaine, USP, is chemically designated as acetamide, 2-(diethylamino)-N-(2,6-dimethylphenyl), has an octanol:water partition ratio of 43 at pH 7.4, and has the following structure:

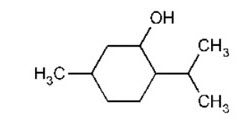
Menthol, USP, is chemically designated as 2--‐Isopropyl--‐5--‐methylcyclohexanol. It contains colorless, hexagonal crystals, usually needle--‐like; fused masses or crystalline powder with a pleasant, peppermint--‐like odor. It has a melting point between 31°C to 36° C. The structural formula is:
Each adhesive patch contains 1.2% w/w of Diclofenac Sodium (132 mg), 4.0% w/w of Lidocaine (440 mg), and 5.0% w/w of Menthol (550 mg) [of adhesive].
Inactive Ingredients: Alpha Tocopherol Acetate, Aluminum Glycinate, Aluminum Hydroxide, Borax, Carbomer, Colloidal Silicon Dioxide, DMDM Hydantoin, Glycerin, Polyacrylic Acid, Polyvinyl Alcohol, Polyvinylpyrrolidone, Propylene Glycol, Purified Water, Sodium Carboxymethyl Cellulose, Sodium Ethylenediaminetetraacetic Acid (EDTA), Sodium Polyacrylate, Sorbitan Monooleate, Tartaric Acid, and Titanium Dioxide.
CLINICAL PHARMACOLOGY
Diclofenac has analgesic, anti-inflammatory, and antipyretic properties. The mechanism of action of diclofenac sodium, like that of other NSAIDs, is not completely understood but involves inhibition of cyclooxygenase (COX-1 and COX-2).
Lidocaine is a topical anesthetic and stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of impulses, thereby effecting local anesthetic action.
Menthol has local anesthetic and counterirritant qualities. It also acts as a weak kappa (ĸ) opioid receptor agonist. Menthol chemically triggers the cold-‑‐sensitive TRPM-‑‐8 receptors in the skin, which are responsible for the well-‑‐documented cooling sensation that occurs when applied to the skin. Menthol's analgesic properties are not fully understood; however, they are mediated through a selective activation of ĸ-‑‐opioid receptors. Menthol also blocks voltage-‑‐sensitive sodium channels, reducing neural activity that may stimulate muscle tissue.
Pharmacodynamics
Trifena™ patch applied to intact skin provides local analgesia by releasing diclofenac sodium, lidocaine, and menthol from the patch into the skin.
Diclofenac is a potent inhibitor of prostaglandin synthesis in vitro. Diclofenac concentrations reached during therapy have produced in vivo effects. Prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain in animal models. Prostaglandins are mediators of inflammation. Because diclofenac is an inhibitor of prostaglandin synthesis, its mode of action may be due to a decrease of prostaglandins in peripheral tissues.
Lidocaine is an amide--‐type local anesthetic agent and is suggested to stabilize neuronal membranes by inhibiting the ionic fluxes required for the initiation and conduction of impulses. The penetration of lidocaine into intact skin after application of Trifena™ patch is sufficient to produce analgesic effect, but less than the amount necessary to produce a complete sensory block.
Menthol works by targeting the k--‐opioid receptor on the TRPM8 neuron. The TRPM8 neuron is normally activated at temperatures between (8° --‐ 28° C). Menthol causes the neuron to fire at temperatures above normal activation, which triggers the characteristic cooling sensation. Also because of Menthol's specific targeting of the k--‐opioid receptor, it is endowed with analgesic properties.
Pharmacokinetics
Absorption
The amount of diclofenac sodium, lidocaine, and menthol systemically absorbed from Trifena™ patch is directly related to both the duration of application and the surface area over which it is applied.
After administration of diclofenac sodium topical solution (40 mg/knee every 12 h; total daily diclofenac exposure: 80 mg/knee) for 7.5 days, the mean (SD) AUC 0-12and mean (SD) C maxwere 77.27 (49.89) ng∙h/mL and 12.16 (7.66) ng/mL, respectively, on Day 1; and 204.58 (111.02) ng∙h/mL and 25.24 (12.95) ng/mL, respectively, at steady state on Day 8. After administration of diclofenac sodium 1.5% (19.3mg/knee every 6 h; total daily diclofenac exposure 77.2 mg/knee), the mean (SD) AUC 0-12and mean (SD) C maxwere 27.46 (23.97) ng∙h/mL and 2.30 (2.02) ng/mL, respectively, on Day 1; and 141.49 (92.47) ng∙h/mL and 17.04 (11.28) ng/mL, respectively, at steady state on Day 8.
The pharmacokinetics and effect of diclofenac sodium were not evaluated under the conditions of heat application, occlusive dressings overlay, or exercise following product application. Therefore, concurrent use of diclofenac sodium under these conditions is not recommended.
When Trifena™ patch is applied topically, diclofenac sodium is absorbed into the epidermis. The systematic bioavailability after topical application of diclofenac sodium is lower than after oral dosing.
In a pharmacokinetic study, three lidocaine patches were applied over an area of 420 cm 2of intact skin on the back of normal volunteers for 12 hours. Blood samples were withdrawn for determination of lidocaine concentration during the application and for 12 hours after removal of patches. The results are summarized in Table 1.
| Lidocaine Patch | Application Site | Area
(cm 2) | Dose Absorbed
(mg) | C
max
(mcg/mL) | T
max
(hr) |
|---|---|---|---|---|---|
| 3 patches (2100 mg) | Back | 420 | 64 ± 32 | 0.13 ± 0.06 | 11 hr |
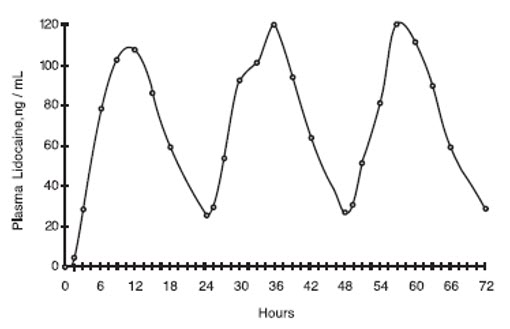
When lidocaine patch is used according to the recommended dosing instructions, only 3 ± 2% of the dose applied is expected to be absorbed. At least 95% (665 mg) of lidocaine will remain in a used patch. Mean peak blood concentration of lidocaine is about 0.13 mcg/mL (about 1/10 of the therapeutic concentration required to treat cardiac arrhythmias). Repeated application of three patches simultaneously for 12 hours (recommended maximum daily dose), once per day for three days, indicated that the lidocaine concentration does not increase with daily use. The mean plasma pharmacokinetic profile for the 15 healthy volunteers is shown in Figure 1.
Figure 1
Mean lidocaine blood concentrations after three consecutive daily applications of three lidocaine patches simultaneously for 12 hours per day in healthy volunteers (n =15).
Distribution
Diclofenac is more than 99% bound to human serum proteins, primarily to albumin.
Diclofenac diffuses into and out of the synovial fluid. Diffusion into the joint occurs when plasma levels are higher than those in the synovial fluid, after which the process reverses and synovial fluid levels are higher than plasma levels. It is not known whether diffusion into the joint plays a role in the effectiveness of diclofenac.
When Lidocaine is administered intravenously to healthy volunteers, the volume of distribution is 0.7 to 2.7 L/kg (mean 1.5 ± 0.6 SD, n = 15). At concentrations produced by application of Trifena™ patch, approximately 70% of the lidocaine dose is reported to be bound to plasma proteins, primarily alpha-1-acid glycoprotein. At much higher plasma concentrations (1 to 4 mcg/mL of free base), the plasma protein binding of lidocaine is concentration dependent. Lidocaine crosses the placental and blood brain barriers, presumably by passive diffusion.
Metabolism
It is not known if Trifena™ patch is metabolized in the skin.
Metabolism of diclofenac sodium following topical administration is thought to be similar to that after oral administration. The small amounts of diclofenac sodium and its metabolites appearing in the plasma following topical administration makes the quantification of specific metabolites imprecise.
Five diclofenac metabolites have been identified in human plasma and urine. The metabolites include 4'-hydroxy-, 5-hydroxy-, 3'-hydroxy-, 4',5-dihydroxy- and 3'-hydroxy-4'-methoxy diclofenac. The major diclofenac metabolite, 4'-hydroxy-diclofenac, has very weak pharmacologic activity. The formation of 4'-hydroxy diclofenac is primarily mediated by CYP2C9. Both diclofenac and its oxidative metabolites undergo glucuronidation or sulfation followed by biliary excretion. Acyl glucuronidation mediated by UGT2B7 and oxidation mediated by CYP2C8 may also play a role in diclofenac metabolism. CYP3A4 is responsible for the formation of minor metabolites, 5-hydroxy and 3'-hydroxy-diclofenac.
Lidocaine is metabolized rapidly by the liver to a number of metabolites, including menoethylglycinexylidie (MEGX) and glycinexylidide (GX), both of which have pharmacologic activity similar to, but less potent than that of Lidocaine. A minor metabolite, 2,6--‐xylidine, has unknown pharmacologic activity but is carcinogenic in rats. The blood concentration of this metabolite is negligible following application of Lidocaine Patch 5%. Following intravenous administration, MEGX and GX concentrations in serum range from 11% to 36% and from 5% to 11% of Lidocaine concentrations, respectively.
Humans rapidly metabolize Menthols primarily in the liver by the microsomes, using the enzyme CYP2A6. Cytochrome P450--‐mediated oxidation occurs in humans, yielding various alcohol and hydroxy acid derivatives. These are eliminated in the urine unchanged or conjugated with glucuronic acid.
Excretion
Diclofenac is eliminated through metabolism and subsequent urinary and biliary excretion of the glucuronide and the sulfate conjugates of the metabolites. Little or no free unchanged diclofenac is excreted in the urine.
Lidocaine and its metabolites are excreted by the kidneys. Less than 10% of lidocaine is excreted unchanged. The half-life of lidocaine elimination from the plasma following IV administration is 81 to 149 minutes (mean 107 ± 22 SD, n = 15). The systemic clearance is 0.33 to 0.90 L/min (mean 0.64 ± 2 max max 0.18 SD, n = 15).
Menthols are largely eliminated as glucuronides. In an experiment, 79% of a 1g (Quick, 1928) and 78% of a 10--‐20mg (Atzl et al., 1972) oral dose of Menthol was eliminated as the glucuronic acid conjugate within 6 h after administration to volunteers. Of a dose of 47 mg/kg bw [3--‐3H]--‐(--‐)--‐Menthol, 82% was eliminated in the urine 17 hours after administration. Smaller amounts were distributed in the feces and ileum; only 1% of the activity remained in the liver (Clegg et al., 1982).
INDICATIONS AND USAGE
Trifena™ patch is indicated for the temporary relief of pain associated with arthritis, backache, cramps, discomfort, neck ache, soreness, sprains, strains. It should be applied only to intact skin.
Sun avoidance is indicated during therapy.
CONTRAINDICATIONS
Trifena™ patch is contraindicated in patients with known hypersensitivity to diclofenac.
Trifena™ patch should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients (see WARNINGS – Anaphylactic Reactions, and PRECAUTIONS - Preexisting Asthma) .
Trifena™ patch is contraindicated in patients with a known history of sensitivity to local anesthetics of the amide type, or to any other component of the product.
Trifena™ patch is contraindicated in patients in the setting of coronary artery bypass graft (CABG) surgery.
Trifena™ patch should not be applied to non-intact or damaged skin resulting from any etiology e.g. exudative dermatitis, eczema, infected lesion, burns or wounds.
Medicines intended to be applied to the skin should not be swallowed.
Trifena™ patch is flammable. Keep away from open flame.
You should never heat, microwave, or add the medicine to hot water.
WARNINGS
Risk of Serious Cardiovascular Events
Cardiovascular Thrombotic Events
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Patients should be informed about the signs and/or symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID does increase the risk of serious GI events (see WARNINGS – Gastrointestinal Bleeding, Ulceration, and Perforation) .
Two large, controlled, clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10-14 days following CABG surgery found an increased incidence of myocardial infarction and stroke (see CONTRAINDICATIONS).
Gastrointestinal Bleeding, Ulceration, and Perforation
NSAIDs, including diclofenac, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3-6 months, and in about 2-4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
Risk Factors for GI Bleeding, Ulceration, and Perforation
Patients with a prior history of peptic ulcer disease and/or GI bleeding who used NSAIDs had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include longer duration of NSAID therapy; concomitant use of oral corticosteroids, aspirin, anticoagulants, or selective serotonin reuptake inhibitors (SSRIs); smoking; use of alcohol; older age; and poor general health status. Most postmarketing reports of fatal GI events occurred in elderly or debilitated patients. Additionally, patients with advanced liver disease and/or coagulopathy are at increased risk for GI bleeding.
Strategies to Minimize the GI Risks in NSAID-treated patients
- Use the lowest effective dosage for the shortest possible duration.
- Avoid administration of more than one NSAID at a time.
- Avoid use in patients at higher risk unless benefits are expected to outweigh the increased risk of bleeding. For such patients, as well as those with active GI bleeding, consider alternate therapies other than NSAIDs.
- Remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy.
- If a serious GI adverse event is suspected, promptly initiate evaluation and treatment, and discontinue diclofenac sodium until a serious GI adverse event is ruled out.
- In the setting of concomitant use of low-dose aspirin for cardiac prophylaxis, monitor patients more closely for evidence of GI bleeding (see Drug Interactions) .
Hepatotoxicity
In clinical trials of oral diclofenac containing products, meaningful elevations (i.e., more than 3 times the ULN) of AST (SGOT) occurred in about 2% of approximately 5,700 patients at some time during diclofenac treatment (ALT was not measured in all studies).
In a large, open-label, controlled trial of 3,700 patients treated with oral diclofenac for 2 - 6 months, patients were monitored first at 8 weeks and 1,200 patients were monitored again at 24 weeks. Meaningful elevations of ALT and/or AST occurred in about 4% of 3,700 patients and included marked elevations (greater than 8 times the ULN) in about 1% of the 3,700 patients. In that open-label study, a higher incidence of borderline (less than3 times the ULN), moderate (3 to 8 times the ULN), and marked (greater than 8 times the ULN) elevations of ALT or AST was observed in patients receiving diclofenac when compared to other NSAIDs. Elevations in transaminases were seen more frequently in patients with osteoarthritis than in those with rheumatoid arthritis.
Almost all meaningful elevations in transaminases were detected before patients became symptomatic. Abnormal tests occurred during the first 2 months of therapy with oral diclofenac in 42 of the 51 patients in all trials who developed marked transaminase elevations.
In postmarketing reports, cases of drug-induced hepatotoxicity have been reported in the first month, and in some cases, the first 2 months of NSAID therapy, but can occur at any time during treatment with diclofenac.
Postmarketing surveillance has reported cases of severe hepatic reactions, including liver necrosis, jaundice, fulminant hepatitis with and without jaundice, and liver failure. Some of these reported cases resulted in fatalities or liver transplantation.
In a European retrospective population-based, case-controlled study, 10 cases of oral diclofenac associated drug-induced liver injury with current use compared with non-use of diclofenac were associated with a statistically significant 4-fold adjusted odds ratio of liver injury. In this particular study, based on an overall number of 10 cases of liver injury associated with diclofenac, the adjusted odds ratio increased further with female gender, doses of 150 mg or more, and duration of use for more than 90 days.
Physicians should measure transaminases at baseline and periodically in patients receiving long-term therapy with diclofenac, because severe hepatotoxicity may develop without a prodrome of distinguishing symptoms. The optimum times for making the first and subsequent transaminase measurements are not known. Based on clinical trial data and postmarketing experiences, transaminases should be monitored within 4 to 8 weeks after initiating treatment with diclofenac. However, severe hepatic reactions can occur at any time during treatment with diclofenac.
If abnormal liver tests persist or worsen, if clinical signs and/or symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, abdominal pain, diarrhea, dark urine, etc.), diclofenac sodium should be discontinued immediately.
Inform patients of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, diarrhea, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), discontinue diclofenac sodium immediately, and perform a clinical evaluation of the patient.
To minimize the potential risk for an adverse liver-related event in patients treated with diclofenac sodium, use the lowest effective dose for the shortest duration possible. Exercise caution when prescribing diclofenac sodium with concomitant drugs that are known to be potentially hepatotoxic (e.g., acetaminophen, antibiotics, anti-epileptics).
Hypertension
NSAIDs, including diclofenac sodium, can lead to new onset of hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking angiotensin converting enzyme (ACE) inhibitors, thiazides diuretics, or loop diuretics may have impaired response to these therapies when taking NSAIDs (see PRECAUTIONS: Drug Interactions) .
Monitor blood pressure (BP) during the initiation of NSAID treatment and throughout the course of therapy.
Heart Failure and Edema
The Coxib and traditional NSAID Trialists' Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalization for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of diclofenac may blunt the CV effects of several therapeutic agents used to treat these medical conditions (e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers [ARBs]) (see PRECAUTIONS: Drug Interactions) .
Avoid the use of diclofenac in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If diclofenac is used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
Renal Toxicity and Hyperkalemia
Renal Toxicity
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury.
Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors or ARBs, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
No information is available from controlled clinical studies regarding the use of diclofenac sodium in patients with advanced renal disease. The renal effects of diclofenac sodium may hasten the progression of renal dysfunction in patients with pre-existing renal disease.
Correct volume status in dehydrated or hypovolemic patients prior to initiating diclofenac sodium. Monitor renal function in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia during use of diclofenac sodium delayed-release tablets (see PRECAUTIONS: Drug Interactions) . Avoid the use of diclofenac sodium in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function. If diclofenac sodium is used in patients with advanced renal disease, monitor patients for signs of worsening renal function.
Anaphylactic Reactions
Diclofenac has been associated with anaphylactic reactions in patients with and without known hypersensitivity to diclofenac and in patients with aspirin-sensitive asthma ( see CONTRAINDICATIONS, WARNINGS: Exacerbation of Asthma Related to Aspirin Sensitivity).
Exacerbation of Asthma Related to Aspirin Sensitivity
A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps; severe, potentially fatal bronchospasm; and/or intolerance to aspirin and other NSAIDs. Because cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, diclofenac sodium are contraindicated in patients with this form of aspirin sensitivity (see CONTRAINDICATIONS). When diclofenac sodium are used in patients with preexisting asthma (without known aspirin sensitivity), monitor patients for changes in the signs and symptoms of asthma.
Serious Skin Reactions
NSAIDs, including diclofenac, can cause serious skin adverse reactions such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Inform patients about the signs and symptoms of serious skin reactions, and to discontinue the use of diclofenac sodium at the first appearance of skin rash or any other sign of hypersensitivity. Diclofenac sodium is contraindicated in patients with previous serious skin reactions to NSAIDs (See CONTRAINDICATIONS) .
Do not apply diclofenac sodium to open skin wounds, infections, inflammations, or exfoliative dermatitis, as it may affect absorption and tolerability of the drug.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) has been reported in patients taking NSAIDs such as diclofenac sodium. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, reaction, lymphadenopathy, and/or facial swelling. Other clinical manifestations may include hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis. Sometimes symptoms of DRESS may resemble an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its presentation, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though reaction is not evident. If such signs or symptoms are present, discontinue diclofenac sodium and evaluate the patient immediately.
Fetal Toxicity
Premature Closure of Fetal Ductus Arteriosus
Avoid use of NSAIDs, including diclofenac sodium, in pregnant women at about 30 weeks gestation and later. NSAIDs including diclofenac sodium, increase the risk of premature closure of the fetal ductus arteriosus at approximately this gestational age.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs, including diclofenac sodium, at about 20 weeks gestation or later in pregnancy may cause fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. Oligohydramnios is often, but not always, reversible with treatment discontinuation. Complications of prolonged oligohydramnios may, for example, include limb contractures and delayed lung maturation. In some postmarketing cases of impaired neonatal renal function, invasive procedures such as exchange transfusion or dialysis were required.
If NSAID treatment is necessary between about 20 weeks and 30 weeks gestation, limit diclofenac sodium use to the lowest effective dose and shortest duration possible. Consider ultrasound monitoring of amniotic fluid if diclofenac sodium treatment extends beyond 48 hours. Discontinue diclofenac sodium if oligohydramnios occurs and follow up according to clinical practice (see PRECAUTIONS - Pregnancy).
Hematologic Toxicity
Anemia has occurred in NSAID-treated patients. This may be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis. If a patient treated with diclofenac sodium, has any signs or symptoms of anemia, monitor hemoglobin or hematocrit.
NSAIDs, including diclofenac sodium, may increase the risk of bleeding events. Co-morbid conditions such as coagulation disorders, concomitant use of warfarin, other anticoagulants, antiplatelet agents (e.g., aspirin), serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) may increase this risk. Monitor these patients for signs of bleeding (see PRECAUTIONS: Drug Interactions).
Risk of Methemoglobinemia
Cases of methemoglobinemia have been reported in association with lidocaine use. Although all patients are at risk for methemoglobinemia, patients with glucose-6- phosphate dehydrogenase deficiency, congenital or idiopathic methemoglobinemia, cardiac or pulmonary compromise, infants under 6 months of age, and concurrent exposure to oxidizing agents or their metabolites are more susceptible to developing the condition. If lidocaine must be used in these patients, close monitoring for symptoms and signs of methemoglobinemia is recommended. Signs of methemoglobinemia may occur immediately or may be delayed some hours after exposure and are characterized by a cyanotic skin discoloration and/or abnormal coloration of the blood.
Methemoglobin levels may continue to rise; therefore, immediate treatment is required to avert more serious central nervous system and cardiovascular adverse effects, including seizures, coma, arrhythmias, and death. Discontinue lidocaine and any other oxidizing agents. Depending on the severity of the signs and symptoms, patients may respond to supportive care, i.e., oxygen therapy, hydration. A more severe clinical presentation may require treatment with methylene blue, exchange transfusion, or hyperbaric oxygen.
Accidental Exposure in Children
Even a used Trifena™ patch contains a large amount of diclofenac sodium, lidocaine, and menthol. The potential exists for a small child or a pet to suffer serious adverse effects from chewing or ingesting a new or used Trifena™ patch, although the risk with this formulation has not been evaluated. It is important for patients to store and dispose of Trifena™ patch beyond the reach of children, pets and others (See HANDLING AND DISPOSAL) .
Excessive Dosing
Excessive dosage or short interval between doses can result in high plasma levels and serious adverse effects. Patients should be instructed to strictly adhere to the recommended dosage and administration guidelines set forth in this literature and on your prescription label. The management of serious adverse reactions may require the use of resuscitative equipment, oxygen or other resuscitative drugs.
Excessive dosing by applying Trifena™ patch to larger areas for longer than the recommended wearing time could result in increased absorption of diclofenac sodium, lidocaine, and menthol and high blood concentrations, leading to serious adverse effects.
Lidocaine toxicity could be expected at Lidocaine blood concentrations above 5 µg/mL. The blood concentration of Lidocaine is determined by the rate of systemic absorption and elimination. Longer duration of application, application of more than the recommended number of patches, smaller patients, or impaired elimination may all contribute to increasing the blood concentration of Lidocaine. With recommended dosing of Trifena™ patch the average blood concentration is about 0.13 µg/mL, but concentration higher than 0.25 µg/mL have been observed in some patients.
PRECAUTIONS
General
Trifena™ patch should be used with caution in patients with active gastrointestinal ulceration or bleeding and severe renal or hepatic impairments.
Trifena™ patch should not be applied to open skin wounds, infections, or exfoliative dermatitis.
Because of the possibility of sedation, patients should be cautioned regarding the use of heavy machinery or automobiles, also any activities made hazardous by decreased alertness.
Hepatic Effects
Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs including Trifena™ patch. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis and hepatic failure, some of them with fatal outcomes have been reported.
A patient with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, should be evaluated for evidence of the development of a more severe hepatic reaction while on therapy with Trifena™ patch. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), Trifena™ patch should be discontinued.
Hepatic Disease
Patients with severe hepatic disease are at greater risk of developing toxic blood concentrations of lidocaine, because of their inability to metabolize lidocaine normally.
Hematological Effects
Anemia is sometimes seen in patients receiving NSAIDs. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including Trifena™ patch, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia. NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible. Patients receiving Trifena™ patch who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants, should be carefully monitored.
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and other nonsteroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, Trifena™ patch should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
Allergic Reactions
Patients allergic to para-aminobenzoic acid derivatives (procaine, tetracaine, benzocaine, etc.) have not shown cross sensitivity to lidocaine. However, Trifena™ patch should be used with caution in patients with a history of drug sensitivities, especially if the etiologic agent is uncertain.
Non-intact Skin
Application to broken or inflamed skin, although not tested, may result in higher blood concentrations of lidocaine from increased absorption. Trifena™ patch is only recommended for use on intact skin.
External Heat Sources
Placement of external heat sources, such as heating pads or electric blankets, over Trifena™ patch is not recommended as this has not been evaluated and may increase plasma lidocaine levels.
Eye Exposure
The contact of Trifena™ patch with eyes, although not studied, should be avoided based on the findings of severe eye irritation with the use of similar products in animals. If eye contact occurs, immediately wash out the eye with water or saline and protect the eye until sensation returns. Consult a physician if irritation persists for more than an hour.
Information for Patients
Methemoglobinemia
Inform patients that use of local anesthetics may cause methemoglobinemia, a serious condition that must be treated promptly. Advise patients or caregivers to stop use and seek immediate medical attention if they or someone in their care experience the following signs or symptoms: pale, gray, or blue colored skin (cyanosis); headache; rapid heart rate; shortness of breath; lightheadedness; or fatigue.
NSAIDs
Patients should be informed of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. Patients should also be encouraged to read the NSAID Medication Guide that accompanies each prescription dispensed.
- Trifena™ patch, like other NSAIDs, may cause serious CV side effects, such as MI or stroke, which may result in hospitalization and even death. Although serious CV events can occur without warning symptoms, patients should be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and should ask for medical advice when observing any indicative sign or symptoms. Patients should be apprised of the importance of this follow-up (see WARNINGS – Risk of Serious Cardiovascular Events).
- Trifena™ patch, like other NSAIDs, may cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients should be alert for the signs and symptoms of ulcerations and bleeding, and should ask for medical advice when observing any indicative sign or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Patients should be apprised of the importance of this follow-up (see WARNINGS – Gastrointestinal Bleeding, Ulceration, and Perforation).
- Trifena™ patch, like other NSAIDs, may cause serious skin side effects such as exfoliative dermatitis, SJS, and TEN, which may result in hospitalizations and even death. Although serious skin reactions may occur without warning, patients should be alert for the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and should ask for medical advice when observing any indicative signs or symptoms. Patients should be advised to stop the drug immediately if they develop any type of rash and contact their physicians as soon as possible. (see WARNINGS - Serious Skin Reactions).
- Patients should be instructed to promptly report signs or symptoms of unexplained weight gain or edema to their physicians (see WARNINGS – Heart Failure and Edema).
- Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, patients should be instructed to stop therapy and seek immediate medical therapy.
- Patients should be informed of the signs of an anaphylactoid reaction (e.g. difficulty breathing, swelling of the face or throat). If these occur, patients should be instructed to seek immediate emergency help (see WARNINGS - Anaphylactic Reactions, PRECAUTIONS – Allergic Reactions, and ADVERSE REACTIONS – Allergic Reactions).
- In late pregnancy, as with other NSAIDs, Trifena™ patch should be avoided because it may cause premature closure of the ductus arteriosus.
- Patients should be advised not to use Trifena™ patch if they have an aspirin-sensitive asthma. Trifena™ patch, like other NSAIDs, could cause severe and even fatal bronchospasm in these patients (see WARNINGS: Exacerbation of Asthma Related to Aspirin Sensitivity). Patients should discontinue use of Trifena™ patch and should immediately seek emergency help if they experience wheezing or shortness of breath.
- Patients should be informed that Trifena™ patch should be used only on intact skin.
- Patients should be advised to avoid contact of Trifena™ patch with eyes and mucosa. Patients should be instructed that if eye contact occurs, they should immediately wash out the eye with water or saline, and consult a physician if irritation persists for more than an hour.
- Patients and caregivers should be instructed to wash their hands after applying, handling or removing the patch.
- Patients should be informed that, if Trifena™ patch begins to peel off, the edges of the patch may be taped down.
- Patients should be instructed not to wear Trifena™ patch during bathing or showering. Bathing should take place in between scheduled patch removal and application (see DOSAGE AND ADMINISTRATION).
- Patients should be advised to store Trifena™ patch and to discard used patches out of the reach of children and pets. If a child or pet accidentally ingests Trifena™ patch, medical help should be sought immediately (see WARNINGS – Accidental Exposure in Children, PRECAUTIONS - Accidental Exposure in Children).
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. Patients on long-term treatment with NSAIDs, should have their CBC and a chemistry profile checked periodically. If clinical signs and symptoms consistent with liver or renal disease develop, systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if abnormal liver tests persist or worsen, Trifena™ patch should be discontinued.
Drug Interactions
Specific interaction studies between Trifena™ patch and other topical or oral agents were not performed.
| Drugs That Interfere with Hemostasis | |
| Clinical Impact: |
|
| Intervention: | Monitor patients with concomitant use of diclofenac sodium with anticoagulants (e.g., warfarin), antiplatelet agents (e.g., aspirin), selective serotonin reuptake inhibitors (SSRIs), and serotonin norepinephrine reuptake inhibitors (SNRIs) for signs of bleeding [see WARNINGS - Gastrointestinal Bleeding, Ulceration, and Perforationand PRECAUTIONS – Hematological Effects]. |
| Aspirin | |
| Clinical Impact: | Controlled clinical studies showed that the concomitant use of NSAIDs and analgesic doses of aspirin does not produce any greater therapeutic effect than the use of NSAIDs alone. In a clinical study, the concomitant use of an NSAID and aspirin was associated with a significantly increased incidence of GI adverse reactions as compared to use of the NSAID alone [see WARNINGS - Gastrointestinal Bleeding, Ulceration, and Perforation]. |
| Intervention: | Concomitant use of diclofenac sodium and analgesic doses of aspirin is not generally recommended because of the increased risk of bleeding [see WARNINGS - Gastrointestinal Bleeding, Ulceration, and Perforation]. Diclofenac sodium is not a substitute for low dose aspirin for cardiovascular protection. |
| ACE Inhibitors, Angiotensin Receptor Blockers, and Beta-Blockers | |
| Clinical Impact: |
|
| Intervention: |
|
| Diuretics | |
| Clinical Impact: | Clinical studies, as well as post-marketing observations, showed that NSAIDs reduced the natriuretic effect of loop diuretics (e.g., furosemide) and thiazide diuretics in some patients. This effect has been attributed to the NSAID inhibition of renal prostaglandin synthesis. |
| Intervention: | During concomitant use of diclofenac sodium with diuretics, observe patients for signs of worsening renal function, in addition to assuring diuretic efficacy including antihypertensive effects [see WARNINGS – Renal Toxicity and Hyperkalemia]. |
| Digoxin | |
| Clinical Impact: | The concomitant use of diclofenac with digoxin has been reported to increase the serum concentration and prolong the half-life of digoxin. |
| Intervention: | During concomitant use of diclofenac sodium and digoxin, monitor serum digoxin levels. |
| Lithium | |
| Clinical Impact: | NSAIDs have produced elevations in plasma lithium levels and reductions in renal lithium clearance. The mean minimum lithium concentration increased 15%, and the renal clearance decreased by approximately 20%. This effect has been attributed to NSAID inhibition of renal prostaglandin synthesis. |
| Intervention: | During concomitant use of diclofenac sodium and lithium, monitor patients for signs of lithium toxicity. |
| Methotrexate | |
| Clinical Impact: | Concomitant use of NSAIDs and methotrexate may increase the risk for methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction). |
| Intervention: | During concomitant use of diclofenac sodium and methotrexate, monitor patients for methotrexate toxicity. |
| Cyclosporine | |
| Clinical Impact: | Concomitant use of diclofenac sodium and cyclosporine may increase cyclosporine's nephrotoxicity. |
| Intervention: | During concomitant use of diclofenac sodium and cyclosporine, monitor patients for signs of worsening renal function. |
| NSAIDs and Salicylates | |
| Clinical Impact: | Concomitant use of diclofenac with other NSAIDs or salicylates (e.g., diflunisal, salsalate) increases the risk of GI toxicity, with little or no increase in efficacy [see WARNINGS - Gastrointestinal Bleeding, Ulceration, and Perforation]. |
| Intervention: | The concomitant use of diclofenac with other NSAIDs or salicylates is not recommended.
Do not use combination therapy with diclofenac sodium and an oral NSAID unless the benefit outweighs the risk and conduct periodic laboratory evaluations. |
| Pemetrexed | |
| Clinical Impact: | Concomitant use of diclofenac sodium and pemetrexed may increase the risk of pemetrexed-associated myelosuppression, renal, and GI toxicity (see the pemetrexed prescribing information). |
| Intervention: | During concomitant use of diclofenac sodium and pemetrexed, in patients with renal impairment whose creatinine clearance ranges from 45 to 79 mL/min, monitor for myelosuppression, renal and GI toxicity. NSAIDs with short elimination half-lives (e.g., diclofenac, indomethacin) should be avoided for a period of two days before, the day of, and two days following administration of pemetrexed.
In the absence of data regarding potential interaction between pemetrexed and NSAIDs with longer half-lives (e.g., meloxicam, nabumetone), patients taking these NSAIDs should interrupt dosing for at least five days before, the day of, and two days following pemetrexed administration. |
Drugs That May Cause Methemoglobinemia When Used with Trifena™ Patch
Patients who are administered local anesthetics are at increased risk of developing methemoglobinemia when concurrently exposed to the following drugs, which could include other local anesthetics.
| Class | Examples |
|---|---|
| Nitrates/Nitrites | nitric oxide, nitroglycerin, nitroprusside, nitrous oxide |
| Local anesthetics | articaine, benzocaine, bupivacaine, lidocaine, mepivacaine, prilocaine, procaine, ropivacaine, tetracaine |
| Antineoplastic agents | cyclophosphamide, flutamide, hydroxyurea, ifosfamide, rasburicase |
| Antibiotics | dapsone, nitrofurantoin, para-aminosalicylic acid, sulfonamides |
| Antimalarials | chloroquine, primaquine |
| Anticonvulsants | phenobarbital, phenytoin, sodium valproate |
| Other drugs | acetaminophen, metoclopramide, quinine, sulfasalazine |
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of Trifena™ patch.
Carcinogenicity studies in mice and rats administered diclofenac sodium as a dietary constituent for 2 years resulted in no significant increases in tumor incidence at doses up to 2 mg/kg/day approximately 0.53 and 1.04 times, respectively, the maximum recommended human topical dose of diclofenac sodium 1.2% (based on apparent bioavailability and body surface area comparison).
In a dermal carcinogenicity study conducted in albino mice, daily topical applications of diclofenac sodium for two years at concentrations up to 0.035% diclofenac sodium (a 34-fold lower diclofenac sodium concentration than present in diclofenac sodium, 1.2%) did not increase neoplasm incidence.
In a photococarcinogenicity study conducted in hairless mice, topical application of diclofenac sodium at doses up to 0.035% diclofenac sodium (a 34-fold lower diclofenac sodium concentration than present in diclofenac sodium, 1.2%) resulted in an earlier median time of onset of tumors.
A minor metabolite, 2,6-xylidine, has been found to be carcinogenic in rats. The blood concentration of this metabolite is negligible following application of lidocaine patch 5%.
Mutagenesis
Diclofenac was not mutagenic or clastogenic in a battery of genotoxicity tests that included the bacterial reverse mutation assay, in vitro mouse lymphoma point mutation assay, chromosomal aberration studies in Chinese hamster ovarian cells in vitro, and in vivo rat chromosomal aberration assay of bone marrow cells.
Lidocaine HCl is not mutagenic in Salmonella/mammalian microsome test nor clastogenic in chromosome aberration assay with human lymphocytes and mouse micronucleus test.
Impairment of Fertility
The effect of Trifena™ patch on fertility has not been studied.
Fertility studies have not been conducted with diclofenac sodium topical solution. Diclofenac sodium administered to male and female rats at doses up to 4 mg/kg/day (approximately 2.08 times the MRHD of diclofenac sodium 1.2% based on apparent bioavailability and body surface area comparison) did not affect fertility.
Pregnancy
Risk Summary
Use of NSAIDs, including diclofenac sodium, during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including diclofenac sodium, in pregnant women starting at 30 weeks of gestation (third trimester).
There are no adequate and well-controlled studies of diclofenac sodium in pregnant women. Data from observational studies regarding potential embryofetal risks of NSAID use in women in the first or second trimesters of pregnancy are inconclusive. In the general U.S. population, all clinically recognized pregnancies, regardless of drug exposure, have a background rate of 2 to 4% for major malformations, and 15 to 20% for pregnancy loss. In animal reproduction studies, no evidence of teratogenicity was observed in mice, rats, or rabbits given diclofenac during the period of organogenesis at doses up to approximately 0.6, 0.6, and 1.3 times, respectively, the maximum recommended human dose (MRHD) of diclofenac sodium topical solution, despite the presence of maternal and fetal toxicity at these doses [see Data]. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as diclofenac resulted in increased pre- and post-implantation loss.
Labor and Delivery
Trifena™ patch has not been studied in labor and delivery.
Clinical Considerations
In rat studies with NSAIDs, as with other drugs known to inhibit prostaglandin synthesis, an increased incidence of dystocia, delayed parturition, and decreased pup survival occurred. The effects of Trifena™ patch on labor and delivery in pregnant women are unknown.
Data
Animal data
Reproductive and developmental studies in animals demonstrated that diclofenac sodium administration during organogenesis did not produce teratogenicity despite the induction of maternal toxicity and fetal toxicity in mice at oral doses up to 20 mg/kg/day (approximately 0.6 times the maximum recommended human dose [MRHD] of diclofenac sodium, 162 mg/day, based on body surface area (BSA) comparison), and in rats and rabbits at oral doses up to 10 mg/kg/day (approximately 0.6 and 1.3-times, respectively, the MRHD based on BSA comparison). In rats, maternally toxic doses of diclofenac were associated with dystocia, prolonged gestation, reduced fetal weights and growth, and reduced fetal survival.
Lidocaine patch 5% has not been studied in labor and delivery. Lidocaine is not contraindicated in labor and delivery. Should lidocaine patch 5% be used concomitantly with other products containing lidocaine, total doses contributed by all formulations must be considered.
Nursing Mothers
Trifena™ patch has not been studied in nursing mothers.
Risk Summary
Based on available data, diclofenac may be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for diclofenac sodium and any potential adverse effects on the breastfed infant from the diclofenac sodium or from the underlying maternal condition.
Data
One woman treated orally with a diclofenac salt, 150 mg/day, had a milk diclofenac level of 100 mcg/L, equivalent to an infant dose of about 0.03 mg/kg/day. Diclofenac was not detectable in breast milk in 12 women using diclofenac (after either 100 mg/day orally for 7 days or a single 50 mg intramuscular dose administered in the immediate postpartum period).
Lidocaine patch 5% has not been studied in nursing mothers. Lidocaine is excreted in human milk, and the milk:plasma ratio of lidocaine is 0.4. Caution should be exercised when lidocaine patch 5% is administered to a nursing woman.
Geriatric Use
Reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, start dosing at the low end of the dosing range, and monitor patients for adverse effects (see WARNINGSand PRECAUTIONS).
Of the 911 patients treated with diclofenac sodium topical solution 1.5% in seven controlled, Phase 3 clinical trials, 444 subjects were 65 years of age and over. There was no age-related difference in the incidence of adverse events. Of the 793 patients treated with diclofenac sodium 1.5% in one open-labeled safety trial, 334 subjects were 65 years of age and over including 107 subjects 75 and over. There was no difference in the incidence of adverse events with long-term exposure to diclofenac sodium 1.5% for this elderly population.
ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Thrombotic Events (see WARNINGS - Risk of Serious Cardiovascular Events).
- GI Bleeding, Ulceration, and Perforation (see WARNINGS - Gastrointestinal Bleeding, Ulceration, and Perforation).
- Hepatotoxicity [see WARNINGS – Hepatotoxicity, and PRECAUTIONS].
- Hypertension [see WARNINGS - Hypertension].
- Heart Failure and Edema [see WARNINGS - Heart Failure and Edema]
- Renal Toxicity and Hyperkalemia [see WARNINGS – Renal Toxicity and Hyperkalemia].
- Anaphylactic Reactions [see Contraindications, WARNINGS – Anaphylactic Reactions, and PRECAUTIONS – Allergic Reactions, ADVERSE REACTIONS – Allergic Reactions].
- Serious Skin Reactions [see WARNINGS – Serious Skin Reactions].
- Hematologic Toxicity [see WARNINGS – Hematological Toxicity, PRECAUTIONS – Hematological Effects].
Application Site Reactions
The most common adverse reactions occur at the application site, including dermatitis, itching or scaling. These tend to be dose--‐limiting and diminish with time.
Serious adverse experiences following the administration of Trifena™ patch are similar in nature to those observed in other amide anesthetic--‐containing agents. These adverse experiences are, in general, dose--‐related and may result from high plasma levels caused by excessive dosage, rapid absorption, or may result from hypersensitivity, idiosyncrasy, or a diminished tolerance on the part of the patient. Serious adverse experiences are generally systemic in nature.
During or immediately after treatment with Trifena™ patch, the skin at the site of application may develop blisters, bruising, burning sensation, depigmentation, dermatitis, discoloration, edema, erythema, exfoliation, irritation, papules, petechia, pruritus, vesicles, or may be the locus of abnormal sensation. These reactions are generally mild and transient, resolving spontaneously within a few minutes to hours.
Allergic Reactions
Allergic and anaphylactoid reactions associated with lidocaine, although rare, can occur. They are characterized by angioedema, bronchospasm, dermatitis, dyspnea, hypersensitivity, laryngospasm, pruritus, shock, and urticaria. If they occur, consult your doctor.
Other Adverse Events
Due to the nature and limitation of spontaneous reports in post marketing surveillance, causality has not been established for additional reported adverse events including:
Asthenia, confusion, disorientation, dizziness, headache, hyperesthesia, hypoesthesia, lightheadedness, metallic taste, nausea, nervousness, pain exacerbated, paresthesia, somnolence, taste alteration, vomiting, visual disturbances such as blurred vision, flushing, tinnitus, and tremor.
Systemic (Dose-Related) Reactions
Systemic adverse reactions following appropriate use of Trifena™ patch are unlikely, due to the small dose absorbed (see CLINICAL PHARMACOLOGY, Pharmacokinetics - Absorption). Systemic adverse effects of lidocaine is similar in nature to those observed with other amide local anesthetic agents, including CNS excitation and/or depression (light headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensations of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression and arrest). Excitatory CNS reactions may be brief or not occur at all, in which case the first manifestation may be drowsiness merging into unconsciousness. Cardiovascular manifestations may include bradycardia, hypotension and cardiovascular collapse leading to arrest.
To report SUSPECTED ADVERSE REACTIONS, contact Trifluent Pharma at (210) 944-6920 or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch for voluntary reporting of adverse reactions
OVERDOSAGE
Symptoms following acute NSAID overdosages have been typically limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which have been generally reversible with supportive care. Gastrointestinal bleeding has occurred. Hypertension, acute renal failure, respiratory depression, and coma have occurred but were rare. (see WARNINGSand PRECAUTIONS) .
Manage patients with symptomatic and supportive care following an NSAID overdosage. There are no specific antidotes. Consider activated charcoal (60 to 100 grams in adults, 1 to 2 grams per kg of body weight in pediatric patients) and/or osmotic cathartic in symptomatic patients seen within four hours of ingestion or in patients with a large overdosage (5 to 10 times the recommended dosage).
Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
Lidocaine overdose from cutaneous absorption is rare but could occur. Excessive dosing by applying Trifena™ patch to larger areas could result in increased absorption of lidocaine and high blood concentrations, leading to serious adverse effects (see ADVERSE REACTIONS, Systemic (Dose-Related) Reactions). Longer duration of application of more than the recommended number of doses, smaller patients, or impaired elimination may all contribute to increased blood concentration of lidocaine. Due to the low systemic absorption of topically-applied diclofenac sodium, overdosage of diclofenac sodium is unlikely.
For additional information about overdosage treatment, contact a poison control center (1-800-222-1222).
DOSAGE AND ADMINSTRATION
Apply Trifena™ patch to intact skin to cover the most painful area. Clean and dry the affected area. Apply product directly to your skin, up to 2 times daily. Trifena™ patch should not be worn for longer than 12 hours per application. Clothing may be worn over the area of application. Patches may be cut into smaller sizes with scissors prior to removal of the protective film. Smaller areas of treatment are recommended in a debilitated patient, or a patient with impaired elimination.
If irritation or a burning sensation occurs during application, wash the product off your skin and do not reapply until the irritation subsides.
When Trifena™ patch is used concomitantly with other products containing local anesthetic agents, the amount absorbed from all formulations must be considered.
HANDLING AND DISPOSAL
Hands should be washed after the handling of Trifena™ patch, and eye contact with Trifena™ patch should be avoided. Store in a cool, dry place. Do not store patch outside of the sealed pouch bag. Fold used patches so the adhesive side sticks to itself, then safely discard used patches where children and pets cannot access them.
Trifena™ PATCH SHOULD BE KEPT OUT OF THE REACH OF CHILDREN.
HOW SUPPLIED
Trifena™ patch is available as the following:
15 patches individually wrapped in a re-sealable pouch.
NDC: 73352-568-15
Manufactured for:
Trifluent Pharma, LLC
San Antonio, TX 78213
For more information, contact Trifluent Pharma at 210-944-6920 and visit https://trifenapatches.com/
Rev 01 11/2024
Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:
-
Increased risk of a heart attack or stroke that can lead to death.This risk may happen early in treatment and may increase:
- with increasing doses of NSAIDs
- with longer use of NSAIDs
Do not take NSAIDs right before or after a heart surgery called a "coronary artery bypass graft (CABG)."
Avoid taking NSAIDs after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack.
-
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
- anytime during use
- without warning symptoms
- that may cause death
The risk of getting an ulcer or bleeding increases with:
- past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs
- taking medicines called "corticosteroids", "anticoagulants", "SSRIs", or "SNRIs"
|
|
NSAIDs should only be used:
- exactly as prescribed
- at the lowest dose possible for your treatment
- for the shortest time needed
What are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain.
Who should not take NSAIDs?
Do not take NSAIDS:
- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs.
- right before or after heart bypass surgery.
Before taking NSAIDs, tell your health care provider about all of your medical conditions, including if you:
- have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant. Taking NSAIDs at about 20 weeks of pregnancy or later may harm your unborn baby. If you need to take NSAIDs for more than 2 days when you are between 20 and 30 weeks of pregnancy, you healthcare provider may need to monitor the amount of fluid in your womb around your baby. You should not take NSAIDs after 20 weeks of pregnancy.
- are breastfeeding or plan to breast feed.
Tell your health care provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements. NSAIDs and some other medicines can interact with each other and cause serious side effects. Do not start taking new medicine without talking to your health care provider first.
What are the possible side effects of NSAIDs? NSAIDs can cause serious side effects, including:
See "
What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?"
- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting and dizziness.
Get emergency help right away if you get any of the following symptoms:
- shortness of breath or trouble breathing
- chest pain
- weakness in one part or side of your body
- slurred speech
- swelling of the face or throat
Stop taking your NSAID and call your health care provider right away if you get any of the following symptoms:
- nausea
- more tired or weaker than usual
- diarrhea
- itching
- your skin or eyes look yellow
- indigestion or stomach pain
- flu-like symptoms
- vomit blood
- there is blood in your bowel movement or it is black and sticky like tar
- unusual weight gain
- skin rash or blisters with fever
- swelling of the arms, legs, hands, and feet
If you take too much of your NSAID, call your health care provider or get medical help right away.
These are not all the possible side effects of NSAIDs. For more information, ask your health care provider or pharmacist about NSAIDs.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Other information about NSAIDs
- Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.
Manufactured for:
Trifluent Pharma
San Antonio, TX 78213
For more information, call (210) 944-6920
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised: 11/2024
| TRIFENA
diclofenac, lidocaine, menthol patch |
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
| Labeler - Trifluent Pharma LLC (117167281) |
Trademark Results [Trifena]
Mark Image Registration | Serial | Company Trademark Application Date |
|---|---|
 TRIFENA 78052893 not registered Dead/Abandoned |
POSITIVE BIOTECH INC. 2001-03-13 |
© 2026 FDA.report
This site is not affiliated with or endorsed by the FDA.
